Abstract
In the article we review the current role of diffusion tensor imaging (DTI), a modern magnetic resonance (MR) technique, in the diagnosis and the management of cervical spondylotic myelopathy (CSM), the most serious complication of degenerative cervical spine disease (DCSD). The pathogenesis of DCSD is presented first with an emphasis placed on the pathological processes leading to myelopathy development. An understanding of the pathophysiological background of DCSD is necessary for appropriate interpretation of MR images, both plain and DTI. Conventional MRI is currently the imaging modality of choice in DCSD and provides useful information concerning the extent of spondylotic changes and degree of central spinal canal stenosis; however its capability in myelopathy detection is limited. DTI is a state of the art imaging method which recently has emerged in spinal cord investigations and has the potential to detect microscopic alterations which are beyond the capability of plain MRI. In the article we present the physical principles underlying DTI which determine its sensitivity, followed by an overview of technical aspects of DTI acquisition with a special consideration of spinal cord imaging. Finally, the scientific reports concerning DTI utility in DSCD are also reviewed. DTI detects spinal cord injury in the course of DCSD earlier than any other method and could be useful in predicting surgical outcomes in CMS patients, however technical and methodology improvement as well as standardization of acquisition protocols and postprocessing methods among the imaging centers are needed before its implementation in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative cervical spine disease (DCSD), often referred to as cervical spondylosis, is a common disorder, affecting up to two-third of the population during one’s lifetime [1]. While often benign and moderately troublesome in nature, in a small percentage of patients it may result in the severe syndrome of spinal cord dysfunction known as cervical spondylotic myelopathy (CSM) [2, 3]. CSM is the most common nontraumatic cause of spinal cord pathology and impaired function [4]. Although magnetic resonance imaging (MRI) is the modality of choice for quantifying the extent of spondylotic alterations, it is characterized by low sensitivity in myelopathy detection, ranging according to different sources from 15 to 65 % [3, 5–8]. These divergences between conventional anatomical MR findings and clinical manifestation stimulate the search for new, more accurate methods of myelopathy evaluation.
Diffusion tensor imaging (DTI) is a novel MR technique which allows for in vivo evaluation of water molecules movements in directionally dependent tissues such as nervous tissue of the spinal cord. The information essential to create DTI images is derived from the cellular level, which makes this method sensitive to microstructure alterations and therefore even minor spinal cord tissue injury. Despite the impressive number of scientific reports confirming DTI utility in detecting subtle damage to the CNS tissue, both in the brain and spinal cord, this method is still not widely used in a clinical setting.
The aim of this review is to explore and discuss the current trends and possibilities in DTI evaluation of the CMS in the course of DCSD. For a more thorough understanding, the pathophysiology of DCSD as well as the basic principles of diffusion tensor imaging in the spinal cord domain are presented.
Degenerative Cervical Spine Disease: Mechanism and Pathophysiology
DCSD represents a mixed group of pathologies involving all parts of the so-called disco-vertebral unit, a functional unit of the spine, which comprises the intervertebral disc, adjacent vertebral bodies, facet joints, uncovertebral joints, ligamenta flava, and longitudinal ligaments at the given level [9–11]. Although spondylosis may affect only a single motion segment or predominantly one structure of the spine (e.g., facet joints in a process called spondyloarthrosis), multi-level and comprehensive spinal segment involvement is most frequently encountered. The lower part of the cervical spine (C4–C7) is most commonly involved [9]. The degenerative process usually proceeds in a certain pattern, as a cascade of related events, starting with a narrowing of the intervertebral disc due to the progressive loss of water content and disc herniation. Subsequent segmental instability places increased stress on adjacent vertebral endplates, facet, and uncovertebral joints stimulating osteophyte formation as a compensation for spine hypermobility secondary to disc degeneration [4]. The hypertrophy of the posterior longitudinal ligament and ligamenta flava often coexists. A special form of degenerative changes is the ossification of the posterior longitudinal ligament (OPLL), a condition most commonly encountered in Asian populations [12]. All these degenerative alterations may contribute to spinal stenosis, that is narrowing of the central canal and/or neural foramina lateral recess.
In contrast to the lumbar spine, which houses only a small part of the spinal cord, obliteration of the cervical spinal canal can far more frequently lead to a direct compromise of the spinal cord, resulting in its injury and a syndrome of severe neurological deficits called myelopathy. The pathophysiology of cervical spondylotic myelopathy is multifactorial [13], involving not only static (structural stenosis), but also dynamic and biologic factors [13–15]. As already mentioned above, spondylotic changes may lead to acquired canal stenosis which can be facilitated by the preexisting congenitally narrow spinal canal [10, 13, 16]. During the movement, the canal diameter is further reduced by 2–3 mm in flexion with the SC stretching over the posterior vertebral spurs, while extension can cause inward buckling of the ligamenta flava and dorsal compression [15]. These effects of functional (dynamic) stenosis appear to play a major role in CSM development. Transition and angulation between vertebral bodies in flexion—extension can also transiently narrow the spinal canal [13]. Frequently MR images of the cervical spine in a neutral position show no spinal cord involvement whereas kinematic examination reveals SC impingement from spondylotic spurs or intervertebral disc bulging/herniation occurring only during the movement [17].
Both chronic and intermittent compression of the SC contributes to myelopathy development through two basic, usually concurrent, mechanisms: direct trauma and ischemia. Considerable evidence exists to support ischemia as a major pathologic event [4, 13]. The reduction in SC blood flow occurs when degenerative elements compress arterial and/or venous blood vessels that supply the cervical spinal cord [4]. On a cellular level, ischemia triggers a biomolecular cascade ending with cells apoptosis [13, 18]. According to cadaveric studies of patients with CSM there is a common pattern of lesion progression in diseased SC [19, 20]. Atrophy and neuronal loss starts in the anterior horn and intermediate zone of the gray matter (GM), supplied by transverse arterioles which originate from the anterior sulcal arteries and are very susceptible to tension [21]. Next, the degeneration of lateral and posterior funiculus of the white matter (WM) precedes, at the beginning manifesting as demyelination. This can be explained by particular sensitivity of oligodendrocytes (the myelinating cells of the central nervous system) to ischemic injury [13, 22]. Oligodendrocytes’ apoptosis was found to precede the axonal degeneration in myelopathy [13]. Corticospinal tracts are particularly vulnerable to negative effects of compression, and undergo early demyelination in the course of CSM [15, 23–25]. Eventually, marked atrophy develops throughout the entire gray matter and severe degeneration occurs in the lateral funiculus [19]. Degeneration of the medial portions of the posterior columns is usually not noted until severe SC compression occurs, while relative preservation of anterior columns can be observed (Fig. 1c).
Magnetic resonance T2-weighted images in sagittal (a) and axial (b) planes. Multilevel degenerative cervical spine disease with severe central canal stenosis. Spinal cord is compressed and subtle hyperintense signal indicative of myelopathy is noted at the C3–4 level. c A schematic diagram of the cervical spinal cord cross section: a posterior funiculi, b lateral funiculus, c anterior funiculi, d ventral horn, e intermediate zone, f posterior horn. In the course of myelopathy, neuronal degeneration starts in the anterior horn and intermediate zone of the gray matter, followed by demyelination of lateral and posterior funiculi of the white matter
Conventional Anatomical MRI in DCSD
Unlike pathomorphological findings, which closely correlate with the clinical manifestation and myelopathy duration [10], the relationship between MR presentation and actual SC condition is often not that obvious. Conventional MR examination provides useful anatomical information concerning the extent of spondylotic changes and degree of central spinal canal stenosis [2], although its specificity is hampered by the high rate of degenerative changes found in asymptomatic individuals [26–28]. As for the SC, conventional anatomical MRI allows for the quantitative assessment of the degree of SC compression as well as for the evaluation of intramedullary signal intensity changes (Fig. 1a, b). AP compression ratio (AP diameter/transverse diameter of the SC) is the parameter often used for the assessment of SC involvement and according to pathomorphological studies the critical degree of AP compression ratio to induce histopathological changes in the SC was estimated as 30 % [29]. MR signal intensity changes within the SC, which are sometimes visible in the course of DCSD, are thought to represent structural lesions of the injured spinal cord. Intramedullary hyperintensity on T2-weighted images was related to edema, vascular stasis, ischemia, Wallerian degeneration, and gliosis [20]. Less frequently encountered hypointensity on T1-weighted images is thought to represent a more advanced phase of degeneration, such as cystic necrosis, spongiform changes, and cavitation [20]. In a recent comprehensive literature review, Vedantam et al. [30] established that a sharp and intense intramedullary T2 signal was associated with a poorer surgical outcome and thus is indicative of more severe myelopathy, in opposition to a fuzzy-bordered and/or faint T2 signal which is thought to represent a less advanced stage of degeneration with better prognosis [20]. Coexistence of high signal intensity on T2 images and low signal intensity on T1 images has the most (universally) poor prognosis [20]. Still, in many cases, the relationship between MR signal abnormalities and their clinical and prognostic significance is not straightforward [5, 6, 31–34].
DTI–the Basic Principles
DTI is an advanced magnetic resonance technique which in opposition to conventional MR images provides more functional than anatomical information about the examined tissues. At the cellular level of the human body water particles move continuously, propelled by their own thermal energy. This movement, called diffusion, is impeded and directed due to the presence of tissue components, mainly cell membranes. Both diffusion MR techniques—diffusion weighted imaging (DWI) and DTI—arise from the powerful concept that during diffusion-driven displacement, water molecules probe tissue structure on a microscopic scale [35]. Continuing with this idea, any disturbance in cellular environment would alter water diffusion and could be detected in MR diffusion study, which makes this technique a very sensitive diagnostic tool. Whereas DWI simply reflects the magnitude of diffusion within the voxel volume of tissue, DTI provides additional information concerning water molecules directionality. The two main parameters derived from DTI data are: (1) mean diffusivity (MD), which is approximately equal to mean apparent diffusion coefficient (ADC) used in DWI and (2) fractional anisotropy (FA), which reflects the degree of directionality of water molecules motion and vary between 0 (for isotropic diffusion—equal in all directions, e.g., within fluid spaces) and 1 (diffusion occurring in only one direction—complete anisotropic diffusion). In tissues with a preferred orientation whose structure is highly organized, such as the central nervous system (CNS) white matter, water molecules motion occurs predominantly in one direction, along the long axis of the fibers (Fig. 2). Anisotropy originates from the specific organization as densely packed bundles of axonal fibers running in parallel [35]. Diffusion perpendicular to fiber orientation is restricted due to the presence of axonal membranes as well as well-aligned protein fibers within an axon body [36]. One of the most unique features of diffusion MR measurements is that it detects water motion only along the applied gradient axis [37]. As a result, to fully appreciate diffusion characteristics of directionally dependent tissues, diffusion would have to be measured along a high number of directions which would be unfeasible in a clinical setting. To simplify this issue, the concept of diffusion tensor was introduced [37]. In this model measurements along different axes are fitted to a three-dimensional (3D) ellipsoid, separate for each voxel. An ellipsoid is a 3D representation of the diffusion distance covered in voxel volume by molecules in a given diffusion time [35]. To obtain six parameters necessary to create a diffusion ellipsoid (three eigenvalues ƛ1, ƛ2, ƛ3 representing respectively the longest, middle, and the shortest axes, and three eigenvectors V1, V2, V3 reflecting the axes’ orientation) at least six direction measurements are necessary. The large number of directions improves the quality and reliability of DTI examination. However, it also results in scanning time prolongation. According to our experience, 15 non-collinear, diffusion gradient directions are optimal for the examination of the cylindrical-shaped spinal cord [38]. Lee et al. [39] in a study investigating the influence of different acquisition parameters on tractography reconstruction, concluded that 15 diffusion-encoding gradient directions are sufficient for cervical spinal cord tractography and ensure optimal tractography reconstruction quality. In the clinical setting, the application of 15 encoding directions in DTI studies of the cervical SC is a reasonable compromise between acquisition time and resulting image quality.
The diffusion ellipsoids for isotropic (left) and anisotropic (right) diffusion. Water molecules in the human body are constantly moving (i.e., in Brownian motion) which is illustrated in the picture by a red line. When motion is unconstrained diffusion is isotropic, which means that motion occurs equally and randomly in all directions (sphere on the left). When motion is constrained, as in white-matter tracts (illustrated on the right), diffusion is anisotropic, meaning that motion is oriented more in one direction than another
Information which can be derived from a diffusion tensor model includes: mean diffusivity (MD) which is in fact an average ellipsoid size eigenvalue (MD = (ƛ1 + ƛ2,+ ƛ3)/3), the degree of anisotropy (FA) reflected by ellipsoid eccentricity and the main direction of diffusivities (vector of the longest ellipsoid axes) which indicates the fiber orientation [35, 37]. The indices mentioned above change in the presence of diffusion disturbances caused by pathological processes.
While attempting to connect MR diffusion study observation to the underlying anatomy one must remember that microscopic information is averaged over the large (2–5 mm) voxel volume. This is important, as changes in diffusion anisotropy sometimes resulted not from microscopic alterations such as demyelination, but from the macroscopic reorganization of axons [37]. Because the SC contains uniformly oriented pathways, some of the complexities of interpretation relevant in the brain like the “powder averaging” effect of crossing fibers can be obviated [40]. In opposition to brain investigations, the major difficulty in spinal cord DTI studies lies not in the limitation of diffusion methodology, but in the technical details of diffusion-weighted imaging and pulse sequence used [40]. By inserting an additional pair of gradients equal in magnitude but opposite in direction, any MRI sequence can be sensitized to water molecules diffusion. In practice, single-shot echo-planar imaging (ss-EPI) is the most commonly used and found to be indispensable in brain investigations. ss-EPI acquires the whole of k-space after a single excitation and this robustness is crucial for diffusion techniques that are particularly sensitive to subject motion. However, ss-EPI was found to be of limited usefulness in the SC [41, 42]. The anatomy of the spine as well as the abundance of susceptibility variations make it particular difficult to obtain high-quality ss-EPI images of the spinal cord. The SC is surrounded by flowing cerebrospinal fluid (CSF) and is adjacent to moving structures in the thorax and abdomen; the adjacent bony structure of the vertebral column causes magnetic susceptibility artifacts. At the same time a small cross section of the SC requires high-resolution imaging to obtain meaningful information [41]. Standard single-shot EPI offers limited spatial resolution and signal-to-noise ratio (SNR) and is particularly sensitive to motion and magnetic susceptibility variations [41]. Several modifications to EPI sequence which aim to overcome these limitations have been proposed, including interleaved [43–45] and parallel EPI [46–48] approaches as well as reduced field of view (rFOV) acquisition [49–54]. Interleaved EPI (IEPI) is based on multi-shot imaging, where k-space is split into several acquisitions with multiple EPI interleaves in the phase-encoding (PE) direction. IEPI reduces the off-resonance induced distortions proportionally to the number of interleaves and leads to an SNR improvement [55]. The trade-off for using a multi-shot EPI is that the segmentation of k-space not only increases the scan time compared with ss-EPI but also results in phase error discontinuities which require correction by means of navigator echoes, which further increases the scan time [56]. Despite the use of navigators, significant patient motion between the acquisition of different interleaves leads to ghosting artifacts or even can cause gaps in k-space, resulting in aliasing artifacts [56]. An alternative multi-shot approach that is less prone to motion is readout-segmented EPI (RS-EPI), which covers k-space with series of consecutive segments [56]. In RS-EPI, each segment acquires a full-FOV image that is largely motion-free and the correction for motion is required only between segments [56].
Another way to mitigate the shortcomings of ss-EPI is parallel imaging [57, 58] based on specialized imaging coils. Parallel imaging methods provide acceleration in k-space by utilizing the complementary spatial encoding information from multiple receiver coil elements to reduce the number of acquired k-space lines [47, 59]. Combining parallel imaging with EPI provides the advantages of a multi-shot EPI without the need of multi-shot although potentially compromises the SNR [55]. The sequence that can provide the SNR enhancement while maintaining the advantages of parallel EPI was recently proposed by Nana et al. [55]. The authors demonstrated that it is possible to increase the SNR with the use of an appropriate echo combination strategy and this SNR gain can be further used to reduce the number of measurements needed or to improve the image resolution.
More recently, methods aimed at reducing the effective FOV have been proposed for high-resolution EPI images of the spinal cord [51, 52, 54, 60]. The morphology of the spinal cord, particularly its small cross sectional size, is suitable for the reduced FOV approach. The key idea with reduced FOV is similar to parallel imaging [61]. By restricting the FOV in the PE direction fewer k-space lines are needed for a given image resolution which enables ss-EPI with shorter readout duration, leading to a reduction of susceptibility artifacts [61, 62]. As expected, the SNR is also reduced by the square root of that of the full FOV [56, 61]. Reduced FOV acquisition may be based on outer volume suppression or inner volume excitation. Most reduced-FOV methods use additional radiofrequency (RF) pulses to suppress or dephase the signal intensity from tissues outside the desired FOV [60, 62]. One such method called ZOOM-EPI (zonally magnified, oblique, multislice EPI) [50] combines a regular 90° excitation pulse with an obliquely applied 180° refocusing pulse [62]. Only the inner volume that experiences both pulses contributes to the signal readout [60]. The main limitation of this sequence is that it cannot be used to acquire contiguous slices, because the two regions excited by the two pulses overlap with adjacent sections [60]. In the modified version of ZOOM-EPI called contiguous-slice ZOOM-EPI (CO-ZOOM-EPI) [53], there is no necessity for the interslice gaps. CO-ZOOM-EPI uses two 180° refocusing pulses that are selective in the phase-encoding direction to readout a rectangular FOV, while simultaneously suppressing the signal arising from outside the desired FOV [60, 61].
A fundamentally different approach to reduced-FOV imaging is to actively excite only the ROI by using a two-dimensional spatially selective echo-planar RF (2D-EPRF) excitation pulse [62]. This method enables contiguous multislice imaging and allows simultaneous suppression of signal from fat, which is important for EPI-based imaging [60, 61]. However, due to the periodic nature of the rFOV pulse [52] only a certain number of slices can be imaged simultaneously without affecting the signal level [62]. This is not an issue while acquiring the diffusion images of the spinal cord in the sagittal plane, nonetheless, for the axial imaging of the spinal cord, it is desirable to acquire as many slices as possible along the length of the spine, to avoid multiple acquisitions and long scan times [62]. Recently, some modifications to rFOV ss-EPI have been proposed, including Hadamard slice-encoding scheme [62] and improved 2DRF pulse design [60]. These can be used to significantly increase the number of contiguous sections while preserving the original method’s high-resolution imaging capabilities.
Several non-EPI approaches have been proposed as an alternative for acquiring high-quality diffusion images of the spinal cord. These include line scan diffusion imaging (LSDI) [63–66], fast-spin echo (FSE) [67], and propeller-based imaging [68–70]. Line scan imaging uses spin echo technique and consists of sequential single-shot acquisition of PE lines. It is relatively insensitive to magnetic field inhomogeneities, Eddy currents, and bulk motion and can provide rectangular FOV for SC imaging [61, 63, 71, 72]. However, the trade-off of line scan imaging acquisition schemes is the relatively prolonged acquisition time, and missing k-space lines in the presence of extensive motion [56]. FSE and turbo spin echo (TSE) are variations of rapid acquisition with relaxation enhancement (RARE) sequence which is a spin echo sequence with refocusing pulses after RF excitation to significantly decrease relaxation time. The RF refocusing yields signal decay with T2 rather than T2*, making this sequence less sensitive to off-resonance effects and eddy currents [73]. Some studies have demonstrated the benefits of FSE for imaging the human spinal cord with DTI [58, 74, 75]. However, despite potential advantages of FSE, the EPI technique is still preferable for DWI applications in the spinal cord [43]. In PROPELLER approach, k-space is acquired in small blade-shaped segments that are rotated about the origin of k-space with each excitation [61]. All readout trajectories are symmetric to the origin of k-space and are equivalent with respect to the reconstruction, hence this sequence is less prone to degradation by a single corrupted data [56]. The PROPELLER readout can be both a FSE train [68] or a short-axis EPI train [76].
Although most of the above described approaches were tested for DWI acquisition, diffusion tensor imaging inherently benefits from the advances in DWI techniques, as DWI images form the foundation for DTI [61]. A combination of the above mentioned methods can be used in order to add their benefits for reducing distortion [56]. For example, reduced FOV ss-EPI can be combined in a straightforward manner with parallel imaging and IEPI to reduce off-resonance artifacts and improve spatial resolution, though at the cost of longer scan time [60]. The retrospective correction methods can further reduce remaining artifacts and even compensate for some of the drawbacks of the reported new acquisition approaches [77].
High field (3T) MR units are considered to be a better tool for performing DTI studies due to the significant increase in SNR and therefore image quality [38, 42]. Interestingly, Rossi et al. [78], in a study comparing DTI results obtained from 1.5 and 3T MR units found comparable FA and MD values of normal WM at both field strengths. SNR can be also increased by multiplying number of excitations (NEX) although acquiring more distinct diffusion encoding directions, instead of repeated acquisitions, has become more widely used [79]. Further possible optimization for SC examination is decreased reconstruction matrix and smaller slice thickness compared to the brain DTI [38].
After acquisition, DTI data can be postprocessed either with the use of a workstation equipped with dedicated software—in our department is the GE Advantage Workstation 4.6 and Ready View program—or with software packages such as DTIStudio, MedINRIA, FSL, AFNI, etc. Typically, color-coded FA and MD (ADC) parametric maps were generated. For quantitative analysis of tensor data several approaches can be used: regions of interest (ROI) setting method, voxel-based method, histogram analysis, and tractography. Fiber tracking (DTT: diffusion tensor tractography), a 3D fiber tracts reconstruction, is undoubtedly the most spectacular way to present diffusion study results (Fig. 3). Using the data collected from DTI study and the special reconstruction algorithms, water molecules’ movement along the nervous fibers become the basis for 3D nervous bundles reconstruction. On such created images, the precise site of fiber displacement, interruption, or deformation resulting from any pathological process altering the diffusion can be visualized (Fig. 4). DTT is not the only visualization tool enabling macroscopic fiber tracts assessment. There are several software packages allowing for DTI values (FA and ADC) extraction from voxels within virtually reconstructed fibers, which creates an operator-independent alternative for ROI positioning method. By means of tractography, it is possible to extract specific nervous tract within the spinal cord and to obtain quantitative measurements along the reconstructed pathway. This enables correlation of the integrity of specific tracts with the severity of clinical deficit [80]. Before performing tractography, visual inspections of diffusion-weighted images as well as motion and susceptibility artifacts correction should be always performed, because of the possible prominent tractography reconstruction errors [81]. The obtained values of tensor metrics in the SC depend mainly on accurate segmentation of gray and white matter. Another crucial element of the analysis is the selection of appropriate fiber reconstruction algorithm. The three main fiber reconstruction methods include: streamline tracking technique (STT), tensor deflection technique (TEND), and probabilistic tractography. The main difference between tractography algorithms involves the technique in which artificial tracts utilize adjacent information to plan their next trajectory [36]. STT primarily utilizes information from the largest eigenvector to create tracts [36, 82]. TEND deflects the incoming eigenvector by the diffusion tensor orientation [83, 84], whereas in probabilistic approach, ADC is first measured in a large number of directions, every image voxel is considered a seed point for tract growth, and the most probable tract orientations are calculated [85]. In the spinal cord tractography similar reconstruction parameters to these optimized for descending or ascending pathways in the brain can be successfully used [86].
Diffusion tensor imaging (DTI) tractography presenting the disruption of the cervical spinal cord fibers in cervical spondylotic myelopathy patient. a Sagittal T2-weighted magnetic resonance imaging. b DTI tractography overlaid onto sagittal T2-weighted image. DTT tracts are color-coded to indicate tract orientation: red for left–right orientation, green for anterior–posterior orientation, and blue for superior–inferior orientation
Application of DTI in the Evaluation of Cervical Spondylotic Myelopathy—State of the Art
DTI was first introduced and widely used in brain investigations for a long time before it was applied to the SC, mainly due to technical conditions described above. The first reports about examination of the SC with the DTI technique were published in 1999 [67], and since then a great number of related articles have occurred. DTI utility has been investigated in numerous pathological states afflicting the SC, such as acute spinal injury, multiple sclerosis, neuromyelitis, amyotrophic lateral sclerosis, spinal cord ischemia, syringomyelia, neoplasms, and finally degenerative cervical spine disease [41, 87–92]. DCSP is definitely the most common entity from those mentioned above, providing a large field for scientific studies. Although spondylotic changes of the vertebral column as well as adjacent soft tissues (intervertebral disc and ligaments, etc.) abnormalities can be fully appreciated on conventional anatomical MRI images, nervous tissue (spinal cord and spinal nerves) involvement is often not that obvious. Especially as far as spinal cord myelopathy is concerned, there are often discrepancies between radiological findings and clinical manifestation. Abnormal T2 signal intensity of the compressed spinal cord, which is considered to reflect myelopathic changes, is not always present, even in very advanced stages of clinically evident myelopathy, and poorly correlates with disease severity [32, 92–96]. Conventional anatomical MRI sensitivity in myelopathy detection was estimated for 15–65 % [3, 5–8]. In a natural way, the DTI technique, which was proven to detect alterations in the course of disease even in normal appearing brain tissue, was implemented in SC myelopathy investigations.
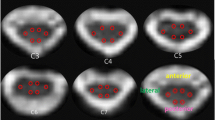
As already mentioned above, there are huge discrepancies between studies regarding technical aspects of SC DTI acquisition. How great an influence it has on the research results is only to mention that FA values significantly depend on the number of acquisitions and number of gradient directions used, as well as on the voxel size [97, 98]. Great differences are noticeable in diffusion measurements methodology as well. This is mostly visible when comparing DTI indices measured in healthy control groups. FA values range from 0.52 to 0.83 [92], and ADC from 0.781 to 1.14 × 10−3 mm2/s [8] in different studies, depending mostly on the measurements method used. Most authors set ROIs on transverse FA and ADC maps to obtain the results, however the localization and the size of ROIs vary. Researchers who placed ROIs predominantly in the SC white matter (WM) obtained higher FA and lower ADC values due to the almost one-directional organization of WM tracts. For some reasons, inclusion of an entire SC cross section surface for DTI measurements seems to be a reasonable approach. First of all, in the studies employing a 1.5T MR unit, it is difficult to distinguish between white and gray matter in diffusion images. This is also an issue in a heavily compressed SC, where white and gray matter are often indistinguishable, even in the diffusion images obtained from high-field MR units. As already mentioned above, myelopathic changes start within the gray matter, and then spread to the white matter of the spinal cord. Therefore, in order to detect early myelopathic changes, the SC gray matter should be included in the measurements. This results in averaging FA and ADC values of white and gray matter giving the relatively low FA value ranging from 0.58 to 0.55 at different cervical spinal cord levels in healthy patients [2]. Special attention during ROI setting needs to be paid to avoid partial volume effect of an adjacent CSF as CSF contamination may cause an overestimation of diffusion values and an underestimation of FA [41].
Another way to obtain DTI values is to extract them from tractography images. In opposition to ROI positioning, a DTI-FT-based approach is operator-independent and therefore provides more reliable results and an excellent inter-observer agreement. In a study performed by Budzik et al. [98] semi-automatic axial stratified analysis of FA and MD values was made. Investigators used 0.2 FA threshold for fiber reconstruction which resulted in incorporating gray matter into calculations giving relatively low values of FA ranging 0.42–0.59 for different SC levels. According to the study performed by Bosma and Stroman [99] which is highly referential, due to the k-means clustering method used for extracting white matter containing voxels, WM of the cervical spinal cord alone is characterized by an average 0.7 FA value. However, in the presence of pathology, WM FA often decreases below the average GM values (i.e., 0.45) [99] and therefore low threshold limit for DTT is necessary if we want to avoid excluding the voxels of the pathologically changed WM. This could be a limitation for DTI-FT-based method studies in case of diseases which predominantly affect SC WM.
Despite the methodology differences, all investigators report high DTI sensitivity in myelopathy detection, significantly exceeding the capability of conventional MR examination [8, 98, 100, 101]. Decrease of FA values with concomitant increase of ADC values were found in patients presenting clinical syndromes of myelopathy, but without T2-hyperintensity in conventional MR images [100, 101]. Moreover, statistically significant changes in DTI parameters were also reported in spondylotic patients in the presence of only slight SC compression [8] or even in cases without visible SC involvement in static MR examination [2]. The abovementioned results can be most probably related to dynamic factors that is physiological motion of the spine. During the movement, the spinal canal diameter is reduced by about 2–3 mm on flexion with the narrowing of the anterior space and anterior shifting of the cervical cord, which can be then be exposed to a so-called pincer effect. Furthermore, displacement of the spinal cord within the spinal canal, even without obvious spinal cord compression, may lead to abnormal tension patterns within the cord. This results in extracellular edema, which could cause the decrease of FA and increase of ADC values, as reported elsewhere in brain diseases [35]. There is also an interesting hypothesis raised, among others, by Xiangshui et al., concerning the influence of increased pressure of cerebrospinal fluid on the internal pressure of the spinal cord. Cerebrospinal fluid flow disturbances, resulting from degenerative changes both in static position and during movement, could increase the pressure around the spinal cord and, in turn, alter interstitial diffusion which would result in FA and ADC changes [8].
Although DTI metrics alterations in the absence of SC compression strongly support the hypothesis of remarkable DTI sensitivity, the clinical significance of these findings is borderline. Degenerative changes of the spine are to some extent a natural, age-related phenomena, almost universally present by the time of Late Middle Ages and affecting more than 80 % of patients over 60 years without producing any symptoms [27]. This is in someway consistent with the study results of Mamata et al. [102], who found that FA decreases and ADC increases with age in the normal SC of healthy population. To conclude, DTI parameter changes do not necessarily indicate major SC pathology, especially in the elderly.
In more advanced stages of chronic degenerative stenosis with obvious SC involvement, FA and ADC alterations could be related to mechanical disruption that is, tearing of fibers and myelin sheaths and to the consequences of ischemia: Wallerian degeneration, demyelination, liquefaction, cystic degeneration, and neuronal death [92]. A decreased number of fibers and loss of their directional organization lead to the expansion of extracellular space with water molecules moving more freely, which results in increased ADC and lower FA values. These DTI parameters change visible in the course of chronic SC compression have been verified in experimental studies, employing animal models [103, 104].
It should be mentioned that contrary changes, that is, an increase in FA and decrease in ADC values were reported in cases of acute SC compression [92]. One of the possible explanations could be cytotoxic edema as the consequence of acute SC injury with extracellular water displacement into cells which leads to shrinking of extracellular space (decreased ADC) and tighter packing of axon bundles (FA elevation). Some authors noticed the same DTI changes in patients with CMS at the site of compression [102]. The characteristic of this finding is unclear; however it should be rather related to some recent event of compression in the course of CDSD, rather than the effects of chronic stenosis.
The scientific reports concerning the correlation between DTI results and clinical findings are contrary. Lee et al. [101] found no differences in DTI parameters between neurologically worse and better groups whereas Budzik et al. [98] reported positive correlation between the severity of clinical impairment and FA. Both researchers used Japanese Orthopedic Association (JOA) score to quantitatively assess myelopathy severity. In a more recent publication, Kerkovsky et al. [97] found significant differences in FA and ADC values between symptomatic and asymptomatic patients with radiological features of cervical spinal cord compression. Moreover, DTI showed higher potential to discriminate between these two clinical subgroups in comparison with standard MRI and electrophysiological findings. Only a few authors have investigated the relationship between DTI findings and surgical outcomes, however these reports are quite promising [101, 105]. Jones et al. [105] found that high baseline FA value was correlated with better postoperative functional recovery and concluded that FA may serve as a useful predictor of the outcome. Lee et al. [101] reported statistically significant correlation between tractography patterns and postoperative neurologic improvement. In opposition, conventional anatomical MRI parameters such as T2-weighted signal changes, cross sectional area of the SC, and anteroposterior (AP) diameter of the SC were not found useful in predicting surgical outcome in patients with CSM [32, 106]. The relationship between myelopathy severity and DTI results which, once established, could facilitate the decision about further patient management, certainly deserves further investigation.
Summary
The decision whether and when to perform invasive surgical treatment in patients with CSM remains the most controversial issue in the management of patients with degenerative cervical spine disease. This decision is usually made on the basis of clinical symptoms as conventional MR examination is characterized by limited sensitivity in myelopathy detection. New magnetic resonance techniques such as DTI, provides quantitative information about the myelopathy severity could help to select patients who would benefit most from surgical decompression, indicating the best moment for intervention, before irreversible myelopathy occurs. Although proven to be very sensitive to neural tissue damage, the DTI method still seeks technical and methodology improvement as well as standardization of acquisition protocols and postprocessing methods among the imaging centers. Implementation of the DTI technique in everyday clinical practice needs further investigation as only when clinical and imaging abnormalities are well correlated, focused treatment can be initiated.
Conflict of Interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
References
Todd AG. Cervical spine: degenerative conditions. Curr Rev Musculoskelet Med. 2011;4:168–74.
Banaszek A, Bladowska J, Szewczyk P, Podgórski P, Sąsiadek M. Usefulness of diffusion tensor MR imaging in the assessment of intramedullary changes of the cervical spinal cord in different stages of degenerative spine disease. Eur Spine J. 2014;23:1523–30.
Demir A, Ries M, Moonen CT, Vital JM, Dehais J, Arne P, Caillé JM, Dousset V. Diffusion-weighted MR imaging with apparent diffusion coefficient and apparent diffusion tensor maps in cervical spondylotic myelopathy. Radiology. 2013;229:37–43.
Mattei TA, Goulart CR, Milano JB, Dutra LP, Fasset DR. Cervical spondylotic myelopathy: pathophysiology, diagnosis, and surgical techniques. ISRN Neurol. 2011;2011:463729.
Matsuda Y, Miyazaki K, Tada K, Yasuda A, Nakayama T, Murakami H, Matsuo M. Increased MR signal intensity due to cervical myelopathy. Analysis of 29 surgical cases. J Neurosurg. 1991;74:887–92.
Takahashi M, Yamashita Y, Sakamoto Y, Kojima R. Chronic cervical cord compression: clinical significance of increased signal intensity on MR images. Radiology. 1989;173:219–24.
Matsumoto M, Toyama Y, Ishikawa M, Chiba K, Suzuki N, Fujimura Y. Increased signal intensity of the spinal cord on magnetic resonance images in cervical compressive myelopathy. Does it predict the outcome of conservative treatment? Spine. 2000;25:677–82.
Xiangshui M, Xiangjun C, Xiaoming Z, Qingshi Z, Yi C, Chuanqiang Q, Xiangxing M, Chuanfu L, Jinwen H. 3 T magnetic resonance diffusion tensor imaging and fiber tracking in cervical myelopathy. Clin Radiol. 2010;65:465–73.
Sasiadek MJ, Bladowska J. Imaging of degenerative spine disease–the state of the art. Adv Clin Exp Med. 2012;21:133–42.
Yarbrough CK, Murphy RK, Ray WZ, Stewart TJ. The natural history and clinical presentation of cervical spondylotic myelopathy. Adv Orthop. 2012;2012:480643.
Salvi FJ, Jones JC, Weigert BJ. The assessment of cervical myelopathy. Spine J. 2006;6:182–9.
Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history. Neurosurgery. 2006;58:1027–39.
Baptiste DC, Fehlings MG. Pathophysiology of cervical myelopathy. Spine J. 2006;6:190–7.
Bohlman HH, Emery SE. The pathophysiology of cervical spondylosis and myelopathy. Spine. 1988;13:843–6.
Fehlings MG, Skaf G. A review of the pathophysiology of cervical spondylotic myelopathy with insights for potential novel mechanisms drawn from traumatic spinal cord injury. Spine. 1998;23:2730–7.
Morishita Y, Naito M, Hymanson H, Miyazaki M, Wu G, Wang JC. The relationship between the cervical spinal canal diameter and the pathological changes in the cervical spine. Eur Spine J. 2009;18:877–83.
Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH, Heller M, Resnic D. Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol. 1998;19:1763–71.
Kim DH, Vaccaro AR, Henderson FC, Benzel EC. Molecular biology of cervical myelopathy and spinal cord injury: role of oligodendrocyte apoptosis. Spine J. 2003;3:510–9.
Ito T, Oyanagi K, Takahashi H, Takahashi HE, Ikuta F. Cervical spondylotic myelopathy. Clinicopathologic study on the progression pattern and thin myelinated fibers of the lesions of seven patients examined during complete autopsy. Spine. 1996;21:827–33.
Mink JH, Gordon RE, Deutsch AL. The cervical spine: radiologist’s perspective. Phys Med Rehabil Clin N Am. 2003;14:493–548.
Fried LC, Doppman JL, Di Chiro G. Direction of blood flow in the primate cervical spinal cord. J Neurosurg. 1970;33:325–30.
Crowe MJ, Bresnahan JC, Shuman SL, Masters JN, Beattie MS. Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nat Med. 1997;3:73–6.
Breig A, Turnbull I, Hassler O. Effects of mechanical stresses on the spinal cord in cervical spondylosis. A study on fresh cadaver material. J Neurosurg. 1966;25:45–56.
Gledhill RF, Harrison BM, McDonald WI. Demyelination and remyelination after acute spinal cord compression. Exp Neurol. 1973;38:472–87.
Shuman SL, Bresnahan JC, Beattie MS. Apoptosis of microglia and oligodendrocytes after spinal cord contusion in rats. J Neurosci Res. 1997;50:798–808.
Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, Shiga H. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19–24.
Lee TH, Kim SJ, Lim SM. Prevalence of disc degeneration in asymptomatic korean subjects. Part 2: cervical spine. J Korean Neurosurg Soc. 2013;53:89–95.
Bednarik J, Kadanka Z, Dusek L, Kerkovsky M, Vohanka S, Novotny O, Urbanek I, Kratochvilova D. Presymptomatic spondylotic cervical myelopathy: an updated predictive model. Eur Spine J. 2008;17:421–31.
Iwabuchi M, Kikuchi S, Sato K. Pathoanatomic investigation of cervical spondylotic myelopathy. Fukushima J Med Sci. 2004;50:47–54.
Vedantam A, Rajshekhar V. Does the type of T2-weighted hyperintensity influence surgical outcome in patients with cervical spondylotic myelopathy? A review. Eur Spine J. 2013;22:96–106.
Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:1178–84.
Wada E, Ohmura M, Yonenobu K. Intramedullary changes of the spinal cord in cervical spondylotic myelopathy. Spine. 1995;20:2226–32.
Suri A, Chabbra RP, Mehta VS, Gaikwad S, Pandey RM. Effect of intramedullary signal changes on the surgical outcome of patients with cervical spondylotic myelopathy. Spine J. 2003;3:33–45.
Morio Y, Teshima R, Nagashima H, Nawata K, Yamasaki D, Nanjo Y. Correlation between operative outcomes of cervical compression myelopathy and mri of the spinal cord. Spine. 2001;26:1238–45.
Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nat Rev Neurosci. 2003;4:469–80.
Mori S, van Zijl PC. Fiber tracking: principles and strategies–a technical review. NMR Biomed. 2002;15:468–80.
Mori S, Zhang J. Principles of diffusion tensor imaging and its applications to basic neuroscience research. Neuron. 2006;51:527–39.
Sąsiadek MJ, Szewczyk P, Bladowska J. Application of diffusion tensor imaging (DTI) in pathological changes of the spinal cord. Med Sci Monit. 2012;18:73–9.
Lee JW, Kim JH, Kang HS, Lee JS, Choi JY, Yeom JS, Kim HJ, Chung HW. Optimization of acquisition parameters of diffusion-tensor magnetic resonance imaging in the spinal cord. Invest Radiol. 2006;41:553–9.
Clark CA, Werring DJ. Diffusion tensor imaging in spinal cord: methods and applications–a review. NMR Biomed. 2012;15:578–86.
Maier SE. Examination of spinal cord tissue architecture with magnetic resonance diffusion tensor imaging. Neurotherapeutics. 2007;4:453–9.
Vargas MI, Delavelle J, Jlassi H, Rilliet B, Viallon M, Becker CD, Lövblad KO. Clinical applications of diffusion tensor tractography of the spinal cord. Neuroradiology. 2008;50:25–9.
Bammer R, Augustin M, Prokesch RW, Stollberger R, Fazekas F. Diffusion-weighted imaging of the spinal cord: interleaved echo-planar imaging is superior to fast spin-echo. J Magn Reson Imaging. 2002;15:364–73.
Zhang J, Huan Y, Qian Y, Sun L, Ge Y. Multishot diffusion-weighted imaging features in spinal cord infarction. J Spinal Disord Tech. 2005;18:277–82.
Bammer R, Stollberger R, Augustin M, Simbrunner J, Offenbacher H, Kooijman H, Ropele S, Kapeller P, Wach P, Ebner F, Fazekas F. Diffusion-weighted imaging with navigated interleaved echo-planar imaging and a conventional gradient system. Radiology. 1999;211:799–806.
Tsuchiya K, Fujikawa A, Suzuki Y. Diffusion tractography of the cervical spinal cord by using parallel imaging. AJNR Am J Neuroradiol. 2005;26:398–400.
Cercignani M, Horsfield MA, Agosta F, Filippi M. Sensitivity-encoded diffusion tensor MR imaging of the cervical cord. AJNR Am J Neuroradiol. 2003;24:1254–6.
Holdsworth SJ, Skare S, Newbould RD, Guzmann R, Blevins NH, Bammer R. Readout-segmented EPI for rapid high resolution diffusion imaging at 3 T. Eur J Radiol. 2008;65:36–46.
Kim TH, Zollinger L, Shi XF, Kim SE, Rose J, Patel AA, Jeong EK. Quantification of diffusivities of the human cervical spinal cord using a 2D single-shot interleaved multisection inner volume diffusion-weighted echo-planar imaging technique. AJNR Am J Neuroradiol. 2010;31:682–7.
Wheeler-Kingshott CA, Parker GJ, Symms MR, Hickman SJ, Tofts PS, Miller DH, Barker GJ. ADC mapping of the human optic nerve: increased resolution, coverage, and reliability with CSF suppressed ZOOM-EPI. Magn Reson Med. 2002;47:24–31.
Jeong EK, Kim SE, Guo J, Kholmovski EG, Parker DL. High-resolution DTI with 2D interleaved multislice reduced FOV single-shot diffusion-weighted EPI (2D ss-rFOVDWEPI). Magn Reson Med. 2005;54:1575–79.
Saritas EU, Cunningham CH, Lee JH, Han ET, Nishimura DG. DWI of the spinal cord with reduced FOV single-shot EPI. Magn Reson Med. 2008;60:468–73.
Dowell NG, Jenkins TM, Ciccarelli O, Miller DH, Wheeler-Kingshott CA. Contiguous-slice zonally oblique multislice (CO-ZOOM) diffusion tensor imaging: examples of in vivo spinal cord and optic nerve applications. J Magn Reson Imaging. 2009;29:454–60.
Wilm BJ, Svensson J, Henning A, Pruessmann KP, Boesiger P, Kollias SS. Reduced field-of-view MRI using outer volume suppression for spinal cord diffusion imaging. Magn Reson Med. 2007;57:625–30.
Nana R, Zhao T, Hu X. Single-shot multiecho parallel echo-planar imaging (EPI) for diffusion tensor imaging (DTI) with improved signal-to-noise ratio (SNR) and reduced distortion. Magn Reson Med. 2008; 60:1512–7
Cohen-Adad J, Wheeler-Kingshott CAM. Quantitative MRI of the spinal cord. 1st ed. San Diego: Academic Press; 2014.
Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999;42:952–62.
Griswold MA, Jakob PM, Heidemann RM, Nittka M, Jellus V, Wang J, Kiefer B, Haase A. Generalized autocalibrating partially parallel acquisitions (GRAPPA). Magn Reson Med. 2002;47:1202–10.
Tsuchiya K, Katase S, Fujikawa A, Hachiya J, Kanazawa H, Yodo K. Diffusion-weighted MRI of the cervical spinal cord using a single-shot fast spin-echo technique: findings in normal subjects and in myelomalacia. Neuroradiology. 2003;45:90–4.
Zaharchuk G, Saritas EU, Andre JB, Chin CT, Rosenberg J, Brosnan TJ, Shankaranarayan A, Nishimura DG, Fischbein NJ. Reduced field-of-view diffusion imaging of the human spinal cord: comparison with conventional single-shot echo-planar imaging. AJNR Am J Neuroradiol. 2011;32:813–20.
Andre JB, Bammer R. Advanced diffusion-weighted magnetic resonance imaging techniques of the human spinal cord. Top Magn Reson Imaging. 2010;21:367–78.
Saritas EU, Lee D, Çukur T, Shankaranarayanan A, Nishimura DG. Hadamard slice encoding for reduced-FOV diffusion-weighted imaging. Magn Reson Med. 2014;72:1277–90.
Gudbjartsson H, Maier SE, Mulkern RV, Mórocz IA, Patz S, Jolesz FA. Line scan diffusion imaging. Magn Reson Med. 1996;36:509–19.
Maier SE, Gudbjartsson H, Patz S, Hsu L, Lovblad KO, Edelman RR, Warach S, Jolesz FA. Line scan diffusion imaging: characterization in healthy subjects and stroke patients. AJR Am J Roentgenol. 1998;171:85–93.
Bammer R, Herneth AM, Maier SE, Butts K, Prokesch RW, Do HM, Atlas SW, Moseley ME. Line scan diffusion imaging of the spine. AJNR Am J Neuroradiol. 2003;24:5–12.
Kubicki M, Maier SE, Westin CF, Mamata H, Ersner-Hershfield H, Estepar R, Kikinis R, Jolesz FA, McCarley RW, Shenton ME. Comparison of single-shot echo-planar and line scan protocols for diffusion tensor imaging. Acad Radiol. 2004;11:224–32.
Clark CA, Barker GJ, Tofts PS. Magnetic resonance diffusion imaging of the human cervical spinal cord in vivo. Magn Reson Med. 1999;41:1269–73.
Pipe JG, Farthing VG, Forbes KP. Multishot diffusion-weighted FSE using PROPELLER MRI. Magn Reson Med. 2002;47:42–52.
Fellner C, Menzel C, Fellner FA, Ginthoer C, Zorger N, Schreyer A, Jung EM, Feuerbach S, Finkenzeller T. BLADE in sagittal T2-weighted MR imaging of the cervical spine. AJNR Am J Neuroradiol. 2010;31:674–81.
Larson PE, Lustig MS, Nishimura DG. Anisotropic field-of-view shapes for improved PROPELLER imaging. Magn Reson Imaging. 2009;27:470–79.
Finsterbusch J, Frahm J. Diffusion-weighted single-shot line scan imaging of the human brain. Magn Reson Med. 1999;42:772–8.
Finsterbusch J, Frahm J. Diffusion tensor mapping of the human brain using single-shot line scan imaging. J Magn Reson Imaging. 2000;12:388–94.
Hennig J, Nauerth A, Friedburg H. RARE imaging: a fast imaging method for clinical MR. Magn Reson Med. 1986;3:823–33.
Xu D, Henry RG, Mukherjee P, Carvajal L, Miller SP, Barkovich AJ, Vigneron DB. Single-shot fast spin-echo diffusion tensor imaging of the brain and spine with head and phased array coils at 1.5 T and 3.0 T. Magn Reson Imaging. 2004;22:751–9.
Sarlls JE, Newbould RD, Altbach MI, Gmitro AF, Seeger J, Trouard TP. Isotropic diffusion weighting in radial fast spin-echo magnetic resonance imaging. Magn Reson Med. 2005;53:1347–54.
Skare S, Newbould RD, Clayton DB, Bammer R. Propeller EPI in the other direction. Magn Reson Med. 2006;55:1298–130.
Mohammadi S, Freund P, Feiweier T, Curt A, Weiskopf N. The impact of post-processing on spinal cord diffusion tensor imaging. Neuroimage. 2013;70:377–85.
Rossi C, Boss A, Lindig TM, Martirosian P, Steidle G, Maetzler W, Claussen CD, Klose U, Schick F. Diffusion tensor imaging of the spinal cord at 1.5 and 3.0 Tesla. Rofo. 2007;179:219–24.
Polders DL, Leemans A, Hendrikse J, Donahue MJ, Luijten PR, Hoogduin JM. Signal to noise ratio and uncertainty in diffusion tensor imaging at 1. 5, 3.0, and 7.0 Tesla. J Magn Reson Imaging. 2011;33:1456–63.
Schwartz ED, Chin CL, Shumsky JS, Jawad AF, Brown BK, Wehrli S, Tessler A, Murray M, Hackney DB. Apparent diffusion coefficients in spinal cord transplants and surrounding white matter correlate with degree of axonal dieback after injury in rats. AJNR Am J Neuroradiol. 2005;26:7–18.
Cohen-Adad J, Lundell H, Rossignol S. Distortion correction in spinal cord DTI. What’s the best approach? Proceedings of the 17th Annual Meeting of ISMRM. Honolulu, USA; 2009:3178.
Basser PJ, Pajevic S, Pierpaoli C, Duda JT, Aldroubi A. In vivo tractography using DT-MRI data. Magn Reson Med. 2000;44:625–32.
Weinstein DM, Kindlmann GL, Lundberg EC. Tensorlines: advection-diffusion based propagation through diffusiontensor fields. In: IEEE Visualization Proceedings. 1999. SanFrancisco.
Lazar M, Weinstein D, Hasan K, Alexander AL. Axon tractography with tensor lines. Proc Intl Soc Mag Reson Med. 2000;8:482.
Behrens TE, Woolrich MW, Jenkinson M, Johansen-Berg H, Nunes RG, Clare S, Matthews PM, Brady JM, Smith SM. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn Reson Med. 2003;50:1077–88.
Parizel PM, Van Rompaey V, Van Loock R, Van Hecke W, Van Goethem JW, Leemans A, Sijbers J. Influence of user-defined parameters on diffusion tensor tractography of the corticospinal tract. Neuroradiol J. 2007;20:139–47.
Valsasina P, Agosta F, Benedetti B, Caputo D, Perini M, Salvi F, Prelle A, Filippi M. Diffusion anisotropy of the cervical cord is strictly associated with disability in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2007;78:480–4.
Toosy AT, Werring DJ, Orrell RW, Howard RS, King MD, Barker GJ, Miller DH, Thompson AJ. Diffusion tensor imaging detects corticospinal tract involvement at multiple levels in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2003;74:1250–7.
Renoux J, Facon D, Fillard P, Huynh I, Lasjaunias P, Ducreux D. MR diffusion tensor imaging and fiber tracking in inflammatory diseases of the spinal cord. AJNR Am J Neuroradiol. 2006;27:1947–51.
Ducreux D, Lepeintre JF, Fillard P, Loureiro C, Tadié M, Lasjaunias P. MR diffusion tensor imaging and fiber tracking in 5 spinal cord astrocytomas. AJNR Am J Neuroradiol. 2006;27:214–6.
Agosta F, Rovaris M, Benedetti B, Valsasina P, Filippi M, Comi G. Diffusion tensor MRI of the cervical cord in a patient with syringomyelia and multiple sclerosis. J Neurol Neurosurg Psychiatry. 2004;75:1647.
Facon D, Ozanne A, Fillard P, Lepeintre JF, Tournoux-Facon C, Ducreux D. MR diffusion tensor imaging and fiber tracking in spinal cord compression. AJNR Am J Neuroradiol. 2005;26:1587–94.
Song T, Chen WJ, Yang B, Zhao HP, Huang JW, Cai MJ, Dong TF, Li TS. Diffusion tensor imaging in the cervical spinal cord. Eur Spine J. 2011;20:422–8.
Chen CJ, Lyu RK, Lee ST, Wong YC, Wang LJ. Intramedullary high signal intensity on T2-weighted MR images in cervical spondylotic myelopathy: prediction of prognosis with type of intensity. Radiology. 2001;221:789–94.
Fernández de Rota JJ, Meschian S, Fernández de Rota A, Urbano V, Baron M. Cervical spondylotic myelopathy due to chronic compression: the role of signal intensity changes in magnetic resonance images. J Neurosurg Spine. 2007;6:17–22.
Aota Y, Niwa T, Uesugi M, Yamashita T, Inoue T, Saito T. The correlation of diffusion-weighted magnetic resonance imaging in cervical compression myelopathy with neurologic and radiologic severity. Spine. 2008;33:814–20.
Kerkovský M, Bednarík J, Dušek L, Sprláková-Puková A, Urbánek I, Mechl M, Válek V, Kadanka Z. Magnetic resonance diffusion tensor imaging in patients with cervical spondylotic spinal cord compression: correlations between clinical and electrophysiological findings. Spine. 2012;37:48–56.
Budzik JF, Balbi V, Thuc V L, Duhamel A, Assaker R, Cotten A. Diffusion tensor imaging and fibre tracking in cervical spondylotic myelopathy. Eur Radiol. 2011;21:426–33.
Bosma RL, Stroman PW. Characterization of DTI indices in the cervical, thoracic, and lumbar spinal cord in healthy humans. Radiol Res Pract. 2012;2012:143705.
Kara B, Celik A, Karadereler S, Ulusoy L, Ganiyusufoglu K, Onat L, Mutlu A, Ornek I, Sirvanci M, Hamzaoglu A. The role of DTI in early detection of cervical spondylotic myelopathy: a preliminary study with 3-T MRI. Neuroradiology. 2011;53:609–16.
Lee JW, Kim JH, Park JB, Park KW, Yeom JS, Lee GY, Kang HS. Diffusion tensor imaging and fiber tractography in cervical compressive myelopathy: preliminary results. Skeletal Radiol. 2011;40:1543–51.
Mamata H, Jolesz FA, Maier SE. Apparent diffusion coefficient and fractional anisotropy in spinal cord: age and cervical spondylosis-related changes. J Magn Reson Imaging. 2005;22:38–43.
Nevo U, Hauben E, Yoles E, Agranov E, Akselrod S, Schwartz M, Neeman M. Diffusion anisotropy MRI for quantitative assessment of recovery in injured rat spinal cord. Magn Reson Med. 2001;45:1–9.
Cheung MM, Li DT, Hui ES, Fan S, Ding AY, Hu Y, Wu EX. In vivo diffusion tensor imaging of chronic spinal cord compression in rat model. Conf Proc IEEE Eng Med Biol Soc. 2009:2715–8.
Jones JG, Cen SY, Lebel RM, Hsieh PC, Law M. Diffusion tensor imaging correlates with the clinical assessment of disease severity in cervical spondylotic myelopathy and predicts outcome following surgery. AJNR Am J Neuroradiol. 2013;34:471–8.
Chiewvit P, Tritrakarn SO, Phawjinda A, Chotivichit A. Predictive value of magnetic resonance imaging in cervical spondylotic myelopathy in prognostic surgical outcome. J Med Assoc Thai. 2011;94:346–54.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Banaszek, A., Bladowska, J., Podgórski, P. et al. Role of Diffusion Tensor MR Imaging in Degenerative Cervical Spine Disease: a Review of the Literature. Clin Neuroradiol 26, 265–276 (2016). https://doi.org/10.1007/s00062-015-0467-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-015-0467-y