Abstract
The purpose of this chapter is to review current evidence on indications, techniques, and outcomes of computer-navigated surgical treatment of pelvic ring injuries and acetabular fractures, particularly computer-navigated screw fixation.
Iliosacral screw fixation of pelvic ring injury using navigation is attracting attention because the biomechanical stabilization of posterior pelvic ring disruption is of primary importance and is widely indicated because it does not require complete reduction of the fracture site. A cadaver study with a simulated zone II sacral fracture demonstrated a substantial compromise in the space available for iliosacral screws with displacements greater than 10 mm. It is possible to reduce the fracture fragment prior to intraoperative imaging in 2D or 3D fluoroscopic navigation. The use of 3D fluoroscopic navigation reportedly results in lower rates of iliosacral screw malpositioning than the use of the conventional technique or 2D fluoroscopic navigation. Moreover, compared with the conventional technique, it reduces radiation exposure and lowers revision rates. However, the malposition rate associated with 3D fluoroscopic navigation ranges from 0% to 31%, demonstrating that there is still room to improve the navigation performance.
Conversely, complete articular surface reduction is required when treating a displaced acetabular fracture to prevent residual hip pain and subsequent osteoarthritic changes. Treating a severely displaced acetabular fracture by screw fixation is very challenging, even with the use of 3D fluoroscopic navigation, because of the difficulty in performing closed anatomical reduction. The indication for percutaneous screw fixation is limited to cases with a small articular displacement. Using 3D fluoroscopic navigation for open surgeries reportedly improves the quality of radiographic fracture reduction, limits the need for an extended approach, and lowers the complication rate.
In conclusion, percutaneous screw fixation for pelvic ring injuries is widely indicated, and navigation makes these procedures safe and reliable. The indication for percutaneous screw fixation of acetabular fractures is limited to cases with a small articular displacement. Using 3D fluoroscopic navigation when performing open surgeries is reported to be useful in evaluating fracture reduction and screw position.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Pelvic ring injury
- Acetabular fracture
- 2D fluoroscopic navigation
- 3D fluoroscopic navigation
- CT-based navigation
- Iliosacral screw
- Anterior column screw
- Posterior column screw
- Supraacetabular screw
22.1 Introduction
A pelvic ring injury and acetabular fracture are life-threatening injuries caused by high-energy trauma, which are often accompanied by multiple organ damage [1]. Early stabilization of the pelvic ring and acetabulum is required to prevent further bleeding from the fracture sites and facilitate early functional recovery. Thus, it is ideal to perform minimally invasive surgery as soon after the injury as possible. In developed countries, the number of high-energy accidents such as a motor vehicle crashes or falls from great heights at construction sites is slowly decreasing, while due to the increase of an aging population, the number of fragility fractures of the pelvis is reportedly increasing [2]. Conservative treatment is a standard option for fragility fractures of the pelvis, but this approach is often accompanied by immobility-associated complications such as loss of waking function, pneumonia, decubitus, and venous thromboembolism. Rommens et al. [2] classified these fractures to the localization of the instability. They recommended a minimally invasive surgical treatment, except for isolated anterior pelvic ring lesions, in order to achieve stable fixation and earlier mobilization [3].
Percutaneous screw fixation under fluoroscopic guidance, including that of an iliosacral screw, transsacral screw, posterior column screw, anterior column (or pubic) screw, and supraacetabular screw, is a good minimally invasive treatment option, but it requires detailed knowledge and experience to correlate the osseous landmarks of the pelvic ring and acetabulum with their corresponding fluoroscopic images and find a secure screw corridor by rotating fluoroscopic views. In order to make these procedures safe and reliable, various types of navigation systems have been applied, including computed tomography (CT)-based navigation [4,5,6], two-dimensional (2D) fluoroscopic navigation [5, 7,8,9,10,11,12,13,14,15,16,17], and three-dimensional (3D) fluoroscopic navigation [5, 8, 12,13,14, 18,19,20,21,22,23]. Their indication and efficacy in surgical treatments of pelvic ring injuries and acetabular fractures are now being debated [13, 24, 25]. The 3D intraoperative imaging modalities and image-based navigation have also been applied to open surgeries for pelvic ring injury and acetabular fracture, and their efficacy in fracture reduction and screw position has been focused on [26,27,28]. The purpose of this chapter is to review current evidence on the indications, techniques, and outcomes of computer-navigated surgical treatment of pelvic ring injuries and acetabular fractures and especially computer-navigated screw fixation.
22.2 Navigated Iliosacral Screw Fixation for the Surgical Treatment of a Pelvic Ring Injury
22.2.1 Indications and Outcomes
Iliosacral screw fixation under fluoroscopic guidance has become a popular technique to stabilize unstable pelvic ring fractures [29,30,31] because the biomechanical stabilization of a posterior pelvic ring disruption is of most importance in the treatment of pelvic ring injury. The use of percutaneous iliosacral screw fixation has minimized the risk of operative blood loss, skin necrosis, and infection associated with open procedures fractures [31,32,33]. Due to the complex 3D sacral anatomy, percutaneous iliosacral screw insertion is a technically demanding procedure because the placement corridors are narrow and variable [34, 35]. It is sometimes difficult to achieve clear and optimal fluoroscopic sacral visualization due to excessive bowel gas, obesity, and/or osteoporosis [36, 37]. Screw malposition rates with fluoroscopic guidance have been reported to range from 2% to 68% [18, 19, 38, 39], with an incidence of neurologic injury between 0.5% and 7.9% [38, 39]. This method requires detailed knowledge and experience to correlate the osseous landmarks of the sacrum with their corresponding fluoroscopic images and to determine a secure screw corridor by rotating the inlet, outlet, and lateral fluoroscopic views [36]. A trigonometric analysis of patients’ CT data suggested that a deviation of the surgeon’s hand by as little as 4° could direct iliosacral screws either into the S1 foramina or through the anterior cortex of the sacrum [35]. Several factors reportedly increase the risk of screw malpositioning such as the presence of a dysmorphic sacrum [34], the use of S2 screws [38], the number of S1 screws used [9], the extent of the dislocation [9], and the surgeon’s experience [9, 40].
To make iliosacral screw fixation under fluoroscopic guidance safe and reliable, various types of computer-assisted techniques, including CT-based navigation [4,5,6], 2D fluoroscopic navigation [5, 7,8,9,10,11,12,13,14, 17], and 3D fluoroscopic navigation systems [5, 8, 12,13,14, 18,19,20], have been developed. It has also been reported that the use of intraoperative 3D imaging modalities in an assessment of iliosacral screws was effective in improving screw position [41, 42]. Iliosacral screw fixation using CT-based navigation is indicated for a minimally displaced pelvic ring injury of 5 mm or less because it is not possible to reduce the fracture. In 2D or 3D fluoroscopic navigation, it is possible to reduce the fracture fragment if the navigation tracker was fixed on the contralateral ilium (Fig. 22.1). A cadaver study with a simulated zone II sacral fracture demonstrated a substantial compromise of the space available for iliosacral screws with displacements greater than 10 mm [43]. Thus, the indication of iliosacral screw fixation using 2D or 3D fluoroscopic navigation could be extended to a displacement of 10 mm or more if a traction table or some special device which could assist and maintain the fracture reduction is used.
The schema shows the pelvic ring before (a) and after manipulative fracture reduction (b). Displaced and reduced bone fragments are colored yellow. The navigation system can track the movement of the sacrum even after reduction because the reference tracker is fixed to the contralateral iliac crest. The black arrows indicate vertical displacement of bone fragments before manipulative fracture reduction. (Reprinted with permissions from [47])
On the other hand, even with the use of 2D and 3D fluoroscopic navigation, the procedure requires substantial experience and detailed anatomical knowledge to find the proper entry point and trajectory of a guide-wire on 2D and 3D fluoroscopic images [9, 20]. Using 3D fluoroscopic navigation reportedly results in lower rates of malpositioning of iliosacral screws compared with conventional fluoroscopic guidance [18, 19, 44] and 2D fluoroscopic navigation [44, 45]. In addition, it has been reported that 3D fluoroscopic navigation reduces radiation time and dose [18] and lowers the revision rate [19] as compared with conventional navigation. However, the malposition rate associated with 3D fluoroscopic navigation reportedly ranged from 0% to 31% when malpositioning was defined as perforation of grade 1 or more [18, 19, 44, 46] (Table 22.1). This means that there is still room for improvement in the accuracy of 3D fluoroscopic navigation for the insertion of iliosacral screws. In most studies, screw perforations were graded according to an established classification method used for pedicle screw placement: grade 0 indicated no perforation, grade 1 indicated a perforation of less than 2 mm, grade 2 indicated a perforation of 2–4 mm, and grade 3 indicated a perforation greater than 4 mm [14].
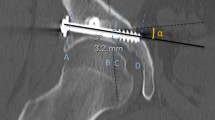
The navigation system guides the sleeve device for guide-wire insertion, not the guide-wire or the screw itself, which could be a cause of screw malposition. In addition, the flexibility of the guide-wire is a concern. The guide-wire diameter of standard iliosacral screws is 2.8–3.2 mm. Richter et al. [46] reported greater screw perforation rates for transsacral screws (45%) than for standard iliosacral screws (4.4%) inserted using navigation combined with robot arm-assisted 3D fluoroscopy. Greater guide-wire flexibility is therefore one possible reason for the greater degree of positional error using transsacral long screws.
Grossterlinden et al. [20] reported that the surgeon experience affected the malposition rates in screw placement in cadaveric pelvises, even when using 3D fluoroscopic navigation. It is difficult for less experienced surgeons to find a safe corridor in the multiple reconstructed planes of 3D fluoroscopic images [40]. We hypothesized that 3D fluoroscopic navigation combined with a preoperative CT-based plan could assist even less experienced surgeons to perform iliosacral screw insertion safely and reliably [40, 47]. A 3D fluoroscopic navigation system using the flat-panel detector-equipped C-arm has made it possible to overlap the preoperative CT-based plan on intraoperative 3D fluoroscopic images of the pelvis with an accuracy of 0.8 mm [48, 49]. In the previous cadaveric study, guide-wires were inserted bilaterally across the ilia into the S1 and S2 vertebral bodies by four novice orthopedic surgeons using fluoroscopic guidance and 3D fluoroscopic navigation with and without CT-based preoperative planning. They could not avoid perforation of the guide-wires, even using 3D fluoroscopic navigation, but the combination of 3D fluoroscopic navigation and CT-based preoperative planning enabled them to insert a guide-wire successfully with a single short. This result showed that the “3D cognitive” skill required to recognize bone structure and position of a guide-wire by viewing 2D or 3D fluoroscopic images is very difficult for trainees to acquire in percutaneous iliosacral screw insertion. Training is necessary for novice orthopedic surgeons to find a proper corridor for the guide-wire viewing either 2D or 3D fluoroscopic images. We initially reported on six cases of pelvic ring injury treated by percutaneous iliosacral screw guided by CT-3D-fluoroscopy matching navigation [47].
The 3D intraoperative imaging modality and image-based navigation have also been applied to open surgeries to evaluate fracture reduction and screw position. We applied CT-3D-fluoroscopy matching navigation to anterior sacroiliac plate fixation through the anterior approach for a type C1 pelvic ring fracture. Intraoperative lumbosacral nerve visualization using computer navigation was useful to recognize the “at risk area” for nerve injury during anterior sacroiliac plate fixation [26] (Fig. 22.2).
For an anterior sacroiliac plate fixation, the direction and depth of screw drilling were checked by inserting the navigation pointer to the drilled holes in the sacral ala instead of fluoroscopic imaging through an anterior approach to the sacroiliac joint (a). A navigation monitor image shows that there is no perforation to the sacral canal, neural foramen, or sacroiliac joint. The navigation pointer is colored green and the lumbosacral nerves are white (b). (Reprinted with permissions from [26])
22.2.2 Surgical Technique
Surgical procedures for iliosacral screw fixation using 3D fluoroscopic navigation combined with CT-based plan are summarized in the flowchart shown in Fig. 22.3. The navigation procedure was performed using a computer navigation system (Stryker Navigation System II-Cart; Stryker, Kalamazoo, MI, USA) and a mobile 3D C-arm equipped with a flat-panel detector (Ziehm Vision FD Vario 3D; Ziehm Imaging, Nuremberg, Germany). The screw position was planned preoperatively using a CT-based planning software (OrthoMap 3D; Stryker) within the navigation unit. During preoperative CT-based planning, three orthogonal reconstructions were viewed along the planned screw axis. In the sagittal-reconstructed plane passing through the nerve root tunnel, the screw position was adjusted to keep a safety margin of more than 3 mm from the upper cortical alar and the S1 and S2 nerve root tunnels (Fig. 22.4).
Three orthogonal reconstructions along the planned screw axis were viewed on a CT-based navigation workstation. The screw position was adjusted to gain a sufficient margin on the sagittal-reconstructed plane (a) passing throughout the nerve root tunnel. Screw direction and length were determined on coronal (b) and axial (c) planes parallel or perpendicular to the sacrum. Each screw was advanced just beyond the sacral midline
The patients were placed in a supine or prone position on a radiolucent operating table or traction table (Fig. 22.5). The navigation computer was placed at each patient’s caudal side. The mobile 3D C-arm approached from the opposite side to the operating surgeon. A reference tracker was fixed to the contralateral anterior or posterior iliac crest using the external fixation device. The C-arm was connected to the navigation system and calibrated by registering three points on the detector using a pointing device. A 3D fluoroscopy scan of the sacrum was performed intraoperatively with the scan center aimed at the S2 vertebral body. Image matching between preoperative CT data and intraoperative 3D fluoroscopic image volume was done using an image registration technique (Fig. 22.6) [47] after the image data were transferred to the navigation system.
Setup of percutaneous iliosacral screw fixation with the patient supine on a radiolucent operating table. The navigation computer was placed at the patient’s caudal side (a). The mobile 3D C-arm approached from the opposite side to the operating surgeon (b). A reference tracker was fixed to the contralateral anterior iliac crest using the external fixation device (b)
Image matching between preoperative CT data and intraoperative 3D fluoroscopic image volume (broken lines) was done using an image registration technique. The accuracy of image matching can be visually assessed on coronal (a), sagittal (b), axial (c), and digitally reconstructed radiographic images (d)
The guide-wire sleeve was calibrated, and a guide-wire was then placed into the S1 and S2 vertebrae according to the preoperative plan with the navigation sleeve while viewing the navigation monitor (Fig. 22.7). It was also possible to perform screw insertion viewing intraoperative 3D fluoroscopic images (Fig. 22.8). The guide-wire was advanced until it penetrated the iliosacral joint. The wire placement was checked fluoroscopically on the inlet and outlet views. For iliosacral screw fixation, the guide-wire was advanced up to the center of the vertebral body because bone density is higher around the vertebral body center [50]. For transsacral screw fixation, the guide-wire was advanced to penetrate the contralateral sacroiliac joint. Drilling and tapping were performed on the ipsilateral sacroiliac joint, and a cannulated 6.5 or 8.0 mm in diameter threaded screw was inserted.
22.3 Navigated Periacetabular Screw Fixation for the Surgical Treatment of an Acetabular Fracture
22.3.1 Indications and Outcomes
Treatment of a displaced acetabular fracture requires complete reduction of the articular surface to prevent residual hip pain and subsequent osteoarthritic changes. An open reduction and internal fixation is the standard treatment option for displaced acetabular fractures. It remains difficult even in the hands of experts, and good postoperative results cannot always be guaranteed. Matta et al. [21] graded the reduction according to one of four categories: anatomical (0–1 mm displacement), imperfect (2–3 mm displacement), poor (>3 mm displacement), or surgical secondary congruence (the acetabulum is reduced anatomically, but displacements in the innominate bone alter the position of the joint) on an anteroposterior and 45° oblique (Judet) radiograph. The reduction was graded as anatomical in 185 of 262 hips (71%), and the quality of the reduction was strongly associated with the clinical result. Giannoudis et al. [51] reported in a meta-analysis of operative treatment of displaced fractures of the acetabulum that if the reduction was satisfactory (≤2 mm displacement), the incidence of osteoarthritis was 13.2%. However, if the reduction was not satisfactory (>2 mm displacement), it increased to 43.5%.
In an experimental study of navigated periacetabular screws using artificial pelvis models and human cadaver specimens, the screw deviation severity from the predefined placement was reportedly significantly lower using a 3D fluoroscopic navigation compared to a 2D fluoroscopic navigation and the conventional technique [13]. In the real clinical setting, it is challenging to treat a displaced acetabular fracture by percutaneous screw fixation even with the use of 3D fluoroscopic navigation because of the difficulty of an anatomical reduction in a closed manner. The indication of percutaneous screw fixation should be limited to cases with a small articular displacement or impaired general condition not allowing for general anesthesia regardless of the amount of fracture displacement. Patients unable to maintain partial weight bearing due to dementia or other psychological disorders are also a good indication given that a non-operative treatment would necessitate several weeks of bed rest with an increased risk of complications such as venous thromboembolism or pneumonia. Schwabe et al. [22] reported very good radiographic and functional outcome of acetabular fractures treated with closed reduction and percutaneous 3D fluoroscopy-based navigated screw fixation. They excluded patients with a fragment displacement >1 cm, comminution, isolated or combined wall fractures, associated both-column fractures, or mildly displaced fractures with intraarticular fragments. Another advantage of percutaneous screwing is that it allows surgery to be performed as soon as possible after the injury due to its inherent minimal invasiveness, which allows for an easy reduction of fractures. Mears et al. [52] reported that if surgery was delayed for more than 11 days after injury, there were significantly fewer anatomical reductions.
The 3D intraoperative imaging modality and image-based navigation have been applied to open surgeries to evaluate fracture reduction and screw position. Oberst et al. [27] compared an acetabular fracture treatment before and after the introduction of a navigation system and a 3D image intensifier. They reported that 25% of the patients with acetabular fractures could be treated with percutaneous screwing using the navigation. The remaining patients were treated by open surgery. Using a navigation system in combination with a 3D image intensifier for open reduction and internal fixation of displaced acetabular fractures led to a significant increase in skin-to-skin time, but the 3D fluoroscopic navigation improved the quality of radiographic fracture reduction, limited the need for an extended approach, and lowered the complication rate. It has been also reported that the use of intraoperative 3D imaging modalities in the treatment of a displaced acetabular fractures led to an improvement in fracture reduction and screw position [28].
After the introduction of the 3D fluoroscopic navigation system, 17 patients with a displaced acetabular fracture were treated operatively in our hospital. Acetabular fractures were classified according to the Judet–Letournel classification as posterior wall in three patients, anterior column in one patient, transverse in one patient, transverse and posterior wall in three patients, anterior column and posterior hemi-transverse in five patients, and both-column in four patients. Five patients (29%) were treated with percutaneous periacetabular screw fixation guided by CT-3D-fluoroscopic navigation. The fracture type was posterior wall in one patient, anterior column in one patient, transverse and posterior wall in one patient, and both-column in two patients. We excluded patients with a fragment displacement >1 cm, comminution, dislocation, or mildly displaced fractures with intraarticular fragments. In the postoperative CT-based analysis, there was no articular or cortical perforation by the screws. The maximal gap of the acetabular articular surface was reduced from 4.8 to 2.5 mm, and the maximal step of the acetabular articular surface changed from 0.2 to 0 mm. These results were comparable to those of other reports (Table 22.2) [15,16,17, 22, 23, 27].
22.3.2 Surgical Technique
Surgical procedures for retrograde pubic screw fixation using 3D fluoroscopic navigation combined with CT-based plan are summarized in the flowchart shown in Fig. 22.9. In preoperative CT-based planning, three orthogonal reconstructions were viewed along the planned screw axis (Fig. 22.10). The screw position was adjusted to avoid articular penetration and cortical perforation. The patients were placed in a supine or prone position on a radiolucent operating table or traction table. The navigation computer was placed at each patient’s caudal side. The mobile 3D C-arm approached from the opposite side to the operating surgeon. A reference tracker was fixed to the contralateral or ipsilateral and anterior or posterior iliac crest using the external fixation device. The C-arm was connected to the navigation system and calibrated by registering three points on the detector using a pointing device. A 3D fluoroscopy scan of the pelvis was performed intraoperatively with the scan center aimed at the screw entry point. Image matching between the preoperative CT data and the intraoperative 3D fluoroscopic image volume was performed using an image registration technique [47] after the image data were transferred to the navigation system.
In the supraacetabular screw and retrograde posterior column screw insertion, a guide-wire was placed into the anterior inferior iliac spine or ischial tuberosity using the navigated drilling sleeve (Fig. 22.11). In retrograde pubic screw insertion, the pubic cortex at an entry point was penetrated using a navigated awl because the screw trajectory is almost parallel to the cortical surface, and a guide-wire tends to be placed extracortically (Fig. 22.12). A navigated pedicle feeler was inserted into the superior pubic ramus to prepare the screw corridor without cortical perforation. The guide-wire was inserted into the hole and the wire placement was checked fluoroscopically. Cannulated 5.0, 6.5, or 8.0 mm in diameter partial thread screws were inserted.
For supraacetabular screw placement, a guide-wire was placed into the anterior inferior iliac spine using the navigated sleeve (a) while viewing the orthogonal screw trajectory (b and c) and digitally reconstructed radiograph (d). Reduction of the acetabular fracture was performed through a mini-incision using a reduction bar viewing intraoperative fluoroscopy (e)
For retrograde anterior column screw placement, the pubic cortex as an entry point was penetrated using a navigated awl. A navigated pedicle feeler (a) was inserted into the superior pubic ramus while viewing orthogonal screw trajectory views, which showed the feeler position in real time (b and c). The guide-wire was inserted into the hole
22.4 Discussion
Advantages and disadvantages of a CT-based system as well as 2D and 3D fluoroscopic navigation systems are summarized in Table 22.3. A systematic review reported malpositioning and revision rates using different iliosacral screw fixation techniques including the conventional technique, 2D or 3D fluoroscopic navigation, and CT-based navigation [24]. CT-based navigation had the lowest rate of screw malposition, and 2D/3D fluoroscopic navigation showed a slightly lower rate of complications than the conventional technique; however, the difference was not statistically significant. It is difficult to compare the performance of different navigation systems by systematic review because the indication for navigation in treating pelvic and acetabular fractures is different among navigation systems because of the differences in their own performance. In addition, the definition and diagnostic imaging modality of screw perforation differ among studies. A prospective, randomized clinical study and/or a well-designed cadaveric study is necessary to compare the performance of navigation systems in the treatment of pelvic and acetabular fractures.
The current navigation system has three possible drawbacks that call for improvement. First, guidance of the screw itself is not possible with the commercially available system, which further reduces the incidence of screw perforation and fluoroscopic time and dose. Second, no navigation system can guide fracture reduction maneuvers, although the level of fracture reduction is a critical factor in determining postoperative outcomes [21, 51]. To accomplish this, it would be necessary to collect quantitative data on fracture reduction maneuvers by skillful surgeons and develop an artificial intelligence system specifically for fracture reduction. Third, surgeons must learn how to use the navigation system to utilize it in surgery. Few studies have evaluated the learning curve of computer-assisted techniques. Peng et al. used intraoperative CT with an integrated navigation system in percutaneous iliosacral screw fixation, reporting that the operation time decreased to half after the first five procedures and further decreased to one-third after the tenth procedure [6]. A training system using virtual reality technology and an easy-to-use device, such as a smartphone, would be required.
22.5 Conclusion
The indication of percutaneous screw fixation for pelvic ring injuries is relatively wide, and the navigation has made these procedures safe and reliable. In particular, the efficacy of 3D fluoroscopic navigation in iliosacral screw insertion has been noted. The indication of percutaneous screw fixation for acetabular fractures is limited to cases with a small articular displacement; therefore, there are few reports regarding the use of navigation. The application of 3D fluoroscopic navigation to open surgeries is reported to evaluate fracture reduction and screw position. In the future, development of a navigation system which can guide fracture reduction is expected.
References
Hauschild O, Strohm PC, Culemann U, Pohlemann T, Suedkamp NP, Koestler W, Schmal H (2008) Mortality in patients with pelvic fractures: results from the German pelvic injury register. J Trauma 64(2): 449–455
Rommens PM, Hofmann A (2013) Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury 44(12):1733–1744
Wagner D, Ossendorf C, Gruszka D, Hofmann A, Rommens PM (2015) Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg 41(4):349–362
Arand M, Kinzl L, Gebhard F (2004) Computer-guidance in percutaneous screw stabilization of the iliosacral joint. Clin Orthop Relat Res 422:201–207
Briem D, Linhart W, Lehmann W, Begemann PG, Adam G, Schumacher U, Cullinane DM, Rueger JM, Windolf J (2006) Computer-assisted screw insertion into the first sacral vertebra using a three-dimensional image intensifier: results of a controlled experimental investigation. Eur Spine J 15(6):757–763
Peng KT, Li YY, Hsu WH, Wu MH, Yang JT, Hsu CH, Huang TJ (2013) Intraoperative computed tomography with integrated navigation in percutaneous iliosacral screwing. Injury 44(2):203–208
Gras F, Marintschev I, Wilharm A, Klos K, Muckley T, Hofmann GO (2010) 2D-fluoroscopic navigated percutaneous screw fixation of pelvic ring injuries--a case series. BMC Musculoskelet Disord 11:153
Behrendt D, Mutze M, Steinke H, Koestler M, Josten C, Bohme J (2012) Evaluation of 2D and 3D navigation for iliosacral screw fixation. Int J Comput Assist Radiol Surg 7(2):249–255
Grossterlinden L, Rueger J, Catala-Lehnen P, Rupprecht M, Lehmann W, Rucker A, Briem D (2011) Factors influencing the accuracy of iliosacral screw placement in trauma patients. Int Orthop 35(9): 1391–1396
Collinge C, Coons D, Tornetta P, Aschenbrenner J (2005) Standard multiplanar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: a cadaver model. J Orthop Trauma 19(4):254–258
Hinsche AF, Giannoudis PV, Smith RM (2002) Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res 395:135–144
Gras F, Marintschev I, Klos K, Muckley T, Hofmann GO, Kahler DM (2012) Screw placement for acetabular fractures: which navigation modality (2-dimensional vs. 3-dimensional) should be used? An experimental study. J Orthop Trauma 26(8):466–473
Ochs BG, Gonser C, Shiozawa T, Badke A, Weise K, Rolauffs B, Stuby FM (2010) Computer-assisted periacetabular screw placement: comparison of different fluoroscopy-based navigation procedures with conventional technique. Injury 41(12):1297–1305
Smith HE, Yuan PS, Sasso R, Papadopolous S, Vaccaro AR (2006) An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine (Phila Pa 1976) 31(2):234–238
Crowl AC, Kahler DM (2002) Closed reduction and percutaneous fixation of anterior column acetabular fractures. Comput Aided Surg 7(3):169–178
Mosheiff R, Khoury A, Weil Y, Liebergall M (2004) First generation computerized fluoroscopic navigation in percutaneous pelvic surgery. J Orthop Trauma 18(2):106–111
Hong G, Cong-Feng L, Cheng-Fang H, Chang-Qing Z, Bing-Fang Z (2010) Percutaneous screw fixation of acetabular fractures with 2D fluoroscopy-based computerized navigation. Arch Orthop Trauma Surg 130(9):1177–1183
Zwingmann J, Konrad G, Kotter E, Sudkamp NP, Oberst M (2009) Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res 467(7): 1833–1838
Zwingmann J, Konrad G, Mehlhorn AT, Sudkamp NP, Oberst M (2010) Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs. conventional). J Trauma 69(6):1501–1506
Grossterlinden L, Nuechtern J, Begemann PG, Fuhrhop I, Petersen JP, Ruecker A, Rupprecht M, Lehmann W, Schumacher U, Rueger JM, Briem D (2011) Computer-assisted surgery and intraoperative three-dimensional imaging for screw placement in different pelvic regions. J Trauma 71(4):926–932
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am 78(11):1632–1645
Schwabe P, Altintas B, Schaser KD, Druschel C, Kleber C, Haas NP, Maerdian S (2014) Three-dimensional fluoroscopy-navigated percutaneous screw fixation of acetabular fractures. J Orthop Trauma 28(12):700–706 discussion 706
He J, Tan G, Zhou D, Sun L, Li Q, Yang Y, Liu P (2016) Comparison of Isocentric C-arm 3-dimensional navigation and conventional fluoroscopy for percutaneous retrograde screwing for anterior column fracture of acetabulum: an observational study. Medicine (Baltimore) 95(2):e2470
Zwingmann J, Hauschild O, Bode G, Sudkamp NP, Schmal H (2013) Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133(9):1257–1265
Zwingmann J, Sudkamp NP, Konig B, Culemann U, Pohlemann T, Aghayev E, Schmal H (2013) Intra- and postoperative complications of navigated and conventional techniques in percutaneous iliosacral screw fixation after pelvic fractures: results from the German pelvic trauma registry. Injury 44(12): 1765–1772
Takao M, Nishii T, Sakai T, Sugano N (2014) Navigation-aided visualization of lumbosacral nerves for anterior sacroiliac plate fixation: a case report. Int J Med Robot 10(2):230–236
Oberst M, Hauschild O, Konstantinidis L, Suedkamp NP, Schmal H (2012) Effects of three-dimensional navigation on intraoperative management and early postoperative outcome after open reduction and internal fixation of displaced acetabular fractures. J Trauma Acute Care Surg 73(4):950–956
Eckardt H, Lind D, Toendevold E (2015) Open reduction and internal fixation aided by intraoperative 3-dimensional imaging improved the articular reduction in 72 displaced acetabular fractures. Acta Orthop 86(6):684–689
Vanderschot PM, Broens PM, Vermeire JI, Broos PL (1999) Trans iliac-sacral-iliac bar stabilization to treat bilateral sacroiliac joint disruptions. Injury 30(9):637–640
Matta JM, Saucedo T (1989) Internal fixation of pelvic ring fractures. Clin Orthop Relat Res 242: 83–97
Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9(3):207–214
Shuler TE, Boone DC, Gruen GS, Peitzman AB (1995) Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions. J Trauma 38(3):453–458
Templeman D, Goulet J, Duwelius PJ, Olson S, Davidson M (1996) Internal fixation of displaced fractures of the sacrum. Clin Orthop Relat Res 329:180–185
Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML Jr (2010) Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma 24(10):622–629
Templeman D, Schmidt A, Freese J, Weisman I (1996) Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res 329:194–198
Ziran BH, Wasan AD, Marks DM, Olson SA, Chapman MW (2007) Fluoroscopic imaging guides of the posterior pelvis pertaining to iliosacral screw placement. J Trauma 62(2):347–356 discussion 356
Sagi HC, Lindvall EM (2005) Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy. J Orthop Trauma 19(2):130–133
van den Bosch EW, van Zwienen CM, van Vugt AB (2002) Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma 53(1):44–48
Routt ML Jr, Simonian PT, Mills WJ (1997) Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma 11(8): 584–589
Takao M, Nishii T, Sakai T, Sugano N (2013) CT-3D-fluoroscopy matching navigation can reduce the malposition rate of iliosacral screw insertion for less-experienced surgeons. J Orthop Trauma 27(12): 716–721
Beck M, Krober M, Mittlmeier T (2010) Intraoperative three-dimensional fluoroscopy assessment of iliosacral screws and lumbopelvic implants stabilizing fractures of the os sacrum. Arch Orthop Trauma Surg 130(11):1363–1369
Kim JW, Oh CW, Oh JK, Lee HJ, Min WK, Kyung HS, Yoon SH, Mun JU (2013) Percutaneous iliosacral screwing in pelvic ring injury using three-dimensional fluoroscopy. J Orthop Sci 18(1):87–92
Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF (2003) The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma 17(2):88–94
Matityahu A, Kahler D, Krettek C, Stockle U, Grutzner PA, Messmer P, Ljungqvist J, Gebhard F (2014) Three-dimensional navigation is more accurate than two-dimensional navigation or conventional fluoroscopy for percutaneous sacroiliac screw fixation in the dysmorphic sacrum: a randomized multicenter study. J Orthop Trauma 28(12): 707–710
Thakkar SC, Thakkar RS, Sirisreetreerux N, Carrino JA, Shafiq B, Hasenboehler EA (2017) 2D versus 3D fluoroscopy-based navigation in posterior pelvic fixation: review of the literature on current technology. Int J Comput Assist Radiol Surg 12(1): 69–76
Richter PH, Gebhard F, Dehner C, Scola A (2016) Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. Injury 47(2):402–407
Takao M, Nishii T, Sakai T, Yoshikawa H, Sugano N (2014) Iliosacral screw insertion using CT-3D-fluoroscopy matching navigation. Injury 45(6): 988–994
Takao M, Yabuta K, Nishii T, Sakai T, Sugano N (2011) Accuracy of a 3D fluoroscopic navigation system using a flat-panel detector-equipped C-arm. Comput Aided Surg 16(5):234–239
Takao M, Nishii T, Sakai T, Sugano N (2012) Application of a CT-3D fluoroscopy matching navigation system to the pelvic and femoral regions. Comput Aided Surg 17(2):69–76
Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM (2016) Sacral bone mass distribution assessed by averaged three-dimensional CT models: implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am 98(7):584–590
Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H (2005) Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br 87(1):2–9
Mears DC, Velyvis JH, Chang CP (2003) Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res 407:173–186
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Takao, M., Hamada, H., Sakai, T., Sugano, N. (2018). Clinical Application of Navigation in the Surgical Treatment of a Pelvic Ring Injury and Acetabular Fracture. In: Zheng, G., Tian, W., Zhuang, X. (eds) Intelligent Orthopaedics. Advances in Experimental Medicine and Biology, vol 1093. Springer, Singapore. https://doi.org/10.1007/978-981-13-1396-7_22
Download citation
DOI: https://doi.org/10.1007/978-981-13-1396-7_22
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1395-0
Online ISBN: 978-981-13-1396-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)