Abstract
Background
Iliosacral screw fixation is a popular technique for treatment of unstable pelvic injuries involving the posterior ring. However, screw malposition may result in dangerous complications involving injury to adjacent neurovascular structures. This study was conducted in order to evaluate the results and efficacy of using three-dimensional fluoroscopy in the performance of iliosacral screw fixation.
Methods
Twenty-nine patients (31 cases, two bilateral) who suffered injury to the pelvic ring requiring surgical treatment were included in this study. According to the Association for Osteosynthesis-Orthopaedic Trauma Association (AO-OTA) classification, there were 14 patients with type B, 13 patients with type C, and 2 patients with a bilateral sacral fracture. The mean age of patients was 39 years. Once the guide pin had been inserted, its safety was confirmed using three-dimensional fluoroscopy; screw fixation was then performed. Eighteen patients underwent percutaneous iliosacral screw fixation and anterior fixation, while 11 patents underwent screw fixation only. Postoperative computed tomography (CT) was performed for evaluation of the screw position, including any invasion into the sacral foramen or canal and neurovascular injury. The perforation of the screw was divided according to the location (sacral zones I, II, and III) and the degree (grade 0, no perforation; grade 1, perforation <2 mm; grade 2, perforation between 2 and 4 mm; grade 3, perforation >4 mm).
Results
The mean operation time was 35.6 min, and the mean radiation exposure time was 85.9 s. For accurate location of the guide pin, one patient underwent three-dimensional reconstruction twice. None of the patients required reoperation or suffered any neurovascular injury. Although seven cases involved perforation, all were less than 2 mm (grade 0: 24 cases, grade 1: 7 cases).
Conclusions
When performing percutaneous iliosacral screw fixation in a patient with an unstable pelvic ring injury, use of three-dimensional fluoroscopy may allow for accurate location of the screw and result in fewer complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unstable pelvic ring injury is associated with serious complications and a high rate of mortality; therefore, stable fixation for both the anterior and posterior pelvic ring is essential. Iliosacral screw fixation, which has been widely used for stabilization of injury to the posterior ligament complex and sacral fractures, can be performed in a percutaneous, minimally invasive manner. Its excellent biomechanical stability has also been demonstrated [1, 2]. However, achieving successful screw fixation without intrusion of the anterior surface of the sacrum or sacral foramina is not easy, and accurate anatomical knowledge and surgical experience are required. Knowledge of the angle of the screw in all directions, as well as the exact location of the screw, is a prerequisite. Until now, evaluation of the anatomical structure of the sacroiliac joint and sacrum has been mainly dependent on two-dimensional fluoroscopy. However, when using two-dimensional fluoroscopy, accurate viewing of the sacral foramina is not always possible, and positional and angular variation of first sacral foraminal anatomy is relatively common. As a result, there have been limitations to precise understanding of the three-dimensional location of sacral foramen using simple radiographs.
Postoperative malposition of a screw during use of simple fluoroscopy has been reported [3, 4], and may result in injury to adjacent nerves and vessels [5, 6]. Therefore, when fixing an iliosacral screw, placement of the screw within the sacrum in order to avoid extraosseous violation is of utmost importance.
Use of two-dimensional fluoroscopy [7] or computed tomography [8] for precise screwing has been reported; however, this is inefficient with regard to operating room space and technical limitations. When considering the efficacy and economic worth, as well as the need to use a computer system [9, 10], its value is limited. Using a fluoroscope that allows for assembly of three-dimensional images, we confirmed the position of the screw in advance, and definite iliosacral screwing was performed. The purpose of this study was to investigate the pros and cons, as well as the accuracy, of this method.
Materials and methods
From January to December 2010, 29 patients suffering from pelvic ring injuries requiring surgical treatment underwent operative treatment at our institution. The study included 17 men and 12 women, with a mean age of 39 (range 17–70). The institution approved the study, which was conducted in strict adherence with established guidelines for treatment of subjects. Mechanisms of injury included traffic accidents (13 patients: 9 pedestrian, 1 motor-vehicle, and 3 motorcycle), a fall from a height (11 patients), and a crushing work-related injury (5 patients). Of these 29 patients, 28 had associated injuries or fractures, with a mean injury severity score (ISS) of 25.2 (range 9–84).
All patients underwent a preoperative radiological evaluation (simple anteroposterior, inlet, and outlet views of the pelvis), including computed tomography (CT) scans for observation of characteristics and the degree of displacement of fractures. According to the AO-OTA classification, there were 14 patients with type B, 13 patients with type C, and 2 patients with bilateral sacral fractures. With consideration for associated injuries and the clinical condition of the patient, early operative intervention was performed as soon as possible. When surgery needed to be delayed because of patients’ general medical condition, skeletal traction was applied until surgery could be performed. On average, the period of time from injury to a definite operative treatment was 8 days (range 0–40). Eighteen patients underwent concomitant anterior plating and percutaneous iliosacral screwing, and the remaining 11 patients (13 cases) underwent iliosacral screwing only. All surgical procedures were performed by a single experienced surgeon.
Operation
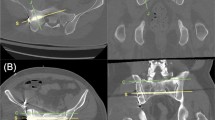
All patients were placed in a supine position on the radiolucent table. When anterior pelvic ring fixation was required, the operation for treatment of this injury was performed first. A 7.0-mm cannulated screw (Synthes®, Switzerland) was used to perform iliosacral screwing. With the guidance of the pelvic lateral, inlet, and outlet view by rotating and steering the fluoroscope, a metal guide pin was inserted from the iliac wing to the body of the first sacrum until it passed through the center of the sacral body. Then, in order to determine the accurate position of the guide pin, multiplanar reconstruction was performed using three-dimensional fluoroscopy (ARCADIS Orbic C-Arm, Siemens, Erlangen, Germany) after a 190° rotation on the anterior, posterior, and lateral sides. After confirming the safe position of the guide pin within the sacrum, drilling was performed over the guide pin using a 5-mm bit, and a cannulated screw of adequate length was fixed (Figs. 1, 2, 3, 4).
A guide pin was inserted percutaneously on the pelvic inlet and lateral views using fluoroscopy (a, b). Then, image reconstruction was achieved using three-dimensional fluoroscopy. Outlet and axial reconstruction images show the safe location of the guide pin (arrows) (c, d). A three-dimensional image also shows that the guide pin is located inside the sacral body (e)
Pelvic inlet/outlet images on a three-dimensional postoperative CT scan. The inserted screw was fixed adequately without suspicion of intrusion into the spinal canal or anterior to the sacral body. Using a long reconstruction plate, the anterior disruption of the pelvic ring was reduced and fixed (a, b)
The operation time for iliosacral screwing was measured from insertion of the guide pin to skin closure. In addition, radiation exposure time—only the time required for iliosacral screw fixation—was measured separately. For assessment of the position of the screw in relation to the sacral foramen or canal, a postoperative CT scan was performed in order to determine the location of the iliosacral screw.
The position of screw perforation was assessed at zones I, II, and III of the sacrum and classified as anterior and posterior or superior and inferior. The degree of perforation was classified as grade 0 (no perforation), grade 1 (perforation <2 mm), grade 2 (perforation between 2 and 4 mm), and grade 3 (perforation >4 mm) [11]; cases involving grade 2 or higher were classified as malposition.
Results
The mean operation time was 35.6 min (range 18–83); it was 34.6 min (range 18–58) and 37.4 min (range 23–83), respectively, for procedures performed for treatment of type B and C fractures. Compared to type B fractures, the mean operation time for treatment of type C fractures was longer, but this was not statistically significant. Three-dimensional reconstruction was performed twice in one case involving a type B fractures as the position of the guide pin was inaccurate after assessment using a multiplanar reconstruction image.
The mean time for radiation exposure was 84.0 s (range 22–160) and that for type B fractures was 90.1 s (range 22–160), which was longer than that for type C fractures, 82.4 s (range 43–109); however, the difference was not statistically significant.
In postoperative radiologic evaluation using CT scans, perforation of the screw occurred in seven cases (7/31, 22.6 %); however, all perforations were less than 2 mm (grade 0: 24, grade I: 7), and no malposition greater than 2 mm was observed. Locations of perforation were zone II in four cases, zone III in three cases, anterior perforation in two cases, and posterior perforation in five cases. Perforation occurred in four cases involving type B (4/14, 28.6 %) and three cases involving type C (3/15, 20.0 %), respectively, and four cases involving fixation of the anterior pelvic ring together (4/17, 23.5 %) and three cases involving fixation of the posterior pelvic ring alone (3/14, 21.4 %). No correlation was observed between perforation and type of fracture or treatment modality. Even if a perforation developed, there were no complicated cases associated with neurological deficits up to the final follow-up.
Among 31 patients who underwent surgery, there was no occurrence of neurovascular injury caused by intrusion of the spinal canal or sacral foramen, and also other complications, such as postoperative hematoma, wound infection, or wound necrosis, did not occur.
Discussion
Fracture or injury of the sacroiliac joint is commonly accompanied by pelvic ring injury. Use of reduction and internal fixation has been reported to promote early ambulation, reduce the preoperative and postoperative mortality rate, and aid in improvement of the functional outcome [12]. Compared with open reduction, the percutaneous iliosacral screwing used in this study requires a short operation time and can be performed with minimal injury to adjacent tissue. Due to its excellent biomechanical stability, it is popular for use in stabilizing the posterior pelvic ring [1, 13]. Because of the anatomical variation of the sacroiliac joint and the presence of the fifth lumbar nerve root and iliac vessels, preoperative CT scans and intraoperative fluoroscopic guidance are essential to obtain an accurate locus of the screw. However, due to personal variations in patients, such as obesity, bowel gas, and sacral dysplasia, obtaining clear two-dimensional images and applying proper interpretation is not easy. The rate of screw malposition in conjunction with fluoroscopy has been reported to be approximately 2–15 % [14, 15], and that of nerve injury has been reported to be up to 0.5–7.7 % [16]. Therefore, caution regarding the risk of surgery is always needed. In an experimental study using cadavers [11], use of a conventional method resulted in approximately 75 % perforation; in our series, occurrence of perforation was 22.6 %. However, all were within the minute range, less than 2 mm. In addition, because none of the patients experienced neurovascular complications, the safety and effectiveness appear to be sufficient.
When performing iliosacral screw fixation using fluoroscopy, it is clear that the radiation hazard to both the patient and surgical team is a potential risk, and radiation exposure should be reduced as much as possible. Zwingmann et al. [10] reported an average radiation exposure time of 141 s with conventional fluoroscopy, while it was 84.0 s in our series, and a significant decrease might be possible. In addition, during fluoroscopy for reconstruction of three-dimensional images, members of the surgical team and operating room personnel can stay out of the operating room in order to avoid radiation hazards, except to the patient.
In patients with severe pelvic ring injury, the operation time should be reduced as much as possible. Collinge et al. [9] reported no significant difference in operating time compared to a conventional method. In our series, the average time required to fix an iliosacral screw was 35.6 min, which was shorter than that of other reports using a conventional method [16]. We believe that this was possible because the proper position of the guide pin could be determined by three-dimensional imaging, and subsequent screw fixation could proceed rapidly. For one of the patients in our series, deviation of the guide pin outside the sacrum, which was observed during the operation, caused an additional time delay, and three-dimensional reconstruction was performed again. However, using a conventional method, screw malposition can be assessed mainly by postoperative CT scans, and reoperation should be required. In addition, the diameter of the definite screw is thicker than that of the guide pin, and serious neurovascular complications may occur as a result of the presence of the screw itself. We believe that our method offers an additional advantage in this situation.
Computer navigation-assisted surgery, which can decrease the level of radiation exposure to a minimum value and allow for very accurate selection of the screw position, has recently been attempted; however, expensive hardware and the necessity of a large operating space are disadvantages of this method. Zwingmann et al. [10] reported 63–93 s of radiation exposure time using navigation. Although direct comparison is difficult, results of our series were similar, and, in view of its economic advantage, the use of three-dimensional fluoroscopy is considered effective.
Learning about the proper location for accurate placement of the screw requires time and effort. When three-dimensional fluoroscopy is not available, it is difficult to determine whether or not the screw is fixed in the optimal position at the time of surgery. Under the guidance of conventional fluoroscopy, after obtaining an adequate lateral view, the entry point for the iliosacral screw, which should be caudally located relative to the ilio-cortical density (ICD) and contained appropriately within the midportion of the sacral ala, should be determined [17]. With the guidance of the pelvic inlet and outlet view, the guide pin should be inserted from the outer table of the iliac wing, and care should be taken to ensure that it does not intrude upon the sacral canal or sacral foramen [10]. At the time of drilling, gentle advancement of the drill in steps to ensure that the drill remains in bone is very important.
Limitations of our study include the small number of patients and the fact that this is not a prospective study compared to a conventional method. In addition, even if the degree of perforation was minimal and symptoms did not present, results showing 22.6 % perforation should not be overlooked. It is clear that sufficient anatomical knowledge and experience are required for placement of the guide pin into its proper position.
Conclusions
Use of three-dimensional fluoroscopy in iliosacral screwing is a safe modality and may allow for accurate location of the screw and avoidance of neurovascular complications.
References
Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM. Safe placement of S1 and S2 iliosacral screws: the “vestibule” concept. J Orthop Trauma. 2000;14:264–9.
Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995;9:207–14.
Routt ML Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997;11:584–9.
Xu R, Ebraheim NA, Robke J, Yeasting RA. Radiologic evaluation of iliosacral screw placement. Spine. 1996;21:582–8.
Altman DT, Jones CB, Routt ML Jr. Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999;13:220–7.
Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma. 1997;43:146–9.
Peng KT, Huang KC, Chen MC, Li YY, Hsu RW. Percutaneous placement of iliosacral screws for unstable pelvic ring injuries: comparison between one and two C-arm fluoroscopic techniques. J Trauma. 2006;60:602–8.
Ziran BH, Smith WR, Towers J, Morgan SJ. Iliosacral screw fixation of the posterior pelvic ring using local anaesthesia and computerised tomography. J Bone Joint Surg Br. 2003;85:411–8.
Collinge C, Coons D, Tornetta P, Aschenbrenner J. Standard multiplanar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: a cadaver model. J Orthop Trauma. 2005;19:254–8.
Zwingmann J, Konrad G, Mehlhorn AT, Sudkamp NP, Oberst M. Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs. conventional). J Trauma. 2010;69:1501–6.
Smith HE, Yuan PS, Sasso R, Papadopolous S, Vaccaro AR. An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine. 2006;31:234–8.
Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989;242:83–97.
Oh CW, Kim PT, Kim JW, Min WK, Kyung HS, Kim SY, Oh SH, Ihn JC. Anterior plating and percutaneous iliosacral screwing in an unstable pelvic ring injury. J Orthop Sci. 2008;13:107–15.
Hinsche AF, Giannoudis PV, Smith RM. Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res. 2002;395:135–44.
Templeman D, Schmidt A, Freese J, Weisman I. Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res. 1996;329:194–8.
van den Bosch EW, van Zwienen CM, van Vugt AB. Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma. 2002;53:44–8.
Routt ML Jr, Simonian PT, Agnew SG, Mann FA. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clnical study. J Orthop Trauma. 1996;10:171–7.
Conflict of interest
All authors have certified that they have no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with this article.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kim, JW., Oh, CW., Oh, JK. et al. Percutaneous iliosacral screwing in pelvic ring injury using three-dimensional fluoroscopy. J Orthop Sci 18, 87–92 (2013). https://doi.org/10.1007/s00776-012-0320-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-012-0320-y