Abstract
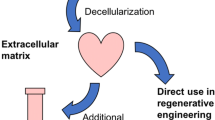
Decellularization is a technique to remove cellular components from native tissues, which could reduce immune reactions to the scaffolds. Decellularized matrices are valuable for tissue engineering, as they preserve tissue-specific structural, mechanical, and biochemical microenvironments, while promoting cellular engraftment and functions in the matrix. So far, various tissues have been decellularized by combinations of mechanical, chemical, and enzymatic processes and utilized in preparing bioscaffolds to provide tissue-specific environments for various cell types, including primary cells, progenitor cells, and stem cells. In addition, decellularized matrices could be manipulated into several formats according to the final application, such as tissue-engineering scaffolds, artificial organs, cell culture matrices, and transplantation carriers. In this chapter, we describe various types of decellularized tissue matrices and their extensive use in regenerative medicine, including reconstruction of artificial organs and regeneration of damaged tissues.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Decellularization
- Tissue engineering
- Stem cell
- Regenerative medicine
- Organ transplantation
- Artificial organ
1 Tissue-Derived Natural Scaffold: Decellularized Matrix
In the scope of tissue engineering and regenerative medicine, investigations of functional biomaterials and development of in vivo-like systems are essential to maximize the efficacy of tissue regeneration. Various extracellular matrix (ECM)-derived components and synthetic biomaterials have been utilized to construct tissue-mimicking scaffolds and provide tissue-like microenvironments for improved functionalities of cells (Hubbell 1995; O’brien 2011; Place et al. 2009). However, the complex structural interactions and biomolecular composition of native tissues cannot currently be reconstituted with combinations of available simple fabrication techniques.
To prepare functional scaffolds for successful tissue regeneration, decellularization of organs has been increasingly studied in the last few decades, using different types of xenogenic, allogenic, and autologous tissues (Gilbert et al. 2006). During decellularization through stepwise processes of physical, chemical, and enzymatic methods, most cells within the organ are removed, while the tissue-specific structures and functional biomolecules of the tissue ECM are retained, providing a tissue-specific microenvironment (Fig. 10.1) (Gilbert et al. 2006; Guyette et al. 2014). With the excellent biocompatibility of organ-derived natural materials, various types of cells such as primary cells and stem cells can be reseeded onto the decellularized matrix to fabricate tissue-engineered artificial organs, which show greatly enhanced cellular engraftment and tissue regeneration with improved functionalities compared to conventional scaffolds (Fig. 10.1) (Badylak et al. 2011). The biochemical microenvironment, based on the retained ECMs, glycoproteins, proteoglycans, and tissue-specific functional molecules and mechanical properties similar to those of native tissues, significantly enhanced the regenerative efficacy of the matrix and showed potential in therapeutic replacement of damaged tissues (Badylak et al. 2011; Ott et al. 2008; Reing et al. 2010). Importantly, removal of native cells could minimize immune rejection and immune-related issues, which facilitates the use of these biomaterials in regenerative medicine and further clinical applications (Gilbert et al. 2006).
Tissue-engineering strategy using the recellularization of various cell types into decellularized tissue matrices prepared with diverse chemical and enzymatic methodologies. Decellularized matrices from various tissues (e.g. blood vessel, intestine, bladder, skin, trachea, bone, tendon, and skeletal muscle) can be utilized as functional bioscaffolds for tissue regeneration. Solubilized decellularized matrices can be used as injectable hydrogels for cell transplantation
2 Decellularized Matrix as a Functional Bioscaffold for Tissue Engineering
2.1 Blood Vessel
Replacement of diseased blood vessels is a common surgical treatment for treating coronary artery and peripheral vascular diseases (e.g. atherosclerosis) (Chlupac et al. 2009). Although autologous vessels are a major candidate for bypass graft transplantation, proper vessels might not always be available and harvesting autologous vessels entails substantial surgical costs and complex procedures and causes secondary morbidity (Wilson et al. 1995). Therefore, artificial blood vessels comprised of natural or synthetic polymers have been developed over the last few decades (L’Heureux et al. 2006, 2007). However, these scaffolds usually fail to maintain functional vessels for long-term patency owing to restenosis and thrombosis after transplantation, especially for artificial vessels with diameters below 6 mm (Wilson et al. 1995).
Since the early 1990s, acellular tissue-engineered blood vessels have been highlighted as natural scaffolds for vessel replacement (Wilson et al. 1995; Kaushal et al. 2001; Cho et al. 2005a, 2006). ECM components in decellularized vessels, such as collagen, elastin, and glycosaminoglycan (GAG), can promote repopulation of endothelial cells and smooth muscle cells, resulting in functional vessel construction and host integration without thrombosis (Kaushal et al. 2001). Decellularized vessels can be acquired from various arteries and veins, including carotid arteries (Cho et al. 2005b), iliac arteries (Kaushal et al. 2001), umbilical arteries (Gui et al. 2009), saphenous veins (Schaner et al. 2004), inferior vena cava (Cho et al. 2005a; Bertanha et al. 2014a; Lee et al. 2014), and jugular veins (Lee et al. 2014). Decellularization of the native vessel includes diverse ionic (e.g. sodium dodecyl sulfate [SDS], deoxycholate) (Gui et al. 2009; Schaner et al. 2004) or non-ionic (e.g. Triton X-100) detergents (Kaushal et al. 2001), and enzymatic (e.g. trypsin, RNase, DNase) treatments (Wilson et al. 1995; Kaushal et al. 2001). Among them, the Triton X-100-based mild chemical procedure has been generally adopted to remove cellular components and retain similar structural integrity, mechanical properties, and ECM components of the native vessel (Samouillan et al. 1999).
For successful fabrication of tissue-engineered blood vessels, rapid endothelialization and host integration with the endothelium and smooth muscle layers are essential for reducing the possibility of restenosis and subsequent graft failure. Diverse cell types have been seeded onto the matrix to potentiate functionality and long-term patency of the artificial decellularized vessels. Stem cells, having the potential to differentiate into endothelial cells, have been considered an ideal candidate to construct the endothelium, which is important for physiological functions involved in inhibiting inflammation, thrombosis, and restenosis after transplantation (Kaushal et al. 2001). For example, endothelial progenitor cells (EPCs) were isolated from peripheral blood and seeded inside the lumen of the decellularized vessel for preconditioning of the graft. The confluent monolayer of EPCs on the decellularized vessel graft greatly extended in vivo patency with physiological functionalities (Kaushal et al. 2001; Quint et al. 2011). Smooth muscle cells (SMCs) play major roles in the medial layer of the vessel as supporting cells in the mechanical and physiological functions of native blood vessels (Dora 2001). Thus, several studies coseeded SMCs with ECs and showed significantly enhanced in vivo maturation and contractile functionality of the engineered vessel graft (Yazdani et al. 2009; Neff et al. 2011). In addition, bone marrow-derived cells (Cho et al. 2005a) and mesenchymal stem cells (MSCs) (Zhao et al. 2010; Bertanha et al. 2014b) were differentiated into EC-like cells or SMC-like cells and used in reconstruction of endothelium and vessel grafts, resulting in improved long-term patency.
2.2 Small Intestine
Decellularized small intestinal submucosa (SIS) is one of the most widely studied decellularized ECM scaffolds. SIS is a thin layer of intestinal tissue that supports the mucosa and joins it to the muscularis propria layer. With the high content of collagens and structural integrity of the decellularized SIS, it has been mostly used as a transplantable natural scaffold for clinical applications (Hodde 2002; Badylak 1993). Indeed, SIS has been used in treating patients requiring blood vessel replacement, bladder reconstruction, dural repair, tendon and ligament substitute, and chronic wound healing (Huynh et al. 1999; Franklin et al. 2002; Badylak et al. 1989, 1999, 2002; Prevel et al. 1995; Cheng and Kropp 2000; Cobb et al. 1999). Other popular clinical usages of SIS scaffolds include reconstruction of urinary bladder (Misseri et al. 2005; Caione et al. 2006), urethra (Jones et al. 2005), diaphragm (Oelschlager et al. 2003), and integument (MacLeod et al. 2004; Zhang et al. 2003). In earlier studies, the whole small intestine tissue section was examined for implantable biomaterial usage. However, having all the layers in the small intestine appeared to be too enzymatically active for clinical uses, especially in wound treatments. Subsequent studies involved examination of the various layers of the small intestine, and it was concluded that the layer consisting solely of the submucosa was the most suitable for implantation usage (Brown-Etris et al. 2002). The submucosal layer appears to be the best option in terms of biofunctionality for transplantation because of its high content of fibroblast growth factor (FGF), transforming growth factor-beta (TGF-β), and collagens (Badylak et al. 1989; Badylak 2004). Not only do the factors induce rapid regeneration of the submucosal layer, but the fibrous collagen network in the layer also gives mechanical strength to the whole intestine.
There are various methods to produce completely decellularized intestine, that include physical, chemical, and enzymatic methods (Luo et al. 2011; Syed et al. 2014; Oliveira et al. 2013), but generally, decellularized SIS does not need complex decellularization steps to remove all cellular and nuclear materials because it already contains relatively few, if any, connective tissue cells. In most cases, mechanical force has been used to delaminate the layers of the small intestine, and the extent of the force used is enough to separate the SIS layer from the small intestine with minimal disruption to the three-dimensional (3D) ECM structures. Despite the relative lack of cellular materials to start with, additional chemical methods including treatments with Triton X-100, peracetic acid, and deoxycholate have been used in many studies to ensure that there are no immune responses upon transplantation (Wu et al. 2011; Totonelli et al. 2012).
For cell therapeutic purposes, stem cells have been used as a cell source for SIS transplantation, since stem cells can differentiate and contribute to the regeneration of the intestinal epithelium. It has been reported that adult stem cells such as human MSCs, including bone-marrow derived cells, can repair the damaged intestinal epithelium (Patil et al. 2013). Other studies for reconstruction of urethral tissue involve the isolation of human MSCs from voided urine that can differentiate into multiple bladder cell lineages (Wu et al. 2011). Urine-derived stem cells and smooth muscle cells could be seeded onto SIS scaffolds to mimic urethral tissues for transplantation.
2.3 Bladder
The urinary bladder is a hollow muscular sac where urine is contained until it is evacuated from the body by the parasympathetic nervous system. Spinal cord injury can affect the activity of the urinary bladder and cause bladder dysfunction, eventually leading to urinary tract infections, which significantly affects the quality of life of the patient. The conventional treatment for repairing a damaged urinary bladder involves partial or complete replacement of the bladder with gastrointestinal segments (Kropp et al. 2004). Upon transplantation, several issues can arise, such as metabolic disturbances, increased mucus production, and malignant tissue formation (Soergel et al. 2004). Owing to these problems, more attempts have been made to approach urinary bladder treatment from a tissue engineering perspective. Synthetic materials such as polyvinyl sponge (Kudish 1957) or collagen matrices (Monsour et al. 1987) had been used in experimental and clinical settings, but they usually failed to generate functional bladders due to their lack of biocompatibility and insufficient layer formation of bladder tissues. Since decellularization is an efficient method to produce bioscaffolds for regeneration of diverse organs, an acellular bladder matrix has also been considered for the repair and regeneration of urinary bladder. Bladder augmentation using decellularized matrix has been proposed to improve the function of neurogenic bladder (Obara et al. 2006; Urakami et al. 2007).
The decellularization protocols for the bladder included sodium deoxycholate (Obara et al. 2006; Urakami et al. 2007), Triton X-100 with ammonium hydroxide (Consolo et al. 2016), sodium azide (Sievert et al. 2006), SDS (Youssif et al. 2005), and RNase/DNase treatments (Reddy et al. 2000). Most studies also involved physical lamination and removal of the muscular and serosal layers prior to the chemical and enzymatic procedures to facilitate the later steps (Youssif et al. 2005; Davis et al. 2011). The studies that optimized the protocol to remove almost all the cellular contents while preserving the ECM structural architecture and growth factors combined lamination of the layers and SDS solution treatment (Youssif et al. 2005; Rosario et al. 2008). This method enhanced the reseeding and proliferation of urothelial and bladder stromal cells.
When the decellularized bladder matrix is used without reseeding, it augments the bladder to induce the formation of the urothelial layer (Brown et al. 2002). In other studies that used a seeded matrix of the bladder, urothelial cells are used for the patients needing bladder augmentation (Yoo et al. 1998). For the treatment of patients with bladder cancer, alternative cell sources such as stem cells are a candidate because the patient’s own stem cells can be used to generate more specialized bladder tissue. The stem cells for recellularization of the bladder matrix include bone marrow-derived mesenchymal stem cells (BMMSCs) (Chung et al. 2005), bone marrow-derived endothelial progenitor cells (Chen et al. 2011), adipose-derived stem cells (ADSCs) (Zhu et al. 2010), or amniotic fluid-derived stem cells (De Coppi et al. 2007). It has been shown that the decellularized bladder matrix can provide the cells with an environment suitable to promote cell migration, growth, and differentiation. Therefore, decellularization methods hold a great deal of promise for bladder repair.
2.4 Skin
Skin is the largest organ in vertebrates, playing roles as a mechanical barrier against pathogens and excessive water loss, as well as an insulator for temperature moderation. Despite the large advancements in regenerative medicine, treating skin disorders and injuries with fully functional skin tissues has faced substantial limitations. Although autologous dermis transplantation is a popular therapeutic for skin regeneration, development of bioscaffolds that can be applied immediately after severe injuries such as burns is essential to reduce lethality and minimize issues regarding shortages of skin replacement, especially for skin reconstruction of large-scale, full-thickness injuries. Earlier studies developed skin scaffolds from natural polymers and synthetic biodegradable polymers (Eaglstein and Falanga 1997). However, synthetic materials appeared to have poor biocompatibility and low mechanical strength to resist wound contraction (Ono et al. 1999). Moreover, large scale skin defects arising from surgery, acute trauma, chronic wounds, cancer, or vascular disease require skin transplantation, which cannot be accomplished solely with conventional synthetic scaffolds (Ruszczak 2003). Thus, a bioengineered acellular dermal matrix has been the next desirable candidate for skin substitutes.
Recent studies have presented several methods for producing natural matrices derived from decellularized skin tissue (Chen et al. 2004; Hoganson et al. 2010). They demonstrated successful decellularization methods that exhibited low antigenicity, excellent structural integrity, and comparable functional performances to native skin. For eliminating cells from dense skin tissue, SDS (Wainwright 1995; Livesey et al. 1995) and Triton X-100 treatments along with other enzymes such as dispase (Takami et al. 1996) have been employed. The process of skin decellularization usually requires more than just one treatment and takes much longer than the conventional decellularization protocols for other organs due to high collagen density of skin tissue.
Decellularized skin scaffolds are not only useful in skin reconstruction, but also in reconstruction of several other body parts including the esophagus (Bozuk et al. 2006) and urinary tract (Kimuli et al. 2004). To further promote skin regeneration and efficient structural reconstruction of thick skin tissue by decellularized matrices, cell reseeding has also been explored. There have been several studies that utilize ADSCs, a widely investigated stem cell type in regenerative medicine, to enhance wound healing using decellularized skin tissues (Nie et al. 2009; Huang et al. 2012; Altman et al. 2008). The decellularized dermal matrix can act as a functional biomaterial platform to promote ADSC differentiation or as a delivery vehicle to carry stem cells capable of secreting angiogenic factors to the injured sites for accelerated wound healing. Autologous BMMSCs (Zhao et al. 2012) and keratinocyte-like cells differentiated from ADSCs (Chavez-Munoz et al. 2013) have also been used to reconstruct skin tissues using a decellularized skin matrix.
2.5 Trachea
Trachea, a cartilaginous airway is one of the most well-studied tissues in regards to engineering concepts based on decellularization techniques. Malignant tracheal injuries often require tissue resection and artificial trachea implantation, especially when the removed length exceeds 30% of the native trachea (Macchiarini et al. 2008). Therefore, tubular scaffolds made of various biocompatible natural and synthetic polymers have been utilized for the fabrication of tissue-engineered tracheae and successful tracheal replacement (Jungebluth et al. 2011; Grillo 2002). However, anatomical complications and exposure to external pathogens usually induce immune reaction, inflammation, and subsequent restenosis, leading to failures in long-term patency (Grillo 2002).
Therefore, a decellularized trachea has been investigated as an attractive natural scaffold for preparing a functional tissue construct and trachea replacement. Detergent-based (e.g. sodium deoxycholate, SDS, and Triton X-100) and enzymatic (e.g. DNase-I) decellularization methods were adopted to remove cellular components from native tracheal tissues (Macchiarini et al. 2008; Gray et al. 2012; Jungebluth et al. 2014). Generally, decellularization of tracheal tissue is a more time-consuming process compared to that for other organs due to difficulties in eliminating chondrocytes from the cartilaginous layer. However, repeated cycles of the process resulted in depletion of DNA content after decellularization, thus minimizing immune reactions. Decellularized trachea matrix scaffolds successfully preserved trachea-specific 3D structures and ECM components such as collagen, laminin, and GAG, even after the decellularization process (Partington et al. 2013). Moreover, the decellularized trachea showed comparable mechanical properties to a native trachea (Jungebluth et al. 2014; Partington et al. 2013), which is a crucial factor for long-term maintenance and functionality after transplantation, although several studies employed chemical fixation methods for mechanical strength enhancement (Haag et al. 2012).
Decellularized trachea matrix was further engineered with stem cells to improve the efficacy of practical tracheal reconstruction. MSCs differentiated into the chondrogenic lineage (Gray et al. 2012; Go et al. 2010) were seeded or coseeded with epithelial cells on the decellularized matrix to facilitate trachea reconstruction, suggesting the regenerative potential of the engineered matrix. Stem cells are thought to participate directly in tissue regeneration for physiological functions, simultaneously withstanding the mechanical demands required for tracheal functions. A clinical trial using a tissue-engineered trachea was firstly attempted in a patient with end-stage tracheal disease in 2008 by engineering the decellularized matrix with autologous epithelial cells and MSC-derived chondrocytes (Macchiarini et al. 2008). Since then, several clinical applications have also been performed and successful regeneration of the trachea was confirmed in several clinically relevant follow-up studies (Gonfiotti et al. 2014; Jungebluth and Macchiarini 2014). However, the need for additional stent insertions and initial side effects including immune reactions, inflammation, and partial stenosis also occurred in many cases. Therefore, to be accepted as a universal treatment for tracheal reconstruction, decellularized trachea matrix-based approaches need to be further studied in terms of improving host integration without restenosis and satisfying mechanical properties for long-term patency.
2.6 Bone
Unlike most tissues in the body, bone is a hard connective tissue made up of different osteogenic lineage cells such as osteoblasts, osteocytes, and osteoclasts and is usually dense with a honeycomb-like network. The hardness comes from the inorganic components of bone including calcium phosphate and calcium carbonate. The mineralization by these inorganic materials gives bone its strength and rigidity (Clarke 2008; Kalfas 2001). One of the most common defects in bone is a bone fracture that occurs when excess force is applied or when osteoporosis lowers bone density. As the bone regeneration process takes a long time and the healing process is accompanied by swelling and pain in daily activities, bone substitutes or supports accelerating bone healing are greatly in demand (Burge et al. 2007).
The requirements for bone grafts include having the mechanical strength, chemical composition, and structural architecture that mimic natural bone. The bone graft must be strong and osteoinductive to generate fully functioning bone tissue. Lack of immunogenicity and biocompatibility are also key requirements for bone grafts, like any other biological grafts. To this end, inorganic materials such as hydroxyapatite (Bucholz et al. 1987, 1989) and calcium phosphate (Jarcho 1981) have been widely used as biomaterials that meet these criteria. Similar to other organs and tissues, decellularization strategy could be applied for generation of functional bone grafts. Since bone tissue has physically different features from other organs in terms of interconnectivity, permeability, and mechanical properties, decellularized bone matrix can provide multifaceted mimicry of the native bone tissue, which is rarely achieved by conventional scaffold systems. Several decellularization protocols using detergent containing Triton X-100 (Woods and Gratzer 2005), trypsin (Gerhardt et al. 2013), SDS (Grayson et al. 2008), or enzymes (Fröhlich et al. 2009) and hydrostatic pressure (Hashimoto et al. 2011) have been tested to decellularize bone tissue. In some studies, demineralization using hydrochloric acid (HCl) was used before decellularization, but this process might cause a reduction in active growth factors (e.g. bone morphogenetic proteins) (Pietrzak et al. 2011).
Owing to the osteogenic potential of decellularized bone matrix, several studies have reported that decellularized bone matrix indeed promotes proliferation and osteogenic differentiation of the seeded stem cells (Hashimoto et al. 2011; Lee et al. 2016; Datta et al. 2005). Decellularized bone scaffolds seeded with BMMSCs have shown successful bone regeneration after transplantation into defective calvarial bone (Lee et al. 2016). Other studies have involved culture of stem cells derived from adipose, dental pulp, and umbilical cord blood on decellularized bone ECM supplemented with growth factors to induce osteogenic differentiation for bone regeneration (Fröhlich et al. 2009; Paduano et al. 2016, 2017; Liu et al. 2010). To further expand the applicability and versatility of decellularized bone graft, recent work solubilized the matrix through enzymatic digestion to generate a hydrogel platform (Paduano et al. 2016; Sawkins et al. 2013). Osteogenic cells from calvaria or dental pulp were cultured on hydrogel made from decellularized bone matrix, significantly enhancing proliferation and odontogenic differentiation. These studies employed gelation of bone ECM, which demonstrated the advantages of using a decellularized bone matrix that could be formulated into various 3D scaffolds and used as a functional biomaterial for enhanced bone regeneration.
2.7 Tendon
Tendon is a tough, fibrous connective tissue that connects muscle to bone, usually requiring a high capacity for withstanding a large amount of force or tension during movement and exercise. In tendon tissue, collagen fibers allow tendons to resist tensile stress while proteoglycans give them the ability to resist compression. Tendons need to have sufficient elasticity to store energy for their function and thus control finer movements of the muscle at the same time. Since tendon tends to have a dense and intricate network of collagen and proteoglycans, repairing ruptured tendons is not an easy task (Clayton and Court-Brown 2008). There have been several candidates for tendon grafts including synthetic polymers such as poly(glycolic acid) (PGA), poly(lactic-co-glycolic acid) (PLGA), and polytetrafluoroethylene (PTFE) to provide biological functions as well as mechanical properties (Ouyang et al. 2003; Stoll et al. 2010); however, synthetic materials have shown poor performance in regards to biocompatibility, quality of regeneration, and mechanical durability (Chen et al. 2009).
The decellularization method for tendon repair has been a focus of research because of the naturally aligned, intricate construction of thick collagen and tendon ECMs. With various sources in body, tendon tissues from Achilles (Ko et al. 2016), neck (Ko et al. 2016), tibia (Lee et al. 2013a), flexor (Youngstrom et al. 2013; Martinello et al. 2014), and diaphragm (Deeken et al. 2011) tendon have been decellularized through protocols involving freeze-thaw cycles (Youngstrom et al. 2013; Deeken et al. 2011) and the use of mechanical forces (Ingram et al. 2007) along with the aid of chemical treatments such as non-ionic detergent (e.g. Triton X-100), ionic detergent (e.g. SDS), and zwitterionic detergent (e.g. tributyl phosphate) (Ko et al. 2016; Deeken et al. 2011; Alberti et al. 2015). Importantly, the dense, aligned fibrous structures, mechanical properties, and stiffness of native tendon tissue could be preserved even after the decellularization, which are all essential for improved and prolonged tendon regeneration and function.
For recellularization of tendon scaffolds, stem cells such as BMMSCs, ADSCs, and tendon-derived stem cells that can differentiate into tenocytes can be used (Martinello et al. 2014; Ning et al. 2015; Yin et al. 2013). It was found that the intrinsic alignment of tendon ECMs preserved in the decellularized tendon scaffold could provide a sufficiently favorable microenvironment for enhancing cell distribution, proliferation, and tenogenic differentiation of stem cells. Other cell candidates also include mesenchymal stromal cells, tenocytes, and fibroblasts (Angelidis et al. 2010; Whitlock et al. 2013; Burk et al. 2013). For improving engraftment efficiency, supporting hydrogels can also be used during cellular repopulation into the decellularized tendon tissue (Martinello et al. 2014). In addition, bioreactors that can provide cyclic mechanical stress after cell seeding onto the decellularized tendons could contribute to better cellular orientation and mechanically stronger tendon regeneration (Angelidis et al. 2010).
2.8 Skeletal Muscle
Skeletal muscle is composed of bundles of muscle fibers that together function to generate forces to facilitate voluntary movement (Gans 1982). Even when muscle is damaged, the muscle can repair itself with the biochemical and biophysical cues provided by the ECMs (Hill et al. 2003); however, if the damage exceeds the self-healing capacity, the repair process mediated by ECMs is not efficient, and the lost muscle volume will be replaced with fibrotic scar tissue. Cell transplantation has been attempted to regenerate muscle tissue and restore functions of injured muscle, but cell therapy alone has shown rather marginal regenerative effects on muscle.
With the insufficient therapeutic functional restoration provided by cell transplantation, several synthetic (e.g. poly-ε-caprolactone [PCL]) (Chen et al. 2013) or natural (e.g. fibrin (Layman et al. 2010), gelatin (Layman et al. 2007), and alginate (Ruvinov et al. 2010) biomaterials have been used for treating muscular damage. However, due to immune rejection, low degradability of polymers, bioinertness, and lacking imitation of the natural ECMs, conventional biomaterials were not suitable for the efficient muscle regeneration. The ideal scaffold for addressing muscle damage should replace the native ECMs of musculofascial tissue, which is not an easy task to be accomplished with conventional methods. Therefore, recent studies have focused on using decellularized skeletal muscle tissue to guide skeletal muscle regeneration at the defect site. Decellularized muscle scaffolds are suitable for muscle tissue engineering because they are expected to provide proper biological and biophysical signals to guide differentiation and proliferation of muscle progenitor cells and myoblasts for skeletal muscle regeneration (Stern et al. 2009).
Different approaches for muscle decellularization have been explored using combinations of different treatments. These methods include detergent solutions containing Triton X-100 (Stern et al. 2009; Gillies et al. 2010; Wang et al. 2013; Wolf et al. 2012), SDS (Hurd et al. 2015; Perniconi et al. 2011; DeQuach et al. 2010; Merritt et al. 2010a), or sodium deoxycholate (Wolf et al. 2012), along with other enzymatic treatments involving DNase (Gillies et al. 2010) and trypsin/ethylenediaminetetraacetic acid (EDTA) (Porzionato et al. 2015). These methods for muscle tissue decellularization successfully removed cellular components from native muscle tissue, while retaining muscle ECMs (e.g. collagens, fibronectin, and laminin), growth factors, and GAG components with the intact muscular architectures providing cell-to-matrix interactions (Stern et al. 2009; Gillies et al. 2010; Wang et al. 2013; Wolf et al. 2012).
Decellularized muscle scaffolds can be engineered by culturing cells on the matrix to improve regeneration efficiency. There are usually two types of platforms on which the cells could be seeded. In earlier studies, most cells were seeded onto the decellularized muscle graft itself (Hurd et al. 2015; Perniconi et al. 2011). The cell candidates for muscle regeneration using decellularized muscle matrix include BMMSCs that can differentiate into muscle cells and induce functional recovery after full-thickness defects (Merritt et al. 2010b). Myoblasts, skeletal muscle stem cells, fibroblasts, and endothelial cells have also been used with decellularized muscle matrix in muscular remodeling (Wolf et al. 2012). However, more recent studies have utilized the biochemical properties of ECM from the decellularized matrix in the form of a hydrogel or surface coating instead of using the whole muscle scaffold; this approach gives the materials more benefits in terms of versatility and applicability (DeQuach et al. 2010, 2012; Ungerleider et al. 2015). Even in their solubilized form, the natural muscle-specific proteins, peptides, and proteoglycans, including heparin sulfate and decorin, could promote differentiation and maturation of the skeletal myoblasts (DeQuach et al. 2010). There have been numerous studies on injectable skeletal muscle matrix-based hydrogels that can induce proliferation of smooth muscle cells and skeletal myoblasts to improve neovascularization in hindlimb ischemia models (DeQuach et al. 2012) and in volumetric muscle loss injury models with the addition of MSCs (Merritt et al. 2010b).
3 Whole Organ Decellularization for Functional Organ Replacement
3.1 Heart
As one of the major causes of death, heart failure is a fatal disorder, especially for the many patients with end-stage heart disease. Whole heart transplantation has been considered the only treatment option, but donor shortages and immunological issues have substantially limited the application of this approach. Fabrication of functional heart tissue involves complicated issues in terms of mimicking complex structures with mechanical demands, diverse cellular populations, and physiological functions including heart beating.
In 2008, a perfusion-based whole organ decellularization technique was first suggested for the heart (Ott et al. 2008). For efficient decellularization, various detergent solutions containing SDS, Triton X-100, trypsin, and sodium deoxycholate were tested, and SDS has been proven to be an essential compound for successful decellularization of native heart tissue, though there were some differences in composition of the detergents and perfusion time among the species tested (Fig. 10.2) (Ott et al. 2008; Lu et al. 2013; Kitahara et al. 2016; Oberwallner et al. 2014). When detergent is perfused through the coronary artery, most cellular components, lipids and soluble factors were removed after several days of the decellularization process, but structural ECMs, such as collagens, laminin, and fibronectin, were preserved to provide the proper microenvironment for heart tissue (Ott et al. 2008; Maher 2013). Recently, Kitahara et al. reported a shorter method for preparing whole decellularized porcine heart tissue that is suitable for clinical applications, which would minimize loss of biofunctional molecules in native cardiac tissue and side effects induced by residual DNA contents (Kitahara et al. 2016). More importantly, the cardiac-specific 3D architecture that supports persistent contractions and relaxations during circulation was maintained without any distortion or collapse. Although substantial advances have been made in whole heart decellularization since the first success in rat heart tissue (Ott et al. 2008), fabricating fully functional whole hearts using decellularized matrix is still a challenging task. To scale-up for human use, the process of removing cells while preserving the biochemical microenvironment and mechanical/structural properties of native cardiac tissue needs to be further optimized. Moreover, functional cell incorporation into the matrix needs to be achieved for physiological functioning of the regenerated heart tissue.
Construction of transplantable bioengineered organs via whole organ decellularization and subsequent recellularization through perfusion-based cell seeding methods. Whole organs (e.g. heart, liver, kidney, and lung) from donors can be decellularized using detergents and recellularized with various cell types to reconstitute native organs with the native circulatory system
Recellularization using neonatal cardiac cells and endothelial cells resulted in contracting and functional cardiac tissues (Ott et al. 2008). Later, induced pluripotent stem cell (iPSC)-derived cardiovascular progenitor cells were also used in repopulating the decellularized heart (Lu et al. 2013). The progenitor cells were distributed throughout the whole decellularized heart via a perfusion seeding method and efficiently differentiated into cardiomyocytes, smooth muscle cells, and endothelial cells within histologically relevant regions of the decellularized matrix, resulting in spontaneous contractions of the engineered heart tissue (Fig. 10.2). With the potential to differentiate into myogenic lineages, adult stem cells such as BMMSCs and cord blood-derived mesenchymal stem cells (CBMSCs) have also been exploited as promising cell sources for reconstructing a functional heart using a decellularized heart matrix (Kitahara et al. 2016; Oberwallner et al. 2014; Eitan et al. 2009; Wang et al. 2010).
3.2 Liver
The liver is one of the largest organs with integral functions in metabolism, detoxification, and biosynthesis of various proteins. The liver can be damaged by various innate or acquired conditions such as genetic abnormality, viral infection, and alcoholic liver cirrhosis, but proper therapies to treat patients with end-stage liver diseases have not been developed as an alternative to orthotopic liver transplantation (Lee and Cho 2012). However, substantial shortages of donor livers and immune reactions have limited the practical application of liver transplantations to replace damaged livers. Moreover, as the liver is one of the most highly vascularized and largest organs in our body, previous tissue-engineering scaffolds could not generate the complex and interconnected vascular pathways in liver tissue. Perfusion-based decellularization techniques using whole liver tissue have provided insight into solving the hurdles of liver transplantation. In 2010, a whole organ decellularization technique was used in the fabrication of an artificial liver construct in a rat model (Uygun et al. 2010). Perfusion of an SDS-based detergent solution successfully removed cellular components while retaining the hepatic sinusoidal structural ECM components (e.g. collagen type IV and fibronectin) and basement membranous ECM components of the native liver (e.g. laminin-β1). Along with liver tissue-derived ECM components, the retained GAGs and proteoglycans play important roles in improving hepatic functions of the cultured cells, as well as mechanical support of the matrix (Stuart and Panitch 2008). Other decellularizing detergents that have been used include Triton X-100, sodium deoxycholate, and chelating agents such as EDTA and ethylene glycol tetraacetic acid (EGTA). Importantly, decellularized liver tissue contains intact and interconnected vasculature structures in the matrix even after the cell removal process, which is crucial in reconstructing blood circulation for oxygen transfer and nutrient supply for the cells in the whole matrix.
To develop a functional artificial liver construct, various cell types composing native liver tissues were seeded into the decellularized liver matrix. Primary hepatocytes, stem cell-derived hepatocyte-like cells, liver progenitor cells, and hepatic satellite cells were seeded to endow the inherent functionality of the liver such as protein synthesis, urea metabolism, detoxification, and enzymatic activity (Uygun et al. 2010; Soto-Gutierrez et al. 2011; Mazza et al. 2015; Wang et al. 2014). Endothelial cells were also coseeded with hepatocytes to reconstruct physiologically durable vasculature and reduce thrombosis (Baptista et al. 2011). Establishing proper cell seeding methods is another issue for artificial liver construction because of the large volume of tissue matrix and difficulties in evenly distributing the seeded cells throughout whole decellularized matrix (Baptista et al. 2011; Faulk et al. 2015). Multiple cell perfusion via the portal vein has shown efficient cellular engraftment of over 90% of the infused cells compared to other less efficient approaches including direct parenchymal injection or continuous perfusion method (Uygun et al. 2010; Soto-Gutierrez et al. 2011). For constructing a functional bioengineered liver with a decellularized liver matrix, vasculature modifications using antibodies have also been utilized to improve re-endothelialization after cell seeding (Ko et al. 2015). Recently, enzymatically solubilized whole decellularized liver matrix was used in preparing different formats of liver-specific scaffolds for functionally improved hepatocyte culture and transplantation, which has broadened the utility of decellularized liver matrices (Lee et al. 2013b).
3.3 Kidney
The kidney filters the blood to make urine for the purpose of removing waste and nitrogen from the body. Despite this important role of the kidney, the number of patients who suffer from chronic renal diseases increases every year with approximately 30 million patients in the United States alone (Stats F 2017). In the case of end-stage renal disease, chronic dialysis or kidney transplantation is indispensable for survival of the patients. Even with the accelerated development of dialysis systems, kidney transplantation is often the ultimate curative treatment for end-stage patients. However, the number of kidney donors is insufficient to meet the demand. It is a devastating fact that after kidney transplantation, the recipients often suffer from acute rejection. Thus, tissue-engineering approaches for functional artificial kidney construction appear to be a necessary alternative to renal transplantation.
In the early conception of tissue engineering a kidney, an extracorporeal device using a hemofiltration cartridge was developed as an artificial renal tubule (Humes et al. 2002). Cells with endocrine activity were grown along the inner surface of the cartridge. However, it seemed that a more functional bioscaffold is required for the growth and functions of renal cells or precursor cells in order to replace kidney functions in the long term. Therefore, since 2009, decellularization of the whole kidney has started to be considered for artificial kidney reconstruction (Ross et al. 2009). The whole decellularized kidney matrix can retain its naturally occurring renal architectures and ECM structures for the glomerulus and renal tubule including the abundant growth factors and vasculature to promote cell engraftment and renal regeneration (Ross et al. 2009; Song et al. 2013; Caralt et al. 2015).
The first approach to kidney regeneration using decellularization was reported in 2009, in which the whole rat kidney was decellularized so that pluripotent murine embryonic stem cells could be repopulated in the scaffold (Ross et al. 2009). Later, decellularized kidneys from other species have also been investigated for generation of renal ECM scaffolds, including porcine (Song et al. 2013; Batchelder et al. 2015; Sullivan et al. 2012), monkey (Nakayama et al. 2010), and human (Song et al. 2013). To obtain decellularized whole kidney scaffolds, several treatments can be applied, including SDS (Caralt et al. 2015; Batchelder et al. 2015; Nakayama et al. 2010; McKee and Wingert 2016; Wang et al. 2015), Triton X-100 (Caralt et al. 2015; Nakayama et al. 2010; McKee and Wingert 2016; Wang et al. 2015), trypsin (Caralt et al. 2015), and DNase (Sullivan et al. 2012) or combinations of these treatments. In general, SDS and Triton X-100 are the mostly widely adopted methods to remove cellular components from renal tissue.
Functional renal regeneration requires recellularization with various cells into the 3D ECM architectures of the decellularized kidney tissues. Conventionally, cells are seeded through renal arterial perfusion so that they can be distributed throughout the matrix by the native circulatory system (Song et al. 2013; McKee and Wingert 2016). Diverse cell candidates have been tested to repopulate the kidney matrix, and stem cells are regarded as an ideal cell source for kidney regeneration in terms of immune tolerance and differentiation capacity. Stem cells could differentiate into cell types for renal regeneration such as endothelial cells or renal progenitor cells (Caralt et al. 2015; Bonandrini et al. 2014). Embryonic stem cells (ESCs) have been used to repopulate the decellularized kidney matrix since they can differentiate into renal lineage cells. It appeared that renal ECM scaffolds can sufficiently induce renal differentiation of ESCs without the addition of other factors (Ross et al. 2009). It was also reported that the 3D ECM architectures of the decellularized kidney matrix influences not only cell morphology, adhesion, migration, and proliferation, but also the differentiation of the infused ESCs into the meso-endodermal lineage and renal progenitors (Bonandrini et al. 2014). Endothelial cells derived from iPSCs were also utilized for constructing functional renal tissue using decellularized kidney matrix (Song et al. 2013; Caralt et al. 2015; Du et al. 2016). The endothelial cells successfully repopulated the vasculature in the kidney matrix and formed tubules with metabolic activity.
3.4 Lung
The lung is one of the major organs of the body involved with the respiratory system for gas exchange. As the lung directly comes into contact with the outside atmosphere containing various toxic materials such as viruses, dust, and air pollutants, it is prone to various diseases, including pneumonia, lung cancer, asthma, and cystic fibrosis (Schoene 1999). In severe cases, partial or whole lung transplantation is the only clinical option for patients, but the organ shortages and immune rejection are issues with lung transplantation like with other organs. Therefore, biological scaffolds for lung reconstruction have been identified as an alternative to lung grafts. However, fabricating lung-specific structures such as alveoli and pulmonary capillaries, which are essential for gas exchange, has been a challenge in constructing functional lung grafts for clinical applications.
Earlier studies of lung scaffolds dealt with a whole organ perfusion method for decellularization (Ott et al. 2010; Petersen et al. 2012). Decellularization using perfusion was preferred because the whole lung turns into a functional scaffold with intact alveolar and vascular networks and native ECM structures. In the whole lung perfusion method, detergent solutions are flowed into the organ via blood vessels so that the detergents can successfully remove all cellular components along the capillaries. Generally, chemical solutions such as Triton X-100, sodium deoxycholate, SDS, and 3-[(3-cholamidopropyl) dimethylammonio]-1-propanesulfonate (CHAPS) (Ott et al. 2010; Petersen et al. 2010, 2012; O’Neill et al. 2013) have been applied for lung decellularization. In another study, the lung was cut into smaller pieces for more efficient decellularization, while preserving the ECM components, microstructures, and mechanical properties intrinsic to the lung (O’Neill et al. 2013). The decellularized lungs are usually then reseeded with endothelial cells and pulmonary epithelial cells prior to transplantation into the recipient.
The cell sources for lung grafts include ESCs (Longmire et al. 2012), BMMSCs, and ADSCs (Mendez et al. 2014; Bonvillain et al. 2012) that can differentiate into the cell types needed to reconstitute lung tissues, which includes lung progenitor cells and airway epithelial cells. iPSCs, another type of pluripotent stem cells reprogrammed from somatic cells, have also been used to recellularize the decellularized lung scaffolds (Gilpin et al. 2014; Ren et al. 2015). Ren et al. reported that iPSCs reseeded onto a decellularized lung scaffold differentiated into endothelial and perivascular cells, which opened up a new possibility to advance decellularization techniques to vascularized organs with a larger scale (Ren et al. 2015). Other cell sources for recellularization include human umbilical vein endothelial cells, fetal lung cells (Ott et al. 2010), and lung epithelial cells (Petersen et al. 2010). However, the issue of ensuring that specific cell types settle at desired locations during recellularization still remains, which is mainly due to technical difficulties in cell seeding and localization.
References
Alberti KA, Sun J-Y, Illeperuma WR, Suo Z, Xu Q (2015) Laminar tendon composites with enhanced mechanical properties. J Mater Sci 50(6):2616–2625
Altman AM, Matthias N, Yan Y, Song Y-H, Bai X, Chiu ES, Slakey DP, Alt EU (2008) Dermal matrix as a carrier for in vivo delivery of human adipose-derived stem cells. Biomaterials 29(10):1431–1442
Angelidis IK, Thorfinn J, Connolly ID, Lindsey D, Pham HM, Chang J (2010) Tissue engineering of flexor tendons: the effect of a tissue bioreactor on adipoderived stem cell–seeded and fibroblast-seeded tendon constructs. J Hand Surg 35(9):1466–1472
Badylak SF (1993) Small intestinal submucosa (SIS): a biomaterial conducive to smart tissue remodeling. Tissue Eng: Springer, 179–189
Badylak SF (2004) Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol 12(3):367–377
Badylak SF, Lantz GC, Coffey A, Geddes LA (1989) Small intestinal submucosa as a large diameter vascular graft in the dog. J Surg Res 47(1):74–80
Badylak S, Arnoczky S, Plouhar P, Haut R, Mendenhall V, Clarke R, Horvath C (1999) Naturally occurring extracellular matrix as a scaffold for musculoskeletal repair. Clin Orthop Relat Res 367:S333–S343
Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R (2002) Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 103(2):190–202
Badylak SF, Taylor D, Uygun K (2011) Whole-organ tissue engineering: decellularization and recellularization of three-dimensional matrix scaffolds. Annu Rev Biomed Eng 13:27–53
Baptista PM, Siddiqui MM, Lozier G, Rodriguez SR, Atala A, Soker S (2011) The use of whole organ decellularization for the generation of a vascularized liver organoid. Hepatology 53(2):604–617
Batchelder CA, Martinez ML, Tarantal AF (2015) Natural scaffolds for renal differentiation of human embryonic stem cells for kidney tissue engineering. PLoS One 10(12):e0143849
Bertanha M, Moroz A, Jaldin RG, Silva RA, Rinaldi JC, Golim MA, Felisbino SL, Domingues MA, Sobreira ML, Reis PP (2014a) Morphofunctional characterization of decellularized vena cava as tissue engineering scaffolds. Exp Cell Res 326(1):103–111
Bertanha M, Moroz A, Almeida R, Alves FC, Valério MJA, Moura R, Domingues MAC, Sobreira ML, Deffune E (2014b) Tissue-engineered blood vessel substitute by reconstruction of endothelium using mesenchymal stem cells induced by platelet growth factors. J Vasc Surg 59(6):1677–1685
Bonandrini B, Figliuzzi M, Papadimou E, Morigi M, Perico N, Casiraghi F, Sangalli F, Conti S, Benigni A, Remuzzi A (2014) Recellularization of well-preserved acellular kidney scaffold using embryonic stem cells. Tissue Eng A 20(9-10):1486–1498
Bonvillain RW, Danchuk S, Sullivan DE, Betancourt AM, Semon JA, Eagle ME, Mayeux JP, Gregory AN, Wang G, Townley IK (2012) A nonhuman primate model of lung regeneration: detergent-mediated decellularization and initial in vitro recellularization with mesenchymal stem cells. Tissue Eng A 18(23-24):2437–2452
Bozuk MI, Fearing NM, Leggett PL (2006) Use of decellularized human skin to repair esophageal anastomotic leak in humans. JSLS 10(1):83
Brown A, Farhat W, Merguerian P, Wilson G, Khoury A, Woodhouse K (2002) 22 week assessment of bladder acellular matrix as a bladder augmentation material in a porcine model. Biomaterials 23(10):2179–2190
Brown-Etris M, Cutshall WD, Hiles MC (2002) A new biomaterial derived from small intestine submucosa and developed into a wound matrix device. Wounds 14(4):150–166
Bucholz RW, Carlton A, Holmes RE (1987) Hydroxyapatite and tricalcium phosphate bone graft substitutes. Orthop Clin N Am 18(2):323–334
Bucholz RW, Carlton A, Holmes R (1989) Interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Clin Orthop Relat Res 240:53–62
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475
Burk J, Erbe I, Berner D, Kacza J, Kasper C, Pfeiffer B, Winter K, Brehm W (2013) Freeze-thaw cycles enhance decellularization of large tendons. Tissue Eng Part C Methods 20(4):276–284
Caione P, Capozza N, Zavaglia D, Palombaro G, Boldrini R (2006) In vivo bladder regeneration using small intestinal submucosa: experimental study. Pediatr Surg Int 22(7):593–599
Caralt M, Uzarski JS, Iacob S, Obergfell KP, Berg N, Bijonowski BM, Kiefer KM, Ward HH, Wandinger-Ness A, Miller WM (2015) Optimization and critical evaluation of decellularization strategies to develop renal extracellular matrix scaffolds as biological templates for organ engineering and transplantation. Am J Transplant 15(1):64–75
Chavez-Munoz C, Nguyen KT, Xu W, Hong S-J, Mustoe TA, Galiano RD (2013) Transdifferentiation of adipose-derived stem cells into keratinocyte-like cells: engineering a stratified epidermis. PLoS One 8(12):e80587
Chen R-N, Ho H-O, Tsai Y-T, Sheu M-T (2004) Process development of an acellular dermal matrix (ADM) for biomedical applications. Biomaterials 25(13):2679–2686
Chen J, Xu J, Wang A, Zheng M (2009) Scaffolds for tendon and ligament repair: review of the efficacy of commercial products. Expert Rev Med Devices 6(1):61–73
Chen B-S, Xie H, Zhang S-L, Geng H-Q, Zhou J-M, Pan J, Chen F (2011) Tissue engineering of bladder using vascular endothelial growth factor gene-modified endothelial progenitor cells. Int J Artif Organs 34(12):1137–1146
Chen M-C, Sun Y-C, Chen Y-H (2013) Electrically conductive nanofibers with highly oriented structures and their potential application in skeletal muscle tissue engineering. Acta Biomater 9(3):5562–5572
Cheng EY, Kropp BP (2000) Urologic tissue engineering with small-intestinal submucosa: potential clinical applications. World J Urol 18(1):26–30
Chlupac J, Filova E, Bacakova L (2009) Blood vessel replacement: 50 years of development and tissue engineering paradigms in vascular surgery. Physiol Res 58:S119
Cho S-W, Park HJ, Ryu JH, Kim SH, Kim YH, Choi CY, Lee M-J, Kim J-S, Jang I-S, Kim D-I (2005a) Vascular patches tissue-engineered with autologous bone marrow-derived cells and decellularized tissue matrices. Biomaterials 26(14):1915–1924
Cho S-W, Lim SH, Kim I-K, Hong YS, Kim S-S, Yoo KJ, Park H-Y, Jang Y, Chang BC, Choi CY (2005b) Small-diameter blood vessels engineered with bone marrow–derived cells. Ann Surg 241(3):506
Cho SW, Lim JE, Chu HS, Hyun HJ, Choi CY, Hwang KC, Yoo KJ, Kim DI, Kim BS (2006) Enhancement of in vivo endothelialization of tissue-engineered vascular grafts by granulocyte colony-stimulating factor. J Biomed Mater Res A 76((2):252–263
Chung SY, Krivorov NP, Rausei V, Thomas L, Frantzen M, Landsittel D, Kang YM, Chon CH, Ng CS, Fuchs GJ (2005) Bladder reconstitution with bone marrow derived stem cells seeded on small intestinal submucosa improves morphological and molecular composition. J Urol 174(1):353–359
Clarke B (2008) Normal bone anatomy and physiology. Clin J Am Soc Nephrol 3(Supplement 3):S131–S139
Clayton RA, Court-Brown CM (2008) The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 39(12):1338–1344
Cobb MA, Badylak SF, Janas W, Simmons-Byrd A, Boop FA (1999) Porcine small intestinal submucosa as a dural substitute. Surg Neurol 51(1):99–104
Consolo F, Brizzola S, Tremolada G, Grieco V, Riva F, Acocella F, Fiore G, Soncini M (2016) A dynamic distention protocol for whole-organ bladder decellularization: histological and biomechanical characterization of the acellular matrix. J Tissue Eng Regen Med 10(2):E101–E112
Datta N, Holtorf HL, Sikavitsas VI, Jansen JA, Mikos AG (2005) Effect of bone extracellular matrix synthesized in vitro on the osteoblastic differentiation of marrow stromal cells. Biomaterials 26(9):971–977
Davis NF, Mooney R, Callanan A, Flood HD, McGloughlin TM (2011) Augmentation cystoplasty and extracellular matrix scaffolds: an ex vivo comparative study with autogenous detubularised ileum. PLoS One 6(5):e20323
De Coppi P, Callegari A, Chiavegato A, Gasparotto L, Piccoli M, Taiani J, Pozzobon M, Boldrin L, Okabe M, Cozzi E (2007) Amniotic fluid and bone marrow derived mesenchymal stem cells can be converted to smooth muscle cells in the cryo-injured rat bladder and prevent compensatory hypertrophy of surviving smooth muscle cells. J Urol 177(1):369–376
Deeken C, White A, Bachman S, Ramshaw B, Cleveland D, Loy T, Grant S (2011) Method of preparing a decellularized porcine tendon using tributyl phosphate. J Biomed Mater Res B Appl Biomater 96((2):199–206
DeQuach JA, Mezzano V, Miglani A, Lange S, Keller GM, Sheikh F, Christman KL (2010) Simple and high yielding method for preparing tissue specific extracellular matrix coatings for cell culture. PLoS One 5(9):e13039
DeQuach JA, Lin JE, Cam C, Hu D, Salvatore MA, Sheikh F, Christman KL (2012) Injectable skeletal muscle matrix hydrogel promotes neovascularization and muscle cell infiltration in a hindlimb ischemia model. Eur Cells Mater 23:400
Dora KA (2001) Cell-cell communication in the vessel wall. Vasc Med 6(1):43–50
Du C, Narayanan K, Leong MF, Ibrahim MS, Chua YP, Khoo VMH, Wan AC (2016) Functional kidney bioengineering with pluripotent stem-cell-derived renal progenitor cells and decellularized kidney scaffolds. Adv Healthcare Mater 5(16):2080–2091
Eaglstein WH, Falanga V (1997) Tissue engineering and the development of Apligraf®, a human skin equivalent. Clin Ther 19(5):894–905
Eitan Y, Sarig U, Dahan N, Machluf M (2009) Acellular cardiac extracellular matrix as a scaffold for tissue engineering: in vitro cell support, remodeling, and biocompatibility. Tissue Eng Part C Methods 16(4):671–683
Faulk DM, Wildemann JD, Badylak SF (2015) Decellularization and cell seeding of whole liver biologic scaffolds composed of extracellular matrix. J Clin Exp Hepatol 5(1):69–80
Franklin M, Gonzalez J, Michaelson R, Glass J, Chock D (2002) Preliminary experience with new bioactive prosthetic material for repair of hernias in infected fields. Hernia 6(4):171–174
Fröhlich M, Grayson WL, Marolt D, Gimble JM, Kregar-Velikonja N, Vunjak-Novakovic G (2009) Bone grafts engineered from human adipose-derived stem cells in perfusion bioreactor culture. Tissue Eng A 16(1):179–189
Gans C (1982) Fiber architecture and muscle function. Exerc Sport Sci Rev 10(1):160–207
Gerhardt LC, Widdows KL, Erol MM, Nandakumar A, Roqan IS, Ansari T, Boccaccini AR (2013) Neocellularization and neovascularization of nanosized bioactive glass-coated decellularized trabecular bone scaffolds. J Biomed Mater Res A 101((3):827–841
Gilbert TW, Sellaro TL, Badylak SF (2006) Decellularization of tissues and organs. Biomaterials 27(19):3675–3683
Gillies AR, Smith LR, Lieber RL, Varghese S (2010) Method for decellularizing skeletal muscle without detergents or proteolytic enzymes. Tissue Eng Part C Methods 17(4):383–389
Gilpin SE, Ren X, Okamoto T, Guyette JP, Mou H, Rajagopal J, Mathisen DJ, Vacanti JP, Ott HC (2014) Enhanced lung epithelial specification of human induced pluripotent stem cells on decellularized lung matrix. Ann Thorac Surg 98(5):1721–1729
Go T, Jungebluth P, Baiguero S, Asnaghi A, Martorell J, Ostertag H, Mantero S, Birchall M, Bader A, Macchiarini P (2010) Both epithelial cells and mesenchymal stem cell–derived chondrocytes contribute to the survival of tissue-engineered airway transplants in pigs. J Thorac Cardiovasc Surg 139(2):437–443
Gonfiotti A, Jaus MO, Barale D, Baiguera S, Comin C, Lavorini F, Fontana G, Sibila O, Rombolà G, Jungebluth P (2014) The first tissue-engineered airway transplantation: 5-year follow-up results. Lancet 383(9913):238–244
Gray FL, Turner CG, Ahmed A, Calvert CE, Zurakowski D, Fauza DO (2012) Prenatal tracheal reconstruction with a hybrid amniotic mesenchymal stem cells–engineered construct derived from decellularized airway. J Pediatr Surg 47(6):1072–1079
Grayson WL, Bhumiratana S, Cannizzaro C, Chao P-HG, Lennon DP, Caplan AI, Vunjak-Novakovic G (2008) Effects of initial seeding density and fluid perfusion rate on formation of tissue-engineered bone. Tissue Eng A 14(11):1809–1820
Grillo HC (2002) Tracheal replacement: a critical review. Ann Thorac Surg 73(6):1995–2004
Gui L, Muto A, Chan SA, Breuer CK, Niklason LE (2009) Development of decellularized human umbilical arteries as small-diameter vascular grafts. Tissue Eng A 15(9):2665–2676
Guyette JP, Gilpin SE, Charest JM, Tapias LF, Ren X, Ott HC (2014) Perfusion decellularization of whole organs. Nat Protoc 9(6):1451
Haag J, Baiguera S, Jungebluth P, Barale D, Del Gaudio C, Castiglione F, Bianco A, Comin CE, Ribatti D, Macchiarini P (2012) Biomechanical and angiogenic properties of tissue-engineered rat trachea using genipin cross-linked decellularized tissue. Biomaterials 33(3):780–789
Hashimoto Y, Funamoto S, Kimura T, Nam K, Fujisato T, Kishida A (2011) The effect of decellularized bone/bone marrow produced by high-hydrostatic pressurization on the osteogenic differentiation of mesenchymal stem cells. Biomaterials 32(29):7060–7067
Hill M, Wernig A, Goldspink G (2003) Muscle satellite (stem) cell activation during local tissue injury and repair. J Anat 203(1):89–99
Hodde J (2002) Naturally occurring scaffolds for soft tissue repair and regeneration. Tissue Eng 8(2):295–308
Hoganson DM, O’Doherty EM, Owens GE, Harilal DO, Goldman SM, Bowley CM, Neville CM, Kronengold RT, Vacanti JP (2010) The retention of extracellular matrix proteins and angiogenic and mitogenic cytokines in a decellularized porcine dermis. Biomaterials 31(26):6730–6737
Huang S-P, Hsu C-C, Chang S-C, Wang C-H, Deng S-C, Dai N-T, Chen T-M, Chan JY-H, Chen S-G, Huang S-M (2012) Adipose-derived stem cells seeded on acellular dermal matrix grafts enhance wound healing in a murine model of a full-thickness defect. Ann Plast Surg 69(6):656–662
Hubbell JA (1995) Biomaterials in tissue engineering. Nat Biotechnol 13(6):565–576
Humes HD, Fissell WH, Weitzel WF, Buffington DA, Westover AJ, MacKay SM, Gutierrez JM (2002) Metabolic replacement of kidney function in uremic animals with a bioartificial kidney containing human cells. Am J Kidney Dis 39(5):1078–1087
Hurd SA, Bhatti NM, Walker AM, Kasukonis BM, Wolchok JC (2015) Development of a biological scaffold engineered using the extracellular matrix secreted by skeletal muscle cells. Biomaterials 49:9–17
Huynh T, Abraham G, Murray J, Brockbank K, Hagen P-O, Sullivan S (1999) Remodeling of an acellular collagen graft into a physiologically responsive neovessel. Nat Biotechnol 17(11):1083–1086
Ingram JH, Korossis S, Howling G, Fisher J, Ingham E (2007) The use of ultrasonication to aid recellularization of acellular natural tissue scaffolds for use in anterior cruciate ligament reconstruction. Tissue Eng 13(7):1561–1572
Jarcho M (1981) Calcium phosphate ceramics as hard tissue prosthetics. Clin Orthop Relat Res 157:259–278
Jones JS, Rackley RR, Berglund R, Abdelmalak JB, Deorco G, Vasavada SP (2005) Porcine small intestinal submucosa as a percutaneous mid-urethral sling: 2-year results. BJU Int 96(1):103–106
Jungebluth P, Macchiarini P (2014) Airway transplantation. Thorac Surg Clin 24(1):97–106
Jungebluth P, Alici E, Baiguera S, Blomberg P, Bozóky B, Crowley C, Einarsson O, Gudbjartsson T, Le Guyader S, Henriksson G (2011) Tracheobronchial transplantation with a stem-cell-seeded bioartificial nanocomposite: a proof-of-concept study. Lancet 378(9808):1997–2004
Jungebluth P, Haag JC, Sjöqvist S, Gustafsson Y, Rodríguez AB, Del Gaudio C, Bianco A, Dehnisch I, Uhlén P, Baiguera S (2014) Tracheal tissue engineering in rats. Nat Protoc 9(9):2164–2179
Kalfas IH (2001) Principles of bone healing. Neurosurg Focus 10(4):1–4
Kaushal S, Amiel GE, Guleserian KJ, Shapira OM, Perry T, Sutherland FW, Rabkin E, Moran AM, Schoen FJ, Atala A (2001) Functional small-diameter neovessels created using endothelial progenitor cells expanded ex vivo. Nat Med 7(9):1035–1040
Kimuli M, Eardley I, Southgate J (2004) In vitro assessment of decellularized porcine dermis as a matrix for urinary tract reconstruction. BJU Int 94(6):859–866
Kitahara H, Yagi H, Tajima K, Okamoto K, Yoshitake A, Aeba R, Kudo M, Kashima I, Kawaguchi S, Hirano A (2016) Heterotopic transplantation of a decellularized and recellularized whole porcine heart. Interact Cardiovasc Thorac Surg 22(5):571–579
Ko IK, Peng L, Peloso A, Smith CJ, Dhal A, Deegan DB, Zimmerman C, Clouse C, Zhao W, Shupe TD (2015) Bioengineered transplantable porcine livers with re-endothelialized vasculature. Biomaterials 40:72–79
Ko E, Alberti K, Lee JS, Yang K, Jin Y, Shin J, Yang HS, Xu Q, Cho S-W (2016) Nanostructured tendon-derived scaffolds for enhanced bone regeneration by human adipose-derived stem cells. ACS Appl Mater Interfaces 8(35):22819–22829
Kropp BP, Cheng EY, Lin H-k, Zhang Y (2004) Reliable and reproducible bladder regeneration using unseeded distal small intestinal submucosa. J Urol 172((4):1710–1713
Kudish HG (1957) The use of polyvinyl sponge for experimental cystoplasty. J Urol 78(3):232–235
L’Heureux N, Dusserre N, Konig G, Victor B, Keire P, Wight TN, Chronos NA, Kyles AE, Gregory CR, Hoyt G (2006) Human Tissue Engineered Blood Vessel For Adult Arterial Revascularization. Nat Med 12(3):361
L’Heureux N, McAllister TN, de la Fuente LM (2007) Tissue-engineered blood vessel for adult arterial revascularization. N Engl J Med 357(14):1451–1453
Layman H, Spiga M-G, Brooks T, Pham S, Webster KA, Andreopoulos FM (2007) The effect of the controlled release of basic fibroblast growth factor from ionic gelatin-based hydrogels on angiogenesis in a murine critical limb ischemic model. Biomaterials 28(16):2646–2654
Layman H, Rahnemai-Azar AA, Pham SM, Tsechpenakis G, Andreopoulos FM (2010) Synergistic angiogenic effect of codelivering fibroblast growth factor 2 and granulocyte-colony stimulating factor from fibrin scaffolds and bone marrow transplantation in critical limb ischemia. Tissue Eng A 17(1-2):243–254
Lee JS, Cho S-W (2012) Liver tissue engineering: Recent advances in the development of a bio-artificial liver. Biotechnol Bioprocess Eng 17(3):427–438
Lee KI, Lee JS, Kim JG, Kang KT, Jang JW, Shim YB, Moon SH (2013a) Mechanical properties of decellularized tendon cultured by cyclic straining bioreactor. J Biomed Mater Res A 101(11):3152–3158
Lee JS, Shin J, Park H-M, Kim Y-G, Kim B-G, Oh J-W, Cho S-W (2013b) Liver extracellular matrix providing dual functions of two-dimensional substrate coating and three-dimensional injectable hydrogel platform for liver tissue engineering. Biomacromolecules 15(1):206–218
Lee JS, Lee K, Moon SH, Chung HM, Lee JH, Um SH, Kim DI, Cho SW (2014) Mussel-inspired cell-adhesion peptide modification for enhanced endothelialization of decellularized blood vessels. Macromol Biosci 14(8):1181–1189
Lee DJ, Diachina S, Lee YT, Zhao L, Zou R, Tang N, Han H, Chen X, Ko C-C (2016) Decellularized bone matrix grafts for calvaria regeneration. J Tissue Eng 7:2041731416680306
Liu G, Li Y, Sun J, Zhou H, Zhang W, Cui L, Cao Y (2010) In vitro and in vivo evaluation of osteogenesis of human umbilical cord blood-derived mesenchymal stem cells on partially demineralized bone matrix. Tissue Eng A 16(3):971–982
Livesey SA, Herndon DN, Hollyoak MA, Atkinson YH, Nag A (1995) Transplanted acellular allograft dermal matrix: potential as a template for the reconstruction of viable dermis. Transplantation 60(1):1–9
Longmire TA, Ikonomou L, Hawkins F, Christodoulou C, Cao Y, Jean J, Kwok LW, Mou H, Rajagopal J, Shen SS (2012) Efficient derivation of purified lung and thyroid progenitors from embryonic stem cells. Cell Stem Cell 10(4):398–411
Lu T-Y, Lin B, Kim J, Sullivan M, Tobita K, Salama G, Yang L (2013) Repopulation of decellularized mouse heart with human induced pluripotent stem cell-derived cardiovascular progenitor cells. Nat Commun 4:2307
Luo J-C, Chen W, Chen X-H, Qin T-W, Huang Y-C, Xie H-Q, Li X-Q, Qian Z-Y, Yang Z-M (2011) A multi-step method for preparation of porcine small intestinal submucosa (SIS). Biomaterials 32(3):706–713
Macchiarini P, Jungebluth P, Go T, Asnaghi MA, Rees LE, Cogan TA, Dodson A, Martorell J, Bellini S, Parnigotto PP (2008) Clinical transplantation of a tissue-engineered airway. Lancet 372(9655):2023–2030
MacLeod T, Sarathchandra P, Williams G, Sanders R, Green C (2004) Evaluation of a porcine origin acellular dermal matrix and small intestinal submucosa as dermal replacements in preventing secondary skin graft contraction. Burns 30(5):431–437
Maher B (2013) How to build a heart. Nature 499(7456):20
Martinello T, Bronzini I, Volpin A, Vindigni V, Maccatrozzo L, Caporale G, Bassetto F, Patruno M (2014) Successful recellularization of human tendon scaffolds using adipose-derived mesenchymal stem cells and collagen gel. J Tissue Eng Regen Med 8(8):612–619
Mazza G, Rombouts K, Hall AR, Urbani L, Luong TV, Al-Akkad W, Longato L, Brown D, Maghsoudlou P, Dhillon AP (2015) Decellularized human liver as a natural 3D-scaffold for liver bioengineering and transplantation. Sci Rep 5:13079
McKee RA, Wingert RA (2016) Repopulating decellularized kidney scaffolds: an avenue for ex vivo organ generation. Materials 9(3):190
Mendez JJ, Ghaedi M, Steinbacher D, Niklason LE (2014) Epithelial cell differentiation of human mesenchymal stromal cells in decellularized lung scaffolds. Tissue Eng A 20(11-12):1735–1746
Merritt EK, Hammers DW, Tierney M, Suggs LJ, Walters TJ, Farrar RP (2010a) Functional assessment of skeletal muscle regeneration utilizing homologous extracellular matrix as scaffolding. Tissue Eng A 16(4):1395–1405
Merritt EK, Cannon MV, Hammers DW, Le LN, Gokhale R, Sarathy A, Song TJ, Tierney MT, Suggs LJ, Walters TJ (2010b) Repair of traumatic skeletal muscle injury with bone-marrow-derived mesenchymal stem cells seeded on extracellular matrix. Tissue Eng A 16(9):2871–2881
Misseri R, Cain MP, Casale AJ, Kaefer M, Meldrum KK, Rink RC (2005) Small intestinal submucosa bladder neck slings for incontinence associated with neuropathic bladder. J Urol 174(4):1680–1682
Monsour M, Mohammed R, Gorham S, French D, Scott R (1987) An assessment of a collagen/vicryl composite membrane to repair defects of the urinary bladder in rabbits. Urol Res 15(4):235–238
Nakayama KH, Batchelder CA, Lee CI, Tarantal AF (2010) Decellularized rhesus monkey kidney as a three-dimensional scaffold for renal tissue engineering. Tissue Eng A 16(7):2207–2216
Neff LP, Tillman BW, Yazdani SK, Machingal MA, Yoo JJ, Soker S, Bernish BW, Geary RL, Christ GJ (2011) Vascular Smooth muscle enhances functionality of tissue-engineered blood vessels in vivo. J Vasc Surg 53(2):426–434
Nie C, Yang D, Morris SF (2009) Local delivery of adipose-derived stem cells via acellular dermal matrix as a scaffold: a new promising strategy to accelerate wound healing. Med Hypotheses 72(6):679–682
Ning L-J, Zhang Y-J, Zhang Y, Qing Q, Jiang Y-L, Yang J-L, Luo J-C, Qin T-W (2015) The utilization of decellularized tendon slices to provide an inductive microenvironment for the proliferation and tenogenic differentiation of stem cells. Biomaterials 52:539–550
O’brien FJ (2011) Biomaterials & scaffolds for tissue engineering. Mater Today 14(3):88–95
O’Neill JD, Anfang R, Anandappa A, Costa J, Javidfar J, Wobma HM, Singh G, Freytes DO, Bacchetta MD, Sonett JR (2013) Decellularization of human and porcine lung tissues for pulmonary tissue engineering. Ann Thorac Surg 96(3):1046–1056
Obara T, Matsuura S, Narita S, Satoh S, Tsuchiya N, Habuchi T (2006) Bladder acellular matrix grafting regenerates urinary bladder in the spinal cord injury rat. Urology 68(4):892–897
Oberwallner B, Brodarac A, Choi YH, Saric T, Anić P, Morawietz L, Stamm C (2014) Preparation of cardiac extracellular matrix scaffolds by decellularization of human myocardium. J Biomed Mater Res A 102(9):3263–3272
Oelschlager BK, Barreca M, Chang L, Pellegrini CA (2003) The use of small intestine submucosa in the repair of paraesophageal hernias: initial observations of a new technique. Am J Surg 186(1):4–8
Oliveira AC, Garzón I, Ionescu AM, Carriel V, de la Cruz Cardona J, González-Andrades M, del Mar Pérez M, Alaminos M, Campos A (2013) Evaluation of small intestine grafts decellularization methods for corneal tissue engineering. PLoS One 8(6):e66538
Ono I, Tateshita T, Inoue M (1999) Effects of a collagen matrix containing basic fibroblast growth factor on wound contraction. J Biomed Mater Res A 48(5):621–630
Ott HC, Matthiesen TS, Goh S-K, Black LD, Kren SM, Netoff TI, Taylor DA (2008) Perfusion-decellularized matrix: using nature’s platform to engineer a bioartificial heart. Nat Med 14(2):213–221
Ott HC, Clippinger B, Conrad C, Schuetz C, Pomerantseva I, Ikonomou L, Kotton D, Vacanti JP (2010) Regeneration and orthotopic transplantation of a bioartificial lung. Nat Med 16(8):927–933
Ouyang HW, Goh JC, Thambyah A, Teoh SH, Lee EH (2003) Knitted poly-lactide-co-glycolide scaffold loaded with bone marrow stromal cells in repair and regeneration of rabbit Achilles tendon. Tissue Eng 9(3):431–439
Paduano F, Marrelli M, White LJ, Shakesheff KM, Tatullo M (2016) Odontogenic differentiation of human dental pulp stem cells on hydrogel scaffolds derived from decellularized bone extracellular matrix and collagen type I. PLoS One 11(2):e0148225
Paduano F, Marrelli M, Alom N, Amer M, White LJ, Shakesheff KM, Tatullo M (2017) Decellularized bone extracellular matrix and human dental pulp stem cells as a construct for bone regeneration. J Biomater Sci Polym Ed 28(8):730–748
Partington L, Mordan N, Mason C, Knowles J, Kim H, Lowdell M, Birchall M, Wall I (2013) Biochemical changes caused by decellularization may compromise mechanical integrity of tracheal scaffolds. Acta Biomater 9(2):5251–5261
Patil PB, Chougule PB, Kumar VK, Almström S, Bäckdahl H, Banerjee D, Herlenius G, Olausson M, Sumitran-Holgersson S (2013) Recellularization of acellular human small intestine using bone marrow stem cells. Stem Cells Transl Med 2(4):307–315
Perniconi B, Costa A, Aulino P, Teodori L, Adamo S, Coletti D (2011) The pro-myogenic environment provided by whole organ scale acellular scaffolds from skeletal muscle. Biomaterials 32(31):7870–7882
Petersen TH, Calle EA, Zhao L, Lee EJ, Gui L, Raredon MB, Gavrilov K, Yi T, Zhuang ZW, Breuer C (2010) Tissue-engineered lungs for in vivo implantation. Science 329(5991):538–541
Petersen TH, Calle EA, Colehour MB, Niklason LE (2012) Matrix composition and mechanics of decellularized lung scaffolds. Cells Tissues Organs 195(3):222–231
Pietrzak WS, Ali SN, Chitturi D, Jacob M, Woodell-May JE (2011) BMP depletion occurs during prolonged acid demineralization of bone: characterization and implications for graft preparation. Cell Tissue Bank 12(2):81–88
Place ES, Evans ND, Stevens MM (2009) Complexity in biomaterials for tissue engineering. Nat Mater 8(6):457
Porzionato A, Sfriso MM, Pontini A, Macchi V, Petrelli L, Pavan PG, Natali AN, Bassetto F, Vindigni V, De Caro R (2015) Decellularized human skeletal muscle as biologic scaffold for reconstructive surgery. Int J Mol Sci 16(7):14808–14831
Prevel CD, Eppley BL, Summerlin D-J, Sidner R, Jackson JR, McCarty M, Badylak SF (1995) Small intestinal submucosa: utilization as a wound dressing in full-thickness rodent wounds. Ann Plast Surg 35(4):381–388
Quint C, Kondo Y, Manson RJ, Lawson JH, Dardik A, Niklason LE (2011) Decellularized tissue-engineered blood vessel as an arterial conduit. Proc Natl Acad Sci 108(22):9214–9219
Reddy PP, Barrieras DJ, Wilson G, Bägli DJ, McLORIE GA, Khoury AE, Merguerian PA (2000) Regeneration of functional bladder substitutes using large segment acellular matrix allografts in a porcine model. J Urol 164(3:936–941
Reing JE, Brown BN, Daly KA, Freund JM, Gilbert TW, Hsiong SX, Huber A, Kullas KE, Tottey S, Wolf MT (2010) The effects of processing methods upon mechanical and biologic properties of porcine dermal extracellular matrix scaffolds. Biomaterials 31(33):8626–8633
Ren X, Moser PT, Gilpin SE, Okamoto T, Wu T, Tapias LF, Mercier FE, Xiong L, Ghawi R, Scadden DT (2015) Engineering pulmonary vasculature in decellularized rat and human lungs. Nat Biotechnol 33(10):1097–1102
Rosario DJ, Reilly GC, Ali Salah E, Glover M, Bullock AJ, MacNeil S (2008) Decellularization and sterilization of porcine urinary bladder matrix for tissue engineering in the lower urinary tract. Regen Med 3(2):145–146
Ross EA, Williams MJ, Hamazaki T, Terada N, Clapp WL, Adin C, Ellison GW, Jorgensen M, Batich CD (2009) Embryonic stem cells proliferate and differentiate when seeded into kidney scaffolds. J Am Soc Nephrol 20(11):2338–2347
Ruszczak Z (2003) Effect of collagen matrices on dermal wound healing. Adv Drug Deliv Rev 55(12):1595–1611
Ruvinov E, Leor J, Cohen S (2010) The effects of controlled HGF delivery from an affinity-binding alginate biomaterial on angiogenesis and blood perfusion in a hindlimb ischemia model. Biomaterials 31(16):4573–4582
Samouillan V, Dandurand-Lods J, Lamure A, Maurel E, Lacabanne C, Gerosa G, Venturini A, Casarotto D, Gherardini L, Spina M (1999) Thermal analysis characterization of aortic tissues for cardiac valve bioprostheses. J Biomed Mater Res 46(4):531–538
Sawkins M, Bowen W, Dhadda P, Markides H, Sidney L, Taylor A, Rose F, Badylak S, Shakesheff K, White L (2013) Hydrogels derived from demineralized and decellularized bone extracellular matrix. Acta Biomater 9(8):7865–7873
Schaner PJ, Martin ND, Tulenko TN, Shapiro IM, Tarola NA, Leichter RF, Carabasi RA, DiMuzio PJ (2004) Decellularized vein as a potential scaffold for vascular tissue engineering. J Vasc Surg 40(1):146–153
Schoene RB (1999) Lung disease at high altitude. Hypoxia: Springer, pp 47–56
Sievert K-D, Fandel T, Wefer J, Gleason CA, Nunes L, Dahiya R, Tanagho EA (2006) Collagen I: III ratio in canine heterologous bladder acellular matrix grafts. World J Urol 24(1):101–109
Soergel TM, Cain MP, Misseri R, Gardner TA, Koch MO, Rink RC (2004) Transitional cell carcinoma of the bladder following augmentation cystoplasty for the neuropathic bladder. J Urol 172((4):1649–1652
Song JJ, Guyette JP, Gilpin SE, Gonzalez G, Vacanti JP, Ott HC (2013) Regeneration and experimental orthotopic transplantation of a bioengineered kidney. Nat Med 19(5):646–651
Soto-Gutierrez A, Zhang L, Medberry C, Fukumitsu K, Faulk D, Jiang H, Reing J, Gramignoli R, Komori J, Ross M (2011) A whole-organ regenerative medicine approach for liver replacement. Tissue Eng Part C Methods 17(6):677–686
Stats F (2017) National Chronic Kidney Disease Fact Sheet
Stern MM, Myers RL, Hammam N, Stern KA, Eberli D, Kritchevsky SB, Soker S, Van Dyke M (2009) The influence of extracellular matrix derived from skeletal muscle tissue on the proliferation and differentiation of myogenic progenitor cells ex vivo. Biomaterials 30(12):2393–2399
Stoll C, John T, Endres M, Rosen C, Kaps C, Kohl B, Sittinger M, Ertel W, Schulze-Tanzil G (2010) Extracellular matrix expression of human tenocytes in three-dimensional air–liquid and PLGA cultures compared with tendon tissue: Implications for tendon tissue engineering. J Orthop Res 28(9):1170–1177
Stuart K, Panitch A (2008) Influence of chondroitin sulfate on collagen gel structure and mechanical properties at physiologically relevant levels. Biopolymers 89(10):841–851
Sullivan DC, Mirmalek-Sani S-H, Deegan DB, Baptista PM, Aboushwareb T, Atala A, Yoo JJ (2012) Decellularization methods of porcine kidneys for whole organ engineering using a high-throughput system. Biomaterials 33(31):7756–7764
Syed O, Walters NJ, Day RM, Kim H-W, Knowles JC (2014) Evaluation of decellularization protocols for production of tubular small intestine submucosa scaffolds for use in oesophageal tissue engineering. Acta Biomater 10(12):5043–5054
Takami Y, Matsuda T, Yoshitake M, Hanumadass M, Walter R (1996) Dispase/detergent treated dermal matrix as a dermal substitute. Burns 22(3):182–190
Totonelli G, Maghsoudlou P, Garriboli M, Riegler J, Orlando G, Burns AJ, Sebire NJ, Smith VV, Fishman JM, Ghionzoli M (2012) A rat decellularized small bowel scaffold that preserves villus-crypt architecture for intestinal regeneration. Biomaterials 33(12):3401–3410
Ungerleider J, Johnson T, Rao N, Christman K (2015) Fabrication and characterization of injectable hydrogels derived from decellularized skeletal and cardiac muscle. Methods 84:53–59
Urakami S, Shiina H, Enokida H, Kawamoto K, Kikuno N, Fandel T, Vejdani K, Nunes L, Igawa M, Tanagho EA (2007) Functional improvement in spinal cord injury-induced neurogenic bladder by bladder augmentation using bladder acellular matrix graft in the rat. World J Urol 25(2):207–213
Uygun BE, Soto-Gutierrez A, Yagi H, Izamis M-L, Guzzardi MA, Shulman C, Milwid J, Kobayashi N, Tilles A, Berthiaume F (2010) Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Nat Med 16(7):814–820
Wainwright D (1995) Use of an acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. Burns 21(4):243–248
Wang B, Borazjani A, Tahai M, de Jongh Curry AL, Simionescu DT, Guan J, To, F, Elder SH, Liao J (2010) Fabrication of cardiac patch with decellularized porcine myocardial scaffold and bone marrow mononuclear cells. J Biomed Mater Res A 94(4):1100–1110
Wang L, Johnson JA, Chang DW, Zhang Q (2013) Decellularized musculofascial extracellular matrix for tissue engineering. Biomaterials 34(11):2641–2654
Wang X, Cui J, Zhang BQ, Zhang H, Bi Y, Kang Q, Wang N, Bie P, Yang Z, Wang H (2014) Decellularized liver scaffolds effectively support the proliferation and differentiation of mouse fetal hepatic progenitors. J Biomed Mater Res A 102(4):1017–1025
Wang Y, Bao J, Wu Q, Zhou Y, Li Y, Wu X, Shi Y, Li L, Bu H (2015) Method for perfusion decellularization of porcine whole liver and kidney for use as a scaffold for clinical-scale bioengineering engrafts. Xenotransplantation 22(1):48–61
Whitlock P, Seyler T, Northam C, Smith T, Poehling G, Koman L, Van Dyke M (2013) Effect of cyclic strain on tensile properties of a naturally derived, decellularized tendon scaffold seeded with allogeneic tenocytes and associated messenger RNA expression. J Surg Orthop Adv 22(3):224–232
Wilson GJ, Courtman DW, Klement P, Lee JM, Yeger H (1995) Acellular matrix: a biomaterials approach for coronary artery bypass and heart valve replacement. Ann Thorac Surg 60:S353–S358
Wolf MT, Daly KA, Reing JE, Badylak SF (2012) Biologic scaffold composed of skeletal muscle extracellular matrix. Biomaterials 33(10):2916–2925
Woods T, Gratzer PF (2005) Effectiveness of three extraction techniques in the development of a decellularized bone–anterior cruciate ligament–bone graft. Biomaterials 26(35):7339–7349
Wu S, Liu Y, Bharadwaj S, Atala A, Zhang Y (2011) Human urine-derived stem cells seeded in a modified 3D porous small intestinal submucosa scaffold for urethral tissue engineering. Biomaterials 32(5):1317–1326
Yazdani SK, Watts B, Machingal M, Jarajapu YP, Van Dyke ME, Christ GJ (2009) Smooth muscle cell seeding of decellularized scaffolds: the importance of bioreactor preconditioning to development of a more native architecture for tissue-engineered blood vessels. Tissue Eng A 15(4):827–840
Yin Z, Chen X, Zhu T, Hu J-j, Song H-x, Shen W-l, Jiang L-y, Heng BC, Ji J-f, Ouyang H-W (2013) The effect of decellularized matrices on human tendon stem/progenitor cell differentiation and tendon repair. Acta Biomater 9(12):9317–9329
Yoo JJ, Meng J, Oberpenning F, Atala A (1998) Bladder augmentation using allogenic bladder submucosa seeded with cells. Urology 51(2):221–225
Youngstrom DW, Barrett JG, Jose RR, Kaplan DL (2013) Functional characterization of detergent-decellularized equine tendon extracellular matrix for tissue engineering applications. PLoS One 8(5):e64151
Youssif M, Shiina H, Urakami S, Gleason C, Nunes L, Igawa M, Enokida H, Tanagho EA, Dahiya R (2005) Effect of vascular endothelial growth factor on regeneration of bladder acellular matrix graft: histologic and functional evaluation. Urology 66(1):201–207
Zhang F, Zhu C, Oswald T, Lei M-P, Lineaweaver WC (2003) Porcine small intestinal submucosa as a carrier for skin flap prefabrication. Ann Plast Surg 51(5):488–492
Zhao Y, Zhang S, Zhou J, Wang J, Zhen M, Liu Y, Chen J, Qi Z (2010) The development of a tissue-engineered artery using decellularized scaffold and autologous ovine mesenchymal stem cells. Biomaterials 31(2):296–307
Zhao Y, Zhang Z, Wang J, Yin P, Zhou J, Zhen M, Cui W, Xu G, Yang D, Liu Z (2012) Abdominal hernia repair with a decellularized dermal scaffold seeded with autologous bone marrow-derived mesenchymal stem cells. Artif Organs 36(3):247–255
Zhu W-d, Xu Y-m, Feng C, Fu Q, Song L-j, Cui L (2010) Bladder reconstruction with adipose-derived stem cell-seeded bladder acellular matrix grafts improve morphology composition. World J Urol 28(4):493–498
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Lee, J.S., Choi, Y.S., Cho, SW. (2018). Decellularized Tissue Matrix for Stem Cell and Tissue Engineering. In: Noh, I. (eds) Biomimetic Medical Materials. Advances in Experimental Medicine and Biology, vol 1064. Springer, Singapore. https://doi.org/10.1007/978-981-13-0445-3_10
Download citation
DOI: https://doi.org/10.1007/978-981-13-0445-3_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-0444-6
Online ISBN: 978-981-13-0445-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)