Abstract
The objective of this study was to investigate the limitations of a heterologous bladder acellular matrix graft (BAMG) and the influence of the collagen ratio on functional regeneration in a large animal model. Ten female dogs underwent partial cystectomy; eight received BAMG (two homologous; six heterologous) and two partial cystectomy only. A cystometry was performed prior to surgery and 7 months postoperatively when all animals underwent sacral root stimulation. Tissue specimens were studied by histologic and immunohistochemical techniques and for collagen types. At month 7, all animals survived and bladder capacity in the grafted animals was increased. All grafts demonstrated all components of a normal bladder wall. Nerves were seen with the density decreasing with distance from the anastomosis. The BAMG processing and follow-up demonstrated no changes in the homologous tissue, whereas in the heterologous tissue, the amount of collagen changed with the processing during implantation. None of these heterologous specimens demonstrated a similar collagen ratio to the hosts’. The homologous BAMG undergoes more complete regeneration. In the heterologous BAMG, collagen seems not to be replaced. The amounts and ratio of collagen types I and III seem to influence smooth muscle regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gleeson and Griffith [6] have defined the ideal material for bladder augmentation that would effect tissue regeneration without adverse side effects: it should be biocompatible and mechanically reliable; should deter or tolerate intraluminal infection; and should be easy to surgically implant. Functionally, it should preserve renal activity, provide adequate urinary storage at low pressure, and allow volitional, complete evacuation of urine per urethram. During the recent years, the publications about BAMG supported that acellular matrix fulfills all these requested criteria [12, 10, 18].
Our laboratory has previously reported studies in the rodent with organ-specific bladder acellular matrix grafts (BAMGs) that were both homologous and heterologous [18]. However, in the dog, only a homologous graft has so far been reported [13]. To address the problem of a shortage of homologous tissue available for human transplant, we undertook the present study to evaluate the effectiveness of heterologous bladder augmentation in a large animal model to prove if regenerated BAMGs of different species demonstrate equivalent histological findings with a similar function.
Materials and methods
Graft production
Bladders obtained from our institution’s tissue-sharing program (three monkeys, three humans, one dog) were processed as previously described [3]. The excised tissue was placed in 10 mM phosphate-buffered saline (PBS, pH 7.0) and 1% sodium azide for partial cell lysis, which was completed in 1 M sodium chloride containing 2,000 KU DNase (Sigma; St. Louis, MO). The specimens were stirred in 50 ml of 4% sodium desoxycholate containing 0.1% sodium azide for 24 to 72 h to solubilize the lipid membranes; this step was repeated once. The resultant acellular matrix was washed three times in PBS and stored in 10% neomycin sulfate at 4°C until grafted. Acellularity was confirmed by microscopy after staining with hematoxylin and eosin as well as trichrome.
The circumference of all harvested bladder domes, cut open, was measured. To establish a standard and to avoid traction, the tissues were first measured, then flattened on a glass disk and measured after compression with a second glass disk of 5 kg.
Animals
In accordance with the protocol approved by our Institution’s Committee on Animal Research, ten healthy female mongrel dogs (age 1 year; weight 20.4–29.6 kg) were divided into four groups: homologous BAMG (n=2), monkey BAMG (n=3); human BAMG (n=3) and partial cystectomy (n=2), which served as controls.
Surgical procedure
Anesthesia and analgesia
The dogs were sedated with acepromazine (0.05 mg/kg, i.m.), and anesthesia was maintained after endotracheal intubation with isofluorane (1–2%). The animals breathed spontaneously and were monitored continuously. Postoperative analgesia was buprenorphine s.c. (0.01–0.02 mg/kg) every 4–6 h for 2 days.
Technique
Bladder capacity was evaluated by transurethral cystometry, repeated for verification, and cystoscopy was performed to verify a normal bladder appearance. The bladder was emptied with an 8-French single-use catheter (C.R. Bard Inc., Covington GA) sutured to the vulva, and the bladder was then exposed through a lower abdominal midline incision. In all animals, more than 50% of the bladder wall was resected and either closed in layers by running sutures (in the two controls) or replaced with a BAMG of equal size (Table 2). Four monofilament nonresorbable sutures (Dermalon® 3–0) were placed to fix the BAMG in position and to identify the matrix borders (anterior, posterior, left and right) at sacrifice 7 months later. The gaps between the sutures were closed by inner 5–0 polyglactin sutures (Vicryl®, Ethicon Inc.; Somerville, NJ) and outer 2–0 polyglactin running sutures. The bladder was filled with 200 ml saline solution to ensure watertightness and facilitate measurement of the BAMG. To promote healing, the abdominal wound was closed in layers with a running 3–0 polyglactin suture, and the skin with an inverted running 3–0 polyglactin suture (Vicryl-Rapid®, Ethicon).
The transurethrally placed and sutured 8-French catheter, used for cystography, was shortened for postoperative urinary drainage. The dogs received enrofloxacin (Baytril®, Bayer Corp.; Shawnee, KA), 2.5 mg/kg body weight i.v. intraoperatively and twice a day orally until catheter removal at day 7. After this time the animals voided normal transurethrally.
Functional evaluation
At the day of sacrifice, anesthesia was performed as described above. The bladder capacity was evaluated by transurethral cystometry, repeated for verification, followed by cystography. The dog was then placed in the prone position, and a dorsal laminectomy (L6–S1) exposed the spine and the sacral roots for extradural stimulation. The roots were gently lifted and placed on bipolar hook electrodes. The correct placement of the transurethral microtip catheter (MILLAR®), used to record bladder and sphincteric pressure, was verified during rectangular pulse stimulation of S1–S3. The pressure changes were analyzed simultaneously on a customized personal computer (LabView®4.0; Macintosh Quadra 800). The sphincter was fatigued by prestimulation of the S2 with a 100-Hz biphasic sinusoidal signal, and an additional 20-Hz pulse to the S3 initiated micturition [15]. This was done unilaterally and bilaterally and repeated twice with a 10-min interval.
After neurostimulation, the bladder was exposed through a lower abdominal midline incision. Atraumatic needles were placed through the bladder wall at the site of the identification sutures to mark the border of the BAMG. Cystoscopy was performed transurethrally to view BAMG regeneration in vivo. The distance between opposing marking sutures was measured with the aid of bladder filling (see above). The bladder was then excised (its shape maintained with a balloon catheter filled with 30 ml saline) and processed for microscopy. Finally, the animal was sacrificed by pentobarbital (200 mg/kg body weight) followed by Euthasol® (390 mg/kg).
Histologic evaluation
The specimens for light microscopic examination were maintained in the distended state described above for at least 24 h. They were then longitudinally dissected, with inclusion of two of the four identification sutures (diagonally opposed to ensure that the entire diameter was included), and immersed overnight in 10% buffered formalin. After dehydration in graded ethanol solutions and clearing in Histoclear, the longitudinally sectioned bladder was embedded in paraffin (the two opposing marking sutures of the grafted area enabled precise orientation). Sections (5 μm) were cut, air-dried onto precoated slides, and stained with trichrome for collagen and smooth muscle; hematoxylin and eosin (H and E) for nuclei; α-actin for smooth muscle; and for nerves as detailed below. In addition, slides were stained with picrosirius red for collagen I and III.
Staining procedures
Paraffin sections were hydrated to water, followed by blocking endogenous peroxidase (20 min with 0.3% H2O2 in methanol) and nonspecific protein binding (overnight with 3% normal horse serum in PBS, pH 7.4, containing 0.3% Triton X-100). After rinsing, sections were treated with 3% goat serum in PBS/0.3% Triton X-100 for at least 60 min to eliminate nonspecific protein binding. For nerve staining, the slides were incubated with specific antibodies (anti-protein gene product [PGP] 9.5, 1:8,000 [Accurate Chemical & Scientific Corporation, Westbury, NY]; anti-calcitonin gene-related peptide [CGRP], 1:1,800; anti-Substance P, 1:8,000; anti-neuropeptide Y [NPY], 1:6,000; and anti-tyrosine hydroxylase [TH], 1:20 [Novo Castra, Newcastle Upon Tyne, UK]). All sections were incubated at room temperature overnight, except for CGRP, for which sections were incubated for 60 min. After washing with buffer, sections were immunostained according to the avidin–biotin–peroxidase method (Vectastain Elite Kit, Vector Laboratories, Burlingame, CA) with 3,3′-diaminobenzidine with hydrogen peroxide as the chromogen.
The sections for the smooth muscle stain were incubated for 60 min at room temperature with mouse monoclonal anti-smooth-muscle α-actin (1:6,000, Sigma Chemicals; St. Louis, MO).
As a negative control, some sections were immunostained without exposure to primary antibody [17]. All sections were counterstained with hematoxylin, dehydrated to xylene, and mounted.
For collagen staining, sections were deparaffinized, hydrated, and left for 60 min in a 0.1% solution of sirius red dissolved in aqueous saturated picric acid. Sections were rapidly washed in running water and dehydrated to xylene. Results were analyzed according to the method of Kiraly et al. [7].
Randomly chosen fields of each picrosirius red-stained specimen (donor bladder wall, BAMG, regenerated matrix [area of the anastomosis, center of the BAMG [dome], and area between]) were analyzed at 400× magnification with polarizing filters (Leika light microscope DM RB attached to a digital camera [Nikon N 90]). The collagen types I:III ratio was quantified with the aid of Adobe PhotoShop™ 4.0 (Adobe Systems Inc.; Mountain View, CA) installed on a Power Macintosh G3 (Apple Computer, Inc. Cupertino, CA). The polarized microscopic pictures were analyzed with custom filters and the mean of the analyzed areas was used to compare the group differences. The different tissue areas of the regenerated matrix (anastomosis, dome, and the area between) were compared with donor bladder and the bladder wall of the host by paired Student’s t test (GB-STAT, Dynamic Microsystems Inc.; Silver Spring, MD). The data are presented as mean (± SD). Values were considered significant at P<0.05.
Results
None of the animals died during the study. The urine probes were stopped when urinalysis results returned to normal, at which time the transurethral catheter was removed.
Unilateral neurostimulation was effective in seven of ten animals (the two controls, the two dogs with the homologous BAMG, two with a monkey BAMG, and one with a human BAMG), resulting in complete micturition without residual volume. Bilateral stimulation provoked micturition in two of those remaining (one with a monkey and one with a human BAMG), but with a mean residual volume of 110 ml (Table 1). The last animal (with a human BAMG) did not respond to sacral stimulation at all, although we saw no sign of retention or change in the upper urinary tract.
Cystometry at sacrifice at 7 months revealed greater bladder capacity (282 ml) than preoperatively (247 ml) and notably greater than in controls (163 ml) (Table 1). Leak-point pressure was unchanged from preoperative values.
Postoperative cystography demonstrated that the augmented matrix, regardless of species, gave the bladder the shape of a mushroom. After 7 months, the bladder recovered its normal shape in all animals (Fig. 1).
While preparing the bladder through the abdominal approach, no significant scarring of the augmented bladder was noticeable. None of the augmented animals had gross evidence of increased scarring. Only in the dome was less vascularization apparent. This area was slightly bigger in those augmented with a human BAMG. In the controls the inner bladder surface was completely normal. The upper urinary tract was normal in all animals, with no evidence of hydronephrosis.
The three types of BAMG, when measured at processing, revealed growth of at least 50% in the dog and over 90% in the human (Table 2). (The circumference in the monkey BAMG increased approximately 70%.) The implanted BAMG was round, with a diameter of 6.0–6.3 cm, with the exception of the monkey BAMG (4.5 cm) because the harvested bladder is smaller. After 7 months the BAMGs of the dog, monkey, and human were still 13, 23, and 41%, respectively, larger than the harvested specimen (Table 2).
Histologic examination of the homologous BAMG demonstrated regeneration up to the dome similar to that in the host (Fig. 2). The surface was covered with a multilayer urothelium containing small vessels at the basal membrane. In the bladder wall itself, vessels of different diameters were seen. The muscle bundle arrangement, size, and appearance resembled that of the host bladder. PGP 9.5-immunoreactive nerves were in close proximity. Staining also revealed positive immunoreactivity for NPY, CGRP, SP and TH, but appeared less numerous toward the center of the graft.
Findings were similar in the heterologous BAMGs, among which the monkey regenerated better than the human. The urothelial lining was normal in all animals, independent of the BAMG used. The main difference between heterologous and homologous BAMGs was the smaller amount of smooth muscle and, accordingly, the quality and quantity of immunoreaction to the different nerve stains (Fig. 3 and Table 3).
Longitudinal section through a bladder augmented with a heterologous BAMG (human) 7 months postoperatively (no magnification). Dome (□) of the regenerated tissue (magnification: ×20): a normal-appearing urothelium (hematoxylin and eosin) (magnification: ×40); b smooth muscle cells and vessels (α-actin) (magnification: ×40); and c nerves in the neighborhood of vessels and smooth muscle cell bundles (PGP 9.5) (magnification: ×60)
On light microscopy with polarizing lenses of the specimens stained with picrosirius red, collagen type I appeared as thick, strongly birefringent, yellow or red fibers and collagen type III as thin, weakly birefingent, greenish fibers that could be identified as reticulin fibers, indicating a collagen shift after processing of the donor tissue (although the human donor bladder appeared to be stable).
Seven months after augmentation, the ratio of collagen I:III of the dog and monkey BAMG appeared to become similar to the host collagen ratio (see donor dog, Table 4). The dog BAMG revealed a shift towards collagen type III in comparison with the donor bladder wall, whereas collagen type I increased in the monkey BAMG (Table 4).
Visual comparison of the three types of BAMG demonstrated the obvious percentage difference of collagen I to III in each of the categories (Fig. 4). The ratio of collagen I to III demonstrates the collagen composition of the different BAMGs (Table 4, second column). However, an examination of the numbers of pixels at the same resolution permits a more detailed analysis (Table 4). The human bladder wall has the lowest while the monkey has the highest density of collagen fibers. After processing, the number of fibers in the human and monkey BAMG is almost equivalent, whereas the dog BAMG has only half the number of fibers per field. These fiber densities are not changed after 7 months. The dog matrix became similar to the host throughout the augmented tissue, which is also reflected in the histologic regeneration. In the regenerated human BAMG, the collagen fibers increased and fewer nerve fibers were seen (Table 3).
The three BAMGs (top line prior to implantation, bottom line after 7 months of regeneration) stained with picrosirius red viewed through a polarizing microscope (magnification ×40) and analyzed by a customized filter. For the dog BAMG both types of collagens are seen whereas in the human BAMG the collagen III makes the biggest portion. Seven months postoperatively both heterologous matrices became similar to the host, but the human tissue still differs more than the monkey graft. The collagen fibers of the human BAMG are compact compared to the other two
The processing of the donor tissue seems to alter the amount of collagen and even the ratio. After 7 months the collagen ratio of the heterologous grafts in the anastomosis did not become equal to that in the host, but, interestingly, reflected the regeneration of the muscle and nerve structure. After 7 months, the changes seen after processing in the homologous graft returned to “normal” with slight differences throughout the regenerated BAMG. Similar results were found in the regenerated monkey BAMG, with the major difference being that the amount of collagen was still almost double that of the host, but almost equal to the donor monkey tissue (see Table 4).
Discussion
In the present study, prompted by the ongoing problem of limited homologous tissue reserves, we investigated the feasibility of a heterologous BAMG in the large animal model.
The harvested bladder tissue was measured before and after processing. In addition we measured the size of the augment before implantation and at the time of harvesting the bladder at 7 months. As previously found in the urethral acellular matrix, [14] the size increased with processing. In the present study, we noted that the size increase was greater and we attribute this to the higher density of contractile tissue lost. Over 50% of the bladder dome was resected and replaced with a homologous or heterologous BAMG. The animals that underwent only partial cystectomy still had, as one might expect, a smaller bladder capacity at month 7. In contrast, those animals that received the BAMG had a higher bladder capacity at sacrifice than preoperatively.
The organ-specific acellular matrix is a scaffold of collagen and elastin. The observation that the change in the collagen I:III ratio during matrix processing is species-dependent has been evaluated before in the urethra [14]. In contrast to the report of Kiraly et al. [7] in normal tissue, it became obvious that, with processing, the collagen I fibers became difficult to verify. In the homologous BAMG, the amount of collagen III was slightly different from that in the donor tissue. We assumed before, and have been able to demonstrate here, that the collagen fibers were not replaced or restructured by the host, as Atala et al. [3] reported by using a preformed polyglactin structure.
With the regeneration of contractile tissue, the BAMG will become smaller—a consideration in planning the size for harvest. The removal of the transurethral catheter at postoperative day 7 may have avoided early shrinkage. Cystography demonstrated that the bladder, after augmentation, assumed the shape of a mushroom, but had resumed its normal configuration at 7 months, as compared with a prefabricated seromucular enterocystoplasty demonstrated by Aktug et al. [1]. This functional recovery was also recently investigated in a neurostimulation setting to confirm the contractility of the bladder under stimulation [15]. The fact that unilateral stimulation did not provoke voiding in all augmented animals may be due to a neuronal cause or could be the result of incomplete bladder wall regeneration. Although we did not obtain X-ray images during stimulation, it seems likely that the ipsilateral bladder wall contracted and the contralateral side gave way, preventing the pressure increase necessary to voiding, as suggested by Martinez et al. [8], who demonstrated that the bladder wall is innervated from each side. It is seen once in a while that unilateral neuromodulation is ineffective in the one or the other animal although without any evidence of a nerve lesion.
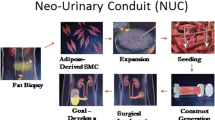
Colonization of the mesh by host cells entails the following steps: urothelium migration; fibroblast invasion with neovascularization (granulation tissue); and fibroblast transformation into smooth muscle cells and reorganization of the vascular structure. In a homologous rodent BAMG, functional neural regeneration has been reported [11], and homologous augmentation has proved feasible in a larger animal [13].
Although to our knowledge the used acellular matrix carries no genetic information, the scaffold itself appears to influence the regeneration process. Piechota et al. [11] analyzed several species and found scaffold differences on transmission electron microscopy. In the present study with polarization microscopy, picrosirius red revealed different amounts of collagen types I and III among the different BAMGs. Baskin et al. [4] have shown that normal urethral spongiosum and urethral stricture scar tissue were principally collagen types I and type III, respectively. They postulated that normal fibroblasts synthesize both, but that, with a change in the surrounding environment, collagen synthesis becomes imbalanced, resulting in stricture in the urethra. This is demonstrated by increased m-RNA levels for collagen type I in scar tissue. We used picrosirius red polarization to reveal collagen ratio changes [9], used before successfully in other organs.
The observation that the process of matrix production appears to cause a change in the collagen types I:III ratio that may be species-dependent (a greater alteration in the dog) to our knowledge has not been evaluated before. However, it remains unclear how and why the ratio in the implanted scaffold changed only partially postoperatively and seemed to be more or less the same after 7 months, although the decreased ratio became significant, even in the homologous graft, in comparison with donor tissue. Because scar development has been explained as a result of increased collagen type I and decreased collagen type III production by fibroblasts [4], a decrease in the collagen type I:III ratio might explain the lack of stricture development in our specimens. It is still unclear how the surrounding environment regulated the amount of each collagen type synthesized by fibroblasts, as the implanted graft did not demonstrate any signs of inflammatory reaction.
The high amount of collagen III in the human tissue probably relates to the thickness of the tissue, which collapsed after contractile tissue lysis and did not recover in the area of the anastomosis after 7 months.
The best regeneration was seen in the homologous grafted tissue after the time period of 7 months, implying that the scaffold must hold some information for regeneration. Although the implanted heterologous matrix did not show evidence of macroscopic signs of rejection, it did not support or promote tissue regeneration compared to the homologous regenerated BAMG within the same follow-up time. To our knowledge, it has not been demonstrated before that tissue regeneration is dependent on the original collagen structure used. These findings support our suggestion that donor tissue should be chosen from a location equivalent to its intended placement. In addition to being organ-specific, the matrix selected should be homologous, if available. Upon histologic examination, all components of the homologous BAMG regenerated up to the dome; regeneration in the heterologous BAMG was in an earlier stage—neither as rapid nor as complete. However, although smooth muscle cell growth into the heterologous graft was less than in the homologous BAMG, internal epithelialization and angiogenesis were complete. In contrast to the study of Badylak et al. who used small intestinal submucosa in the dog model for a large-diameter vascular graft [11], we were not able to confirm the replacement of the matrix by the host. In order to make a final decision regarding the importance of the origin of the acellular matrix that influences regeneration, it will be necessary to compare homologous BAMG with homologous SIS. This will need to be addressed in a different approach.
Immunostaining revealed nerve fibers along with the regenerated smooth muscle cells and small vessels. Positive immunoreactivity to PGP 9.5 was subclassified into several specific immunostains. Neuropeptide Y is found in cholinergic postganglionic neurons [4], while CGRP and substance P are distributed in visceral afferent fibers [9]. These peptides are reported to be involved in the modulation of efferent and afferent neurotransmission [2]. Even TH, as a neuropeptide of autonomic sympathetic nerve fibers, [5] was demonstrated in the regenerated bladder tissue, although it is usually seen more frequently in the bladder neck and the urethra [16]. The number of nerve fibers decreased with the distance from the anastomosis toward the center of the regenerated BAMG.
Further work, with an increased sample size, is needed to determine if there are additional factors influencing regeneration and functional outcome.
Conclusion
This study demonstrates that augmentation with the acellular bladder matrix is possible, although the outcome seems to be dependent on the BAMG’s origin although the sample size is small. Heterologous BAMG can be used, but the histologic outcome, at least after 7 months, is not as good as when homologous bladder tissue is used. These histologic results are supported by the immunohistologic findings. Although the functional outcome for all three types of BAMG was satisfactory, homologous bladder wall donor tissue is clearly preferable.
References
Aktug T, Ozdemir T, Agartan C, Ozer E, Olguner M, Akgur FM (2001) Experimentally prefabricated bladder. J Urol 165:2055–2058
Andersson KE, Persson K (1994) Nitric oxide synthase and nitric oxide-mediated effects in lower urinary tract smooth muscles. World J Urol 12:274–280
Atala A, Freeman MR, Vacanti JP, Shepard J, Retik AB (1993) Implantation in vivo and retrieval of artificial structures consisting of rabbit and human urothelium and human bladder muscle. J Urol 150:608–612
Baskin LS, Constantinescu SC, Howard PS, McAninch JW, Ewalt DH, Duckett JW, Snyder HM, Macarak EJ (1993) Biochemical characterization and quantitation of the collagenous components of urethral stricture tissue. J Urol 150:642–647
Bickel A, Grehl H, Butz M, Schmelz M, Engelhardt A, Neundorfer B, Neuhuber WL, Handwerker HO (1999) Neuropeptide content of peripheral nerve in relation to nerve function in neuropathy. Clin Neuropathol 18:181–189
Gleeson MJ, Griffith D (1992) The use of alloplastic biomaterials in bladder substitution. J Urol 148:1377–1382
Kiraly K, Hyttinen MM, Lapvetelainen T, Elo M, Kiviranta I, Dobai J, Modis L, Helminen HJ, Arokoski JP (1997) Specimen preparation and quantification of collagen birefringence in unstained sections of articular cartilage using image analysis and polarizing light microscopy. Histochem J 29:317–327
Martinez Portillo FJ, Seif C, Braun PM, Bohler G, Osmonov DK, Leissner J, Hohenfellner R, Alken P, Juenemann KP (2003) Risk of detrusor denervation in antireflux surgery demonstrated in a neurophysiological animal model. J Urol 170:570–573; discussion 573–574
Montes GS, Junqueira LCU (1988) Histochemical localization of collagen of proteoglycans in tissues. In: Nimni ME (ed) Collagen, vol II, Chapter 3. CRC Press, Inc., Boca Raton, pp 41–72
Piechota HJ, Dahms SE, Nunes LS, Dahiya R, Lue TF, Tanagho EA (1998) In vitro functional properties of the rat bladder regenerated by the bladder acellular matrix graft. J Urol 159:1717–1724
Piechota HJ, Dahms SE, Probst M, Gleason CA, Nunes LS, Dahiya R, Lue TF, Tanagho EA (1998) Functional rat bladder regeneration through xenotransplantation of the bladder acellular matrix graft. Br J Urol 81:548–559
Probst M, Dahiya R, Carrier S, Tanagho EA (1997) Reproduction of functional smooth muscle tissue and partial bladder replacement. Br J Urol 79:505–515
Probst M, Piechota HJ, Dahiya R, Tanagho EA (2000) Homologous bladder augmentation in dog with the bladder acellular matrix graft. BJU Int 85:362–371
Sievert KD, Wefer J, Bakircioglu ME, Nunes L, Dahiya R, Tanagho EA (2001) Heterologous acellular matrix graft for reconstruction of the rabbit urethra: histological and functional evaluation. J Urol 165:2096–2102
Sievert KD, Gleason CA, Junemann KP, Alken P, Tanagho EA (2002) Physiologic bladder evacuation with selective sacral root stimulation: sinusoidal signal and organ-specific frequency. Neurourol Urodyn 21:80–91
Sievert KD, Bakircioglu ME, Tsai T, Nunes L, Lue TF (2004) The effect of labor and/or ovariectomy on rodent continence mechanism-The neuronal changes. World J Urol 22:244–250
Skalli O, Ropraz P, Trezciak A, Benzonana G, Gillessen D, Gabbiani D (1986) A monoclonal antibody against a smooth muscle actin. A new probe for smooth muscle differentiation. J Cell Biol 103:2787
Wefer J, Sievert KD, Schlote N, Wefer AE, Nunes L, Dahiya R, Gleason CA, Tanagho EA (2001) Time dependent smooth muscle regeneration and maturation in a bladder acellular matrix graft: histological studies and in vivo functional evaluation. J Urol 165:1755–1759
Acknowledgement
Supported in part by the Deutsche Forschungsgemeinschaft (Grant Si 679/1-1) and the United States Department of Health and Human Services (NIH grant RO1 NS 18029). The work was honored by the Forum Urodynamicum (2002) with the Eugin-Rehfisch Prize.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sievert, KD., Fandel, T., Wefer, J. et al. Collagen I:III ratio in canine heterologous bladder acellular matrix grafts. World J Urol 24, 101–109 (2006). https://doi.org/10.1007/s00345-006-0052-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-006-0052-8