Abstract
Pancreatic cancer continues to be a life-threatening disease with poor long term outcomes despite various treatments. Progress has been slow, although results of surgery have improved, and mortality rates have fallen. Surgery is still the modality with the highest potential to cure pancreatic cancer. We examine some of the key issues relating to the treatment of pancreatic cancer, largely to the description of issues related to pancreatic head cancer.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Pancreatic Cancer
- Hepatic Artery
- National Comprehensive Cancer Network
- Uncinate Process
- Multivisceral Resection
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Pancreatic cancer continues to be a life-threatening disease with poor long term outcomes despite various treatments. Progress has been slow, although results of surgery have improved, and mortality rates have fallen. Surgery is still the modality with the highest potential to cure pancreatic cancer. We examine some of the key issues relating to the treatment of pancreatic cancer, largely to the description of issues related to pancreatic head cancer.
6.1 Controversies: the Top Seven Questions
-
1.
What is the natural history of pancreatic cancer?
-
2.
Is an R0 resection the key to improved survival?
-
3.
How can the margins of resection be examined precisely?
-
4.
Do vascular resections help?
-
5.
Are multivisceral resections justifiable?
-
6.
What should be the extent of lymphadenectomy?
-
7.
Have laparoscopic and robotic technologies made a difference?
6.1.1 What Is the Natural History of Pancreatic Cancer and the System of Spread of the Disease?
In 2016 there were 53,070 new cases of pancreatic cancer in the USA alone with 41,780 deaths [1]. Thus, pancreatic cancer has a poor overall prognosis. This may be due to the fact that even localized cancer may be systemic from its onset. The evidences in favour of a systemic disease are: (i) among 285 patients with margin-positive resection, 76 % had distant disease; [2] (ii) 70–85 % of patients who have undergone resection die of metastatic disease; [3] (iii) adjuvant radiation has no significant benefit in prolonging survival (indirect evidence); [4, 5] (iv) there is no advantage of chemoradiation over chemotherapy; [6, 7] (v) 15–32 % of patients on neoadjuvant therapy progress to systemic disease while on treatment; [8, 9] and not least, (vi) among specimens of extended lymphadenectomy, it has been shown that pancreatic cancer spreads by complex pathways to more distant lymph nodes [10].
While surgery continues to be the treatment of choice for localized pancreatic cancer, there is increasing evidence that a multimodality approach based on systemic therapy may be necessary to produce improvements in survival.
6.1.2 Is R0 Resection the Key to Improved Survival?
It is logical to presume that resection with negative margins (R0) can provide better local/locoregional control of the disease. Long term survivors invariably have R0 resections performed [11].
There is some controversy whether an R1 resection (microscopic involvement of the margin) for pancreatic cancer is justifiable. Despite excellent preoperative imaging, abutment of the tumour to the superior mesenteric artery is not always clearly defined, and surgeons may well discover it late in the course of the dissection that tumour free margins are difficult to achieve. While R0 resections lead to improved survival, it may also be true that the biology of the cancer may play a part. Hence, R1 resections must not be condemned as a surgical misadventure. An R2 resection (macroscopic residual disease) may also occur rarely, but every attempt should be made to avoid this eventuality.
The situation is rendered more complex by the fact that determination of R0 status is by no means standardized. The transection margins comprise (i) stomach or duodenum, (ii) pancreatic neck, and (iii) the bile duct and establishment of a negative margin is easy to achieve. However, circumferential margins are more unclear. This will be addressed in detail in the section on reporting of pathology.
There have been wide variations in R0 rates published from 20 to 80 %. Further, R0 resections did not confer any survival benefit and it was attributed to the poor biology of the disease—despite R1 resection rates of 17 %, survival in the R0 and R1 groups were similar (66 % and 68 %) [12]. Better histopathology approaches have created a realistic R1 rate, which may occur in up to 82 % of pancreatic head cancers, and 72 % of bile duct cancers, but are less likely in ampullary cancers (25 %). Multifocal residual disease may occur. Overall, survival was better in R0 resections as determined by the new standardized pathology protocols [13].
The technical aspects of achieving an R0 resection are complex and hitherto undefined completely. Radicality has two components: (i) margins of the resection on the pancreaticoduodenectomy (PD) specimen, and (ii) margins on the lymphadenectomy. The issue is further complicated by the fact that there is no buffer of areolar or fatty tissue around the uncinate process of the pancreas which provides an opportunity for complete resection. The uncinate process of the pancreas may be densely applied to the proximal course of the superior mesenteric artery (SMA) and a tumour free margin may not be available despite peri-adventitial dissection of the uncinate process off the artery. The mesopancreas is defined as the soft connective tissue between the SMA and the region from the pancreatic head to the uncinate process, including the inferior pancreaticoduodenal artery (IPDA) as well as the lymphatic, nervous and vascular structures on the fusion fascia of the ligament of Treitz [14–16]. Clearance of the mesopancreas involves all tissue to the right of the SMA and can decrease the number of R1 resections with R0 resection rates of 93 % as compared to standard resection with 60 % R0 resection [17]. Dissections of the pancreatic head have failed to reveal a clear fascial envelope akin to the mesorectum [18, 19], but clearance of the area may be beneficial to the locoregional control of pancreatic cancer, although more data and larger studies are required [20]. Recent reports have described many approaches to clear this area. [21, 22] There may be one further anatomical fact which is not apparent from the published data. The mesentery of the uncinate process is continuous with the mesentery of the proximal jejunum, and even when the SMA is cleared, there may still exist a portion of the proximal jejunal mesentery which may harbour disease and fail to be cleared at surgery. Thus the artery may not represent the ‘last frontier’ in dissection of pancreatic cancer. However, there is recent data which suggests that the ‘mesopancreatic stromal clearance’ can be assessed by preoperative imaging [23], and patients in whom this clearance may not be possible could become candidates for preoperative chemo/chemoradiotherapy [23].
Perhaps the best evidence in favour of R0 resection is the description of improved survival figures with re-resection after a positive margin on frozen section, and the conversion from R1 to R0 status. Patients with R0 confirmed by frozen section, R0 after re-resection confirmed by frozen section, and R1 after re-resection despite frozen section had median survival figures of 29, 36 and 13 months [24]. Survival is also determined by the tumour biology (lymph node metastases) and treatment parameters such as major perioperative complications and blood loss [12], or tumour grade, performance status and tumour size as described by the guidelines published by the International Association of Pancreatology/European Pancreatic Club [25–27].
There is a lack of clarity as to terminology used to describe the circumferential margin. Up to 28 different names have been used and this has prevented uniformity of reporting and comparison of surgical approaches [28].
A final contentious issue is the margin (in millimetres) that is considered as adequate for R0 resection. While the American Joint Cancer Committee (AJCC) guidelines describe uninvolved margins as R0, the Royal College of Pathology have described a 1 mm margin [29]. Patients with margins greater than 1 mm had survival figures twice as those with less than 1 mm. French data also recommended a 1 mm margin [30], but Chang et al. prescribed a 1.5 mm margin [31]. This emphasizes the need for accurate histopathological examination. A recent meta-analysis has also confirmed the need for a 1 mm margin [32].
There is no doubt that every surgeon embarking upon a PD must achieve the best possible local clearance of the tumour. While R0 rates are a measure of the quality of the surgery, and the experience of the surgeon (surgeons who have performed more than 60 resections have a lower R1 rate) [33], R1 resection may not be a marker of low quality surgery, but high quality pathological examination! [34].
6.1.3 How Can the Resected Margins Be Examined Precisely?
In 2006, Verbecke [35] and associates described a standard protocol for pathological examination of the PD specimen. This included a defined distance taken for microscopic involvement (currently 1 mm), colour inking of the margins (anterior, posterior, and superior mesenteric margins), axial slicing of the specimen and reporting of all the margins. There was a close correlation between R0 on the Leeds pathology protocol (LEPP) and survival. Some reports describe a posterior margin (retroperitoneal) and a distinct SMA margin (medial part of the uncinate process and further medial from the groove of the superior mesenteric vein [SMV]) [35–37]. In effect, the SMA margin and the retroperitoneal margins are the final frontier unless the SMV is involved.
A standardized approach to pathology reporting is advisable despite recent reports that survival may not depend entirely on the R0 status derived from such examination [38].
6.1.4 Do Vascular Resections Help?
In 1992, Fuhrman reported that en bloc resection of the SMV with the pancreatic head cancer is justifiable––a case of anatomical involvement rather than biological aggressiveness of the tumour [39]. Venous involvement may be classified (Ishikawa) [40] as type 1: normal; type 2: smooth shift; type 3: unilateral narrowing; type 4: bilateral narrowing; and type 5: bilateral narrowing with collateral veins. Histological involvement of the vein ranged from 0 % with types 1 and 2, 51 % in type 3, 74 % in type 4 and 93 % in type 5 [41]. Some critical aspects of venous resection in pancreatic cancer are: (i) sleeve resections may be required when the lateral aspect of the SMV alone is involved; however, there may be difficulty in repair of the vein due to kinking. A vein patch may be necessary; (ii) end-to-end anastomosis of up to 5 cm of the vein can be achieved without difficulty with mobilization of the two ends and an adequate Cattell–Brasch technique; if the splenic vein is to be ligated, it can be done with impunity; reconstruction is only required if the inferior mesenteric vein (IMV) has been interrupted [42]. If the IMV is not patent, left-sided portal hypertension may result; (iii) if the reconstruction cannot be achieved by end-to-end anastomosis, then the following can be used for the repair: (a) left renal vein; [43] (b) internal jugular vein; (c) external iliac vein; (d) cryopreserved grafts; (e) polytetrafluoroethylene (PTFE); or (f) Dokmak peritoneal patch; [44, 45] (iv) in general, an autogenous vein is preferred, although a prosthetic graft can be used—postoperative aspirin may be necessary [46]. In general survival outcomes are better when the portal venous resection is considered preoperatively and planned rather than when it is decided on the table [47]. The key principle is not to separate the portal vein–SMV junction from the tumour bearing head of pancreas when preliminary dissection suggests abutment. In such cases, a full mobilization of the uncinate process is also completed leaving the tumour bearing head attached to a segment of the vein which is then resected en bloc; the best results have been described among patients who had a portal vein resection and had uninvolved margins [48]. This has been validated in a meta-analysis as well [49].
Turrini and colleagues suggested that the portal vein should be routinely resected during pancreaticoduodenectomy even if the vein was not involved by tumour. Their retrospective analysis suggested that patients with PD with portal vein resection who did not have invasion of the vein wall had superior survival to those who had a standard PD without venous resection [39, 50]. This represents a partial throwback to the regional pancreatectomy of Fortner where the portal vein was resected along with the hepatic artery/SMA and the mesocolon [51]. The Turrini approach needs to be validated by prospective studies before finding application in practice.
Arterial resections on the other hand are to be considered only in select situations. In general, survival is poor [52]. Occasionally reconstruction of the hepatic artery involved by an adenocarcinoma of the neck of the pancreas may be considered where a small area of involvement is the only impediment to the accomplishment of an R0 resection. Also, reconstruction of a replaced right hepatic or common hepatic (arising from the SMA) can be considered. If the origin from the SMA is uninvolved and a stump is available, end-to-end anastomosis or an autologous interposition graft with gastroepiploic artery, gastroduodenal artery, right gastric artery, middle colic artery, splenic artery, radial artery, great saphenous vein or cadaver iliac artery; occasionally the origin from the SMA is involved and in such cases, a long PTFE jump graft may be used from the aorta or the right iliac artery [53].
6.1.5 Are Multivisceral Resections Justifiable?
Locally advanced pancreatic cancer may involve adjacent organs. In view of the poor outcomes in pancreatic cancer, there is a widely held view that multivisceral resections may not provide any benefit. However, data has emerged that suggest that additional organ resection is justified if the surgeon and centre are experienced in the procedure, and if an R0 resection can be accomplished at the end of the resection. The most common organs resected are the right colon, right kidney and a segment of the liver. Mortality rates were high initially [54], but are now comparable to a standard PD and superior to a palliative bypass [55, 56]. An additional nephrectomy may have the maximum negative outcome. Complication rates are higher, and R0 resection rates are no higher than with standard PD. The International Study Group for Pancreatic Surgery recommended that multivisceral (extended) pancreatectomy may be performed in selected cases [57].
6.1.6 What Should Be the Extent of Lymphadenectomy?
The extent of lymphadenectomy is a subject of much controversy. Published trials have failed to establish an advantage with extended lymphadenectomy. The value of these publications has been diminished further by the lack of uniformity in terms of nomenclature, definitions, classification of lymph node stations or the extent of the lymph node clearance. Four randomized trials [58–61], two consensus meetings [62, 63], and two meta-analyses [64] have failed to establish any benefit with extended lymphadenectomy. The optimum number of lymph nodes to be removed during a standard PD is 15 [65, 66]. A retrospective analysis of over 200 PDs with an average lymph node yield of 30.8 revealed that the number of lymph nodes involved, the number of lymph node stations involved, and involvement of station 14 may all have an adverse prognostic impact on survival [67].
A consensus was reached that the following groups of lymph nodes must be dissected during a standard PD.
-
1.
Station 5: Suprapyloric
-
2.
Station 6: Subpyloric
-
3.
Station 8a: Hepatic artery superior
-
4.
Station 12b: Right side of hepatoduodenal ligament close to common bile duct
-
5.
Station 12c: Cystic duct lymph node
-
6.
Station 13: Posterior pancreaticoduodenal
-
7.
Station 14a, b: Right side of SMA from origin to inferior pancreaticoduodenal
-
8.
Station 17: Anterior pancreaticoduodenal
In left-sided resections the following lymph node stations need to be removed.
-
1.
Station 10: Splenic hilum
-
2.
Station 11: Splenic artery node
-
3.
Station 18: Along the inferior border of the body and tail of pancreas
-
4.
Station 9: Coeliac axis node in patients with carcinoma of the body of pancreas
The nomenclature of lymph nodes is based on the classification of the Japanese Pancreas Society.
No consensus was reached as to whether the 8p lymph node (posterior to the hepatic artery) should be dissected, as also regarding the 16b1 (interaortocaval) lymph node. However, the latter may be an integral part of clearance of the mesopancreas if it is considered a valid option in PD [68]. Others have suggested that it may have a poor prognosis and if positive, resection can be abandoned [69].
6.1.7 Have Laparoscopic and Robotic Technologies Made a Difference?
The first laparoscopic PD was reported by Gagner in 1994 [70]. Over two decades later, laparoscopic PD is still not the standard of care. There are several reasons for this: (i) laparoscopic PD demands a high degree of technical skill in laparoscopy and also experience in pancreatic surgery so that oncological outcomes (which are the main objectives of the procedure) are favourable [71]; (ii) the learning curve is long and it may span as many as 40 cases [72]. If there is a low volume of <10 cases/year, then it is very difficult to achieve the necessary expertise for safe PD; (iii) intraoperative complications may lead to mortality [73]; and finally (iv) long term oncological outcomes are lacking.
Several series including meta-analysis have shown equivalence in intraoperative and perioperative outcomes with laparoscopic PD as compared to open PD. Operating times are generally longer, but blood loss is diminished. Margin positivity and lymph node harvest rates have been similar [74–78]. A nationwide survey found that the complication rates, hospital stay and mortality were lower in the laparoscopy group. This is probably because in the absence of randomized trials, there is likely to be bias in selection of tumours for laparoscopic PD. Patients with low grade tumours such as intraductal papillary mucinous tumours, mucinous cystadenomas, and those away from the superior mesenteric vessels were included in the laparoscopic group. However, it must be emphasized that even major vein resection and reconstruction has been reported [76, 79]. There have also been suggestions that laparoscopic PD is preferably avoided in high risk pancreatic anastomosis such as those with soft glands and narrow ducts [80].
The current status of laparoscopic PD is therefore still not clearly defined. The operation is feasible and safe in the hands of surgeons who possess laparoscopic skills in abundance, and may have lower complication rates in a selected group of patients. However, the indications require to be defined more clearly. One must remember that these technical ‘advances’ are superimposed on the open technique of PD which is also evolving.
What about robotic PD? The advantages of robotic surgery are the three dimensional binocular vision and the high numbers of degrees of freedom in the movements that can be executed. This helps to overcome some of the restrictions that laparoscopic surgery places during a complex procedure such as PD. The feasibility and safety of the procedure has been established in case series. Boggi showed that robotic PD can be done safely without conversions; increased operating time and high costs being the major problems [81]. A meta-analysis of over 200 cases of robotic PD revealed comparable outcomes to open surgery. There was a marked heterogeneity among the cases. Patients could be categorized into (i) totally robotic technique, (ii) laparoscopic resection and robotic reconstruction, (iii) hand-port assisted laparoscopic resection and robotic reconstruction, or (iv) robotic resection and mini-laparotomy reconstruction. Conversion to open surgery occurred in 14 % of cases [82]. Zeh reported lower margin positivity rates in robotic PD [83] and attributed it to case selection—the use of the Pittsburgh model where (i) vascular involvement, (ii) tumour size >2.6 cm, and (iii) endoscopic ultrasound (EUS) staging showing advanced disease were associated with higher R1 resections [84]. In such cases, robotic PD was not used. It is arguable that these cases may well be candidates for neoadjuvant therapy.
Editorial Comments
The authors have dealt with some of the ongoing debates in pancreatic cancer surgery. There are other issues which too need attention and these are discussed below:
Borderline resectable cancer
This is a distinct clinical entity recognized in recent times. There is lack of prospective data by which one can advocate a suitable treatment strategy for the management of this entity. For the same reason, its definition has eluded broad consensus. By and large, these lesions fall between the obviously resectable and the locally advanced unresectable disease. Quite a few definitions are available. What is common in all is the use of a CT image to ascertain the relationship of the lesion with the vascular structures namely portal/superior mesenteric vein (PV/SMV), and superior mesenteric, gastroduodenal, hepatic and coeliac arteries.
A definition was initially proposed by the National Comprehensive Cancer Network (NCCN) in 2008 [85]. Soon after, the American HepatopancreatobiliaryAssociation (AHPBA), Society for Surgery of the Alimentary Tract (SSAT) and Society of Surgical Oncology (SSO) [86] developed a consensus statement, which was later accepted by the NCCN. According to this, borderline resectable cancer can be of three categories:
-
1.
Venous involvement of the SMV/PV: either abutment, encasement or short segment occlusion with a suitable vessel proximal and distal to the involved vessels which can be used for resection and reconstruction.
-
2.
Gastroduodenal artery encasement upto hepatic artery and short segment encasement/direct abutment of the hepatic artery without encroaching on the coeliac axis
-
3.
Less than 180 degree involvement of the SMA.
The MD Anderson group [87, 88] have defined borderline resectable pancreatic cancer as follows:
Type A: One or more of the following: Tumour abutment up to 180 degree of the circumference of SMA or coeliac axis or abutment or encasement more than 180 degree of a short segment of hepatic artery (usually at the origin of the gastroduodenal artery) or short segment occlusion of the SMV, PV or SMV–PV junction such that resection and reconstruction is possible.
Type B: Above features of borderline resectable disease with CT findings suggestive but not diagnostic of extra-pancreatic metastatic disease and proven N1 disease either by laparoscopy or EUS fine needle aspiration cytology.
Type C: Features of borderline resectable disease but with marginal performance status or better performance status but with associated severe co-existing co-morbid conditions precluding operation.
I feel this classification is more confusing than elaborative. Borderline resectable disease is an anatomical description. Adding non-anatomical factors in the classification of this entity does not serve any meaningful purpose as has been pointed out by Choti in the discussion accompanying the article from MD Anderson [88]. This is not to suggest that this is less important. In fact, it is the reverse.
The other classification has been described by Ishikawa et al. in 1992 [40]. It is based on radiological image characteristics that ascertain the relationship of the tumour with SMV and PV. Accordingly there are 5 types.
-
Type 1: Normal anatomy
-
Type 2: Smooth shift without narrowing
-
Type 3: Unilateral narrowing
-
Type 4: Bilateral narrowing and
-
Type 5: Bilateral narrowing with presence of collateral veins
This classification is simple, comprehensive and yet useful in most clinical situations. True, it is silent on extension of the tumour on the SMA. However, if we consider tumour extension on both sides of SMV–PV (Types 4 and 5), almost invariably the SMA will be involved with very occasional exceptions.
More recently, Tran Cao et al. [89] have given another useful classification based on tumour vein circumferential interface (TVI) describing as no interface, or up to 180 degree of circumference or more than 180 degree of circumference or occlusion. This system can predict if a patient needs venous resection. The classification correlates well with histological evidence of venous involvement. Not surprisingly, this system has been reported to predict survival as well [89].
There is much attention focused on borderline resectable disease. In pancreatic surgery for cancer, the margin status plays a major role in the prognosis. The results are better following R0 than R1 resections. Results of R2 resection are no better than non-operatively treated patients [90]. Borderline resectable cancer has the potential for a R0 resection. Involvement of vascular structures in the region of the pancreatic head is related more to anatomical than biological characteristics of the tumour. Therefore, all attempts should be made to achieve an R0 resection, if need be by resecting the affected vessel. The definitions outlined above will help the surgeon undertake such measures. Pathological examination of the resected specimens will identify if the margin is truly negative (R0) or microscopically positive (R1). The results of R1 resection are inferior to R0 resection but are still acceptable, as has been mentioned by the authors [90–92]. It may not be out of place to mention here that not all anatomical abnormalities on imaging are attributable to tumour invasion of the vessels. On a number of occasions, I have found no involvement of the vessels even when preoperative imaging has suggested involvement. I am inclined to believe that desmoplasia (quite common in pancreatic malignancy) [93] can explain this phenomenon.
The other approach is to down stage the disease by using neoadjuvant protocols; thereby converting all such tumours to be resectable. The details of this approach are beyond the scope of this write up.
Artery first approach for pancreaticoduodenectomy (PD)
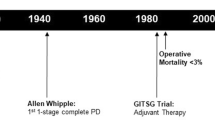
Even after 8 decades of the introduction of PD for pancreatic head cancer, the procedure is still evolving. This is related to better understanding of the pathobiology of this cancer, its image characteristics, technical advances in surgery and impact of resection margin. In the past tumours were resected only after it was ascertained that the PV/SMV is free of the disease. It was subsequently realised that venous involvement per se is not a contraindication for PD and resection and reconstruction of these veins can be done safely with results no different from standard PD [94]. Venous resection in a suitable patient is increasingly being done in contemporary surgical practice as long as a R0 status can be achieved. At present the focus has been on the SMA—whether it is involved or not. Its resection is technically feasible but it has increased mortality and morbidity. Moreover, it is not associated with better survival and hence it is not considered as a standard practice for PD. Thus the emphasis today is on accurate staging of the disease by high resolution CT imaging displaying the anatomy of the SMA and its relation with the tumour. Involvement of the SMA is a contraindication for PD [95]. For borderline resectable tumours, the artery-first approach is the most appropriate because it allows early detection of arterial involvement so that an irretrievable situation is avoided (not too uncommon a problem in the past when a surgeon used to proceed with a PD realising only at the end that the tumour has in fact involved the SMA—by that time a point of no return has already been reached!). This situation has to be avoided. The SMA first approach is a measure in that direction. There are a number of artery-first approaches described; each having its own advantage and disadvantage and are described below.
Posterior approach [96]: This is indicated for lesions located in the head and neck and for ampullary tumours extending to the head. Its advantage is early detection of arterial and venous involvement, detection of replaced/accessory right hepatic artery, and it allows adequate lymphadenectomy. However, it is difficult in the presence of severe inflammation.
Superior approach [97]: Tumours situated in the upper border of the pancreas can be best approached by this technique. All the relevant arteries can be identified by this approach (common hepatic, coeliac and superior mesenteric arteries).
Inferior supracolic (also called anterior approach) [98]: This is reserved for lesions of the lower border of the pancreas. The stomach and the neck of pancreas is resected early and this allows the so-called ‘no touch’ technique which facilitates en bloc resection without undue handling of the tumour.
Inferior infracolic approach [99]: Usually followed for lesions affecting the SMA at its origin but also can be done for lesions of the uncinate process. Its main advantage is early detection of a replaced right hepatic artery, early ligation of the inferior pancreaticoduodenal artery and superior dissection of the SMA especially its posterior aspect. It is particularly difficult to do in heavily built individuals.
Medial uncinate approach [100]: This is suitable for uncinate process lesions. It allows early detection of SMA involvement. Its advantage is ligation of the inferior pancreaticoduodenal artery can be done early due to which bleeding can be minimised. It is especially useful for lesions requiring total pancreatectomy. The main problem is identification of a replaced right hepatic artery.
Left posterior approach [101]: It is suitable for lesions confined to the ventral pancreas as well as uncinate process. SMA can be dissected even without Kocherization. Inferior pancreaticoduodenal artery ligation can be done early and it minimises bleeding. Since it skeletonises the SMA extensively, the incidence of postoperative bothersome diarrhoea is high (due to damage to autonomic sympathetic nerves).
Lymphadenectomy during PD
The most important factor to determine prognosis following PD is involvement of the lymph nodes. The other bad prognostic markers are positive resection margins of the pancreas and the retroperitoneal tissues. We now have better imaging, surgical techniques, pre- and postoperative therapies but the results of PD for adenocarcinoma of the pancreatic head is no better than what it was in the past [102]. Clearly, this reflects true biological behaviour of these cancers. In a meta-analysis of 4005 patients of PD, the overall survival was only 13 months with a 5-year survival of 6.8 % [103]. Almost similar results (median survival of 13–18 months and a 5-year survival of 15 %–30 %) have been reported by Wilkowski et al. [104]. Standard PD for cancer is associated with high recurrence rate possibly due to positive lymph nodes [27]. Therefore, it should be logical to do a more extensive lymphadenectomy. The International Congress in Italy advised excision of all lymph nodes and soft tissues along the proper hepatic artery, anterior surface of the vena cava and aorta; extending the same soft tissue excision along the portal vein up to the inferior mesenteric artery [62].
Lymphatic drainage of the pancreatic head occurs through the superior and inferior channels. The superior one drains in lymph nodes around the coeliac trunk and the inferior one drains into lymph nodes situated in relation to the origin of the SMA. In addition, there are certain lymphatic channels which drain into the cisterna chylae, either directly or through the para-aortic lymph nodes [105]. These latter channels, when disrupted can cause chyle leak following PD. The Japanese nodal staging system based on this lymphatic drainage patterns focuses on specific lymph node groups. The lymph nodes in the head region are located either anteriorly (station 17) or posteriorly (station 13). From these, the efferent vessels drain into lymph nodes along the SMA (station 14) before reaching the para-aortic nodes (station 16). Occasionally, lymphatics drain directly into lymph nodes along the hepatic artery proper (station 8) ultimately reaching the para-aortic nodes via the coeliac nodes (station 9).
Standard lymphadenectomy involves removal of all of the following lymph nodes—from above downwards these are lymph nodes along hepatoduodenal ligament (station 12), supra and infra pyloric lymph nodes (stations 5 and 6), those along the front of the common hepatic artery (station 8), anterior and posterior pancreatoduodenal lymph nodes (stations 17 and 13) and lymph nodes along the SMA (station 14) [106].
Extended lymphadenectomy on the other hand removes lymphatics starting from the porta hepatis on the right to the aortic opening of the diaphragm on the left. Dissection further continues to the splenic and both renal hila and then downwards up to the inferior mesenteric artery circumferentially removing tissues and lymph nodes around the origins of the coeliac and superior mesenteric arteries; in the process lymph nodes at station 7 (left gastric), station 9 (coeliac trunk), station 10 (splenic hilum), station 11 (splenic artery), station 16 (para-aortic) and station 18 (inferior border of pancreas) are removed in addition to what is removed in a standard dissection [58].
The fact that the local recurrence rate even after adjuvant therapy following surgical resection is high (ranging from 70 to 88 %) calls for wide clearance of the retroperitoneal soft tissues around the pancreatic head (the so-called mesopancreas consisting of loose areolar tissue, fat, lymphatics, capillaries and nerve plexus) and the related arteries as mentioned earlier. This improves not only the R0 resection rates, but also removes the affected lymph nodes in the draining areas [106]. So should one do a standard or an extended lymph node dissection? At least 7 prospective studies have assessed results (especially survival) of extended lymphadenectomy. None of these has found any survival benefit [107]. However, the procedure has similar morbidity and mortality as a standard lymphadenectomy [108]. Extended lymph nodal resections can be associated with troublesome delayed gastric emptying and disturbing diarrhoea. In view of these, most experts recommend standard rather than extended lymphatic clearance. The consensus meeting of the International Study Group on Pancreatic Surgery (ISGPS) which was held in 2014 in Verona. made the following statements on this subject: (i) For classification of lymph node stations, the classification of the Japanese Pancreas Society should be followed; (ii) Extended lymphadenectomy should be avoided as it does not improve oncological outcome; (iii) lymphadenectomy should include removal of nodes at stations 5, 6, 12, 8, 13, 17 and 14 for pancreatoduodenectomy and stations 9, 10, 11 and 18 for tumours of the body of pancreas [63]. The disadvantage of lymphadenectomy is that it removes lymph nodes which are normal with potential immunoprotective function such as trapping the offending agent like the tumour cell and the bacteria. Therefore its unnecessary removal deprives the normal lymphocytes their important immune function against cancer cells [109].
The consensus statement of the ISGPS (mentioned above) as well as various other publications stresses that at least 15 lymph nodes should be removed and pathologically examined for accurate lymph nodal staging. Lymph node positivity has a variable impact on survival. While some have reported survival benefit in N0 patients, others have reported better survival in N1 patients. Still others have reported that the number of lymph nodes is not a predictor of survival [63]. The ratio of positive to total number of lymph nodes >0.2 is also considered to be a poor predictor of postoperative survival [63].
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30.
Gnerlich JL, Luka SR, Deshpande AD, Dubray BJ, Weir JS, Carpenter DH, et al. Microscopic margins and patterns of treatment failure in resected pancreatic adenocarcinoma. Arch Surg. 2012;147:753–60.
Hishinuma S, Ogata Y, Tomikawa M, Ozawa I, Hirabayashi K, Igarashi S. Patterns of recurrence after curative resection of pancreatic cancer, based on autopsy findings. J Gastrointest Surg. 2006;10:511–8.
Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004;350:1200–10.
Smeenk HG, van Eijck CHJ, Hop WC, Erdmann J, Tran KCK, Debois M, et al. Long-term survival and metastatic pattern of pancreatic and periampullary cancer after adjuvant chemoradiation or observation: long-term results of EORTC trial 40891. Ann Surg. 2007;246:734–40.
Van Laethem J-L, Hammel P, Mornex F, Azria D, Van Tienhoven G, Vergauwe P, et al. Adjuvant gemcitabine alone versus gemcitabine-based chemoradiotherapy after curative resection for pancreatic cancer: a randomized trial. J Clin Oncol. 2010;28:4450–6.
Hammel P, Huguet F, van Laethem J-L, Goldstein D, Glimelius B, Artru P, et al. Effect of chemoradiotherapy vs chemotherapy on survival in patients with locally advanced pancreatic cancer controlled after 4 months of gemcitabine with or without erlotinib: The LAP07 randomized clinical trial. JAMA. 2016;315:1844–53.
Andriulli A, Festa V, Botteri E, Valvano MR, Koch M, Bassi C, et al. Neoadjuvant/preoperative gemcitabine for patients with localized pancreatic cancer: a meta-analysis of prospective studies. Ann Surg Oncol. 2012;19:1644–62.
Gillen S, Schuster T, Meyer Zum Buschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;7:e1000267.
Kanda M, Fujii T, Nagai S, Kodera Y, Kanzaki A, Sahin TT, et al. Pattern of lymph node metastasis spread in pancreatic cancer. Pancreas. 2011;40:951–5.
Adham M, Jaeck D, Le Borgne J, Oussoultzouglou E, Chenard-Neu M-P, Mosnier J-F, et al. Long-term survival (5–20 years) after pancreatectomy for pancreatic ductal adenocarcinoma: a series of 30 patients collected from 3 institutions. Pancreas. 2008;37:352–7.
Raut CP, Tseng JF, Sun CC, Wang H, Wolff RA, Crane CH, et al. Impact of resection status on pattern of failure and survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann Surg. 2007;246:52–60.
Menon KV, Gomez D, Smith AM, Anthoney A, Verbeke CS. Impact of margin status on survival following pancreatoduodenectomy for cancer: The Leeds Pathology Protocol (LEEPP. HPB (Oxford). 2009;11:18–24.
Gaedcke J, Gunawan B, Grade M, Szoke R, Liersch T, Becker H, et al. The mesopancreas is the primary site for R1 resection in pancreatic head cancer: relevance for clinical trials. Langenbecks Arch Surg. 2010;395:451–8.
Gockel I, Domeyer M, Wolloscheck T, Konerding MA, Junginger T. Resection of the mesopancreas (RMP): a new surgical classification of a known anatomical space. World J Surg Oncol. 2007;5:44.
Popescu I, Dumitrascu T. Total meso-pancreas excision: key point of resection in pancreatic head adenocarcinoma. Hepatogastroenterology. 2011;58:202–7.
Kawabata Y, Tanaka T, Nishi T, Monma H, Yano S, Tajima Y. Appraisal of a total meso-pancreatoduodenum excision with pancreaticoduodenectomy for pancreatic head carcinoma. Eur J Surg Oncol. 2012;38:574–9.
Peparini N, Caronna R, Chirletti P. The ‘meso’ of the rectum and the ‘meso’ of the pancreas: similar terms but distinct concepts in surgical oncology. Hepatobiliary Pancreat Dis Int. 2015;14:548–51.
Chowdappa R, Challa VR. Mesopancreas in pancreatic cancer: where do we stand—review of literature. Indian J Surg Oncol. 2015;6:69–74.
Dumitrascu T, Popescu I. Total mesopancreas excision in pancreatic head adenocarcinoma: the same impact as total mesorectal excision in rectal carcinoma? Comment on article ‘surgical technique and results of total mesopancreas excision in pancreatic tumours’ by Adham M and Singhirunnusorn J, Eur J Surg Oncol, 2012. Eur J Surg Oncol 2012;38:725; author reply 726.
Welsch T, Bork U, Distler M, Weitz J. Top-down approach to the superior mesenteric artery and the mesopancreas during pancreatoduodenectomy for pancreatic cancer. J Surg Oncol. 2016;113:668–71.
Adham M, Singhirunnusorn J. Surgical technique and results of total mesopancreas excision (TMpE) in pancreatic tumors. Eur J Surg Oncol. 2012;38:340–5.
Wellner UF, Krauss T, Csanadi A, Lapshyn H, Bolm L, Timme S, et al. Mesopancreatic stromal clearance defines curative resection of pancreatic head cancer and can be predicted preoperatively by radiologic parameters: a retrospective study. Medicine (Baltimore). 2016;95:e2529.
Nitschke P, Volk A, Welsch T, Hackl J, Reissfelder C, Rahbari M, et al. Impact of intraoperative re-resection to achieve R0 status on survival in patients with pancreatic cancer: a single-center experience with 483 patients. Ann Surg 2016; published online June 8.
Takaori K, Bassi C, Biankin A, Brunner TB, Cataldo I, Campbell F, et al. International Association of Pancreatology (IAP)/European Pancreatic Club (EPC) consensus review of guidelines for the treatment of pancreatic cancer. Pancreatology. 2016;16:14–27.
Neoptolemos JP, Stocken DD, Bassi C, Ghaneh P, Cunningham D, Goldstein D, et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA. 2010;304:1073–81.
Evans DB, Farnell MB, Lillemoe KD, Vollmer CJ, Strasberg SM, Schulick RD. Surgical treatment of resectable and borderline resectable pancreas cancer: expert consensus statement. Ann Surg Oncol. 2009;16:1736–44.
Gill AJ, Johns AL, Eckstein R, Samra JS, Kaufman A, Chang DK, et al. Synoptic reporting improves histopathological assessment of pancreatic resection specimens. Pathology 2009;41:161–7.
Campbell F, Smith RA, Whelan P, Sutton R, Raraty M, Neoptolemos JP, et al. Classification of R1 resections for pancreatic cancer: the prognostic relevance of tumour involvement within 1 mm of a resection margin. Histopathology. 2009;55:277–83.
Delpero JR, Bachellier P, Regenet N, Le Treut YP, Paye F, Carrere N, et al. Pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: a French multicentre prospective evaluation of resection margins in 150 evaluable specimens. HPB (Oxford). 2014;16:20–33.
Chang DK, Johns AL, Merrett ND, Gill AJ, Colvin EK, Scarlett CJ, et al. Margin clearance and outcome in resected pancreatic cancer. J Clin Oncol. 2009;27:2855–62.
Chandrasegaram MD, Goldstein D, Simes J, Gebski V, Kench JG, Gill AJ, et al. Meta-analysis of radical resection rates and margin assessment in pancreatic cancer. Br J Surg. 2015;102:1459–72.
Tseng JF, Pisters PWT, Lee JE, Wang H, Gomez HF, Sun CC, et al. The learning curve in pancreatic surgery. Surgery. 2007;141:694–701.
Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess H, et al. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 2008;15:1651–60.
Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232–7.
Rau BM, Moritz K, Schuschan S, Alsfasser G, Prall F, Klar E. R1 resection in pancreatic cancer has significant impact on long-term outcome in standardized pathology modified for routine use. Surgery. 2012;152:S103–11.
Maksymov V, Hogan M, Khalifa MA. An anatomical-based mapping analysis of the pancreaticoduodenectomy retroperitoneal margin highlights the urgent need for standardized assessment. HPB (Oxford). 2013;15:218–23.
Gebauer F, Tachezy M, Vashist YK, Marx AH, Yekebas E, Izbicki JR, et al. Resection margin clearance in pancreatic cancer after implementation of the Leeds Pathology Protocol (LEEPP): clinically relevant or just academic? World J Surg. 2015;39:493–9.
Fuhrman GM, Leach SD, Staley CA, Cusack JC, Charnsangavej C, Cleary KR, et al. Rationale for en bloc vein resection in the treatment of pancreatic adenocarcinoma adherent to the superior mesenteric-portal vein confluence. Pancreatic Tumor Study Group. Ann Surg. 1996;223:154–62.
Ishikawa O, Ohigashi H, Imaoka S, Furukawa H, Sasaki Y, Fujita M, et al. Preoperative indications for extended pancreatectomy for locally advanced pancreas cancer involving the portal vein. Ann Surg. 1992;215:231–6.
Nakao A, Kanzaki A, Fujii T, Kodera Y, Yamada S, Sugimoto H, et al. Correlation between radiographic classification and pathological grade of portal vein wall invasion in pancreatic head cancer. Ann Surg. 2012;255:103–8.
Pilgrim CHC, Tsai S, Tolat P, Patel P, Rilling W, Evans DB, et al. Optimal management of the splenic vein at the time of venous resection for pancreatic cancer: Importance of the inferior mesenteric vein. J Gastrointest Surg. 2014;18:917–21.
Smoot RL, Christein JD, Farnell MB. An innovative option for venous reconstruction after pancreaticoduodenectomy: the left renal vein. J Gastrointest Surg. 2007;11:425–31.
Dokmak S. Pancreaticoduodenectomy with reconstruction of the mesentericoportal vein by the parietal peritoneum: ‘Safi Dokmak Vascular Graft’. Ann Surg Oncol 2015;22 Suppl 3:S343–S344.
Dokmak S, Aussilhou B, Sauvanet A, Nagarajan G, Farges O, Belghiti J. Parietal peritoneum as an autologous substitute for venous reconstruction in hepatopancreatobiliary surgery. Ann Surg. 2015;262:366–71.
Smoot RL, Christein JD, Farnell MB. Durability of portal venous reconstruction following resection during pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1371–5.
Kim PTW, Wei AC, Atenafu EG, Cavallucci D, Cleary SP, Moulton C-A, et al. Planned versus unplanned portal vein resections during pancreaticoduodenectomy for adenocarcinoma. Br J Surg. 2013;100:1349–56.
Barreto SG, Windsor JA. Justifying vein resection with pancreatoduodenectomy. Lancet Oncol. 2016;17:e118–24.
Yu XZ, Li J, DL F, Di Y, Yang F, Hao SJ, et al. Benefit from synchronous portal-superior mesenteric vein resection during pancreaticoduodenectomy for cancer: a meta-analysis. Eur J Surg Oncol. 2014;40:371–8.
Turrini O, Ewald J, Barbier L, Mokart D, Blache JL, Delpero JR. Should the portal vein be routinely resected during pancreaticoduodenectomy for adenocarcinoma? Ann Surg. 2013;257:726–30.
Fortner JG, Kim DK, Cubilla A, Turnbull A, Pahnke LD, Shils ME. Regional pancreatectomy: en bloc pancreatic, portal vein and lymph node resection. Ann Surg. 1977;186:42–50.
Mollberg N, Rahbari NN, Koch M, Hartwig W, Hoeger Y, Buchler MW, et al. Arterial resection during pancreatectomy for pancreatic cancer: a systematic review and meta-analysis. Ann Surg. 2011;254:882–93.
Hicks CW, Burkhart RA, Weiss MJ, Wolfgang CL, Cameron AM, Pawlik TM. Management of type 9 hepatic arterial anatomy at the time of pancreaticoduodenectomy: considerations for preservation and reconstruction of a completely replaced common hepatic artery. J Gastrointest Surg. 2016;20:1400–4.
Klempnauer J, Ridder GJ, Bektas H, Pichlmayr R. Extended resections of ductal pancreatic cancer—impact on operative risk and prognosis. Oncology. 1996;53:47–53.
Hartwig W, Hackert T, Hinz U, Hassenpflug M, Strobel O, Buchler MW, et al. Multivisceral resection for pancreatic malignancies: risk-analysis and long-term outcome. Ann Surg. 2009;250:81–7.
Burdelski CM, Reeh M, Bogoevski D, Gebauer F, Tachezy M, Vashist YK, et al. Multivisceral resections in pancreatic cancer: identification of risk factors. World J Surg. 2011;35:2756–63.
Hartwig W, Vollmer CM, Fingerhut A, Yeo CJ, Neoptolemos JP, Adham M, et al. Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS). Surgery. 2014;156:1–14.
Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P, Pasquali C, et al. Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study group. Ann Surg. 1998;228:508–17.
Yeo CJ, Cameron JL, Sohn TA, Coleman J, Sauter PK, Hruban RH, et al. Pancreaticoduodenectomy with or without extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma: comparison of morbidity and mortality and short-term outcome. Ann Surg. 1999;229:613–22.
Nimura Y, Nagino M, Takao S, Takada T, Miyazaki K, Kawarada Y, et al. Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci. 2012;19:230–41.
Farnell MB, Pearson RK, Sarr MG, DiMagno EP, Burgart LJ, Dahl TR, et al. A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery. 2005;138:618–28.
Pedrazzoli S, Beger HG, Obertop H, Andren-Sandberg A, Fernandez-Cruz L, Henne-Bruns D, et al. A surgical and pathological based classification of resective treatment of pancreatic cancer. Summary of an international workshop on surgical procedures in pancreatic cancer. Dig Surg. 1999;16:337–45.
Tol JAMG, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS. Surgery. 2014;156:591–600.
Michalski CW, Kleeff J, Wente MN, Diener MK, Buchler MW, Friess H. Systematic review and meta-analysis of standard and extended lymphadenectomy in pancreaticoduodenectomy for pancreatic cancer. Br J Surg. 2007;94:265–73.
Pedrazzoli S, Michelassi F. Extent of lymphadenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas. J Gastrointest Surg. 2000;4:229–30.
Pedrazzoli S. Extent of lymphadenectomy to associate with pancreaticoduodenectomy in patients with pancreatic head cancer for better tumor staging. Cancer Treat Rev. 2015;41:577–87.
Malleo G, Maggino L, Capelli P, Gulino F, Segattini S, Scarpa A, et al. Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the standard International Study Group of Pancreatic Surgery definition of lymphadenectomy for cancer. J Am Coll Surg 2015;221:367–379.e4.
Peparini N. Para-Aortic dissection in pancreaticoduodenectomy with mesopancreas excision for pancreatic head carcinoma: Not only an N-staging matter. J Gastrointest Surg. 2016;20:1080–1.
Paiella S, Malleo G, Maggino L, Bassi C, Salvia R, Butturini G. Pancreatectomy with para-aortic lymph node dissection for pancreatic head adenocarcinoma: pattern of nodal metastasis spread and analysis of prognostic factors. J Gastrointest Surg. 2015;19:1610–20.
Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994;8:408–10.
Mesleh MG, Stauffer JA, Asbun HJ. Minimally invasive surgical techniques for pancreatic cancer: ready for prime time? J Hepatobiliary Pancreat Sci. 2013;20:578–82.
Wang M, Meng L, Cai Y, Li Y, Wang X, Zhang Z, et al. Learning curve for laparoscopic pancreaticoduodenectomy: a CUSUM analysis. J Gastrointest Surg. 2016;20:924–35.
Gooiker GA, van Gijn W, Wouters MWJM, Post PN, van de Velde CJH, Tollenaar RAEM. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg. 2011;98:485–94.
Cho A, Yamamoto H, Nagata M, Takiguchi N, Shimada H, Kainuma O, et al. Comparison of laparoscopy-assisted and open pylorus-preserving pancreaticoduodenectomy for periampullary disease. Am J Surg. 2009;198:445–9.
Palanivelu C, Jani K, Senthilnathan P, Parthasarathi R, Rajapandian S, Madhankumar MV. Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg. 2007;205:222–30.
Palanisamy S, Deuri B, Naidu SB, Vaiyapurigoundar Palanisamy N, Natesan AV, Palanivelu PR, et al. Major venous resection and reconstruction using a minimally invasive approach during laparoscopic pancreaticoduodenectomy: one step forward. Asian J Endosc Surg. 2015;8:468–72.
Doula C, Kostakis ID, Damaskos C, Machairas N, Vardakostas DV, Feretis T, et al. Comparison between minimally invasive and open pancreaticoduodenectomy: a systematic review. Surg Laparosc Endosc Percutan Tech. 2016;26:6–16.
Correa-Gallego C, Dinkelspiel HE, Sulimanoff I, Fisher S, Vinuela EF, Kingham TP, et al. Minimally-invasive vs open pancreaticoduodenectomy: systematic review and meta-analysis. J Am Coll Surg. 2014;218:129–39.
Kendrick ML, Sclabas GM. Major venous resection during total laparoscopic pancreaticoduodenectomy. HPB (Oxford). 2011;13:454–8.
Dokmak S, Fteriche FS, Aussilhou B, Bensafta Y, Levy P, Ruszniewski P, et al. Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg. 2015;220:831–8.
Boggi U, Signori S, De Lio N, Perrone VG, Vistoli F, Belluomini M, et al. Feasibility of robotic pancreaticoduodenectomy. Br J Surg. 2013;100:917–25.
Cirocchi R, Partelli S, Trastulli S, Coratti A, Parisi A, Falconi MA. Systematic review on robotic pancreaticoduodenectomy. Surg Oncol. 2013;22:238–46.
Zeh HJ, Zureikat AH, Secrest A, Dauoudi M, Bartlett D, Moser AJ. Outcomes after robot-assisted pancreaticoduodenectomy for periampullary lesions. Ann Surg Oncol. 2012;19:864–70.
Bao P, Potter D, Eisenberg DP, Lenzner D, Zeh HJ, Lee Iii KK, et al. Validation of a prediction rule to maximize curative (R0) resection of early-stage pancreatic adenocarcinoma. HPB (Oxford). 2009;11:606–11.
National comprehensive cancer network practice guidelines in oncology for pancreatic adenocarcinoma. November 2008. Available at www.nccn.org . Accessed on 15 Jun 2016.
Callery MP, Chang KJ, Fishman EK, Talamonti MS, William Traverso L, Linehan DC. Pretreatment assessment of resectable and borderline resectable pancreatic cancer: expert consensus statement. Ann Surg Oncol. 2009;16:1727–33.
Varadhachary GR, Tamm EP, Abbruzzese JL, Xiong HQ, Crane CH, Wang H, et al. Borderline resectable pancreatic cancer: definitions, management, and role of preoperative therapy. Ann Surg Oncol. 2006;13:1035–46.
Katz MH, Pisters PW, Evans DB, Sun CC, Lee JE, Fleming JB, et al. Borderline resectable pancreatic cancer: The importance of this emerging stage of disease. J Am Coll Surg 2008;206:833–846; discussion 846–8.
Tran Cao HS, Balachandran A, Wang H, Nogueras-González GM, Bailey CE, Lee JE, et al. Radiographic tumor-vein interface as a predictor of intraoperative, pathologic, and oncologic outcomes in resectable and borderline resectable pancreatic cancer. J Gastrointest Surg 2014;18:269–278; discussion 278.
Bilimoria KY, Talamonti MS, Sener SF, Bilimoria MM, Stewart AK, Winchester DP, et al. Effect of hospital volume on margin status after pancreaticoduodenectomy for cancer. J Am Coll Surg. 2008;207:510–9.
Neoptolemos JP, Stocken DD, Dunn JA, Almond J, Beger HG, Pederzoli P, et al. European Study Group for Pancreatic Cancer. Influence of resection margins on survival for patients with pancreatic cancer treated by adjuvant chemoradiation and/or chemotherapy in the ESPAC-1 randomized controlled trial. Ann Surg. 2001;234:758–68.
Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 2006;10:1199–1210; discussion 1210–1.
Apte MV, Park S, Phillips PA, Santucci N, Goldstein D, Kumar RK, et al. Desmoplastic reaction in pancreatic cancer: role of pancreatic stellate cells. Pancreas. 2004;29:179–87.
Allema JH, Reinders ME, van Gulik TM, van Leeuwen DJ, de Wit LT, Verbeek PC, et al. Portal vein resection in patients undergoing pancreatoduodenectomy for carcinoma of the pancreatic head. Br J Surg. 1994;81:1642–6.
Seufferlein T, Bachet JB, Van Cutsem E, Rougier P; ESMO Guidelines Working Group. Pancreatic adenocarcinoma: ESMO-ESDO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2012;23 Suppl 7:vii33–40.
Pessaux P, Varma D, Arnaud JP. Pancreaticoduodenectomy: Superior mesenteric artery first approach. J Gastrointest Surg. 2006;10:607–11.
Makino I, Kitagawa H, Ohta T, Nakagawara H, Tajima H, Ohnishi I, et al. Nerve plexus invasion in pancreatic cancer: Spread patterns on histopathologic and embryological analyses. Pancreas. 2008;37:358–65.
Hirota M, Kanemitsu K, Takamori H, Chikamoto A, Tanaka H, Sugita H, et al. Pancreatoduodenectomy using a no-touch isolation technique. Am J Surg. 2010;199:e65–8.
Weitz J, Rahbari N, Koch M, Büchler MW. The “artery first” approach for resection of pancreatic head cancer. J Am Coll Surg. 2010;210:e1–4.
Hackert T, Werner J, Weitz J, Schmidt J, Büchler MW. Uncinate process first—a novel approach for pancreatic head resection. Langenbecks Arch Surg. 2010;395:1161–4.
Kurosaki I, Minagawa M, Takano K, Takizawa K, Hatakeyama K. Left posterior approach to the superior mesenteric vascular pedicle in pancreaticoduodenectomy for cancer of the pancreatic head. JOP. 2011;12:220–9.
Pavlidis TE, Pavlidis ET, Sakantamis AK. Current opinion on lymphadenectomy in pancreatic cancer surgery. Hepatobiliary Pancreat Dis Int. 2011;10:21–5.
Glanemann M, Shi B, Liang F, Sun XG, Bahra M, Jacob D, et al. Surgical strategies for treatment of malignant pancreatic tumors: extended, standard or local surgery? World J Surg Oncol. 2008;6:123.
Wilkowski R, Wolf M, Heinemann V. Primary advanced unresectable pancreatic cancer. Recent Results Cancer Res. 2008;177:79–93.
Kitagawa H, Ohta T, Makino I, Tani T, Tajima H, Nakagawara H, et al. Carcinomas of the ventral and dorsal pancreas exhibit different patterns of lymphatic spread. Front Biosci. 2008;13:2728–35.
Kostov D. Lymphadenectomy in pancreatic cancer surgery. In: Recent advances in pancreatic cancer. Available at www.avidscience.com/book/recent-advances-in-pancreatic-cancer/ . Accessed on 15 Jul 2016.
Kontis E, Prassas E, Srinivasan P, Prachalias A. Extended lymphadenectomy and mesopancreas excision during pancreatoduodenectomy for cancer: is it worth it? Review of current evidence. J Pancreas. 2016;17:149–58.
Pedrrazzoli S, Pasqua C, Sperti C. Extent of lymphadenectomy in the resection of pancreatic cancer. Analysis of the existing evidence. Ann Acad Med Bialoostacensis. 2005;50:85–90.
Cady B. Fundamentals of contemporary surgical oncology: Biologic principles and the threshold concept govern treatment and outcomes. J Am Coll Surg. 2001;192:777–92.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Indian Association of Surgical Gastroenterology
About this chapter
Cite this chapter
Ramesh, H., Mathew, J., Manipadam, J.M., Galodha, S. (2017). Controversies in Surgery for Pancreatic Cancer. In: Sahni, P., Pal, S. (eds) GI Surgery Annual. GI Surgery Annual, vol 23. Springer, Singapore. https://doi.org/10.1007/978-981-10-2678-2_6
Download citation
DOI: https://doi.org/10.1007/978-981-10-2678-2_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2677-5
Online ISBN: 978-981-10-2678-2
eBook Packages: MedicineMedicine (R0)