Abstract
Tumor recurrence is the main limitation of liver transplantation in patients with hepatocellular carcinoma (HCC) and can be promoted by immunosuppressants. However, no prevention or treatment exists for HCC recurrence after liver transplantation. Here, we describe an adoptive immunotherapy approach that uses natural killer (NK) cells derived from both living and deceased donor liver graft perfusates. Liver NK cells exhibited the vigorous cytotoxicity against hepatoma cell line after IL-2 stimulation through the tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL)-TRAIL receptor pathway. In an in vivo mouse model, adoptive transfer of TRAIL-expressing liver NK cells inhibited the growth of liver tumors. Taken together, these findings suggest that we have established a method of retrieving NK cells from donor liver graft perfusate under current good manufacturing practice conditions for the treatment of liver transplant recipients with HCC. Clinical trials of adoptive immunotherapy with liver NK cells have been conducted in both living and deceased donor liver transplantations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Hepatocellular carcinoma (HCC) is one of the most common reasons for liver transplantation. However, HCC recurrence remains a serious issue after liver transplantation. The use of postoperative immunosuppression in the transplant recipient poses an additional risk for recurrence and hinders the use of cytotoxic chemotherapy drugs [1–4]. The major problem for HCC recurrence after liver transplantation is that no definitive treatment or prevention modalities exist [5, 6].
Natural killer (NK) cell is a major innate immune component and a first-line defense against invading infectious microbes and neoplastic cells [7]. Functional impairment and decreased number of NK cells have been observed in HCC and cirrhotic patients [8–10]. These functional defects in NK cells might be responsible for the failure of antitumor immune responses after liver transplantation in patients with HCC. Since the immunosuppressive regimen that is currently used after liver transplant reduces adaptive immune components but effectively maintains the innate components of cellular immunity [11–13], augmentation of the NK cell response may be a promising immunotherapeutic approach [14].
2 Immunotherapy Using NK Cells
2.1 Characteristics of NK Cells
NK cells can destroy many solid tissue-derived malignant cells through two major mechanisms that induce target cell apoptosis, granule-dependent killing, and death receptor stimulation [15]. Granule-dependent killing includes the release of perforin and granzymes [16], while the death receptor pathway is mostly mediated by apoptosis-inducing members of the TNF superfamily such as FasL, TNF-α, and tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) [17, 15]. NK cells can also produce high levels of cytokines including IFN-γ, which may play a role in tumor growth regulation [18].
2.2 NK Immunotherapy for Cancers
Adoptive cancer immunotherapy was pioneered by Rosenberg and collaborators using cytokine-induced killer (CIK) cells including many NK cell-containing populations [19], but subsequent studies showed that similar antitumor effects could be achieved with high-dose IL-2 alone [20]. Because of the lack of significant clinical effects after treatment with autologous NK cells [21, 20], the focus has more recently shifted toward the potential of allogeneic NK cells in adoptive cell therapy for cancer treatment [22]. Miller et al. reported successful adoptive immunotherapy using short-term ex vivo activated haploidentical NK cells in patients with blood cancers [13]. In HCC patients, adoptive immunotherapy with cytokine-induced killer (CIK) cells prolonged the overall survival and time to recurrence in some clinical trials [23, 24]. There are few clinical trials that examine adoptive immunotherapy with liver NK cells for HCC because of the limited availability of sufficient NK cells from the liver.
3 Cytotoxic Potential of Liver-Derived NK Cells
3.1 Liver-Derived NK Cells in Mice
NK cells are quite abundant in the liver of mice, in contrast to the relatively small percentage in peripheral lymphatics [25, 26]. In addition, liver NK cells have been shown to mediate higher cytotoxic activity against tumor cells than those derived from the spleen or peripheral blood in rodents [26, 27]. The antitumor activity of liver NK cells was shown to decrease after partial hepatectomy, suggesting that immunosuppressed patients are susceptible to HCC recurrence after partial hepatectomy or liver transplantation [28–30]. We recently tested this hypothesis using a mouse model [14]. CD69 and TRAIL expression levels on liver NK cells were temporarily downregulated after extended partial hepatectomy (Fig. 4.1). The adoptive transfer of NK cells, including those expressing TRAIL, extracted from the liver perfusate of poly I:C-stimulated C57BL/6 (B6) mice inhibited the growth of liver metastasis in B6 or B6xBALB/c F1 (B6CF1) mice that had undergone hepatectomy and received intraportal Hepa 1–6 injection (Fig. 4.2). These findings suggest that adoptive immunotherapy using activated NK cells extracted from normal liver perfusate may be a novel technique for reconstituting the livers of living donor liver transplant recipients with HCC that are immunosuppressed.
The kinetics of TRAIL expression on liver NK cells after hepatectomy. (a) The numbers presented are means ± SEM of the TRAIL-positive cell population in NK cell subsets. *p < 0.01 for day 3, day 7, and day 14 compared to the control. (b) The numbers indicate the mean fluorescence intensity of cells that stained positive for TRAIL. *p < 0.01 for day 1 and day 3 compared to the control
The adoptive transfer of activated liver NK cells inhibited the growth of liver metastasis induced by a portal venous injection of hepatoma cells in extensively hepatectomized mice. (a) Representative histopathological findings of the liver specimen. Specimens from the untreated (left), partially hepatectomized (PHx; middle), and NK cell-receiving groups that were inoculated after partial hepatectomy (right). The adoptive transfer of activated B6 liver NK cells inhibited the growth of liver metastasis induced by a portal venous injection of hepatoma cells (Hepa 1–6; 5 × 105 cells) in extensively hepatectomized B6 mice (b) and B6CF1 mice (c)
3.2 Liver NK Cells in Human
Differences between liver and peripheral blood NK cells have not been extensively investigated in human because of the limited availability of appropriate human samples. We have recently determined the phenotypic and functional properties of NK cells extracted from donor and recipient liver perfusate in clinical living donor liver transplantation [10]. Donor liver NK cells exhibited the most vigorous cytotoxicity against a hepatocellular carcinoma cell line after in vitro IL-2 stimulation, compared to the activities of donor and recipient peripheral blood NK cells and recipient liver NK cells (Fig. 4.3). IL-2 stimulation increased TRAIL expression, which has been shown to be critical for NK cell-mediated antitumor cell killing without affecting normal cells, on liver NK cells (Fig. 4.4) [31, 32]. In addition, we have confirmed that death-inducing TRAIL receptors, TRAIL-R1/death receptor (DR) 4, and TRAIL-R2/DR5, which contain cytoplasmic death domains and signal apoptosis, are expressed in HCC [33, 34]. These findings suggest a novel concept to prevent recurrence of HCC after liver transplantation, the adoptive transfer of IL-2-stimulated NK cells extracted from donor liver graft into recipients.
IL-2-stimulated donor liver NK cells show vigorous cytotoxicity against HepG2 cells. NK cytotoxic activities of indicated effectors against indicated target cells were analyzed by 51Cr release assay. (a) NK cytotoxic activities of IL-2-stimulated liver mononuclear cell (LMNC) and peripheral blood mononuclear cell (PBMC) populations that were cultivated for 4 days in the presence of IL-2 before the cytotoxic assay. Percentages of CD3−CD56+ NK cells in LMNC or PBMC fractions obtained from 4 adult healthy donors and 4 corresponding recipients with cirrhosis are shown in the upper right corner (means ± SEM). (b) NK cytotoxic activities of NK and non-NK cells isolated from IL-2-stimulated donor LMNC and PBMC populations against HepG2 target cells
Liver NK cells inductively express remarkable levels of TRAIL, but peripheral blood NK cells do not. Freshly isolated LMNC and PBMC fractions obtained from healthy donors and corresponding recipients cultivated with of without IL-2 were stained with CD3 and CD56 monoclonal antibodies (MAb) together with TRAIL MAb. (a) Representative histograms show the log fluorescence intensities obtained upon staining for TRAIL after gating on the CD3−CD56+ NK cells subsets of healthy donors. Dotted lines represent negative control staining with isotype-matched MAbs. The numbers indicate the percentages of cells in each group that were positive for TRAIL expression. (b) The numbers indicate the mean fluorescence intensity (MFI) of cells in each group that stained positively for TRAIL on freshly isolated NK cells cultivated with/without IL-2 (LMNC; open column, PBMC; closed column). The data are presented as means ± SEM. Statistical analyses were performed using ANOVA (*p < 0.05)
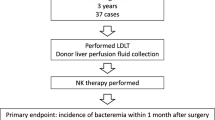
4 Clinical-Scale Isolation of Liver NK Cells from Donor Liver Graft
In order to apply this NK cell immunotherapy to cases of deceased donor liver transplantation, we demonstrated for the first time the phenotypical and functional properties of liver NK cells that were extracted from a deceased donor liver graft perfusate under current good manufacturing practice conditions (cGMP) [35]. First, a large number of NK and NKT cells were verified among liver mononuclear cells, with both subsets possessing characteristics different from those of peripheral blood mononuclear cells. Second, in vitro stimulation with IL-2 induced liver NK cells to strongly upregulate activation markers, cytotoxicity, and cytokine production while maintaining the expression of inhibitory receptors. These results were compatible with those for a living donor liver graft perfusate [10]. Finally, we confirmed that the final product met the lot release criteria and contained a low T-cell number, thereby reducing the possibility of graft versus host disease (GVHD) in a recipient.
4.1 Protocol of NK Isolation
At the time of donor operation, the graft liver was placed in a bag and perfused through the portal vein with 2 L of University of Wisconsin cold storage solution (UW solution) and crystalloids. This perfusate was collected from the hepatic vein and retrieved in our cGMP cell processing facility. Since the UW solution has a high viscosity [36], the perfusate was centrifuged at 2800 × g for 30 min at 4 °C to ensure adequate centrifugation. The cell pellet was then subjected to a Ficoll-Hypaque density gradient centrifugation to separate mononuclear cells. Liver mononuclear cells were cultured with human recombinant IL-2 in complete medium at 37 °C in atmosphere supplemented with 5 % CO2 for 3–5 days. Anti-CD3 monoclonal antibody was added to the culture medium in order to deplete the CD3+ fraction 1 day prior to cell harvesting. On the day of infusion, the cells were washed twice with 0.9 % sodium chloride and resuspended in 5 % human serum albumin for injection. Testing for lot release included cell counts, viability assessment, Gram stain, and endotoxin analysis (Fig. 4.5).
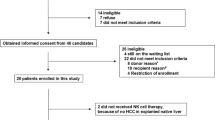
5 Clinical Trials for Living and Deceased Donor Liver Transplantation
On the basis of these results, we started a clinical trial of adjuvant immunotherapy with activated donor liver NK cells for preventing the recurrence of HCC after living donor liver transplantation in 2006. The lymphocytes in the peripheral blood of liver transplant recipients who received immunotherapy in the early postoperative period showed significantly enhanced cytotoxicity against an HCC cell line (HepG2), compared with those in the peripheral blood of liver transplant recipients who did not receive the therapy in the same period (Fig. 4.6a). Correspondingly, the proportions of TRAIL+ NK cells in the peripheral blood of liver transplant recipient who received immunotherapy also significantly increased (Fig. 4.6b). Although the long-term benefits of this approach with regard to HCC recurrence after liver transplantation remain to be elucidated, there were no severe adverse events including GVHD, thus far. With the collaboration of Professors A. Tzakis and S. Nishida at the University of Miami, FL, we successfully performed a phase I study of adoptive immunotherapy using liver NK cells for deceased donor liver transplant recipients with HCC (ClinicalTrials.gov identifier: NCT01147380) beginning in 2009. Both clinical studies are under evaluation and these results will be published soon.
Adoptive immunotherapy with activated donor liver NK cells promoted the cytotoxic activity and TRAIL expression of NK cells in liver transplant recipients. (a) The NK-mediated cytotoxic activities of the indicated effectors against their target cells were analyzed by 51Cr-release assay. The dot plot represents the NK cytotoxic activities of freshly isolated peripheral blood lymphocytes obtained from recipients who received immunotherapy (+) and did not receive immunotherapy (−) against HepG2 target cells (effector/target ratio, 40:1) 3 and 7 days after liver transplantation. NK cytotoxic activities are presented as a proportion (percentage) of the preoperative cytotoxicity in each patient. Horizontal lines indicate the mean.*p < 0.05 for day 7 compared to day 3. (b) The frequency of TRAIL + NK cells increased remarkably in the peripheral blood of liver transplant recipients who received immunotherapy. *p = 0.013 for the immunotherapy group compared to the untreated group on postoperative day 7. (c) Correlation between TRAIL+NK cell ratio and NK cytolytic activity after liver transplantation (Spearman rank-order correlation coefficient r = 0.54, p = 0.01)
References
Horn M, Phebus C, Blatt J. Cancer chemotherapy after solid organ transplantation. Cancer. 1990;66(7):1468–71.
Saab S, Yeganeh M, Nguyen K, Durazo F, Han S, Yersiz H, et al. Recurrence of hepatocellular carcinoma and hepatitis B reinfection in hepatitis B surface antigen-positive patients after liver transplantation. Liver Transpl. 2009;15(11):1525–34.
Vivarelli M, Cucchetti A, La Barba G, Ravaioli M, Del Gaudio M, Lauro A, et al. Liver transplantation for hepatocellular carcinoma under calcineurin inhibitors: reassessment of risk factors for tumor recurrence. Ann Surg. 2008;248(5):857–62. doi:10.1097/SLA.0b013e3181896278.
Yokoyama I, Carr B, Saitsu H, Iwatsuki S, Starzl TE. Accelerated growth rates of recurrent hepatocellular carcinoma after liver transplantation. Cancer. 1991;68(10):2095–100.
Soderdahl G, Backman L, Isoniemi H, Cahlin C, Hockerstedt K, Broome U, et al. A prospective, randomized, multi-centre trial of systemic adjuvant chemotherapy versus no additional treatment in liver transplantation for hepatocellular carcinoma. Transpl Int. 2006;19(4):288–94. doi:10.1111/j.1432-2277.2006.00279.x.
Zimmerman MA, Ghobrial RM, Tong MJ, Hiatt JR, Cameron AM, Hong J, et al. Recurrence of hepatocellular carcinoma following liver transplantation: a review of preoperative and postoperative prognostic indicators. Arch Surg. 2008;143(2):182–8. discussion 8.
Trinchieri G. Biology of natural killer cells. Adv Immunol. 1989;47:187–376.
Balch CM, Tilden AB, Dougherty PA, Cloud GA, Abo T. Heterogeneity of natural killer lymphocyte abnormalities in colon cancer patients. Surgery. 1984;95(1):63–70.
Cai L, Zhang Z, Zhou L, Wang H, Fu J, Zhang S, et al. Functional impairment in circulating and intrahepatic NK cells and relative mechanism in hepatocellular carcinoma patients. Clin Immunol. 2008;129(3):428–37. doi:10.1016/j.clim.2008.08.012.
Ishiyama K, Ohdan H, Ohira M, Mitsuta H, Arihiro K, Asahara T. Difference in cytotoxicity against hepatocellular carcinoma between liver and periphery natural killer cells in humans. Hepatology. 2006;43(2):362–72. doi:10.1002/hep.21035.
Harada N, Shimada M, Okano S, Suehiro T, Soejima Y, Tomita Y, et al. IL-12 gene therapy is an effective therapeutic strategy for hepatocellular carcinoma in immunosuppressed mice. J Immunol. 2004;173(11):6635–44.
Hirata M, Kita Y, Saito S, Nishimura M, Ito M, Mizuta K, et al. Increase in natural killer cell activity following living-related liver transplantation. Transpl Int. 1998;11 Suppl 1:S185–8.
Miller JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun GH, Fautsch SK, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood. 2005;105(8):3051–7.
Ohira M, Ohdan H, Mitsuta H, Ishiyama K, Tanaka Y, Igarashi Y, et al. Adoptive transfer of TRAIL-expressing natural killer cells prevents recurrence of hepatocellular carcinoma after partial hepatectomy. Transplantation. 2006;82(12):1712–9. doi:10.1097/01.tp.0000250935.41034.2d.
Smyth MJ, Cretney E, Kelly JM, Westwood JA, Street SE, Yagita H, et al. Activation of NK cell cytotoxicity. Mol Immunol. 2005;42(4):501–10. doi:10.1016/j.molimm.2004.07.034.
Trapani JA, Smyth MJ. Functional significance of the perforin/granzyme cell death pathway. Nat Rev Immunol. 2002;2(10):735–47. doi:10.1038/nri911.
Screpanti V, Wallin RP, Grandien A, Ljunggren HG. Impact of FASL-induced apoptosis in the elimination of tumor cells by NK cells. Mol Immunol. 2005;42(4):495–9.
Hayakawa Y, Takeda K, Yagita H, Smyth MJ, Van Kaer L, Okumura K, et al. IFN-gamma-mediated inhibition of tumor angiogenesis by natural killer T-cell ligand, alpha-galactosylceramide. Blood. 2002;100(5):1728–33.
Rosenberg SA, Lotze MT, Muul LM, Leitman S, Chang AE, Ettinghausen SE, et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med. 1985;313(23):1485–92. doi:10.1056/NEJM198512053132327.
Law TM, Motzer RJ, Mazumdar M, Sell KW, Walther PJ, O’Connell M, et al. Phase III randomized trial of interleukin-2 with or without lymphokine-activated killer cells in the treatment of patients with advanced renal cell carcinoma. Cancer. 1995;76(5):824–32.
Burns LJ, Weisdorf DJ, DeFor TE, Vesole DH, Repka TL, Blazar BR, et al. IL-2-based immunotherapy after autologous transplantation for lymphoma and breast cancer induces immune activation and cytokine release: a phase I/II trial. Bone Marrow Transplant. 2003;32(2):177–86.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295(5562):2097–100.
Feng YX, Wang T, Deng YZ, Yang P, Li JJ, Guan DX, et al. Sorafenib suppresses postsurgical recurrence and metastasis of hepatocellular carcinoma in an orthotopic mouse model. Hepatology. 2011;53(2):483–92. doi:10.1002/hep.24075.
Xie F, Zhang X, Li H, Zheng T, Xu F, Shen R, et al. Adoptive immunotherapy in postoperative hepatocellular carcinoma: a systemic review. PLoS One. 2012;7(8), e42879. doi:10.1371/journal.pone.0042879.
Shi FD, Ljunggren HG, La Cava A, Van Kaer L. Organ-specific features of natural killer cells. Nat Rev Immunol. 2011;11(10):658–71. doi:10.1038/nri3065.
Ochi M, Ohdan H, Mitsuta H, Onoe T, Tokita D, Hara H, et al. Liver NK cells expressing TRAIL are toxic against self hepatocytes in mice. Hepatology. 2004;39(5):1321–31. doi:10.1002/hep.20204.
Takeda K, Hayakawa Y, Smyth MJ, Kayagaki N, Yamaguchi N, Kakuta S, et al. Involvement of tumor necrosis factor-related apoptosis-inducing ligand in surveillance of tumor metastasis by liver natural killer cells. Nat Med. 2001;7(1):94–100.
Park SK, Brody JI, Wallace HA, Blakemore WS. Immunosuppressive effect of surgery. Lancet. 1971;1(7689):53–5.
Morimoto H, Nio Y, Imai S, Shiraishi T, Tsubono M, Tseng CC, et al. Hepatectomy accelerates the growth of transplanted liver tumor in mice. Cancer Detect Prev. 1992;16(2):137–47.
Minagawa M, Oya H, Yamamoto S, Shimizu T, Bannai M, Kawamura H, et al. Intensive expansion of natural killer T cells in the early phase of hepatocyte regeneration after partial hepatectomy in mice and its association with sympathetic nerve activation. Hepatology. 2000;31(4):907–15.
Walczak H, Miller RE, Ariail K, Gliniak B, Griffith TS, Kubin M, et al. Tumoricidal activity of tumor necrosis factor-related apoptosis-inducing ligand in vivo. Nat Med. 1999;5(2):157–63.
Wiley SR, Schooley K, Smolak PJ, Din WS, Huang CP, Nicholl JK, et al. Identification and characterization of a new member of the TNF family that induces apoptosis. Immunity. 1995;3(6):673–82.
Pan G, O’Rourke K, Chinnaiyan AM, Gentz R, Ebner R, Ni J, et al. The receptor for the cytotoxic ligand TRAIL. Science. 1997;276(5309):111–3.
Sheridan JP, Marsters SA, Pitti RM, Gurney A, Skubatch M, Baldwin D, et al. Control of TRAIL-induced apoptosis by a family of signaling and decoy receptors. Science. 1997;277(5327):818–21.
Ohira M, Nishida S, Tryphonopoulos P, Tekin A, Selvaggi G, Moon J, et al. Clinical-scale isolation of interleukin-2-stimulated liver natural killer cells for treatment of liver transplantation with hepatocellular carcinoma. Cell Transplant. 2012;21(7):1397–406. doi:10.3727/096368911X627589.
Wilson CH, Stansby G, Haswell M, Cunningham AC, Talbot D. Evaluation of eight preservation solutions for endothelial in situ preservation. Transplantation. 2004;78(7):1008–13. doi:00007890-200410150-00009 [pii].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Ohira, M., Nishida, S., Tzakis, A.G., Ohdan, H. (2016). Novel Immunotherapy Using Liver-Derived Natural Killer Cells for Preventing Hepatocellular Carcinoma Recurrence in Liver Transplantation. In: Terai, S., Suda, T. (eds) Gene Therapy and Cell Therapy Through the Liver. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55666-4_4
Download citation
DOI: https://doi.org/10.1007/978-4-431-55666-4_4
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55665-7
Online ISBN: 978-4-431-55666-4
eBook Packages: MedicineMedicine (R0)