Abstract
Liver transplantation (LT) is a viable treatment option for cirrhosis patients with hepatocellular carcinoma (HCC). However, recurrence is the rate-limiting factor of long-term survival. To prevent this, we conducted the phase I study of the adoptive transfer of deceased donor liver-derived natural killer (NK) cells. Liver NK cells were extracted from donor liver graft perfusate and were stimulated in vitro with IL-2. The patient received an intravenous infusion of NK cells 3–5 days after LT. Eighteen LT recipients were treated. There were no severe cell infusion-related adverse events or acute rejection episodes. One patient withdrew from the study because the pathological observation revealed sarcoma instead of HCC. All patients who received this immunotherapy completed the follow-up for at least 2 years without evidence of HCC recurrence (median follow-up, 96 months [range, 17–121 months]). Considering that 9 (52.9%) of the 17 patients pathologically exceeded the Milan criteria, liver NK cell infusion is likely to be useful for preventing HCC recurrence after LT. This is the first-in-human immunotherapy study using deceased donor liver-derived NK cells to prevent HCC recurrence after LT. This treatment was well tolerated and resulted in no HCC recurrence after LT.
Clinical trial registration www.clinicaltrials.gov; NCT01147380; registration date: June 17, 2010.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide and is an indication for liver transplantation (LT). The number of LTs in HCC patients has gradually increased since the Milan criteria have been established for organ allocation in the United States [1, 2]. Among the immunosuppressed conditions, the rate of recurrence of HCC after LT is still 10–20% [3, 4]. However, effective means to prevent HCC recurrence after LT remain unestablished [1, 5,6,7,8,9]. There is an urgent need to develop effective and safe therapeutic interventions that can be used to prevent HCC recurrence, despite the immunosuppressive environment.
Natural killer (NK) cells are a subset of lymphocytes defined by the expression of CD56 and the negative expression of the T cell receptor (CD3), comprising 10–15% of all circulating lymphocytes. NK cells can kill target cells without prior sensitization based on inhibitory receptor recognition (missing-self hypothesis) and activating receptor recognition [10, 11]. It has been demonstrated that the numbers and function of NK cells are attenuated in HCC/cirrhosis patients [12,13,14], implicating that the deficient function of NK cells might be responsible for the failure of anti-tumor immune responses after LT in HCC patients. Since the immunosuppressive regimen that is currently used after organ transplantation reduces the adaptive immune components but effectively maintains the innate components of cellular immunity [15,16,17], augmentation of the NK cell response may be a promising immunotherapeutic approach [18, 19]. In an autologous setting, cytokine-induced killer (CIK) cell therapies were well tolerated and could improve the outcomes of patients with HCC after curative treatment [20, 21]. A recent phase-3 trial study revealed that adjuvant immunotherapy using autologous CIK cells increased recurrence-free survival and overall survival after curative HCC treatment [22]. However, there are no reports on the use of allogeneic NK cells for HCC treatment. Previous clinical studies have demonstrated the safety and efficacy of allogeneic NK cell adoptive transfer therapies as a means for the treatment of hematologic malignancies and, to a lesser extent, of solid tumors [17, 23, 24]. In a Phase I/II study of injecting allogeneic NK cells into patients suffering from renal cell carcinoma, the distribution of the inoculation to the whole body, with a preference for the liver, spleen, and bone marrow and their extended survival were observed [24]. In allogeneic NK cell therapy, the mismatch between the killer cell immunoglobulin-like receptor (KIR) and human leukocyte antigen (HLA) can be harnessed to increase anti-tumor activity. We have previously demonstrated that the multiplicity of the functional compound KIR-HLA genotype in patients with HCC who underwent primary curative hepatectomy is associated with the HCC recurrence rate, indicating that the KIR-HLA axis might be involved in NK-mediated killing of HCC [25]. Hence, with less donor/recipient HLA-matching, DDLT might be advantageous over LDLT in terms of the anti-tumor effects of the immunotherapy.
We have previously reported that liver mononuclear cells (LMNCs) derived from donor liver perfusate contain a large number of NK cells that have vigorous cytotoxicity against hepatoma cells with the expression of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL), a critical molecule for NK cell-mediated anti-tumor cell killing, after IL-2 stimulation [26, 27]. As a preliminary proof of concept study, we have undertaken a pilot clinical trial of adoptive immunotherapy approach, using lymphocytes extracted from liver allograft perfusate, which includes an abundance of NK cells that mount an anti-HCC response, in living donor LT (LDLT) recipients with HCC in Hiroshima University in Japan [18]. In this trial, twenty-four LT recipients safely received NK cell infusion with acceptable outcomes, that is, with the absence of any severe adverse events, including graft-versus-host disease (Table S1) and a recurrence-free satisfactory overall survival (Figure S1). Here, we applied NK cell immunotherapy to deceased donor LT (DDLT) patients with HCC, based on the results of another preliminary study showing that the quality and quantity of liver NK cells derived from cadaveric donors were similar to those of living donors [27]. This study aimed to determine the feasibility of adoptive immunotherapy using activated liver NK cells, to assess the toxicity of this regimen and evaluate its ability to exert an anti-tumor effect in recipients of cadaveric liver transplant.
Methods
Patient eligibility
Primary LT recipients with HCC who were 18 years of age or older were eligible for this study. The absence of serious cardiovascular disease and a satisfactory renal function, as indicated by receiving hemodialysis more than twice a week as well as bone marrow competence (WBC > 1000/mm3, hematocrit > 20%, platelets > 20,000/mm3) were prerequisites for patient enrollment. Exclusion criteria included living donor LT, multiple organ transplant, prior solid organ or bone marrow transplant, fulminant hepatic failure, ABO-incompatible transplant, and intercurrent chemotherapy at the time of enrollment. Donors were negative for serology (HCV, HBsAg, HBcAb, HTLV-1, HTLV-3, and EBV IgM) and had satisfactory liver functions, as indicated by a value of total bilirubin < 3.0 mg/dL and prothrombin time < 35 s. In all cases, the pathologist tentatively confirmed the tumors in the liver before cell administration. If there were no tumors, the final product was not administered.
Study design
Twenty patients were enrolled in this study. Eligible patients received standard LT and were infused with enriched donor liver NK cells 3–5 days after LT. The enrolled patients were divided into two groups according to the following cell doses: the low-dose group, 10–100 × 106 cells; and the high-dose group, 100–1000 × 106 cells/body, according to the results of our preliminary study [27]. Patients and donors were matched by the United Network for Organ Sharing (UNOS) liver allocation system, based on the Model for End-Stage Liver Disease (MELD). The primary aim of this study was to evaluate the safety of intravenous administration of deceased donor liver NK cells after LT. The possible clinical efficacy of this immunotherapy has also been evaluated as a secondary endpoint. Immunosuppression consisted of a 3- to 6-month course of tapering corticosteroids and a calcineurin inhibitor, usually tacrolimus, for maintenance with or without mycophenolate mofetil.
Cell preparation
The method of cell preparation was previously described [27]. Briefly, after organ recovery, the liver was perfused through the portal vein with 2 L of University of Wisconsin solution on the back table. LMNCs were collected by Ficoll-Hypaque density-gradient centrifugation and were cultured with 1000 U/mL of human recombinant interleukin (IL)-2 (Proleukin, Novartis, Emeryville, CA, USA) in complete medium for 3–5 days to prime NK cells with enhanced anti-tumor properties. To prevent graft-versus-host disease (GVHD), that is, to inactivate CD3+ alloreactive T cells, an anti-CD3 monoclonal antibody (mAb) (Orthoclone OKT3, Ortho Biotech, Raritan, NJ, or anti-CD3 antibody), was added to the culture medium (100 µg/mL) 1 day before the cell harvest. A minimum of 1 × 107 cells with a cell viability of > 80% was required to release the NK cell product for infusion. Following quality control verification, including the Gram Stain, culture, endotoxin, and mycoplasma testing, all unfractionated cells, which were processed as described above and defined as the final NK cell products, were infused into the patients via intravenous administration on the day of cell harvesting.
Flow cytometry analysis
All flow cytometry (FCM) analyses were performed on a BD LSR-II flow cytometer (BD Biosciences, San Jose, CA). To detect the surface phenotype, leukocytes were stained with the following monoclonal antibodies: against CD3, TRAIL, NKG2D, CD69, CD226, and CD56. The data were analyzed using FlowJo software (Tree Star, Inc. Ashland, OR).
Cytotoxic assay
The cell cytotoxicity assay was performed using FCM as described previously [27]. Briefly, the target cells were labeled with 0.1 μM carboxyfluorescein diacetate succinimidyl ester (CFDA SE) Cell Tracer Kit (Invitrogen), and the effector cells were co-incubated at various effector/target ratios of target cells for 1 h at 37 °C in 5% CO2. The cytotoxic activity was calculated as a percentage using the following formula: % cytotoxicity = [(% experimental DAPI+ dead targets)-(% spontaneous DAPI+ dead targets)]/[(100-(% spontaneous DAPI+ dead targets)] × 100. K562, a human chronic myelogenous leukemia cell line (ATCC #CCl-243), was cultured in Dulbecco’ s modified Eagle’ s medium (Invitrogen) supplemented with 10% heat-inactivated fetal calf serum (Mediatech, Inc., Manassas, VA, USA), 100 U/mL penicillin, and 100 µg/mL streptomycin (Invitrogen) (complete medium) at 37 °C and 5% CO2.
Statistical analysis
Survival curves were generated using the Kaplan–Meier method and were compared by log-rank tests between the groups. Differences between the results of comparative tests were considered significant if the P-values were less than 0.05. Analyses were performed using JMP statistical software (JMP Pro 15.2.1; SAS Institute Inc., Cary, NC, USA).
Results
Patient Characteristics
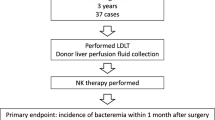
From June 2010 to April 2013, twenty LT patients with HCC were enrolled in this study. Two patients withdrew from the study and did not receive immunotherapy because the provisional pathological observation revealed no tumors in the resected native livers (Fig. 1). The demographics of patients who received immunotherapy and their clinical characteristics are shown in Table 1. One patient was removed from the study after immunotherapy because the final pathology report disclosed sarcoma, not HCC (patient 1). The patient’s median age was 60 years (range, 20–68 years). Twelve (70.6%) of the 17 patients had undergone pretreatment for HCC before transplantation. Eight patients received transarterial chemoembolization, and six patients underwent radiofrequency ablation. Four (23.5%) of the 17 patients had an AFP value of 200 ng/mL or higher. There were nine patients (52.9%) exceeded the Milan criteria based on the pathology of liver explants.
CONSORT flow diagram. ( +) High-risk donor (n = 3), no research consent (n = 2), import donor (n = 2). (#) HCC progression (n = 6), poor condition (n = 2), no HCC (n = 1), expired (n = 1). (*) One patient received NK cell therapy but withdrew from this study because he was diagnosed with sarcoma based on postoperative pathological findings
Characteristics of the NK cells
LMNCs derived from donor liver perfusate contained a median of 57% of NK cells (21–94%) before manipulation. Following ex vivo cultivation with IL-2 and anti-CD3 mAb to prime NK cells and inactivate T cells (processing), the median cell number of the final product was 200 × 106 (range, 18–626 × 106) cells. The viability was 93.3% (range, 86.2–98.1%). Figure 2 shows the representative phenotype of LMNCs before and after processing. The final product contained 64.8% (range, 25.2–98.4%) of CD3−CD56+NK cells, which expressed a high level of TRAIL (53.5%; range 3.1–84.5%). The TRAIL expression of CD56bright NK cells (72.8%; range 6.4–94.8%) was higher than that of CD56dim NK cells (44.4%; range 2.1–70.5%). Cell processing significantly decreased T cell contamination in the final product from 15.0% (range, 0.3–45.0%) to 0.4% (range, 0.0–2.3%), yielding a final T cell dose of 2.3 × 103 cells/kg. Other components of the final product included B cells, monocytes, and granulocytes, with the following percentages: 6.4% (range, 0.1–20.7%), 1.7% (range, 0.1–3.8%), and 5.2% (range, 0.2–12.7%), respectively. The functional assay revealed vigorous cytotoxicity of the final product as 38.0% (range, 10.3–70.0%) with an effector: target ratio of 10:1. All products tested below the accepted limit for endotoxins and Gram staining was negative on the day of infusion. Subsequent microbiological cultures of all infusions were negative (Table 2).
Immunological assessment of the administrated NK cells. (a) The representative phenotype of LMNCs that was obtained from deceased donor liver perfusate before the culture (left) and after the culture (right) was depicted. (b) Histograms show the logarithmic fluorescence intensities of TRAIL after gating of the CD3−CD56+ NK cells (left), CD3−CD56bright NK cells (middle), and CD3−CD56dim NK cells (right). The dotted lines indicate a negative control staining with isotype-matched mAbs. Abbreviations: NK cell, natural killer cell; NKT cell, natural killer T cell; LMNCs, liver mononuclear cells; TRAIL, tumor necrosis factor-related apoptosis-inducing ligand
Toxicity
There were no fatal adverse events including GVHD during the study trial. Within 3 months after cell infusion, there were some adverse events categorized as grade 3–4 in Common Terminology Criteria for Adverse Events (CTCAE) ver 4.0 (Table 3). There were 13 and 11 grade 3–4 adverse events in the high- and low-dose groups, respectively. No signs of acute rejection were observed in this trial. There were no significant differences between the dose-dependent groups. All events were related to LT rather than cell infusion in the decision of the Data Safety Monitoring Board.
Immunological effects
Laboratory tests were performed every week to monitor immune activation. NK cell number and NK cell activation markers in the peripheral blood of the recipient are shown in Fig. 3. NK cell proportion and NK cytotoxicity gradually increased after immunotherapy in both dose groups, but there were no statistically significant differences. The activation markers on the peripheral blood NK cells did not change significantly. Each group had no significant differences in all categories.
Immunological assessment of the recipient. (a) The dot shows the percentage of CD3−CD56+ NK cells isolated from the peripheral blood of the recipient. (b) Cytotoxicity of PBMCs against K562 with an effector:target cell ratio of 10:1 and (c) each molecule of NK cells in the peripheral blood of the recipient. The solid line indicates the high-dose group (n = 11) and the dotted line indicates the low-dose group (n = 5)
Clinical efficacy
All participants were eligible for survival analysis and completed a follow-up period of 2 years. At the time of the data cutoff, the median follow-up duration was 96 months (range, 17–121 months). Nine of 17 patients had to exceed the Milan criteria diagnosed based on pathological findings. Among the 17 patients, no patients experienced HCC recurrence, even though 4 patients died during follow-up. Regarding overall survival, the high-dose group had significantly better survival than the low-dose group (log-rank; p = 0.0064) (Fig. 4).
Discussion
Immunotherapy with donor liver-derived NK cells has been originally applied to LDLT at Hiroshima University, Japan since 2006 [18]. Although the long-term benefits of this approach for the control of HCC recurrence after LT remain to be elucidated, the successful administration of this trial raised a further challenge of expanding the liver-derived NK cell immunotherapy to DDLT recipients. With more ischemia and less controlled procedures, DDLT might in theory lead to more adverse outcomes in immunotherapy than LDLT. Despite such potential concerns, immunotherapy was well tolerated and induced significant objective responses in DDLT patients with HCC. The procedure itself was not associated with serious adverse events and there were no treatment-related deaths. No HCC recurrence was observed in this study, with a follow-up period of over 24 months. The outcomes of this study are especially favorable considering the study population, which included advanced HCC patients (52.9% of them exceeding the Milan criteria); the anticipated incidence of HCC recurrence in similar LT recipients is typically 10–20% within 24 months [3, 4].
The arguments stating that immunosuppression increases the risk of recurrence of malignancy, including HCC, has been accepted. Supporting this, regression of HCC has been described following the discontinuation of immunosuppressive therapy [28]. While immunosurveillance against cancer and microbes is exerted by orchestrating innate and acquired immunity, immunosuppressive drugs currently used after LT preferentially suppress acquired components such as T and B cells [15]. Hence, in the LT setting, innate immunity, including NK cells, plays a major role in prophylactic activity. Consistently, we have previously demonstrated that polymorphisms of genes encoding FcγRIIIa, which is expressed by NK cells and mediates natural antibody-directed activity in innate immunity, can be a predisposing factor for severe bacterial infections and to predict mortality after LT [29]. Despite the important role of NK cells, functional impairment and a decreased number of NK cells have been observed in patients with end-stage liver disease requiring LT [12,13,14]. In LT recipients with HCC, who might be in such an immunological predicament, the augmentation of functionally activated liver NK cells could be a promising approach.
Challenges associated with sourcing allogeneic NK cells have given rise to controversy over the contribution of NK cells to GVHD. LMNCs derived from donor liver perfusate contain contaminating T cells, whose activation with NK-stimulating cytokines has been known to lead to an increased release of proinflammatory cytokines and to trigger the onset of GVHD in vivo. To avoid such an unfavorable response, in this study, anti-CD3 mAb was used during in vitro cell processing to inactivate T cells. As a result, the final product contained 0.002 × 106 CD3+CD56−T cells/kg, a seemingly acceptable level by comparison with the previous clinical trials reporting that the alloreactive T cells were contaminated with 0.01–0.18 × 106 CD3+CD56−T cells/kg [17, 30,31,32]. Therefore, the risk of GVHD would be minimal in this immunotherapy. Regarding regulatory T (Treg) cells, stimulation with IL-2 activated CD4+ T cells in liver-derived lymphocytes, and it is possible that Treg cells were induced. However, to prevent GVHD, T cells were depleted by adding an anti-CD3 mAb prior to cell infusion, and thus, very few Treg cells were transferred to the patients (0.002 × 106 CD3+CD56− T cells/kg). Further research is needed for understanding the merits and demerits of transferring activated lymphocytes without depleting activated T cells including Treg cells.
Various protocols have been used to isolate and preferentially expand primary NK cells from peripheral blood mononuclear cells (PBMCs) because of their ease and convenience for collection [33, 34]. We have previously shown that liver NK cells are more abundant and mediate a higher cytotoxic activity against HCC peripheral blood (PB) NK cells [12,13,14]. NK cells are a heterogeneous population consisting of different subsets with unique phenotypic and functional features. Tissue-resident NK cells, which are distinct from conventional NK cells, are preferentially distributed throughout non-lymphoid tissues, such as the liver, uterus, salivary gland, and adipose tissues. As an organ with predominant innate immunity, the liver is enriched with NK cells, which are phenotypically distinct from PB NK cells [12,13,14]. One of the hallmarks of liver NK cells is the expression of TRAIL. TRAIL binds to at least four receptors. Two of these death-inducing receptors (TRAIL-R1/DR4 and TRAIL-R2/DR5) contain cytoplasmic death domains and signal apoptosis, whereas two other death-inhibitory receptors (TRAIL-R3/DcR1 and TRAIL-R4/DcR2) lack a functional death domain and do not mediate apoptosis, all having similar affinities, and the latter acts as a decoy [35, 36]. We have demonstrated that moderately/poorly differentiated HCCs express remarkable levels of TRAIL-DR4 and -DR5 but do not express TRAIL- DcR1 and -DcR2, indicating susceptibility to TRAIL-expressing NK cell-mediated cell killing [12,13,14]. TRAIL expression was also clearly confirmed in the activated NK cells obtained from deceased donor liver perfusates in this study.
In order to investigate whether the frequency and type of adverse events were affected by the dosage of transferred immune cells, the subjects were divided into two groups: high-dose and low-dose groups. There was no difference in either the incidence or type of adverse events between the two groups. Surprisingly, with respect to the survival rates, the high-dose group showed significantly better survival than the low-dose group. Of note, the survival curves of the two groups dissociated more than one year after LT. Considering the lifespan of the transferred immune cells in vivo, it is possible that the difference in the survival rates of the two groups may be due to the difference in the dose of transferred cells. This said, in the study of LDLT (Hiroshima University), in which donor-derived NK cell chimerism in the peripheral blood was followed by flow cytometry using donor HLA as a marker, the period of detection was restricted to up to one month after LT (data not shown). Importantly the cause of death in the low-dose group was either infectious diseases or the recurrence of diseases other than HCC. It is possible that the administered NK cells might have stimulated liver immunity and maintained it for a long time [37]. As a result, patients in the high-dose group might have maintained their biological defenses and acquired resistance to infection. Additionally, the number of NK cells collected at the time of organ procurement may reflect the graft function. Since all of the collected graft-derived immune cells were cultured and administered, the patients in the high-dose group were transplanted with liver grafts with a higher volume of immune cells. Hence, the survival rate of patients transplanted with better-functioning liver grafts might have been better. In any case, future studies should be designed to determine the appropriate dose of immune cells for immunotherapy.
In conclusion, we can feasibly isolate, activate the liver NK cells from a deceased donor liver graft perfusate, and safely administer them to HCC recipients. This immunotherapy does not increase the risk of GVHD or graft rejection. This immunotherapy could be a potential therapeutic tool for preventing the recurrence of HCC after LT. Larger controlled studies are required in future.
Abbreviations
- CIK:
-
Cytokine-induced killer
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- DDLT:
-
Deceased donor liver transplantation
- FCM:
-
Flow cytometry
- GVHD:
-
Graft-versus-host disease
- HCC:
-
Hepatocellular carcinoma
- HLA:
-
Human leukocyte antigen
- KIR:
-
Killer cell immunoglobulin-like receptor
- LDLT:
-
Living donor liver transplantation
- LMNCs:
-
Liver mononuclear cells
- LT:
-
Liver transplantation
- MELD:
-
The Model for End-Stage Liver Disease
- NK:
-
Natural killer
- PBMCs:
-
Peripheral blood mononuclear cells
- TRAIL:
-
Tumor necrosis factor-related apoptosis-inducing ligand
- UNOS:
-
The United Network for Organ Sharing
References
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F et al (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334(11):693–699. https://doi.org/10.1056/NEJM199603143341104
Ioannou GN, Perkins JD, Carithers RL Jr (2008) Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology 134(5):1342–1351. https://doi.org/10.1053/j.gastro.2008.02.013
Saab S, Yeganeh M, Nguyen K, Durazo F, Han S, Yersiz H et al (2009) Recurrence of hepatocellular carcinoma and hepatitis B reinfection in hepatitis B surface antigen-positive patients after liver transplantation. Liver Transpl 15(11):1525–1534. https://doi.org/10.1002/lt.21882
Levi DM, Tzakis AG, Martin P, Nishida S, Island E, Moon J et al (2010) Liver transplantation for hepatocellular carcinoma in the model for end-stage liver disease era. J Am Coll Surg 210(5):727–734. https://doi.org/10.1016/j.jamcollsurg.2010.01.007
Horn M, Phebus C, Blatt J (1990) Cancer chemotherapy after solid organ transplantation. Cancer 66(7):1468–1471. https://doi.org/10.1002/1097-0142(19901001)66:7%3c1468::aid-cncr2820660705%3e3.0.co;2-b
Vivarelli M, Cucchetti A, La Barba G, Ravaioli M, Del Gaudio M, Lauro A et al (2008) Liver transplantation for hepatocellular carcinoma under calcineurin inhibitors: reassessment of risk factors for tumor recurrence. Ann Surg 248(5):857–862. https://doi.org/10.1097/SLA.0b013e3181896278
Yokoyama I, Carr B, Saitsu H, Iwatsuki S, Starzl TE (1991) Accelerated growth rates of recurrent hepatocellular carcinoma after liver transplantation. Cancer 68(10):2095–2100. https://doi.org/10.1002/1097-0142(19911115)68:10%3c2095::aid-cncr2820681002%3e3.0.co;2-y
Soderdahl G, Backman L, Isoniemi H, Cahlin C, Hockerstedt K, Broome U et al (2006) A prospective, randomized, multi-centre trial of systemic adjuvant chemotherapy versus no additional treatment in liver transplantation for hepatocellular carcinoma. Transpl Int 19(4):288–294. https://doi.org/10.1111/j.1432-2277.2006.00279.x
Zimmerman, M. A., Ghobrial, R. M., Tong, M. J., Hiatt, J. R., Cameron, A. M., Hong, J., et al. (2008). Recurrence of hepatocellular carcinoma following liver transplantation: a review of preoperative and postoperative prognostic indicators. Arch Surg 143(2):182–188; discussion 188. https://doi.org/10.1001/archsurg.2007.39
Ljunggren HG, Karre K (1990) In search of the “missing self”: MHC molecules and NK cell recognition. Immunol Today 11(7):237–244. https://doi.org/10.1016/0167-5699(90)90097-s
Karre K (2002) NK cells, MHC class I molecules and the missing self. Scand J Immunol 55(3):221–228. https://doi.org/10.1046/j.1365-3083.2002.01053.x
Balch CM, Tilden AB, Dougherty PA, Cloud GA, Abo T (1984) Heterogeneity of natural killer lymphocyte abnormalities in colon cancer patients. Surgery 95(1):63–70
Cai L, Zhang Z, Zhou L, Wang H, Fu J, Zhang S et al (2008) Functional impairment in circulating and intrahepatic NK cells and relative mechanism in hepatocellular carcinoma patients. Clin Immunol 129(3):428–437. https://doi.org/10.1016/j.clim.2008.08.012
Ishiyama K, Ohdan H, Ohira M, Mitsuta H, Arihiro K, Asahara T (2006) Difference in cytotoxicity against hepatocellular carcinoma between liver and periphery natural killer cells in humans. Hepatology 43(2):362–372. https://doi.org/10.1002/hep.21035
Harada N, Shimada M, Okano S, Suehiro T, Soejima Y, Tomita Y et al (2004) IL-12 gene therapy is an effective therapeutic strategy for hepatocellular carcinoma in immunosuppressed mice. J Immunol 173(11):6635–6644. https://doi.org/10.4049/jimmunol.173.11.6635
Hirata M, Kita Y, Saito S, Nishimura M, Ito M, Mizuta K et al (1998) Increase in natural killer cell activity following living-related liver transplantation. Transpl Int 11(Suppl 1):S185-188. https://doi.org/10.1007/s001470050457
Miller JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun GH, Fautsch SK et al (2005) Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood 105(8):3051–3057. https://doi.org/10.1182/blood-2004-07-2974
Ohira M, Ishiyama K, Tanaka Y, Doskali M, Igarashi Y, Tashiro H et al (2009) Adoptive immunotherapy with liver allograft-derived lymphocytes induces anti-HCV activity after liver transplantation in humans and humanized mice. J Clin Invest 119(11):3226–3235. https://doi.org/10.1172/JCI38374
Ohira M, Ohdan H, Mitsuta H, Ishiyama K, Tanaka Y, Igarashi Y et al (2006) Adoptive transfer of TRAIL-expressing natural killer cells prevents recurrence of hepatocellular carcinoma after partial hepatectomy. Transplantation 82(12):1712–1719. https://doi.org/10.1097/01.tp.0000250935.41034.2d
Xu L, Wang J, Kim Y, Shuang ZY, Zhang YJ, Lao XM et al (2016) A randomized controlled trial on patients with or without adjuvant autologous cytokine-induced killer cells after curative resection for hepatocellular carcinoma. Oncoimmunology 5(3):e1083671. https://doi.org/10.1080/2162402X.2015.1083671
Li X, Dai D, Song X, Liu J, Zhu L, Xu W (2014) A meta-analysis of cytokine-induced killer cells therapy in combination with minimally invasive treatment for hepatocellular carcinoma. Clin Res Hepatol Gastroenterol 38(5):583–591. https://doi.org/10.1016/j.clinre.2014.04.010
Lee JH, Lee JH, Lim YS, Yeon JE, Song TJ, Yu SJ et al (2015) Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology 148(7):1383-1391 e1386. https://doi.org/10.1053/j.gastro.2015.02.055
Rubnitz JE, Inaba H, Ribeiro RC, Pounds S, Rooney B, Bell T et al (2010) NKAML: a pilot study to determine the safety and feasibility of haploidentical natural killer cell transplantation in childhood acute myeloid leukemia. J Clin Oncol 28(6):955–959. https://doi.org/10.1200/JCO.2009.24.4590
Brand JM, Meller B, Von Hof K, Luhm J, Bahre M, Kirchner H et al (2004) Kinetics and organ distribution of allogeneic natural killer lymphocytes transfused into patients suffering from renal cell carcinoma. Stem Cells Dev 13(3):307–314. https://doi.org/10.1089/154732804323099235
Tanimine N, Tanaka Y, Kobayashi T, Tashiro H, Miki D, Imamura M et al (2014) Quantitative effect of natural killer-cell licensing on hepatocellular carcinoma recurrence after curative hepatectomy. Cancer Immunol Res 2(12):1142–1147. https://doi.org/10.1158/2326-6066.CIR-14-0091
Ohira M, Nishida S, Matsuura T, Muraoka I, Tryphonopoulos P, Fan J et al (2013) Comparative analysis of T-cell depletion method for clinical immunotherapy-anti-hepatitis c effects of natural killer cells via interferon-gamma production. Transplant Proc 45(5):2045–2050. https://doi.org/10.1016/j.transproceed.2013.01.046
Ohira M, Nishida S, Tryphonopoulos P, Tekin A, Selvaggi G, Moon J et al (2012) Clinical-scale isolation of interleukin-2-stimulated liver natural killer cells for treatment of liver transplantation with hepatocellular carcinoma. Cell Transplant 21(7):1397–1406. https://doi.org/10.3727/096368911X627589
Kumar A, Le DT (2016) Hepatocellular Carcinoma Regression After Cessation of Immunosuppressive Therapy. J Clin Oncol 34(10):e90-92. https://doi.org/10.1200/JCO.2013.51.4067
Shimizu S, Tanaka Y, Tazawa H, Verma S, Onoe T, Ishiyama K et al (2016) Fc-gamma receptor polymorphisms predispose patients to infectious complications after liver transplantation. Am J Transplant 16(2):625–633. https://doi.org/10.1111/ajt.13492
Frohn C, Doehn C, Durek C, Bohle A, Schlenke P, Jocham D et al (2000) Feasibility of the adoptive transfusion of allogenic human leukocyte antigen-matched natural killer cells in patients with renal cell carcinoma. J Immunother 23(4):499–504. https://doi.org/10.1097/00002371-200007000-00014
Schulze A, Schirutschke H, Oelschlagel U, Schmitz M, Fussel M, Wassmuth R et al (2008) Altered phenotype of natural killer cell subsets after haploidentical stem cell transplantation. Exp Hematol 36(4):378–389. https://doi.org/10.1016/j.exphem.2007.12.006
Passweg JR, Tichelli A, Meyer-Monard S, Heim D, Stern M, Kuhne T et al (2004) Purified donor NK-lymphocyte infusion to consolidate engraftment after haploidentical stem cell transplantation. Leukemia 18(11):1835–1838. https://doi.org/10.1038/sj.leu.2403524
Sakamoto N, Ishikawa T, Kokura S, Okayama T, Oka K, Ideno M et al (2015) Phase I clinical trial of autologous NK cell therapy using novel expansion method in patients with advanced digestive cancer. J Transl Med 13:277. https://doi.org/10.1186/s12967-015-0632-8
Doskali M, Tanaka Y, Ohira M, Ishiyama K, Tashiro H, Chayama K et al (2011) Possibility of adoptive immunotherapy with peripheral blood-derived CD3(-)CD56+ and CD3+CD56+ cells for inducing antihepatocellular carcinoma and antihepatitis C virus activity. J Immunother 34(2):129–138. https://doi.org/10.1097/CJI.0b013e3182048c4e
Pan G, O’Rourke K, Chinnaiyan AM, Gentz R, Ebner R, Ni J et al (1997) The receptor for the cytotoxic ligand TRAIL. Science 276(5309):111–113. https://doi.org/10.1126/science.276.5309.111
Sheridan JP, Marsters SA, Pitti RM, Gurney A, Skubatch M, Baldwin D et al (1997) Control of TRAIL-induced apoptosis by a family of signaling and decoy receptors. Science 277(5327):818–821. https://doi.org/10.1126/science.277.5327.818
Mikulak J, Bruni E, Oriolo F, Di Vito C, Mavilio D (2019) Hepatic Natural Killer Cells: Organ-Specific Sentinels of Liver Immune Homeostasis and Physiopathology. Front Immunol 10:946. https://doi.org/10.3389/fimmu.2019.00946
Acknowledgements
We would like to thank Oliver Umland for supporting flow cytometry analysis, Drs. Ryosuke Misawa, Taizo Hibi, Koichiro Uchida, Takehiko Dohi, Izumi Carpenter, Ji Fan, David Grant, Panagiotis Tryphonopoulos, Bonnie Blomberg, and Gary Kleiner for study support, and Editage (www.editage.com) for English language editing.
Funding
This study was supported by the research funding the Grant No. 1BG-08 from the Florida Department of Health and the Bankhead-Coley Cancer Research Program (Seigo Nishida), AMED under Grant Number JP21fk0210051 (Hideki Ohdan), and JSPS KAKENHI Grant Number JP20K09104 (Masahiro Ohira).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflict of interest to disclose as described by the Cancer Immunology, Immunotherapy.
Ethical approval
This phase I clinical trial was approved by the Institutional Review Board of the University of Miami Miller School of Medicine (IRB#20100344) and the Food and Drug Administration, and was registered with ClinicalTrials.gov (NCT01147380). The trial was designed and conducted according to the Declaration of Helsinki.
Informed consent
All patients provided written informed consent before enrolling in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ohira, M., Hotta, R., Tanaka, Y. et al. Pilot study to determine the safety and feasibility of deceased donor liver natural killer cell infusion to liver transplant recipients with hepatocellular carcinoma. Cancer Immunol Immunother 71, 589–599 (2022). https://doi.org/10.1007/s00262-021-03005-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-021-03005-3