Abstract
The prognosis is still poor in patients with hepatocellular carcinoma (HCC). One of the reasons for poor prognosis is a frequent tumor recurrence from diseased remnant liver even after potentially curative treatment following early detection of tumor during regular surveillance for HCC. Until now, however, the benefit of any form of adjuvant therapy remains unclear, and current international practice guidelines do not recommend any adjuvant therapy after curative treatment. Meanwhile, a recent randomized controlled trial showed that adjuvant cellular immunotherapy using cytokine-induced killer (CIK) cells is safe and prolongs both recurrence-free survival and overall survival in patients treated with curative treatment. CIK cells are a mixture of T lymphocytes, which are expanded ex vivo with cytokines, comprising CD3+/CD56+ cells, CD3−/CD56+ natural killer cells, and CD3+/CD56− cytotoxic T cells. Among them CD3+/CD56+ natural killer-like T cells have high proliferation rate and are the main effector cells killing tumor without major histocompatibility complex restriction. Several potential methods should be considered to improve the efficacy of CIK cell therapy. Now combination therapy with other cellular immunotherapy such as dendritic cell vaccines or immune checkpoint inhibitors is being investigated to enhance the efficacy of CIK cell immunotherapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
5.1 Need for Adjuvant Therapy in HCC
Most cases of hepatocellular carcinoma (HCC) occur in patients with well-known risk factors such as chronic hepatitis B virus (HBV) or hepatitis C virus (HCV), and nonalcoholic steatohepatitis, as well as other risk factors such as chronic alcoholism and liver cirrhosis. Thus, a regular surveillance program for populations with such risk factors may allow the diagnosis of HCC at early stage, which is candidate for potentially curative treatment. In fact, in Japan and Taiwan, >50% of HCC cases were diagnosed at either a very early or early stage owing to the implementation of a nationwide regular surveillance program [1]. However, the long-term prognosis of HCC is still poor even after curative treatment because of high risk of recurrence in the remnant liver.
In most other malignancies, adjuvant therapy is usually indicated for patients who undergo surgical treatment for locally advanced tumors, but not at a very early or early stage. For example, adjuvant systemic chemotherapy is indicated for gastric cancer of stages IB or IIA, colon cancer of stages II or III, and non-small cell lung cancer of stages II or IIIA but not for any cancer of stage I or IA since there is a low risk of tumor recurrence after curative treatment. However, in contrast, the National Cancer Institute recommends enrolling very early or early stage HCC patients for clinical trials of adjuvant therapy [2]. A very high risk of tumor recurrence, even after potentially curative treatment, is the basis of this exclusive recommendation for early HCC. Potentially curative treatment for early HCC and gastric cancer resulted in 5-year recurrence-free survival rates of <30% [3] and greater than 90%, respectively [4]. This difference may be linked to a significant difference in 5-year survival rates: 76% in early HCC and >90% in early gastric cancer.
The recurrence of HCC can be classified according to its timing. Early recurrence refers to recurrence within 2 years after tumor treatment and usually occurs by the metastasis of remnant tumor cells. Late recurrence means recurrence after 2 years and is thought to be a de novo recurrence from diseased liver [5]. Consequently, early recurrence is closely related to tumor factors including safety margin, vessel invasion, multiple tumor nodules, and serum levels of α-fetoprotein. In contrast, fibrosis and inflammation determined by a HBV and HCV load and histological inflammatory activity is associated with late recurrence.
Numerous efforts have been made to reduce recurrence in the form of the development of novel adjuvant therapies; however, the benefit of such remains uncertain. Till now, the only proven therapy that reduces the risk of HCC recurrence is antiviral treatment for HBV-related HCC patients. However, all adjuvant therapy which aimed to kill residual tumor cells failed to show efficacy. For example, polyprenoic acid (an acyclic retinoid) and sorafenib (a multikinase inhibitor) failed to decrease tumor recurrence in phase III trials. Therefore, current international guidelines do not recommend adjuvant therapy after curative treatment [6, 7]. In response, to overcome the lack of an effective adjuvant therapy, many scientists are trying to utilize adoptive immunotherapy.
5.2 Mechanisms of Immune Tolerability of HCC
Cellular immunity, in particular, T cell-mediated cytotoxicity, is the main armory of the human immune system deployed to combat cancers. Cytotoxic T cells may recognize tumor cells by interactions between the T cell receptor and an antigenic-peptide present on the type I major histocompatibility complex (MHC). Using perforin, T cells induce the formation of pores in the tumor cell membrane, via which granzyme enters to induce tumor cell apoptosis. Malignant cells develop multiple immune evasion mechanisms to avoid host immunity (Fig. 5.1). For example, they may hide themselves by reducing the production of tumor antigens and class I MHC molecules on their surface. Another immune evasion technique demonstrated by tumor cells is their disruption of T cell signaling, leading to the induction of T cell apoptosis in response to their expression of interleukin (IL)-10, transforming growth factor-β (TGF-β), and receptor-binding cancer antigen expressed on SiSo cells 1 (RCAS1). As well as T cells, tumor cells also act to suppress the immune response by the induction of myeloid-derived suppressor cells (MDSC) and regulatory T cells (Tregs). In addition, X-linked inhibitor of apoptosis (XIAP) and FADD-like IL-1β-converting enzyme-inhibitory protein (c-FLIP) interfere with apoptosis induction by T cells, surviving [8].
Mechanisms of immune evasion. Tumors may use several means of escaping the effects of the immune system: (a) cytokines and other molecules expressed by tumor cells may induce T-cell apoptosis or inhibit T-cell signaling; (b) tumor surface MHC molecules, which present tumor peptide epitopes to T-cell receptors (TCR), may not be expressed correctly; (c) the transporter that moves peptides to the endoplasmic reticulum for the formation of peptide-MHC complexes may malfunction; (d) the proteasome may change its methods of breaking down tumor protein into peptides for antigen presentation; and (e) tumor antigen expression becomes decreased or is absent. In the face of apoptosis induced by T cells, the expression of immunoprotective agents (the IAP family, FLIP, and PI9) is upregulated by tumor cells to thwart the activity of granzyme B and interactions by FAS-FAS ligands
CXCL12 chemokine (C-X-C motif) ligand 12, FLIP FLICE (FADD-like interleukin-1β–converting enzyme)–like inhibitory protein, IAP inhibitor of apoptosis protein, IL-10 interleukin-10, PI9 proteinase inhibitor 9, RCAS1 receptor-binding cancer antigen expressed on SiSo cells, TGF-β transforming growth factor-β (Reprinted by permission from Macmillan Publishers Ltd.: (NATURE REVIEWS CANCER) [8], copyright (2002))
In HCC, an environment suitable for immune evasion occurs due to: (i) the inherent tolerogenic nature of liver, (ii) hepatitis virus-related immunosuppression, and (iii) immune impairment induced by the tumor itself.
The liver is known as “an immune-privileged organ” that shows an inherent tolerogenicity in both healthy and diseased states. The liver continuously contacts and clears toxins delivered via the portal circulation. In other to avoid aberrant immunity, the liver has developed a redundant immune regulation mechanism. Hepatocytes prime naïve T cells without co-stimulation, resulting in defective effector function [9]. Immune tolerance in the liver is related to the presence of antigen presenting cells (APCs; i.e. liver sinusoidal endothelial, hepatic dendritic [DCs], and Kupffer cells). Kupffer cells (liver-resident macrophages) produce anti-inflammatory factors, including TGF-β, IL-10, and prostaglandin E2, and reduce antigen-specific CD8+ T cells [10, 11]. Myeloid DC precursors differentiate into IL-10–secreting DCs in the liver. When IL-10–secreting hepatic DCs prime naïve CD4+ T cells, Tregs are induced and the antigen recall process is impaired. More importantly, the expression of programmed death-ligand 1 (PD-L1) on liver sinusoidal endothelial cells and its interaction with programmed death (PD)-1 on T cells leads to the induction of antigen-specific T cell tolerance [10].
Immunosuppression is also enhanced by the most common underlying etiologies of HCC, chronic hepatitis B and C. In response to both virus-specific and unrelated antigens, T cell proliferation and the production of IL-2 are inhibited in a chronic HBV infection and Tregs accumulate in the liver. And with regard to infection with chronic hepatitis C, a reduced effector function of natural killer (NK) cells leads to the inhibition of the maturation of DC in response to various maturation signals. The expression of inhibitory immune checkpoints, such as PD-1, on T cells is enhanced, resulting in dysfunction of both HCV-specific and -nonspecific T cells.
HCC itself also displays a series of immune evasion mechanisms similar to other malignancies. In patients with HCC, the quantity and quality of myeloid DC and NK cells are decreased. Aberrantly activated monocytes in HCC express abundant PD-1 and impair anti-tumor T cell immunity. Immune suppressor cells, including MDSCs and Tregs, accumulate in HCC patients and correlate with tumor volume.
Such mechanisms of immune tolerability of HCC may need to be overcome to develop an effective immunotherapy option.
5.3 Adoptive Immunotherapies for HCC
Chronic inflammation is closely linked to the development and progression of HCC. For example, IL-6, and tumor necrosis factor-α (TNF-α) were found to promote the development of HCC as described by previous studies [12]. After the establishment of HCC cells, mutual interactions between tumor and immune cells, which can exist during chronic inflammation, may create favorable conditions for tumor cell survival [13]. Tumor-associated macrophages, Tregs, and MDSCs may act as immune suppressors and facilitate tumor immune evasion [14]. Tumor growth factor-β, IL-10, and IL-17 are important cytokines that also display an immune suppression function. In contrast to immune suppressors, the numbers and effectiveness of effector cells, such as NK, dendritic, and cytotoxic T cells, are downregulated within the tumor microenvironment [15]. Furthermore, mutations increase during the growth of tumors allowing these to avoid the immune system [16]. Antigen presenting cells and CD8+ T cell activities are also impaired, which leads to the attenuation of their cytotoxic effects dependent on MHC classes [17]. A proportion of HCC cells also express low levels of MHC molecules. Such major constraints of the cytotoxic immune response against HCC can be circumvented by likely beneficial approaches such as increasing and decreasing, respectively, the numbers of MHC-unrestricted direct cytotoxic effector and immune suppressor cells.
5.3.1 Tumor-Infiltrating Lymphocytes
An adoptive cell therapy uses tumor-infiltrating lymphocytes (TILs), a type of lymphocyte found in tumors that are often related to good clinical outcomes. For example, TILs numbers were significantly associated with the prognosis of HCC patients [18]. TIL immunotherapeutic agents can be generated by ex vivo expansion of TILs obtained from tumor fragments or digests with IL-2 containing medium for 14 days following activation with anti-CD3 antibody and irradiated allogenic PBMCs [19]. A prior clinical trial demonstrated a better clinical outcome was achieved by TIL compared to lymphokine-activated killer (LAK) cells in advanced melanoma patients. Unfortunately, TILs in HCC were only partially activated, proliferated only at a very low level, acted in an MHC-restricted manner, and consequently failed to effectively kill tumor cells [20].
5.3.2 Dendritic Cells
Studies into adoptive immunotherapy involving dendritic cells (DCs) pulsed by tumor lysate or antigens were also undertaken. In the cell-mediated immune response, DCs stimulate the proliferation and activation of antigen-specific cytotoxic T cells and, as such, demonstrating the potency of these professional antigen-presenting cells. To increase the body’s immunity against antigens, DCs display large amounts of MHC I and II molecules, costimulatory molecules and stimulatory cytokines (interferon-γ, IL-12) that contribute to an optimal costimulatory environment [21]. This clearly points to the use of autologous DCs as a tumor vaccine, which has been attempted in several cancers including melanoma, prostate cancer, and renal cell carcinoma. In patients with advanced HCC, DCs pulsed ex vivo with a HCC cell line lysate were used intravenously in a phase II trial and showed evidence of antitumor efficacy [22]. In HCC patients immunized with DCs pulsed with four alpha-fetoprotein (AFP) peptides as the immunogenic tumor-associated antigen (TAA) instead of tumor cell lysates in phase I/II trials, strong T-cell responses against AFP were noted. Despite this, treated patients did not show clinical responses [23]. Recently, we used an adjuvant autologous DC vaccine pulsed with cytoplasmic transduction peptide (CTP)-attached to three representative TAAs (i.e., alpha-fetoprotein [AFP], glypican-3 [GPC-3] and melanoma-associated antigen 1 [MAGE-1]) in a phase I/IIa study [24]. In that study, patients who did not experience tumor recurrence showed a higher lymphocyte proliferation rate and function than those who experienced recurrence. The patients treated with a DC vaccine showed significantly prolonged median time-to-progression compared to the historical control (36.6 vs 11.8 months). This has led to an ensuing completed phase IIb trial. In phase IIB trial, TAA-pulsed DC vaccine failed to prolong recurrence-free survival in overall patients, although DC vaccine marginally reduced the tumor recurrence in patients who underwent surgical resection [25]. Currently in progress is a multicenter phase III trial in HCC patients who previously underwent surgical resection.
5.3.3 Natural Killer Cells
NK cells kill cells that are dangerous to the host, such as cancer cells or virus-infected cells, and are regarded as key effector cells in cancer immune-surveillance and early viral immunity. Inhibitory receptors for MHC class I molecules (i.e., killer immunoglobulin-like receptors [KIR] and CD94-NKG2A heterodimers) are found on NK cells. The body’s immune tolerance for its own tissues occurs when NK cells interact with self MHC class I molecules [26]. In spite of this, the expression of MHC class I molecules on the surface of transformed malignant cells is often reduced resulting the disappearance of inhibitory signaling in NK cells. However, the surface of tumor cells can harbor stress-induced ligands that can be recognized by the activating receptors of NK cells, CD226, NKp44, NKp46, NKp30 and NKG2D. NK cells kill tumor cells mainly via granzyme/perforin activity and sometimes by death-receptor pathways. Additionally, the low-affinity activating receptor, CD16, binds the Fc portion of immunoglobulin G1 and mediates antibody-dependent cellular cytotoxicity.
As an adoptive immunotherapy, both autologous (from the patient) and allogeneic (from a healthy donor) NK cells obtained from peripheral blood have been utilized. Interestingly, allogeneic NK cell therapy led to a higher graft-versus-leukemia effect compared to autologous NK cell therapy for patients with acute myeloid leukemia. Since interaction between self-MHC class I molecules (especially HLA-C) with the KIRs of autologous NK cells can mediate inhibitory signals to NK cells, autologous NK cells may be a more potent source for NK cell immunotherapy. Obtaining sufficient numbers of NK cells to transfer, and maintaining their concentration after transfer have been major hurdles preventing significant clinical effects. Our group is now participating in trials to establish an ex vivo expanded and highly activated allogeneic NK cell immunotherapeutic agent from a universal healthy donor. In a phase I trial, allogeneic NK cells derived from unrelated random healthy donors were safely transferred to patients with malignant lymphoma or recurrent solid tumors [27]. A multicenter phase IIa clinical trial to evaluate the efficacy and safety of allogeneic NK cells in patients with intermediate-stage HCC after transarterial chemoembolization (TACE) has recently been launched in Korea (ClinicalTrial.gov ID: NCT02854839).
5.3.4 Lymphokine-Activated Killer Cells
LAK cells were initially described in the early 1980s. Five days of the culture of peripheral blood mononuclear cells (PBMCs) or splenocytes in the presence of IL-2 resulted in the generation of LAK cells, and the killing of tumor cells by effector cells was confirmed in vitro.21 In tumor-bearing mice and patients, LAK cells infused in conjunction with in vivo IL-2 co-administration showed anti-tumor activity. However, the induction of severe, IL-2–related toxicities including pulmonary capillary leak syndrome that were dependent on the IL-2 dose, limited the clinical use of LAK cells. When LAK cells were infused without IL-2 treatment, there was minimal toxicity to the recipient but no significant anti-tumor effect. In a murine immunotherapy protocol using LAK cells, splenocytes were used as the source of these cells. In a human clinical trial protocol, repeated leukapheresis was utilized to obtain LAK cells, but it was difficult to generate sufficient cells to transfer. That low proliferation rate of LAK cells was also another hurdle for the clinical use of LAK cells. An adequate anti-tumor response may be achieved from 2 × 1011 human LAK cells as calculated from a murine immunotherapy model, but is difficult to achieve. Other limitations include the ability of exogenous IL-2 to increase cell numbers and the cytolytic activity of LAK cells grown in vitro being quite low [28].
5.3.5 Cytokine-Induced Killer Cells
In the late 1980s, anti-CD3 stimulating antibodies was shown to be mitogenic for T lymphocytes. In addition, prolonged culturing also contributed to improving the properties of LAK cells. The cell numbers of human PBMCs increased 300- to 1000-fold when cultured for 2 weeks with both IL-2 and anti-CD3 antibody (OKT3). Under both in vitro and in vivo conditions, such anti-CD3/IL-2-stimulated human PBMCs were cytolytic for several types of tumor cells in an MHC-unrestricted manner. On closer examination, heterogeneous cells made up the cell population: CD3+CD56+ NK-like T cells, CD3−CD56+ NK cells, and CD3+CD56− T cells [29]. And because they were stimulated by anti-CD3 and IL-2, such cells were labeled cytokine-induced killer (CIK) cells. In a severe combined immunodeficiency (SCID) mouse model, strong anti-tumor activity was shown by CIK cells against various solid and hematopoietic tumors [30]. In clinical trials, CIK cells exhibited modest tumor killing efficacy against metastatic renal cell carcinoma and melanoma. CIK cells had a higher proliferation ability similar to CD3+ T cells and superior cytolytic activity over LAK cells. Moreover, CIK cells demonstrated potent in vivo cytotoxic activity without the need for IL-2 co-administration, which was the major problem in the clinical application of LAK immunotherapy. Considering the lack of a sufficient number of effector cells is one of the substantial hurdles preventing the clinical application of adoptive immunotherapies, a high proliferation rate without toxic IL-2 administration may be a clinically relevant property of CIK cells.
Among the heterogeneous CIK cell population, less than 2% are CD3−CD56+ NK cells and more than 90% are CD3+ cells, of which up to 35% are CD56+ cells. Similar to NK cells, the anti-tumor activity shown by CD3−CD56+ cells increases when HLA class I molecules on their target cells are blocked. Tumor cells are more susceptible to being killed by CD3+CD56+ NK-like T cells than CD3+CD56− cells for the following reasons: (i) the presence of a high proportion of CD8+ cells, and (ii) having a more terminally differentiated T cell nature, as well as (iii) a higher granzyme content. More importantly, while CD3+CD56− cells are MHC-restricted, the identification and killing of tumor cells by CD3+CD56+ cells is MHC unrestricted, making the latter pivotal effector CIK cells in tumor killing. Similar to NK cells, which do not require prior sensitization, tumor cells are detected by CD3+CD56+ cells by the recognition of the cognate ligands, MHC class I polypeptide-related sequences (MIC)-A and -B in an NKG2D-mediated manner (Fig. 5.2). MHC-T-cell receptor (TCR) interaction is not required for the activation of CIK cells by tumor cells. Instead, CIK cells express leukocyte function-associated antigen-1 (LFA-1) that is involved in the identification of tumor cells by these cells and which leads to their stable conjugation. This means that CIK cell immunotherapy is highly relevant for tumor cells expressing LFA-1 ligands including intracellular adhesion molecules (ICAM)-1, -2, and -3. Unsurprisingly, cytolytic activity induced by CIK cells was inhibited by anti-LFA-1 inhibitors.
For normal bone marrow cells in vitro, CIK cells show little or no cytotoxicity and thus are markedly tumor specific.
5.4 Adjuvant Cytokine-Induced Killer Cell Immunotherapy for HCC
Studies using in vitro and in vivo models showed that CIK cells decreased tumor growth [31]. PBMCs expanded ex vivo in medium lacking interferon-γ, but when containing anti-CD3 antibody and IL-2 for 14 days developed into CIK cells. In an in vitro study of CIK cells, using an effector-target ratio of 30:1 caused 33% of SNU-354 (HCC) cells to die. CIK cells also decreased tumor growth by 60% in a murine HCC model derived from the injection of SNU-354 cells in irradiated nude mice. Mice treated with 1 × 106 or 1 × 107 cells did not show a difference in growth inhibition, which was comparable to treatment with 2 mg/kg of adriamycin. The tumor mass showed a localization of CIK cells in vivo and were repeatedly administered without any apparent major adverse events.
In HCC patients who underwent surgical resection in a controlled randomized trial in Japan, the time to disease recurrence was significantly increased after adoptive immunotherapy, with the risk of tumor recurrence decreased by 40% and no difference in overall survival [32]. However, there was no significant difference in overall survival between 74 control patients and 76 treated with CIK cells.
In a Chinese study of HCC, 85 patients were randomized to an immunotherapy or control group after TACE or radiofrequency ablation (RFA) [33]. After CIK cells were injected via the hepatic artery, the peripheral blood showed significant increases in the proportions of CD3+, CD4+, and CD3+CD56+ cells. The CIK cell treated group showed a significantly lower HCC recurrence compared to the control group (8.9% vs. 30.0%) after 12 months. Only grade 1/2 adverse events were noted for CIK cell therapy.
In another Chinese randomized controlled trial, 127 HCC patients after radical resection were randomized to a CIK cell immunotherapy (three or six cycles) or control group [34]. Undergoing either three or six cycles of CIK cells showed significantly longer disease-free survival than the control group. However, disease-free survival was not different between the three- and six-cycle groups. Multivariate analysis was performed and revealed that treatment with CIK cells was an independent negative predictor of tumor recurrence after adjusting for variables such as vascular invasion, liver cirrhosis and tumor differentiation and size. No survival gain was achieved by CIK cell adjuvant therapy.
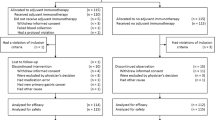
Encouraged by these preceding preclinical and clinical studies, the manufacturing process was refined and standardized, and individualized autologous CIK cell-based immunotherapeutic agents were developed. We then sought to examine whether treatment with such adjuvant CIK cells could prolong recurrence-free survival in stage I or II HCC patients after potentially curative treatment (i.e. percutaneous ethanol injection [PEI], RFA, or surgical resection) in a multicenter randomized controlled phase III trial [35]. Two hundred and thirty patients were randomized in equal numbers to immunotherapy or control groups. Patients in the immunotherapy group had 120 mL of blood collected before treatment. The CIK cell agent was manufactured at a central facility. Mononuclear cells were separated and cultured for 2–3 weeks with IL-2 and stimulating monoclonal antibody to CD3 at 37 °C. The CIK cell agent contained a total of 6.4 (±2.1) × 109 cells, including 1.8 (±1.0) × 109 CIK cells, in 200 mL of fluid. Patients in the immunotherapy group received CIK cell agent intravenously over 60 min and were then observed for at least 30 min. Patients received four treatments of CIK cell agent once a week, and thereafter four treatments every 2, 4 and 8 weeks for a total of 16 treatments. The primary endpoint was recurrence-free survival, with secondary endpoints of safety, and cancer-specific and overall survival. The median recurrence-free survival was 14.0 months longer in the immunotherapy group (44.0 months) than in the control group (30.0 months). The difference in recurrence-free survival between the two groups was statistically significant. The risk of death from tumors or its recurrence decreased by 37% with CIK immunotherapy (Fig. 5.3a). Interestingly, immunotherapy consistently decreased the risk of all types of tumor recurrence: intrahepatic local recurrence (within 2 cm from resection or ablation margin), intrahepatic distant recurrence (beyond 2 cm from margin), and extrahepatic recurrence. In multivariate analysis, CIK cell immunotherapy was a significant prognostic factor after adjustment for age, serum level of serum alpha-fetoprotein, and curative treatment modality. Subgroup analyses showed a beneficial effect on recurrence-free survival for adjuvant therapy compared with no adjuvant treatment, regardless of sex, age, the modality of prior curative treatment, stage of HCC, HCC size, underlying etiology of liver disease, the presence of cirrhosis, and antiviral treatment for HBV (Fig. 5.4). CIK cell immunotherapy also prolonged overall survival: immunotherapy reduced the risk of overall death by 79% (Fig. 5.3b). The immunotherapy group showed significantly longer cancer-specific survival and decreased the risk of HCC-related death by 81%. The immunotherapy group experienced more frequent adverse events but treatment groups did not show a difference in the frequency of grade 3 or 4 adverse events. Common adverse events such as headache (1%), fatigue (3%), chills (8%) and pyrexia (9%) did not contribute to delayed or discontinued CIK cell therapy.
Kaplan-Meier estimates of (a) recurrence-free survival and (b) overall survival (Reprinted by permission from Elsevier: (GASTROENTEROLOGY) [35], copyright (2015))
Recurrence-free survival in selected subsets. Squares (size proportional to the information quantity) indicate hazard ratio (HR) estimates for each subgroup. Horizontal lines represent 95% CIs determined using a Cox proportional hazards model. The line of no effect is represented by a solid vertical line at the HR of unity. Diamonds represent HRs with 95% CIs for all patients. A decrease in the risk of recurrence or death after immunotherapy are represented by HR values less than unity. The HCV subset includes patients co-infected with HBV and HCV. Patients whose serum HBV-DNA levels were ≥2000 IU/mL and who did or did not undergo antiviral treatment are represented by HBV DNA and antiviral agent groups 1 and 2, respectively. Patients whose serum HBV-DNA levels were <2000 IU/mL and who did or did not undergo antiviral treatment are represented by HBV DNA and antiviral agent groups 3 and 4, respectively
AFP α-fetoprotein, ALP alkaline phosphatase, ALT alanine aminotransferase, AST aspartate aminotransferase, ECOG Eastern Cooperative Oncology Group, HCV hepatitis C virus (Reprinted by permission from Elsevier: (GASTROENTEROLOGY) [35], copyright (2015))
The use of a CIK cell agent in this study was convincingly shown to improve cancer-specific, overall and recurrence-free survival. Although the magnitude of absolute gain was modest, the reduction in relative risk was significant: an approximately 30% reduction in tumor recurrence or death and 80% in both overall and cancer-related mortalities. In particular, CIK cell therapy showed a significant gain in overall survival as well as recurrence-free survival. The intensified schedule of CIK cell agent administration and favorable tumor characteristics in our study may account for the prolonged overall survival observed as compared to prior studies. CIK cells were infused more times (16 times) in our study than in preceding studies (3–10 times). Our study also included only patients with American Joint Committee on Cancer (AJCC) stage I or II hepatocellular carcinoma, whereas preceding studies included patients with a more advanced tumor stage (i.e. stage III or IV tumor, tumor with vascular invasion, or large HCC). Patients with a greater tumor burden in preceding studies may have had increased numbers of immune suppressor cells (e.g. MDSC, Tregs) that attenuated the effect of adjuvant immunotherapy [36, 37], and thus may have impeded any survival benefit.
5.5 Current Limitations of CIK Cell Immunotherapy
CIK cell immunotherapy has several limitations. The expansion rate of CIK cells varies among patients according to the degree of immune suppression. MDSCs and defective APCs can inhibit CIK cell expansion. The quality and quantity of T cells is poor in cancer patients. A lack of reliable serum or histological biomarkers for predicting outcomes of CIK immunotherapy is also a problem. Potential biomarkers include the CD4/CD8 ratio and the proportion of NK cells increase after infusion of CIK cells. Inhibitory immune checkpoints and immune suppressor cells may also be related to the prognosis of patients treated with CIK cells; all these factors that impact CIK cell therapy need to be studied further. In addition, among heterogeneous cells included in CIK cell preparations, most potent effector cells with a high level of NKG2D expression and interferon-γ production are prone to apoptosis, which could limit the prolonged efficacy of CIK cell treatment.
5.6 Future Perspectives
As previously mentioned, adjuvant immunotherapy with autologous CIK cells has been proven to significantly prolong both recurrence-free and overall survival. Several potential methods should be considered to improve the efficacy of CIK cell therapy. Firstly, a combination with different types of adoptive immunotherapy (e.g., combination with adoptive TAA-pulsed DC vaccine) should be considered. Since CIK cells also include a number of cytotoxic T cells that have MHC-restricted cytotoxicity and DCs can provide high levels of MHC I and tumor antigens, a synergistic effect of combination therapy would be expected. Secondly, combination therapy with immune checkpoint inhibitors, such as anti–PD-1/PD-L1 agents and anti–cytotoxic T-lymphocyte–associated protein 4 (CTLA4) agents, may be used to circumvent immune evasion by cancer cells and to stimulate antitumor activity. A recent in vitro study reported that blockade of immune checkpoints (including PD-1, KIR, lymphocyte activation gene-3 [LAG-3], and T cell immunoglobulin and mucin-domain-containing-3 [TIM-3]) enhance cytotoxicity of CIK cells against human myeloid leukemic blasts [38]. Thirdly, CIK cells may be stimulated by an increase in MIC-A and -B levels, which bind to NKG2D. The expression of MIC-A and -B can be increased in an epigenetic manner by histone deacetylase inhibitors such as valproic acid and suberoylanilide hydroxamic acid; therefore, combination therapy with these should be considered. Lastly, the downregulation of immune suppressor cells could be helpful in potentiating CIK cell immunotherapy. Low-dose cyclophosphamide treatment was shown to attenuate Tregs [39] and blockade of the signal transducer and activator of transcription 3 (STAT3) suppressed MDSCs [40].
If the efficacy of CIK cell immunotherapy can be maximally potentiated, an investigation of whether CIK cell immunotherapy with/without loco-regional therapy (e.g., TACE) or systemic therapy (e.g., sorafenib) is effective for intermediate or advanced stage HCC may be required. Because maximal tumor reduction before or during adoptive immunotherapy could reduce immune suppressor cells, combination with loco-regional therapy or systemic therapy may allow CIK cells to fight residual tumor cells. In addition, ablation therapies (e.g., RFA) can induce tumor-specific immune responses, which may suggest these could potential combination partners with adoptive immunotherapy [41]. However, combination therapy with CIK cell immunotherapy and sorafenib remains a debatable issue since sorafenib has been reported to impair the function of DCs, tumor-specific T cells, and NK cells, and to increase MDSCs [42,43,44].
5.7 Conclusion
As an adjuvant therapy after potentially curative treatment for HCC, adoptive immunotherapy using ex vivo expanded autologous CIK cells is the only treatment that has been proven to prolong recurrence-free survival as well as overall survival, except for antiviral treatment of HBV-related HCC. The safety of CIK cell immunotherapy has been well demonstrated. However, the clinical efficacy of CIK cells has been shown to exist only for very early or early HCC after curative treatment. Theoretically, maximal tumor reduction before or during adoptive immunotherapy could enhance the efficacy of CIK cells. Combination treatment with other types of adoptive immunotherapy and/or immune checkpoint inhibitors may also potentiate CIK cell therapy.
References
Park JW, Chen M, Colombo M, Roberts LR, Schwartz M, Chen PJ, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35:2155–66.
Llovet JM, Di Bisceglie AM, Bruix J, Kramer BS, Lencioni R, Zhu AX, et al. Design and endpoints of clinical trials in hepatocellular carcinoma. J Natl Cancer Inst. 2008;100:698–711.
Cho EJ, Lee JH, Yoo JJ, Choi WM, Lee MJ, Cho Y, et al. Serum insulin-like growth factor-I level is an independent predictor of recurrence and survival in early hepatocellular carcinoma: a prospective cohort study. Clin Cancer Res. 2013;19:4218–27.
Youn HG, An JY, Choi MG, Noh JH, Sohn TS, Kim S. Recurrence after curative resection of early gastric cancer. Ann Surg Oncol. 2010;17:448–54.
Lai EC, Fan ST, Lo CM, Chu KM, Liu CL, Wong J. Hepatic resection for hepatocellular carcinoma. An audit of 343 patients. Ann Surg. 1995;221:291–8.
Bruix J, Sherman M, American Association for the Study of Liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2.
European Association for The Study of The Liver, European Organisation for Research Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–43.
Yee C, Greenberg P. Modulating T-cell immunity to tumours: new strategies for monitoring T-cell responses. Nat Rev Cancer. 2002;2:409–19.
Bowen DG, Zen M, Holz L, Davis T, McCaughan GW, Bertolino P. The site of primary T cell activation is a determinant of the balance between intrahepatic tolerance and immunity. J Clin Invest. 2004;114:701–12.
Thomson AW, Knolle PA. Antigen-presenting cell function in the tolerogenic liver environment. Nat Rev Immunol. 2010;10:753–66.
Kuniyasu Y, Marfani SM, Inayat IB, Sheikh SZ, Mehal WZ. Kupffer cells required for high affinity peptide-induced deletion, not retention, of activated CD8+ T cells by mouse liver. Hepatology. 2004;39:1017–27.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–99.
Ungefroren H, Sebens S, Seidl D, Lehnert H, Hass R. Interaction of tumor cells with the microenvironment. Cell Commun Signal. 2011;9:18.
Zamarron BF, Chen W. Dual roles of immune cells and their factors in cancer development and progression. Int J Biol Sci. 2011;7:651–8.
Korangy F, Hochst B, Manns MP, Greten TF. Immune responses in hepatocellular carcinoma. Dig Dis. 2010;28:150–4.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–48.
Flecken T, Spangenberg HC, Thimme R. Immunobiology of hepatocellular carcinoma. Langenbeck’s Arch Surg. 2012;397:673–80.
Chew V, Tow C, Teo M, Wong HL, Chan J, Gehring A, et al. Inflammatory tumour microenvironment is associated with superior survival in hepatocellular carcinoma patients. J Hepatol. 2010;52:370–9.
Dudley ME, Wunderlich JR, Shelton TE, Even J, Rosenberg SA. Generation of tumor-infiltrating lymphocyte cultures for use in adoptive transfer therapy for melanoma patients. J Immunother. 2003;26:332–42.
Rosenberg SA, Spiess P, Lafreniere R. A new approach to the adoptive immunotherapy of cancer with tumor-infiltrating lymphocytes. Science. 1986;233:1318–21.
Steinman DA, Rutt BK. On the nature and reduction of plaque-mimicking flow artifacts in black blood MRI of the carotid bifurcation. Magn Reson Med. 1998;39:635–41.
Palmer DH, Midgley RS, Mirza N, Torr EE, Ahmed F, Steele JC, et al. A phase II study of adoptive immunotherapy using dendritic cells pulsed with tumor lysate in patients with hepatocellular carcinoma. Hepatology. 2009;49:124–32.
Butterfield LH, Ribas A, Dissette VB, Lee Y, Yang JQ, De la Rocha P, et al. A phase I/II trial testing immunization of hepatocellular carcinoma patients with dendritic cells pulsed with four alpha-fetoprotein peptides. Clin Cancer Res. 2006;12:2817–25.
Lee JH, Lee Y, Lee M, Heo MK, Song JS, Kim KH, et al. A phase I/IIa study of adjuvant immunotherapy with tumour antigen-pulsed dendritic cells in patients with hepatocellular carcinoma. Br J Cancer. 2015;113:1666–76.
Lee JH, Tak WY, Lee Y, Heo MK, Song JS, Kim HY, et al. Adjuvant immunotherapy with autologous dendritic cells for hepatocellualr carcinoma, randomized phase II study. Oncoimmunology. 2017;
Raulet DH, Vance RE. Self-tolerance of natural killer cells. Nat Rev Immunol. 2006;6:520–31.
Yang Y, Lim O, Kim TM, Ahn YO, Choi H, Chung H, et al. Phase I study of random healthy donor-derived allogeneic natural killer cell therapy in patients with malignant lymphoma or advanced solid tumors. Cancer Immunol Res. 2016;4:215–24.
Ahmadzadeh M, Rosenberg SA. IL-2 administration increases CD4+ CD25(hi) Foxp3+ regulatory T cells in cancer patients. Blood. 2006;107:2409–14.
Ochoa AC, Gromo G, Alter BJ, Sondel PM, Bach FH. Long-term growth of lymphokine-activated killer (LAK) cells: role of anti-CD3, beta-IL 1, interferon-gamma and -beta. J Immunol. 1987;138:2728–33.
Thanendrarajan S, Nowak M, Abken H, Schmidt-Wolf IG. Combining cytokine-induced killer cells with vaccination in cancer immunotherapy: more than one plus one? Leuk Res. 2011;35:1136–42.
Kim HM, Lim J, Yoon YD, Ahn JM, Kang JS, Lee K, et al. Anti-tumor activity of ex vivo expanded cytokine-induced killer cells against human hepatocellular carcinoma. Int Immunopharmacol. 2007;7:1793–801.
Takayama T, Sekine T, Makuuchi M, Yamasaki S, Kosuge T, Yamamoto J, et al. Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: a randomised trial. Lancet. 2000;356:802–7.
Weng DS, Zhou J, Zhou QM, Zhao M, Wang QJ, Huang LX, et al. Minimally invasive treatment combined with cytokine-induced killer cells therapy lower the short-term recurrence rates of hepatocellular carcinomas. J Immunother. 2008;31:63–71.
Hui D, Qiang L, Jian W, Ti Z, Da-Lu K. A randomized, controlled trial of postoperative adjuvant cytokine-induced killer cells immunotherapy after radical resection of hepatocellular carcinoma. Dig Liver Dis. 2009;41:36–41.
Lee JH, Lee JH, Lim YS, Yeon JE, Song TJ, Yu SJ, et al. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology. 2015;148:1383–91. e6
Beyer M, Schultze JL. Regulatory T cells in cancer. Blood. 2006;108:804–11.
Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58:49–59.
Poh SL, Linn YC. Immune checkpoint inhibitors enhance cytotoxicity of cytokine-induced killer cells against human myeloid leukaemic blasts. Cancer Immunol Immunother. 2016;65:525–36.
Greten TF, Ormandy LA, Fikuart A, Hochst B, Henschen S, Horning M, et al. Low-dose cyclophosphamide treatment impairs regulatory T cells and unmasks AFP-specific CD4+ T-cell responses in patients with advanced HCC. J Immunother. 2010;33:211–8.
Vasquez-Dunddel D, Pan F, Zeng Q, Gorbounov M, Albesiano E, Fu J, et al. STAT3 regulates arginase-I in myeloid-derived suppressor cells from cancer patients. J Clin Invest. 2013;123:1580–9.
Greten TF, Duffy AG, Korangy F. Hepatocellular carcinoma from an immunologic perspective. Clin Cancer Res. 2013;19:6678–85.
Hipp MM, Hilf N, Walter S, Werth D, Brauer KM, Radsak MP, et al. Sorafenib, but not sunitinib, affects function of dendritic cells and induction of primary immune responses. Blood. 2008;111:5610–20.
Chen Y, Huang Y, Reiberger T, Duyverman AM, Huang P, Samuel R, et al. Differential effects of sorafenib on liver versus tumor fibrosis mediated by stromal-derived factor 1 alpha/C-X-C receptor type 4 axis and myeloid differentiation antigen-positive myeloid cell infiltration in mice. Hepatology. 2014;59:1435–47.
Krusch M, Salih J, Schlicke M, Baessler T, Kampa KM, Mayer F, et al. The kinase inhibitors sunitinib and sorafenib differentially affect NK cell antitumor reactivity in vitro. J Immunol. 2009;183:8286–94.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Lee, JH., Yoon, JH. (2017). Cytokine-Induced Killer Cells for the Adjuvant Treatment of Patients with HCC. In: F. Greten, T. (eds) Immunotherapy of Hepatocellular Carcinoma. Springer, Cham. https://doi.org/10.1007/978-3-319-64958-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-64958-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-64957-3
Online ISBN: 978-3-319-64958-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)