Abstract
REM sleep behavior disorder (RBD), a condition of dream enactment, often predates Parkinson’s disease (PD) and is the result of early neurodegenerative processes in the brainstem. Normally, REM sleep is characterized by vivid mentation combined with skeletal muscle paralysis. This REM atonia is diminished or absent in RBD, which enables patients to act out their dreams with violent, injurious nocturnal behaviors. Consistent with an impending neurodegenerative disorder, patients with RBD demonstrate subtle motor, autonomic, and cognitive changes frequently seen in synucleinopathies. These disorders include PD as well as multiple system atrophy (MSA) and dementia with Lewy bodies (DLB). In PD, RBD is linked with the akinetic–rigid predominant subtype, gait freezing, and predicts aggressive cognitive impairment. Clinical management is focused upon decreasing the potential for sleep-related injuries (SRIs), treating comorbid sleep disorders, and eliminating exacerbating agents. High-dose melatonin, low-dose clonazepam, and combined melatonin–clonazepam appear to be effective therapies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Obstructive Sleep Apnea
- Deep Brain Stimulation
- Multiple System Atrophy
- Dementia With Lewy Body
- Sodium Oxybate
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Historical Perspective
In 1817, James Parkinson wrote “An Essay on the Shaking Palsy” [1]. This first comprehensive description of the disorder that would later bear his name noted that “sleep becomes much disturbed” in patients and hinted at a disorder of agitated dream enactment.
His (Case VI) attendants observed, that of late the trembling would sometimes begin in his sleep, and increase until it awakened him: when he always was in a state of agitation and alarm.
…when exhausted nature seizes a small portion of sleep, the motion becomes so violent as not only to shake the bed-hangings, but even the floor and sashes of the room.
Prior to Parkinson’s monograph, episodes of dream enactment suggestive of RBD were reported as early by Hippocrates (circa 460–370 BCE), Aristotle (384–322 BCE), and Galen (circa 129–200) and later by Cervantes (1547–1616). By the Renaissance, dream enactment was considered a window into subconscious psychological conflict. In William Shakespeare’s Macbeth, the sleepwalking Lady Macbeth admits to being a coconspirator in murder and reveals her subsequent internal torment.
Out damned spot! Out, I say! …What, will these hands never be clean?
Soon after Aserinsky and Kleitman discovered regularly occurring periods of eye motility during sleep in 1953 [2], investigators began to explore the brainstem mechanisms of REM sleep, including those leading to skeletal muscle paralysis. In 1965, experimental lesions of pontine regions by Jouvet adjacent to the locus coeruleus in cats caused an absence of the expected atonia. These cats demonstrated prominent motor behaviors during REM sleep suspected to be dream mentation (“oneirism”) [3].
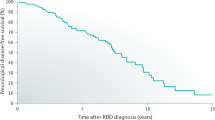
In 1982, Schenck and Mahowald evaluated a 67-year-old man who presented with a history of violent dream-enactment behavior (DEB). A subsequent polysomnogram demonstrated REM sleep without atonia along with vigorous DEB. In 1986, they published a series of patients and named the condition “REM sleep behavior disorder.” By 1996, 38 % of their original series of patients had developed a parkinsonian syndrome and by 2013 the conversion rate reached 81 % [4].
2 Clinical Presentation
Prior to developing bradykinesia, cogwheel rigidity, and tremor, many Parkinson’s disease (PD) patients will describe a parasomnia or abnormal nocturnal behavior emanating from sleep. The sleep-related movements appear purposeful as if the patient is acting out some internal dream plot and when awoken, vivid dreams are described. The condition typically presents in a middle-aged individual without a history of sleepwalking or other parasomnia. The frequency of incidents ranges from once every few months to multiple nightly episodes. Often, there is a prolonged prodrome lasting years with progressively more prominent nocturnal behaviors occurring over time [5, 6].
The spectrum of dream-enactment behavior (DEB) in RBD varies from small hand movements to violent activities such as punching, kicking, or leaping out of bed. Examples of sleep-related injuries include subdural hematoma, shoulder dislocation, cervical fracture, as well as lacerations severing tendons, arteries, and nerves. As bed partners are frequently the target of violent dream enactment, RBD may have forensic implications, with patients wrongly in the criminal justice system [5, 6].
Patients manifest DEB more often during the second half of the night and sleep-related injury (SRI) is more likely to occur in later REM periods. This is related to the progressive increase in phasic activity, frequency, and duration of REM sleep normally seen throughout a night of sleep.
Importantly, RBD patients may not have more violent dreams than normal individuals. Instead, they merely act them out. Sleep-related vocalizations may be loud and frequently laden with expletives. This is most often discordant from waking personality, and RBD patients do not demonstrate greater daytime aggressiveness.
Patients and families may adopt extraordinary measures to prevent SRI: placing obstacles to hinder exiting the bed or sleeping on a floor mattress in a room devoid of furniture. Prolonged diagnostic delay is common and some families deal with these behaviors for decades prior to seeking medical attention.
Prior to the onset, and early in the course of PD, DEB progresses in frequency and intensity. Then late in the disease state a moderation of RBD occurs, likely secondary to diffuse motor circuit impairment [6].
3 Epidemiology
Surveys have revealed that some DEB is nearly universal with 98 % of college-aged students reporting at least one episode of DEB [7]. The vast majority of these cases, however, are transient and nondistressing. Various reports have suggested that the prevalence of RBD is approximately 0.5 % in the general population [5], with higher prevalence among patients with neurodegenerative disease, other sleep disorders, or on antidepressant medications [5, 8]. Thus, there are approximately 35 million patients worldwide; however, the clinical symptoms are frequently dismissed and thus vast majority of cases remain undiagnosed for a long time.
As noted above, RBD is often a heralding manifestation of PD and is common among other alpha-synuclein disorders. According to several studies, approximately one-third to one-half of patients with PD have RBD [6, 9, 10]. Among similar pathologies the frequency is even higher, with 50–80 % of patients with DLB and 80–95 % of patients with MSA [6, 11].
Similar to PD, RBD is associated with various environmental and behavioral risk factors. In particular, RBD patients are more likely to smoke, have a history of traumatic brain injury, farming, pesticide exposure, and fewer years of education [12].
The majority of reported cases are males; however, female RBD is likely underreported. Women present with less injurious dream enactment and thus are less likely to receive medical attention. Further, due to the gender difference in life expectancy, elderly women are less likely to have bed partners than elderly men, and thus less likely to have witnessed parasomnia behaviors [13, 14].
4 RBD and Early Features of Alpha-Synuclein Pathology
Patients with RBD demonstrate clinical and subclinical phenomena suggestive of an impending alpha-synuclein CNS pathology. When fully developed, these disorders manifest as either PD, MSA, DLB or rarely pure autonomic failure.
Motor testing in RBD demonstrates slight, often imperceptible parkinsonian abnormalities. In particular, subtle changes are noted on the Purdue Peg Board, alternate tap test, the Unified Parkinson’s Disease Rating Scale (UPDRS), and timed evaluation of standing and walking [15]. Further, in a survey of normal elderly individuals, the presence of RBD symptoms was associated with at least mild parkinsonian exam findings [6].
Patients with RBD also have subtle cognitive dysfunction. Studies have demonstrated impairments in visuospatial skills as well as in color and facial expression identification [15, 16]. Other investigations have revealed deficits in attention and executive function [6]. Prospectively, the presence of RBD symptoms confers a greater than twofold risk of developing mild cognitive impairment (MCI) over 4 years [17]. Conversely, among patients with MCI or dementia the presence of RBD helps distinguish DLB from Alzheimer’s disease [6, 18].
As in PD, hyposmia/anosmia is frequently noted in RBD. Over half of RBD patients have impairments in smell identification, compared to 10–15 % in age-matched controls [15, 19]. The most common deficit is an inability to identify paint thinner [19]. RBD and hyposmia in combination with impaired color identification place the patient at very high risk of impending PD [16].
In RBD, autonomic dysfunction is consistent with an evolving neurodegenerative disorder. Comorbid enteric neuron pathology manifests as constipation [15] and similar to hyposmia, when combined with impaired color vision predicts progression to PD [20]. Heart rate responses to both orthostasis and arousal are blunted compared to controls and intermediate compared to PD [21]. Cardiac scintigraphy has been used to predict a parkinsonian syndrome. Among RBD patients, reduced uptake of (123) I-metaiodobenzylguanidine, indicating sympathetic denervation, has been demonstrated in PD and DLB but not in MSA [6, 22].
4.1 RBD in PD
RBD is associated with the akinetic/rigid subtype of PD and a greater burden of disease. Removal of tremor scores from the UPDRS increases its sensitivity and specificity in diagnosing early PD among RBD patients [23]. Further, RBD in PD is associated with a higher Hoehn and Yahr stage (increased severity), greater motor fluctuations, and increased levodopa dose [9]. Orthostatic hypotension and constipation are both more common in PD with RBD compared to PD alone [9, 24]. In DLB, the presence of RBD is associated with earlier onset of parkinsonism and visual hallucinations [25].
PD patients with RBD are also more likely to have freezing of gait (FOG) and a higher frequency of falls [24]. Interestingly, many of the same brainstem regions implicated in the pathophysiology of RBD mediate the pathogenesis of FOG. Moreover, it was recently demonstrated that PD patients with FOG demonstrate increased tonic REM EMG tone compared to PD patients without FOG [26].
The presence of RBD predicts greater cognitive dysfunction in PD. Neuropsychological testing has demonstrated at least mild cognitive impairment in nearly all (90 %) PD patients with RBD compared to less than half (38 %) of the patients with PD alone [27]. Among PD patients who are without severe cognitive deficit, RBD predicts dementia. In a 4-year prospective study, 48 % of PD patients with RBD developed dementia compared to none of PD patients without RBD [28].
It has been reported that overnight RBD behaviors in PD lack the bradykinesia and hypophonia that characterize daytime motor performance in PD. This phenomenon suggests that RBD motor activity may bypass the basal ganglia regulatory.
5 Pathophysiology
Prior to the hallmark destruction of dopamine-producing neurons in the substantia nigra (SN), early alpha-synuclein degeneration occurs in the brainstem nuclei that control REM sleep. Under physiological circumstances the suppression of motor activity during REM is the cumulative result of multiple pathways that ultimately terminate on spinal motor neurons, most notably via the magnocellular reticular formation in the medulla. Multiple areas of the brainstem may influence muscle tone including pontine REM-on (precoeruleus and sublateral dorsal) and REM-off (ventral lateral portion of the periaqueductal gray matter and lateral pontine tegmentum) nuclei [6]. Decreased neuronal fiber integrity is seen in these REM-regulating regions among patients with RBD [29].
By the time PD motor abnormalities develop, the majority of dopaminergic cells in the substantial nigra (SN) are dysfunctional. However, in RBD patients who have not yet manifested parkinsonism, neuroimaging reveals a coincident and progressive reduction in dopamine transporters and innervation [30, 31]. Further, transcranial ultrasound hyperechogenicity of substantial nigra in RBD resembles abnormalities seen in PD [32].
Cholinergic function is impaired in RBD and correlates with cognitive decline. Among PD subjects with RBD compared to PD subjects without RBD positron emission tomography reveals cholinergic denervation [33]. These findings are similar to those seen in transcranial magnetic stimulation studies that demonstrate reduced short latency inhibition, indicating impaired cholinergic activity, in RBD. These cholinergic deficits are linked with deficiencies in episodic verbal memory, executive function, and visuospatial cognitive domains [27].
Cortical abnormalities, similar to those seen in PD and related disorders, are noted in patients with RBD. Voxel-based morphology studies demonstrate gray matter reductions that correlate with decreased regional cerebral blood flow (rCBF) in the parieto-occipital and hippocampal regions [34, 35]. Also, an increase in hippocampal rCBF is noted in RBD patients with MCI and predicts those who will ultimately progress to either PD or DLB [36].
RBD is not associated only with alpha-synuclein neurodegenerative disorders. Other etiologies include other forms of neurodegeneration, side effects of medications, structural CNS lesions, and narcolepsy linked to the orexin dysfunction. RBD has been reported in tauopathy-related parkinsonian syndromes (progressive supranuclear palsy, Guadeloupean parkinsonism, corticobasal degeneration), TDP-43opathies (frontotemporal dementia, amyotrophic lateral sclerosis), trinucleotide repeat disorders (SCA-3, Huntington’s disease), and rarely amyloidopathies (Alzheimer’s disease) [6]. However, these disorders are not typically preceded by RBD, but instead RBD develops after the onset of other neurological deficits. Medications such as tricyclic antidepressants and serotonin-specific reuptake inhibitors can precipitate or exacerbate RBD [6, 37]. It is uncertain whether these medications cause a de-novo RBD or, unmask latent RBD. Occasionally, various vascular, demyelinating, and traumatic etiologies are linked to development of RBD [38]. In these cases, cranial imaging typically demonstrates pontine tegmentum pathology. Finally, impaired orexin function can precipitate DEB, with up to 50 % of narcolepsy patients having RBD symptoms. This association is strongest among narcolepsy patients with cataplexy [39].
6 Clinical Evaluation and Diagnosis
6.1 History and Examination
A detailed review of the patient’s sleep and circadian rhythm, preferably with the assistance of a bed partner is the first step in the evaluation of all parasomnia behaviors. Recurrent, brief DEB occurring in the later half of the sleep period followed by complete alertness and orientation upon awakening are features that help to distinguish RBD from other similar disorders. This presentation contrasts with sleepwalking where there is often a lifelong history of prolonged, complex, nonviolent activities emanating from the first half of the sleep period with residual confusion [5].
Validated screening surveys are available to help identify RBD and quantify disease burden. These include the RBD Questionnaire-Hong Kong (RBDQ-HK) and the Innsbruck RBD inventory [40, 41]. In addition, two separate groups of investigators have reported one-question instruments to detect RBD. The Mayo Sleep Questionnaire (MSQ) is a comprehensive sleep health survey, filled out by bed partners, that includes the following question: “Have you ever seen the patient appear to ‘act out his/her dreams’ while sleeping (punched or flailed arms in the air, shouted or screamed)?” [6]. This question is very similar to the RBD Single-Question Screen: “Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams’ while asleep (for example, punching, flailing your arms in the air, making running movements, etc.)?” [42].
It is important to inquire about alpha-synucleinopathies, when assessing a possible RBD. When chronic unexplained hyposmia and/or constipation coexist with RBD, they are highly suggestive of impending neurodegeneration. Further, it is important to assess early bradykinesia and rigidity. These phenomena are often imperceptible and may be dismissed as routine aging. In particular, a question such as “Does a patient have difficulty turning over in bed, or bradykinesia during routine activities such as eating and dressing, or do they have changes in handwriting?” may be very informative. FOG, commonly present in PD, and can be explored with the question. “Do your feet ever feel as if they are stuck to the floor?”
Among patients with known PD inquiring about DEB is a critical part of a comprehensive evaluation. In the setting of PD falling out of bed during sleep is highly suggestive of RBD and a risk factor for sleep-related injury. Both the Innsbruck RBD inventory and RBDQ-HK are effective screens for RBD among patients with Parkinson’s disease.
On examination, careful scrutiny of subtle parkinsonism is essential for accurate longitudinal clinical monitoring. Documentation should contain a patient’s affectation, blink rate, volume of voice, speed of articulation, as well as motor tone with distracting maneuvers to elicit subtle cogwheeling rigidity. Important features on gait testing include any freezing of movement, stride length, arm swing, and number of steps to turn 180°. Further, postural instability (loss of righting reflex with sudden retropulsion) is a risk factor for falling and commonly noted in PD patients with RBD. The UPDRS includes these examination features and can be used to prospectively quantify the burden of disease.
6.2 Polysomnography
Polysomnography (PSG) with time-synchronized video is necessary for definitive RBD diagnosis and to exclude other conditions [43]. Even when abnormal behavior does not occur during a single night study, the PSG is helpful in documenting the absence of REM atonia. The combination of REM without atonia, a history of DEB, and absence of clinically significant sleep disordered breathing can establish a diagnosis. When RBD behaviors do occur, they are often distinguished from other nocturnal behaviors based on appearance alone. RBD movements more typically appear purposeful, pseudohallucinatory, frequently with hand babbling (limb wrist, flexed fingers—like a baby). Other REM sleep phenomena are often present including snoring and in males, penile tumescence [44].
The American Academy of Sleep Medicine has defined a PSG epoch as either sustained elevation of chin EMG activity (greater than 50 % of the 30-s epoch) or excessive bursts of transient muscle activity (at least half of all 3-s mini epochs). Using this criteria to define RBD epochs, 30 % or greater appears to reliably distinguish RBD from non-RBD patients. Subtle dream enactment often involves only the hands and thus forearm EMG monitoring should be included [6].
PSG is particularly helpful in ruling out conditions such as sleep-disordered breathing, periodic limb movement disorder (PLMD), and nocturnal epilepsy as a source of the reported behaviors. The REM sleep fragmentation of obstructive sleep apnea (OSA) can lead to DEB, but typically resolves with CPAP therapy. PLMD, primarily a NREM sleep phenomena, can be confused with RBD by history if the leg movements are especially prominent, but is easily discernible on PSG. Nocturnal seizures should be evaluated with an expanded EEG montage especially if there is a history of stereotyped, abnormal, and repetitive behaviors.
7 Treatment
Modifying the sleeping environment with a focus upon patient safety is the initial step in RBD treatment. The patient should remove any bedside object or furniture that could be injurious. In particular, firearms and windows should not be easily accessible. Bed partners are advised to sleep separately until RBD is brought under control. However, this advice is commonly disregarded as bed partners will describe an ability to pacify DEB with a few firm, but calm words.
RBD inducing or aggravating medications should be eliminated and comorbid sleep disorders treated. Most cases of medication-induced RBD are self-limited following discontinuation of offending medication. DEBs frequently seen in association with OSA typically resolve with treatment of OSA.
When violent nocturnal behaviors persist despite these interventions or in situations with a high probability of injury, pharmacotherapy is appropriate [45]. The most commonly prescribed medications include clonazepam and/or melatonin [6, 46, 47]. As large randomized placebo-controlled therapeutic trials have not yet been performed, consensus treatment has arisen based upon case series and small clinical trials [45, 48].
7.1 Clonazepam
Over the last 30 years, clonazepam has been the most widely prescribed agent for RBD and approximately 90 % of patients initially respond well to low doses (0.5–1.0 mg) administered at bedtime [4, 49]. Clonazepam reduces phasic EMG activity during REM sleep with minimal effect on tonic muscle activity. The agent also appears to be effective in cases that have progressed to PD [4, 6].
Long-term follow-up studies revealed mixed results, ranging from sustained benefit without dose escalation to frequent dose escalations and treatment failures [4, 50–52]. In one series, 58 % of patients on clonazepam reported clinically significant adverse effects with 50 % either stopping the medication or reducing the dose [52]. Also, clonazepam may be particularly problematic in the setting of advanced PD where its prolonged duration of action can result in morning sedation, impaired gait, and cognitive side effects [53].
7.2 Melatonin
Recently, several studies have suggested that melatonin may be an effective and safe first-line treatment for RBD either in combination with clonazepam or as sole therapy. By uncertain mechanisms, melatonin in high doses at bedtime (6–15 mg) augments REM atonia and improves RBD symptoms. Effects persist for weeks after the agent is discontinued [6, 47].
Importantly, a recent direct comparison study noted that melatonin was equal to clonazepam in treatment efficacy and superior in side effect profile. Patients on melatonin reported fewer adverse effects, in particular less falls and injuries compared to clonazepam [54]. In the setting of advanced PD, melatonin is a particularly intriguing option as it is only mildly sedating.
7.3 Pramipexole
Pramipexole may be effective in mild cases of RBD, in particular those associated with frequent PLMs. Compared to clonazepam responsive patients, pramipexole responsive patients have milder disease at baseline as measured by REM atonia. Similar to treating OSA in RBD, pramipexole may decrease nocturnal behaviors by reversing a sleep fragmenting condition. Patients report a decrease in distressing nocturnal behaviors along with a decrease in PLMs; however, pramipexole has no effect upon REM atonia [55].
7.4 Rivastigmine
Cholinergic agents may be useful in RBD among patients who have failed conventional therapy. One small placebo-controlled crossover trial noted that the cholinesterase inhibitor rivastigmine reduced the number of DEB episodes as noted by bed partners [56].
7.5 Other Medications
Various therapies have been reported at least once to be successful. These include imipramine, carbamazepine, levodopa, donepezil, sodium oxybate, triazolam, zopiclone, quetiapine, and clozapine [45, 46, 52].
7.6 Deep Brain Stimulation
Deep brain stimulation (DBS) for PD has thus far not been therapeutic for comorbid RBD. Three case series of PD patients with RBD undergoing DBS noted improvements in subjective sleep quality and sleep architecture on PSG, however, with little to no improvement in DEB or REM atonia [57–59]. These findings were not unexpected as the target of DBS in these studies, the subthalamic nucleus, does not have a known effect upon REM sleep. Other DBS targets for PD include the globus pallidus internus and the paramedian pontine nucleus. The PPN is an REM-modulating nucleus and thus an intriguing target for future RBD investigations.
7.7 Bed Alarm Therapy
Medication refractory RBD is a daunting and potentially life-threatening condition. Exiting the bed while acting out a dream is a particularly high-risk behavior and may result in severe traumatic injury.
The low arousal threshold and rapid transition to alert wakefulness from REM sleep offers a therapeutic window to halt behavior prior to SRI. Despite apparent unconsciousness during REM sleep, the brain is readily responsive to complex auditory sound processing. This contrasts with the high arousal threshold of NREM sleep often demonstrated by the inability to redirect or wake up SW patients (a NREM parasomnia). This phenomenon is often noted by bed partners who describe an ability to calm RBD patients with a simple phrase such as, “sweetheart, you are having a dream go back to sleep.” A customized bed alarm, delivering such a calming message when a patient attempts to leave the bed can halt potentially injurious dream enactment [53].
8 Future Directions
8.1 Possible Neuroprotection
At this time, it is uncertain what measures may be taken to prevent or delay the onset of a neurodegenerative disorder such as PD. However, as RBD may help identify patients at high risk for developing PD, it may also be an important target in studies of neuroprotective/disease-modifying therapies.
These preliminary investigations have begun to explore whether compounds can slow, halt, or possibly even reverse alpha-synuclein neurodegeneration. Recently, riluzole, an antiglutamate compound currently used as neuroprotection in amyotrophic lateral sclerosis, has been demonstrated to both prevent RBD and increase the number of surviving dopamine neurons in the marmoset MPTP model of Parkinson’s disease [60]. Another intriguing agent, already in use among RBD patients, is melatonin. Recently, melatonin has been demonstrated to have antioxidant properties and to protect mitochondrial function, suggesting it has potential as a neuroprotective agent [61]. Obviously, prospective randomized-controlled trials are needed prior to concluding that any substance may prevent or slow neurodegeneration.
References
Parkinson J. An essay on the shaking palsy. London: Sherwood, Neely, and Jones; 1817.
Aserinsky E, Kleitman N. Regularly occurring periods of eye motility, and concomitant phenomena, during sleep. Science. 1953;118(3062):273–4.
Jouvet D, Vimont P, Delorme F. Study of selective deprivation of the paradoxal phase of sleep in the cat. J Physiol Paris. 1964;56:381.
Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81 % of older males initially diagnosed with idiopathic REM sleep behavior disorder (RBD): 16year update on a previously reported series. Sleep Med. 2013;14:744–8.
American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. 2nd ed. Westchester: American Academy of Sleep Medicine; 2005.
Boeve BF. REM sleep behavior disorder: updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann N Y Acad Sci. 2010;1184:15–54.
Nielsen T, Svob C, Kuiken D. Dream-enacting behaviors in a normal population. Sleep. 2009;32(12):1629–36.
Boeve BF, Silber MH, Parisi JE, Dickson DW, Ferman TJ, Benarroch EE, et al. Synucleinopathy pathology and REM sleep behavior disorder plus dementia or parkinsonism. Neurology. 2003;61(1):40–5.
Nihei Y, Takahashi K, Koto A, Mihara B, Morita Y, Isozumi K, et al. REM sleep behavior disorder in Japanese patients with Parkinson’s disease: a multicenter study using the REM sleep behavior disorder screening questionnaire. J Neurol. 2012;259(8):1606–12.
Poryazova R, Oberholzer M, Baumann CR, Bassetti CL. REM sleep behavior disorder in Parkinson’s disease: a questionnaire-based survey. J Clin Sleep Med. 2013;9(1):55–9.
Plazzi G, Corsini R, Provini F, Pierangeli G, Martinelli P, Montagna P, et al. REM sleep behavior disorders in multiple system atrophy. Neurology. 1997;48(4):1094–7.
Postuma RB, Montplaisir JY, Pelletier A, Dauvilliers Y, Oertel W, Iranzo A, et al. Environmental risk factors for REM sleep behavior disorder: a multicenter case-control study. Neurology. 2012;79(5):428–34.
Bodkin CL, Schenck CH. Rapid eye movement sleep behavior disorder in women: relevance to general and specialty medical practice. J Womens Health (Larchmt). 2009;18(12):1955–63.
Bjornara KA, Dietrichs E, Toft M. REM sleep behavior disorder in Parkinson’s disease–is there a gender difference? Parkinsonism Relat Disord. 2013;19(1):120–2.
Postuma RB, Lang AE, Massicotte-Marquez J, Montplaisir J. Potential early markers of Parkinson disease in idiopathic REM sleep behavior disorder. Neurology. 2006;66(6):845–51.
Postuma RB, Gagnon JF, Vendette M, Desjardins C, Montplaisir JY. Olfaction and color vision identify impending neurodegeneration in rapid eye movement sleep behavior disorder. Ann Neurol. 2011;69(5):811–8.
Boot BP, Boeve BF, Roberts RO, Ferman TJ, Geda YE, Pankratz VS, et al. Probable rapid eye movement sleep behavior disorder increases risk for mild cognitive impairment and Parkinson disease: a population-based study. Ann Neurol. 2012;71(1):49–56.
Ferman TJ, Boeve BF, Smith GE, Lin SC, Silber MH, Pedraza O, et al. Inclusion of RBD improves the diagnostic classification of dementia with Lewy bodies. Neurology. 2011;77(9):875–82.
Fantini ML, Postuma RB, Montplaisir J, Ferini-Strambi L. Olfactory deficit in idiopathic rapid eye movements sleep behavior disorder. Brain Res Bull. 2006;70(4–6):386–90.
Ferini-Strambi L. Does idiopathic REM sleep behavior disorder (iRBD) really exist? What are the potential markers of neurodegeneration in iRBD? Sleep Med. 2011;12 Suppl 2:S43–9.
Frauscher B, Nomura T, Duerr S, Ehrmann L, Gschliesser V, Wenning GK, et al. Investigation of autonomic function in idiopathic REM sleep behavior disorder. J Neurol. 2012;259:1056–61.
Miyamoto T, Miyamoto M, Suzuki K, Nishibayashi M, Iwanami M, Hirata K. 123I-MIBG cardiac scintigraphy provides clues to the underlying neurodegenerative disorder in idiopathic REM sleep behavior disorder. Sleep. 2008;31(5):717–23.
Postuma RB, Lang AE, Gagnon JF, Pelletier A, Montplaisir JY. How does parkinsonism start? Prodromal parkinsonism motor changes in idiopathic REM sleep behaviour disorder. Brain. 2012;135(Pt 6):1860–70.
Romenets SR, Gagnon JF, Latreille V, Panniset M, Chouinard S, Montplaisir J, et al. Rapid eye movement sleep behavior disorder and subtypes of Parkinson’s disease. Mov Disord. 2012;27(8):996–1003.
Dugger BN, Boeve BF, Murray ME, Parisi JE, Fujishiro H, Dickson DW, et al. Rapid eye movement sleep behavior disorder and subtypes in autopsy-confirmed dementia with Lewy bodies. Mov Disord. 2012;27(1):72–8.
Videnovic A, Marlin C, Alibiglou L, et al. Increased REM sleep without atonia in Parkinson’s disease patients with freezing of gait. Neurology. 2013;81:1030–5.
Nardone R, Bergmann J, Brigo F, Christova M, Kunz A, Seidl M, et al. Functional evaluation of central cholinergic circuits in patients with Parkinson’s disease and REM sleep behavior disorder: a TMS study. J Neural Transm. 2013;120(3):413–22.
Postuma RB, Bertrand JA, Montplaisir J, Desjardins C, Vendette M, Rios Romenets S, et al. Rapid eye movement sleep behavior disorder and risk of dementia in Parkinson’s disease: a prospective study. Mov Disord. 2012;27(6):720–6.
Scherfler C, Frauscher B, Schocke M, Iranzo A, Gschliesser V, Seppi K, et al. White and gray matter abnormalities in idiopathic rapid eye movement sleep behavior disorder: a diffusion-tensor imaging and voxel-based morphometry study. Ann Neurol. 2011;69(2):400–7.
Eisensehr I, Linke R, Tatsch K, Kharraz B, Gildehaus JF, Wetter CT, et al. Increased muscle activity during rapid eye movement sleep correlates with decrease of striatal presynaptic dopamine transporters. IPT and IBZM SPECT imaging in subclinical and clinically manifest idiopathic REM sleep behavior disorder, Parkinson’s disease, and controls. Sleep. 2003;26(5):507–12.
Iranzo A, Valldeoriola F, Lomena F, Molinuevo JL, Serradell M, Salamero M, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective study. Lancet Neurol. 2011;10(9):797–805.
Miyamoto M, Miyamoto T, Iwanami M, Muramatsu S, Asari S, Nakano I, et al. Preclinical substantia nigra dysfunction in rapid eye movement sleep behaviour disorder. Sleep Med. 2012;13(1):102–6.
Kotagal V, Albin RL, Muller ML, Koeppe RA, Chervin RD, Frey KA, et al. Symptoms of rapid eye movement sleep behavior disorder are associated with cholinergic denervation in Parkinson disease. Ann Neurol. 2012;71(4):560–8.
Hanyu H, Inoue Y, Sakurai H, Kanetaka H, Nakamura M, Miyamoto T, et al. Regional cerebral blood flow changes in patients with idiopathic REM sleep behavior disorder. Eur J Neurol. 2011;18(5):784–8.
Vendette M, Gagnon JF, Soucy JP, Gosselin N, Postuma RB, Tuineag M, et al. Brain perfusion and markers of neurodegeneration in rapid eye movement sleep behavior disorder. Mov Disord. 2011;26(9):1717–24.
Dang-Vu TT, Gagnon JF, Vendette M, Soucy JP, Postuma RB, Montplaisir J. Hippocampal perfusion predicts impending neurodegeneration in REM sleep behavior disorder. Neurology. 2012;79(24):2302–6.
Hoque R, Chesson Jr AL. Pharmacologically induced/exacerbated restless legs syndrome, periodic limb movements of sleep, and REM behavior disorder/REM sleep without atonia: literature review, qualitative scoring, and comparative analysis. J Clin Sleep Med. 2010;6(1):79–83.
Boeve BF, Silber MH, Saper CB, Ferman TJ, Dickson DW, Parisi JE, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain. 2007;130(Pt 11):2770–88.
Dauvilliers Y, Jennum P, Plazzi G. REM sleep behavior disorder and REM sleep without atonia in narcolepsy. Sleep Med. 2013;14:775–81.
Li SX, Wing YK, Lam SP, Zhang J, Yu MW, Ho CK, et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK). Sleep Med. 2010;11(1):43–8.
Frauscher B, Ehrmann L, Zamarian L, Auer F, Mitterling T, Gabelia D, et al. Validation of the Innsbruck REM sleep behavior disorder inventory. Mov Disord. 2012;27(13):1673–8.
Postuma RB, Arnulf I, Hogl B, Iranzo A, Miyamoto T, Dauvilliers Y, et al. A single-question screen for rapid eye movement sleep behavior disorder: a multicenter validation study. Mov Disord. 2012;27(7):913–6.
Neikrug AB, Ancoli-Israel S. Diagnostic tools for REM sleep behavior disorder. Sleep Med Rev. 2012;16:415–29.
Oudiette D, Leu-Semenescu S, Roze E, Vidailhet M, De Cock VC, Golmard JL, et al. A motor signature of REM sleep behavior disorder. Mov Disord. 2012;27(3):428–31.
Aurora RN, Zak RS, Maganti RK, Auerbach SH, Casey KR, Chowdhuri S, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med. 2010;6(1):85–95.
Gagnon JF, Postuma RB, Montplaisir J. Update on the pharmacology of REM sleep behavior disorder. Neurology. 2006;67(5):742–7.
Kunz D, Mahlberg R. A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res. 2010;19(4):591–6.
Seppi K, Weintraub D, Coelho M, Perez-Lloret S, Fox SH, Katzenschlager R, et al. The movement disorder society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord. 2011;26 Suppl 3:S42–80.
Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123(Pt 2):331–9.
Gagnon JF, Petit D, Fantini ML, Rompre S, Gauthier S, Panisset M, et al. REM sleep behavior disorder and REM sleep without atonia in probable Alzheimer disease. Sleep. 2006;29(10):1321–5.
Gugger JJ, Wagner ML. Rapid eye movement sleep behavior disorder. Ann Pharmacother. 2007;41(11):1833–41.
Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med. 2009;5(3):235–9.
Howell MJ, Arneson PA, Schenck CH. A novel therapy for REM sleep behavior disorder (RBD). J Clin Sleep Med. 2011;7(6):639–644A.
McCarter SJ, Boswell CL, St Louis EK, Dueffert LG, Slocumb N, Boeve BF, et al. Treatment outcomes in REM sleep behavior disorder. Sleep Med. 2013;14(3):237–42.
Sasai T, Matsuura M, Inoue Y. Factors associated with the effect of pramipexole on symptoms of idiopathic REM sleep behavior disorder. Parkinsonism Relat Disord. 2013;19(2):153–7.
Di Giacopo R, Fasano A, Quaranta D, Della Marca G, Bove F, Bentivoglio AR. Rivastigmine as alternative treatment for refractory REM behavior disorder in Parkinson’s disease. Mov Disord. 2012;27(4):559–61.
Arnulf I, Bejjani BP, Garma L, Bonnet AM, Houeto JL, Damier P, et al. Improvement of sleep architecture in PD with subthalamic nucleus stimulation. Neurology. 2000;55(11):1732–4.
Iranzo A, Valldeoriola F, Santamaria J, Tolosa E, Rumia J. Sleep symptoms and polysomnographic architecture in advanced Parkinson’s disease after chronic bilateral subthalamic stimulation. J Neurol Neurosurg Psychiatry. 2002;72(5):661–4.
Cicolin A, Lopiano L, Zibetti M, Torre E, Tavella A, Guastamacchia G, et al. Effects of deep brain stimulation of the subthalamic nucleus on sleep architecture in parkinsonian patients. Sleep Med. 2004;5(2):207–10.
Verhave PS, Jongsma MJ, Van Den Berg RM, Vanwersch RA, Smit AB, Philippens IH. Neuroprotective effects of riluzole in early phase Parkinson’s disease on clinically relevant parameters in the marmoset MPTP model. Neuropharmacology. 2012;62(4):1700–7.
Srinivasan V, Cardinali DP, Srinivasan US, Kaur C, Brown GM, Spence DW, et al. Therapeutic potential of melatonin and its analogs in Parkinson’s disease: focus on sleep and neuroprotection. Ther Adv Neurol Disord. 2011;4(5):297–317.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Wien
About this chapter
Cite this chapter
Howell, M.J., Schenck, C.H. (2015). REM Sleep Behavior Disorder. In: Videnovic, A., Högl, B. (eds) Disorders of Sleep and Circadian Rhythms in Parkinson's Disease. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1631-9_10
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1631-9_10
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1630-2
Online ISBN: 978-3-7091-1631-9
eBook Packages: MedicineMedicine (R0)