Abstract
REM sleep behavior disorder (RBD) is known to be observed more frequently in patients with an α-synucleinopathy such as Parkinson’s disease (PD) than in the general population. The precise prevalence of RBD in Japanese PD patients is not known. Therefore, we investigated the prevalence and the clinical characteristics of patients with RBD in a large population of Japanese patients with PD. We investigated various clinical features and employed the Japanese version of the RBD screening questionnaire on 469 non-demented Japanese PD patients in this multicenter study. Probable or possible RBD was detected in 146 patients (31.1%) and was significantly associated with longer PD duration, higher Hoehn and Yahr stage, higher Unified Parkinson’s Disease Rating Scale part III subscale (7 items), more motor fluctuations, and a higher levodopa-equivalent daily dose (p < 0.01). As to the major autonomic dysfunctions, severe constipation was significantly more frequent in PD patients with RBD than in those without it (p < 0.01). The RBD symptoms of 53 patients (39.0%) preceded the onset of PD motor symptoms. The median interval from the onset of RBD symptoms to PD motor symptoms was 17.5 years, and 3 patients had intervals of over 50 years. This large-scale multicenter study revealed that RBD is a frequent non-motor symptom in Japanese patients with PD, which may precede the onset of motor symptoms. Moreover, RBD that increases with the duration and severity of PD may be associated with autonomic dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
REM sleep behavior disorder (RBD) is characterized by abnormal and complicated movement during sleep. Movement is related to the loss of REM sleep muscular atonia and is regarded as an expression of dream content. RBD patients yell, flail, kick, jump, and sometimes injure their partners. Schenck [1] initially reported RBD in 1986. Although the frequency of idiopathic RBD (iRBD) has not been studied in the Japanese population, the prevalence of iRBD is assumed to be about 0.5–2.0%, including the data based on a number of studies including a survey of iRBD patients in Hong Kong [2–4]. RBD is known to occur more frequently in patients with an α-synucleinopathy such as Parkinson’s disease (PD) than in the general population [5, 6]. Previous studies have reported that 33% of PD patients had RBD or REM sleep without atonia by polysomnogram (PSG) [7] and that 9.0% of iRBD patients developed PD within 1 year [8]. Moreover, the interval between the onset of iRBD and the onset of a subsequent neurologic syndrome, including PD, dementia with Lewy bodies (DLB), or multiple system atrophy (MSA), was reported to range up to 50 years, and the median interval was 3–25 years [9–13]. Therefore, RBD is thought to be one of the most frequent premotor symptoms of PD.
Although a definite diagnosis of RBD requires PSG [14], clinical neurologists frequently cannot rely on PSG to support the diagnosis, especially when dealing with a large PD population. In 2007, Stiasny-Kolster [15] proposed the RBD screening questionnaire (RBDSQ), a 10-item, patient self-rating tool, which proved to have high sensitivity and reasonable specificity for RBD diagnosis as confirmed by PSG. A Japanese version of the RBDSQ (RBDSQ-J) was found to have excellent sensitivity and specificity compared with controls and compared with patients who had obstructive sleep apnea [16]. RBDSQ-J is thought to be the most appropriate tool for screening RBD in PD at the present time.
In this multicenter study, we investigated the prevalence of RBD in Japanese PD patients by using RBDSQ-J to examine the various clinical characteristics in PD patients with RBD. We also estimated the interval of RBD onset before the appearance of PD motor symptoms.
Patients and methods
Subjects
A total of 533 patients with PD, who consulted one of the 11 hospitals participating in the Keio-PD database between October 2009 and April 2010 and who agreed to participate in this study, were registered consecutively in the Keio PD database. A total of 469 non-demented PD patients were included in this study; 60 patients with dementia and 4 patients without sufficient information were excluded. Dementia was diagnosed by neurologists using DSM-IV criteria [17]. We considered the RBDSQ-J scores of the patients with dementia or cognitive dysfunction as unreliable. The diagnosis of PD was made according to the UK Parkinson’s Disease Society Brain Bank clinical diagnosis criteria [18].
Assessments of variables
All the registered patients underwent the same assessments and interviews. We investigated their age at the assessment and at the onset of PD, the duration of PD, medications, motor symptoms, and complications including autonomic dysfunctions. The onset of PD was defined as the beginning of classical motor symptoms according to the information from each patient. Motor symptoms were assessed using the Hoehn and Yahr (H&Y) stage and the subscale of seven items from the unified Parkinson’s disease rating scale (UPDRS) part III, which consists of rest tremor, finger taps, rigidity of the four extremities, arising from a chair, gait, posture, and postural stability. We also investigated the presence of motor fluctuations using nine items of the wearing-off questionnaire of 19 symptoms (WOQ-19), which was designed to identify motor/nonmotor symptoms and motor/nonmotor fluctuations [19]. The Japanese version of WOQ-19 is also available. Autonomic dysfunctions including hyperhidrosis, urination difficulty, urinary incontinence, and severe constipation were assessed by neurologists, using the original structured questionnaire. Although we did not evaluate the severity of each autonomic dysfunction, severe constipation was defined as “less than one bowel movement for 3 days.”
We employed the RBDSQ-J to screen for RBD symptoms. RBDSQ-J is a self-reported questionnaire and consists of 10 items. Its score ranges from 0–13 points. According to the original paper, the cutoff score to diagnose probable or possible RBD (pRBD) was 4.5 [15]. Considering the RBDSQ-J score of 5 points as a positive test result, the authors of that report found a sensitivity of 0.89 and a specificity of 0.97 [16]. Furthermore, we investigated whether the pRBD onset preceded the PD onset (preceding pRBD) or not (non-preceding pRBD), and the interval of the pRBD onset before the appearance of PD motor symptoms. Assisted by their bed partners, all the PD patients answered the RBDSQ-J. These patients were also asked to specify if the symptoms compatible with RBD were present before PD. Patients who denied having RBD symptoms at the moment of evaluation were asked if they had experienced such symptoms in the past. Patients with a history of RBD symptoms (either present or past) were also evaluated by RBDSQ-J. A history of ever having had RBD symptoms was considered to indicate positivity for RBD in this study. The bed partner’s input was encouraged but not required.
Statistical analyses
JMP® software version 8.0 (SAS Institute, Japan) was used for the statistical analyses. The level of statistical significance in this study, defined as 0.05. Fisher’s exact test, was employed to estimate the difference in gender and the presence of motor fluctuation, hyperhidrosis, urination difficulty, urinary incontinence, and severe constipation. The Wilcoxon/Mann–Whitney U test was performed to estimate the difference in age at assessment, age at onset of PD, disease duration of PD, H&Y stage, UPDRS part III subscale, number of motor symptoms and total levodopa-equivalent daily dose (total LED) between patients with and without pRBD.
Results
The demographic and clinical features of all 469 eligible patients are shown in Table 1. There were 219 men and 250 women. Their age at the assessment was 71.0 ± 8.3 years (mean ± SD), their age at onset was 64.2 ± 10.3 years, the disease duration of PD was 6.8 ± 5.5 years, the H&Y stage was 2.7 ± 0.9, the UPDRS part III subscale was 10.9 ± 4.4, and the total LED was 417.2 ± 229.9 mg/day. The number of patients with motor fluctuation was 291 (62.0%). The average RBDSQ-J total score of all 469 patients was 3.7 ± 2.4, and 146 patients were classified as having pRBD (31.1%).
The differences in variables between patients with and without pRBD
Table 2 shows the comparison of the variables between the patients with and without pRBD. The averages of disease duration of PD, H&Y stage, UPDRS part III subscale, number of total motor symptoms in WOQ-19, and total LED in patients with pRBD were significantly higher than in those without pRBD, but there were no significant differences in the gender ratio or the mean age at assessment between the two groups. As to the major autonomic dysfunctions, severe constipation was diagnosed significantly more frequent in patients with pRBD than in those without it.
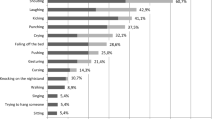
The number of patients with preceding pRBD
The number of preceding pRBD patients with respect to the interval between the onset of RBD and the appearance of motor symptoms is shown in Fig. 1. From the 146 patients with pRBD, 136 valid answers were obtained. The number of patients with preceding pRBD was 53 (39.0%). From these 53 patients, 33 valid answers concerning the age at pRBD onset were obtained. The mean age at pRBD onset was 48.0 ± 16.7 years, and the median interval from the onset of preceding pRBD to the onset of motor symptoms was 17.5 years. It is noteworthy that 3 patients had intervals of over 50 years (range: 0.6–53 years).
The differences in variables between preceding pRBD patients and non-preceding pRBD patients
We also investigated the clinical features of the patients with or without preceding pRBD (Supplementary Table 1). Most clinical characteristics, including gender, age at assessment, H&Y stage, UPDRS part III subscale, number of total motor symptoms in WOQ-19, and RBDSQ-J score were not significantly different between preceding and non-preceding pRBD patients. Age at onset of PD, disease duration of PD, and total LED were significantly different between preceding and non-preceding pRBD patients. As to autonomic dysfunctions, only hyperhidrosis showed a significant difference between preceding and non-preceding pRBD patients; however, the number of patients presenting with hyperhidrosis was small.
Discussion
The present study has described three principal findings. The first is that the prevalence of pRBD in our group of Japanese PD patients was 31.1%. The second is that pRBD significantly correlated with disease duration of PD, H&Y stage, UPDRS part III subscale, number of total motor symptoms in WOQ-19, total LED, and the presence of severe constipation. The third is that the prevalence of preceding pRBD patients was 39.0% and the median preceding interval was 17.5 years. There were 3 patients whose preceding intervals were more than 50 years.
The prevalence of iRBD is assumed to be approximately 0.5–2.0% in the general population [2–4]. On the other hand, several reports have found that 15–58% of PD patients present RBD symptoms [7, 20–22], and some studies have reported that the onset of RBD preceded the onset of neurodegenerative disorders, especially α-synucleinopathies such as PD, DLB, and MSA [5, 6, 10, 11]. Therefore, RBD is thought to be one of the premotor symptoms occurring before PD onset. In the present study, the prevalence of pRBD was similar to those in past reports. It was also reported that the median interval between the onset of RBD and that of neurodegenerative disorders including PD was 3–25 years [5, 9–13]. Moreover, Claassen [9] reported that the interval between RBD and subsequent neurologic syndrome ranged up to 50 years. Our study showed that the median interval was about 17.5 years, and 3 patients had intervals greater than 50 years.
Moreover, pRBD was significantly correlated with PD duration, H&Y stage, and total LED. Our findings are in accordance with the results of another recent study which reported that patients with PD and RBD had longer disease duration, higher H&Y stage, more falls, more fluctuations, and a higher dose of levodopa [22]. These findings suggest that a more advanced stage of neurodegeneration exists in patients with PD and RBD. This is in line with previous studies that also described motor complications [23], a higher rate of falls [24], and psychotic symptoms [25–27] in patients with PD and RBD. The higher LED in patients with PD and RBD may be seen as secondary to disease severity. The presence of RBD, which represents an abnormality in the sleep stage regulation systems [6], may correlate with the progression of PD in parallel with the more extensive Lewy body pathology.
There have been several reports showing that autonomic function is impaired in iRBD [28–38]. Therefore, we investigated the prevalence of major autonomic dysfunctions, including constipation, hyperhidrosis, urination difficulty, and urinary incontinence. Severe constipation, which is the most common autonomic dysfunction of PD, was significantly more frequent in patients with pRBD than in those without it. Although our data were not necessarily based on precise physiological examinations and were partially influenced by anti-cholinergic and dopaminergic therapy, the results of our study strongly suggested a correlation between the presence of pRBD and the severity of autonomic dysfunction in PD. Pathological and imaging studies suggest that RBD is probably related to the degeneration of brain stem nuclei involved in sleep stage regulation, namely the locus coeruleus, pedunculopontine nucleus, raphe nucleus, and substantia nigra [6]. Braak [39] reported that Lewy body pathology already existed in the dorsal nucleus of the vagal nerve, which is thought to control the movement of the gut, and in the locus coeruleus, which is thought to control sleep before the occurrence of PD. According to the hypothesis by Braak, these pontine areas correspond most closely to Braak stage 2, and RBD with Lewy pathology may be an early manifestation of PD.
It appears that RBD affects predominantly males, with an approximate male to female ratio of 9:1 based on the data from Caucasian patients [40]. Although Lin et al. [41] found a female predominance in Chinese–Taiwanese patients with RBD, Chiu et al. [4] pointed out the definite male preponderance in a survey of iRBD patients in Hong Kong. In this study surveying 1,034 elderly, 6 iRBD patients were detected (5 men and 1 woman). Therefore, the racial difference of the male preponderance in iRBD is still an unsolved issue. From our results, there was also no gender difference in Japanese PD patients with RBD. Recently, Sixel-Döring et al. [22] also reported that there was no gender preference in their PD patients with RBD.
Several limitations to our study should be noted. First, we did not include healthy age-matched control subjects or patients with idiopathic RBD. Second, the presence of RBD symptoms was investigated only by RBDSQ-J. Stiasny-Kolster [15] reported that the RBDSQ poorly discriminated patients with sleepwalking and epilepsy. In addition, we may have been unable to detect the presence of mild RBD symptoms in our subjects, and we cannot detect patients with subclinical RBD, who present only with typical PSG findings of RBD and have no clinical history of RBD. There is, thus, a possibility that the clinically evaluated frequency of RBD based on RBDSQ-J might have been underestimated in our study. Since dream enactment behavior is certainly a core feature of RBD, RBDSQ-J may have captured “severe” RBD from PD patients presenting with clinical RBD symptoms in our study. Third, a recall bias could have affected the retrospective assessment of RBD symptoms and the intervals from the onset of preceding pRBD to the PD motor symptoms.
Conclusion
Our study clarified the prevalence and clinical characteristics of Japanese PD patients presenting with pRBD symptoms in a large-scale multicenter study. The results indicated that RBD was not only a frequent non-motor symptom in patients with PD but also a premotor symptom of PD. Moreover, RBD that is characterized by an increase in the duration and severity of PD may be associated with autonomic dysfunction. Screening for RBD symptoms is recommended, especially in patients with a long PD duration and severe motor symptoms and autonomic dysfunctions.
References
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW (1986) Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep 9:293–308
Ohayon MM, Schenck CH (2010) Violent behavior during sleep: prevalence, comorbidity and consequences. Sleep Med 11:941–946
Ohayon MM, Caulet M, Priest RG (1997) Violent behavior during sleep. J Clin Psychiatry 58:369–376
Chiu HF, Wing YK, Lam LC et al (2000) Sleep-related injury in the elderly: an epidemiological study in Hong Kong. Sleep 23:513–517
Gagnon JF, Postuma RB, Mazza S et al (2006) Rapid-eye-movement sleep behaviour disorder and neurodegenerative diseases. Lancet Neurol 5:424–432
Boeve BF, Silber MH, Saper CB et al (2007) Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 130:2770–2788
Gagnon JF, Bedard MA, Fantini ML et al (2002) REM sleep behavior disorder and REM sleep without atonia in Parkinson’s disease. Neurology 59:585–589
Postuma RB, Gagnon JF, Vendette M et al (2009) Idiopathic REM sleep behavior disorder in the transition to degenerative disease. Mov Disord 15:2225–2232
Claassen DO, Josephs KA, Ahrlskog JE, Silber MH, Tippmann-Peikert M, Boeve BF (2010) REM sleep behavior disorder preceding other aspects of synucleinopathies by up to half a century. Neurology 75:494–499
Schenck CH, Budlie SR, Mahowald MW (2003) REM behavior disorder (RBD): delayed emergence of parkinsonism and/or dementia in 65% of older men initially diagnosed with idiopathic RBD, and analysis of the minimum and maximum tonic and/or phasic electromyographic abnormalities found during REM sleep. Sleep 26:A316
Iranzo A, Molinuevo JL, Santamaria J, Serradell M, Marti MJ et al (2006) Rapid-eye movement sleep behaviour disorder as an early marker for a neurodegenerative disorder: a descriptive study. Lancet Neurol 5:572–577
Schenck CH, Bundlie SR, Mahowald MW (1996) Delayed emergence of a parkinsonian disorder in 38% of 29 older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder. Neurology 46:388–393
Olson EJ, Boeve BF, Silber MH (2000) Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain 123:331–339
American Academy of Sleep Medicine (2005) International classification of sleep disorders, 2nd edn. Diagnostic and coding manual. Westchester, Illinois, pp 177–180
Stiasny-Kolster K, Mayer G, Schäfer S et al (2007) The REM sleep behavior disorder screening questionnaire: a new diagnostic instrument. Mov Disord 22:2386–2393
Miyamoto T, Miyamoto M, Iwanami M et al (2009) The REM sleep behavior disorder screening questionnaire: validation study of Japanese version. Sleep Med 10:1151–1154
American Psychiatric Association Committee on Nomenclature, Statistics (1994) Diagnostic and statistical manual of mental disorders (DSM-IV), 4th edn. American Psychiatric Association, Washington, DC
Hughes AJ, Daniel SE, Kilford L et al (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinio–pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Stacy M, Hauser R (2007) Development of a patient questionnaire to facilitate recognition of motor and non-motor wearing-off in Parkinson’s disease. J Neural Transm 114:211–217
Comella CL, Nardine TM, Diederich NJ, Stebbins GT (1998) Sleep-related violence, injury, and REM sleep behavior disorder in Parkinson’s disease. Neurology 51:526–529
Scaglione C, Vignatelli L, Plazzi G, Marchese R, Negrotti A, Bologna, Genova, Parma and Pisa Universities group for the study of REM sleep behavior disorder in Parkinson’s disease et al (2005) REM sleep behaviour disorder in Parkinson’s disease: a questionnaire-based study. Neurol Sci 25:316–321
Sixel-Döring F, Trautmann E, Mollenhauer B, Trenkwalder C (2011) Associated factors for REM sleep behavior disorder in Parkinson disease. Neurology 77:1048–1054
Ozekmekçi S, Apaydin H, Kiliç E (2005) Clinical features of 35 patients with Parkinson’s disease displaying REM behavior disorder. Clin Neurol Neurosury 107:306–309
Postuma RB, Gagnon JF, Vendette M, Charland K, Montplaisir J (2008) REM sleep behaviour disorder in Parkinson’s disease is associated with specific motor features. J Neurol Neurosurg Psychiatry 79:1117–1121
Sinforiani E, Pacchetti C, Zangaglia R, Pasotti C, Manni R, Nappi G (2008) REM behavior disorder, hallucinations and cognitive impairment in Parkinson’s disease: a two-year follow up. Mov Disord 23:1441–1445
Onofrj M, Thomas A, D’Andreamatteo G, Iacono D, Luciano AL, Di Rollo A, Di Mascio R, Ballone E, Di Iorio A (2002) Incidence of RBD and hallucination in patients affected by Parkinson’s disease: 8-year follow-up. Neurol Sci 23(Suppl 2):S91–S94
Pacchetti C, Manni R, Zangaglia R, Mancini F, Marchioni E, Tassorelli C, Terzaghi M, Ossola M, Martignoni E, Moglia A, Nappi G (2005) Relationship between hallucinations, delusions, and rapid eye movement sleep behavior disorder in Parkinson’s disease. Mov Disord 20:1439–1448
Orimo S, Ozawa E, Nakade S, Sugimoto T, Mizusawa H (1999) 123I-metaiodobenzylguanidine myocardial scintigraphy in Parkinson’s disease. J Neurol Neurosurg Psychiatry 67:189–194
Miyamoto T, Miyamoto M, Inoue Y, Usui Y, Suzuki K, Hirata K (2006) Reduced cardiac 123I-MIBG scintigraphy in idiopathic REM sleep behavior disorder. Neurology 67:2236–2238
Kashihara K, Imamura T, Shinya T (2010) Cardiac 123I-MIBG uptake is reduced more markedly in patients with REM sleep behavior disorder than in those with early stage Parkinson’s disease. Parkinsonism Relat Disord 16:252–255
Kashihara K, Imamura T (2007) Reduced myocardial 123I-MIBG uptake in a patient with idiopathic rapid eye movement sleep behavior disorder. Mov Disord 22:150–151
Koyama S, Tachibana N, Masaoka Y, Homma I, Kawamura M (2007) Decreased myocardial 123I-MIBG uptake and impaired facial expression recognition in a patient with REM sleep behavior disorder. Mov Disord 22:746–747
Lanfranchi PA, Fradette L, Gagnon JF, Colombo R, Montplaisir J (2007) Cardiac autonomic regulation during sleep in idiopathic REM sleep behavior disorder. Sleep 30:1019–1025
Postuma RB, Lanfranchi PA, Blais H, Gagnon JF, Montplaisir JY (2010) Cardiac autonomic dysfunction in idiopathic REM sleep behavior disorder. Mov Disord 25:2304–2310
Haapaniemi TH, Pursiainen V, Korpelainen JT, Huikuri HV, Sotaniemi KA, Myllyla VV (2001) Ambulatory ECG and analysis of heart rate variability in Parkinson’s disease. J Neurol Neurosurg Psychiatry 70:305–310
Postuma RB, Gagnon JF, Vendette M, Charland K, Montplaisir J (2008) Manifestations of Parkinson disease differ in association with REM sleep behavior disorder. Mov Disord 23:1665–1672
Ferini-Strambi L, Oldani A, Zucconi M, Smirne S (1996) Cardiac autonomic activity during wakefulness and sleep in REM sleep behavior disorder. Sleep 19:367–369
Fantini ML, Michaud M, Gosselin N, Lavigne G, Montplaisir J (2002) Periodic leg movements in REM sleep behavior disorder and related autonomic and EEG activation. Neurology 59:1889–1894
Braak H, Del Tredici K, Rub U et al (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Schenck CH, Mahowald MW (1990) Polysomnographic, neurologic, psychiatric, and clinical outcome report on 70 consecutive cases with REM sleep behavior disorder (RBD): sustained clonazepam efficacy in 89.5% of 57 treated patients. Clevel Clin J Med 57:S9–S23
Lin FC, Lai CL, Huang P, Liu CK, Hsu CY (2009) The rapid-eye-movement sleep behavior disorder in Chinese–Taiwanese patients. Psychiatry Clin Neurosci 63:557–562
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of Keio Parkinson’s Disease Database.
A list of the members of the Keio Parkinson’s Disease database is provided in Appendix.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The members of the Keio Parkinson’s Disease database are: Chair: Norihiro Suzuki, MD, PhD, Keio University School of Medicine, Tokyo, Japan. Members: Yoshihiro Nihei, MD, Keio University of Medicine, Tokyo, Japan; Kazushi Takahashi, MD, PhD, Keio University of Medicine, Tokyo, Japan; Atsuo Koto, MD, PhD, Yomiuri Land Keiyu Hospital, Tokyo, Japan; Ban Mihara, MD, PhD, Mihara Memorial Hospital, Gunma, Japan; Kyoko Gotoh, MD, National Hospital Organization Tokyo Medical Center, Tokyo, Japan; Daisuke Yasutomi, MD, PhD, National Hospital Organization Tokyo Medical Center, Tokyo, Japan; Yoko Morita, MD, PhD, National Hospital Organization Tokyo Medical Center; Taro Kadowaki, MD, PhD, Ashikaga Red Cross Hospital, Tochigi, Japan; Kazuo Isozumi, MD, PhD, Ashikaga Red Cross Hospital, Tochigi, Japan; Satoru Komatsumoto, MD, PhD, Ashikaga Red Cross Hospital, Tochigi, Japan; Kouichi Ohta, MD, PhD, Tachikawa Hospital, Tokyo, Japan; Yukito Shinohara, MD, PhD, Tachikawa Hospital, Tokyo, Japan; Kazuhiro Muramatsu, MD, PhD, Saiseikai Yokohama-city Eastern Hospital, Kanagawa, Japan; Masaya Kunimoto, MD, PhD, Yokohama-city Eastern Hospital, Yokohama, Japan; Jun Gotoh, MD, PhD, Saiseikai Central Hospital, Tokyo, Japan; Makoto Takagi, MD, PhD, Saiseikai Central Hospital, Tokyo, Japan; Keiji Yamaguchi, MD, PhD, Mito Red Cross Hospital, Ibaraki, Japan; Katsuyuki Obara, MD, PhD, Mito Red Cross Hospital, Ibaraki, Japan; Yutaka Tomita, MD, PhD, Tomita Hospital, Aichi, Japan; Hideki Sato, MD, Saitama Municipal Hospital, Saitama, Japan; Hidenori Hattori MD, PhD, Saitama Municipal Hospital, Saitama, Japan; Fumio Yoshikawa MD, PhD, Saitama Municipal Hospital, Saitama, Japan; Morinobu Seki, MD, Keio University of Medicine, Tokyo, Japan; Satoko Iwasawa, MD, PhD, Keio University of Medicine, Tokyo, Japan.
Rights and permissions
About this article
Cite this article
Nihei, Y., Takahashi, K., Koto, A. et al. REM sleep behavior disorder in Japanese patients with Parkinson’s disease: a multicenter study using the REM sleep behavior disorder screening questionnaire. J Neurol 259, 1606–1612 (2012). https://doi.org/10.1007/s00415-011-6386-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6386-1