Abstract
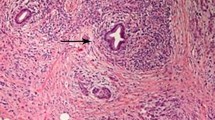
Autoimmune pancreatitis (AIP) is a recently recognized disease affecting the pancreas. It closely mimics pancreatic cancer in presentation. In fact, pancreatic resections performed for presumed pancreatic cancer have historically played a key role in recognition of this disease entity. Characterized by distinct histological features in the pancreas which has formed the basis of diagnosis for a majority of patients historically, increased recognition of this disease has led to development of diagnostic criteria. In the USA, the HISORt criteria introduced in 2006 has formed the backbone of diagnosing this disease. Recently, international consensus criteria have been developed incorporating experiences and practices from across the world. With increasing experience of this disease, treatment and follow-up strategies have now emerged. The disease is characteristically responsive to steroid treatment. However, relapses are common. Interestingly, two groups of AIP patients were observed with distinct patterns of relapse and corresponding distinctive histological and clinical features. This led to subclassification of AIP into two subtypes: type 1 in which relapses are common and histologically corresponding to lymphoplasmacytic sclerosing pancreatitis (LPSP) with IgG4 positivity and type 2 in which relapses are rare and histologically characterized by granulocyte epithelial lesions (GELs). Long-term follow-up data have now established that despite relapses, AIP is a benign disease which does not affect overall survival.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pancreatic Cancer
- Autoimmune Pancreatitis
- Serum IgG4 Elevation
- Ductal Imaging
- Minimum Diagnostic Criterion
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Autoimmune pancreatitis (AIP) is a fibroinflammatory disease of the pancreas which has been recognized and characterized predominantly in the last decade. Previous chapters in this book have introduced and extensively presented the features, associations, diagnosis, treatment, and prognosis of AIP. In this chapter, we aim to provide the readers with a historical account of recognition of AIP and developments regarding this disease in the USA. Further, we will summarize the profile of AIP patients in the USA and discuss clinical practice in the USA regarding their diagnosis and management highlighting the salient differences with respect to the Japanese and Korean practice guidelines.
Progress in AIP: A Historical Perspective
Earliest account of the fibrosclerosing disease of the pancreas with marked inflammatory infiltrate that retrospectively appears to be AIP can be traced back to 1960s by the French group of Sarles et al. [1, 2] which were grouped under chronic inflammatory pancreatitis in the 1988 Marseilles-Rome Pancreatitis Classification [3]. The term autoimmune pancreatitis was introduced in 1995 by Yoshida et al. based on autoimmune etiology-suggestive associations identified in their Japanese cohort [4]. In 1997, the term nonalcoholic duct destructive pancreatitis (NADDP) was used by Ectors et al. [5] in their European cohort. The Japanese formalized their experience with AIP with the development of JPS minimum diagnostic criteria by 2002 [6] after publication of several Japanese cohorts [7–11] including the recognition of serum immunoglobulin subtype 4 (IgG4) elevations [11].
In this section, we will continue the discussion on the historical developments in the USA. While we aim to highlight key contributions from the USA, this is by no means intended to undermine contributions from across the globe which have been extensively reviewed in the preceding chapters and the following chapter on AIP in Europe.
Early Reports of Multifocal Fibrosis from the USA
In 1963, Bartholomew et al. [12] described two cases from Mayo Clinic of sclerosing cholangitis with fibrosis affecting multiple organs. This report had first descriptions of steroid responsiveness and of the recognition that multiple affected organs were manifestations of a single systemic disease. Hache et al. [13] described a cohort of 20 patients from Mayo Clinic in 1962 with fibrosing mediastinitis noting lymphocytic and plasma cell infiltration in the fibrotic tissue. In 1965, another report of sclerosing cholangitis with involvement of other organs appeared which was novel in observing elevation of gamma globulin associated with this disease [14]. The term multifocal fibrosclerosis was introduced in 1967 by Comings et al. [15] emphasizing the association of sclerosing fibrotic disease of multiple organs. Reports of multifocal fibrosclerosis continued to appear in the subsequent years [16–18] including descriptions of pancreatitis in patients with Sjogren’s syndrome (reports from the UK) [19, 20], pancreatic pseudotumor [21], and pancreatic fibrosis in multifocal fibrosclerosis and of duct destructive pancreatitis [22]. Notably, these early reports from pre-AIP recognition era were keen on observing many of the key features of what is now recognized as IgG4-related disease (discussed below) including steroid responsiveness.
Surgical Resection of Pancreatic Mass Mimicking Pancreatic Cancer
Although the existence of AIP as a disease entity was not yet fully established among the US pancreatologists, the possibility of an autoimmune chronic pancreatitis was being increasingly appreciated by 2001. This is reflected in the inclusion of an autoimmune category in the TIGAR-O etiological classification of chronic pancreatitis proposed by Whitcomb et al. in 2001 [23]. It was in the year 2003 that the first sizeable cohorts of AIP were published in the USA from Mayo Clinic [24], Memorial Sloan Kettering Cancer Center [25], and Johns Hopkins Medical School [26].
It is now well recognized that the presentation of AIP mimics that of pancreatic cancer. Not surprisingly, most of the early work on AIP globally was based on retrospective analysis of pancreas resected for presumed pancreatic cancer which turned out noncancerous. The MSKCC cohort described 31 patients with LPSP identified from 1,287 pancreatic resections performed for presumed pancreatic cancer from 1985 to 2001 [25]. The Johns Hopkins cohort described 37 patients with LPSP identified from 1,648 pancreatic resections performed for presumed pancreatic cancer from 1992 to 2002 [26]. In the Mayo Clinic cohort, 35 patients with AIP were identified based on review of pancreatic resections between 1985 and 2002 [24].
Recognition of a New Disease
These first US cohorts of AIP published in 2003 [24–26] served to capture useful data on the clinical presentation, imaging features, histological features, and postsurgical prognosis. The relatively large cohort data [24–26] helped consolidate experiences of experts from multiple centers around the world regarding the existence of this new disease entity and its features. Although AIP was well accepted in Japan by 2003, the defining features of AIP were not fully established. With data from only small case series, there remained a significant risk of enthusiastic overdiagnosis including the dreaded mistake of misdiagnosing pancreatic cancer as AIP. This was well appreciated by the experts who debated the existence of this novel disease entity and its defining features at the American Pancreatic Association Meeting held in the same year (2003) [27]. A global consensus of recognition of AIP as a distinct disease entity emerged as a result [27]. Further, a preliminary set of the defining features of AIP was also agreed upon, with recognition of the need for caution in its diagnosis due to the dreaded consequences of misdiagnoses, and the need for further data [27].
Formulation of Criteria for Diagnosis
The minimum diagnostic criteria of Japanese Pancreatic Society (JPS) (2002) were based on parenchymal and ductal imaging and histology features [6]. Emerging data over the next few years showed multiple extrapancreatic organ involvement in AIP patients (termed other organ involvement), in association with elevated serum IgG4 levels and responsiveness to steroids [28]. Further, in the cohort of AIP defined by histological criteria at Mayo Clinic, wide spectrum of clinical and imaging features were seen which would otherwise not be captured by the minimum diagnostic criteria of JPS [28]. Based on this cohort of histologically confirmed cases at Mayo Clinic, the HISORt criteria were formulated in 2006 [28]. This included Histology, Imaging (parenchymal), Serology (IgG4 elevation), Other organ involvement and Response to treatment with steroids. These criteria were validated in the Mayo Clinic cohort and demonstrated to identify the full spectrum of clinical presentation of AIP [28]. The HISORt criteria continue to form the backbone of AIP diagnosis in the USA which has also been utilized in multiple subsequent published AIP cohorts [29, 30].
Multiple other diagnostic criteria have subsequently emerged from Korea [31], Europe [32], revisions of JPS criteria [33], and combined Asian criteria [34]. These criteria reflect regional variations in practice patterns as well as possible differences in clinical profile and epidemiology. Existence of multiple diagnostic criteria increases the risk of misdiagnosis due to potential diagnostic loopholes as some criteria seem more relaxed and flexible [35]. Further, these criteria, including the HISORt criteria, were not aimed at differentiating the AIP subtypes which were subsequently recognized as described below. In 2009, the revised HISORt criteria were published to differentiate AIP from pancreatic cancer [36]. These criteria were validated in a cohort of AIP and pancreatic cancer patients.
With new developments in the field of AIP as described below which included consensus on the histological and clinical features of AIP subtypes (2009–2011) [37–39], a consensus on the diagnostic criteria for AIP was reached in 2011 [40]. The International Consensus Diagnostic Criteria (ICDC) [40] incorporates most of the features of the revised HISORt criteria [36] and combines the salient features of Asian/Japanese criteria [6, 34] that include ductal imaging (ERP/MRP) as well as ampullary biopsies with IgG4 staining. The ICDC provides a unified framework that allows for regional flexibility in establishing an institutional approach for diagnosing AIP based on available expertise and local practice pattern [40], as discussed in the clinical practice section.
Other Organ Involvement and Recognition of IgG4-Related Disease (IgG4-RD)
Multiple extrapancreatic organ involvement was consistently observed in AIP patients across all cohorts globally [41–45] including the first US cohorts of 2003 [24–26] and other studies published subsequently [28–30, 46–48]. While the syndrome of multifocal fibrosclerosis had been recognized as described earlier, the association between extrapancreatic organ involvement of AIP and multifocal fibrosclerosis was not clear.
The study of Notohara et al. in 2003 suggested that LPSP, but not ICDP (recognition of the two subtypes discussed below), was associated with multiple extrapancreatic manifestations which were likely related to the entity of multifocal fibrosclerosis recognized previously [24]. In the same year, Kamisawa et al. showed that the multiple extrapancreatic organs demonstrated infiltration with IgG4-positive plasma cells similar to that in the pancreas suggesting that AIP and multifocal fibrosclerosis were related [49, 50]. Subsequently, it became clear that distinct histological changes identical to LPSP are seen in the extrapancreatic organs affected in multifocal fibrosclerosis [51]. As the affected organs consistently demonstrate IgG4-rich lymphoplasmacytic infiltrate, the concept of IgG4-related systemic disease was proposed in 2004 by Kamisawa et al. [51, 52]. Multiple organ associations perhaps encompassing all major organs have now been reported with a variety of names [53]. A consensus on nomenclature and definitions has been reached in 2012 [54], which terms this newly characterized systemic disease as IgG4-related disease (IgG4-RD) of which type 1 AIP (histological counterpart, LPSP) is the pancreatic manifestation.
Differentiating AIP from Pancreatic Cancer
Unnecessary surgical treatment can be avoided with a correct and timely diagnosis of AIP. On the other hand, since pancreatic cancer is relatively more common, there is a risk of misdiagnosing pancreatic cancer as AIP which is of grave clinical consequence as discussed in the diagnostic criteria section. Recognition of serum IgG4 elevation in AIP led to this test being proposed for distinguishing AIP from pancreatic cancer [11]. The diagnostic utility of serum IgG4 levels in differentiating AIP from pancreatic cancer was examined by Ghazale et al. in the Mayo Clinic cohort in 2007 [55]. This study found that serum IgG4 elevations (>140 mg/dl) are seen in 70–80 % of AIP patients and also in 5 % of normal population and 10 % of pancreatic cancer making it an unsuitable single marker for diagnosis [55]. Meanwhile, a strategy of 2-week steroid trial was proposed by the Korean group to differentiate AIP from pancreatic cancer [56]. However, unrestricted use of steroid trial posed a serious risk of misdiagnosis [35].
The revised HISORt criteria were formed in 2009 [36], combining the diagnostic potential of serum IgG4 with other features of AIP, and incorporated strict criteria for diagnostic use of steroid trial. These criteria were validated in a cohort of AIP and pancreatic cancer patients with 100 % sensitivity and specificity for AIP [36]. Based on the criteria, a diagnostic strategy to differentiate AIP from pancreatic cancer was proposed in 2009 [36, 57]. As described earlier, the revised HISORt criteria were incorporated into ICDC and a revised diagnostic strategy based on ICDC for distinguishing AIP from pancreatic cancer has subsequently been published [58].
Recognition of AIP Subtypes
The cohort of Notohara et al. (2003) recognized two distinct histological patterns – 23 with LPSP and 13 with IDCP among the 35 patients [24]. Two histologically distinct groups based on presence of GELs (GEL-positive cases being identical to IDCP) were also reported in the European cohort of 53 patients published in the same year [43].
While multiple extrapancreatic manifestations had been recognized in AIP patients in Asian, European, and American cohorts, Notohara et al. noted that LPSP, but not IDCP, is associated with extrapancreatic organ involvement similar to multifocal fibrosis [24]. Further, IBD was noted to be associated with GEL-positive AIP (IDCP) in the European cohort [43].
As long-term follow-up data became available in the Mayo Clinic cohort published in 2010 [47], it was clear that LPSP but not IDCP is associated with frequent relapses. In addition, in this cohort, clinical features of these two subtypes were directly compared noting salient differences [47]. This study established that IgG4 elevations in the serum are seen in LPSP but not in IDCP, IgG4-related other organ involvement is seen in LPSP but not IDCP, and patients with IDCP are younger and are more likely to present with acute pancreatitis compared to LPSP and more likely to have focal findings on parenchymal imaging [47]. Thus, it was clear that distinct histological subtypes LPSP and IDCP had distinctive clinical correlates [47]. This was debated in the joint meeting of APA and JPS in 2009, leading to the consensus of recognizing two subtypes of AIP with the abovementioned clinical phenotypes termed type 1 and type 2 AIP, respectively [37].
The histological diagnostic criteria for LPSP and IDCP were reviewed and consensus reached in 2010–2011 [37–39]. These paved way for the consensus diagnostic criteria of 2011 described previously [40].
Strategies for Treatment
The incidence of surgical resections has declined significantly after 2003 with increasing recognition of this disease [48]. However, strategies of steroid treatment have been highly variable across centers and regions. Our strategy of steroid treatment with short course followed by taper after disease remission (details discussed below) was optimized and validated in the Mayo Clinic cohort published in 2007 [59]. The use of immunomodulators for maintenance treatment for relapsing and use of rituximab for refractory disease or as steroid-sparing agent have been described in Hart et al. [60] recently and discussed elsewhere in this book.
Long-Term Follow-Up Results
Long-term follow-up data from the Mayo Clinic cohort were first published for the IgG4-associated cholangitis (IAC) cohort in 2008 [46] and for AIP cohort in 2010 [47] and 2012 [48]. These studies showed that relapses are common in type 1 AIP but not in type 2 AIP, and patients with IAC (or proximal bile duct involvement) have a much higher risk of relapse. An updated data on relapse rates in AIP in our cohort is shown in Fig. 28.1. Importantly, when long-term survival of AIP patients was compared to matched general population, no differences were found which for the first time showed the benign long-term prognosis of both subtypes of AIP [47]. Cumulative incidence of malignancies was observed in the recent international multicenter cohort of AIP [48] but no matched controls were available to compare the cumulative risk of cancer. Another recent study from the Mayo Clinic cohort showed no increase in immediate pre- or post-diagnosis risk of cancers compared to matched controls [61].
Profile of AIP in the USA
Clinical Practices Regarding AIP in the USA
In this section, we summarize the salient differences in clinical practices regarding diagnosis and management of AIP in the USA as compared to Asian/Japanese strategy described in separate chapters in this book.
Diagnosis of AIP
One important difference in the diagnosis strategy lies in the utility of pancreatic core biopsies. EUS-guided pancreatic core biopsies are routinely performed at our center [63] and have also been routinely done at many other centers in the USA [64]. These are included in the HISORt criteria [28, 36]. In contrary, core biopsies are not performed frequently in Japan and thereby not required in the Asian and Japanese criteria [6, 34].
Another major contention is in the use of ductal imaging (ERP/MRP). The HISORt criteria [28, 36] does not require for ERP/MRP, while the Asian and Japanese criteria require pancreatic duct imaging by ERP/MRP [6, 34]. In the USA, routine ERP/MRP is not performed of obstructive jaundice. The diagnostic utility of ERP from the diagnosis of AIP and differentiating it from pancreatic cancer in the USA was not satisfactory in contrary to that observed in the Japanese centers [65].
The ICDC [40] includes ERP as an additional option which could supplement evidence in favor of AIP to qualify patients for a steroid trial who would otherwise need to be subjected to core biopsy. This is applicable to patients who do not have highly supportive parenchymal imaging and have some collateral evidence (other organ involvement or serum IgG4 elevations) but not sufficient for meeting criteria [40]. In our experience, only 10 % of patients would fall in this category who could be subjected to ductal imaging or core biopsy for diagnosis by ICDC thereby allowing for regional flexibility. About 20 % of patients do not have any collateral evidence and histological diagnosis is mandated in these patients regardless of parenchymal or ductal imaging.
Treatment and Follow-Up of AIP
Our protocol for initial steroid treatment is as follows: prednisone 40 mg/day for 4 weeks and tapering off by 5 mg/week to complete a course of 11 weeks. Treatment response is objectively monitored by clinical follow-up, follow-up imaging, and biochemical tests (LFT). Steroid taper is started once response to treatment is confirmed objectively [59, 60].
In our experience, about half of type 1 AIP patients do not relapse after short course of steroid treatment [60]. No maintenance therapy is necessary in these patients [60]. The major difference from Asian strategy is the need for maintenance steroid therapy [66]. Centers in Japan routinely use a prolonged maintenance therapy for up to 3 years with the logic that most patients relapse within 3 years [66]. In a multicenter study from Japan, it was shown that maintenance therapy reduced the relapse rate to 23 % from 34 % in those who weaned off steroids [66]. In our experience, the risks of universal use of maintenance steroid therapy outweigh the benefits in AIP.
Our strategy for follow-up for relapses involves close monitoring of symptoms with radiological and biochemical confirmation of relapse if symptomatic [60]. Early detection of relapses and prompt institution of treatment are recommended. Steroid retreatment with or without immunomodulators, rituximab treatment, and maintenance therapy with these agents may be necessary in 30–40 % of AIP patients with frequent relapses or refractory disease or steroid intolerance [60]. Details of treatment of relapses and maintenance therapy options are discussed extensively in an earlier chapter.
Conclusion
AIP is a fibroinflammatory disease affecting the pancreas which has recently been characterized. We have described the historical aspects, clinical profile, and practice patterns regarding AIP in the USA.
References
Sarles H, Sarles JC, Muratore R, et al. Chronic inflammatory sclerosis of the pancreas – an autonomous pancreatic disease? Am J Dig Dis. 1961;6:688–98.
Sarles H, Sarles JC, Camatte R, et al. Observations on 205 confirmed cases of acute pancreatitis, recurring pancreatitis, and chronic pancreatitis. Gut. 1965;6(6):545–59.
Sarles H, Adler G, Dani R, et al. The pancreatitis classification of Marseilles-Rome 1988. Scand J Gastroenterol. 1989;24(6):641–2.
Yoshida K, Toki F, Takeuchi T, et al. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40(7):1561–8.
Ectors N, Maillet B, Aerts R, et al. Non-alcoholic duct destructive chronic pancreatitis. Gut. 1997;41(2):263–8.
Society MotCCfAPotJP. Diagnostic criteria for autoimmune pancreatitis by the Japan Pancreas Society. J Jpn Pancreas Soc. 2002;17:585–7.
Uchida K, Okazaki K, Konishi Y, et al. Clinical analysis of autoimmune-related pancreatitis. Am J Gastroenterol. 2000;95(10):2788–94.
Okazaki K, Uchida K, Ohana M, et al. Autoimmune-related pancreatitis is associated with autoantibodies and a Th1/Th2-type cellular immune response. Gastroenterology. 2000;118(3):573–81.
Tanaka S, Kobayashi T, Nakanishi K, et al. Corticosteroid-responsive diabetes mellitus associated with autoimmune pancreatitis. Lancet. 2000;356(9233):910–1.
Ito T, Nakano I, Koyanagi S, et al. Autoimmune pancreatitis as a new clinical entity. Three cases of autoimmune pancreatitis with effective steroid therapy. Dig Dis Sci. 1997;42(7):1458–68.
Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344(10):732–8.
Bartholomew LG, Cain JC, Woolner LB, et al. Sclerosing cholangitis: its possible association with Riedel’s struma and fibrous retroperitonitis. Report of two cases. N Engl J Med. 1963;269:8–12.
Hache L, Woolner LB, Bernatz PE. Idiopathic fibrous mediastinitis. Dis Chest. 1962;41:9–25.
Wenger J, Gingrich GW, Mendeloff J. Sclerosing cholangitis – a manifestation of systemic disease. Increased serum gamma-globulin, follicular lymph node hyperplasia, and orbital pseudotumor. Arch Intern Med. 1965;116(4):509–14.
Comings DE, Skubi KB, Van Eyes J, et al. Familial multifocal fibrosclerosis. Findings suggesting that retroperitoneal fibrosis, mediastinal fibrosis, sclerosing cholangitis, Riedel’s thyroiditis, and pseudotumor of the orbit may be different manifestations of a single disease. Ann Intern Med. 1967;66(5):884–92.
Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 6-1982. A 55-year-old man with eight months of obstructive jaundice. N Engl J Med. 1982;306(6):349–58.
Meijer S, Hoitsma HF, Scholtmeijer R. Idiopathic retroperitoneal fibrosis in multifocal fibrosclerosis. Eur Urol. 1976;2(5):258–60.
Meyer S, Hausman R. Occlusive phlebitis in multifocal fibrosclerosis. Am J Clin Pathol. 1976;65(3):274–83.
Waldram R, Kopelman H, Tsantoulas D, et al. Chronic pancreatitis, sclerosing cholangitis, and sicca complex in two siblings. Lancet. 1975;1(7906):550–2.
Sood S, Fossard DP, Shorrock K. Chronic sclerosing pancreatitis in Sjogren’s syndrome: a case report. Pancreas. 1995;10(4):419–21.
Clark A, Zeman RK, Choyke PL, et al. Pancreatic pseudotumors associated with multifocal idiopathic fibrosclerosis. Gastrointest Radiol. 1988;13(1):30–2.
Scully KA, Li SC, Hebert JC, et al. The characteristic appearance of non-alcoholic duct destructive chronic pancreatitis: a report of 2 cases. Arch Pathol Lab Med. 2000;124(10):1535–8.
Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 2001;120(3):682–707.
Notohara K, Burgart LJ, Yadav D, et al. Idiopathic chronic pancreatitis with periductal lymphoplasmacytic infiltration: clinicopathologic features of 35 cases. Am J Surg Pathol. 2003;27(8):1119–27.
Weber SM, Cubukcu-Dimopulo O, Palesty JA, et al. Lymphoplasmacytic sclerosing pancreatitis: inflammatory mimic of pancreatic carcinoma. J Gastrointest Surg. 2003;7(1):129–37; discussion 37–9.
Hardacre JM, Iacobuzio-Donahue CA, Sohn TA, et al. Results of pancreaticoduodenectomy for lymphoplasmacytic sclerosing pancreatitis. Ann Surg. 2003;237(6):853–8; discussion 8–9.
Pearson RK, Longnecker DS, Chari ST, et al. Controversies in clinical pancreatology: autoimmune pancreatitis: does it exist? Pancreas. 2003;27(1):1–13.
Chari ST, Smyrk TC, Levy MJ, et al. Diagnosis of autoimmune pancreatitis: the Mayo Clinic experience. Clin Gastroenterol Hepatol. 2006;4(8):1010–6; quiz 934.
Raina A, Yadav D, Krasinskas AM, et al. Evaluation and management of autoimmune pancreatitis: experience at a large US center. Am J Gastroenterol. 2009;104(9):2295–306.
Clark CJ, Morales-Oyarvide V, Zaydfudim V, et al. Short-term and long-term outcomes for patients with autoimmune pancreatitis after pancreatectomy: a multi-institutional study. J Gastrointest Surg. 2013;17(5):899–906.
Kim MH, Kwon S. Diagnostic criteria for autoimmune chronic pancreatitis. J Gastroenterol. 2007;42 Suppl 18:42–9.
Schneider A, Lohr JM, Singer MV. The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classifications of the disease. J Gastroenterol. 2007;42(2):101–19.
Okazaki K, Kawa S, Kamisawa T, et al. Japanese consensus guidelines for management of autoimmune pancreatitis: I. Concept and diagnosis of autoimmune pancreatitis. J Gastroenterol. 2010;45(3):249–65.
Otsuki M, Chung JB, Okazaki K, et al. Asian diagnostic criteria for autoimmune pancreatitis: consensus of the Japan-Korea Symposium on Autoimmune Pancreatitis. J Gastroenterol. 2008;43(6):403–8.
Gardner TB, Levy MJ, Takahashi N, et al. Misdiagnosis of autoimmune pancreatitis: a caution to clinicians. Am J Gastroenterol. 2009;104(7):1620–3.
Chari ST, Takahashi N, Levy MJ, et al. A diagnostic strategy to distinguish autoimmune pancreatitis from pancreatic cancer. Clin Gastroenterol Hepatol. 2009;7(10):1097–103.
Chari ST, Kloeppel G, Zhang L, et al. Histopathologic and clinical subtypes of autoimmune pancreatitis: the Honolulu consensus document. Pancreas. 2010;39(5):549–54.
Kloppel G, Detlefsen S, Chari ST, et al. Autoimmune pancreatitis: the clinicopathological characteristics of the subtype with granulocytic epithelial lesions. J Gastroenterol. 2010;45(8):787–93.
Levy MJ, Smyrk TC, Takahashi N, et al. Idiopathic duct-centric pancreatitis: disease description and endoscopic ultrasonography-guided trucut biopsy diagnosis. Pancreatology. 2011;11(1):76–80.
Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40(3):352–8.
Frulloni L, Scattolini C, Falconi M, et al. Autoimmune pancreatitis: differences between the focal and diffuse forms in 87 patients. Am J Gastroenterol. 2009;104(9):2288–94.
Church NI, Pereira SP, Deheragoda MG, et al. Autoimmune pancreatitis: clinical and radiological features and objective response to steroid therapy in a UK series. Am J Gastroenterol. 2007;102(11):2417–25.
Zamboni G, Luttges J, Capelli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch. 2004;445(6):552–63.
Ryu JK, Chung JB, Park SW, et al. Review of 67 patients with autoimmune pancreatitis in Korea: a multicenter nationwide study. Pancreas. 2008;37(4):377–85.
Maire F, Le Baleur Y, Rebours V, et al. Outcome of patients with type 1 or 2 autoimmune pancreatitis. Am J Gastroenterol. 2011;106(1):151–6.
Ghazale A, Chari ST, Zhang L, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology. 2008;134(3):706–15.
Sah RP, Chari ST, Pannala R, et al. Differences in clinical profile and relapse rate of type 1 versus type 2 autoimmune pancreatitis. Gastroenterology. 2010;139(1):140–8; quiz e12–3.
Hart PA, Kamisawa T, Brugge WR, et al. Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 2013;62(12):1771–6.
Kamisawa T, Funata N, Hayashi Y, et al. Close relationship between autoimmune pancreatitis and multifocal fibrosclerosis. Gut. 2003;52(5):683–7.
Kamisawa T. IgG4-positive plasma cells specifically infiltrate various organs in autoimmune pancreatitis. Pancreas. 2004;29(2):167–8.
Kamisawa T, Funata N, Hayashi Y. Lymphoplasmacytic sclerosing pancreatitis is a pancreatic lesion of IgG4-related systemic disease. Am J Surg Pathol. 2004;28(8):1114.
Kamisawa T, Nakajima H, Egawa N, et al. IgG4-related sclerosing disease incorporating sclerosing pancreatitis, cholangitis, sialadenitis and retroperitoneal fibrosis with lymphadenopathy. Pancreatology. 2006;6(1–2):132–7.
Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366(6):539–51.
Stone JH, Khosroshahi V, Deshpande V. IgG4-related disease: recommendations for the nomenclature of this condition and its individual organ system manifestations. Arthritis Rheum. 2012;64(10):3061–7.
Ghazale A, Chari ST, Smyrk TC, et al. Value of serum IgG4 in the diagnosis of autoimmune pancreatitis and in distinguishing it from pancreatic cancer. Am J Gastroenterol. 2007;102(8):1646–53.
Moon SH, Kim MH, Park DH, et al. Is a 2-week steroid trial after initial negative investigation for malignancy useful in differentiating autoimmune pancreatitis from pancreatic cancer? A prospective outcome study. Gut. 2008;57(12):1704–12.
Sugumar A, Chari ST. Distinguishing pancreatic cancer from autoimmune pancreatitis: a comparison of two strategies. Clin Gastroenterol Hepatol. 2009;7(11 Suppl):S59–62.
Sah RP, Chari ST. Autoimmune pancreatitis: an update on classification, diagnosis, natural history and management. Curr Gastroenterol Rep. 2012;14(2):95–105.
Ghazale A, Chari ST. Optimising corticosteroid treatment for autoimmune pancreatitis. Gut. 2007;56(12):1650–2.
Hart PA, Topazian MD, Witzig TE, et al. Treatment of relapsing autoimmune pancreatitis with immunomodulators and rituximab: the Mayo Clinic experience. Gut. 2013;62(11):1607–15.
Hart PA, Law RJ, Dierkhising RA, et al. Risk of cancer in autoimmune pancreatitis: a case-control study and review of the literature. Pancreas. 2014;43(3):417–21.
Kamisawa T, Chari ST, Giday SA, et al. Clinical profile of autoimmune pancreatitis and its histological subtypes: an international multicenter survey. Pancreas. 2011;40(6):809–14.
Levy MJ, Reddy RP, Wiersema MJ, et al. EUS-guided trucut biopsy in establishing autoimmune pancreatitis as the cause of obstructive jaundice. Gastrointest Endosc. 2005;61(3):467–72.
Levy MJ. Endoscopic ultrasound-guided trucut biopsy of the pancreas: prospects and problems. Pancreatology. 2007;7(2–3):163–6.
Sugumar A, Levy MJ, Kamisawa T, et al. Endoscopic retrograde pancreatography criteria to diagnose autoimmune pancreatitis: an international multicentre study. Gut. 2011;60(5):666–70.
Kamisawa T, Shimosegawa T, Okazaki K, et al. Standard steroid treatment for autoimmune pancreatitis. Gut. 2009;58(11):1504–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Sah, R.P., Ahmed, N., Hart, P.A., Chari, S.T. (2015). Autoimmune Pancreatitis in the USA. In: Kamisawa, T., Chung, J. (eds) Autoimmune Pancreatitis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-55086-7_28
Download citation
DOI: https://doi.org/10.1007/978-3-642-55086-7_28
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-55085-0
Online ISBN: 978-3-642-55086-7
eBook Packages: MedicineMedicine (R0)