Abstract
Autoimmune Pancreatitis (AIP) is a recently recognized chronic fibro-inflammatory disease of the pancreas. Although rare, its recognition continues to increase worldwide. Patients often present with painless obstructive jaundice mimicking pancreatic cancer. Two subtypes of AIP are known-type 1 is a multi-organ disease associated with IgG4; type 2 appears to be a pancreas-specific disorder. Dramatic response to steroid treatment is characteristic of both forms. A non-invasive diagnosis of type 1 AIP may be possible using diagnostic criteria (in ~70% cases) while diagnosis of type 2 requires histology. These subtypes differ in natural history- type 1 often relapses while initial reports suggest that type 2 does not. Long term complications include endocrine and exocrine insufficiency and in case of type 1, disease relapses and complications from extra-pancreatic involvement. Neither form affects long term survival. The treatment and follow-up guidelines continue to evolve with our increasing experience in AIP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autoimmune pancreatitis (AIP) was reported as early as 1960s [1] but it was established as a distinct entity only recently [2, 3]. Since then, recognition of AIP worldwide has continued to increase [4–16]. It is a rare disease although currently there is no population-based epidemiologic data on its prevalence. AIP mimics pancreatic cancer in presentation [17••, 18, 19]. While pancreatic cancer is much more common and has altogether different prognosis, AIP is a benign disease with dramatic steroid responsiveness. A correct and timely recognition of AIP saves unnecessary surgery and patient anxiety. However, a misdiagnosis of AIP can be a nightmare in case of a missed diagnosis of pancreatic cancer. Here we review classification, diagnosis, management and natural history of AIP.
Classification
The Need for Sub-classification
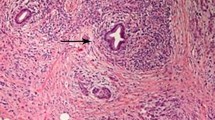
A landmark study in 2001 identified association of AIP with serum IgG4 elevations [20] and in 2004 with tissue infiltration with IgG4 positive cells [21]. It was then apparent that AIP patients frequently had involvement of several extra-pancreatic organs [22]. Histology in these patients revealed a distinct pattern of lymphoplasmacytic infiltrate with fibrosis in most affected organs [23]. Abundant IgG4-positive cells were noted in all affected sites including pancreas and extra-pancreatic organs [21, 24].
However, some of the pancreas specimens were observed to have a different histological pattern characterized by neutrophilic infiltrate in ductal epithelium with duct destruction [25]. These patients had disease confined only to the pancreas and IgG4 association was not seen [25]. On follow-up, it was found that the former group had frequent relapses while the latter group of patient did not have relapses [26••]. These two groups have now been termed type 1 and type 2 AIP, respectively [27••, 28••]. Distinct histological and clinical profiles with different outcomes make such a sub-classification extremely important [26••, 29•, 30].
Geographical Distribution
Type 1 AIP is the more common form worldwide [5••, 31]. This form appears to be the exclusive subtype in Japan and Korea [5••]. In the US, it is the predominant subtype accounting for more than 80% cases [31]. Type 2 AIP seems to be relatively common in Europe though type 1 is still the more prevalent subtype [31, 32•].
Type 1 AIP
Type 1 AIP is associated with characteristic histological pattern known as lymphoplasmacytic sclerosing pancreatitis (LPSP) (Table 1). Extra-pancreatic involvement is frequently seen [33, 34•]. In our series, 60% of type 1 AIP patients had other organ involvement [26••]. With increasing awareness of the disease as well as ever-expanding spectrum of recognized extra-pancreatic manifestations in AIP, the reported prevalence of other organ involvement is increasing [34•]. IgG4-rich lymphoplasmacytic infiltrate is seen on histology in all affected organs [21, 24]. The inflammatory process in all affected organs responds characteristically to steroid treatment though disease relapse in the pancreas or other affected organs is common [26••]. Serum IgG4 elevation is seen in about 80% of type 1 AIP [26••]. The association with IgG4 and multiple extra-pancreatic organ involvement has led to the concept of a multi-organ disease associated with IgG4, now known as IgG4-related Disease (IgG4-RD) [22, 35]. Type 1 AIP is the pancreatic manifestation of IgG4-RD [35] and has also been called as IgG4-related pancreatitis.
While IgG4 rich cellular infiltrate is seen in the affected organs including the pancreas in type 1 AIP, a subset of patients do not have elevated IgG4 levels in the serum. In our series, about 20% patients were seronegative at the time of diagnosis [26••]. The significance of seronegativity is unknown [36] though serum IgG4 levels are known to fluctuate [37•, 38]. It is important to recognize that a subset of type 1 patients may be seronegative and that seronegativity in itself should not be used to reclassify patients as type 2 AIP.
Type 2 AIP
Presence of neutrophils in the pancreas with characteristic granulocyte-epithelial lesions (GELS) on histology defines type 2 AIP [32•, 39] (Table 1). Currently, a definitive diagnosis of type 2 AIP requires histology [17••]. Based on clinical presentation, imaging features, serology and other organ involvement alone, a definitive diagnosis of type 2 AIP cannot be made though these can be suggestive of the diagnosis [17••, 28••]. Type 2 patients present at a younger age compared to type 1 [5••] (Table 1). About a third of these patients present with acute pancreatitis [5••, 26••]. However, obstructive jaundice is still the most common presentation as in type 1 AIP [26••, 27••]. Imaging alone cannot differentiate between the subtypes but type 2 patients are more likely to have focal findings [28••]. These patients do not have involvement of other extra-pancreatic organs [32•, 39]. There is no associated IgG4 rich infiltrate on histology and serum IgG4 elevation is unlikely. Inflammatory bowel disease is seen more commonly, in about 16–30% of patients [5, 26••] (Table 1). Response to steroids is characteristic and, at least in initial reports of histologically confirmed type 2 AIP, relapses do not occur in type 2 AIP [26••].
Diagnosis
The diagnosis of AIP is challenging even at the expert centers [40]. This is partly because AIP is a new entity that is known to be rare whereas its close differential, pancreatic cancer, is relatively more common. Misdiagnosis of AIP in the setting of pancreatic cancer is to be avoided.
In the last decade, many diagnostic criteria for AIP have been put forth [4, 12•, 41–43]. The differences in diagnostic criteria reflect regional differences in practice as well as possible differences in clinical profile and epidemiology. For example, most Asian criteria require pancreatic duct imaging by ERP/MRP [41, 42]. While the Mayo Clinic HISORt criteria [17••] does not require for ERP/MRP as current practice in the US does not include routine ERP/MRP for evaluation of obstructive jaundice. Recently international consensus diagnostic criteria (ICDC) have been developed which unify these diagnostic criteria while accommodating regional differences in practice and strategy [28••]. The ICDC [28••] incorporates most of the features of the revised HISORt criteria and combines the salient features of Asian/Japanese criteria that include ductal imaging (ERP/MRP) as well as ampullary biopsies with IgG4 staining. The ICDC provides a unified framework that allows for regional flexibility in establishing an institutional approach for diagnosing AIP based on available expertise and local practice pattern.
In this brief review we discuss clinical presentation of AIP and focus on the diagnosis of type 1 and type 2 AIP with emphasis on a practical approach to distinguish AIP from pancreatic cancer.
Clinical Presentation and Clues to Diagnosis
The most common presentation of AIP is with obstructive jaundice. About 75% of type 1 and about 50% of type 2 patients have obstructive jaundice at presentation [5••, 26••]. Thus, AIP closely mimics pancreatic cancer in its acute presentation. AIP can also present with acute pancreatitis [44]. In fact, our experience at a tertiary referral center indicates that about 4% of patients evaluated for pancreatitis (both acute and chronic) may have AIP as the etiology [44]. In our series, 15% of type 1 and 32% of type 2 patient presented with acute pancreatitis; however, most also had biliary involvement leading to obstructive jaundice and/or elevated liver enzymes [44]. Recurrent acute pancreatitis without biliary involvement is a rare presentation of AIP. A large proportion of patients experience abdominal pain which is mild (40% type 1 and about 70% of type 2 AIP) [5••]. In fact narcotic requiring chronic pain is not a feature of AIP. A proportion of patients may present late with features of painless chronic pancreatitis (11% in our series) [44].
Similarly the other organ systems involved in type 1 AIP/IgG4-RD frequently mimic organ specific diseases with similar presentation. For example, the clinical and radiological picture in IgG4-associated cholangitis (IAC) may resemble primary sclerosing cholangitis or cholangiocarcinoma [45, 46•], and salivary and lacrimal gland involvement mimics Sjogren’s syndrome [47]. However, the response to steroids in AIP is dramatic which is typically not seen in the corresponding organ-specific counterparts.
International Consensus Diagnostic Criteria for AIP
The clinical profile of AIP has five components- Histology (H), Imaging (I), Serology (S), Other organ involvement (OOI) and Response to steroid treatment (Rt). These form the basis of ICDC [28••] (as well as the revised HISORt criteria [17••]). Unlike older criteria which required both pancreatic parenchymal imaging by CT/MRI (P) [17••] and pancreatic ductal imaging by endoscopic retrograde pancreatogram (ERP) (D) [41, 42], the ICDC allows for either feature to be used (Table 2).
Each of these components may provide level 1 (highly suggestive) or level 2 (supportive) evidence. For example, Serum IgG4 elevation ≥ 2X upper limit of normal is highly suggestive of AIP (denoted as level 1 S), <2X upper limit of normal is supportive of AIP (denoted as level 2 S). The ICDC details and definitions are provided in table 2 [28••]. Different combinations of these features are considered diagnostic.
Diagnostic Groups Based on ICDC
Type 1 AIP may be diagnosed non-invasively, using pancreatic histology or, in select cases, using steroid trial (28) (Table 2)-
-
A.
Non-Invasive Diagnosis: AIP can be diagnosed in patients with
-
1)
highly suggestive parenchymal imaging (level 1 P) if there is any additional collateral evidence of AIP- one of elevated Serology or presence of Other organ involvement (one of S, OOI (level 1 or 2))
-
2)
only supportive parenchymal imaging (level 2 P) with a negative cancer work-up if there are at least two pieces of collateral evidence (two or more level 1 S/OOI) + ductal imaging (level 1 or 2 D))
-
1)
-
B.
Invasive Diagnosis:
Patients can be diagnosed with AIP if there are features of LPSP on resection specimens or core biopsy (Level 1 H) regardless of presence or absence of collateral evidence
-
C.
Steroid trial in a select group:
This approach should be used sparingly. Type 1 AIP can be diagnosed in patients with characteristic response to steroids who have all the following criteria
-
a)
supportive parenchymal imaging (level 2 P)
-
b)
negative cancer work-up and
-
c)
one of the following-
-
i)
one level 1 S/OOI
-
ii)
two level 2 S/OOI
-
iii)
one level 2 S/OOI with ductal imaging (level 1 or 2 D)
-
i)
In a validation study, about 70% of suspected patients could be diagnosed with type 1 AIP by highly suggestive imaging plus one collateral evidence in the form of other organ involvement or serum IgG4 elevations (group 1 above) [17••]. This has great practical utility and forms the basis of the approach described here (Fig. 1). The remaining 30% suspected patients require either histology or a steroid trial [17••]. This is the difficult area requiring meticulous patient selection.
A practical approach to differential diagnosis of AIP Vs Cancer. Initial step in the work-up of a patient with obstructive jaundice and/or pancreatic mass is obtaining parenchymal imaging (CT/MRI). This is followed by clinical and radiologic review for evidence of other organ involvement (OOI), and obtaining serum IgG4 levels (S). At this stage, about 70% of type 1 AIP can be diagnosed. Further stepwise diagnostic approach includes: +/− ERP followed by EUS guided pancreatic core biopsy or steroid trial if all the criteria are met. Based on ICDC, type 1 AIP can be diagnosed when all the criteria listed in any of the diagnostic groups are satisfied. See text for details
A Practical Approach to Differential Diagnosis of AIP Vs Cancer
Initial Parenchymal Imaging- CT Scan/MRI
This approach revolves around initial imaging in the form of a CT scan with contrast or MRI in patients with obstructive jaundice. This is consistent with the usual practice for initial work-up of a patient with painless obstructive jaundice in the US [17••]. Based on imaging features, patients can be stratified into three groups – suggestive of cancer, highly suggestive of AIP, or supportive for AIP.
This is followed by search for the evidence of other organ involvement (clinical review and review of CT scan/MRI) and evaluation of serum IgG4. About 70% patients can be diagnosed as type 1 AIP at this stage [17••].
This may be followed by ERP with ampullary biopsies (for possibility of diagnostic group #2 above) though the diagnostic utility of ERP in the American context [48•] and of ampullary biopsies for IgG4 stain [49–51] are still controversial.
Pancreatic Core Biopsy
FNA is routinely done for evaluation of pancreatic cancer but is not useful for histological evaluation of AIP [4]. We recognize recognized that EUS is available only at expert centers. However, only a handful of suspected patients with AIP require histological evidence [17••]. EUS guided pancreatic biopsies are relatively new in practice. It is believed that as experience with the technique of pancreatic core biopsies and its interpretation increases, it will be accepted as an invaluable tool [52, 53].
Diagnostic Steroid Trial
Use of steroid trial may result in delay in diagnosing cancer and is strongly discouraged except in expert setting in the selected patient group meeting the criteria noted above (Fig. 1, group 4).
Type 2 AIP
Type 2 AIP can be suspected in relatively younger patients with obstructive jaundice who are seronegative and have no other organ involvement typical of type 1 AIP with or without IBD. In all suspected cases after a thorough negative cancer work-up, pancreatic core biopsy is recommended. Currently, the definitive diagnosis of type 2 AIP requires histology [26••, 28••, 32•, 39]. Due to difficulty in diagnosis, it is possible that type 2 AIP is frequently under-recognized and under-reported. Hopefully in future, with greater awareness and recognition of the condition, biomarkers can be identified that can help diagnose type 2 AIP without need for histology.
Diagnostic histology (level 1 H) for type 2 AIP which is called IDCP requires both (28) -
-
1)
GEL with or without granulocytic and lymphoplasmacytic acinar infiltrate
-
2)
absent/scant IgG4 positive cells.
Absence of GELs but presence of rest of the above features constitutes supportive histology (level 2) which may indicate probable type 2 AIP.
AIP-NOS
Some patients may not meet any diagnostic groups. Although possible, these would be rare if the diagnostic steps are carefully carried out. One example would be a patient with obstructive jaundice with negative workup for malignancy, has typical parenchymal imaging features who is seronegative and has no evidence of other organ involvement and histology shows lymphoplasmacytic infiltrate with storiform fibrosis (which is common supportive feature of both type 1 and type 2) [17••] but no IgG4 staining and no GELs. The diagnostic challenge is Type 2 AIP Vs seronegative Type 1 AIP (36). The patients may be classified as AIP-NOS and managed with steroid treatment.
Management
AIP is exquisitely responsive to steroid treatment [10••, 54••, 55]. In fact, response to steroids is so consistent and characteristic that lack of response should prompt consideration of alternate diagnosis [17••, 56]. Multiple case series have studied steroid treatment with improvement in both pancreatic and in case of type 1 AIP, affected extra-pancreatic organs [10••, 54••, 57]. The treatment protocols vary among different centers [54••]. We use a protocol starting with 40 mg/day for 4 weeks and tapering off by 5 mg/week to complete a course of 11 weeks [54••, 55]. Treatment response is objectively monitored by clinical follow-up, follow-up imaging and biochemical tests (LFT) [54••, 55]. Steroid taper is started once response to treatment is confirmed objectively [54••, 55].
Additional Initial Management: Biliary Decompression
Most AIP patients present with obstructive jaundice. The Japanese and Asian guidelines, which require ERP for diagnosis, recommend routine biliary decompression in all patients with obstructive jaundice prior to starting surgery [41, 42, 58]. These guidelines also recommend treatment of diabetes prior to starting steroids [58]. In our experience, if diagnosis of AIP is definitive, routine ERP for drainage is not required as steroid treatment generally improves jaundice quickly without need for drainage in AIP [46•]. However, when diagnosis of AIP is uncertain, biliary drainage could be considered prior to treatment [46•, 54••, 55]. In such cases ERP may aid in diagnosis as in the Asian diagnostic criteria.
Disease Relapse in Type 1 AIP
Disease relapse is common in type 1 AIP while patients with type 2 AIP do not relapse [26••, 59]. Most series estimate the frequency of relapse in type 1 AIP in the range from 30% to 50% [5••, 6–8, 10••, 11, 12•, 13–16, 34•, 54••, 57, 60, 61]. In our series of 78 type 1 AIP patients with a median follow-up of 42 months, symptomatic disease relapse was seen in 47% patients with a 3-year cumulative relapse rate of 59% in type 1 AIP patients who were medically managed [26••]. Lack of a uniform definition of disease relapse, short follow-up, small patient population, lack of identification of subtypes and possible ethnic variability contributes to the wide range of reported relapse rates from across the world [5••, 6–8, 10••, 11–15, 57, 60–62]. In our series, we considered only clinically symptomatic relapse excluding asymptomatic serologic and biochemical recurrence alone as relapse [26••, 46•].
It is also unclear as to what happens to relapse rates as AIP progresses. Some autoimmune diseases are characterized by an active phase and then a burnt-out phase with no recurrences, for example, Hashimoto’s thyroiditis [63]. On the other hand, autoimmune hepatitis is characterized by recurrent relapses and life-long immunosuppressive therapy is indicated [64]. Most relapses (~90%) seem to occur within the first 3 years in type 1 AIP [10••, 26••]. However, to conclude that relapses in the later stage of disease are uncommon will need longer follow-up of patients.
Relapses appear to be common in the proximal bile duct (presenting as biliary stricture with jaundice with or without cholangitis) and in the pancreas (presenting as diffuse swelling, pancreatitis, steatorrhea) [5••, 10••, 26••, 46•, 62]. In our series, 54% patients with relapses had recurrence in proximal bile duct and 27% patients had relapse in the pancreas [26••]. Extra-pancreatic disease relapse are also observed although with much less frequency, the common sites being- RPF, kidney, lungs, lymph nodes and liver [5••, 10••, 26••, 34•, 60].
Predictors of Relapse
In our series, proximal bile duct involvement and diffuse swelling of the pancreas were factors predictive of disease relapse in type 1 AIP in a multivariate analysis with hazard ratios of 2.12 and 2.00 (p = 0.03 and 0.04) respectively for proximal bile duct involvement and diffuse pancreatic swelling [26••]. Similar results have been noted in most other case series [6, 10••, 11, 12•, 16, 34•, 57, 61, 62]. Recently, some case-series have suggested that IgG4 elevations and evidence of other organ involvement may be predictive of relapse [6, 11, 34•, 61, 62]. These appear to be a confounding factors as these series are mixtures of type 1 and type 2 AIP, with type 1 AIP more likely to relapse and also more likely to have IgG4 elevations and other organ involvement. When we analyzed our data after separating AIP subtypes, initial IgG4 elevation as well as other organ involvement other than proximal bile duct did not predict relapses in type 1 AIP [26••]. Further, association of substitution of aspartic acid at position 57 of DQβ1 with increased relapse was described by Park et al. [65] while another study failed to see this association [66].
Management of Relapse and Maintenance Therapy
Corticosteroids are effective in treating relapses as well and long term maintenance therapy may be necessary in patients who relapse [54••]. The role of maintenance corticosteroid therapy for primary prevention of relapses and utility of immunosuppressive drugs like azathioprine in refractory cases remain to be studied in controlled studies, though there is some experience with successful use of immunosuppressive drugs in refractory cases with frequent relapses [6, 16, 46•, 67].
The major point of contention is the need for maintenance steroid therapy. Centers in Japan routinely use a prolonged maintenance therapy for up to 3 years with the logic that most patients relapse within 3 years [10••, 58]. The benefit of universal and prolonged maintenance therapy has not been established. In a multicenter study from Japan, it was shown that maintenance therapy reduced the relapse rate to 23% from 34% in those who weaned off steroids [10••]. In our experience, universal use of maintenance steroid therapy is not recommended because the risks of long term steroid use outweigh the benefits in AIP [54••]. Unlike Autoimmune Hepatitis where relapse is universal on withdrawal of immunosuppressive therapy [64], about half of type 1 AIP patients do not relapse after short-course of steroid treatment [5••, 26••, 54••, 60]. Monitoring of liver enzymes to detect early biliary relapse and prompt steroid treatment of any relapse is beneficial in our experience [26••, 54••, 60]. We start maintenance therapy with azathioprine (2–2.5 mg/kg) after the first or second relapse [54••, 68]. Following this approach, we have observed that 30% to 40% AIP patients will eventually require maintenance therapy to prevent frequent relapses [54••, 68].
Utility of IgG4 in Monitoring Treatment and Relapse
Monitoring serum IgG4 levels could be potentially relevant in two settings-1) monitoring of therapy, and 2) monitoring for disease relapse. However, currently there is no convincing evidence that monitoring of serum IgG4 is helpful in either of these two proposed settings [37•]. A large proportion of treated patients did not normalize IgG4 levels after treatment (115/182 (63%) in the largest multicenter cohort from Japan [10••]). Further, only 30% of these patients with persistent IgG4 elevations relapse (Vs 10% in patients with normalization of IgG4 levels) [10••]. In our cohort, among the 47 patients who had elevated serum IgG4 at presentation, 37 received steroids. Among these 37, we have follow-up IgG4 data on 19 patients. It is interesting to note that only 11/19 (57.9%) patients had normalization of IgG4 levels while in the remaining 8/19 (42.1%), IgG4 levels remained persistently elevated [37•]. Further, we noted that the proportion of patients who normalized serum IgG4 did not differ between patients with and without relapse [46•]. Therefore, it appears that a significant proportion of patients will fail to normalize IgG4 levels upon treatment and only a minority of them may relapse.
Long Term Outcomes
Long Term Survival
We compared long term survival in AIP patients, both type 1 and type 2 to age- and gender-matched population and found that these were similar [26••]. Therefore, despite long term outcomes including pancreatic insufficiency, diabetes, extra-pancreatic involvement, and complication related to therapy that could contribute to morbidity, neither type 1 nor type 2 AIP affects long term survival [26••].
Risk of Malignancy
Several case reports of pancreatic cancer have been described in patients with AIP [10••, 12•, 61, 62, 69–75]. Interestingly one case was noted at the time of presentation of AIP which poses an interesting diagnostic scenario [76]. Whether these malignancies can be attributed to older age is unknown. However, AIP being a rare disease and pancreatic cancer also a relatively uncommon disease, simultaneous occurrence of both in several patients does suggest a cause-effect relationship. Interestingly, Kamisawa et al. [77] observed high frequency of KRAS mutation in the pancreatobiliary region of AIP patients. It is very likely that the process of chronic inflammation and fibrosis in AIP may increase the risk of cancer. Careful long term follow-up of patients for development of malignancies is therefore recommended.
Further, there are some reports of other solid organ malignancies [61, 78, 79] including biliary intra-epithelial neoplasia [75] as well as lymphomas [80] and lymphoproliferative disorders [81]. The exact association of these with AIP is currently unknown
Pancreatic Insufficiency: Exocrine and Endocrine
The pancreatic exocrine and endocrine function of many AIP patients is impaired by extensive destruction of the acini and islets by the inflammatory process [71]. The prevalence of exocrine insufficiency was estimated to be well in the order of 90% if subclinical insufficiency is included as well [82, 83]. Diabetes mellitus was reported in 26% to 78% patients [12•, 84–86]. Though there is no conclusive evidence, some studies indicate improvement of pancreatic function after steroid treatment [71, 84, 87, 88] while one study [85] noted negative effect on glucose tolerance in some older AIP patients treated with steroids. It appears that diabetes in the initial acute phase may improve with steroid treatment or even spontaneously. In the late phase, glycemic control may worsen with steroids and glycemic control may be more difficult to achieve in patients with diabetes while on treatment [54••].
Other Manifestations Affecting Prognosis
Inflammatory bowel disease (IBD) is seen in about 2% to 6% patients with type 1 AIP and 16% to 18% of patients with type 2 AIP [5••, 26••]. Patients with both AIP and IBD may have increased severity of IBD [89]. Similarly, hypothyroidism occurs in a significant proportion of patients requiring thyroxine supplementation [90]. Recently, increased prevalence of asthma and allergic disorders has been described in AIP [91].
Long Term Outcomes of Extrapancreatic Involvement in Type 1 AIP
Proximal bile duct involvement is the most common symptomatic extra-pancreatic manifestation of type 1 AIP/ IgG4-RD which has been given its own name- IgG4 associated Cholangitis (IAC) [46•]. Unlike biliary strictures seen in primary sclerosing cholangitis (PSC), the biliary strictures in IAC typically respond to steroid therapy [45, 46•]. However, untreated IAC may rapidly progress to end stage liver disease [46•]. Salivary gland involvement which is common in type 1 AIP is known as IgG4 related sialoadenitis (Miculicz disease) which differs from Sjogren’s syndrome by lack of anti-SSA and anti-SSB antibodies, lack of association with rheumatoid arthritis, presence of elevated serum IgG4 levels and IgG4-rich infiltrate and response to steroids [47]. Kidney involvement includes tubulointerstitial nephritis (seen in 35% patients with AIP [92]), nodular lesions mimicking metastatic tumors [93], pseudotumors [94]and membranous nephropathy [95] all of which improve on steroid treatment [35, 92]. Retroperitoneal fibrosis (RPF), in which a thick mass covers abdominal aorta and compresses ureters that could lead to lower extremity edema and hydronephrosis/renal failure respectively, is seen in 8% to 16% of type 1 AIP [33, 35, 96]. IgG4 related pulmonary disease, presenting as interstitial infiltrates which could deteriorate to respiratory failure if untreated, has been recently characterized with prevalence from 3% [34•] to 13% [97] in type 1 AIP. Mediastinal or hilar lymphadenopathy is perhaps the most common extrapancreatic involvement, reported in as high as 77% [34•] to 80% [33, 35]. Recently, Chung et al. [98] reported positive IgG4 staining in 9 of 24 liver biopsies of autoimmune hepatitis (AIH) patients that correlated with more dramatic steroid response compared to IgG4-negative AIH, thus suggesting existence of IgG4-related hepatopathy [99]. Numerous other associations in IgG4-RD have been described - IgG4-assocaited prostatitis [100], pericarditis [101], inflammatory pseudotumors, gastric ulcers and gastric and colon polyps associated with IgG4 [60]. Though these are mostly case reports, most of these other IgG4-related lesions appear to be responsive to steroids [60].
Conclusions
AIP is a recently characterized chronic disease of the pancreas. Type 1 AIP, the relatively more common form, is a multi-organ disease associated with IgG4 with characterized by relapsing natural course. Type 2 AIP is confined to pancreas and associated with granulocyte epithelial lesions (GELs) on histology. The diagnosis of type 1 AIP can be made non-invasively in a majority of patients while type 2 AIP can only be diagnosed on histology. Steroid treatment is the mainstay of management, with characteristic dramatic response. Despite long term outcomes including pancreatic insufficiency, extra-pancreatic involvement and complications related to immunosuppressive therapy, neither type 1 nor type 2 AIP affects long term survival.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sarles H, Sarles JC, Muratore R, et al. Chronic inflammatory sclerosis of the pancreas–an autonomous pancreatic disease? Am J Dig Dis. 1961;6:688–98.
Yoshida K, Toki F, Takeuchi T, et al. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40(7):1561–8.
Pearson RK, Longnecker DS, Chari ST, et al. Controversies in clinical pancreatology: autoimmune pancreatitis: does it exist? Pancreas. 2003;27(1):1–13.
Chari ST, Smyrk TC, Levy MJ, et al. Diagnosis of autoimmune pancreatitis: the Mayo Clinic experience. Clin Gastroenterol Hepatol. 2006;4(8):1010–6. quiz 934.
•• Kamisawa T, Chari ST, Giday SA, et al. Clinical profile of autoimmune pancreatitis and its histological subtypes: an international multicenter survey. Pancreas 40(6):809–14. An important study analyzing data from cohorts around the world and specifically examining biopsy-unproven cases of AIP worldwide.
Raina A, Yadav D, Krasinskas AM, et al. Evaluation and management of autoimmune pancreatitis: experience at a large US center. Am J Gastroenterol. 2009;104(9):2295–306.
• Park DH, Kim MH, Chari ST. Recent advances in autoimmune pancreatitis. Gut 2009;58(12):1680–9. A comprehensive review of AIP including discussion on pathogenesis of type 1 and type 2 AIP.
Ryu JK, Chung JB, Park SW, et al. Review of 67 patients with autoimmune pancreatitis in Korea: a multicenter nationwide study. Pancreas. 2008;37(4):377–85.
Song Y, Liu QD, Zhou NX, et al. Diagnosis and management of autoimmune pancreatitis: experience from China. World J Gastroenterol. 2008;14(4):601–6.
•• Kamisawa T, Shimosegawa T, Okazaki K, et al. Standard steroid treatment for autoimmune pancreatitis. Gut 2009;58(11):1504–7. A large multicenter cohort from Japan describing the treatment and response to treatment including relapse in AIP.
Church NI, Pereira SP, Deheragoda MG, et al. Autoimmune pancreatitis: clinical and radiological features and objective response to steroid therapy in a UK series. Am J Gastroenterol. 2007;102(11):2417–25.
• Frulloni L, Scattolini C, Falconi M, et al. Autoimmune pancreatitis: differences between the focal and diffuse forms in 87 patients. Am J Gastroenterol. 2009;104(9):2288–94. A different approach to classifying AIP based on initial radiology into diffuse and focal forms, from a large cohort in Italy.
Noor MT, Lal A, Kochhar R, et al. Autoimmune pancreatitis: a report from India. JOP 11(3):213–9.
Maire F, Le Baleur Y, Rebours V, et al. Outcome of patients with type 1 or 2 autoimmune pancreatitis. Am J Gastroenterol. 106(1):151–6.
Czako L, Gyokeres T, Topa L, et al. Autoimmune pancreatitis in Hungary: a multicenter nationwide study. Pancreatology 11(2):261–7.
Sandanayake NS, Church NI, Chapman MH, et al. Presentation and management of post-treatment relapse in autoimmune pancreatitis/immunoglobulin G4-associated cholangitis. Clin Gastroenterol Hepatol. 2009;7(10):1089–96.
•• Chari ST, Takahashi N, Levy MJ, et al. A diagnostic strategy to distinguish autoimmune pancreatitis from pancreatic cancer. Clin Gastroenterol Hepatol. 2009;7(10):1097–103. An important study that validates the diagnostic approach that forms the basis of the revised HISORt criteria and the new ICDC criteria described in this review. This study showed that more than 70% of type 1 AIP diagnosis can be made non-invasively.
Sugumar A, Chari ST. Distinguishing pancreatic cancer from autoimmune pancreatitis: a comparison of two strategies. Clin Gastroenterol Hepatol. 2009;7(11 Suppl):S59–62.
Sugumar A, Takahashi N, Chari ST. Distinguishing pancreatic cancer from autoimmune pancreatitis. Curr Gastroenterol Rep. 12(2):91–7.
Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344(10):732–8.
Kamisawa T. IgG4-positive plasma cells specifically infiltrate various organs in autoimmune pancreatitis. Pancreas. 2004;29(2):167–8.
Kamisawa T, Funata N, Hayashi Y. Lymphoplasmacytic sclerosing pancreatitis is a pancreatic lesion of IgG4-related systemic disease. Am J Surg Pathol. 2004;28(8):1114.
Zamboni G, Luttges J, Capelli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch. 2004;445(6):552–63.
Zhang L, Notohara K, Levy MJ, et al. IgG4-positive plasma cell infiltration in the diagnosis of autoimmune pancreatitis. Mod Pathol. 2007;20(1):23–8.
Notohara K, Burgart LJ, Yadav D, et al. Idiopathic chronic pancreatitis with periductal lymphoplasmacytic infiltration: clinicopathologic features of 35 cases. Am J Surg Pathol. 2003;27(8):1119–27.
•• Sah RP, Chari ST, Pannala R, et al. Differences in clinical profile and relapse rate of type 1 versus type 2 autoimmune pancreatitis. Gastroenterology 139(1):140–8; quiz e12-3. This study described the clinical profile of type 1 and type 2 AIP for the first time. Also the first data on long term follow-up of AIP including survival and relapse.
•• Chari ST, Kloeppel G, Zhang L, et al. Histopathologic and clinical subtypes of autoimmune pancreatitis: the Honolulu consensus document. Pancreas 39(5):549–54. A consensus document emerging from the important 40th APA and JPS joint meeting discussion on the classification of AIP. A popular meeting widely attended from experts all around the world, this document summarizes the important discussion on the recognition of type 1 and type 2 AIP as distinct subtypes.
•• Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas 40(3):352–8. This paper introduces and describes the ICDC criteria for the diagnosis of AIP (type 1 and type 2).
• Chari ST, Longnecker DS, Kloppel G. The diagnosis of autoimmune pancreatitis: a Western perspective. Pancreas 2009;38(8):846–8. An important discussion on the implication on the diagnosis of AIP after the recognition of two distinct subtypes.
Deshpande V, Gupta R, Sainani N, et al. Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol. 35(1):26–35.
Sugumar A, Kloppel G, Chari ST. Autoimmune pancreatitis: pathologic subtypes and their implications for its diagnosis. Am J Gastroenterol. 2009;104(9):2308–10. quiz 11.
• Kloppel G, Detlefsen S, Chari ST, et al. Autoimmune pancreatitis: the clinicopathological characteristics of the subtype with granulocytic epithelial lesions. J Gastroenterol. 45(8):787–93. This imporatnt study describes the histology features of type 2 AIP.
Hamano H, Arakura N, Muraki T, et al. Prevalence and distribution of extrapancreatic lesions complicating autoimmune pancreatitis. J Gastroenterol. 2006;41(12):1197–205.
• Naitoh I, Nakazawa T, Ohara H, et al. Clinical significance of extrapancreatic lesions in autoimmune pancreatitis. Pancreas 39(1):e1–5. A comprehensive study describing extra-pancreatic manifestations in AIP.
Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008;14(25):3948–55.
Kamisawa T, Takuma K, Tabata T, et al. Serum IgG4-negative autoimmune pancreatitis. J Gastroenterol. 46(1):108–16.
• Sah RP, Chari ST. Serologic issues in IgG4-related systemic disease and autoimmune pancreatitis. Curr Opin Rheumatol. 23(1):108–13. An important review on the role of IgG4 in the diagnosis and follow-up of AIP.
Tabata T, Kamisawa T, Takuma K, et al. Serial changes of elevated serum IgG4 levels in IgG4-related systemic disease. Intern Med. 50(2):69–75.
Levy MJ, Smyrk TC, Takahashi N, et al. Idiopathic duct-centric pancreatitis: disease description and endoscopic ultrasonography-guided trucut biopsy diagnosis. Pancreatology 11(1):76–80.
Gardner TB, Levy MJ, Takahashi N, et al. Misdiagnosis of autoimmune pancreatitis: a caution to clinicians. Am J Gastroenterol. 2009;104(7):1620–3.
Okazaki K, Kawa S, Kamisawa T, et al. Japanese consensus guidelines for management of autoimmune pancreatitis: I. Concept and diagnosis of autoimmune pancreatitis. J Gastroenterol. 45(3):249–65.
Otsuki M, Chung JB, Okazaki K, et al. Asian diagnostic criteria for autoimmune pancreatitis: consensus of the Japan-Korea Symposium on Autoimmune Pancreatitis. J Gastroenterol. 2008;43(6):403–8.
Schneider A, Lohr JM, Singer MV. The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classifications of the disease. J Gastroenterol. 2007;42(2):101–19.
Sah RP, Pannala R, Chari ST, et al. Prevalence, diagnosis, and profile of autoimmune pancreatitis presenting with features of acute or chronic pancreatitis. Clin Gastroenterol Hepatol. 8(1):91–6.
Nakazawa T, Ohara H, Sano H, et al. Clinical differences between primary sclerosing cholangitis and sclerosing cholangitis with autoimmune pancreatitis. Pancreas. 2005;30(1):20–5.
• Ghazale A, Chari ST, Zhang L, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology 2008;134(3):706–15. An important cohort describing IgG4 associated Cholangitis (IAC), including treatment and relapse.
Yamamoto M, Harada S, Ohara M, et al. Clinical and pathological differences between Mikulicz’s disease and Sjogren’s syndrome. Rheumatology (Oxford). 2005;44(2):227–34.
• Sugumar A, Levy MJ, Kamisawa T, et al. Endoscopic retrograde pancreatography criteria to diagnose autoimmune pancreatitis: an international multicentre study. Gut 60(5):666–70. A multicenter effort to recognize important ERP features of AIP and its utility in diagnosis. This study recognized the limited use currently of ERP features in diagnosis of AIP in the western setting.
Moon SH, Kim MH, Park do H, et al. IgG4 immunostaining of duodenal papillary biopsy specimens may be useful for supporting a diagnosis of autoimmune pancreatitis. Gastrointest Endosc. 71(6):960–6.
Kamisawa T, Tu Y, Egawa N, et al. A new diagnostic endoscopic tool for autoimmune pancreatitis. Gastrointest Endosc. 2008;68(2):358–61.
Rebours V, Le Baleur Y, Cazals-Hatem D, et al. IgG4 immunostaining of gastric, duodenal or colonic biopsies is not helpful for the diagnosis of autoimmune pancreatitis. Clin Gastroenterol Hepatol.
Levy MJ. Endoscopic ultrasound-guided trucut biopsy of the pancreas: prospects and problems. Pancreatology. 2007;7(2–3):163–6.
Mizuno N, Bhatia V, Hosoda W, et al. Histological diagnosis of autoimmune pancreatitis using EUS-guided trucut biopsy: a comparison study with EUS-FNA. J Gastroenterol. 2009;44(7):742–50.
•• Pannala R, Chari ST. Corticosteroid treatment for autoimmune pancreatitis. Gut 2009;58(11):1438–9. An rigorous discussion on the differences in treatment practices in the US and Japan and its implications based on available experience.
Ghazale A, Chari ST. Optimising corticosteroid treatment for autoimmune pancreatitis. Gut. 2007;56(12):1650–2.
Moon SH, Kim MH, Park DH, et al. Is a 2-week steroid trial after initial negative investigation for malignancy useful in differentiating autoimmune pancreatitis from pancreatic cancer? A prospective outcome study. Gut. 2008;57(12):1704–12.
Hirano K, Tada M, Isayama H, et al. Long-term prognosis of autoimmune pancreatitis with and without corticosteroid treatment. Gut. 2007;56(12):1719–24.
Kamisawa T, Okazaki K, Kawa S, et al. Japanese consensus guidelines for management of autoimmune pancreatitis: III. Treatment and prognosis of AIP. J Gastroenterol. 45(5):471–7.
Chari ST, Murray JA. Autoimmune pancreatitis, Part II: the relapse. Gastroenterology. 2008;134(2):625–8.
Sah RP, Chari ST. Long Term Prognosis in IgG4-related Systemic Disease (ISD). Curr Immunol Rev. 7(2):239–45.
Kubota K, Iida H, Fujisawa T, et al. Clinical factors predictive of spontaneous remission or relapse in cases of autoimmune pancreatitis. Gastrointest Endosc. 2007;66(6):1142–51.
Kawa S, Hamano H, Ozaki Y, et al. Long-term follow-up of autoimmune pancreatitis: characteristics of chronic disease and recurrence. Clin Gastroenterol Hepatol. 2009;7(11 Suppl):S18–22.
Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med. 2003;348(26):2646–55.
Johnson PJ, McFarlane IG, Williams R. Azathioprine for long-term maintenance of remission in autoimmune hepatitis. N Engl J Med. 1995;333(15):958–63.
Park do H, Kim MH, Oh HB, et al. Substitution of aspartic acid at position 57 of the DQbeta1 affects relapse of autoimmune pancreatitis. Gastroenterology. 2008;134(2):440–6.
Hirano K, Asaoka Y, Tada M, et al. No significant relation between relapse of autoimmune pancreatitis and substitution of aspartic acid at position 57 of DQbeta1. J Gastroenterol. 2009;44(7):799–800.
Topazian M, Witzig TE, Smyrk TC, et al. Rituximab therapy for refractory biliary strictures in immunoglobulin G4-associated cholangitis. Clin Gastroenterol Hepatol. 2008;6(3):364–6.
Sugumar A, Chari ST. Diagnosis and treatment of autoimmune pancreatitis. Curr Opin Gastroenterol. 26(5):513–8.
Ghazale A, Chari S. Is autoimmune pancreatitis a risk factor for pancreatic cancer? Pancreas. 2007;35(4):376.
Loos M, Esposito I, Hedderich DM, et al. Autoimmune pancreatitis complicated by carcinoma of the pancreatobiliary system: a case report and review of the literature. Pancreas 40(1):151–4.
Uchida K, Yazumi S, Nishio A, et al. Long-term outcome of autoimmune pancreatitis. J Gastroenterol. 2009;44(7):726–32.
Inoue H, Miyatani H, Sawada Y, et al. A case of pancreas cancer with autoimmune pancreatitis. Pancreas. 2006;33(2):208–9.
Fukui T, Mitsuyama T, Takaoka M, et al. Pancreatic cancer associated with autoimmune pancreatitis in remission. Intern Med. 2008;47(3):151–5.
Motosugi U, Ichikawa T, Yamaguchi H, et al. Small invasive ductal adenocarcinoma of the pancreas associated with lymphoplasmacytic sclerosing pancreatitis. Pathol Int. 2009;59(10):744–7.
Ohtani H, Ishida H, Ito Y, et al. Autoimmune pancreatitis and biliary intraepithelial neoplasia of the common bile duct: a case with diagnostically challenging but pathogenetically significant association. Pathol Int. 61(8):481–5.
Pezzilli R, Vecchiarelli S, Di Marco MC, et al. Pancreatic ductal adenocarcinoma associated with autoimmune pancreatitis. Case Rep Gastroenterol. 5(2):378–85.
Kamisawa T, Tsuruta K, Okamoto A, et al. Frequent and significant K-ras mutation in the pancreas, the bile duct, and the gallbladder in autoimmune pancreatitis. Pancreas. 2009;38(8):890–5.
Kamisawa T, Okamoto A. Prognosis of autoimmune pancreatitis. J Gastroenterol. 2007;42 Suppl 18:59–62.
Nishino T, Toki F, Oyama H, et al. Long-term outcome of autoimmune pancreatitis after oral prednisolone therapy. Intern Med. 2006;45(8):497–501.
Takahashi N, Ghazale AH, Smyrk TC, et al. Possible association between IgG4-associated systemic disease with or without autoimmune pancreatitis and non-Hodgkin lymphoma. Pancreas. 2009;38(5):523–6.
Masaki Y, Dong L, Kurose N, et al. Proposal for a new clinical entity, IgG4-positive multiorgan lymphoproliferative syndrome: analysis of 64 cases of IgG4-related disorders. Ann Rheum Dis. 2009;68(8):1310–5.
Tanaka S, Kobayashi T, Nakanishi K, et al. Corticosteroid-responsive diabetes mellitus associated with autoimmune pancreatitis: pathological examinations of the endocrine and exocrine pancreas. Ann N Y Acad Sci. 2002;958:152–9.
Ito T, Kawabe K, Arita Y, et al. Evaluation of pancreatic endocrine and exocrine function in patients with autoimmune pancreatitis. Pancreas. 2007;34(2):254–9.
Kamisawa T, Egawa N, Inokuma S, et al. Pancreatic endocrine and exocrine function and salivary gland function in autoimmune pancreatitis before and after steroid therapy. Pancreas. 2003;27(3):235–8.
Nishimori I, Tamakoshi A, Kawa S, et al. Influence of steroid therapy on the course of diabetes mellitus in patients with autoimmune pancreatitis: findings from a nationwide survey in Japan. Pancreas. 2006;32(3):244–8.
Kim KP, Kim MH, Song MH, et al. Autoimmune chronic pancreatitis. Am J Gastroenterol. 2004;99(8):1605–16.
Frulloni L, Scattolini C, Katsotourchi AM, et al. Exocrine and endocrine pancreatic function in 21 patients suffering from autoimmune pancreatitis before and after steroid treatment. Pancreatology 10(2–3):129–33.
Ito T, Nakamura T, Fujimori N, et al. Characteristics of pancreatic diabetes in patients with autoimmune pancreatitis. J Dig Dis. 12(3):210–6.
Ravi K, Chari ST, Vege SS, et al. Inflammatory bowel disease in the setting of autoimmune pancreatitis. Inflamm Bowel Dis. 2009;15(9):1326–30.
Sah RP, Chari ST. Clinical hypothyroidism in autoimmune pancreatitis. Pancreas 39(7):1114–6.
Sah RP, Pannala R, Zhang L, et al. Eosinophilia and allergic disorders in autoimmune pancreatitis. Am J Gastroenterol. 105(11):2485–91.
Takahashi N, Kawashima A, Fletcher JG, et al. Renal involvement in patients with autoimmune pancreatitis: CT and MR imaging findings. Radiology. 2007;242(3):791–801.
Rudmik L, Trpkov K, Nash C, et al. Autoimmune pancreatitis associated with renal lesions mimicking metastatic tumours. CMAJ. 2006;175(4):367–9.
Cornell LD, Chicano SL, Deshpande V, et al. Pseudotumors due to IgG4 immune-complex tubulointerstitial nephritis associated with autoimmune pancreatocentric disease. Am J Surg Pathol. 2007;31(10):1586–97.
Watson SJ, Jenkins DA, Bellamy CO. Nephropathy in IgG4-related systemic disease. Am J Surg Pathol. 2006;30(11):1472–7.
Hamano H, Kawa S, Ochi Y, et al. Hydronephrosis associated with retroperitoneal fibrosis and sclerosing pancreatitis. Lancet. 2002;359(9315):1403–4.
Hirano K, Kawabe T, Komatsu Y, et al. High-rate pulmonary involvement in autoimmune pancreatitis. Intern Med J. 2006;36(1):58–61.
Chung H, Watanabe T, Kudo M, et al. Identification and characterization of IgG4-associated autoimmune hepatitis. Liver Int. 30(2):222–31.
Umemura T, Zen Y, Hamano H, et al. Immunoglobin G4-hepatopathy: association of immunoglobin G4-bearing plasma cells in liver with autoimmune pancreatitis. Hepatology. 2007;46(2):463–71.
Uehara T, Hamano H, Kawakami M, et al. Autoimmune pancreatitis-associated prostatitis: distinct clinicopathological entity. Pathol Int. 2008;58(2):118–25.
Nayar M, Charnley R, Scott J, et al. Autoimmune pancreatitis with multiorgan involvement. A case of pericardial involvement. JOP. 2009;10(5):539–42.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sah, R.P., Chari, S.T. Autoimmune Pancreatitis: An Update on Classification, Diagnosis, Natural History and Management. Curr Gastroenterol Rep 14, 95–105 (2012). https://doi.org/10.1007/s11894-012-0246-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11894-012-0246-8