Abstract
During the last decade, positron emission tomography/computed tomography (PET/CT) and single-photon emission computed tomography/computed tomography (SPECT/CT) have procured advances in research and clinical application of fusion imaging. The recent introduction of systems that combine PET and MRI opens new horizons for multimodality molecular imaging. These systems offer simultaneous morphologic, functional, and molecular information of a living system. Moreover, other combinations of anatomic and functional imaging modalities (for example CT and MRI or PET and optical imaging) are emerging, holding promise in basic medical research or in clinical medicine. These developments are paralleled by advances in the field of biomolecules and particles, to provide new agents useful for more than one imaging modality and to facilitate the study of the same target by different imaging devices. In the near future PET/MRI may emerge as a new powerful multimodality technique in clinical oncology, offering considerable potential for imaging applications beyond correlation of functional and anatomic images. Future developments should include the simultaneous acquisition of multifunctional data such as PET tracer uptake, MR spectroscopy, or fMRI along with high-resolution anatomic MRI.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Attenuation Correction
- Vasoactive Intestinal Peptide
- Pituitary Adenylate Cyclase Activate Polypeptide
- Multimodality Imaging
- Multimodality System
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
To understand genetics of cancer and its proliferative nature remains the main objective of current cancer research. Improved knowledge of cancer pathogenesis results in an array of biomarkers to be used for diagnosis and treatment of the disease. Molecular imaging is the visualization, characterization and measurement of biological processes at the molecular and cellular levels in a living system. Molecular imaging techniques using radiotracers allow the demonstration of functional or phenotypic changes associated with pathology in vivo, and the characterization of both genotypic and phenotypic tumoral signatures.
During the last 10 years, positron emission tomography/computed tomography (PET/CT) and single-photon emission computed tomography/computed tomography (SPECT/CT) have procured advances in research and clinical application of fusion imaging unthinkable before, with simultaneous development of quantitative methods to measure absolute concentration of radiotracers related to the severity and/or progression of cancer.
The recent introduction of systems that combine PET and MRI is opening new horizons for multimodality molecular imaging to acquire simultaneously morphologic, functional, and molecular information of a living system. Moreover, other combinations of anatomic and functional imaging modalities (for example CT and MRI or PET and optical imaging) are emerging, holding promise in basic medical research or in clinical medicine. These developments are paralleled by advances in the field of biomolecules and particles, to provide new agents useful for more than one imaging modality and to facilitate the study of the same target by different imaging devices.
2 Technology and Probe Design
During the last 10 years, the introduction of multimodality systems combining CT with SPECT and PET has changed significantly the capabilities of stand-alone SPECT and PET. Fused functional and anatomic images have gained wide acceptance, becoming a powerful clinical tool, especially in oncology. With multimodality imaging as the current paradigm, present research efforts are focused on the integration of MRI with PET and SPECT (Patton et al. 2009).
2.1 SPECT/CT
New technologies have improved the performance of SPECT and SPECT/CT beyond the technology invented by Hal Anger in 1957 (Anger 1957). The initial primary goal of simultaneous SPECT and CT studies was to facilitate lesion localization and attenuation correction. Recently, with the implementation of diagnostic CT, clinical information from SPECT/CT has been significantly improved. In consequence, guidelines of clinical practice need to be adapted and clinical protocols for staging and restaging of cancer should incorporate SPECT/CT when necessary to facilitate precise diagnosis and to reduce patient radiation burden.
Involuntary motions because of cardiac contraction, respiration, or bowel movement are common technical problems encountered in SPECT/CT. Respiratory motion results in inaccuracy of attenuation correction for lung tumors because of eventual misregistration between emission and transmission data. Considerable research efforts are addressed to develop methods for correction of respiratory motion effects, such as external or internal devices that make possible to estimate respiratory motion gating emission data and the adequate matching to CT cine data, or the use of modeling motion and matching of CT data from a single CT and a respiratory gated emission study. Future developments should provide automated correction with minimal radiation dose. On the other hand, the role of attenuation correction in SPECT/CT for oncologic applications is not fully established, with a relatively small number of studies comparing the diagnostic accuracy of attenuated and non-attenuated SPECT images.
In future, silicon photodiode or solid-state materials incorporated to detectors may replace photomultiplier tube technology, improving spatial and energy resolutions, and increasing stability with a more compact size (Despres et al. 2007). Development of these new technologies, will improve overall performance and cost-effectiveness of future SPECT/CT equipment.
2.2 PET/CT
The introduction of combined PET/CT in 2001 opened a new era in the field of nuclear and molecular imaging, improving the sensitivity and specificity of clinical PET, and facilitating clinical acceptance and implementation of multimodality imaging (Beyer et al. 2000). Compared with two separated systems, the combination of PET and CT into a single gantry has provided the paradigm for multimodality imaging, and has improved and simplified clinical management of patients. PET/CT is now a critical component of diagnosis and treatment management of oncologic disease.
Continuing advances in PET technology include detectors with improved spatial resolution, increased axial field-of-view (aFOV) with subsequent improvement of sensitivity, faster and more efficient iterative reconstruction algorithms, and improved signal-to-noise by incorporating time-of-flight (TOF) information. Motion-free gated imaging is offered for specific applications, such to plan appropriate fields of radiotherapy.
The introduction of lutetium oxyorthosilicate, as faster scintillator than bismuth germinates, improves the count rate capability of PET scanners. The increased light output allows improved spatial resolution and energy resolution with reduction of scatter fraction. The dead-time of system is also decreased allowing reduction of the coincidence window and implementation of TOF. The increased aFOV offers an increase of sensitivity that improves spatial resolution. Moreover, increased aFOV procures fewer acquisition positions taking more advantage of the radiation emitted from the patient. The development of new PET image reconstruction algorithms broadens the point spread function or High-Definition PET or HD-PET and results in improved intrinsic resolution and uniformity throughout the FOV (Panin et al. 2006).
As it happens in SPECT/CT, motion between or during PET/CT studies may pose a technical problem, with remaining uncertainties in the registration process. The correction of respiratory motion effects, that may result in inaccuracy in attenuation correction for lung tumors, represents a challenge for PET/CT. Methods to reduce the effect of respiratory motion include breath hold during treatment, “gating” in which the beam is turned on or off in synchrony with the respiratory cycle and “tracking” in which the beam follows the tumor based on imaging technology (Bundschuh et al. 2008; Cheng et al. 2009; Chang et al. 2010). However, at present, the optimal approach that provides automated correction with minimal radiation dose has yet to be demonstrated.
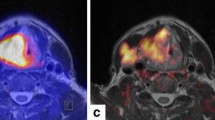
Accurate definition of the boundaries of active disease is of clinical relevance in guiding biopsy sites and in planning surgery and radiotherapy fields. PET/CT studies facilitate the correct anatomical delineation of 18F-FDG uptake optimizing biopsy and improving the planning of surgical procedures (Goerres et al. 2005). The better delineation of tumor tissue by PET/CT has supported the implementation of this multimodality system in radiation therapy planning of various tumors as non-small cell lung carcinomas, head and neck tumors, and lymphoma (Faria et al. 2008; Guido et al. 2009).
2.3 SPECT/MRI and PET/MRI
Since few years, numerous working prototypes of PET/MRI systems have been described and introduced (Catana et al. 2008; Judenhofer et al. 2008; Schlemmer et al. 2008). The combination of SPECT and PET with MRI can be important in areas where this technique is the preferred anatomic imaging modality. There are clear synergies between these modalities in areas where, beyond anatomic landmarking, MRI can detect organ-specific abnormalities and pathologies by spectroscopic quantification of concentrations of molecules. Moreover, the expected radiation dose for SPECT and PET/MRI is significantly less than that for SPECT and PET/CT, which may be of particular importance in oncologic patients that are followed with multiple studies to monitor disease progression and response to therapy.
A potential limitation of MRI in multimodality imaging systems is that this technique does not provide adequate information for attenuation correction of emission studies, being a challenge to separate air and bone, and to measure the variations of density in the lung. Attenuation correction based on MRI is an active area of research, and its developments will be key for future clinical applications of PET/MRI (Hofmann et al. 2008; Zaidi 2007).
To integrate SPECT and PET with MRI is a technical challenge because these systems can interfere each other. At present, several prototypes have been designed and are at various stages of development (Raylman et al. 2006; Woody et al. 2007). Even if to merge the hardware of SPECT or PET and MRI into a single device is limited by space, the principal challenge derives from conventional PET detectors based on photomultiplier tubes (PMTs), which do not operate properly in presence of the magnetic field of MRI. The consequent mutual interference between both image modalities needs to be reduced at maximum to provide high quality studies, as much PET as MRI. PET systems can interfere with MRI systems degrading the homogeneity of magnetic and radiofrequency fields resulting in a loss of image quality with presence of artifacts. On the other hand, the strong external magnetic field of MRI systems can interfere with PET systems deflecting the normal trajectory of electrons into the PMTs, and the radiofrequency field and the gradient system pulses can affect the electronic of PET producing artifacts on image. To solve mutual interference between PET and MRI, light fibers coupled to the scintillation crystals of PET detectors have been used, with only the MRI elements remaining in the magnetic field and directing the scintillations out this field through light fibers. Scintillation crystals produce several distortion and artifacts on MRI image, due to their different magnetic susceptibilities compared with human tissue. The replacement of photomultipliers tubes by solid-state scintillation detectors has been proposed and is being developed (Townsend 2008). These detectors, based on avalanche photodiodes, have the advantage that to be insensitive to magnetic fields and can be directly connected to the scintillation crystal block within the magnetic field using a short 1–2 mm light guide. In this way, light loss is minimized and the conversion of light to electronic signals takes place inside the MRI system, avoiding the use of optical fibers. Another advantage of avalanche photodiodes is that these are smaller than PMTs allowing a design with a fully integrated PET. This design has the advantages that no metallic components are placed directly in the MRI field of view and that the short light guides loss less light. At present, the design of compact systems using solid-state light detectors and based on superconducting magnet (split magnet) or on field cycling MRI, is a challenging task (Cherry et al. 2008). Certainly, new fully integrated PET/MR systems, eventually coupled to SPECT will be developed and become available in the near future.
3 Tracers
Tumors are hypermetabolic and may be distinguished from nonmalignant tissue by their elevated glucose metabolism. 18F-FDG is a nonspecific tracer for detecting malignant tumors employed for PET imaging and quantification of glucose metabolism in vivo. The standardized uptake value (SUV) is a simple semi-quantitative method widely used to standardize the 18F-FDG uptake. The presence or absence of 18F-FDG accumulation is used to characterize CT findings in multimodality imaging of cancer patients using PET/CT (Bar-Shalom et al. 2003; Gerth et al. 2007; Czernin et al. 2007; la Fougère et al. 2006; Raanani et al. 2006).
In parallel to the technological advances in PET/CT, positron emitter labeled radiopharmaceuticals beyond 18F-FDG are in continuing development, from isotopes such as 124I to highly specific compounds such as 68Ga-DOTATOC. 124I has favorable conditions as much for dosimetry as for quality of images. Its half-life of 4.2 days allows imaging over some biological half-lives of iodine accumulation in thyroid cancer metastases. In consequence, iodine accumulation in lesions even in the submillimeter range, may be detected because of lower background activity (Freudenbersg et al. 2008), with assessment of tumor volumes and adequate dosimetric calculations (Jentzen et al. 2008a, b). As example of highly specific tracer, 68Ga-DOTATOC binds to somatotropin receptors, which are frequently overexpressed in neuroendocrine tumors that may be clinically active even when having very little dimensions. Therefore, their early detection represents an important clinical challenge (Buchmann et al. 2007). Other tracers available for PET/CT, such as as choline labeled with 11C or 18F for prostate cancer, may be less specific. These radiopharmaceuticals are inhomogeneously distributed in the background and may shows some nonspecific binding in the intestine, being the tumor specific binding only moderate (Bouchelouche and Oehr 2008).
New PET compounds for multimodality imaging include those capable to target specific key biologic processes in oncogenesis, such as proliferation (18F-3-fluoro-3-deoxy-L-thymidine [18F-FLT]), hypoxia (18F-fluoromisonidazole [18F-FMISO] and 18F-fluoroazomycin arabinoside [18F-FAZA]), angiogenesis (18F-galacto-arginine-glycine-aspartic acid [18F-galacto-RGD]), and apoptosis (124I- or 64Cu-Annexin V). Imaging of these biologic targets is expected to provide meaningful information for the selection and monitoring of targeted therapy in individual cancer patients, facilitating personalized treatment of the disease.
18F-FMISO is a highly stable radiopharmaceutical directly derived from misonidazole and is the most extensively studied PET agent for hypoxia mapping. 18F-FMISO shows high accumulation in hypoxic tissue which is proportional to the hypoxic fraction of the tumor. PET/CT using 18F-FMISO offers the possibility of in vivo mapping of regional tumor hypoxia, identifying patients who may benefit from changes in their therapeutic regimen because hypoxia has been identified as a major adverse prognostic factor for tumor progression and for resistance to anticancer treatment. In addition, such mapping of hypoxia can be used to guide intensity-modulated radiotherapy (Rajendran et al. 2003; Hicks et al. 2005). At present, assessment of therapy response with hypoxia tracers is still experimental.
The thymidine analog 18F-FLT, derived from the cytostatic drug azidovudine, has been suggested for noninvasive assessment of proliferation and more specific tumor imaging than 18F-FDG. This tracer is stable in vitro and accumulates in proliferating tissues and malignant tumors (Shields et al. 1998; Wells et al. 2002). However, at present the uptake mechanism of 18F-FLT is only partially understood, and the influence of membrane transporters and various nucleoside-metabolizing enzymes remains to be determined. Preliminary data have described a significant correlation between tumoral proliferation and 18F-FLT uptake in various malignant tumors, suggesting that 18F-FLT could be used for therapeutic monitoring in various clinical settings (Salskov et al. 2007; Bading and Shields 2008). Clinical trials are needed to further validate 18F-FLT as a marker for therapy response.
At present, one of the primary goals in cancer research is to increase the knowledge on genetics of cancer and its proliferative nature. Along this line, non-somatostatin receptors biomarkers overexpressed on the surface of malignant cell have been explored. These are VPAC receptors, a family of 3G protein-coupled receptors located on the plasma membrane of tumor cells that mediate the biological action of vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase activating polypeptide (PACAP). These receptors are present on several common tumors, as breast, prostate, bladder, and colon, and VIP and PACAP can be labeled with 99mTc and also with 64Cu, with opportunities to image these oncologic diseases early and specifically in the future (Germano et al. 2004; Schulz et al. 2004).
Another exciting and challenging goal in cancer research is the possibility to target intracellular biomarkers for diagnostic application. It has been demonstrated that oncogene expression of tumoral cells is different from their normal cohorts. Targeting specific oncogene mRNAs copies with 99mTc and 64Cu for SPECT or PET in dividing cells may permit imaging of oncogene expression in several tumors. This technique could be also useful to monitor effectiveness of therapy, with assessment of the upregulation or downregulation of oncogene mRNA copies and of proliferative tumoral status after treatment (Lendvai et al. 2009; Chakrabarti et al. 2005, 2007; Tian et al. 2004, 2005, 2007).
Molecular biology is rapidly progressing and offering new opportunities to molecular imaging. In the future, by use of new imaging probes it may be possible to determine cellular transcription in a cell or its rate of proliferation, predicting its susceptibility for cancer. At present, studies have examined the utility to assess tumor suppressor gene p53 transcription in a cell or to determine the expression of Ki-67 protein as proliferative index of tumoral cells (Shah et al. 2009; Tan et al. 2005). Currently, therapeutic approaches are focused to block the division of cells, even if these approaches do not discriminate between normal and cancerous cells. To increase cell specificity, antisense technology has emerged. It is based on the sequence-specific binding of an antisense oligonucleotide to target RNA, preventing the oncogene mRNA translation, and modulating the oncogene expression involved in the pathogenesis of oncologic diseases (Lendvai et al. 2009; Hersey et al. 2009). However, at present there are still some challenges to be resolved, as in vivo stability, sequence length, and poor uptake in malignant cells. Moreover, the high costs of targeted therapy approaches and the considerable toxic side-effects are important obstacles for to overcome. Major challenges of new targeted therapy approaches comprise the identification of the correct concentration of therapeutic agent and its dose schedule, the selection of patients suitable to benefit from treatment, and the assessment of the response of the tumor to therapy (Bennett and Swayze 2010). There are opportunities for targeted molecular multimodality imaging to help in all those challenges and to offer new means for non-invasive assessment of cancer biology.
Main existing PET tracers of 18F and of other positron-emitting radionuclides available for multimodality molecular imaging and their biochemical process, mechanism of uptake and localization are respectively shown in Tables 1 and 2.
4 Optical Imaging
Optical techniques allow imaging of fluorescently tagged living cells in three dimensions with a high sensitivity down to the single-molecule level, with high submicrometric spatial resolution and with temporal resolution in the order of a millisecond. However, these techniques have limited penetration depth of light in living tissue, while the commonly used organic fluorophores and genetically encoded fluorescent proteins are often insufficiently bright and stable. Moreover, the toxic radicals and photoproducts generated prevent long-term in vivo imaging.
At present, advances in nanotechnology offer a vast array of artificial particulate systems capable of targeting different cells in vivo. The most desirable property of such nanoparticles is multifunctionality, containing both therapeutic components and multimodality imaging labels for efficient, specific in vivo delivery of drugs and for accurate quantitative assessment of the therapeutic efficacy noninvasively over time. Described nanoparticles are of several natures and include quantum dots, colloidal gold, superparamagnetic iron-oxide crystals, dendrimers, polymeric micelles and liposomes, nanotubes, nanowires, nanoshells, and others (Kirui et al. 2010; Hu et al. 2009; Bentolila et al. 2009). Molecules, such as peptides, proteins, and antibodies can be attached to these nanoparticles to perform PET, SPECT, MRI, ultrasound as well as optical imaging. Research on nanoparticles is focused on optimization of biocompatibility, in vivo kinetics, targeting efficacy, toxicity, and cost-effectiveness. These new nanoparticles and derived imaging probes will need to be translated into clinical applications.
Bioluminescence imaging is related to the light produced by the enzymatic reaction of a luciferase enzyme with its substrate. The most frequent luciferase enzyme used is the firefly (Photinus pyralis) luciferase. It is commonly used for preclinical cellular and molecular imaging in small animals. At present, bioluminescence imaging is a powerful tool to assess mechanisms of disease and to promote drug development in preclinical models. On the other hand, fluorescence imaging is obtained from a target fluorescent molecule that is excited by an external light of appropriate wavelength. This process is followed by release of longer-wavelength, lower-energy light as signal for imaging. Targets for fluorescence imaging may be endogenous molecules, as collagen or hemoglobin, fluorescent proteins or optical contrast agents that can be used for cellular and molecular imaging in small animal models. Both optical techniques have been used to assay pharmacodynamics of therapeutic agents in vivo, establishing dosing parameters to guide initial clinical trials, and eventual clinical applications (Erickson et al. 2010). Future challenges include the improvement and development of new near-infrared spectroscopic methods useful for to identify cancer biomarkers and to retrospectively determine if benign and malignant lesions could be distinguished by using these methods (Kukreti et al. 2010).
Prototype instruments for optical/PET and optical/SPECT in small animals are under development in research laboratories (Peter and Semmler 2006; Vu et al. 2006). Hybridizing nuclear medicine and optical imaging systems can serve as a translational platform between the widely used bioluminescent or fluorescent techniques in small animal models, and the nuclear radiotracer medicine assays in human (Cherry 2004). The same rationale can be applied to optical imaging and MRI, localizing any significant and little optical signal on high-resolution 3D structural imaging. A promising line lies on the development of handheld-based optical imaging devices for the purpose of in vivo clinical studies, in particular in minimally invasive surgical environments. At present, there are new devices for in vivo clinical studies with demonstrated ability to perform fast 2D imaging and to detect a fluorescent target within a heterogeneous tissue-mimicking background as well as real human tissue (Erickson et al. 2010).
5 Future and Conclusions
Molecular imaging employing multimodality systems will strongly influence the practice of medicine in the next generations. Specific imaging biomarkers will be developed to enable physicians to ensure better strategies of patient management, to stratify cancer, and to perform personalized medicine. Smarter devices, coupling different imaging modalities, with higher spatial resolution and greater sensitivity will be developed, allowing the visualization of a cluster of cells in vivo. These smart devices will use smart probes to target specific biologic phenomena that will provide a true early diagnosis and will drive the design of therapy and the assessment of its effectiveness.
Even if PET/CT with 18F-FDG for tumor imaging will ultimately replace SPECT/CT, advances in SPECT instrumentation, CT technology, and development of radiotracers have the potential to advance SPECT/CT beyond its current level of performance. The horizon for SPECT/CT imaging lies in the development of new tumor-specific agents that can improve oncologic clinical diagnostic and therapeutic applications.
In the near future PET/MRI may emerges as a new powerful multimodality technique in clinical oncology, offering considerable potential for imaging applications beyond simply correlation of functional and anatomic images. Future developments should include the simultaneous acquisition of multifunctional data, such as PET tracer uptake, MR spectroscopy, or fMRI along with high-resolution anatomic MRI.
The use of imaging as a surrogate endpoint requires demonstration of a significant relationship between imaging results and clinical outcome. Cooperation with the pharmaceutical and the instrumentation industry is needed to foster prospective randomized multicenter trials that are mandatory to demonstrate the relationship between appropriate use of multimodality imaging and better patient outcomes.
References
Anger HO (1957) Scintillation camera. Rev Sci Instrum 29:27–33
Bading JR, Shields AF (2008) Imaging of cell proliferation: status and prospects. J Nucl Med 49:64S–80S
Bar-Shalom R, Yefremov N, Guralnik L et al (2003) Clinical performance of PET/CT in evaluation of cancer: additional value for diagnostic imaging and patient management. J Nucl Med 44:1200–1209
Bennett CF, Swayze EE (2010) RNA targeting therapeutics: molecular mechanisms of antisense oligonucleotides as a therapeutic platform. Annu Rev Pharmacol Toxicol 50:259–293
Bentolila LA, Ebenstein Y, Weiss S (2009) Quantum dots for in vivo small-animal imaging. J Nucl Med 50:493–496
Beyer T, Townsend DW, Brun T et al (2000) A combined PET/CT scanner for clinical oncology. J Nucl Med 41:1369–1379
Bouchelouche K, Oehr P (2008) Positron emission tomography and positron emission tomography/computerized tomography of urological malignancies: An update review. J Urol 179:34–45
Buchmann I, Henze M, Engelbrecht S et al (2007) Comparison of 68Ga-DOTATOC PET and 111In-DTPAOC (Octreoscan) SPECT in patients with neuroendocrine tumours. Eur J Nucl Med Mol Imaging 34:1617–1626
Bundschuh R, Martínez-Möller A, Essler M et al (2008) Local motion correction for lung tumours in PET/CT—First results. Eur J Nucl Med Mol Imaging 35:1981–1988
Catana C, Procissi D, Wu YB et al (2008) Simultaneous in vivo positron emission tomography and magnetic resonance imaging. Proc Natl Acad Sci USA 105:3705–3710
Chakrabarti A, Aruva MR, Sajankila SP (2005) Synthesis of novel peptide nucleic acid-peptide chimera for non-invasive imaging of cancer. Nucleosides Nucleotides Nucleic Acids 24:409–414
Chakrabarti A, Zhang K, Aruva MR et al (2007) Radiohybridization PET imaging of KRAS G12D mRNA expression in human pancreas cancer xenografts with [64Cu]DO3A-peptide nucleic acid-peptide nanoparticles. Cancer Biol Ther 6:948–956
Chang G, Chang T, Pan T, Clark JW Jr, Mawlawi OR (2010) Implementation of an automated respiratory amplitude gating technique for PET/CT: clinical evaluation. J Nucl Med 51:16–24
Cheng NM, Yu CT, Ho KC, Wu YC, Liu YC, Wang CW, Yen TC (2009) Respiration-averaged CT for attenuation correction in non-small-cell lung cancer. Eur J Nucl Med Mol Imaging 36:607–615
Cherry SR (2004) In vivo molecular and genomic imaging: new challenges for imaging physics. Phys Med Biol 49:R13–R48
Cherry SR, Louie AY, Jacobs RE (2008) The integration of positron emission tomography with magnetic resonance imaging. Proc IEEE 96:416–438
Czernin J, Allen-Auerbach M, Schelbert HR (2007) Improvements in cancer staging with PET/CT: literature-based evidence as of september 2006. J Nucl Med 48:78S–88S
Despres P, Funk T, Shah KS et al (2007) Monte Carlo simulations of compact gamma cameras based on avalanche photodiodes. Phys Med Biol 52:3057–3074
Erickson SJ, Ge J, Sanchez A, Godavarty A (2010) Two-dimensional fast surface imaging using a handheld optical device: in vitro and in vivo fluorescence studies. Transl Oncol 3:16–22
Faria SL, Menard S, Devic S, Sirois C, Souhami L, Lisbona R, Freeman CR (2008) Impact of FDG-PET/CT on radiotherapy volume delineation in non-small-cell lung cancer and correlation of imaging stage with pathologic findings. Int J Radiat Oncol Biol Phys 70:1035–1038
Freudenberg LS, Antoch G, Frilling A et al (2008) Combined metabolic and morphologic imaging in thyroid carcinoma patients with elevated serum thyroglobulin and negative cervical ultrasonography: role of 124I-PET/CT and FDG-PET. Eur J Nucl Med Mol Imaging 35:950–977
Germano PM, Le SV, Oh DS et al (2004) Differential coupling of PAC1 SV1 splice variant of human colonic tumors to the activation of intracellular cAMP but not intracellular Ca2+ does not activate tumor proliferation. J Mol Neurosci 22:83–92
Gerth HU, Juergens KU, Dirksen U et al (2007) Significant benefit of multimodal imaging: PET/CT compared with PET alone in staging and follow-up of patients with Ewing tumors. J Nucl Med 48:1932–1939
Goerres GW, Stupp R, Barghouth G et al (2005) The value of PET, CT and in-line PET/CT in patients with gastrointestinal stromal tumours: long-term outcome of treatment with imatinib mesylate. Eur J Nucl Med Mol Imaging 32:153–162
Guido A, Fuccio L, Rombi B, Castellucci P, Cecconi A, Bunkheila F, Fuccio C, Spezi E, Angelini AL, Barbieri E (2009) Combined 18F-FDG-PET/CT imaging in radiotherapy target delineation for head-and-neck cancer. Int J Radiat Oncol Biol Phys 73:759–763
Hersey P, Bastholt L, Chiarion-Sileni V, Cinat G, Dummer R, Eggermont AM, Espinosa E, Hauschild A, Quirt I, Robert C, Schadendorf D (2009) Small molecules and targeted therapies in distant metastatic disease. Ann Oncol 20:(Suppl6) vi35–40
Hicks RJ, Rischin D, Fisher R et al (2005) Utility of FMISO PET in advanced head and neck cancer treated with chemoradiation incorporating a hypoxia-targeting chemotherapy agent. Eur J Nucl Med Mol Imaging 32:1384–1391
Hofmann M, Steinke F, Scheel V et al (2008) MRI-based attenuation correction for PET/MRI: a novel approach combining pattern recognition and atlas registration. J Nucl Med 49:1875–1883
Hu R, Yong K-T, Roy I, Ding H, He S, Prasad PN (2009) Metallic nanostructures as localized plasmon resonance enhanced scattering probes for multiplex dark field targeted imaging of cancer cells. J Phys Chem C Nanomater Interfaces 113:2676–2684
Jentzen W, Freudenberg L, Eising EG et al (2008a) Optimized 124I PET dosimetry protocol for radioiodine therapy of differentiated thyroid cancer. J Nucl Med 49:1017–1023
Jentzen W, Weise R, Kupferschläger J et al (2008b) Iodine-124 PET dosimetry in differentiated thyroid cancer: recovery coefficient in 2D and 3D modes for PET(/CT) systems. Eur J Nucl Med Mol Imaging 35:611–623
Judenhofer MS, Wehrl HF, Newport DF et al (2008) Simultaneous PET-MRI: a new approach for functional and morphological imaging. Nat Med 14:459–465
Kirui DK, Rey DA, Batt CA (2010) Gold hybrid nanoparticles for targeted phototherapy and cancer imaging. Nanotechnology 21:1–10
Kukreti S, Cerussi AE, Tanamai W, Hsiang D, Tromberg BJ, Gratton E (2010) Characterization of metabolic differences between benign and malignant tumors: high-spectral-resolution diffuse optical spectroscopy. Radiology 254:277–284
la Fougère C, Hundt W, Bröckel N et al (2006) Value of PET/CT versus PET and CT performed as separate investigations in patients with Hodgkin’s disease and non-Hodgkin’s lymphoma. Eur J Nucl Med Mol Imaging 33:1417–1425
Lendvai G, Estrada S, Bergström M (2009) Radiolabelled oligonucleotides for imaging of gene expression with PET. Curr Med Chem 16:4445–4461
Panin VY, Kehren F, Michel C et al (2006) Fully 3-D PET reconstruction with system matrix derived from point source measurements. IEEE Trans Med Imaging 25:907–921
Patton JA, Townsend DW, Hutton BF (2009) Hybrid imaging technology: from dreams and vision to clinical devices. Semin Nucl Med 39:247–263
Peter J, Semmler W (2006) Performance investigation of a dual-modality SPECT/optical small animal imager. Eur J Nucl Med Mol Imaging 33:S117–S117
Raanani P, Shasha Y, Perry C et al (2006) Is CT scan still necessary for staging in Hodgkin and non-Hodgkin lymphoma patients in the PET/CT era? Ann Oncol 17:117–122
Rajendran JG, Wilson DC, Conrad EU et al (2003) [18F-]FMISO and [18F-]FDG PET imaging in soft tissue sarcomas: correlation of hypoxia, metabolism and VEGF expression. Eur J Nucl Med Mol Imaging 30:695–704
Raylman RR, Majewski S, Lemieux SK et al (2006) Simultaneous MRI and PET imaging of a rat brain. Phys Med Biol 51:6371–6379
Salskov A, Tammisetti VS, Grierson J, Vesselle H (2007) FLT: measuring tumor cell proliferation in vivo with positron emission tomography and 3’-deoxy-3’-[18F]fluorothymidine. Semin Nucl Med 37:429–439
Schlemmer HPW, Pichler BJ, Schmand M et al (2008) Simultaneous MR/PET imaging of the human brain: feasibility study. Radiology 248:1028–1035
Schulz S, Rocken C, Mawrin C et al (2004) Immunocytochemical identification of VPAC1, VPAC2 and PAC1 receptors in normal and neoplastic human tissues with subtype specific antibodies. Clin Cancer Res 10:8234–8242
Shah C, Miller TW, Wyatt SK, McKinley ET, Olivares MG, Sanchez V, Nolting DD, Buck JR, Zhao P, Ansari MS, Baldwin RM, Gore JC, Schiff R, Arteaga CL, Manning HC (2009) Imaging biomarkers predict response to anti-HER2 (ErbB2) therapy in preclinical models of breast cancer. Clin Cancer Res 15:4712–4721
Shields AF, Grierson JR, Dohmen BM et al (1998) Imaging proliferation in vivo with 18F-FLT and positron emission tomography. Nat Med 4:1334–1336
Tan PH, Bay BH, Yip G et al (2005) Immunohistochemical detection of Ki67 in breast cancer correlates with transcriptional regulation of genes related to apoptosis and cell death. Mod Pathol 18:374–381
Tian X, Aruva MR, Qin W et al (2004) External imaging of CCND1 cancer gene activity in experimental human breast cancer xenografts with 99mTc-peptide–peptide nucleic acid-peptide chimeras. J Nucl Med 45:2070–2082
Tian X, Aruva MR, Wolfe HR et al (2005) Tumor-targeting peptide-PNA peptide chimeras for imaging overexpressed oncogene mRNAs. Nucleosides Nucleotides Nucleic Acids 24:1085–1091
Tian X, Aruva MR, Zhang K et al (2007) PET imaging of CCND1 mRNA in human MCF7 estrogen receptor positive breast cancer xenografts with oncogene-specific [64Cu] chelator-peptide nucleic acid-IGF1 analog radiohybridization probes. J Nucl Med 48:1699–1707
Townsend DW (2008) Multimodality imaging of structure and function. Phys Med Biol 53:R1–R39
Vu NT, Silverman RW, Chatziioannou AF (2006) Preliminary performance of optical PET (OPET) detectors for the detection of visible light photons. Nucl Instrum Methods 569:563–566
Wells P, Gunn RN, Alison M et al (2002) Assessment of proliferation in vivo using 2-[11C] thymidine positron emission tomography in advanced intra-abdominal malignancies. Cancer Res 62:5698-5702
Woody C, Schlyer D, Vaska P et al (2007) Preliminary studies of a simultaneous PET/MRI scanner based on the RatCAP small animal tomograph. Nucl Instrum Methods A 571:102–105
Zaidi H (2007) Is MR-guided attenuation correction a viable option for dualmodality PET/MR imaging? Radiology 244:639–642
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Estorch, M., Carrio, I. (2013). Future Challenges of Multimodality Imaging. In: Schober, O., Riemann, B. (eds) Molecular Imaging in Oncology. Recent Results in Cancer Research, vol 187. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-10853-2_14
Download citation
DOI: https://doi.org/10.1007/978-3-642-10853-2_14
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-10852-5
Online ISBN: 978-3-642-10853-2
eBook Packages: MedicineMedicine (R0)