Abstract
It has been defined by Conn and colleagues in 2000 that “Cardiac remodelling may be characterized as genome expression, molecular, cellular and interstitial changes that are manifested clinically as changes in size, shape and function of the heart after cardiac injury”, associated with ventricular dysfunction, malignant arrhythmias and poor prognosis. Conversely, the various definitions of cardiac remodelling stress on common molecular, biochemical, and mechanical pathways. Although the right ventricle and left ventricle show significant distinctions in embryology, form, and function, they have many similar findings when they adjust to damaging loading or when they fail. Having a number of key differentiations in their molecular response to failure this offer a future platform for right ventricle for a particular therapeutic intervention. It has been suggested by Friedberg and Redington in 2014 that “Focus on the molecular pathways specific to the failing right ventricle, and targeting the interactions between both ventricles may guide to successful treatments for the right ventricle and left ventricle failure”. A shortly review is made with updated information for all factors that cause and affect cardiac remodelling process, especially in case of right heart.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
To date, the term ‘cardiac remodelling’ (CR) was firstly coined by Hockman and Buckey on myocardial infarction (MI) to study replacement of myocardial injury with scar tissue [1]. Later, Janice Pfeffer applied the name CR to illustrate the progressive dilatation of the left ventricle (LV) on vivo studies [2]. Nonetheless, Pfeffer and Braunwald utilized the term CR for morphological changes caused by MI, especially for LV remodelling [3]. In this regard, an international forum published in 2000 a consensus on CR, that defined “CR as a group of molecular, cellular and interstitial changes that clinically manifest as changes in size, shape and function of the heart resulting from cardiac injury” [4]. In biology, the term remodelling characterizes adjustments that cause reorganizing of initial structures [5]. Even if CR was used initially to describe the geometric and structural modifications caused by MI [3, 6], CR is actually applied to a large variety of cardiac conditions. Esentially, Swynghedauw classified etiology of CR as being (1) acquired diseases (postmyocardial infarction, hypertensive cardiopathy, valve and congenital disease, myocarditis, and Chagas disease); (2) genetics (inherited cardiomyopathies, familial hypertrophic cardiomyopathy, dilated cardiomyopathy, Marfan disease, hemochromatose, transgenic models, transgenic models of cardiac hypertrophy, transgenic models of cardiac failure); and (3) miscellaneous causes (aging; heart rate; use of catecholamines, thyroxine, or growth hormone; salt, mineralo- and glucocorticoid; diabetes mellitus; B6 vitamin deficiency; atrophy due to heterotopic transplantation and hypertrophy due to homeotopic transplantation (?)) [5, 7, 8]. Further, CR is separated into structural (hypertrophy and fibrosis) and electrical remodelling . Shortly, any type of stress induces cardiomyocytes (CMs) to become hypertrophic with altered electrical function, while cardiac fibroblasts (CFs) transform in ‘activated’ myofibroblasts (MyoFb), which further multiply and boost extracellular matrix (ECM) tissue with fibrosis [9].
During international forum from 2000 [4], two types of CR were established: (1) physiological (adaptive) remodelling and (2) pathological remodelling. Further, Dorn et al. defined CR as being ‘adaptive or maladaptive’ [10]. It should be noted, that Hill and Olson stated that heart can respond to environmental stimuli by increase of myocardial mass or atrophy starting with a “least 100%” [11]. More important is other mechanisms than remodelling also can alter the evolution of heart disease, even in the absence of remodelling process. To reiterate, CR can be a physiologic or pathologic condition [4]. Physiologic CR is a physiological alteration in size and function of the heart due to physiologic stimuli such as exercise (“athlete’s heart”) and pregnancy. In addition, pathologic CR occurs with pressure overload conditions (e.g., aortic stenosis, hypertension), with volume overload conditions (e.g., valvular regurgitation), with cardiac injury or coronary artery disease (CAD) , and with inflammatory myocardial disease (e.g., myocarditis), or idiopathic dilated cardiomyopathy [4]. Equally, physiologic CR may lead to pathologic remodelling [12].
Constrictive pericardial disease, selected forms of congenital heart diseases (CHD) , inflow obstruction, primary myocardial disease, and pressure or volume overload are each well-described causes of right ventricular (RV) remodelling , RV systolic dysfunction, and cor pulmonale [13]. Emerging evidence suggests that RV dysfunction is the mainly marker of poor prognosis in pulmonary hypertension (PH) [14, 15].
For simplicity, the first adaptive reaction of the RV to pressure overload is hypertrophy. If untreated, the RV dilates to compensate increased RV preload and to maintain stroke volume according to the Frank-Starling principle. When further increase in RV end-diastolic filling volume do not balance progressive RV contractile dysfunction, clinically evident RV failure ensues. In advanced stages, RV dilation may also impair LV diastolic filling kinetics that contributes further to global pump dysfunction and, consequently, to the congestive heart failure (CHF) syndrome [16].
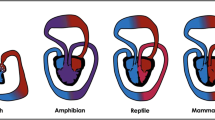
It should be restated that the RV and the LV don’t have same embryologic origins. The RV stems from the secondary/anterior heart tube and the LV from early/primary heart tube [17]. Accordingly, RV formation is specifically controlled by several genes, including Hand2 and Tbx20 [18]. This different embryologic origin of RV is associated with cellular divergence that controls the duration of early development to different LV and RV cardiomyocytes, and go on with distinct cell signalling and Ca2+ handling pathways for both chambers, altogether suggestive of certain essential differentiation at the cellular level for both ventricles [19]. For the foetal period, the RV propels blood into the pulmonary circulation, placenta and into the inferior body. Further, during the switch from the foetal circulation to the postnatal circulation with the reduction of pulmonary vascular resistance (PVR), the RV develops into a thin-walled, heavily trabeculated chamber pushing a cardiac output (CO) same to the LV but with lesser energy cost [20]. Normal crescent–shaped RV with thinner walls is a low-pressure chamber that faces the low impedance of pulmonary circulation. Thus, although the RV is a low-resistance and low-capacitance pump, the LV is an high-resistance and high-pressure pump [20]. Additionally, the RV has a different metabolism and morphology in comparison with LV [20]. RV cardiomyoytes are disposed longitudinally and demonstrate faster twitch velocities than the radially oriented LV cardiomyocytes. As a result, because of these anatomical and physiological differences, both ventricles present various reactions to disease forms. According to current evidences, it seems that RV hypertrophy (RVH), RV remodelling and RV failure (RVF) can develop at the same time instead of progression development (Fig. 4.1) [21].
(a) An overview of changes associated with RV pressure overload. Key triggers of RV pressure overload include pulmonary hypertension, RV outflow tract obstruction or RV being the systemic ventricle. RV pressure overload induces RVH that, through remodelling, leads to RV failure. It is of note, however, that RV failure is a continuous process and may begin as the time of hypertrophy and remodelling rather than being seen as a sequential process. (b) Effect of RVH-induced ischaemia. RVH is characterised by tissue hypoxia arising from ischaemia and microcirculatory insufficiency. Ischaemia-derived ROS, through the activation of transcription factors, drive the metabolic remodelling, contractile dysfunction and fibrosis that occur in RV failure. RVH, RV hypertrophy; PA, pulmonary artery; ROS, reactive oxygen species; MMPs, matrix metalloproteinases. (From Iacobazzi [21]. It is an open access article)
Also, in response to increased afterload, there is an activation of the foetal gene pattern in RV, re-expressing of genes from normal foetal RV. This includes a shift from α- to β-myosin heavy chain expression and an increase in adrenergic receptors, calcineurin activation [22,23,24], and phosphodiesterase type-5 (PDE5) expression [25]. The foetal gene pattern re-expression, particularly the myosin heavy chain shift from the α to β isoform, an hallmark of foetal gene reactivation, is also triggered in LV failure (LVF) [22].
Further, using microarray gene chip studies of mice, Urashima et al. compared LV hypertrophy (LVH) from aortic banding with RVH from pulmonary banding, and they demonstrated both similar and different LV and RV adaptive mechanisms [26]. One pathway that is more activated in the pressure-loaded RV compared with the pressure-loaded LV is the Wnt signalling pathway (Fig. 4.2) [27,28,29]. Wnt regulates glycogen synthesis kinase-3b activity, a serine/threonine protein kinase active in multiple intracellular signalling pathways, including cell proliferation, migration, inflammation, glucose regulation, and apoptosis [28, 29]. Also, there are multiple variation concerning the RV and LV in their adaptation to increased loading and likely differences in metabolism, mitochondrial remodelling, and glycolysis-to glucose oxidation coupling. These metabolic changes may subsequently lead to hyperpolarization of the mitochondrial membrane potential in RV hypertrophy, inefficient energy metabolism, and increased lactate production at an earlier stage of maladaptation compared with the LV [30].
The Wnt/β-catenin signaling pathway . In the Wnt-off state, defined by the absence of an active Wnt ligand, β-catenin is phosphorylated by the destruction complex (formed from the two kinases Gsk3 and Ck1, the scaffolding protein Axin, and the tumor suppressor Apc) and degraded by the ubiquitin-proteasome pathway. In the Wnt-on state, active Wnt ligands interact with the Fz receptors and the Lrp5/6 coreceptor. Phosphorylation of Lrp5/6 by Gsk3 and Ck1 recruits Dvl and Axin to the receptor complex and hence inhibits the destruction complex. This, in turn, inhibits β-catenin phosphorylation and stabilizes β-catenin in the cytoplasm. β-catenin is then translocated into the nucleus, by a complex including Fam53b/Smp, and regulates target gene expression with the Tcf/Lef transcription factors. Many modulators including the inhibitors sFrps and Wif are known to tightly regulate the signaling cascade. (From Ozhan et al. [27]. It is an open access article)
In CR process, several cell markers may indicate an undergoing CR progression, as well as alterations with an rise in α- and a reduction in β-myosin heavy chain, raised exhibition of Glucose transporter type (GLUT)-1, α-actin, natriuretic peptides, galectin, caveolin, neuronal nitric oxide synthase (NOS), angiotensin-converting enzyme (ACE), reduction of GLUT-4, sarcoplasmic/endoplasmic reticulum Ca(2+)ATPase 2a (SERCA 2a), and a change from free fatty acids oxidation to glucose metabolism [31, 32].
To sum up, cardiac dysfunction is the most important effect of CR. Because of cardiac injury, CR begin with genetic alterations, with reexpression of foetal genes, with cellular and molecular modifications, and gradually damage of ventricular function that develops with signs and symptoms of HF (Fig. 4.3) [4, 31, 33,34,35].
Sequence of events from cardiac injury to cardiac dysfunction. (From Azevedo [33]. It is an open access article)
2 Adaptive Versus Maladaptive Cardiac Remodelling
As already stated, CR is an adjusting and a maladaptive process. The adjusting process sustains heart function due to pressure overload or volume overload in case of acute cardiac injury [36]. Even if CAD affects directly RV with regional or global ischemia, RV physiology and RVF are mainly influenced by raised preload or afterload [20]. It has to be underlined that RV is exclusively dependent on afterload. Even small changes in total PVR, as demonstrated by modest increases in mean airway pressure during positive pressure ventilation, can reduce RV contractile performance and lower CO even when RV preload is maintained [37]. In contrast, significant changes in LV afterload may induces only modest changes in LV stroke volume [38]. Although patients with acute changes in systemic vascular resistance can compensate over a wide range, those with acute pulmonary arterial hypertension (PAH) if associate acute lung failure, often develop overt RVF and compromised CO [20]. In the largest part of clinical scenarios, even acute mild/moderate raises in RV afterload produce significant falls in RV output, including PAH and RV outflow obstruction, with the mention that usually changes in afterload are chronic and occur progressively [20]. Undeniably, in the chronic conditions, the relative increase in RV afterload is much greater in PAH than the increase in LV afterload in systemic hypertension [20].
Only that, long-term CR is damaging and correlated with a weak prognosis [39, 40]. Significant CR causes the increase of failing cardiac function [39, 41] that is related with bad prognosis especially for MI [40]. Actually, there is no evidence to suggest the time of occurrence from adaptive remodelling to maladaptive remodelling or if CR can be recognized at right moment. For instance, continuing CR is usual after an initial, moderately large anterior MI, but is uncommon after an initial small inferior MI [41]. CR after acute MI involving the LV may progress with LV dilatation and with later RV dilatation. Biventricular (BiV) remodelling comprises a group of patients with extremely poor outcomes [42]. Importantly, BiV failure is regarded as the terminal phase of CR [43, 44]. On the other hand, there is no clear knowledge regarding the effects of acute MI of LV and RV remodelling. It seems that the most important pathophysiological mechanism is the PH followed by raise of the RV afterload.
It should be mentioned that about 50% of patients with cardiac failing will die in five years. Moreover, about 40% of patients with HF die during first one year of hospitalization [45]. Also, an important number of deaths related with CR and cardiac failing are produced by sudden death [46] suggestive of the fact that an asymptomatic patient doesn’t mean a convinced good prognosis. In the face of raised survival with up-to-date current treatments, death rates have inadmissible values [47].
3 Basic Concepts of Cardiac Remodelling
As already mentioned that “CR may be characterized as genome expression, molecular, cellular and interstitial changes that are manifested clinically as changes in size, shape and function of the heart after cardiac injury” [4], the myocyte or cardiomyocyte (CM) is the most important cardiac cell implicated in the CR process. Conversely, the various explanations of CR share common molecular, biochemical, and mechanical pathways. Furthermore, the interstitium, fibroblasts, collagen, coronary vasculature, hemodynamic load, and neurohumoral activation affect the process of CR. A shortly review is made with updated information for all factors that influence CR process especially in case of right heart.
3.1 Functional Changes
RV and LV are different in their anatomy and physiology. Moreover, morphologically and functionally, both ventricles are comprehensible linked not only in health but also as they react to disease [20]. In same time, alterations in ventricular mass, and changes in composition and volume negatively modify the cardiac function [39, 41, 48,49,50]. As CR continues over time, the heart dilates and becomes spherical instead of elliptical form [51, 52], with thinning of cardiac walls and mitral valve incompetence. Even so, the evolution of CR depends on the primary disease, the severity of the underlying disease, genotype, intermittent ischemia episodes, neuroendocrine activation, and recommended treatment [41, 53, 54].
3.2 Cellular and Molecular Changes
It should be emphasized that CR is related with numerous cellular changes as well as myocite hypertrophy, deficit of myocytes due to apoptosis [55,56,57] or necrosis [58], fibroblast proliferation [59] and fibrosis [60, 61]. At molecular level, recent literature has highlighted differences between the RV and LV in the expression of genes involved in the response to pressure loading and failure [62]. Some of these differences are detailed in the following text and are summarized in Table 4.1 [20, 25, 27, 63,64,65,66,67,68,69, 71, 72].
3.3 The Cardiomyocyte (CM)
Human myocardiums are composed of myocytes tied and hold up by connective tissue mainly created from fibrillar collagen. The adult human heart have about 4–5 billions CMs but the myocardium has insignificant basic regenerative capability, and the damage of an important mass of cardiac muscle causes scar. In fact, the normal myocardium consists of four components that are highly interrelated: CMs, CFs, the microcirculation and the extracellular matrix (ECM) [73]. All four above components have decisive role in the progression of chamber remodelling with hypertrophy [73]. RV myocytes have mainly longitudinal myocyte direction with angulated intrusion of superficial myocytes toward the endocardium creating a peristaltic contraction from the inlet to outlet and a bellows-like motion of the free wall toward the septum [74]. In addition, RV myocytes present quicker twitch velocities than LV myocytes [75].
Even if the RV and the LV have related cellular and molecular responses to stress, there are various distinctions at the cellular and molecular levels in their responses to stress such as pressure overload. Furthermore, both ventricles show comparable modifications in genes controlling ECM and cytoskeleton remodelling, but with significant differentiation in genes controlling energy production, mitochondrial function, reactive oxygen species (ROS) production, antioxidant protection, and angiogenesis [26, 70].
Unlike the CMs that comprise almost 1/3 of all heart’s cells [76], endothelial cells (ECs) [77], vascular smooth muscle cells (VSMCs) [77], CFs, macrophages and surrounding ECM that exist in the cardiac interstitium are together named as nonmyocyte cells [78]. The development of nonmyocyte cells is mentioned as interstitial structural remodelling and is characterized by the increase of collagen [78, 79]. Because the increase of nonmyocytes and myocytes is unrelated of each other, the hypertrophic process may be a similar and proportional or heterogeneous with excessive nonmyocytes raise, correspondingly [80, 81].
Since CMs have low ability for cellular multiplication, it is clear that they can growth by cellular enlargement. Consequently, the cross-sectional area and diameter of CMs are raised. Furthermore, typical characteristics of hypertrophy develop too: (1) sarcomere is intense restructured; (2) raised CMs size and myocardial mass by boost of protein synthesis; and (3) cardiac specific gene expression suffers alterations [11, 82]. A part of these modifications are known as re-activation of foetal gene program that implies only the re-expression of normal genes from embryonic and neonatal heart, together with contractile foetal proteins such as skeletal α-actin, atrial myosin light chain-1 and β-myosin heavy chain, and signal transduction proteins such as atrial natriuretic peptide (ANP) or B-type natriuretic peptide (BNP) [9, 83]. Abnormal existence of these foetal proteins in adult human heart has an effect on cardiac contraction, myocardial metabolism including Ca2+ control, resulting in maladaptive CR [84]. Of particular interest, the presence of the foetal gene program does not exist in physiological hypertrophy [85].
Changes of CMs in the size, shape, and function are related with the raise of cell death as well. Deficit of CMs is mainly related to the chronic CR process with progression to HF, increased apoptosis [86], and decreased cardiac function of heart. For that reason, the equilibrium between CMs survival and apoptotic pathways seems the mainly factor of the shift process from hypertrophy to ventricular dilatation [87].
It has previously described that the term matricellular proteins don’t have any significant role in cardiac tissue structure, but they are stimulated by injury with the alteration of cell to cell and cell to matrix connections [88]. Therefore, the production of matricellular proteins in the cardiac matrix, causes their attachment to growth factors, cytokines, and cardiac cells receptors of transducing signalling cascades. Consequently, matricellular proteins are controlled in CR process and have a significant function in controlling of inflammatory, reparation, fibrotic and angiogenic process [88]. It should be remembered that the term matricellular protein has been created by Bornstein [89] for ECM proteins which have no involvement in the structure of the ECM, except they appear and control cardiac cellular function subsequent to injury. According to current evidence, matricellular proteins implied in CR comprise secreted protein acidic and rich in cysteine (SPARC), osteopontin, thrombospondin (TSP), periostin, and tenascin families [88, 90]. Also, initiation of the matricellular proteins (TSP-1, tenascin-C, SPARC) can produce the process of “de-adhesion” in tissue remodelling. This process may be significant in supporting cell motility during inhibition of cell anoikis [88].
To sum up, the normal adult heart contains CMs, a complicated system of ECM, and nonmyocytes that are more numerous than CMs. Every CM is encircled by collagen (endomysium), and connective tissue (perimysium) demarcates individual fibbers. Also, the normal mammalian heart has a rich vascular system consisted of capillary, venous and arteriolar endothelial cells, pericytes, smooth muscle cells, numerous CFs, minor numbers of macrophages, mast cells, lymphocytes and dendritic cells [88]. After an injury of sufficient degree, CMs diminish and develop into elongated or hypertrophied cells to sustain stroke volume [49, 50]. As well as, the width of ventricles wall may raise due to myocyte hypertrophy [48,49,50]. Changing of heart loading conditions like raised preload further causes stretching of cell membranes and increases of wall stress both have the ability to initiate the effect of hypertrophy genes. More precisely, in cardiac myocytes may be triggered new contractile proteins synthesis joining with new sarcomere. The final result is believed to be CMs elongation or the increase of their diameter [91].
It seems that RV dysfunction is described in PAH or RV obstruction [21]. Patients with RV dysfunction are put together even though the CHD can initiate different molecular, cellular and functional remodelling in the RV [21]. In addition, the evaluation of RV function is mainly based on techniques which assess structure and function of RV (e.g. echocardiography, MRI and pulmonary angiography) instead of exploring the cellular and the molecular irregularities of the RV dysfunction from CHD [21]. For instance, some studies demonstrated the alteration of gene expression in signalling pathways that control heart growth in children with Tetralogy of Fallot (TOF). Modifications such as significant suppression of genes in the Notch and Wnt pathways, in VEGF gene expression and numerous ECM proteins are identified as factors that lead to TOF [92, 93]. Another genome-wide array study has demonstrated obvious difference in gene expression between the TOF and other RVH phenotypes, including VSD and ASD. Genes related with cardiac maldevelopment such as SNIP, A2BP1 and KIAA1437 are more active in the TOF group, and genes linked with stress reaction and cell proliferation are more exhibited in the RVH conditions [94].
In addition, a molecular conversion from RV to LV characteristics appears for the period of RV adjustment to pressure overload, with the mention that altered genes from RVH have a normal representation same to the normal LV tissue. Additionally, the association of tissue hypoxia and hypertrophy can boost the protein phosphatase PP1 activity leading to raised phospholamban (PLN-Ser16) dephosphorylation in CMs, followed by cardiac dysfunction [95]. As already described, hypoxia-inducible factor-1 (HIF1α) is a further contributor factor in the RV adjustment to tissue hypoxia and mechanical stress. In acute hypoxia, HIF1α is cardioprotective based on its property to produce angiogenic, metabolic and erythropoietic genes [96]. Conversely, HIF1α sustain transforming growth factor beta TGFβ1-mediated organ fibrosis in chronic hypoxic states [96]. Also, genetic differences of HIF1α change myocardial adjustment to hypoxia during postsurgical period and before RV remodelling process [97]. Therefore, the adjustment of RV to hypoxia prior to TOF surgery is based on the HIF1α pathway and could have an effect on RV phenotype after surgery.
3.4 Matricellular Proteins: TSP Family
It should be underlined that one of the matricellular proteins, TSP family contains five members divided into two groups. TSP-1 and TSP-2 form homotrimers (Subgroup A), while TSP-3, TSP-4 and TSP-5 (COMP) form homopentamers (Subgroup B) [73, 98,99,100] (Figs. 4.4 and 4.5).
Structure of the two thrombospondin (TSP) subgroups . Subgroup A form homotrimers and consist of TSP-1 and TSP-2, while Subgroup B form homopentamers and consist of TSP-3, TSP-4, and TSP-5 (COMP). Subgroup A has domains that bind to CD36 and inhibit MMPs. The N-terminal domains tend to be family member specific, while the CTD has high homology between the family members. NTD N-terminal domain (specific to each family member), vWF-C vonWillebrand factor C-type domain, MMP matrix metalloproteinase, EGF epidermal growth factor, CTD C-terminal domain. (From Kirk et al. [73] with permission)
Recent work has identified several roles for TSPs once the heart has transitioned to heart failure. The effects of the TSPs on matrix remodeling and inflammation are still important in HF. However, they also regulate a number of pathophysiologically important elements within the cardiac myocyte, which exhibits hypertrophy, apoptosis, and contractile dysfunction with HF. However, our knowledge of the mechanistic function of each of the TSPs in the HF myocyte is still incomplete. (From Kirk et al. [73] with permission)
These matricellular proteins induced by heart injury with CR named TSPs have a significant function during cardiac growth [101]. However, numerous TSP proteins activity increases to stress. They have the capacity to attach with the components of the ECM such as cytokines and growth factors. In addition, it’s convenient at this point to discuss that pressure overload quickly raise TSP expression, mainly TSP-1 and TSP-4 [102, 103], and volume overload shows a significant raise in TSP-4 mRNA [104]. In most of the cases, the mechanisms implied are same to the post-MI, as well as inflammation [105] and fibrosis [106].
3.5 Endoplasmic Reticulum Stress
Theoretically, stress factors such as hypoxia, ischemia/reperfusion, hypertrophy, pressure overload, and drug-induced insults can cause activation of endoplasmic reticulum (ER) stress in the heart [107]. ER stress being closely implied in the protection of cardiovascular homeostasis, it proves a significant therapeutic aim for cardiovascular diseases treatment. Figure 4.6 shows a schematic illustration of ER stress pathways with particular highlighting on their role in cardiac physiology and pathology [108]. The ER stress response or ‘unfolded protein response’ (UPR) is essential for normal cellular protection, but in CR like HF can generate apoptosis [107, 108]. A simplistic explanation is TSP-1 and TSP-2 have anti-inflammatory, pro-fibrotic, and antiangiogenic properties, as TSP-4 induces pro-inflammatory and pro-angiogenic consequences [109]. Also, the TSPs are significant aims for stopping the evolution from MI to HF.
ER stress signaling pathways. (a) PERK-dependent pathway activated by ER stress. PERK, a transmembrane kinase and endoribonuclease, interacts with BiP/GRP78 under nonstressed conditions. On activation of ER stress, BiP/GRP78 dissociates from PERK, resulting in dimerization of PERK and activation of its kinase domain, autophosphorylation, and subsequent phosphorylation of eIF2α. Phosphorylation of eIF2α results in attenuation of protein synthesis. However, expression of ATF4 is not inhibited, and the transcription factor induces expression of ERSR-containing genes. (b) ATF6 pathway. Under nonstress conditions, ATF6, a transmembrane protein localized to the ER, interacts with BiP/GRP78 and calreticulin. After ER stress, BiP/GRP78 and calreticulin dissociate from ATF6, and the protein translocates to the Golgi, where it undergoes cleavage by S1P and S2P proteases. This cleavage yields a cytoplasmic transcription factor (N-ATF6) that translocates to the nucleus and induces ERSR-containing genes. (c) IRE1 pathway. IRE1 is an ER transmembrane protein containing a serine–threonine kinase domain and a carboxyl-terminal endoribonuclease domain in its cytoplasmic region and binds to BiP/GRP78. Under ER stress conditions, BiP/GRP78 is released from IRE1 followed by IRE1 homodimerization and autophosphorylation. Phosphorylation is essential for IRE1 endoribonuclease activity that is responsible for splicing of XBP1 mRNA, yielding spliced XBP1s mRNA encoding a potent transcription factor. The XBP1s splice variant binds to ERSE-containing promoters and activates ERSE genes. XBP1s also binds to a second cis-acting motif, termed the UPRE, resulting in upregulation of genes involved in ERAD. (From Groenendyk et al. [108] with permission)
3.6 Pleiotropic Functions of Cardiac Fibroblasts (CFs)
In particular, CFs include over 50% of the cells in the adult heart [110] being implied in the development and deterioration of the cardiac ECM by generating collagens, proteoglycans, MMPs and TIMPs. As well, CFs produce different bioactive mediators such as VEGF-A, fibroblast growth factors (FGFs), transforming growth factor beta (TGF-β), platelet-derived growth factor (PDGF) which affect cardiac angiogenesis and CM proliferation. Furthermore, CFs have an effect on cardiac electrophysiology by protecting CM bundles, spreading of electrical signals, and changing mechanical stimuli in electronic signals [111]. In fact, CFs develop intracellular electrical coupling and interconnect with CMs through gap junctions (Fig. 4.7) [112,113,114]. Also, CFs being the most abundant cardiac cell type, they monitor CM proliferation during heart development. Therefore, CFs activation is a critical early repair response after cardiac injury.
Cell Communication Between Cardiac Fibroblasts and Myocytes . Z-section of a cell aggregate containing cardiac fibroblasts that were dual loaded with Lucifer Yellow and CMRA and myocytes that were unloaded. Cardiac fibroblasts appear as yellow or orange cells. The orange cells are fibroblasts that have transferred their green dye to an adjacent cell (orange arrow). Note the green cells, which are myocytes that have received green dye from an adjacent fibroblast (white arrow). (From Souders et al. [112] with permission)
3.7 Collagen Synthesis and Degradation
Collagen is synthesized by interstitial CFs which are degraded by locally formed enzymes named collagenases, such as matrix metalloproteinases (MMPs). The cardiac interstitium consist of 95% of type I and type III collagen fibers. The most important roles of collagen network are to control apoptosis, fix pathological processes, preserve the configuration of structures, control the resistance conduction during fiber shortening, and produce cytokines and growth factors [115]. Each heart has inactive myocardial collagenases in the ventricles but they are activated after a myocardial injury [116]. As already noted above, in any failing heart, CR primarily arises as a preventing reaction to protect the myocardium structure, but with gradually collagen deposit can causes cardiac fibrosis with diastolic and systolic dysfunction [117,118,119,120]. Importantly, collagen XIV is necessary to produce and preserve the ECM network in the heart growth [121]. Throughout fibrosis process, CMs undertake hypertrophic modifications, while MyoFb continue with collagen production and scar formation at the site of injury. In addition, collagen XI is necessary for myocardial growth supporting the nucleation of type I and II fibrils [122]. Therefore, the increased activity of collagen type XI alpha 2 chain (COL11A2) gene can be correlated with production of heterotypic fibrils with collagen I that is implicated in CR [123]. Nevertheless, persistence of CFs in injury area leads to chronic scar and remodelling [119].
According to evidence, the atypical deposit of type III collagen and type I collagen was discovered in cardiac injury, produced by several signalling pathways such as TGF-β, endothelin-1 (ET-1), angiotensin II (Ang II), connective tissue growth factor, and PDGF. In this situation, fibrosis is related with raised myocardial stiffness, decreased diastolic function, reduced contraction, failed coronary flow and malignant arrhythmias [124, 125].
As a result, collagen has an important role in the protection of cardiac structure and function. In CR, the equilibrium between collagen production and degeneration is altered with numerous side effects. To prevent developing of CR to HF is necessary of timely developed stable scar that restores the injured tissue [126]. This equilibrium is preserved to some extent by MMPs that alter the ECM and tissue inhibitors of MMP (TIMPs) [127, 128]. In case of post MI, numerous mechanisms are run by CFs that change into MyoFb [129].
It should be noted, that there is a direct support between TSP-1 and the cardiac collagen. More important, TSP-1 and TSP-2 can preserve ECM normal structure by controlling the MMPs [73, 130, 131] (Table 4.2). TSP-1 and TSP-2 can directly attach to MMP2 and MMP9 through their Type 1 Repeats [132], but this attachment doesn’t cause their inhibition directly [133]. When TSPs perform their activation by TGFβ, this diminishes MMP transcription [134]. Also, TSP-1 can attach to collagen V and fibrinogen [135, 136] and hasten fiber growth [137]. On the other hand, TSP-4 increases fibrosis by production of collagens I, II, III, and V [138] that support its direct role on the ECM remodelling process [139]. Essentially, in order to regulate cardiac fibrosis, TSP-4 expression is controlled by the transcription factor Krüppel-like factor 6 (KLF6) [140]. Also, TSP-4 triggers TGF-β [73] necessary for the transdifferentiation of MyoFb from CFs [141]. Further, MyoFb are indispensable to the cardiac fibrosis by production of collagen [142].
3.8 Apoptosis
There are three main mechanisms involved in myocyte death: apoptosis or programmed cell death, necrosis and autophagy. According to data, cardiac dysfunction is correlated with modifications produced by autophagy, that can be adaptive or deleterious [143,144,145]. Initially, Sharov et al. have been suggested that raised cardiac apoptosis with CMs damage increases LV dysfunction with chronic HF [55]. Conversely, Olivetti et al. showed on myocardial samples from patients who underwent heart transplantation that cardiac apoptosis was increased more than 200-fold in the patients with failing heart [57]. In general, apoptosis has an important function in cardiac growth and in various heart diseases with ischemic and non-ischemic origin [146, 147]. However, the major mechanism of CM death from MI is the coagulation necrosis, even if apoptosis is also implied in CMs damage (Fig. 4.8) [148, 149].
Typical appearance of different types of cell death. (a, c, e) Confocal micrographs: counterstaining for actin, red; nuclei, blue; specific fluorescence, green. (b, d, f) Electron microscopic pictures (all bars = 2 μm). (a, b) Apoptotic cell death . (a) Nuclei with DNA fragmentation are green. (b) Nuclei show condensed chromatin. (c, d) Oncotic cell death. (c) Single cell oncosis labeled with C9. (d) Nuclei are electron-lucent with clumped chromatin, mitochondria are damaged with flocculent densities. (e, f) Autophagic cell death. (e) Ubiquitin deposition and loss of nuclei. (f) Ultrastructural appearance with numerous autophagic vacuoles. (From Kostin et al. [148] with permission)
It is important to note, that there is a fast triggering of caspase-3 in MI during 1 h after the onset of ischemia [150, 151], and the process of CM apoptosis can be completed within 24 h (Figs. 4.9 and 4.10) [42, 152, 153]. Previous reports have been shown that apoptosis is associated with unfavourable CR and HF post-MI in case of ablated proapoptotic protein Bnip3 [154, 155]. Also, TSP-1 and TSP-2 trigger apoptosis in ECs from microcirculation [156, 157]. Apoptosis inhibits endothelial tubule development and consequently has antiangiogenic effect. Further, vitro studies showed that matricellular proteins relate with the transmembrane glycoprotein CD36 [157,158,159,160,161,162], being the mainly mechanism that causes the antiangiogenic effect. Also, Primo et al. showed in cultured human ECs the inhibition of angiogenesis by the pathway of the VEGF receptor modulated by TSP-1 [163]. Attachment of TSP-1 to CD36 causes apoptosis of ECs by raise of death receptors and Fas ligand [164].
Schematic depiction of pathways leading to programmed cardiomyocyte death , as described in the text. Mechanisms of cell death (bottom) are, from left to right, caspase-dependent apoptosis, caspase-independent apoptosis, programmed necrosis, and authophagy. Solid lines show primary effects; interrupted lines depict cross-talk between pathways. (From Dorn [152] with permission).
Demonstration of apoptosis . (a) Labelling of nuclear DNA fragmentation using terminal deoxynucleotidyl transferase mediated dUTP nick end labelling (TUNEL). Colocalisation of (b) TUNEL and actin and of (c) TUNEL and activated caspase 3. (From Bussani et al. [42] with permission)
ADAMTS-7 is a member of the disintegrin and MMPs with TSP motifs (ADAMTS) family [73, 165], being newly recognized to be considerably correlated genome-wide with angiographic CAD [73, 166]. It has been previously confirmed that ADAMTS-7 support VSMCs migration and post injury neointima production via degradation of the matrix protein ‘Cartilage Oligomeric Matrix Protein’ (COMP or TSP-5) [73, 167]. Same researchers demonstrated that ADAMTS-7 breaks down the TSP-1 with re-endothelialization prevention [73, 168]. Also, the extracellular proteases thrombin, cathepsins, leukocyte elastases and plasmin can degenerate the TSPs [169].
Autophagy is defined as the intracellular process that removes needless cytoplasmatic components by lysosomes [144]. To date, the ubiquitin-proteasome system (UPS) and the autophagic-lysosomal pathway (ALP) are two major pathways in charge for most cellular proteins deterioration. Modifications of UPS and ALP pathways are correlated with the increase of proteotoxic defective proteins in the heart, a characteristic of frequent heart disease [144]. Acute ALP inhibition (proteasome inhibition) boost occasionally ‘intrinsic proteasome peptidase activities’, but chronic ALP inhibition blocks UPS pathway functioning in ubiquitinated protein stage [144]. As a result, autophagy has a significant function in proteotoxicity prevention by the ubiquitin system [144], and chaperones (heat shock protein-HSP) [145]. Particularly, the co-chaperones Bag3 and HspB8 have significant role in the heart autophagy by chaperone-assisted selective autophagy [170, 171]. Regardless of myocyte death, the gradual decrease of CMs thas a significant function in CR and could be a potential target for therapeutic interventions.
4 Fibrosis
Just as RV fibrosis is commonly seen in the setting of both severe RV afterload and chronic pulmonary regurgitation, LV fibrosis is common in both aortic stenosis and regurgitation [172,173,174]. At the site of MI, acute focal fibrotic scarring provides myocardial healing and prevents rupture [175]. In contrast, chronic diffuse or focal reactive myocardial fibrosis is a result of either pressure overload or volume overload due to persisting hypertension, metabolic disorders, valvular heart diseases, ischemic injury (in areas remote from the infarction), or diffuse myocardial diseases, such as cardiomyopathies [175].
Myocardial fibrosis is defined by dysregulated collagen turnover characterized by increased synthesis that dominates over unaffected or reduced degradation [176, 177] with excessive diffuse collagen accumulation in the interstitial and perivascular spaces [178]. For that reason, the dysregulation of distinct pro- and antifibrotic factors, including cytokines and chemokines, growth factors, proteases, hormones, and ROS, is responsible for the alteration of the collagen matrix (Fig. 4.11) [179, 180].
Schematic representation of biochemical and cellular mechanisms of cardiac fibrosis . Under physiological conditions (left), fibroblasts secrete extracellular procollagen chains into the interstitium that assemble into fibrils and are cross-linked by lysyl oxidase. Several cell types are implicated in fibrotic remodelling of the heart either directly by producing matrix proteins (fibroblasts), or indirectly by secreting fibrogenic mediators (macrophages, mast cells, lymphocytes, cardiomyocytes, and vascular cells). Under pathological conditions (right), alterations in the matrix environment, induction and release of growth factors and cytokines, and increase of mechanical stress dynamically modulate fibroblast transdifferentiation into myofibroblasts. Higher collagen cross-linking results in increased myocardial tensile strength. Resistance to degradation by matrix metalloproteinases (MMPs) increases cross-linked collagen, which favours matrisome expansion. Pink, grey, and green boxes list part of the secretome of mycocytes, myofibroblasts, and macrophages/leucocytes/mast cells, respectively, that trigger and maintain fibrosis. Gal-3 galectin-3, IL interleukin, PDGF platelet-derived growth factor, RAAS renin–angiotensin–aldosterone system, ROS reactive oxygen species, TGF transforming growth factor, TNF tumour necrosis factor. (From Gyöngyösi et al. [179]. It is an open access article)
The degeneration of collagen turnover takes place mainly in phenotypically transformed fibroblasts, termed MyoFb [79, 181]. The shift of CFs in MyoFb implies the expression of α-SMA, a characteristic of SMCs [79, 181,182,183,184,185,186]. As well as, the development of a wide active ER stimulated by a number of bioactive effectors [79, 181,182,183,184,185,186]. CFs and particularly MyoFb form collagen type I and III fibrils and develop into cross-linked to form the final fibres [176]. Collagen cross-linking is a significant post-translational stage that raises the resistance of collagen fibres to degradation by MMPs [187, 188]. Only that, myocardial fibrosis disrupts the myocardial architecture, contributes to myocardial disarray, and determines mechanical [189], electrical [190, 191] and vasomotor [192] dysfunction, thus promoting the progression of cardiac diseases to HF [175]. Fibrosis is induced by various genetic disorders, pressure or volume stress, heart injuries, and other diseases. There is evidence that depending on the particular trigger, distinct molecular pathways have varying importance for the individual types of fibrosis. As the development of myocardial fibrosis is characterized by a complex dysregulation of a number of different factors including inflammatory chemokines, angiotensin II (Ang II), and endothelin signalling, the FIBROTARGETS consortium that is a multinational consortium with industrial and academic partners, funded by the European Commission is primarily aimed for characterizing novel emerging mechanisms of myocardial fibrosis [180]. Targets and biomarkers under investigation include especially proteins, proteoglycans, and microRNAs (miRNAs) [180].
In increased volume loading, the RV appears more prone than the LV to develop fibrosis [63]. Similarly, patients after surgical repair of TOF who have long-standing RV volume load secondary to pulmonary insufficiency develop RV fibrosis [172]. This is clinically important as risk factor for increased propensity to arrhythmias, exercise intolerance, and RVF [172, 193]. It has been suggested that these differences in response between the RV and LV to volume loading may stem from the different embryological origin of the two ventricles [63].
Several single or multimodal imaging technologies have been used to assess the extent and type of myocardial fibrosis. Besides the direct morphological display of the fibrotic tissue, indirect cardiac functional imaging may evidence fibrosis correlated with decrease of systolic function and increased myocardial stiffness with diastolic dysfunction [175]. Cardiac magnetic resonance imaging (MRI) provides detailed tissue characterization, identifying focal myocardial fibrotic scars with late gadolinium enhancement (ventricular LGE) and an estimation of diffuse myocardial fibrosis with post-contrast enhanced T1 and T2 mapping (Fig. 4.12) [179, 194].
Representative native and T1 cardiac magnetic resonance imaging (cMRI) of diffuse myocardial fibrosis. (a) Diffuse myocardial fibrosis on the short-axis view of the cMRI image, with the circumference of the anteroseptal myocardial area (region of interest). (b) cMRI T1 map of a patient with moderate aortic stenosis and moderate diffuse myocardial fibrosis. (c) cMRI T1 map of another patient with severe aortic stenosis and severe diffuse fibrosis of the left ventricle. (From Gyöngyösi et al. [179]. It is an open access article)
Positron emission tomography (PET) imaging performed by using 15O-labelled water (H2 15O) and carbon monoxide (C15O) allowed the non-invasive quantification of both myocardial perfusion and fibrosis [195]. Combining PET and MRI has the potential for sensitive and quantitative imaging of cardiovascular anatomy and function with detection of molecular events at the same time [196, 197]. It’s worthwhile to specify that PET–MRI (Biograph mMRI, Siemens AG) image allows the simultaneous detection of myocardial global and regional function, ECM volume, and tissue perfusion and metabolism [198].
Histopathological analysis of endomyocardial biopsy specimens is the current gold standard for diagnosis and assessment of cardiac fibrosis. A number of circulating biomarkers, including (pro-) collagen cleavage products, processing enzymes, but also miRNAs (Table 4.3), have been proposed and analysed [179]. Details of these biomarkers and potential targets have been described previously including proteins and proteoglycans that impact fibrosis and miRNAs that act in fibrosis [180]. For their use as cardiac fibrosis biomarkers, it seems reasonable that a combination of several from these increases the predictive power, particularly in the case of miRNAs [199, 200].
As a consequence, the treatment of HF patients improves clinical symptoms, but does not reverse fibrosis. Furthermore, the severity of histological proven myocardial fibrosis has been reported to be associated with higher long-term mortality in patients with cardiac diseases, mainly patients with HF [200, 201].
4.1 miRNAs
Genetic variations exist among the RV and the LV. Drake et al. [71] note the dissimilarity between gene expression patterns in normal RV and LV in both mRNA and microRNAs (miRNA) types. More precisely, the transcription factor Irx2 is not exhibited in the RV but insulin-like growth factor 1 (IGF-1) is exhibited mainly in the LV. Moreover, same team made the assumption that these dissimilarities can be the result of different embryologic origin or the RV is a low-pressure chamber compared to the LV. Also, Reddy et al. [66] demonstrated firstly that changes in miRNAs exist in RV remodeling from RVH to RVF and are mostly comparable to pressure-stressed LV but with separate signalling regulatory pathways.
RV dysfunction is described entirely in RV obstruction or PAH [21]. Only that, all patients with RV dysfunction are put together regardless of the fact that CHD have various functional, molecular and cellular remodelling patterns in the RV [21] (Fig. 4.13). Blood biomarkers, similar to plasma proteins and miRNAs represent an important way to evaluate the function and remodelling of RV [21]. Heart miRNAs are constant and quantifiable discharged in the blood flow as exosomes, microvesicles or joining with high-density lipoproteins (HDL) and RNA-binding proteins [21].
Dysregulated miRNAs in congenital heart diseases (CHDs) . A figure showing the link between CHD and miRNAs in cardiomyocytes. Small number of miRNAs are upregulated in cardiomyocyte during CHD. These miRNAs can be released from the cell in microvesicles, by incorporation into exosomes, by linkage to high-density lipoproteins or bound to RNA-binding proteins. Dysregulated levels of miRNAs, crucial in RV development, are found in the bloodstream of children with VSD. The differentially expressed has-miR-222-3p, has-let-7e-5p and has-miR-433 bind with specific transcription factors (NOTCH1, GATA4, HAND1 and ZFPM) associated with RV morphogenesis. (From Iacobazzi et al. [21]. It is an open access article)
There are numerous disrupted miRNAs during CR and RHF [21, 202,203,204,205] (Fig. 4.14). miRNAs are non-coding single-stranded RNAs formed from 19–24 nucleotides that adjust in the negative way the exhibition of a particular mRNA via translational degeneration or suppression [206]. According to data, there have been shown in children with VSD in comparison with controls eight various miRNAs. Particularly, NOTCH1 is implied in ventricular growth, and GATA4 has an important function in atrial and ventricular growth, heart partition, and atrioventricular valve development [21, 207].
Functional role of miRNAs in the normal and diseased heart. A normal and a hypertrophic heart are shown in schematic form, depicting miRNAs that contribute to normal function or pathological remodelling. The expression of selected miRNAs within the heart is shown, along with their corresponding functions. All arrows denote the normal action of each component or process. miR-1 and miR-133 are involved in the development of a normal heart (left) by regulating proliferation, differentiation and cardiac conduction. For example, proliferation is promoted by cell-cycle regulators, but miR-1 and miR-133 block these regulators, thus blocking proliferation. miR-208a also contributes to the regulation of the conduction system. After cardiac injury (right), various miRNAs contribute to pathological remodelling and the progression to heart failure. miR-29 and miR-21 block and promote cardiac fibrosis, respectively. miR-29 blocks fibrosis by inhibiting the expression of ECM components, whereas miR-21 promotes fibrosis by stimulating mitogen-activated protein kinase (MAPK) signalling. miR-208 controls myosin isoform switching, cardiac hypertrophy and fibrosis. miR-23a promotes cardiac hypertrophy by inhibiting ubiquitin proteolysis, which itself inhibits hypertrophy. Hypoxia results in the repression of miR-320 and miR-199, which promote and block apoptosis, respectively. ECM extracellular matrix, LV left ventricle, MHC myosin heavy chain, RV right ventricle. (From Small et al. [205] with permission)
A low number of studies have studied the blood miRNAs in adult patients diagnosed with systemic RV [21]. Patients with the RV as the SV after transposition of the great arteries (TGA) had altered miRNAs profile. On the whole, from the 24 miRNAs various regulated, miRNA18a and miRNA486-5p related negatively with systemic ventricular contractility [21, 208]. Also, miRNA423_5p defined as a biomarker of LVF, has same expression in healthy adults and in SV after atrial repair of TGA adults [21, 209].
It seems that gene expression in signalling is changed in heart growth of children with TOF [21]. Alteration of VEGF gene expression and of a number of ECM proteins is established as contributors of TOF [92]. Important inhibition of genes in the Notch and Wnt pathways implied in heart growth are also found in children with TOF [21, 93]. Even if RVH is a component of TOF, there is a clear molecular difference between TOF and RVH gene expression, including VSD and ASD [21]. Whereas TOF children have unregulated genes for heart growth such as SNIP, A2BP1 and KIAA1437, RVH has a higher expression of genes implied in stress reaction and cell proliferation [21, 94]. What’s more, there is a molecular conversion from RV to LV features that appears during RV adjustment to pressure overload, as a result dysregulated gene phenotype from RVH is same with normal LV [21]. Another study based on cardiac tissues from RV in CHD [95], found dissimilar miRNAs in RV outflow tract obstruction (RVOT) in comparison with RVOT of normal infants [210]. Specifically, miRNA-424 and miRNA-222 had higher expression and they correlated with the decrease of heart growth being correlated with NF1 and HAS2 genes. Correspondingly, the increased expression of miR-421 in RV tissue from children with TOF is correlated with SOX4 gene necessary for cardiac outflow tract formation (Fig. 4.14) [21, 211, 212].
miRNA 133a is thought to suppress cardiac fibrosis and is decreased in LVF secondary to aortic constriction [213, 214]. This aligns with the marked upregulation of connective tissue growth factor/CCN2 and other profibrotic signalling molecules in the course of RV and LV fibrosis in models of RV afterload and RVF [71, 88, 215]. In contrast, miRNA 21 and 34c* may increase during LVF but decrease in RVF [71]. Reddy et al. [66] investigated miRNAs during the transition from RVH to RVF and compared these with miRNA expression in LVH or LVF. During RVH, there was altered expression of miRNAs 199a-3p, which is associated with CM survival and growth. With the progression to RVF and switching on the foetal gene phenotype, there was increased miRNA 208b, miRNA 34, miRNA 21, and miRNA1, which are associated with apoptosis and fibrosis [83]. These patterns of miRNA expression are largely related to LVH and LVF. Conversely, there are important distinction relating RV and LV miRNAs linked to cell survival, proliferation, metabolism, ECM production, and proteasome malfunction (miRNA 28, miRNA 148a, and miRNA 93), which were unregulated in RVH or RVF and downregulated or unchanged in LVH or LVF [66].
Common findings in both RVH and LVH are collagen deposition, fibrosis, and ECM remodelling [216]. The mechanisms inducing fibrosis are multiple, and in the setting of increased ventricular afterload, recognized triggers may include regional ischemia, necrosis, and apoptosis, among others [176]. There is an important match of the miRNA expression phenotype in human HF and foetal hearts in comparison with the adult normal heart tissue [204]. More studies data are necessary for a higher knowledge of these subcellular events that can guide to the development of new ventricle-specific treatments [217].
5 Other Factors
Factors that can also contribute to CR comprise endothelin, cytokines (tumor necrosis factor-alpha-TNFα and interleukins) [218], oxidative stress, MMPs, and peripheral monocytosis [219].
Endothelins (ET) are powerful vasoconstrictor peptides which increase in HF. The endothelin family of peptides is typically recognized for its vasoconstrictive properties. There are two known receptors for ET-1 in the heart, the ETA and ETB receptors, which have been shown to play differing and sometimes opposing roles. Importantly, ET-1 activation of the ETA receptor is known to increase collagen production in isolated human CFs [220]. Furthermore, MyoFb isolated from scar tissue after experimental MI have elevated levels of ET-1, suggesting an important function for ET within these cells [221].
ET-1 is a 21-amino acid peptide formed and discharged by the ECs and it has a quickest vasoconstrictive effect [222]. Cardiac ET-1 is active in both autocrine and paracrine effects by attaching to ETB receptors from cardiac ECs and ETA receptors from CMs [222]. The attachment of ET-1 to ETB receptors causes the discharge of signalling molecules such as NO and prostaglandin I2 [222]. If ET-1 attaches to the ETA receptors from CMs, it triggers CM constriction [222, 223]. As a consequence, there may exist a feedback mechanism concerning cardiac ECs and CMs that run CM constriction by the ET-1 system [222]. Also, patients with HF have raised exhibition of cardiac ET receptors and raised plasma ET-1 levels, both linked with disease severity [224]. ET antagonists they will be additionally efficacious in the treatment of pathological fibrosis in the heart [225]. Preliminary trials in humans had demonstrated beneficial hemodynamic and cardiac effects in patients with end-stage HF [226].
Cytokines (tumor necrosis factor-alpha TNFα and interleukins) are small peptides or glycoproteins that are discharged by nucleated cells [227]. Their temporary discharge adjust immune or repair processes by controlling cells growth, process of differentiating, metabolism, and protein synthesis [228]. Fibrinogen is an acute inflammatory regulator discharged by hepatocytes triggered by different cytokines. Also, CRP is an acute-phase reactant synthesized and discharged largely by hepatocytes in response to the cytokine IL-6. The highest levels of CRP are correlated with MI size but are reduced by early reperfusion [229]. It seems that IL-3 is a new biomarker of inflammation and can induce the multiplication of lymphocytes, macrophages, neutrophils, and monocytes with infiltration of heart where trigger the discharge of cytokines from CMs. Moreover, IL-3 can have significant functions in tissue repair. Understanding better inflammatory response could offer measurable ways of immune injury to tissues.
Leukocytosis was studied especially in MI [230, 231]. The ischemic-reperfusion stage produces the discharge of oxygen free radicals, cytokines, and other inflammation markers [231]. The presence of leukocytes in the microcirculation is followed by inflammatory reaction [232]. The transfer of leukocytes from blood flow to the vessel wall with tissue injury and inflammation is regulated by the selectin family of adhesion molecules with attachment of leukocytes to the ECs by involvement of integrins and diapedesis [233, 234]. Recruitment of leukocytes is mediated by complement triggering, TGF-β, IL-8, monocyte chemotactic protein-1 (MCP-1), and platelet activating factor (PAF) [235]. Also, the collection of neutrophils in the ischemic-reperfusion tissue could discharge proteolytic enzymes or ROS with further injury of myocytes. ROS directly injure CMs and vascular cells, and by triggering cytokines causes inflammation [236, 237]. Marginated neutrophils exert powerful cytotoxic effects through the adhesion with intercellular adhesion molecule-1 (ICAM-1) expressing CMs [235]. CD11b/ICAM-1 adherence activates the neutrophils respiratory burst resulting in myocyte oxidative injury [235].
Oxidative Stress produces important alteration of sarcolemmal and sarcoplasmic reticulum (SR) membrane, causing raise of intracellular Ca2+ levels with severe contraction of CMs, followed by mitochondrial damage and cell death [238, 239]. Specifically, ROS and redox signaling have an important function in apoptosis, including upstream signaling pro-apoptotic pathways and the mitochondria [240, 241]. There are signaling pro-apoptotic pathways that comprise the activation of ASK-1, JNK, p38MAPK, and CaMKII, as well as signaling anti-apoptotic pathways, such as Akt, Bcl2, and HSPs [241].
The cell resources of ROS comprise mitochondrial respiratory chain enzymes, xanthine oxidases (XOs), lipoxygenases, myeloperoxidases, uncoupled nitric oxide synthases (NOSs), and Nox proteins [242, 243]. Moreover, the important sources of ROS in the cardiovascular system comprise mitochondria, NADPH oxidases, NOSs, xanthine oxidases, cytochrome P450-based enzymes, and infiltrating inflammatory cells [243]. ROS are represented by free radicals (species with one or more unpaired electrons) such as superoxide (O2•−) and hydroxyl radicals (OH•), and nonradical species such as hydrogen peroxide (H2O2) [243]. In healthy adults, production of ROS is inhibited by enzymatic and nonenzymatic antioxidant systems that decrease ROS levels with preserving of a right redox balance in cells and tissues [243].
The first report of the presence of NADPH oxidases in human myocardium is of Heymes et al. [244]. NADPH or NADH-dependent ROS-generating activity are existent in nonphagocytic cell types [243], including VSMC [245, 246], ECs [247, 248], adventitial and CFs [249], and CMs [250]. Noxs are multi-subunit transmembrane enzymes that use NADPH as an electron donor to decrease oxygen to superoxide anion (O2−) and hydrogen peroxide (H2O2) [243]. Firstly, Noxs were described in phagocytes with the description of the Nox2 isoform that it also named gp91phox) [243, 251]. The rest comprise 6 other family members each coded by dissimilar genes, identified as Nox1, Nox3, Nox4, Nox5, dual oxidase 1 (Duox1), and Duox2 [243, 252,253,254]. All forms of Nox proteins demonstrate 21–59% similarity to Nox2, from which Nox3 is most alike with Nox2 and Nox5 mostly unrelated [243].
Therefore, the NADPH oxidase (Nox) family (Fig. 4.15) is formed from 7 catalytic subunits termed Nox1-5 and Duox1 and Duox2 (for Dual Oxidase), regulatory subunits p22phox, p47phox or Noxo1, p67phox or Noxa1, p40phox. Further, the Nox1, 2, 4 and 5 enzymes are existent in normal cardiovascular tissues, and trigger the progression of cardiovascular disease. Nox enzymes are located in VSMCs, ECs, adventitial fibroblasts, macrophages, CMs and fibroblasts, plus adipocytes and stem cells. They are associated with hypertension, atherosclerosis, HF, ischemia reperfusion injury and CR, but upregulation can be physiologically beneficial such as in angiogenesis [243, 244, 255, 256]. The acutely upregulation of cardiovascular NADPH oxidase activity by a large various patho-physiological stimuli comprise [243] (a) G-protein coupled receptor agonists such as Ang II and ET-1; (b) growth factors such as VEGF, thrombin, PDGF, and EGF; (c) cytokines such as TNF-β, IL-1 and TGF-β; (d) metabolic factors such as elevated glucose, insulin, free fatty acids, and advanced glycation end products (AGE); (e) oxidized LDL, lysophosphatidylcholine, and hypercholesterolemia; (f) mechanical forces such as oscillatory shear stress; and (g) ischemia-related stimuli such as nutrient deprivation, membrane depolarization, flow cessation, hypoxia–reoxygenation, and ischemia [243].
Structure of NADPH oxidase in the heart. NADPH oxidase complex is composed of two major components. Plasma membrane spanning cytochrome b558 composed of p22phox and a Nox subunit (gp91phox (Nox2), Nox4) and cytosolic components composed of four regulatory subunits (p47phox, p67 phox, p40 phox and Rac1). The low molecular weight G protein rac1 participates in assembly of the active complex. Upon activation, cytosolic components interact with cytochrome b558 to form an active NADPH oxidase enzyme complex, resulting in release of ·O2−. The primary Nox subunit isoforms in cardiac cells are Nox2 and Nox4. Nox4 oxidase localizes intracellular organelles around the nucleus. The activity of Nox4 results in the direct release of hydrogen peroxide (H2O2) in mitochondria. The mechanisms underlying the generation of hydrogen peroxide by Nox4 oxidase are yet to be fully characterized. (From Kayama et al. [255]. It is an open access article)
Nox2 and Nox4 are the mainly isoform exhibited in CMs. Triggered Nox2 is mainly exhibited at the plasma membrane [244]. According to data, Nox derived ROS are implied in CM apoptosis. Pro-apoptotic signaling pathway and generation of CaMKII in pro-apoptotic signaling pathway are triggered both by Ca2+, by Nox2-derived ROS, and downstream of Ang II [257]. Norepinephrine, aldosterone, and doxorubicin are also reported to promote CM apoptosis through the activation of Nox2 [258,259,260]. Contrary to Nox2 function in Ang II-induced cardiac hypertrophy, Nox2 is not implied in cardiac hypertrophy induced by pressure overload (Fig. 4.16) [261]. The major agonists and stimuli of Nox2 activation in CMs and ECs comprise G-protein coupled receptor agonists (GPCRs) such as Ang II and ET-1, growth factors, cytokines (TNF-α), mechanical forces, metabolic factors (glucose, insulin), glycated proteins [262], and oxidized low-density lipoprotein (ox-LDL) (Fig. 4.17) [261, 263, 264]. To sum up, evidence supports different functions for Nox2 and Nox4 in hypertrophic reaction to pressure overload [243]. Important redox-sensitive downstream signaling pathways in the heart that can be affected by NADPH oxidase activation such as RAS, the MAPKs (p38MAPK, ERK1/2, JNK), c-src, p90RSK, the PI3 kinase (PI3K)/Akt pathway, AP-1, NF-ĸB, HIF-1, and others [243].
Representative immunofluorescence micrographs of human heart sections labeled for the nicotinamide adenine dinucleotide 3-phosphate (reduced form) oxidase subunit gp91phox. Panels a, c, e, and g show nonfailing heart tissue and panels b, d, f, and h show end-stage failing tissue. Transverse (a, b) and longitudinal (c, d) sections labeled for gp91phox show increased labeling in end-stage heart failure. Labeling for alpha-actinin (e, f) shows a typical intracellular pattern of myocyte costamer and intercalated disc labeling. Panels g and h show suprerposition of gp91phox and alpha-actinin labeling. All scale bars = 20 μm. (From Heymes et al. [244] with permission.)
Schematic illustrating involvement of Nox2 NADPH oxidase in the cardiac response to activation of the renin angiotensin aldosterone system (RAAS) or to chronic pressure overload. Hypertrophy in response to short-term RAAS activation is dependent upon Nox2, whereas the hypertrophic response to pressure overload is not. However, Nox2 is essential for the development of interstitial fibrosis in response to either stimulus. (From Murdoch et al. [261] with permission.)
In case of RV, metabolic and ischemic modifications typical to RV remodelling are also correlated with accumulation of ROS [21, 265] (Fig. 4.18). The presence of ROS activates the cellular and molecular modifications with decrease of contractile function, lacking of energy production and fibrosis. Alteration of SM channels by oxidative stress produces damaging of RyR2 activation and decrease of sarco/endoplasmic reticulum Ca2+-ATPase (SERCA) activity, as a result appears temporary malfunction of myocyte Ca2+ and contractile dysfunction [21, 92]. Additionally, increased ROS amounts cause conversion of nitrotyrosine rests in TIMPs and discharge active MMPs with CR and fibrosis [21, 266]. To date, vivo studies with histological examination of collagen content in RV samples from pulmonary artery showed a significant raise of ROS, important collagen deposition with high levels of MMP-2, MMP-9 and MMP-13 and diminished TIMP-4 protein amounts. Additionally, ROS are second messengers within CMs for numerous signalling molecules (ATII, TGFβ1, TNFα and ET-1) to generate hypertrophic pathways including MAPKs, PKC and Src [21, 62]. Taken together, raised amounts of ROS can damage cellular, molecular and structural components with CR and failure. It is important to underline that malondialdehyde levels represent an indirect index of oxidative stress and are notably elevated in the RV in comparison with the LV. To sum up, these features support a decreased resistance of RV in oxidative stress being a contributor in the development of HF [267].
ROS-induced intracellular changes in cardiomyocyte . The increased intracellular ROS levels occurring in RV pressure overload affect several cardiomyocytes functions. ROS can stimulate pro-hypertrophic pathways by targeting key molecules in this process, such as MAPK, PKC and Src proteins. The redox-mediated activation of target transcription factors (HIF-1α, cMyc and FOXO1) might be responsible for the abnormal PKD activation, which inhibits mitochondrial oxidative metabolism, leading to mitochondrial dysfunction. Sustained ROS levels cause mPTP opening and mitochondrial membrane depolarisation. As a consequence, more ROS are produced and cytochrome c is release from mitochondria causing cell apoptosis. HIF-1α activation also decreases the activity of the O2-sensitive Kv channel (Kv1.5), resulting into membrane depolarisation and elevation of cytosolic Ca2+. The surplus of cytosolic Ca2+, in addition to the excessive Ca2+ released from the sarcoplasmic reticulum, as a consequence ROS-mediated RyR2 channel activation and SERCA inhibition, contributes to myocytes contractile dysfunction. ROS are also responsible for the MMPs/TIMPs imbalance that drives ECM remodelling and fibrosis. Antioxidant compounds, like Folic acid or EUK-134, by scavenging the ROS in excess, can help restore the impaired cardiomyocyte function. Furthermore, DCA can restore ROS production and mitochondrial membrane potential by inhibiting PDK and thereby improving glucose oxidation. “Upwards arrow” indicates increase in levels; “Lowerwards arrow” indicates decrease in level. ROS reactive oxygen species, PCK protein kinase C, MAPK mitogen-activated protein kinase, mPTP mitochondrial permeability transition pore, PDK pyruvate dehydrogenase kinase, HIF hypoxia-inducible factor, FOXO1 Forkhead box protein O1, cMyc v-myc avin myelocytomastosis viral oncogene homologue, RyR2 ryanodine receptor 2, Kv 1.5 potassium voltage channel, SR sarcoplasmic reticulum, SERCA sarcoplasmic reticulum Ca2+-ATPase, MMP matrix metalloproteinases, TIMP tissue inhibitor metalloproteinases, ECM extracellular matrix, DCA dichloroacetate, PKD protein kinase D. (From Iacobazzi et al. [21]. It is an open access article)
Peripheral Monocytosis is a sign of monocyte and macrophage infiltration of the necrotic myocardium which arises two to three days after an acute MI. Likewise, a higher peak monocyte level is related with a larger LV end-diastolic volume and inferior LVEF. It was shown that a peak monocyte count ≥900/μL independently predicts HF, LV aneurysm formation, and cardiac events [219]. It should be stressed that monocytes have the capacity to generate and discharge inhibitory mediators of inflammation such as IL-10 and TGF-β [268]. There are varied monocytes with different functions in inflammatory response showed in humans such as CD16-monocytes that exhibit important amounts of CCR2 with pro-inflammatory properties same to murine Ly6Chi cells [268]. Further, inhibition of inflammatory signal pathways is correlated with Ly6Clo/CX3CR1hi monocytes entrapment that generates angiogenic mediators with infarct healing. On the other hand, in patients with ST elevation MI, CD14+/CD16-cells have an early peak and are negatively correlated with heart recovery [269].
6 Factors Influencing Cardiac Remodelling
6.1 Myocardial Infarction
It is the most frequent condition in which CR comes about. Taken together, heart ischemia leads to ‘necrotic cell death’. Further, the post-MI evolution implies apoptosis, inflammation, ECM remodelling, fibrotic scar formation, proliferation and differentiation of MyoFb, angiogenesis, and scar maturation [21]. All these reactions are determined to cause healing on short term, but they produce evolution to HF on long time. Therefore, after MI occurrence, the poor evolution continues with additional CR, hypertrophy, dilation, and systolic dysfunction [21, 73].
A number of innate immune pathways are triggered in MI [149]. It appears the production of “damage-associated molecular patterns (DAMP) ” by necrotic cells that further trigger membrane-bound “Toll-Like Receptors” (TLRs) [270, 271]. Also, among others innate immune pathways such as the “High mobility group box 1” (HMGB1), the “receptor for advanced glycation end-products” (RAGE) [21, 272] and the complement system are also triggered in the onset of inflammation after MI [21]. As a result, ROS are produced at ischemic injury with further activation of inflammatory signals pathways and myocardial dysfunction [149]. All triggered “innate immune pathways ” set off Nuclear Factor NF-κB with further initiation of inflammatory cytokines and chemokines [273]. As already described, pro-inflammatory cytokines significantly modulate the inflammatory reaction to cardiac ischemic injury. IL-1 triggers chemokines production in MI with entrapment of leukocytes [274]. An inactive precursor named pro-IL-1β generates active IL-1β by the converting enzyme caspase-1. Further, caspase-1 function is strongly controlled in multiprotein complexes named “inflammasomes ”, which further monitor production of IL-1β [275]. In MI, “inflammasome” initiation is restricted only in leukocytes and CFs with IL-1-mediated inflammatory cell infiltration and cytokine production [276]. ROS production and K+ efflux have a significant function in inflammasome triggering from CFs. Importantly, chemokines activation is a significant finding of post-MI inflammation [277]. The activation of chemokines receptors from leukocytes in MI exhibit a chemokines profile that controls the composition of the leucocytes infiltrate. Therefore, neutrophils are triggered firstly in MI followed by monocytes and lymphocytes. Apoptotic neutrophils as negative mediators of inflammation are exposed in Fig. 4.19 [149].
The role of neutrophil clearance in suppression of the inflammatory response. Abundant neutrophils infiltrate the infarcted myocardium. Neutrophils are short-lived cells that undergo apoptosis; dying neutrophils may contribute to repression of the post-infarction inflammatory response through several distinct mechanisms. First apoptotic neutrophils may release lactoferrin, an inhibitor of granulocyte transmigration. Second, during clearance of apoptotic neutrophils, macrophages secrete large amounts of anti-inflammatory and proresolving mediators including IL-10, TGF-β and lipoxins. Third, expression of decoy cytokine receptors by neutrophils may promote cytokine scavenging. Increased expression of chemokine receptors (such as CCR5) in apoptotic neutrophils may serve as a molecular trap for chemokines terminating their action. (From Frangogiannis [149] with permission)
The activation of neutrophils in the MI triggers apoptosis. Shortly, they are eliminated in MI by macrophages which activate powerful inhibitory pathways. Mediators such as TNF-α and IL-1β can maintain activated neutrophils in MI [278]. On the other hand, within 3–7 days after MI, the neutrophils undertake apoptosis [279].
6.2 Changes in Hemodynamic Load
In case of patients with anterior MI, the early LV dilation may be increased, as well as ventricular hypertrophy turns up to be a late and restricted modification during the first year [41]. Generally, the outcome of ongoing CR with ventricular dilation and abnormal ventricular hypertrophy causes a significant growing in total LV wall tension [41, 280]. As it will become evident, triggering of wall stress can activate further an amount of mechanisms that in the absence of any efficient therapy may cause further CR with progressive HF [50, 281].
6.3 Blood Pressure
Correspondingly, high blood pressure (BP) triggers structural modifications in the LVH with interstitial alterations, which further may produce diastolic dysfunction with HF. Additionally the functional effect of pressure overload hypertrophy may be determined by the features of the CR process. For example, if remodelling is eccentric with LV dilatation with normal relative wall thickness and raised wall stress [282], HF by a functional damage was described. On the other hand, HF does not occur in animals with concentric CR defined as normal chamber volume, raised relative wall thickness and normal wall stress. Previous hypertension may be related with extensive damaging CR and progression of HF after MI. This finding was shown by Richards et al. in 1093 patients, where 68% experienced serial neurohormonal sampling and assessment of LV function one to four days and three to 5 months post-MI [283]. In this study, in comparison with normotensives, hypertensive patients had significantly higher plasma levels of neurohormones at serial sampling with a significantly enhanced raise in LV volumes by remodelling at five months. Conversely, only normotensive patients had a recovery in LV ejection fraction at five months. Also, previous diagnosis of hypertension was related with a greater risk of HF necessitating hospitalization at a mean follow-up of two years (12.4 versus 5.5% in normotensives) [283]. Moreover, Cingolani et al. discovered that TSP-4 from CMs, adjusts cardiac contraction function to acute stress and it has a major role in chronic CR and HF [21, 284].
6.4 Neurohormonal Activation
Progressing HF is connected with an initially compensatory neurohumoral activation that may be a factor to the development of the structural defects. Both the sympathetic system and the renin–angiotensin–aldosterone system (RAAS) are implied in CR. Triggering of both systems turns on intracellular signaling pathways that increase the production of protein in CMs and CFs, with hypertrophy, fibrosis, switching on of growth factors and MMPs [285,286,287]. Moreover, it appears hemodynamic overload by vasoconstriction and water retention, raise of oxidative stress activity with direct cytotoxic effect, and apoptosis [285,286,287]. Therefore, the inhibition of these systems can has a major therapeutic role in attenuation or prevention of CR. Unfortunately, elevated plasma norepinephrine, renin activity, and antidiuretic hormone levels [288, 289] are indicators for poor survival in these patients [290]. Even if, neurohumoral activation is firstly adjustable, it is damaging over the long term by pathologic remodelling, especially in case of Ang II and norepinephrine [291]. The studies data are most convincing for the activation of the RAAS. Also, the plasma BNP concentrations are raised in progressive HF and interrelated with prognosis [292]. In spite of this, the release of BNP from myocytes in HF may defend against pathologic remodelling [293].
The RAAS has a significant function in the control of BP and electrolyte equilibrium. Within RAAS, Ang II produces triggering of sympathetic nervous system with vasoconstriction, sodium and water retention, and anorexia [294]. The damaging effects of RAAS in cardiovascular tissues cause CR by local triggering of the RAAS with autocrine and paracrine mechanisms [295,296,297]. Mainly, the pathophysiological effects of Ang II in the cardiovascular system are controlled by a member of the GPCR family termed the 7 transmembrane (TM7) spanning AT1 receptor [296, 298, 299]. According to recent data, the mechanical stress together with systemically and locally Ang II cause by the triggering of AT1 receptor, cardiac hypertrophy [295,296,297, 300]. It seems that studies with the AT1 receptor blockers (ARBs) as candesartan showed that switching off of triggered AT1 receptor by mechanical stress, notably reduced hypertrophic reaction in cultured CMs [301,302,303]. Therefore, mechanical stress causes cardiac hypertrophy in vivo by initiation of the AT1 receptor with no correlation of Ang II [295, 296].
Mechanical stretch and Ang II by attachment to the AT1 receptor causes to its structure to switch on with occurrence of Cys residues inside the ligand-binding pocket. Further, if mechanical stress continues, TM7 undertakes a counter clockwise rotation with a modification in the ligand-binding pocket [304]. It is not determined exactly by current studies the mechanisms by which mechanical stress activates the AT1 receptor perceives its structure change, preparing for dissimilar initiation of particular intracellular signaling mediators [303].
6.5 Role of Angiotensin II
Significance of angiotensin II (Ang II) in pathologic CR is demonstrated by data of large trials in humans that have been shown that angiotensin-converting-enzyme inhibitors (ACEI) increase survival in HF by decrease or even reverse of some parameters of CR [305, 306]. Shortly, Ang II is produced and has locally and systemically effects. So that, mechanical stretch directly boost Ang II release from CMs [301]. Also, Ang II seems to sustain directly CR. Previous studies have been showed that human CFs cultured from cardiomyopathic and ischemic hearts have on CMs the expression of AT1 receptors [307, 308]. In fact, these CFs reply to Ang II with raise of collagen production by activation of AT1 receptor [309,310,311]. Despite the fact that Ang II is produced locally or systemically, it may directly support CR. In fact, these CFs may reply to Ang II with AT1 receptor-mediated collagen synthesis [309,310,311]. On the other hand, Ang II acts via the AT1 receptor with boosting of protein synthesis and results in hypertrophy of CMs [309]. Both ACEI and Ang II receptor antagonists can reverse remodelling in HF [212].
Aldosterone secretion is increased by Ang II, and also may be a factor in CR. The heart contains mineralocorticoid receptors and takes out aldosterone after a MI, supporting the post MI remodelling [312]. Moreover, the secondary hyperaldosteronism commonly seen in patients with HF may participate to cardiac hypertrophy and fibrosis [313, 314]. It should be stressed that the benefit effects connected with spironolactone or eplerenone, which both link the mineralocorticoid receptor may result with diminished fibrosis [315].
6.6 Energy Metabolism and Cardiac Remodelling
Ischemia, pressure and volume overload are forms of stress that activates human heart to adapt its metabolic function to use glucose instead of the free fatty acids [316]. It seems that free fatty acids provide the highest quantity of ATP to human heart [317]. On the other hand, the glucose metabolism needs a reduced amount of oxygen consuming for same quantity of ATP synthesis, being the most effective alternative in highest metabolic states such as short-term of severe cardiac stress [318]. As a rule, in normal heart, free fatty acids are the main energy substance representing about 60–90% of energy reserves. Both free fatty acids and glucose metabolites undergo β-oxidation and glycolysis in the citric acid cycle, resulting in FADH2 and NADH. Finally, the obtained energy is accumulated and carried as phosphocreatine (Fig. 4.20) [319].
Schematic representation of classic pathways of cardiac metabolism . Substrates are transported across the extracellular membrane into the cytosol and are metabolized in various ways. For oxidation, the respective metabolic intermediates (e.g., pyruvate or acyl-CoA) are transported across the inner mitochondrial membrane by specific transport systems. Once inside the mitochondrion, substrates are oxidized or carboxylated (anaplerosis) and fed into the Krebs cycle for the generation of reducing equivalents (NADH2 and FADH) and GTP. The reducing equivalents are used by the electron transport chain to generate a proton gradient, which in turn is used for the production of ATP. This principal functionality can be affected in various ways during HF thereby limiting ATP production or affecting cellular function in other ways (see text and further Figures for details). IMS mitochondrial intermembrane space, GLUT glucose transporter, FAT fatty acid transporter, MPC mitochondrial pyruvate transporter. (Illustration Credit: Ben Smith). (From Doenst et al. [319] with permission)
During stress is stopped the normal inhibition of glucose oxidation by free fatty acids [303]. It seems that the nuclear receptor peroxisome proliferator-activated receptor-α (PPARα) is a significant contributory factor that changes from fatty acid metabolism to glucose metabolism [316, 320]. Further, Karbowska et al. showed on ventricular biopsies from 5 patients a 54% fall of PPARα protein levels in end-stage HF in comparison with controls [316, 321]. Therefore, CR implies cardiac dysfunction with energy loss due to the disproportion from the oxygen reserve and use, with a diminished free fatty acids oxidation and raised glucose oxidation [316]. In addition, β-oxidation fall leads to deposit of triglycerides and lipotoxicity, mitochondrial dysfunction [316]. Altogether, these modifications causes for myocardial proteins further low levels of energy reserves with oxidative stress and ROS, with their sides effects (Fig. 4.21) [316, 321,322,323,324].
Overview of metabolic remodeling and proposed mechanisms linking it to other processes in the progression to HF. Metabolic pathways are blue. Bold lines indicate pathways/processes that are increased or dominant. Thin lines represent pathways/ processes that are decreased. The question marks imply unknown causes/ effects. In general, metabolic remodeling in cardiac hypertrophy and failure is characterized by a shift away from energy production to activation of biosynthetic pathways required for structural remodeling processes such as ventricular hypertrophy and fibrosis. Particularly, fatty acid oxidation is decreased and may not be sufficiently compensated given the lack of increase in glucose oxidation. These alterations and further mitochondrial defects result in ATP depletion. Instead of being oxidized, pyruvate may be preferentially used for anaplerosis to maintain Krebs cycle moieties, which might be increasingly channeled into protein synthesis. Hypertrophic mediators such as MAPKs and NFAT are activated as a result of increased mitochondrial ROS and flux through the HBP, respectively. Overproduction of mitochondrial ROS causes oxidative damage. Although the flux through the PPP is increased, anti-oxidative defense might be inadequate due to the consumption of NADPH by the anaplerotic malic enzyme. Mitochondrial damage and ATP depletion may stimulate autophagy. Increased activity of autophagy and the UPS may contribute to hypertrophy by providing amino acids and other metabolites. Increase in mitophagy may trigger myocardial inflammation by releasing mitochondrial DNA. H hexosamine biosynthetic pathway (HBP), P pentose phosphate pathway (PPP), G glycolysis, A anaplerosis, O oxidation, ETC electron transport chain, ROS reactive oxygen species, UPS ubiquitin-proteasome system. (From Doenst et al. [319] with permission)
In case of RV, the metabolism data is from the LV studies. As already described, the RV has smaller afterload than the LV due the decreased pulmonary vascular resistance [316]. Even if, RV and LV have similar stroke volumes, the RV has near 25% from the stroke volume of the LV because of the low PVR [316, 325]. Extensive “transcriptional, translational and energetic” disturbances to physiologic and pathophysiologic stress occur in RV. The conversion from pressure overload and volume overload to cardiac hypertrophy and later RVF is correlated with the switch from free fatty acids to glucose metabolism for ATP production. As a result, the RVF is an energy-deprived state with deficient ATP amounts. For this reason, PET using specific radioactive tracers provides a complete description of RV metabolism [316]. These metabolic differences might corelate with the dissimilarities in ventricular wall stress and intraventricular pressure dynamics (Fig. 4.22) [316].
Right ventricular metabolism . (From Altin et al. [316] with permission)
To sum up, metabolic alteration in the hypertrophied RV imitates metabolic alteration of the hypertrophied and failing LV [316]. Nagaya et al. [326] studied 21 patients with RVH due to PH by using magnetic resonance spectroscopic imaging (MRSI) that associates cardiac structure with metabolic function. They found important RV contraction dysfunction in patients with altered myocardial free fatty acid metabolism. Further, in a study of 16 patients with idiopathic PAH, Bokhari et al. proved that PET imaging is for determining myocardial glucose assimilation and use [316, 327]. They demonstrated that RV glucose usage is associated with hemodynamic parameters such as mean PA pressure, doubtlessly implying that RV dysfunction is switched on myocardial glucose metabolism and being a sign of RV dysfunction. Can et al. [328] have been demonstrated same features on 23 patients with PAH and 16 healthy controls evaluated by PET. Their results established that raised fludeoxyglucose (18F) increase in the RV myocardium were connected with raised RV loading conditions and with the existence of elevated pulmonary artery pressures but not with their stage [316, 328].
Also, MRSI for the study of myocardial triglyceride load demonstrated an accurate statistically significance correlation with triglycerides from RV biopsy [316, 329]. Currently, no other study tried to measure in the RV the lipid transitional products.
It is not determined if cardiac metabolic alterations maintain during the development of RVH, that is characterized by important decrease of CO, increase of RV filling pressure and raised fibrosis [21, 330]. Consequently, RVH is correlated with increased mitochondrial ROS, which downregulates HIF1α and triggers p53 pathways, in the end with dysregulated pyruvate dehydrogenase kinase (PDK) and diminished glucose uptake [21, 331]. Raised PDK expression is a frequent feature in RVH during glucose oxidation, as a result there is a decrease in mitochondrial respiration [21, 330]. A number of clinical trials directed on molecular dysfunction in RVH and RV failure are undergoing, even if the precise outcomes for pharmacologic involvements on RV abnormal metabolism are not determined [316].
6.7 Electrical Remodelling in Cardiac Remodelling
As already been described, the functional, structural, and electrical modifications of CMs to stress described by hypertrophy, HF, and ischemia define CR, which disposes to raised occurrence of ventricular ectopy and arrhythmias. “Arrhythmia-induced changes in the electrophysiological properties of heart tissue which predisposes to an increased frequency of ventricular ectopy and arrhythmias are referred to as electrical remodelling” [332].
Specifically, Na+-Ca2+ exchanger (NCX) mediates intracellular Ca2+ concentration and its activity is controlled by intracellular concentrations of Ca2+, Na+, ATP, pH, and phosphorylation of NCX, all being modified in HF [332]. Therefore, HF with contractile dysfunction and arrhythmogenesis may be explicated by amplified NCX and diminished SERCa2+a function, consequently with raised Ca2+ discharge from CMs and delayed afterdepolarizations [332,333,334]. Also, during cardiac diastole dysfunction, NCX sustains Ca2+ transportation from intracellular space and diminishes SERCa2+a function [332, 333]. It has to be underlined, that NCX activity is mediated in cardiac hypertrophy, function sustained by diminished NCX activity but with raised NCX protein and transcript levels [332]. It seems that calcineurin inhibition weakens the boost of NCX1 transcript and protein levels correlated with pressure overload, advocating that calcineurin is vital in the adjustment of NCX1 transcript synthesis and degeneration [332, 335].
Also, there is a diminished expression and function of Na+-K+ATPase in HF [332, 336] that make susceptible cardiac tissue to arrhythmias by raised action potential duration, and increased depolarizing current, and extracellular K+ [332]. According to experimental cardiomyopathic studies, ETA receptor blockers demonstrated to stop electrical remodelling and ventricular arrhythmias by diminishing K+ and Ca2+ current expression, rising QT interval and action potential duration [332, 337].
Electrical anisotropy caused by myocardial fibrosis and modifications of intracellular Ca2+ could produce the electrophysiological remodelling and arrhythmias from hypertrophy [332]. Further, modification of the collagen amount, type, and cross-linking is correlated with myocardial fibrosis and CR with electrophysiological abnormalities [338].
RVH, dilation, and septal displacement also create RV dyssynchronous motion [339,340,341] and dyssynchronous RV-LV contraction [341,342,343]. Delayed RV lateral wall contraction and interventricular dyssynchrony in PAH are not related to QRS duration or abnormal electric activation such as left bundle-branch block but rather to RV wall stress, septal shift, LV end-diastolic volume, and stroke volume [342, 343]. These ventricular-ventricular interactions almost certainly increase the ratio of systolic to diastolic duration because interventricular dyssynchrony is related to lengthening of the RV contraction [343].
To sum up, existing data supports that myocardial hypertrophy form determines the electrical CR and the reverse of it [332, 344]. Nevertheless, in pressure-overload states with reverse of hypertrophy is correlated with the reverse of the electrical remodelling [345,346,347]. However, the dissimilarity between the reverse of electrical remodelling in pressure-versus volume-overload states is unknowable [332]. Both structure and electrical CR should be regarded as independent clinical disorders [332]. The assessment of risk factors for arrhythmias has a significant function in the regress of hypertrophy and the electrical CR [347].
6.8 Coronary Vascular Remodelling in Cardiac Remodelling
Coronary vascular remodelling causes adjustable reactions such as the rapid adaptation of vessel diameter by modifications in smooth muscle tone, changes in vessel diameter structure, adding or elimination of vessels by “angiogenesis (sprouting/splitting)”, or “vascular pruning” [348]. It important to underline that physiological vascular adaptation keeps an appropriate perfusion, but vascular maladaptation takes place in disorders such as hypertension [348]. Also, regulatory mechanisms in larger vessels are different from microcirculation that has a vital role in physiological vascular adaptation and pathological states [348]. Generally speaking, growing of size and number of microvessels during exercise or involution with microvascular remodelling because of constant decline of physical activity appear [349]. Reduction of epicardial arteries with hemodynamic- and metabolic modifications causes process of collateralization or arteriogenesis defined by “structural enlargement of arteriolar vessels and arterio-arterial anastomoses” [348, 350].
As a result, constant chronic remodelling of coronary vessels leads to over-prolonged modifications of vessels diameter with or without shifts in wall mass (Fig. 4.23) [348, 352, 353]. Therefore, coronary vessels adjust to mechanical stimuli, such as fluid shear stress acting on ECs, circumferential wall stress and metabolic signals [348, 354, 355].
Mechanisms and models of vascular remodelling . Left: Signals for vascular adaptation include wall shear stress at the endothelial surface (t), circumferential wall stress (s), and metabolic signals. Metabolic signals maybe elicited by low oxygen availability and act as vasodilators and stimulate vascular growth, or they could be vasoconstricting mediators produced at high oxygen partial pressures but in decreasing amounts with decreasing pO2. Metabolic substances are convected downstream, but elicit also a signal that is conducted upstream within the vessel wall. Middle: Vascular responses elicited by these stimuli comprise changes of diameter and wall mass. Right: An integrated model [351] which connects the local conditions (pressure, flow, and metabolic state) with derived stimuli (σ, τ, and metabolic stimuli) and the vascular changes in vessel diameter or wall mass. Lines indicate biological reactions (solid) and physical relations (dashed). (From Pries et al. [348] with permission)
Essentially, exposure of the LV to afterload stress causes firstly the development of new capillaries or angiogenesis, to sustain the raised blood flow of hypertrophied CMs. In case of angionesis are implied raised production of the proangiogenic factors hypoxia HIF1α and VEGF. If the LV starts to fail, the capillary density starts to decrease. On the other hand, the capillary density of the RV reduces with the beginning of pressure overload upsurge. RVF is a frequent side effect of chronic RV pressure overload with progression to RV ischemia. Specifically, increased pulmonary arterial pressure boosts RV wall tension and oxygen demand in correlation with alteration of coronary blood flow. For instance, Eisenmenger’s syndrome produces a level of RV afterload same to idiopathic PAH, only that the survival is longer with latent overt RVF [356]. In addition, PAH during diagnosis protocol have different degrees of RVF even if the RV afterload is highly developed.
7 Reverse Cardiac Remodelling
CR can be reversed with maximized therapy that initiates ongoing recovery of cardiac function and thus enhances prognosis of patients [357]. Even if, reverse CR could arise unexpectedly in heart pathologies, it is more frequently seen as reaction to medical, device-based, or surgical therapies, such as beta-blockers, cardiac resynchronization therapy (CRT), revascularization and valve surgery [358]. The various cardiac pathologies with noticed reverse CR prove that myocardial remodelling is bidirectional and takes place no matter of the myocardial disease aetiology, length, and severity (Fig. 4.24) [358]. Moreover, prognosis is improved in patients with reverted heart dysfunction, for that reason reversal of CR should be the most important treatment aim. Therefore, effective treatment should reverse cardiac remodelling [359].
Myocardial recovery in clinical settings. The segments of the outmost ring highlight pathophysiological processes implicated by reverse remodeling in particular clinical settings that comprise the middle ring. Abbreviations: ALM acute lymphocytic myocarditis, CPAP continuous positive airway pressure, RAAS renin–angiotensin–aldosterone system, LVAD left ventricular assist device, MVR mitral valve repair/replacement, AVR aortic valve replacement, CSD cardiac support device, CRT cardiac resynchronization therapy. (From Hellawell et al. [358] with permission)
Both ACEI and Ang II receptor antagonists, also known as angiotensin receptor blockers (ARBs) have been utilized to prevent CR. Preventing raised RAAS stimulation that may limit subsequent maladaptive cardiac remodelling. For instance, RV samples taken from control patients showed higher ventricular weight with raised collagen and foetal contractile protein genes, and diminished SR Ca2+-ATPase. Moreover, ACEI exert antioxidant effects by inhibiting the transcription factor NF-kB that controls the synthesis of various genes associated with inflammatory response, such as cytokines, chemokines, growth factors, and cell adhesion molecules [360,361,362,363]. The complexity of the intramyocardial mechanisms involved in CR should also take into account endothelial damage, on which PDE5 inhibition acts positively, as recently demonstrated in a meta-analysis of type 2 diabetic cardiovascular patients [364]. Also, clinically relevant evidence suggests that PDE5 inhibition has favourable direct myocardial effects via cGMP and cAMP activities that may counterbalance hypertrophic and proapoptotic signaling, including adrenergic stimulation [365].
7.1 Cardiac Regenerative Medicine
Production of “induced cardiac-like myocytes” (iCLMs) shows all the signs of a new future successful method to regenerate damaged CMs [366]. Replacing lost CMs by injecting cardiac progenitors, cardiospheres, or CMs derived from “induced pluripotent stem cells” (iPSCs) and/or “embryonic stem cells” (ESCs) has been researched intensively [367]. Importantly, miRNAs are important for stem cell differentiation, as well as indirect and direct reprogramming to multiple lineages [368,369,370,371]. To sum up, miRNA based therapy can be used to promote CMs proliferation, reprogram directly fibroblasts to CMs or indirectly to iPSc as well as driving the differentiation of iPSCs, ESCs or CPCs to CMs (Fig. 4.25) [367]. Another new treatment choice is to release cells in the damaged myocardium. According to evidence, various cell categories have been utilized for heart regeneration, such as ESCs, CMs obtained from iPSCs, mesenchymal stem cells (MSCs), bone marrow MSCs, cardiac stem cells, cardiac progenitor cells, skeletal myoblasts, ECs, adipose tissue-derived stem cells (ATDSCs), and CMs [372]. Nevertheless, studies have still unremarkable outcomes.
miRNAs and reprogramming. miRNAs promote the generation of cardiomyocytes via a number of mechanisms. Fibroblasts can be reprogrammed into cardiomyocytes by miRNAs directly or through an intermediate iPSC state. miRNAs also promote cardiac progenitor cell (CPC) and embryonic stem cell (ESC) cardiac differentiation. miRNAs can promote or inhibit cardiomycyte proliferation. (From Hodgkinson et al. [367] with permission)
7.2 Device-Based Therapies
Pharmacological treatments that diminish on either side PVR or systemic vascular resistance can reduce the development of fibrosis in the RV and LV, respectively. Likewise, non-pharmacological mechanical decrease of LV load by LV assist devices (LVADs) can attenuate fibrosis in both ventricles [373].
For instance, cardiac resynchronization therapy (CRT) with biventricular (BiV) pacing is an well-known choice therapy in case of patients with overt HF, diminished LV systolic EF, and delayed ventricular conduction with enlarged QRS complex (e.g. electrical dyssynchrony). In fact, Sachse et al. [374] showed that CRT reduces symptoms and mortality in patients affected by dyssynchronous heart failure (DHF) produced by dyssynchronous electrical and mechanical activation of the left and right ventricle. Also, they concluded that CR of electrophysiological properties, hemodynamic and protein expression due to DHF is partially restored by CRT. Specifically, CRT can reverse damages of intracellular structures and function of CMs from HF, with early successful signs of recovery as tubular system structure [374].
Ventricular Assist Devices (VADs) can prevent ongoing CR and produce reverse CR, mainly by decrease of mechanical load of the damaged ventricles [373]. Also, VADs are not same thing with artificial hearts, which are planned for temporary taking up of cardiac function with their latter withdrawal from the patient’s heart [373]. VADs are designed to support the LVAD, the right ventricle (RVAD) or both ventricles (BiVAD). LVAD is the most frequent device used in a damaged heart, but in case of increased pulmonary arterial resistance, RVAD will be added to help with cardiac circulation. According to data, the evaluation of LVAD outcomes looking the reverse of RV remodelling, showed there were no change in CMs size among patients with LVADs and control group [373]. Conversely, LVAD therapy produced diminishing of collagen and TNF-α from RV, supporting that LVAD can reduce RVH by inhibiting the paracrine factors [373]. Further, Barbone et al. studied the involvement of these factors in reverse of CR [375]. Shortly, they studied heart samples from patients who required either LVAD or pharmacological treatment for severe HF [375]. Regardless of LVAD type, the RV volume and CM size enlarged, but isolated RV muscle pieces from inserted LVAD showed a diminished force formation at high pacing rates. Finally, they concluded that reverse RV remodelling after LVAD placing is minimum [375]. In conclusion, LVADs implantation is largely helpful for showing biology of reverse CR: changes of mRNA and microRNA profiles, decrease of apoptosis, diminishing of inflammatory cytokines (e.g., TNF-α), ECM remodelling, regression of action potential lengthening, regression of cardiac myocyte hypertrophy, improved contractility, regression of shape distortions, and improved β-adrenergic responsiveness [358].
Other studies evaluated hearts from end-stage CHF with no VADs, with LVAD or with BiVAD [376]. In comparison with LVAD, BiVAD-supported hearts showed notably diminished right atrium pressures with nearly normal RV end-diastolic pressure-volume interactions. Moreover, the hearts with BiVAD demonstrated normalized RV myocyte diameter and myocardial contraction when isoproterenol perfusion was used. All these modifications were not demonstrated in hearts with LVADs. However, LVADs diminish only RV afterload. To sum up, VADs could induce RV remodelling, but further studies data is necessary [376].
Conclusions
RV remodelling is correlated with functional, cellular and molecular changes [316]. CMs hypertrophy and hyperplasia modify RV geometry, while apoptosis rate and damages of intracellular structures induce further remodelling [316]. RVH and RV dilatation can be correlated with diminished ventricular volume, associated or not with changed hemodynamic status [316]. As a result, physiologic and pathophysiologic stress produces in RV serious transcriptional, translational and energetic modifications [316]. The development of cardiac hypertrophy from pressure and volume overload with failing is correlated with transition from free fatty acids to glucose metabolism for ATP formation [316]. RVF is an energy-depleted condition with lacking ATP levels. Reassuring successful molecular targets are established by ongoing clinical trials studying the molecular alteration from RVH and failure [316]. Ultimately, medical therapy with vasodilators seems to raise both RV stroke volume and CO, while ACEI and ARBs can postpone RVH by diminishing the exhibition of hypertrophy-related genes in the RV. Nonetheless, immunomodulator therapy is correlated with diminishing of RVH and remodelling-related gene expression [316].
References
Hochman JS, Bulkley BH. Expansion of acute myocardial infarction: an experimental study. Circulation. 1982;65(7):1446–50.
Pfeffer JM, Pfeffer MA, Braunwald E. Influence of chronic captopril therapy on the infarcted left ventricle of the rat. Circ Res. 1985;57(1):84–95.
Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990;81(4):1161–72.
Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000;35(3):569–82.
Swynghedauw B. Molecular mechanisms of myocardial remodeling. Physiol Rev. 1999;79(1):215–62.
Roberts CS, Maclean D, Maroko P, Kloner RA. Early and late remodeling of the left ventricle after acute myocardial infarction. Am J Cardiol. 1984;54(3):407–10.
Swynghedauw B. Remodeling of the heart in chronic pressure overload. Basic Res Cardiol. 1991;86(Suppl 1):99–105.
Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity. Physiol Rev. 2008;88(2):389–419. https://doi.org/10.1152/physrev.00017.2007.
Heineke J, Molkentin JD. Regulation of cardiac hypertrophy by intracellular signalling pathways. Nat Rev Mol Cell Biol. 2006;7(8):589–600. https://doi.org/10.1038/nrm1983.
Dorn GW, Robbins J, Sugden PH. Phenotyping hypertrophy: eschew obfuscation. Circ Res. 2003;92(11):1171–5. https://doi.org/10.1161/01.RES.0000077012.11088.BC.
Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358(13):1370–80. https://doi.org/10.1056/NEJMra072139.
Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA. Controversies in ventricular remodelling. Lancet. 2006;367(9507):356–67. https://doi.org/10.1016/S0140-6736(06)68074-4.
Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117(13):1717–31. https://doi.org/10.1161/CIRCULATIONAHA.107.653584.
D'Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Kernis JT, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991;115(5):343–9.
McLaughlin VV, McGoon MD. Pulmonary arterial hypertension. Circulation. 2006;114(13):1417–31. https://doi.org/10.1161/CIRCULATIONAHA.104.503540.
Machuca TN, de Perrot M. Mechanical support for the failing right ventricle in patients with precapillary pulmonary hypertension. Circulation. 2015;132(6):526–36. https://doi.org/10.1161/CIRCULATIONAHA.114.012593.
Zaffran S, Kelly RG, Meilhac SM, Buckingham ME, Brown NA. Right ventricular myocardium derives from the anterior heart field. Circ Res. 2004;95(3):261–8. https://doi.org/10.1161/01.RES.0000136815.73623.BE.
Thomas T, Yamagishi H, Overbeek PA, Olson EN, Srivastava D. The bHLH factors, dHAND and eHAND, specify pulmonary and systemic cardiac ventricles independent of left-right sidedness. Dev Biol. 1998;196(2):228–36.
Kondo RP, Dederko DA, Teutsch C, Chrast J, Catalucci D, Chien KR, Giles WR. Comparison of contraction and calcium handling between right and left ventricular myocytes from adult mouse heart: a role for repolarization waveform. J Physiol. 2006;571(Pt 1):131–46.
Friedberg MK, Redington AN. Right versus left ventricular failure: differences, similarities, and interactions. Circulation. 2014;129(9):1033–44. https://doi.org/10.1161/CIRCULATIONAHA.113.001375.
Iacobazzi D, Suleiman MS, Ghorbel M, George SJ, Caputo M, Tulloh RM. Cellular and molecular basis of RV hypertrophy in congenital heart disease. Heart. 2016;102(1):12–7. https://doi.org/10.1136/heartjnl-2015-308348.
Lowes BD, Minobe W, Abraham WT, Rizeq MN, Bohlmeyer TJ, Quaife RA, Roden RL, Dutcher DL, Robertson AD, Voelkel NF, Badesch DB, Groves BM, Gilbert EM, Bristow MR. Changes in gene expression in the intact human heart. Downregulation of alpha-myosin heavy chain in hypertrophied, failing ventricular myocardium. J Clin Invest. 1997;100(9):2315–24.
Bakerman PR, Stenmark KR, Fisher JH. Alpha-skeletal actin messenger RNA increases in acute right ventricular hypertrophy. Am J Phys. 1990;258(4 Pt 1):L173–8.
Bartelds B, Borgdorff MA, Smit-van Oosten A, Takens J, Boersma B, Nederhoff MG, Elzenga NJ, van Gilst WH, De Windt LJ, Berger RM. Differential responses of the right ventricle to abnormal loading conditions in mice: pressure vs. volume load. Eur J Heart Fail. 2011;13(12):1275–82. https://doi.org/10.1093/eurjhf/hfr134.
Nagendran J, Archer SL, Soliman D, Gurtu V, Moudgil R, Haromy A, St Aubin C, Webster L, Rebeyka IM, Ross DB, Light PE, Dyck JR, Michelakis ED. Phosphodiesterase type 5 is highly expressed in the hypertrophied human right ventricle, and acute inhibition of phosphodiesterase type 5 improves contractility. Circulation. 2007;116(3):238–48.
Urashima T, Zhao M, Wagner R, Fajardo G, Farahani S, Quertermous T, Bernstein D. Molecular and physiological characterization of RV remodeling in a murine model of pulmonary stenosis. Am J Physiol Heart Circ Physiol. 2008;295(3):H1351–68.
Ozhan G, Weidinger G. Wnt/β-catenin signaling in heart regeneration. Cell Regen. 2015;4(1):3.
Woodgett JR. Regulation and functions of the glycogen synthase kinase-3 subfamily. Semin Cancer Biol. 1994;5(4):269–75.
Embi N, Rylatt DB, Cohen P. Glycogen synthase kinase-3 from rabbit skeletal muscle. Separation from cyclic-AMP-dependent protein kinase and phosphorylase kinase. Eur J Biochem. 1980;107(2):519–27.
Nagendran J, Gurtu V, Fu DZ, Dyck JR, Haromy A, Ross DB, Rebeyka IM, Michelakis ED. A dynamic and chamber-specific mitochondrial remodeling in right ventricular hypertrophy can be therapeutically targeted. J Thorac Cardiovasc Surg. 2008;136(1):168–78. 178.e1–3
Zornoff LA, Paiva SA, Duarte DR, Spadaro J. Ventricular remodeling after myocardial infarction: concepts and clinical implications. Arq Bras Cardiol. 2009;92(2):150–64.
Mesquita ET, Montera MW, de Souza Neto JD, Bernardez-Pereira S, Freitas AF Jr, Volschan A, Biolo A, Nunes Filho AC, Chagas AC, Jorge AJ, Almeida DR, Arteaga E, dos Santos Junior EG, Fernandes F, Ramires FJ, Bacal F, Tarasoutshi F, Feitosa GS, Villacorta H Jr, Ferreira JF, Vieira JM Jr, Moura LA, Pires LJ, Correia LC, Rohde LE, Rivas M, Moreira Mda C, Kaiser SE, Ferreira SM, Martins SM, Martinez TL. Biomarkers in cardiology--part 1--in heart failure and specific cardiomyopathies. Arq Bras Cardiol. 2014;103(6):451–9.
Azevedo PS, Polegato BF, Minicucci MF, Paiva SA, Zornoff LA. Cardiac remodeling: concepts, clinical impact, pathophysiological mechanisms and pharmacologic treatment. Arq Bras Cardiol. 2016;106(1):62–9.
Anand IS, Florea VG, Solomon SD, Konstam MA, Udelson JE. Noninvasive assessment of left ventricular remodeling: concepts, techniques, and implications for clinical trials. J Card Fail. 2002;8(6 Suppl):S452–64.
Heusch G, Libby P, Gersh B, Yellon D, Böhm M, Lopaschuk G, Opie L. Cardiovascular remodelling in coronary artery disease and heart failure. Lancet. 2014;383(9932):1933–43.
Sabbah HN, Goldstein S. Ventricular remodelling: consequences and therapy. Eur Heart J. 1993;14(Suppl C):24–9.
Henning RJ. Effects of positive end-expiratory pressure on the right ventricle. J Appl Physiol. 1986;61(3):819–26.
MacNee W. Pathophysiology of cor pulmonale in chronic obstructive pulmonary disease. Part one. Am J Respir Crit Care Med. 1994;150(3):833–52.
Gaudron P, Eilles C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation. 1993;87(3):755–63.
White HD, Norris RM, Brown MA, Brandt PW, Whitlock RM, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 1987;76(1):44–51.
Rumberger JA, Behrenbeck T, Breen JR, Reed JE, Gersh BJ. Nonparallel changes in global left ventricular chamber volume and muscle mass during the first year after transmural myocardial infarction in humans. J Am Coll Cardiol. 1993;21(3):673–82.
Bussani R, Abbate A, Biondi-Zoccai GG, Dobrina A, Leone AM, Camilot D, Di Marino MP, Baldi F, Silvestri F, Biasucci LM, Baldi A. Right ventricular dilatation after left ventricular acute myocardial infarction is predictive of extremely high peri-infarctual apoptosis at postmortem examination in humans. J Clin Pathol. 2003;56(9):672–6.
Oakley C. Importance of right ventricular function in congestive heart failure. Am J Cardiol. 1988;62(2):14A–9A.
Di Salvo TG, Mathier M, Semigran MJ, Dec GW. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol. 1995;25(5):1143–53.
Liu L, Eisen HJ. Epidemiology of heart failure and scope of the problem. Cardiol Clin. 2014;32(1):1–8. vii
Pimentel M, Zimerman LI, Rohde LE. Stratification of the risk of sudden death in nonischemic heart failure. Arq Bras Cardiol. 2014;103(4):348–57.
Braunwald E. Heart failure. JACC Heart Fail. 2013;1(1):1–20.
McKay RG, Pfeffer MA, Pasternak RC, Markis JE, Come PC, Nakao S, Alderman JD, Ferguson JJ, Safian RD, Grossman W. Left ventricular remodeling after myocardial infarction: a corollary to infarct expansion. Circulation. 1986;74(4):693–702.
Anversa P, Olivetti G, Capasso JM. Cellular basis of ventricular remodeling after myocardial infarction. Am J Cardiol. 1991;68(14):7D–16D.
Grossman W, Jones D, McLaurin LP. Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Invest. 1975;56(1):56–64.
Douglas PS, Morrow R, Ioli A, Reichek N. Left ventricular shape, afterload and survival in idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 1989;13(2):311–5.
Mitchell GF, Lamas GA, Vaughan DE, Pfeffer MA. Left ventricular remodeling in the year after first anterior myocardial infarction: a quantitative analysis of contractile segment lengths and ventricular shape. J Am Coll Cardiol. 1992;19(6):1136–44.
Weisman HF, Bush DE, Mannisi JA, Bulkley BH. Global cardiac remodeling after acute myocardial infarction: a study in the rat model. J Am Coll Cardiol. 1985;5(6):1355–62.
Jugdutt BI. Effect of captopril and enalapril on left ventricular geometry, function and collagen during healing after anterior and inferior myocardial infarction in a dog model. J Am Coll Cardiol. 1995;25(7):1718–25.
Sharov VG, Sabbah HN, Shimoyama H, Goussev AV, Lesch M, Goldstein S. Evidence of cardiocyte apoptosis in myocardium of dogs with chronic heart failure. Am J Pathol. 1996;148(1):141–9.
Teiger E, Than VD, Richard L, Wisnewsky C, Tea BS, Gaboury L, Tremblay J, Schwartz K, Hamet P. Apoptosis in pressure overload-induced heart hypertrophy in the rat. J Clin Invest. 1996;97(12):2891–7.
Olivetti G, Abbi R, Quaini F, Kajstura J, Cheng W, Nitahara JA, Quaini E, Di Loreto C, Beltrami CA, Krajewski S, Reed JC, Anversa P. Apoptosis in the failing human heart. N Engl J Med. 1997;336(16):1131–41.
Tan LB, Jalil JE, Pick R, Janicki JS, Weber KT. Cardiac myocyte necrosis induced by angiotensin II. Circ Res. 1991;69(5):1185–95.
Villarreal FJ, Kim NN, Ungab GD, Printz MP, Dillmann WH. Identification of functional angiotensin II receptors on rat cardiac fibroblasts. Circulation. 1993;88(6):2849–61.
Anderson KR, Sutton MG, Lie JT. Histopathological types of cardiac fibrosis in myocardial disease. J Pathol. 1979;128(2):79–85.
Weber KT, Pick R, Silver MA, Moe GW, Janicki JS, Zucker IH, Armstrong PW. Fibrillar collagen and remodeling of dilated canine left ventricle. Circulation. 1990;82(4):1387–401.
Bogaard HJ, Abe K, Vonk Noordegraaf A, Voelkel NF. The right ventricle under pressure: cellular and molecular mechanisms of right-heart failure in pulmonary hypertension. Chest. 2009;135(3):794–804.
Modesti PA, Vanni S, Bertolozzi I, Cecioni I, Lumachi C, Perna AM, Boddi M, Gensini GF. Different growth factor activation in the right and left ventricles in experimental volume overload. Hypertension. 2004;43:101–8.
Colucci WS, Elkayam U, Horton DP, Abraham WT, Bourge RC, Johnson AD, Wagoner LE, Givertz MM, Liang CS, Neibaur M, Haught WH, LeJemtel TH. Intravenous nesiritide, a natriuretic peptide, in the treatment of decompensated congestive heart failure. Nesiritide Study Group. Engl J Med. 2000;343(4):246–53.
Raizada V, Thakore K, Luo W, McGuire PG. Cardiac chamber-specific alterations of ANP and BNP expression with advancing age and with systemic hypertension. Mol Cell Biochem. 2001;216(1-2):137–40.
Reddy S, Zhao M, DQ H, Fajardo G, Hu S, Ghosh Z, Rajagopalan V, JC W, Bernstein D. Dynamic microRNA expression during the transition from right ventricular hypertrophy to failure. Physiol Genomics. 2012;44:562–75.
Wang GY, McCloskey DT, Turcato S, Swigart PM, Simpson PC, Baker AJ. Contrasting inotropic responses to alpha1-adrenergic receptor stimulation in left versus right ventricular myocardium. Am J Physiol Heart Circ Physiol. 2006;291:H2013–7.
Irlbeck M, Muhling O, Iwai T, Zimmer HG. Different response of the rat left and right heart to norepinephrine. Cardiovasc Res. 1996;31:157–62.
Michaels AD, Chatterjee K, De Marco T. Effects of intravenous nesiritide on pulmonary vascular hemodynamics in pulmonary hypertension. J Card Fail. 2005;11(6):425–31.
Piao L, Marsboom G, Archer SL. Mitochondrial metabolic adaptation in right ventricular hypertrophy and failure. J Mol Med. 2010;88(10):1011–20.
Drake JI, Bogaard HJ, Mizuno S, Clifton B, Xie B, Gao Y, Dumur CI, Fawcett P, Voelkel NF, Natarajan R. Molecular signature of a right heart failure program in chronic severe pulmonary hypertension. Am J Respir Cell Mol Biol. 2011;45(6):1239–47.
Klinger JR, Thaker S, Houtchens J, Preston IR, Hill NS, Farber HW. Pulmonary hemodynamic responses to brain natriuretic peptide and sildenafil in patients with pulmonary arterial hypertension. Chest. 2006;129(2):417–25.
Kirk JA, Cingolani OH. Thrombospondins in the transition from myocardial infarction to heart failure. J Mol Cell Cardiol. 2016;90:102–10.
Geva T, Powell AJ, Crawford EC, Chung T, Colan SD. Evaluation of regional differences in right ventricular systolic function by acoustic quantification echocardiography and cine magnetic resonance imaging. Circulation. 1998;98(4):339–45.
Rouleau JL, Paradis P, Shenasa H, Juneau C. Faster time to peak tension and velocity of shortening in right versus left ventricular trabeculae and papillary muscles of dogs. Circ Res. 1986;59(5):556–61.
Zak R. Cell proliferation during cardiac growth. Am J Cardiol. 1973;31(2):211–9.
Vanhoutte PM. Endothelium and control of vascular function. State of the art lecture. Hypertension. 1989;13(6 Pt 2):658–67.
Weber KT, Brilla CG. Pathological hypertrophy and cardiac interstitium. Fibrosis and renin-angiotensin-aldosterone system. Circulation. 1991;83(6):1849–65.
Weber KT, Sun Y, Bhattacharya SK, Ahokas RA, Gerling IC. Myofibroblast-mediated mechanisms of pathological remodelling of the heart. Nat Rev Cardiol. 2013;10(1):15–26.
Owens GK. Growth response of aortic smooth muscle cells in hypertension. In: Lee RMKW, editor. Blood vessel changes in hypertension: structure and function. Boca Raton: CRC Press; 1989. p. 45–63.42.
Weber KT, Clark WA, Janicki JS, Shroff SG. Physiologic versus pathologic hypertrophy and the pressure-overloaded myocardium. J Cardiovasc Pharmacol. 1987;10(Suppl 6):S37–50.
Olson EN. A decade of discoveries in cardiac biology. Nat Med. 2004;10(5):467–74.
MacLellan WR, Schneider MD. Genetic dissection of cardiac growth control pathways. Annu Rev Physiol. 2000;62:289–319.
Frey N, Katus HA, Olson EN, Hill JA. Hypertrophy of the heart: a new therapeutic target? Circulation. 2004;109(13):1580–9.
McMullen JR, Jennings GL. Differences between pathological and physiological cardiac hypertrophy: novel therapeutic strategies to treat heart failure. Clin Exp Pharmacol Physiol. 2007;34(4):255–62.
Li Z, Bing OH, Long X, Robinson KG, Lakatta EG. Increased cardiomyocyte apoptosis during the transition to heart failure in the spontaneously hypertensive rat. Am J Phys. 1997;272(5 Pt 2):H2313–9.
MacLellan WR, Schneider MD. Death by design. Programmed cell death in cardiovascular biology and disease. Circ Res. 1997;81(2):137–44.
Frangogiannis NG. Matricellular proteins in cardiac adaptation and disease. Physiol Rev. 2012;92(2):635–88.
Bornstein P. Diversity of function is inherent in matricellular proteins: an appraisal of thrombospondin 1. J Cell Biol. 1995;130(3):503–6.
Bradshaw AD. The role of secreted protein acidic and rich in cysteine (SPARC) in cardiac repair and fibrosis: does expression of SPARC by macrophages influence outcomes? J Mol Cell Cardiol. 2016;93:156–61.
Francis GS, McDonald KM. Left ventricular hypertrophy: an initial response to myocardial injury. Am J Cardiol. 1992;69(18):3G–7G. discussion 7G–9G
Sharma K, Kass DA. Heart failure with preserved ejection fraction: mechanisms, clinical features, and therapies. Circ Res. 2014;115(1):79–96.
Bittel DC, Butler MG, Kibiryeva N, Marshall JA, Chen J, Lofland GK, O’Brien JE Jr. Gene expression in cardiac tissues from infants with idiopathic conotruncal defects. BMC Med Genet. 2011;4(1). https://doi.org/10.1186/1755-8794-4-1.
Kaynak B, von Heydebreck A, Mebus S, Seelow D, Hennig S, Vogel J, Sperling HP, Pregla R, Alexi-Meskishvili V, Hetzer R, Lange PE, Vingron M, Lehrach H, Sperling S. Genome-wide array analysis of normal and malformed human hearts. Circulation. 2003;107(19):2467–74.
Wu Y, Feng W, Zhang H, Li S, Wang D, Pan X, Hu S. Ca2+-regulatory proteins in cardiomyocytes from the right ventricle in children with congenital heart disease. J Transl Med. 2012;10:67. https://doi.org/10.1186/1479-5876-10-67.
Tekin D, Dursun AD, Xi L. Hypoxia inducible factor 1 (HIF-1) and cardioprotection. Acta Pharmacol Sin. 2010;31(9):1085–94. https://doi.org/10.1038/aps.2010.132.
Jeewa A, Manickaraj AK, Mertens L, Manlhiot C, Kinnear C, Mondal T, Smythe J, Rosenberg H, Lougheed J, McCrindle BW, van Arsdell G, Redington AN, Mital S. Genetic determinants of right-ventricular remodeling after tetralogy of Fallot repair. Pediatr Res. 2012;72(4):407–13. https://doi.org/10.1038/pr.2012.95.
Lawler J, Duquette M, Whittaker CA, Adams JC, McHenry K, DeSimone DW. Identification and characterization of thrombospondin-4, a new member of the thrombospondin gene family. J Cell Biol. 1993;120(4):1059–67.
Lawler J, Hynes RO. The structure of human thrombospondin, an adhesive glycoprotein with multiple calcium-binding sites and homologies with several different proteins. J Cell Biol. 1986;103(5):1635–48.
Adams JC, Lawler J. The thrombospondins. Cold Spring Harb Perspect Biol. 2011;3(10):a009712.
Adams JC. Thrombospondins: multifunctional regulators of cell interactions. Annu Rev Cell Dev Biol. 2001;17:25–51.
Xia Y, Dobaczewski M, Gonzalez-Quesada C, Chen W, Biernacka A, Li N, Lee DW, Frangogiannis NG. Endogenous thrombospondin 1 protects the pressure-overloaded myocardium by modulating fibroblast phenotype and matrix metabolism. Hypertension. 2011;58(5):902–11.
Mustonen E, Aro J, Puhakka J, Ilves M, Soini Y, Leskinen H, Ruskoaho H, Rysä J. Thrombospondin-4 expression is rapidly upregulated by cardiac overload. Biochem Biophys Res Commun. 2008;373(2):186–91.
Melenovsky V, Benes J, Skaroupkova P, Sedmera D, Strnad H, Kolar M, Vlcek C, Petrak J, Benes J Jr, Papousek F, Oliyarnyk O, Kazdova L, Cervenka L. Metabolic characterization of volume overload heart failure due to aorto-caval fistula in rats. Mol Cell Biochem. 2011;354(1-2):83–96.
Swinnen M, Vanhoutte D, Van Almen GC, Hamdani N, Schellings MW, D'hooge J, Van der Velden J, Weaver MS, Sage EH, Bornstein P, Verheyen FK, VandenDriessche T, Chuah MK, Westermann D, Paulus WJ, Van de Werf F, Schroen B, Carmeliet P, Pinto YM, Heymans S. Absence of thrombospondin-2 causes age-related dilated cardiomyopathy. Circulation. 2009;120(16):1585–97.
Schroen B, Heymans S, Sharma U, Blankesteijn WM, Pokharel S, Cleutjens JP, Porter JG, Evelo CT, Duisters R, van Leeuwen RE, Janssen BJ, Debets JJ, Smits JF, Daemen MJ, Crijns HJ, Bornstein P, Pinto YM. Thrombospondin-2 is essential for myocardial matrix integrity: increased expression identifies failure-prone cardiac hypertrophy. Circ Res. 2004;95(5):515–22.
Toth A, Nickson P, Mandl A, Bannister ML, Toth K, Erhardt P. Endoplasmic reticulum stress as a novel therapeutic target in heart diseases. Cardiovasc Hematol Disord Drug Targets. 2007;7:205–18.
Groenendyk J, Sreenivasaiah PK, Kim DH, Agellon LB, Michalak M. Biology of endoplasmic reticulum stress in the heart. Circ Res. 2010;107(10):1185–97.
Frangogiannis NG, Ren G, Dewald O, Zymek P, Haudek S, Koerting A, Winkelmann K, Michael LH, Lawler J, Entman ML. Critical role of endogenous thrombospondin-1 in preventing expansion of healing myocardial infarcts. Circulation. 2005;111(22):2935–42.
Snider P, Standley KN, Wang J, Azhar M, Doetschman T, Conway SJ. Origin of cardiac fibroblasts and the role of periostin. Circ Res. 2009;105(10):934–47.
Krenning G, Zeisberg EM, Kalluri R. The origin of fibroblasts and mechanism of cardiac fibrosis. J Cell Physiol. 2010;225(3):631–7.
Souders CA, Bowers SL, Baudino TA. Cardiac fibroblast: the renaissance cell. Circ Res. 2009;105(12):1164–76.
Chilton L, Giles WR, Smith GL. Evidence of intercellular coupling between co-cultured adult rabbit ventricular myocytes and myofibroblasts. J Physiol. 2007;583(Pt 1):225–36.
Baudino TA, McFadden A, Fix C, Hastings J, Price R, Borg TK. Cell patterning: interaction of cardiac myocytes and fibroblasts in three-dimensional culture. Microsc Microanal. 2008;14(2):117–25.
Zannad F, Rossignol P, Iraqi W. Extracellular matrix fibrotic markers in heart failure. Heart Fail Rev. 2010;15(4):319–29.
Cleutjens JP, Kandala JC, Guarda E, Guntaka RV, Weber KT. Regulation of collagen degradation in the rat myocardium after infarction. J Mol Cell Cardiol. 1995;27(6):1281–92.
Segura AM, Frazier OH, Buja LM. Fibrosis and heart failure. Heart Fail Rev. 2014;19(2):173–85.
Olivetti G, Capasso JM, Sonnenblick EH, Anversa P. Side-to-side slippage of myocytes participates in ventricular wall remodeling acutely after myocardial infarction in rats. Circ Res. 1990;67(1):23–34.
Deb A, Ubil E. Cardiac fibroblast in development and wound healing. J Mol Cell Cardiol. 2014;70:47–55.
Spinale FG, Janicki JS, Zile MR. Membrane-associated matrix proteolysis and heart failure. Circ Res. 2013;112(1):195–208.
Tao G, Levay AK, Peacock JD, Huk DJ, Both SN, Purcell NH, Pinto JR, Galantowicz ML, Koch M, Lucchesi PA, Birk DE, Lincoln J. Collagen XIV is important for growth and structural integrity of the myocardium. J Mol Cell Cardiol. 2012;53(5):626–38.
Ricard-Blum S. The collagen family. Cold Spring Harb Perspect Biol. 2011;3(1):a004978.
Gil-Cayuela C, Rivera M, Ortega A, Tarazón E, Triviño JC, Lago F, González-Juanatey JR, Almenar L, Martínez-Dolz L, Portolés M. RNA sequencing analysis identifies new human collagen genes involved in cardiac remodeling. Am Coll Cardiol. 2015;65(12):1265–7.
López B, González A, Ravassa S, Beaumont J, Moreno MU, San José G, Querejeta R, Díez J. Circulating biomarkers of myocardial fibrosis: the need for a reappraisal. J Am Coll Cardiol. 2015;65(22):2449–56.
Leask A. Getting to the heart of the matter: new insights into cardiac fibrosis. Circ Res. 2015;116(7):1269–76.
Sun Y, Kiani MF, Postlethwaite AE, Weber KT. Infarct scar as living tissue. Basic Res Cardiol. 2002;97(5):343–7.
Zamilpa R, Lindsey ML. Extracellular matrix turnover and signaling during cardiac remodeling following MI: causes and consequences. J Mol Cell Cardiol. 2010;48(3):558–63.
Lindsey ML, Iyer RP, Jung M, DeLeon-Pennell KY, Ma Y. Matrix metalloproteinases as input and output signals for post-myocardial infarction remodeling. J Mol Cell Cardiol. 2016;91:134–40.
Booz GW, Baker KM. Molecular signalling mechanisms controlling growth and function of cardiac fibroblasts. Cardiovasc Res. 1995;30(4):537–43.
Gonzalez-Quesada C, Cavalera M, Biernacka A, Kong P, Lee DW, Saxena A, Frunza O, Dobaczewski M, Shinde A, Frangogiannis NG. Thrombospondin-1 induction in the diabetic myocardium stabilizes the cardiac matrix in addition to promoting vascular rarefaction through angiopoietin-2 upregulation. Circ Res. 2013;113(12):1331–44.
Ma Y, Yabluchanskiy A, Lindsey ML. Thrombospondin-1: the good, the bad, and the complicated. Circ Res. 2013;113(12):1272–4.
Bein K, Simons M. Thrombospondin type 1 repeats interact with matrix metalloproteinase 2. Regulation of metalloproteinase activity. J Biol Chem. 2000;275(41):32167–73.
Yang Z, Strickland DK, Bornstein P. Extracellular matrix metalloproteinase 2 levels are regulated by the low density lipoprotein-related scavenger receptor and thrombospondin 2. J Biol Chem. 2001;276(11):8403–8.
Hall MC, Young DA, Waters JG, Rowan AD, Chantry A, Edwards DR, Clark IM. The comparative role of activator protein 1 and Smad factors in the regulation of Timp-1 and MMP-1 gene expression by transforming growth factor-beta 1. J Biol Chem. 2003;278(12):10304–13.
Leung LL, Nachman RL. Complex formation of platelet thrombospondin with fibrinogen. J Clin Invest. 1982;70(3):542–9.
Mumby SM, Raugi GJ, Bornstein P. Interactions of thrombospondin with extracellular matrix proteins: selective binding to type V collagen. J Cell Biol. 1984;98(2):646–52.
Bale MD, Mosher DF. Effects of thrombospondin on fibrin polymerization and structure. J Biol Chem. 1986;261(2):862–8.
Narouz-Ott L, Maurer P, Nitsche DP, Smyth N, Paulsson M. Thrombospondin-4 binds specifically to both collagenous and non-collagenous extracellular matrix proteins via its C-terminal domains. J Biol Chem. 2000;275(47):37110–7.
Mustonen E, Ruskoaho H, Rysä J. Thrombospondin-4, tumour necrosis factor-like weak inducer of apoptosis (TWEAK) and its receptor Fn14: novel extracellular matrix modulating factors in cardiac remodelling. Ann Med. 2012;44(8):793–804.
Sawaki D, Hou L, Tomida S, Sun J, Zhan H, Aizawa K, Son BK, Kariya T, Takimoto E, Otsu K, Conway SJ, Manabe I, Komuro I, Friedman SL, Nagai R, Suzuki T. Modulation of cardiac fibrosis by Krüppel-like factor 6 through transcriptional control of thrombospondin 4 in cardiomyocytes. Cardiovasc Res. 2015;107(4):420–30.
Desmoulière A, Geinoz A, Gabbiani F, Gabbiani G. Transforming growth factor-beta 1 induces alpha-smooth muscle actin expression in granulation tissue myofibroblasts and in quiescent and growing cultured fibroblasts. J Cell Biol. 1993;122(1):103–11.
Ma Y, de Castro Brás LE, Toba H, Iyer RP, Hall ME, Winniford MD, Lange RA, Tyagi SC, Lindsey ML. Myofibroblasts and the extracellular matrix network in post-myocardial infarction cardiac remodeling. Pflugers Arch. 2014;466(6):1113–27.
Burchfield JS, Xie M, Hill JA. Pathological ventricular remodeling: mechanisms: part 1 of 2. Circulation. 2013;128(4):388–400.
Wang C, Wang X. The interplay between autophagy and the ubiquitin-proteasome system in cardiac proteotoxicity. Biochim Biophys Acta. 2015;1852(2):188–94.
Tarone G, Brancaccio M. Keep your heart in shape: molecular chaperone networks for treating heart disease. Cardiovasc Res. 2014;102(3):346–61.
James TN. Normal and abnormal consequences of apoptosis in the human heart. From postnatal morphogenesis to paroxysmal arrhythmias. Circulation. 1994;90(1):556–73.
Narula J, Haider N, Virmani R, DiSalvo TG, Kolodgie FD, Hajjar RJ, Schmidt U, Semigran MJ, Dec GW, Khaw BA. Apoptosis in myocytes in end-stage heart failure. N Engl J Med. 1996;335(16):1182–9.
Kostin S, Pool L, Elsässer A, Hein S, Drexler HC, Arnon E, Hayakawa Y, Zimmermann R, Bauer E, Klövekorn WP, Schaper J. Myocytes die by multiple mechanisms in failing human hearts. Circ Res. 2003;92(7):715–24.
Frangogiannis NG. Regulation of the inflammatory response in cardiac repair. Circ Res. 2012;110(1):159–73. https://doi.org/10.1161/CIRCRESAHA.111.243162.
Freude B, Masters TN, Robicsek F, Fokin A, Kostin S, Zimmermann R, Ullmann C, Lorenz-Meyer S, Schaper J. Apoptosis is initiated by myocardial ischemia and executed during reperfusion. J Mol Cell Cardiol. 2000;32(2):197–208.
Black SC, Huang JQ, Rezaiefar P, Radinovic S, Eberhart A, Nicholson DW, Rodger IW. Co-localization of the cysteine protease caspase-3 with apoptotic myocytes after in vivo myocardial ischemia and reperfusion in the rat. J Mol Cell Cardiol. 1998;30(4):733–42.
Dorn GW. Apoptotic and non-apoptotic programmed cardiomyocyte death in ventricular remodelling. Cardiovasc Res. 2009;81(3):465–73. https://doi.org/10.1093/cvr/cvn243.
Maruyama R, Takemura G, Aoyama T, Hayakawa K, Koda M, Kawase Y, Qiu X, Ohno Y, Minatoguchi S, Miyata K, Fujiwara T, Fujiwara H. Dynamic process of apoptosis in adult rat cardiomyocytes analyzed using 48-hour videomicroscopy and electron microscopy: beating and rate are associated with the apoptotic process. Am J Pathol. 2001;159(2):683–91.
Diwan A, Krenz M, Syed FM, Wansapura J, Ren X, Koesters AG, Li H, Kirshenbaum LA, Hahn HS, Robbins J, Jones WK, Dorn GW. Inhibition of ischemic cardiomyocyte apoptosis through targeted ablation of Bnip3 restrains postinfarction remodeling in mice. J Clin Invest. 2007;117(10):2825–33.
Whelan RS, Mani K, Kitsis RN. Nipping at cardiac remodeling. J Clin Invest. 2007;117(10):2751–3.
Dawson DW, Volpert OV, Pearce SF, Schneider AJ, Silverstein RL, Henkin J, Bouck NP. Three distinct D-amino acid substitutions confer potent antiangiogenic activity on an inactive peptide derived from a thrombospondin-1 type 1 repeat. Mol Pharmacol. 1999;55(2):332–8.
Dawson DW, Pearce SF, Zhong R, Silverstein RL, Frazier WA, Bouck NP. CD36 mediates the In vitro inhibitory effects of thrombospondin-1 on endothelial cells. J Cell Biol. 1997;138(3):707–17.
Asch AS, Silbiger S, Heimer E, Nachman RL. Thrombospondin sequence motif (CSVTCG) is responsible for CD36 binding. Biochem Biophys Res Commun. 1992;182(3):1208–17.
Jiménez B, Volpert OV, Reiher F, Chang L, Muñoz A, Karin M, Bouck N. c-Jun N-terminal kinase activation is required for the inhibition of neovascularization by thrombospondin-1. Oncogene. 2001;20(26):3443–8.
Jiménez B, Volpert OV, Crawford SE, Febbraio M, Silverstein RL, Bouck N. Signals leading to apoptosis-dependent inhibition of neovascularization by thrombospondin-1. Nat Med. 2000;6(1):41–8.
Simantov R, Febbraio M, Silverstein RL. The antiangiogenic effect of thrombospondin-2 is mediated by CD36 and modulated by histidine-rich glycoprotein. Matrix Biol. 2005;24(1):27–34.
Yee KO, Connolly CM, Duquette M, Kazerounian S, Washington R, Lawler J. The effect of thrombospondin-1 on breast cancer metastasis. Breast Cancer Res Treat. 2009;114(1):85–96.
Primo L, Ferrandi C, Roca C, Marchiò S, di Blasio L, Alessio M, Bussolino F. Identification of CD36 molecular features required for its in vitro angiostatic activity. FASEB J. 2005;19(12):1713–5.
Volpert OV, Zaichuk T, Zhou W, Reiher F, Ferguson TA, Stuart PM, Amin M, Bouck NP. Inducer-stimulated Fas targets activated endothelium for destruction by anti-angiogenic thrombospondin-1 and pigment epithelium-derived factor. Nat Med. 2002;8(4):349–57.
Zhang P, Shen M, Fernandez-Patron C, Kassiri Z. ADAMs family and relatives in cardiovascular physiology and pathology. J Mol Cell Cardiol. 2016;93:186–99.
Reilly MP, Li M, He J, Ferguson JF, Stylianou IM, Mehta NN, Burnett MS, Devaney JM, Knouff CW, Thompson JR, Horne BD, Stewart AF, Assimes TL, Wild PS, Allayee H, Nitschke PL, Patel RS, Martinelli N, Girelli D, Quyyumi AA, Anderson JL, Erdmann J, Hall AS, Schunkert H, Quertermous T, Blankenberg S, Hazen SL, Roberts R, Kathiresan S, Samani NJ, Epstein SE, Rader DJ, Myocardial Infarction Genetics Consortium; Wellcome Trust Case Control Consortium. Identification of ADAMTS7 as a novel locus for coronary atherosclerosis and association of ABO with myocardial infarction in the presence of coronary atherosclerosis: two genome-wide association studies. Lancet. 2011;377(9763):383–92.
Wang L, Zheng J, Bai X, Liu B, Liu CJ, Xu Q, Zhu Y, Wang N, Kong W, Wang X. ADAMTS-7 mediates vascular smooth muscle cell migration and neointima formation in balloon-injured rat arteries. Circ Res. 2009;104(5):688–98.
Kessler T, Zhang L, Liu Z, Yin X, Huang Y, Wang Y, Fu Y, Mayr M, Ge Q, Xu Q, Zhu Y, Wang X, Schmidt K, de Wit C, Erdmann J, Schunkert H, Aherrahrou Z, Kong W. ADAMTS-7 inhibits re-endothelialization of injured arteries and promotes vascular remodeling through cleavage of thrombospondin-1. Circulation. 2015;131(13):1191–201.
Iruela-Arispe ML. Regulation of thrombospondin1 by extracellular proteases. Curr Drug Targets. 2008;9(10):863–8.
Arndt V, Dick N, Tawo R, Dreiseidler M, Wenzel D, Hesse M, Fürst DO, Saftig P, Saint R, Fleischmann BK, Hoch M, Höhfeld J. Chaperone-assisted selective autophagy is essential for muscle maintenance. Curr Biol. 2010;20(2):143–8.
Carra S, Seguin SJ, Landry J. HspB8 and Bag3: a new chaperone complex targeting misfolded proteins to macroautophagy. Autophagy. 2008;4(2):237–9.
Babu-Narayan SV, Kilner PJ, Li W, Moon JC, Goktekin O, Davlouros PA, Khan M, Ho SY, Pennell DJ, Gatzoulis MA. Ventricular fibrosis suggested by cardiovascular magnetic resonance in adults with repaired tetralogy of fallot and its relationship to adverse markers of clinical outcome. Circulation. 2006;113(3):405–13.
Weidemann F, Herrmann S, Störk S, Niemann M, Frantz S, Lange V, Beer M, Gattenlöhner S, Voelker W, Ertl G, Strotmann JM. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation. 2009;120(7):577–84. https://doi.org/10.1161/CIRCULATIONAHA.108.847772.
Hein S, Arnon E, Kostin S, Schönburg M, Elsässer A, Polyakova V, Bauer EP, Klövekorn WP, Schaper J. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003;107(7):984–91.
Jellis C, Martin J, Narula J, Marwick TH. Assessment of nonischemic myocardial fibrosis. J Am Coll Cardiol. 2010;56(2):89–97. https://doi.org/10.1016/j.jacc.2010.02.047.
Kong P, Christia P, Frangogiannis NG. The pathogenesis of cardiac fibrosis. Cell Mol Life Sci. 2014;71(4):549–74. https://doi.org/10.1007/s00018-013-1349-6.
Li AH, Liu PP, Villarreal FJ, Garcia RA. Dynamic changes in myocardial matrix and relevance to disease: translational perspectives. Circ Res. 2014;114(5):916–27. https://doi.org/10.1161/CIRCRESAHA.114.302819.
Weber KT, Pick R, Jalil JE, Janicki JS, Carroll EP. Patterns of myocardial fibrosis. J Mol Cell Cardiol. 1989;21(Suppl 5):121–31.
Gyöngyösi M, Winkler J, Ramos I, Do QT, Firat H, McDonald K, González A, Thum T, Díez J, Jaisser F, Pizard A, Zannad F. Myocardial fibrosis: biomedical research from bench to bedside. Eur J Heart Fail. 2017;19(2):177–91. https://doi.org/10.1002/ejhf.696.
Heymans S, González A, Pizard A, Papageorgiou AP, López-Andrés N, Jaisser F, Thum T, Zannad F, Díez J. Searching for new mechanisms of myocardial fibrosis with diagnostic and/or therapeutic potential. Eur J Heart Fail. 2015;17(8):764–71. https://doi.org/10.1002/ejhf.312.
Camelliti P, Borg TK, Kohl P. Structural and functional characterisation of cardiac fibroblasts. Cardiovasc Res. 2005;65(1):40–51.
Lajiness JD, Conway SJ. Origin, development, and differentiation of cardiac fibroblasts. J Mol Cell Cardiol. 2014;70:2–8. https://doi.org/10.1016/j.yjmcc.2013.11.003.
Watson CJ, Phelan D, Collier P, Horgan S, Glezeva N, Cooke G, Xu M, Ledwidge M, McDonald K, Baugh JA. Extracellular matrix sub-types and mechanical stretch impact human cardiac fibroblast responses to transforming growth factor beta. Connect Tissue Res. 2014;55(3):248–56. https://doi.org/10.3109/03008207.2014.904856.
Brilla CG, Maisch B, Zhou G, Weber KT. Hormonal regulation of cardiac fibroblast function. Eur Heart J. 1995;16(Suppl C):45–50.
Schellings MW, Pinto YM, Heymans S. Matricellular proteins in the heart: possible role during stress and remodeling. Cardiovasc Res. 2004;64(1):24–31.
Kumarswamy R, Thum T. Non-coding RNAs in cardiac remodeling and heart failure. Circ Res. 2013;113(6):676–89. https://doi.org/10.1161/CIRCRESAHA.113.300226.
Robins SP. Biochemistry and functional significance of collagen cross-linking. Biochem Soc Trans. 2007;35(Pt 5):849–52.
Shoulders MD, Raines RT. Collagen structure and stability. Annu Rev Biochem. 2009;78:929–58. https://doi.org/10.1146/annurev.biochem.77.032207.120833.
López B, Querejeta R, González A, Larman M, Díez J. Collagen cross-linking but not collagen amount associates with elevated filling pressures in hypertensive patients with stage C heart failure: potential role of lysyl oxidase. Hypertension. 2012;60(3):677–83. https://doi.org/10.1161/HYPERTENSIONAHA.112.196113.
Kawara T, Derksen R, de Groot JR, Coronel R, Tasseron S, Linnenbank AC, Hauer RN, Kirkels H, Janse MJ, de Bakker JM. Activation delay after premature stimulation in chronically diseased human myocardium relates to the architecture of interstitial fibrosis. Circulation. 2001;104(25):3069–75.
Anderson KP, Walker R, Urie P, Ershler PR, Lux RL, Karwandee SV. Myocardial electrical propagation in patients with idiopathic dilated cardiomyopathy. J Clin Invest. 1993;92(1):122–40.
Schwartzkopff B, Brehm M, Mundhenke M, Strauer BE. Repair of coronary arterioles after treatment with perindopril in hypertensive heart disease. Hypertension. 2000;36(2):220–5.
Wald RM, Haber I, Wald R, Valente AM, Powell AJ, Geva T. Effects of regional dysfunction and late gadolinium enhancement on global right ventricular function and exercise capacity in patients with repaired tetralogy of Fallot. Circulation. 2009;119(10):1370–7. https://doi.org/10.1161/CIRCULATIONAHA.108.816546.
van Oorschot JW, Gho JM, van Hout GP, Froeling M, Hoefer IE, Doevendans PA, Luijten PR, Chamuleau SA, Zwanenburg JJ, Jansen Of Lorkeers SJ. Endogenous contrast MRI of cardiac fibrosis: beyond late gadolinium enhancement. J Magn Reson Imaging. 2015;41(5):1181–9. https://doi.org/10.1002/jmri.24715.
Sado DM, Flett AS, Moon JC. Novel imaging techniques for diffuse myocardial fibrosis. Futur Cardiol. 2011;7(5):643–50. https://doi.org/10.2217/fca.11.45.
Gyöngyösi M, Blanco J, Marian T, Trón L, Petneházy O, Petrasi Z, Hemetsberger R, Rodriguez J, Font G, Pavo IJ, Kertész I, Balkay L, Pavo N, Posa A, Emri M, Galuska L, Kraitchman DL, Wojta J, Huber K, Glogar D. Serial noninvasive in vivo positron emission tomographic tracking of percutaneously intramyocardially injected autologous porcine mesenchymal stem cells modified for transgene reporter gene expression. Circ Cardiovasc Imaging. 2008;1(2):94–103. https://doi.org/10.1161/CIRCIMAGING.108.797449.
Rischpler C, Nekolla SG, Dregely I, Schwaiger M. Hybrid PET/MR imaging of the heart: potential, initial experiences, and future prospects. J Nucl Med. 2013;54(3):402–15. https://doi.org/10.2967/jnumed.112.105353.
Li XG, Roivainen A, Bergman J, Heinonen A, Bengel F, Thum T, Knuuti J. Enabling [(18)F]-bicyclo[6.1.0]nonyne for oligonucleotide conjugation for positron emission tomography applications: [(18)F]-anti-microRNA-21 as an example. Chem Commun. 2015;51(48):9821–4. https://doi.org/10.1039/c5cc02618k.
Fang L, Ellims AH, Moore XL, White DA, Taylor AJ, Chin-Dusting J, Dart AM. Circulating microRNAs as biomarkers for diffuse myocardial fibrosis in patients with hypertrophic cardiomyopathy. J Transl Med. 2015;13:314. https://doi.org/10.1186/s12967-015-0672-0.
Azevedo CF, Nigri M, Higuchi ML, Pomerantzeff PM, Spina GS, Sampaio RO, Tarasoutchi F, Grinberg M, Rochitte CE. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol. 2010;56(4):278–87. https://doi.org/10.1016/j.jacc.2009.12.074.
Aoki T, Fukumoto Y, Sugimura K, Oikawa M, Satoh K, Nakano M, Nakayama M, Shimokawa H. Prognostic impact of myocardial interstitial fibrosis in non-ischemic heart failure -comparison between preserved and reduced ejection fraction heart failure. Circ J. 2011;75(11):2605–13.
van Rooij E, Sutherland LB, Liu N, Williams AH, McAnally J, Gerard RD, Richardson JA, Olson EN. A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc Natl Acad Sci U S A. 2006;103(48):18255–60.
Ikeda S, Kong SW, Lu J, Bisping E, Zhang H, Allen PD, Golub TR, Pieske B, Pu WT. Altered microRNA expression in human heart disease. Physiol Genomics. 2007;31(3):367–73.
Thum T, Galuppo P, Wolf C, Fiedler J, Kneitz S, van Laake LW, Doevendans PA, Mummery CL, Borlak J, Haverich A, Gross C, Engelhardt S, Ertl G, Bauersachs J. MicroRNAs in the human heart: a clue to fetal gene reprogramming in heart failure. Circulation. 2007;116(3):258–67.
Small EM, Olson EN. Pervasive roles of microRNAs in cardiovascular biology. Nature. 2011;469(7330):336–42. https://doi.org/10.1038/nature09783.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97.
Li D, Ji L, Liu L, Liu Y, Hou H, Yu K, Sun Q, Zhao Z. Characterization of circulating microRNA expression in patients with a ventricular septal defect. PLoS One. 2014;9(8):e106318. https://doi.org/10.1371/journal.pone.0106318.
Lai CT, Ng EK, Chow PC, Kwong A, Cheung YF. Circulating microRNA expression profile and systemic right ventricular function in adults after atrial switch operation for complete transposition of the great arteries. BMC Cardiovasc Disord. 2013;13:73. https://doi.org/10.1186/1471-2261-13-73.
Tutarel O, Dangwal S, Bretthauer J, Westhoff-Bleck M, Roentgen P, Anker SD, Bauersachs J, Thum T. Circulating miR-423_5p fails as a biomarker for systemic ventricular function in adults after atrial repair for transposition of the great arteries. Int J Cardiol. 2013;167(1):63–6. https://doi.org/10.1016/j.ijcard.2011.11.082.
Zhang J, Chang JJ, Xu F, Ma XJ, Wu Y, Li WC, Wang HJ, Huang GY, Ma D. MicroRNA deregulation in right ventricular outflow tract myocardium in nonsyndromic tetralogy of fallot. Can J Cardiol. 2013;29(12):1695–703. https://doi.org/10.1016/j.cjca.2013.07.002.
Bittel DC, Kibiryeva N, Marshall JA, O’Brien JE. MicroRNA-421 dysregulation is associated with tetralogy of Fallot. Cells. 2014;3(3):713–23. https://doi.org/10.3390/cells3030713.
Tamura T, Said S, Harris J, Lu W, Gerdes AM. Reverse remodeling of cardiac myocyte hypertrophy in hypertension and failure by targeting of the renin-angiotensin system. Circulation. 2000;102(2):253–9.
van Rooij E, Sutherland LB, Qi X, Richardson JA, Hill J, Olson EN. Control of stress-dependent cardiac growth and gene expression by a microRNA. Science. 2007;316(5824):575–9.
Liu N, Bezprozvannaya S, Williams AH, Qi X, Richardson JA, Bassel-Duby R, Olson EN. microRNA-133a regulates cardiomyocyte proliferation and suppresses smooth muscle gene expression in the heart. Genes Dev. 2008;22(23):3242–54. https://doi.org/10.1101/gad.1738708.
Apitz C, Honjo O, Humpl T, Li J, Assad RS, Cho MY, Hong J, Friedberg MK, Redington AN. Biventricular structural and functional responses to aortic constriction in a rabbit model of chronic right ventricular pressure overload. J Thorac Cardiovasc Surg. 2012;144(6):1494–501. https://doi.org/10.1016/j.jtcvs.2012.06.027.
Unverferth DV, Fetters JK, Unverferth BJ, Leier CV, Magorien RD, Arn AR, Baker PB. Human myocardial histologic characteristics in congestive heart failure. Circulation. 1983;68(6):1194–200.
Montgomery RL, Hullinger TG, Semus HM, Dickinson BA, Seto AG, Lynch JM, Stack C, Latimer PA, Olson EN, van Rooij E. Therapeutic inhibition of miR-208a improves cardiac function and survival during heart failure. Circulation. 2011;124:1537–47.
Hwang MW, Matsumori A, Furukawa Y, Ono K, Okada M, Iwasaki A, Hara M, Miyamoto T, Touma M, Sasayama S. Neutralization of interleukin-1beta in the acute phase of myocardial infarction promotes the progression of left ventricular remodeling. J Am Coll Cardiol. 2001;38(5):1546–53.
Maekawa Y, Anzai T, Yoshikawa T, Asakura Y, Takahashi T, Ishikawa S, Mitamura H, Ogawa S. Prognostic significance of peripheral monocytosis after reperfused acute myocardial infarction:a possible role for left ventricular remodeling. J Am Coll Cardiol. 2002;39(2):241–6.
Hafizi S, Wharton J, Chester AH, Yacoub MH. Profibrotic effects of endothelin-1 via the ETA receptor in cultured human cardiac fibroblasts. Cell Physiol Biochem. 2004;14(4-6):285–92.
Katwa LC. Cardiac myofibroblasts isolated from the site of myocardial infarction express endothelin de novo. Am J Physiol Heart Circ Physiol. 2003;285(3):H1132–9.
Hsieh PC, Davis ME, Lisowski LK, Lee RT. Endothelial-cardiomyocyte interactions in cardiac development and repair. Annu Rev Physiol. 2006;68:51–66.
Rich S, McLaughlin VV. Endothelin receptor blockers in cardiovascular disease. Circulation. 2003;108:2184–90.
Zolk O, Quattek J, Sitzler G, Schrader T, Nickenig G, et al. Expression of endothelin-1, endothelin-converting enzyme, and endothelin receptors in chronic heart failure. Circulation. 1999;99:2118–23.
Leask A. Potential therapeutic targets for cardiac fibrosis: TGFbeta, angiotensin, endothelin, CCN2, and PDGF, partners in fibroblast activation. Circ Res. 2010;106(11):1675–80. https://doi.org/10.1161/CIRCRESAHA.110.217737.
Sütsch G, Kiowski W, Yan XW, Hunziker P, Christen S, Strobel W, Kim JH, Rickenbacher P, Bertel O. Short-term oral endothelin-receptor antagonist therapy in conventionally treated patients with symptomatic severe chronic heart failure. Circulation. 1998;98(21):2262–8.
Thomson A. Interleukins. In: Oppenheim JJ, editor. The cytokine handbook. 3rd ed. San Diego: Academic; 1998. p. 146–62.
Henry G, Garner WL. Inflammatory mediators in wound healing. Surg Clin North Am. 2003;83(3):483–507.
Pietilä K, Hermens WT, Harmoinen A, Baardman T, Pasternack A, Topol EJ, Simoons ML. Comparison of peak serum C-reactive protein and hydroxybutyrate dehydrogenase levels in patients with acute myocardial infarction treated with alteplase and streptokinase. Am J Cardiol. 1997;80(8):1075–7.
Furman MI, Becker RC, Yarzebski J, Savegeau J, Gore JM, Goldberg RJ. Effect of elevated leukocyte count on in-hospital mortality following acute myocardial infarction. Am J Cardiol. 1996;78(8):945–8.
Jordan JE, Zhao ZQ, Vinten-Johansen J. The role of neutrophils in myocardial ischemia-reperfusion injury. Cardiovasc Res. 1999;43(4):860–78.
Engler RL. Free radical and granulocyte-mediated injury during myocardial ischemia and reperfusion. Am J Cardiol. 1989;63(10):19E–23E.
Lasky LA. Selectins: interpreters of cell-specific carbohydrate information during inflammation. Science. 1992;258(5084):964–9.
Ebnet K, Vestweber D. Molecular mechanisms that control leukocyte extravasation: the selectins and the chemokines. Histochem Cell Biol. 1999;112(1):1–23.
Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res. 2002;53(1):31–47.
Lefer DJ, Granger DN. Oxidative stress and cardiac disease. Am J Med. 2000;109(4):315–23.
Dhalla NS, Elmoselhi AB, Hata T, Makino N. Status of myocardial antioxidants in ischemia-reperfusion injury. Cardiovasc Res. 2000;47(3):446–56.
Hausenloy DJ, Yellon DM. The therapeutic potential of ischemic conditioning: an update. Nat Rev Cardiol. 2011;8(11):619–29.
Foo RS, Mani K, Kitsis RN. Death begets failure in the heart. J Clin Invest. 2005;115(3):565–71.
Filomeni G, Ciriolo MR. Redox control of apoptosis: an update. Antioxid Redox Signal. 2006;8(11-12):2187–92.
Matsuzawa A, Ichijo H. Stress-responsive protein kinases in redox-regulated apoptosis signaling. Antioxid Redox Signal. 2005;7(3-4):472–81.
Giordano FJ. Oxygen, oxidative stress, hypoxia, and heart failure. J Clin Invest. 2005;115(3):500–8.
Cave AC, Brewer AC, Narayanapanicker A, Ray R, Grieve DJ, Walker S, Shah AM. NADPH oxidases in cardiovascular health and disease. Antioxid Redox Signal. 2006;8(5-6):691–728.
Heymes C, Bendall JK, Ratajczak P, Cave AC, Samuel JL, Hasenfuss G, Shah AM. Increased myocardial NADPH oxidase activity in human heart failure. J Am Coll Cardiol. 2003;41(12):2164–71.
Griendling KK, Sorescu D, Lassegue B, Ushio-Fukai M. Modulation of protein kinase activity and gene expression by reactive oxygen species and their role in vascular physiology and pathophysiology. Arterioscler Thromb Vasc Biol. 2000;20(10):2175–83.
Ushio-Fukai M, Zafari AM, Fukui T, Ishizaka N, Griendling KK. p22phox is a critical component of the superoxide-generating NADH/NADPH oxidase system and regulates angiotensin II-induced hypertrophy in vascular smooth muscle cells. J Biol Chem. 1996;271(38):23317–21.
Görlach A, Brandes RP, Nguyen K, Amidi M, Dehghani F, Busse R. A gp91phox containing NADPH oxidase selectively expressed in endothelial cells is a major source of oxygen radical generation in the arterial wall. Circ Res. 2000;87(1):26–32.
Jones SA, O'Donnell VB, Wood JD, Broughton JP, Hughes EJ, Jones OT. Expression of phagocyte NADPH oxidase components in human endothelial cells. Am J Phys. 1996;271(4 Pt 2):H1626–34.
Chamseddine AH, Miller FJ Jr. Gp91phox contributes to NADPH oxidase activity in aortic fibroblasts but not smooth muscle cells. Am J Physiol Heart Circ Physiol. 2003;285(6):H2284–9.
Wenzel S, Taimor G, Piper HM, Schlüter KD. Redox-sensitive intermediates mediate angiotensin II-induced p38 MAP kinase activation, AP-1 binding activity, and TGF-beta expression in adult ventricular cardiomyocytes. FASEB J. 2001;15(12):2291–3.
Lambeth JD. NOX enzymes and the biology of reactive oxygen. Nat Rev Immunol. 2004;4(3):181–9.
Aguirre J, Lambeth JD. Nox enzymes from fungus to fly to fish and what they tell us about Nox function in mammals. Free Radic Biol Med. 2010;49(9):1342–53.
Brandes RP, Weissmann N, Schröder K. NADPH oxidases in cardiovascular disease. Free Radic Biol Med. 2010;49(5):687–706.
Geiszt M. NADPH oxidases: new kids on the block. Cardiovasc Res. 2006;71(2):289–99.
Kayama Y, Raaz U, Jagger A, Adam M, Schellinger IN, Sakamoto M, Suzuki H, Toyama K, Spin JM, Tsao PS. Diabetic cardiovascular disease induced by oxidative stress. Int J Mol Sci. 2015;16(10):25234–63. https://doi.org/10.3390/ijms161025234.
Lassègue B, San Martín A, Griendling KK. Biochemistry, physiology, and pathophysiology of NADPH oxidases in the cardiovascular system. Circ Res. 2012;110(10):1364–90. https://doi.org/10.1161/CIRCRESAHA.111.243972.
Erickson JR, Joiner ML, Guan X, Kutschke W, Yang J, Oddis CV, Bartlett RK, Lowe JS, O'Donnell SE, Aykin-Burns N, Zimmerman MC, Zimmerman K, Ham AJ, Weiss RM, Spitz DR, Shea MA, Colbran RJ, Mohler PJ, Anderson ME. A dynamic pathway for calcium-independent activation of CaMKII by methionine oxidation. Cell. 2008;133(3):462–74. https://doi.org/10.1016/j.cell.2008.02.048.
Gilleron M, Marechal X, Montaigne D, Franczak J, Neviere R, Lancel S. NADPH oxidases participate to doxorubicin-induced cardiac myocyte apoptosis. Biochem Biophys Res Commun. 2009;388(4):727–31. https://doi.org/10.1016/j.bbrc.2009.08.085.
Hayashi H, Kobara M, Abe M, Tanaka N, Gouda E, Toba H, Yamada H, Tatsumi T, Nakata T, Matsubara H. Aldosterone nongenomically produces NADPH oxidase-dependent reactive oxygen species and induces myocyte apoptosis. Hypertens Res. 2008;31(2):363–75. https://doi.org/10.1291/hypres.31.363.
Li Y, Arnold JM, Pampillo M, Babwah AV, Peng T. Taurine prevents cardiomyocyte death by inhibiting NADPH oxidase-mediated calpain activation. Free Radic Biol Med. 2009;46(1):51–61. https://doi.org/10.1016/j.freeradbiomed.2008.09.025.
Murdoch CE, Zhang M, Cave AC, Shah AM. NADPH oxidase-dependent redox signalling in cardiac hypertrophy, remodelling and failure. Cardiovasc Res. 2006;71(2):208–15.
Akki A, Zhang M, Murdoch C, Brewer A, Shah AM. NADPH oxidase signaling and cardiac myocyte function. J Mol Cell Cardiol. 2009;47(1):15–22.
Lu J, Mitra S, Wang X, Khaidakov M, Mehta JL. Oxidative stress and lectin-like ox-LDL-receptor LOX-1 in atherogenesis and tumorigenesis. Antioxid Redox Signal. 2011;15(8):2301–33. https://doi.org/10.1089/ars.2010.3792.
Zhang M, Perino A, Ghigo A, Hirsch E, Shah AM. NADPH oxidases in heart failure: poachers or gamekeepers? Antioxid Redox Signal. 2013;18(9):1024–41. https://doi.org/10.1016/j.yjmcc.2009.04.004.
Misra MK, Sarwat M, Bhakuni P, Tuteja R, Tuteja N. Oxidative stress and ischemic myocardial syndromes. Med Sci Monit. 2009;15(10):RA209–19.
Qipshidze N, Tyagi N, Metreveli N, Lominadze D, Tyagi SC. Autophagy mechanism of right ventricular remodeling in murine model of pulmonary artery constriction. Am J Physiol Heart Circ Physiol. 2012;302(3):H688–96. https://doi.org/10.1152/ajpheart.00777.2011.
Borchi E, Bargelli V, Stillitano F, Giordano C, Sebastiani M, Nassi PA, d'Amati G, Cerbai E, Nediani C. Enhanced ROS production by NADPH oxidase is correlated to changes in antioxidant enzyme activity in human heart failure. Biochim Biophys Acta. 2010;1802(3):331–8.
Robbins CS, Swirski FK. The multiple roles of monocyte subsets in steady state and inflammation. Cell Mol Life Sci. 2010;67(16):2685–93. https://doi.org/10.1007/s00018-010-0375-x.
Tsujioka H, Imanishi T, Ikejima H, Kuroi A, Takarada S, Tanimoto T, Kitabata H, Okochi K, Arita Y, Ishibashi K, Komukai K, Kataiwa H, Nakamura N, Hirata K, Tanaka A, Akasaka T. Impact of heterogeneity of human peripheral blood monocyte subsets on myocardial salvage in patients with primary acute myocardial infarction. J Am Coll Cardiol. 2009;54(2):130–8. https://doi.org/10.1016/j.jacc.2009.04.021.
Arslan F, Smeets MB, O’Neill LA, Keogh B, McGuirk P, Timmers L, Tersteeg C, Hoefer IE, Doevendans PA, Pasterkamp G, de Kleijn DP. Myocardial ischemia/reperfusion injury is mediated by leukocytic toll-like receptor-2 and reduced by systemic administration of a novel anti-toll-like receptor-2 antibody. Circulation. 2010;121(1):80–90. https://doi.org/10.1161/CIRCULATIONAHA.109.880187.
Mann DL. The emerging role of innate immunity in the heart and vascular system: for whom the cell tolls. Circ Res. 2011;108(9):1133–45. https://doi.org/10.1161/CIRCRESAHA.110.226936.
Andrassy M, Volz HC, Igwe JC, Funke B, Eichberger SN, Kaya Z, Buss S, Autschbach F, Pleger ST, Lukic IK, Bea F, Hardt SE, Humpert PM, Bianchi ME, Mairbäurl H, Nawroth PP, Remppis A, Katus HA, Bierhaus A. High-mobility group box-1 in ischemia-reperfusion injury of the heart. Circulation. 2008;117(25):3216–26. https://doi.org/10.1161/CIRCULATIONAHA.108.769331.
Gordon JW, Shaw JA, Kirshenbaum LA. Multiple facets of NF-κB in the heart: to be or not to NF-κB. Circ Res. 2011;108(9):1122–32. https://doi.org/10.1161/CIRCRESAHA.110.226928.
Bujak M, Dobaczewski M, Chatila K, Mendoza LH, Li N, Reddy A, Frangogiannis NG. Interleukin-1 receptor type I signaling critically regulates infarct healing and cardiac remodeling. Am J Pathol. 2008;173(1):57–67. https://doi.org/10.2353/ajpath.2008.070974.
Schroder K, Tschopp J. The inflammasomes. Cell. 2010;140(6):821–32. https://doi.org/10.1016/j.cell.2010.01.040.
Kawaguchi M, Takahashi M, Hata T, Kashima Y, Usui F, Morimoto H, Izawa A, Takahashi Y, Masumoto J, Koyama J, Hongo M, Noda T, Nakayama J, Sagara J, Taniguchi S, Ikeda U. Inflammasome activation of cardiac fibroblasts is essential for myocardial ischemia/reperfusion injury. Circulation. 2011;123(6):594–604. https://doi.org/10.1161/CIRCULATIONAHA.110.982777.
Frangogiannis NG. Chemokines in ischemia and reperfusion. Thromb Haemost. 2007;97(5):738–47.
Colotta F, Re F, Polentarutti N, Sozzani S, Mantovani A. Modulation of granulocyte survival and programmed cell death by cytokines and bacterial products. Blood. 1992;80(8):2012–20.
Dewald O, Ren G, Duerr GD, Zoerlein M, Klemm C, Gersch C, Tincey S, Michael LH, Entman ML, Frangogiannis NG. Of mice and dogs: species-specific differences in the inflammatory response following myocardial infarction. Am J Pathol. 2004;164(2):665–77.
Rumberger JA. Ventricular dilatation and remodeling after myocardial infarction. Mayo Clin Proc. 1994;69(7):664–74.
Aikawa Y, Rohde L, Plehn J, Greaves SC, Menapace F, Arnold MO, Rouleau JL, Pfeffer MA, Lee RT, Solomon SD. Regional wall stress predicts ventricular remodeling after anteroseptal myocardial infarction in the Healing and Early Afterload Reducing Trial (HEART): an echocardiography-based structural analysis. Am Heart J. 2001;141(2):234–42.
Norton GR, Woodiwiss AJ, Gaasch WH, Mela T, Chung ES, Aurigemma GP, Meyer TE. Heart failure in pressure overload hypertrophy. The relative roles of ventricular remodeling and myocardial dysfunction. J Am Coll Cardiol. 2002;39(4):664–71.
Richards AM, Nicholls MG, Troughton RW, Lainchbury JG, Elliott J, Frampton C, Espiner EA, Crozier IG, Yandle TG, Turner J. Antecedent hypertension and heart failure after myocardial infarction. J Am Coll Cardiol. 2002;39(7):1182–8.
Cingolani OH, Kirk JA, Seo K, Koitabashi N, Lee DI, Ramirez-Correa G, Bedja D, Barth AS, Moens AL, Kass DA. Thrombospondin-4 is required for stretch-mediated contractility augmentation in cardiac muscle. Circ Res. 2011;109(12):1410–4.
Sayer G, Bhat G. The renin-angiotensin-aldosterone system and heart failure. Cardiol Clin. 2014;32(1):21–32. vii
Albuquerque FN, Brandão AA, Silva DA, Mourilhe-Rocha R, Duque GS, Gondar AF, Neves LM, Bittencourt MI, Pozzan R, Albuquerque DC. Angiotensin-converting enzyme genetic polymorphism: its impact on cardiac remodeling. Arq Bras Cardiol. 2014;102(1):70–9.
Florea VG, Cohn JN. The autonomic nervous system and heart failure. Circ Res. 2014;114(11):1815–26.
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon AB, Rector T. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984;311(13):819–23.
Vantrimpont P, Rouleau JL, Ciampi A, Harel F, de Champlain J, Bichet D, Moyé LA, Pfeffer M. Two-year time course and significance of neurohumoral activation in the Survival and Ventricular Enlargement (SAVE) study. Eur Heart J. 1998;19(10):1552–63.
Lee WH, Packer M. Prognostic importance of serum sodium concentration and its modification by converting-enzyme inhibition in patients with severe chronic heart failure. Circulation. 1986;73(2):257–67.
Packer M. The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol. 1992;20(1):248–54.
Maeda K, Tsutamoto T, Wada A, Mabuchi N, Hayashi M, Tsutsui T, Ohnishi M, Sawaki M, Fujii M, Matsumoto T, Kinoshita M. High levels of plasma brain natriuretic peptide and interleukin-6 after optimized treatment for heart failure are independent risk factors for morbidity and mortality in patients with congestive heart failure. J Am Coll Cardiol. 2000;36(5):1587–93.
Tamura N, Ogawa Y, Chusho H, Nakamura K, Nakao K, Suda M, Kasahara M, Hashimoto R, Katsuura G, Mukoyama M, Itoh H, Saito Y, Tanaka I, Otani H, Katsuki M. Cardiac fibrosis in mice lacking brain natriuretic peptide. Proc Natl Acad Sci U S A. 2000;97(8):4239–44.
Yamamoto R, Akazawa H, Fujihara H, Ozasa Y, Yasuda N, Ito K, Kudo Y, Qin Y, Ueta Y, Komuro I. Angiotensin II type 1 receptor signaling regulates feeding behavior through anorexigenic corticotropin-releasing hormone in hypothalamus. J Biol Chem. 2011;286(24):21458–65.
Akazawa H, Yasuda N, Komuro I. Mechanisms and functions of agonist-independent activation in the angiotensin II type 1 receptor. Mol Cell Endocrinol. 2009;302(2):140–7.
Kamo T, Akazawa H, Komuro I. Pleiotropic effects of angiotensin II receptor signaling in cardiovascular homeostasis and aging. Int Heart J. 2015;56(3):249–54.
Ozasa Y, Akazawa H, Qin Y, Tateno K, Ito K, Kudo-Sakamoto Y, Yano M, Yabumoto C, Naito AT, Oka T, Lee JK, Minamino T, Nagai T, Kobayashi Y, Komuro I. Notch activation mediates angiotensin II-induced vascular remodeling by promoting the proliferation and migration of vascular smooth muscle cells. Hypertens Res. 2013;36(10):859–65.
Akazawa H, Yano M, Yabumoto C, Kudo-Sakamoto Y, Komuro I. Angiotensin II type 1 and type 2 receptor-induced cell signaling. Curr Pharm Des. 2013;19(17):2988–95.
Sato M. Roles of accessory proteins for heterotrimeric G-protein in the development of cardiovascular diseases. Circ J. 2013;77(10):2455–61.
Wu J, You J, Wang S, Zhang L, Gong H, Zou Y. Insights into the activation and inhibition of angiotensin II type 1 receptor in the mechanically loaded heart. Circ J. 2014;78(6):1283–9.
Sadoshima J, Xu Y, Slayter HS, Izumo S. Autocrine release of angiotensin II mediates stretch-induced hypertrophy of cardiac myocytes in vitro. Cell. 1993;75(5):977–84.
Yamazaki T, Komuro I, Kudoh S, Zou Y, Shiojima I, Mizuno T, Takano H, Hiroi Y, Ueki K, Tobe K, et al. Angiotensin II partly mediates mechanical stress-induced cardiac hypertrophy. Circ Res. 1995;77(2):258–65.
Akazawa H. Mechanisms of cardiovascular homeostasis and pathophysiology--from gene expression, signal transduction to cellular communication. Circ J. 2015;79(12):2529–36.
Yasuda N, Miura S, Akazawa H, Tanaka T, Qin Y, Kiya Y, Imaizumi S, Fujino M, Ito K, Zou Y, Fukuhara S, Kunimoto S, Fukuzaki K, Sato T, Ge J, Mochizuki N, Nakaya H, Saku K, Komuro I. Conformational switch of angiotensin II type 1 receptor underlying mechanical stress-induced activation. EMBO Rep. 2008;9(2):179–86.
Konstam MA, Rousseau MF, Kronenberg MW, Udelson JE, Melin J, Stewart D, Dolan N, Edens TR, Ahn S, Kinan D, et al. Effects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dysfunction in patients with heart failure. SOLVD Investigators. Circulation. 1992;86(2):431–8.
Greenberg B, Quinones MA, Koilpillai C, Limacher M, Shindler D, Benedict C, Shelton B. Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation. 1995;91(10):2573–81.
Hafizi S, Wharton J, Morgan K, Allen SP, Chester AH, Catravas JD, Polak JM, Yacoub MH. Expression of functional angiotensin-converting enzyme and AT1 receptors in cultured human cardiac fibroblasts. Circulation. 1998;98(23):2553–9.
Matsusaka T, Katori H, Inagami T, Fogo A, Ichikawa I. Communication between myocytes and fibroblasts in cardiac remodeling in angiotensin chimeric mice. J Clin Invest. 1999;103(10):1451–8.
Sadoshima J, Izumo S. Molecular characterization of angiotensin II--induced hypertrophy of cardiac myocytes and hyperplasia of cardiac fibroblasts. Critical role of the AT1 receptor subtype. Circ Res. 1993;73(3):413–23.
McEwan PE, Gray GA, Sherry L, Webb DJ, Kenyon CJ. Differential effects of angiotensin II on cardiac cell proliferation and intramyocardial perivascular fibrosis in vivo. Circulation. 1998;98(24):2765–73.
Kawano H, Do YS, Kawano Y, Starnes V, Barr M, Law RE, Hsueh WA. Angiotensin II has multiple profibrotic effects in human cardiac fibroblasts. Circulation. 2000;101(10):1130–7.
Hayashi M, Tsutamoto T, Wada A, Maeda K, Mabuchi N, Tsutsui T, Matsui T, Fujii M, Matsumoto T, Yamamoto T, Horie H, Ohnishi M, Kinoshita M. Relationship between transcardiac extraction of aldosterone and left ventricular remodeling in patients with first acute myocardial infarction: extracting aldosterone through the heart promotes ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol. 2001;38(5):1375–82.
Lijnen P, Petrov V. Induction of cardiac fibrosis by aldosterone. J Mol Cell Cardiol. 2000;32(6):865–79.
Fullerton MJ, Funder JW. Aldosterone and cardiac fibrosis: in vitro studies. Cardiovasc Res. 1994;28(12):1863–7.
Zannad F, Alla F, Dousset B, Perez A, Pitt B. Limitation of excessive extracellular matrix turnover may contribute to survival benefit of spironolactone therapy in patients with congestive heart failure: insights from the randomized aldactone evaluation study (RALES). Rales Investigators. Circulation. 2000;102(22):2700–6.
Altin SE, Schulze PC. Metabolism of the right ventricle and the response to hypertrophy and failure. Prog Cardiovasc Dis. 2012;55(2):229–33. https://doi.org/10.1016/j.pcad.2012.07.010.
Dias CA, Assad RS, Caneo LF, Abduch MC, Aiello VD, Dias AR, Marcial MB, Oliveira SA. Reversible pulmonary trunk banding. II. An experimental model for rapid pulmonary ventricular hypertrophy. J Thorac Cardiovasc Surg. 2002;124(5):999–1006.
Taegtmeyer H, Golfman L, Sharma S, Razeghi P, van Arsdall M. Linking gene expression to function: metabolic flexibility in the normal and diseased heart. Ann N Y Acad Sci. 2004;1015:202–13.
Doenst T, Nguyen TD, Abel ED. Cardiac metabolism in heart failure: implications beyond ATP production. Circ Res. 2013;113(6):709–24.
Barger PM, Kelly DP. PPAR signaling in the control of cardiac energy metabolism. Trends Cardiovasc Med. 2000;10(6):238–45.
Karbowska J, Kochan Z, Smolenski RT. Peroxisome proliferator-activated receptor alpha is downregulated in the failing human heart. Cell Mol Biol Lett. 2003;8(1):49–53.
Campos DH, Leopoldo AS, Lima-Leopoldo AP, Nascimento AF, Oliveira SA Jr, Silva DC, Sugizaki MM, Padovani CR, Cicogna AC. Obesity preserves myocardial function during blockade of the glycolytic pathway. Arq Bras Cardiol. 2014;103(4):330–7.
Azevedo PS, Minicucci MF, Santos PP, Paiva SA, Zornoff LA. Energy metabolism in cardiac remodeling and heart failure. Cardiol Rev. 2013;21(3):135–40.
Santos PP, Oliveira F, Ferreira VC, Polegato BF, Roscani MG, Fernandes AA, Modesto P, Rafacho BP, Zanati SG, Di Lorenzo A, Matsubara LS, Paiva SA, Zornoff LA, Minicucci MF, Azevedo PS. The role of lipotoxicity in smoke cardiomyopathy. PLoS One. 2014;9(12):e113739.
Voelkel NF, Quaife RA, Leinwand LA, et al. Right ventricular function and failure: report of a National Heart, Lung and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114(17):1883–91. https://doi.org/10.1161/CIRCULATIONAHA.106.632208.
Nagaya N, Goto Y, Satoh T, et al. Impaired regional fatty acid uptake and systolic dysfunction in hypertrophied right ventricle. J Nucl Med. 1998;39:1676–80.
Bokhari S, Raina A, Rosenweig EB, et al. PET imaging may provide a novel biomarker and understanding of right ventricular dysfunction in patients with idiopathic pulmonary arterial hypertension. Circ Cardiovasc Imaging. 2011;4:641–7. https://doi.org/10.1161/CIRCIMAGING.110.963207.
Can MM, Kaymaz C, Tanboga IH, et al. Increased right ventricular glucose metabolism in patients with pulmonary arterial hypertension. Clin Nucl Med. 2011;36:743–8. https://doi.org/10.1097/RLU.0b013e3182177389.
O’Connor RD, Xu J, Ewald GA, et al. Intramyocardial triglyceride quantification by magnetic resonance spectroscopy: in vivo and ex vivo correlation in human subjects. Magn Reson Med. 2011;65:1234–8. https://doi.org/10.1002/mrm.22734.
Ryan JJ, Archer SL. The right ventricle in pulmonary arterial hypertension: disorders of metabolism, angiogenesis and adrenergic signaling in right ventricular failure. Circ Res. 2014;115:176–88. https://doi.org/10.1161/CIRCRESAHA.113.301129.
Sutendra G, Dromparis P, Paulin R, et al. A metabolic remodeling in right ventricular hypertrophy is associated with decreased angiogenesis and a transition from a compensated to a decompensated state in pulmonary hypertension. J Mol Med. 2013;91(11):1315–27. https://doi.org/10.1007/s00109-013-1059-4.
Wasson S, Reddy HK, Dohrmann ML. Current perspectives of electrical remodeling and its therapeutic implications. J Cardiovasc Pharmacol Ther. 2004;9(2):129–44.
Hasenfuss G, Schillinger W, Lehnart SE, et al. Relationship between Na+-Ca2+-exchanger protein levels and diastolic function of failing human myocardium. Circulation. 1999;99(5):641–8.
Bers DM, Pogwizd SM, Schlotthauer K. Upregulated Na/Ca exchange is involved in both contractile dysfunction and arrhythmogenesis in heart failure. Basic Res Cardiol. 2002;97(Suppl 1):I36–42.
Wang Z, Nolan B, Kutschke W, Hill JA. Na+-Ca2+ exchanger remodeling in pressure overload cardiac hypertrophy. J Biol Chem. 2001;276(21):17706–11.
Houser SR, Freeman AR, Jaegar JM, et al. Resting potential changes associated with Na+-K+ pump in failing heart muscle. Am J Phys. 1981;240(2):H168–76.
Matsumoto Y, Aihara H, Yamauchi-Kohno R, et al. Long-term endothelin a receptor blockade inhibits electrical remodeling in cardiomyopathic hamsters. Circulation. 2002;106(5):613–9.
Sipido KR, Volders PG, de Groot SH, et al. Enhanced Ca2+ release and Na+/Ca2+ exchange activity in hypertrophied canine ventricular myocytes: potential link between contractile adaptation and arrhythmogenesis. Circulation. 2000;102(17):2137–44.
Kalogeropoulos AP, Georgiopoulou VV, Howell S, Pernetz MA, Fisher MR, Lerakis S, Martin RP. Evaluation of right intraventricular dyssynchrony by two-dimensional strain echocardiography in patients with pulmonary arterial hypertension. J Am Soc Echocardiogr. 2008;21(9):1028–34. https://doi.org/10.1016/j.echo.2008.05.005.
López-Candales A, Dohi K, Rajagopalan N, Suffoletto M, Murali S, Gorcsan J, Edelman K. Right ventricular dyssynchrony in patients with pulmonary hypertension is associated with disease severity and functional class. Cardiovasc Ultrasound. 2005;3:23.
Vonk-Noordegraaf A, Marcus JT, Gan CT, Boonstra A, Postmus PE. Interventricular mechanical asynchrony due to right ventricular pressure overload in pulmonary hypertension plays an important role in impaired left ventricular filling. Chest. 2005;128(6 Suppl):628S–30S.
Feneley MP, Gavaghan TP, Baron DW, Branson JA, Roy PR, Morgan JJ. Contribution of left ventricular contraction to the generation of right ventricular systolic pressure in the human heart. Circulation. 1985;71(3):473–80.
Marcus JT, Gan CT, Zwanenburg JJ, Boonstra A,Allaart CP, Götte MJ, Vonk-Noordegraaf A.Interventricular mechanical asynchrony in pulmonary arterial hypertension: left-to-right delay in peak shortening is related to right ventricular overload and left ventricular underfilling. J Am Coll Cardiol. 2008;51(7):750–7. https://doi.org/10.1016/j.jacc.2007.10.041.
Peschar M, Vermooy K, Vangat WYR, et al. Absence of reeverse electrical remodeling during regression of volume overload hypertrophy in canine ventricles. Cardiovasc Res. 2003;58(3):510–7.
Mayet J, Shahi M, McGrath K, Poulter NR, Sever PS, Foale RA, et al. Left ventricular hypertrophy and QT dispersion in hypertension. Hypertension. 1996;28(5):791–6.
Darbar D, Cherry CJ, Kerins DM. QT dispersion is reduced after valve replacement in patients with aortic stenosis. Heart. 1999;82(1):15–8.
Reddy HK, Wasson S, Koshy SK, et al. Structural correlates of electrical remodeling in ventricular hypertrophy. Cardiovasc Res. 2003;58(3):495–7.
Pries AR, Badimon L, Bugiardini R, Camici PG, Dorobantu M, Duncker DJ, Escaned J, Koller A, Piek JJ, de Wit C. Coronary vascular regulation, remodelling, and collateralization: mechanisms and clinical implications on behalf of the working group on coronary pathophysiology and microcirculation. Eur Heart J. 2015;36(45):3134–46. https://doi.org/10.1093/eurheartj/ehv100.
Laughlin MH, Bowles DK, Duncker DJ. The coronary circulation in exercise training. Am J Physiol Heart Circ Physiol. 2012;302(1):H10–23. https://doi.org/10.1152/ajpheart.00574.2011.
Schaper W. Collateral circulation: past and present. Basic Res Cardiol. 2009;104(1):5–21. https://doi.org/10.1007/s00395-008-0760-x.
Pries AR, Reglin B, Secomb TW. Remodeling of blood vessels: responses of diameter and wall thickness to hemodynamic and metabolic stimuli. Hypertension. 2005;46(4):725–31.
Mulvany MJ. Small artery remodelling in hypertension. Basic Clin Pharmacol Toxicol. 2012;110(1):49–55. https://doi.org/10.1111/j.1742-7843.2011.00758.x.
Zakrzewicz A, Secomb TW, Pries AR. Angioadaptation: keeping the vascular system in shape. News Physiol Sci. 2002;17:197–201.
Koller A. Flow-dependent remodeling of small arteries: the stimuli and the sensors are (still) in question. Circ Res. 2006;99(1):6–9.
Pries AR, Reglin B, Secomb TW. Structural adaptation of microvascular networks: functional roles of adaptive responses. Am J Physiol Heart Circ Physiol. 2001;281(3):H1015–25.
Hopkins WE, Ochoa LL, Richardson GW, et al. Comparison of the hemodynamics and survival of adults with severe primary pulmonary hypertension or Eisenmenger syndrome. J Heart Lung Transplant. 1996;15(1 Pt 1):100–5.
Reis Filho JR, Cardoso JN, Cardoso CM, Pereira-Barretto AC. Reverse cardiac remodeling: a marker of better prognosis in heart failure. Arq Bras Cardiol. 2015;104(6):502–6. https://doi.org/10.5935/abc.20150025.
Hellawell JL, Margulies KB. Myocardial reverse remodeling. Cardiovasc Ther. 2012;30(3):172–81. https://doi.org/10.1111/j.1755-5922.2010.00247.x.
Kramer DG, Trikalinos TA, Kent DM, Antonopoulos GV, Konstam MA, Udelson JE. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction: a meta-analytic approach. J Am Coll Cardiol. 2010;56(5):392–406. https://doi.org/10.1016/j.jacc.2010.05.011.
Ruiz-Ortega M, Lorenzo O, Ruperez M, Konig S, Wittig B, Egido J. Angiotensin II activates nuclear transcription factor kappa B through AT(1) and AT(2) in vascular smooth muscle cells: molecular mechanisms. Circ Res. 2000;86(12):1266–72.
Marui N, Offermann MK, Swerlick R, Kunsch C, Rosen CA, Ahmad M, Alexander RW, Medford RM. Vascular cell adhesion molecule-1 (VCAM-1) gene transcription and expression are regulated through an antioxidant-sensitive mechanism in human vascular endothelial cells. J Clin Invest. 1993;92(4):1866–74.
Pi XJ, Chen X. Captopril and ramiprilat protect against free radical injury in isolated working rat hearts. J Mol Cell Cardiol. 1989;21(12):1261–71.
Chen F, Castranova V, Shi X, Demers LM. New insights into the role of nuclear factor kappa B, a ubiquitous transcription factor in the initiation of diseases. Clin Chem. 1999;45(1):7–17.
Santi D, Giannetta E, Isidori AM, Vitale C, Aversa A, Simoni M. Therapy of endocrine disease: effects of chronic use of phosphodiesterase inhibitors on endothelial markers in type 2 diabetes mellitus: a meta-analysis. Eur J Endocrinol. 2015;172(3):R103–14. https://doi.org/10.1530/EJE-14-0700.
Pofi R, Gianfrilli D, Badagliacca R, Di Dato C, Venneri MA, Giannetta E. Everything you ever wanted to know about phosphodiesterase 5 inhibitors and the heart (but never dared ask): how do they work? J Endocrinol Investig. 2016;39(2):131–42. https://doi.org/10.1007/s40618-015-0339-y.
Nam YJ, Song K, Olson EN. Heart repair by cardiac reprogramming. Nat Med. 2013;19(4):413–5. https://doi.org/10.1038/nm.3147.
Hodgkinson CP, Kang MH, Dal-Pra S, Mirotsou M, Dzau VJ. MicroRNAs and cardiac regeneration. Circ Res. 2015;116(10):1700–11. https://doi.org/10.1161/CIRCRESAHA.116.304377.
Jayawardena TM, Egemnazarov B, Finch EA, Zhang L, Payne JA, Pandya K, Zhang Z, Rosenberg P, Mirotsou M, Dzau VJ. MicroRNA-mediated in vitro and in vivo direct reprogramming of cardiac fibroblasts to cardiomyocytes. Circ Res. 2012;110(11):1465–73. https://doi.org/10.1161/CIRCRESAHA.112.269035.
Rao PK, Kumar RM, Farkhondeh M, Baskerville S, Lodish HF. Myogenic factors that regulate expression of muscle-specific microRNAs. Proc Natl Acad Sci U S A. 2006;103(23):8721–6.
Takaya T, Nishi H, Horie T, Ono K, Hasegawa K. Roles of microRNAs and myocardial cell differentiation. Prog Mol Biol Transl Sci. 2012;111:139–52. https://doi.org/10.1016/B978-0-12-398459-3.00006-X.
Joladarashi D, Thandavarayan RA, Babu SS, Krishnamurthy P. Small engine, big power: microRNAs as regulators of cardiac diseases and regeneration. Int J Mol Sci. 2014;15(9):15891–911. https://doi.org/10.3390/ijms150915891.
Katz MG, Fargnoli AS, Pritchette LA, Bridges CR. Gene delivery technologies for cardiac applications. Gene Ther. 2012;19(6):659–69. https://doi.org/10.1038/gt.2012.11.
Küçüker SA, Stetson SJ, Becker KA, Akgül A, Loebe M, Lafuente JA, Noon GP, Koerner MM, Entman ML, Torre-Amione G. Evidence of improved right ventricular structure after LVAD support in patients with end-stage cardiomyopathy. J Heart Lung Transplant. 2004;23(1):28–35.
Sachse FB, Torres NS, Savio-Galimberti E, Aiba T, Kass DA, Tomaselli GF, Bridge JH. Subcellular structures and function of myocytes impaired during heart failure are restored by cardiac resynchronization therapy. Circ Res. 2012;110(4):588-97. Circ Res. 2012;110(4):588–97. https://doi.org/10.1161/CIRCRESAHA.111.257428.
Barbone A, Holmes JW, Heerdt PM, et al. Comparison of right and left ventricular responses to left ventricular assist device support in patients with severe heart failure: a primary role of mechanical unloading underlying reverse remodeling. Circulation. 2001;104(6):670–5.
Klotz S, Naka Y, Oz MC, Burkhoff D. Biventricular assist device-induced right ventricular reverse structural and functional remodeling. J Heart Lung Transplant. 2005;24(9):1195–201.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Bontaş, E., Radu-Ioniţă, F., Munteanu, A., Mocanu, I. (2018). Basic Aspects of Cardiac Remodelling. In: Dumitrescu, S., Ţintoiu, I., Underwood, M. (eds) Right Heart Pathology. Springer, Cham. https://doi.org/10.1007/978-3-319-73764-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-73764-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-73763-8
Online ISBN: 978-3-319-73764-5
eBook Packages: MedicineMedicine (R0)