Abstract
This chapter describes the clinical approach and dialytic management of neonatal hyperammonemia. Newborns with hyperammonemia typically present as a metabolic emergency between the ages of 24 and 48 h. Early management including glucose infusion, protein restriction, and pharmacologic intervention with nitrogen scavengers is important to limit neurological damage. Dialysis is required to urgently remove ammonia if pharmacologic intervention is insufficient to remove the ammonia load, with high-dose continuous venovenous hemodiafiltration (CVVHDF) the modality of choice in most cases. Intermittent hemodialysis may be required initially in the presence of severe hyperammonemia to rapidly reduce ammonia levels, followed by CVVHDF to prevent ammonia rebound. The severity of the neurological outcome appears to be related to the duration of severe hyperammonemia and not to peak ammonia levels.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Neonatal hyperammonemia
- Urea cycle disorders
- Hemodialysis
- Continuous venovenous hemodiafiltration
- Nitrogen scavengers
- Metabolic emergency
Case Presentation
A newborn female presented at 36 h of life with a poor suck. She was born to first-degree consanguineous parents at 38 weeks gestation following a normal pregnancy and normal vaginal delivery, with a birth weight of 3,260 g. Apgar scores were 9 at 1 and 5 min. On examination, she was noted to be quiet. Her temperature was 34.6 °C. She was noted to be tachypneic and grunting, with a respiratory rate of 60 breaths per minute. Pulses were palpable with a capillary refill time of 3 s. Cardiac and respiratory examination was unremarkable. The anterior fontanelle was normal. The liver was palpable 2 cm below the right subcostal margin, but there was no splenomegaly. Oxygen saturation was 100% on hood box. As the maternal high vaginal swab had heavy growth of Group B Streptococcus, she was initially investigated for sepsis and started on empiric intravenous crystalline penicillin and gentamicin after blood cultures were taken. A complete blood count showed a total white count of 20.3 × 109/L with neutrophilia. Hemoglobin was 24.5 g/dL with a hematocrit of 65.8% and a platelet count of 433 × 109/L. C-reactive protein was <20 mg/L. A lumbar puncture was performed and showed normal cerebrospinal fluid cell counts and biochemistry. Chest X-ray was normal.
At 45 h of life, her condition deteriorated. She was noted to be frothing from the mouth, with a depressed sensorium and reacting only to pain. Her muscle tone was increased, with an incomplete Moro response. Her pupils were 2 mm bilaterally and equally reactive to light. An arterial blood gas on FiO2 of 30% showed the presence of respiratory alkalosis, with pH of 7.563, pCO2 of 22 mmHg, pO2 of 62 mmHg, and a standard bicarbonate level of 20 mmol/L. Blood glucose was 4.3 mmol/L (77.4 mg/dL). She subsequently (48 h of life) developed an episode of apnea with oxygen desaturation down to 70%, associated with facial twitching. She was immediately intubated and ventilated, and intravenous phenobarbitone (25 mg/kg) was administered to control the seizures. The serum ammonia level was high at 881 umol/L (1,234 ug/dL), with a venous blood lactate of 2.6 mmol/L (23.4 mg/dL). A diagnosis of hyperammonemia secondary to a presumed urea cycle defect was made, and she was transferred to the pediatric intensive care unit for further management at 52 h of life. She was hydrated with intravenous 10% dextrose solution and intravenous sodium benzoate, and arginine chloride (sodium phenylacetate was not available) therapy was initiated. In addition, pediatric nephrology was consulted for acute hemodialysis.
A double-lumen 6.5 French catheter was inserted into the patient’s right femoral vein. Hemodialysis was commenced 2 h after transfer using a 0.4 m2 polysulfone dialyzer (Hemoflow F3, Fresenius, Homburg, Germany) and neonatal lines with blood priming of the circuit which had a total priming volume of 72 mL (~27% of patient’s blood volume). The initial blood flow rate was 30 mL/min, and the dialysate flow rate was 500 mL/min, with a dialysate bath containing bicarbonate 35 mmol/L, potassium 2 mmol/L, and calcium 1.75 mmol/L. Heparin anticoagulation was used, maintaining the activated clotting time between 150 and 200 s. Intravenous 20% mannitol, 1 g/kg, was infused over the first hour of dialysis. Her blood ammonia at the time of dialysis initiation had increased to 2,091 umol/L (2,928 ug/dL), and her general condition was noted to have worsened, as she was not responding to pain. Her fontanelle was full and her pupils were fixed at 3 mm. During the dialysis procedure, her blood pressure remained stable ranging from 80/60 to 95/70 mmHg. After 4 h of dialysis, her blood ammonia had decreased to 1,853 umol/L (2,596 ug/dL). At this point, the dialyzer clotted and hemodialysis was discontinued. As the patient’s neurological status remained poor as reflected by flaccid tone and fixed/dilated pupils, her parents opted not to continue with dialysis, and the patient died 12 h later. Postmortem liver biopsy enzyme analysis confirmed complete carbamoyl phosphate synthetase I deficiency.
Clinical Questions
-
1.
What are the causes of neonatal hyperammonemia?
-
2.
What is the recommended approach to the diagnostic assessment of a neonate with hyperammonemia?
-
3.
What is the recommended initial clinical management of the neonate with hyperammonemia?
-
4.
What is the dialytic modality of choice for the neonate with hyperammonemia?
-
5.
What are the outcomes of dialytic therapy in neonatal hyperammonemia?
Diagnostic Discussion
-
1.
Neonatal hyperammonemia is a clinical condition characterized by marked elevation of the serum ammonia level resulting in neurologic abnormalit ies including drowsiness, poor feeding, vomiting, hypotonia, posturing, seizures, and coma [1, 2]. It can result in cerebral edema with severe damage to the developing brain leading to cognitive impairment, epilepsy, cerebral palsy, and even death, if left untreated. The international prevalence of neonatal hyperammonemia ranges from 1:8,000 to 1:44,000 live births [3].
The causes of neonatal hyperammonemia include urea cycle defects, organic acidemias, fatty acid oxidation defects, disorders of pyruvate metabolism, hyperammonemia-hyperornithinemia-hypocitrullinemia, lysinuric protein intolerance, carbonic anhydrase VA deficiency, hyperinsulinism-hyperammonemia, transient hyperammonemia of the newborn, severe dehydration, and liver failure. Urea cycle disorder s are due to a deficiency of enzymes that convert nitrogen to urea for excretion, and these include carbamoyl phosphate synthetase I deficiency, ornithine transcarbamylase deficiency, argininosuccinate synthetase deficiency (type I citrullinemia) and argininosuccinate lyase deficiency (argininosuccinic aciduria), N-acetyl glutamate synthetase deficiency, and arginase deficiency (argininemia).
-
2.
Newborn infants with hyperammonemia typically appear well initially but present between 24 and 48 h after birth with drowsiness, poor suck, hypothermia, and tachypnea, following the introduction of dietary protein intake in the form of milk feeds. A major differential diagnosis is sepsis, and this should be promptly evaluated and excluded. In this setting, metabolic emergencies must always be considered in the absence of risk factors or evidence of sepsis, and the patient evaluation should include measurement of arterial pH and pCO2, serum bicarbonate, glucose, ammonia, electrolytes, lactate, amino acids, and urine organic acids and orotic acid [3]. The concomitant presence of a high anion gap metabolic acidosis with hyperlactatemia, ketosis, and hypoglycemia suggests organic acidemias, defects of pyruvate metabolism, or liver disease; the presence of respiratory alkalosis and a normal lactate suggests urea cycle disorders such as hyperammonemia-hyperornithinemia-hypocitrullinemia, lysinuric protein intolerance, or transient hyperammonemia of the newborn; the presence of mixed metabolic acidosis and respiratory alkalosis and hypoglycemia suggests fatty acid oxidation defects (with hypoketosis) and carbonic anhydrase VA deficiency (with ketosis). Concomitant elevation of liver enzymes suggests the presence of liver failure. Further diagnostic evaluation such as tissue enzyme activity assays or DNA sequencing, in conjunction with array comparative genomic hybridization, is required to establish the specific enzyme deficiency.
-
3.
The severity and duration of hyperammonemia in the neonate significantly correlate with the subsequent degree of neurological damage and cognitive impairment. Early intervention may improve survival [4]. Initial management should include the provision of glucose at 10 mg/kg/min in order to minimize protein catabolism [3]. Close patient monitoring is important to avoid fluid overload which may worsen any preexistent cerebral edema. Intubation and assisted ventilation should be performed if the patient’s respiratory status deteriorates so as to minimize the work of breathing, thus reducing caloric demands and nitrogen catabolism. Protein intake should be stopped for at least 24–48 h and until there is initial patient stabilization; thereafter, it can be restarted at 1.5–1.75 g/kg per day with intravenous amino acids to prevent protein catabolism and with close monitoring of the serum ammonia level at least every 3 h.
Prompt removal of ammonia is imperative in order to limit the severity of the neurological dysfunction. Ammonia is removed by pharmacologic interventions and dialysis. In urea cycle disorders , a combination of sodium phenylacetate and sodium benzoate at a dose of 250 mg/kg, each diluted in 25–35 mL 10% dextrose and infused over 90 min, is used as nitrogen scavenger s [5]. The conjugation products, phenylacetylglutamine and hippurate, are water soluble and are excreted in the urine; hence, there must be adequate renal function for these compounds to be removed to avoid toxicity [6].
Except in the case of congenital arginase deficiency, the presence of arginine deficiency associated with a urea cycle disorder results in a catabolic state; therefore, intravenous arginine hydrochloride (200 mg/kg) is added to the infusion empirically, and the maintenance dose is subsequently adjusted once a definitive diagnosis of the enzyme deficiency is identified.
Dialysis should be started in the neonate with hyperammonemia when the serum ammonia level is greater than 500 umol/L (700 ug/dL) and at lower levels between 350 and 400 umol/L (490–560 ug/dL) if the response to medical management after 4 h is inadequate [3, 7].
-
4.
Extracorporeal dialysis is the modality of choice for removal of ammonia, as diffusion of ammonium occurs readily across synthetic dialysis membranes [2]. Diffusion of ammonia is slower across the peritoneal membrane resulting in lower ammonium clearances with peritoneal dialysis. Intermittent hemodialysis (IHD) using blood flow rates of 10–12 mL/kg per minute and a dialysate flow rate of 500 mL/min is an efficient modality for removal of small molecules compared to conventional continuous venovenous hemodiafiltration (CVVHDF) at a clearance of 2 L/h per 1.73m2 [2]. By removing amino acids such as citrulline, glycine, and glutamine, IHD also enhances the efficiency of nitrogen removal. However, CVVHDF, which utilizes both diffusive and convective transport, is preferred in the hemodynamically unstable neonate in whom low systemic blood pressure and the use of drugs such as arginine that causes vasodilatation through nitric oxide release preclude the higher blood flow rates required for IHD [8]. In addition, although IHD can rapidly reduce very high serum ammonium levels with the potential for resultant improved neurological outcomes, the procedure is unfortunately associated with a high risk of ammonia rebound [2]. This occurs because of ongoing catabolism, especially if there is accompanying infection, and also as a result of a delay in the effect of the pharmacologic nitrogen scavenger s which may take up to 48 h to reverse the catabolic process. In turn, continuing with CVVHDF after the initial IHD may be useful to keep the ammonia levels stable during this period of potential rebound. Moreover, CVVHDF provides the advantage of being able to maintain a normal electrolyte profile in terms of potassium and phosphate in the metabolically unstable infant. To improve the efficacy of CVVHDF in clearing ammonia, a high-dose prescription consisting of a blood flow rate of 10 ml/kg/min and a dialysate flow rate ranging from 3 to 5 L/h may be used [2].
Extracorporeal membrane oxygenation (ECMO ) together with HD has high blood flow rates of 170–200 mL/min, and has been used in some centers to rapidly reduce markedly elevated ammonia levels [9]. However, this modality is associated with higher morbidity as it requires surgical vascular access and may not be necessary with the advent of the combined modalities of IHD and high-dose CVVHDF.
Although peritoneal dialysis is not the modality of choice for the dialytic treatment of neonatal hyperammonemia, it is easier to perform in sick neonates compared to the extracorporeal techniques and may be initiated earlier while awaiting transport to a specialized center for extracorporeal dialysis. Even in centers where extracorporeal dialysis is available, significant therapy downtime secondary to technical issues related to the ability of the HD catheter to attain adequate blood flow rates and circuit clotting can negate the advantages of higher ammonia clearance by these modalities [10, 11]. Moreover, peritoneal dialysis can provide additional benefits in terms of an intraperitoneal glucose load to minimize catabolism, as well as removal of albumin and amino acids to achieve a negative nitrogen balance, thus reducing the ammonia load [11]. If peritoneal dialysis is the only modality available, the dialysis prescription should, in turn, be optimized to include 1.5% glucose dialysis solution with a fill volume of 40–50 mL/kg and hourly cycles for greater than 48 h in order to remove the ammonia load. Of course, it should be noted that peritoneal dialysis in neonates can be fraught with technical problems as well, such as poor catheter function, dialysate leakage, and infection, all of which could have a negative impact on ammonia management.
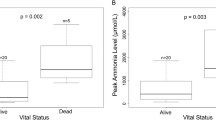
Based on the principles noted above, in the presence of severe hyperammonemia with a serum ammonia concentration of greater than 1,500 umol/L (2,101 ug/dL), many centers prescribe IHD initially to rapidly reduce the ammonia load to less than 200 umol/L (280 ug/dL), followed by CVVHDF to prevent ammonia rebound. In contrast, other centers prefer high-dose CVVHDF, using a blood flow rate of at least 10 ml/kg/min and a dialysate flow rate of 2–3 times the blood flow rate, especially for those patients with a serum ammonia concentration of 500–1,500 umol/L (700–2,101 ug/dL) (Fig. 41.1). Once dialysis has been initiated, the serum ammonia levels should be monitored on an hourly basis until the levels are sustained below 200 umol/L (280 ug/dL), at which time dialysis can be stopped with control of protein catabolism dependent on the provision of adequate nutrition and the activity of nitrogen scavenger s. Unfortunately, both IHD and CVVHDF also remove the pharmacological agents sodium phenylacetate and sodium benzoate, both of which are small molecules and readily dialyzable; hence, dose adjustments may have to be made to maintain the serum ammonia level below 200 umol/L (280 ug/dL) [12].
-
5.
Earlier reports on survival rates for neonatal hyperammonemia due to urea cycle disorders were dismal, with survival at about 20% [13]. Thankfully, this has improved, and survival rates have been about 80% over the past 20 years due to better nutritional and pharmacologic management and better dialytic options [1, 2, 4, 13]. However, despite these advances, the prognosis in terms of neurodevelopmental outcome for neonates with urea cycle disorde rs is still guarded, especially when the serum ammonia is greater than 350 umol/L(490 ug/dL) [13]. Neurodevelopmental complications include cerebral palsy, intellectual disability, learning problems, seizure disorders, speech disorders, and attention-deficit hyperactivity disorders. Other studies have shown that the neurological outcome may not be related to peak ammonia levels but to the duration of severe hyperammonemia, with better cognitive outcomes in those whose exposure was less than 24 h [2, 4].
Clinical Pearls
-
1.
Newborns with hyperammonemia typically present as a metabolic emergency between the ages of 24 and 48 h.
-
2.
Early management including glucose infusion, protein restriction, and pharmacologic intervention with nitrogen scavenger s is important to limit neurological damage. Dialysis is required to urgently remove ammonia if pharmacologic intervention is insufficient to remove the ammonia load.
-
3.
The severity of the neurological outcome appears to be related to the duration of severe hyperammonemia and not to the peak ammonia levels.
References
Gropman AL, Summar M, Leonard JV. Neurological implications of urea cycle disorders. J Inherit Metab Dis. 2007;30:865–9.
Auron A, Brophy PD. Hyperammonemia in review: pathophysiology, diagnosis, and treatment. Pediatr Nephrol. 2012;27:207–22.
Häberle J, Boddaert N, Burlina A, Chakrapani A, Dixon M, Huemer M, Karall D, Martinelli D, Crespo PS, Santer R, Servais A, Valayannopoulos V, Lindner M, Rubio V, Dionisi-Vici C. Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J Rare Dis. 2012;7:32. doi:10.1186/1750-1172-7-32.
Emms GM. Nitrogen sparing therapy revisited 2009. Mol Genet Metab. 2010;100:565–71.
Summar M. Current strategies for the management of neonatal urea cycle disorders. J Pediatr. 2001;138:S30–9.
Brusilow SW, Valle DL, Batshaw M. New pathways of nitrogen excretion in inborn errors of urea synthesis. Lancet. 1979;2(8140):452–4.
Schaefer F, Straube E, Oh J, Mehls O, Mayatepek E. Dialysis in neonates with inborn errors of metabolism. Nephrol Dial Transplant. 1999;14:910–8.
Fakler CR, Kaftan HA, Nelin LD. Two cases suggesting a role for the L-arginine nitric oxide pathway in neonatal blood pressure regulation. Acta Paediatr. 1995;84:460–2.
Summar M, Pietsch J, Deshpande J, Schulman G. Effective hemodialysis and hemofiltration driven by an extracorporeal membrane oxygenation pump in infants with hyperammonemia. J Pediatr. 1996;128:379–82.
Picca S, Dionisi-Vici C, Bartuli A, De Palo T, Papdia F, Montini G, Materassi M, Donati MA, Verrina E, Schiaffino MC, Pecoraro C, Iaccarino E, Vidal E, Burlina A, Emma F. Short-term survival of hyperammonemic neonates treated with dialysis. Pediatr Nephrol. 2015;30:839–47.
Bunchman TE. The complexity of dialytic therapy in hyperammonemic neonates. Pediatr Nephrol. 2015;30:701–2.
Bunchman TE, Barletta GM, Winters JW, Gardner JJ, Crumb TL, McBryde KD. Phenylacetate and benzoate clearance in a hyperammonemic infant on sequential hemodialysis and hemofiltration. Pediatr Nephrol. 2007;22:1062–5.
Kido J, Nakamura K, Mitsubuchi H, Ohura T, Takayanagi M, Matsuo M, Yoshino M, Shigematsu Y, Yorifuji T, Kasahara M, Horikawa R, Endo F. Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis. 2012;35:777–85.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Yap, HK. (2017). Neonatal Hyperammonemia. In: Warady, B., Schaefer, F., Alexander, S. (eds) Pediatric Dialysis Case Studies. Springer, Cham. https://doi.org/10.1007/978-3-319-55147-0_41
Download citation
DOI: https://doi.org/10.1007/978-3-319-55147-0_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55145-6
Online ISBN: 978-3-319-55147-0
eBook Packages: MedicineMedicine (R0)