Abstract
Urea cycle disorders (UCDs) are one of the most frequently inherited metabolic diseases in Japan, with an estimated prevalence of 1 per 50,000 live births. Here, we investigated the clinical manifestations, treatment, and prognosis of 177 patients with UCDs who were evaluated and treated from January 1999 to March 2009. These included 77 cases of neonatal-onset UCDs and 91 cases of late-onset UCDs. The most common UCD was ornithine transcarbamylase deficiency (OTCD), which accounted for 116 out of 177 patients. This result is similar to a previous study performed between 1978 and 1995 in Japan: OTCD accounted for about two-thirds of the total number of UCD cases. We studied the relationship between prognosis and the peak blood ammonia level at the onset in 151 UCD patients. Compared with a previous survey conducted in Japan, we found that a greater number of patients survived without any mental retardation despite their peak blood ammonia levels being greater than 360 μmol/l. The 5-year survival rate of patients with OTCD improved to 86% for those with the neonatal-onset type and to 92% for those with the late-onset type. We hypothesize that the increased survival rate is due to early diagnosis and better treatments that are now available in Japan. It is very important to diagnose and treat UCDs, especially OTCD, when the blood ammonia levels in patients are low. The outcome in patients with low blood ammonia levels was better than that in patients with high blood ammonia levels.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Urea cycle disorders (UCDs) are one of the most frequently inherited metabolic diseases in Japan, with an estimated prevalence of 1 per 50,000 live births. The urea cycle is the metabolic pathway that eliminates excess endogenous and exogenous nitrogen from the body by detoxification of ammonia into urea. This cycle comprises six different enzymes. Three of these enzymes are found in the mitochondrial matrix [N-acetylglutamate synthase (NAGS) EC 2.3.1.1; carbamoyl-phosphate synthetase 1 (CPS1) EC 6.3.5.5; and ornithine transcarbamylase (OTC) EC 2.1.3.3], and the other three are found in the cytosol [arginosuccinate synthetase (AS) EC 6.3.4.5; arginosuccinate lyase (AL) EC 4.3.2.1; and arginase-1 (AG) EC 3.5.3.1]. Dysfunction of these enzymes causes hyperammonemia. Nagata et al. (1991a) reported the prevalence rate of all five UCDs in Japan: CPS1 deficiency (CPSD; Mc Kusick no. 237300), 1 per 800,000 births; OTC deficiency (OTCD; Mc Kusick no. 311250), 1 per 80,000 births; classic AS deficiency (ASD; Mc Kusick no. 215700), 1 per 530,000 births; AL deficiency (ALD; Mc Kusick no. 207900), 1 per 800,000 births; and AG deficiency (AGD; Mc Kusick no. 207800), 1 per 2,200,000 births. OTCD is an X-linked disorder, whereas CPSD, ASD, ALD, and AGD are autosomal recessive disorders (Matsuda and Tanase 1997). The traditional treatment for UCDs is a low-protein diet. Sodium benzoate and/or sodium phenylbutyrate are used as an alternative pathway therapy (Brusilow et al. 1979; Brusilow 1991). Because arginine is lacking in all UCDs except AGD, arginine can be administered as therapy (Nagasaka et al. 2006). If necessary, treatment with essential amino acids and L-carnitine is recommended (Leonard 2001). Citrulline treatment is recommended for OTCD and CPSD patients (Feillet and Leonard 1998; Batshaw et al. 2001). Hemodialysis is more effective than peritoneal dialysis to rapidly eliminate blood ammonia (Schaefer et al. 1999). If medical therapy fails to control the general condition of UCD patients, a liver transplant is necessary (Uemoto et al. 1997).
There are many reports about the long-term outcome of UCD patients in Japan and overseas (Bachmann 2003; Maestri et al. 1996; Matsuda et al. 1991; Msall et al. 1984; Nagata et al. 1991b; Nassogne et al. 2005; Nicolaides et al. 2002; Uchino et al. 1998). Fifteen years have passed since the previous study was carried out in Japan. We assume that living-donor liver transplants and hemodialysis are more frequently performed now as compared to 15 years ago, and therefore we studied the long-term outcome and treatment of UCDs in Japan today.
Patients and methods
Study patients
In 2009, we sent a questionnaire to 928 institutions, including the departments of pediatrics, endocrinology and metabolism, neonatology, genetics, and transplant surgery, asking doctors if they had diagnosed or provided medical care to UCD patients. Each institution was the medical center for a local area in Japan and had 300 or more beds. Of the 928 institutions, 668 (72%) responded. Of these 668 institutions, 125 had treated patients with UCDs. A second questionnaire was then sent to these 125 institutions in 2009, of which 87 (70%) responded. Based on the reports of doctors who had diagnosed and treated patients with UCDs from January 1999 to March 2009, 177 cases of UCDs were studied. We excluded patients with secondary UCDs (citrin deficiency and lysinuric protein intolerance) and patients with unexplained hyperammonemia. We regarded a patient who visited several institutions as a single patient. The 177 cases of UCDs (CPSD, OTCD, ASD, ALD, and AGD) were diagnosed on the basis of clinical manifestations, family history, enzyme activity, metabolite analysis (blood amino acids and urinary orotic acid), and/or DNA analysis. Cognitive evaluations to diagnose mental retardation were performed by a pediatrician or child psychiatrist who treated patients with UCDs. The patient’s IQ was evaluated using standardized tests such as the Wechsler Intelligence Scale for Children (WISC) or the Wechsler Adult Intelligence Scale (WAIS). We described cognitive evaluation according to assessments by these doctors. The previous study (Uchino et al. 1998) was conducted in 1994 and reported on UCD patients from 1978 to 1995. At least 131 patients who were born after January 1996 or manifested symptoms after January 1996 were newly registered.
This study was approved by the ethics committee of the Faculty of Life Science, Kumamoto University.
Statistical analysis
Blood ammonia levels in the hemodialysis group and the nonhemodialysis group as well as the time when a liver transplant was performed after the onset were expressed as median and interquartile range (IQR) and analyzed by Mann-Whitney U test with IBM SPSS version 19. A P value of <0.05 was considered statistically significant (Supplemental data 1).
Kaplan-Meier curves of estimated survival rate were generated with the error bars representing 95% confidence interval (CI) for the mean, and comparisons between the groups were performed using a two-sided log-rank test by Graphpad Prism 5.
Results
We investigated the methods used to confirm diagnosis and found that enzyme activity was measured in 24% (43/177) of the patients with UCDs, and genotype analysis was performed in 56% (99/177); genotypes were identified in 32% (57/177) of the patients with UCDs. Eleven patients (6%) were diagnosed by DNA and enzymatic analysis. DNA was analyzed in 73 patients (male: 36, female: 37) with OTCD, 15 patients with CPSD, 10 patients with ASD, and 1 patient with ALD. In the analyzed patients, identifiable mutations were detected at a rate of 64% (23/36) in male-OTCD, 43% (16/37) in female-OTCD, 67% (10/15) in CPSD, 70% (7/10) in ASD, and 100% (1/1) in ALD.
Frequency of neonatal-onset and late-onset UCDs
Table 1 presents the rate of enzyme deficiencies, identifiable mutations, and number of UCD patients by age at disease onset: 77 patients (44%) manifested symptoms in the neonatal period and 91 patients (51%) were late-onset (presented symptoms after day 28 post-partum). OTCD was by far the most common UCD, accounting for 36% (28/77) of all neonatal-onset cases and 88% (80/91) of the late-onset cases. Among the CPSD, ASD, and ALD cases, 83% (19/23), 75% (21/28), and 89% (8/9) of patients, respectively, presented symptoms when they were newborns. Figure 1 shows the onset time for patients with OTCD. Of the male and female late-onset OTCD patients, 64% (51/80) presented symptoms between the ages of 1 and 6 years.
The onset time in patients with ornithine transcarbamylase deficiency (OTCD). The most frequent onset time for late-onset patients with OTCD was from 1 to 6 years of age. The unknown group include one treated male case before the onset and seven cases where onset timing was unknown (male: n = 57, female: n = 59)
Long-term survival
Table 2 presents survival numbers of patients with UCDs. Seventeen percent (13/77) of neonatal-onset cases and 10% (9/91) of the late-onset cases died.The overall survival rate after the first hyperammonemic attack was 93% (156/168). There was a 90% (69/77) 1-year survival rate for patients with neonatal-onset UCDs and a 95% (86/91) 1-year survival rate for patients with late-onset UCDs (data not shown). Among the deceased patients with neonatal-onset disease, 62% (8/13) died within 1 month after the first hyperammonemic attack. In the late-onset cases, 44% (4/9) of all deaths occurred within 1 month of the first hyperammonemic attack (data not shown).
Figure 2a represents the survival curve of patients with OTCD. The 5-year survival rate of patients with OTCD was 86% for those with the neonatal-onset type and 92% for those with the late-onset type. The 10-year survival rate for the three types of OTCD, except for female neonate-onset OTCD, was more than 80%. One of the seven female patients with neonatal onset of OTCD died 7 years and 4 months after the onset. Figure 2b and c represents the survival age of patients with late-onset OTCD. We compared the Kaplan-Meier survival curves of the previous study (Uchino et al. 1998) with those of the present study. The survival rate of male patients with late-onset OTCD was 89.4% at age 20 years in the present study (n = 30) and was 45.0% at age 20 years in the previous study (n = 48). The long-term survival rate of male patients with late-onset OTCD was significantly improved in this study (P = 0.004). The survival rate of female patients with late-onset OTCD was 83.8% at age 20 years in the present study (n = 50) and 29.8% at age 20 years in the previous study (n = 51). The long-term survival rate of female patients with late-onset OTCD was also improved in this study (P < 0.001).
a Survival rate after the onset in patients with ornithine transcarbamylase deficiency (OTCD). Survival plots of OTCD are shown by Kaplan-Meier survival curves. The 10-year survival rate in the three types of OTCD except for female neonate-onset OTCD was more than 80%. One of the seven female neonate-onset OTCD patients died 7 years and 4 months after the onset. [Male late-onset OTCD (black line), n = 30; female late-onset OTCD (gray line), n = 50; male neonate-onset OTCD (black dashed line), n = 21; female neonate-onset OTCD (gray dashed line), n = 7]. b Survival rate at each age in patients with late-onset male OTCD. The survival rates of OTCD patients at each age are shown by Kaplan-Meier survival curves with 95% CI. The survival rate of male OTCD patients in this study was higher than that in the previous study (Uchino et al. 1998). [Male late-onset OTCD from this study (black bold line), n = 30; male late-onset OTCD from the previous study (black dashed line), n = 48; P = 0.004]. c Survival rate at each age in patients with late-onset female OTCD. The survival rates of OTCD patients at each age are shown by Kaplan-Meier survival curves with 95% CI. The survival rate of female OTCD patients in this study was higher than that in the previous study (Uchino et al. 1998). [Female late-onset OTCD (black bold line), n = 50; female late-onset OTCD from the previous study (black dashed line), n = 51; P < 0.001]
Relationship between peak blood ammonia levels during the first hyperammonemic attack and cognitive development
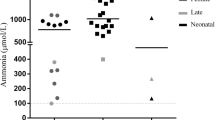
Figure 3a presents the relationship between peak blood ammonia levels during the first hyperammonemic attack and cognitive outcome. The peak blood ammonia levels at the onset and neurodevelopmental outcomes were known for 151 patients with UCDs. The two patients with a maximum ammonia concentration of less than 60 μmol/l survived, had not developed mental retardation, and had normal brain CT and MRI images and a normal electroencephalogram. When the maximum ammonia concentration was between 60 and 180 μmol/l, 64% (18/28) of patients survived, had not developed mental retardation, and had normal brain CT and MRI images and a normal electroencephalogram. Furthermore, 21% (6/28) of these patients had not developed mental retardation but had abnormal brain CT and MRI images and an abnormal electroencephalogram; 14% (4/28) of these patients survived but had developed mental retardation. Twelve patients died at the onset of the UCD, and the maximum ammonia concentration was recorded for 11 of them, which was greater than 360 μmol/l. Of the 74 patients with a maximum ammonia concentration greater than 360 μmol/l, 15% (11/74) died and 51% (38/74) developed mental retardation. In addition, 15% (11/74) of these patients did not develop mental retardation but had abnormal brain CT and MRI images or an abnormal electroencephalogram; 8% (6/74) of patients did not develop mental retardation and had normal brain CT and MRI images and a normal electroencephalogram. Information about mental retardation was unknown for 11% (8/74) of the patients The mental development was unknown for 10 of the 151 patients.
a Relationship between peak blood ammonia levels and neurodevelopmental outcome. Peak plasma ammonia levels were less than 60 μmol/l in 2 cases and greater than 60 μmol/l in 151 cases. The neurodevelopmental outcome was unknown in 10 of the 151 patients. Eighteen urea cycle disorder (UCD) patients with a maximum ammonia concentration greater than 360 μmol/l had normal neurodevelopment. b Survival and neurodevelopmental outcome in the hemodialysis group. Fifty-nine (39%) of 151 patients had received hemodialysis, and 85% (50/59) of these patients had a maximum ammonia concentration greater than 360 μmol/l. Twelve patients with ammonia concentrations greater than 360 μmol/l survived and had normal neurodevelopment. c Survival and neurodevelopmental outcome in the nonhemodialysis group. Ninety-two (61%) of 151 patients had not received hemodialysis, and 74% (68/92) of these patients had a maximum ammonia concentration of less than 360 μmol/l. Forty-nine patients with ammonia concentrations of less than 360 μmol/l survived and had normal neurodevelopment
Relationship between peak blood ammonia levels during the first hyperammonemic attack and treatment
Figure 3b and c present the relationship between peak blood ammonia levels during the first hyperammonemic attack and the outcome with and without hemodialysis. Hemodialysis included hemofiltration and hemodiafiltration. Of the 151 patients whose peak ammonia levels were known during the first hyperammonemic attack, 59 patients (39%) received hemodialysis, and the maximum ammonia concentration was greater than 360 μmol/l in 85% (50/59) of these patients. When the maximum ammonia concentration was more than 300 μmol/l and hemodialysis was not performed, 12 patients received peritoneal dialysis. All patients received hemodialysis or peritoneal dialysis when the maximum ammonia concentration was more than 600 μmol/l. Of the patients whose peak ammonia level at the onset was more than 360 μmol/l and who had not developed mental retardation, 66% (12/18) had received hemodialysis. We compared the hemodialysis group with the nonhemodialysis group regarding survival outcome. The median peak ammonia level at the onset in the hemodialysis group was 856 (IQR = 966) μmol/l (n = 59). The median peak ammonia level at the onset in the nonhemodialysis group was 235 (IQR = 220) μmol/l (n = 92) (P < 0.001) (Supplemental data 1). The long-term survival rate of the hemodialysis group was 84.6% (5 years after the onset), 78.5% (10 years), and 78.5% (15 years) according to the Kaplan-Meier survival curve. The survival rates of the nonhemodialysis group were 96.7% (5 years), 94.8% (10 years), and 94.8% (15 years), which were higher than those in the hemodialysis group (P < 0.001) (data not shown).
We assessed the relationship between peak blood ammonia levels and the occurrence of a liver transplant. Forty-two patients received a liver transplant that was independent of their peak blood ammonia level. Only one patient died of complications after the liver transplant. Thirteen of the surviving patients developed mental retardation (data not shown). Table 3 presents the ages at which liver transplants were performed. More than half of the patients received a liver transplant when they were between 1 month and 6 years of age: 26% (11/42) were between 1 month and 1 year of age and 40% (17/42) were between the ages of 1 and 6 years. Liver transplants were performed from 1 month to 18 years and 10 months after the onset (median 0.83, IQR = 2.46 years after the onset) (Supplemental data 1). We compared the survival outcome between the liver transplant group (n = 42) and the non-liver transplant group (n = 127). The long-term survival rate of the liver transplant group was 100% (5 years after the onset), 94.1% (10 years), and 94.1% (15 years) according to the Kaplan-Meier survival curve. The survival rates of the non-liver transplant group were 89.3% (5 years), 84.3% (10 years), and 81.5% (15 years), which were lower than those of the liver transplant group, although the difference was not statistically significant (P = 0.06) (Supplemental data 2).
Table 4 presents the treatment for UCDs. For OTCD, arginine was administered in 86% (110/116) of patients, sodium benzoate in 75% (87/116) of patients, and citrulline in 16% (19/116) of patients. A low-protein diet was administered in 64% (74/116) of patients. The combination of arginine and sodium benzoate was used in 72% (83/116) of patients with OTCD, in 61% (14/23) of patients with CPSD, in 79% (22/28) of patients with ASD, and in 100% (9/9) of patients with ALD. After the liver transplants, 91% (40/44) of the patients did not continue with these medications. Two patients with OTCD and two patients with ASD were administered arginine after the liver transplant. After the liver transplants, all patients did not require a low-protein diet, sodium benzoate, or sodium phenylbutyrate.
Discussion
Thirteen years ago, Uchino et al. (1998) reported that enzyme activity had been measured in almost 70% of patients with UCDs except for those with AGD. At present, however, enzyme activity is measured in only 22% of all patients with UCDs; we hypothesize that doctors may be unwilling to perform the invasive liver biopsy that is necessary for the enzyme assay and this could be a factor for the decline. In a previous survey, DNA mutations were identified in 4% of CPSD patients. Here, we report a higher percentage of identifiable mutations in patients with CPSD than that in the previous report. However, the rate of identifiable mutations in all patients with UCDs was unchanged. At present, many doctors in Japan diagnose UCDs by measuring blood amino acid levels and orotic acid levels in urine and refer to clinical manifestations and family histories of hyperammonemia. DNA analysis is preferred over enzyme assays for a definitive diagnosis. In this report, 24 institutions, including three academic medical centers, did not respond to the second questionnaire despite us sending three requests. Therefore, there may be a bias because some patients are not included in this study.
All types of UCD patients, including female OTCD patients, presented symptoms at any age. As you described, we mean that our ability to compare the results of our study to the previous one are limited, owing to both genetic (private mutations and lyonization in female-OTCD) and external (metabolic crises provoked by nonpredictable common disorders and leading to hyperammonemic crisis) factors that might have affected the outcomes. In Fig. 2b and c, the long-term survival rate was higher than that previously reported, likely due to improved awareness and competence of centers, which were able to intervene efficiently and rapidly. Unlike the previous study, this study reported that 18 patients with ammonia concentrations higher than 360 μmol/l at the onset had normal neurodevelopment. Bachmann (2003) reported that when the ammonia concentration at the onset was higher than 300 μmol/l, none of the patients had a normal neurodevelopment. Determinations of the risk of mental retardation versus normal development can be improved by using the combination of peak ammonia concentration and duration of coma rather than either parameter individually (Bachmann 2005). Furthermore, the age of the patient when exposed to hyperammonemia may also influence the neurological outcome and should be taken into account (Braissant et al. 2002). In general, a peak ammonia concentration of less than 180 μmol/l at the onset was a marker of good prognosis, and a peak ammonia concentration of more than 360 μmol/l was a marker of poor prognosis.
We compared the hemodialysis group with the nonhemodialysis group regarding survival and neurodevelopmental outcome (Fig. 3b and c). A greater number of patients with ammonia concentrations greater than 360 μmol/l had received hemodialysis. Twelve patients with ammonia concentrations greater than 360 μmol/l who had received hemodialysis had normal neurological development. However, patients with ammonia concentrations higher than 360 μmol/l had poor survival and neurodevelopmental outcome despite receiving hemodialysis. Many patients without hemodialysis with peak ammonia levels higher than 180 μmol/l died or developed mental retardation. Patients with a peak ammonia level greater than 180 μmol/l at the onset should receive hemodialysis.
In Japan, definitive criteria for liver transplants are controversial. An indication for a liver transplant does not depend on severity at the onset. We considered a liver transplant when hyperammonemia was not improved by medical therapy, if the patient experienced frequent hyperammonemic attacks. We did not evaluate mental development before a liver transplant, therefore we could not describe improved neurodevelopment by a liver transplant. Improved survival outcome might be attributed to a liver transplant. The metabolic derangement was resolved in 41 patients who had a successful liver transplant, and they could consume a normal protein diet without medication. Some patients did not experience hyperammonemia when they were under stress such as common cold. Liver transplants contributed to an improved quality of life in UCD patients. There are some reports about the improved quality of life in UCD patients after liver transplants in Japan and overseas (Whitington et al. 1998; Morioka et al. 2005; Kasahara et al. 2010)
Arginine and sodium benzoate are frequently used as therapy for UCDs in Japan (Table 4). The use of citrulline is recommended in cases of OTCD and CPSD (Feillet and Leonard 1998; Summar 2001). Apart from being expensive, citrulline, sodium benzoate, and sodium phenylbutyrate are not government-approved drugs in Japan, and, therefore, patients have to pay for them. Less than 75% of patients with CPSD and ASD were treated with a low-protein diet. Patients with CPSD and ASD who were not treated with a low-protein diet included patients that received a liver transplant, those who were treated with nonprotein formulas, or those for which information regarding treatment with a low-protein diet was unknown. Reports from other centers about patients who received a liver transplant for a UCD described the need for citrulline or arginine supplements, although these treatments have not been well accepted in Japan. UCD patients were rarely provided with citrulline or arginine supplements after a liver transplant.
In conclusion, we report the long-term outcome and intervention of UCDs in Japan. Compared with a previous study, we found a lower mortality rate at the onset of UCDs and an improved long-term outcome in patients.
References
Bachmann C (2003) Outcome and survival of 88 patients with urea cycle disorders: a retrospective evaluation. Eur J Pediatr 162:410–416
Bachmann C (2005) Long-term outcome of urea cycle disorders. Acta Gastroenterol Belg 68(4):466–468
Batshaw ML, MacArthur RB, Tuchman M (2001) Alternative pathway therapy for urea cycle disorders: twenty years later. J Pediatr 138(1 Suppl):S46–S54
Braissant O, Henry H, Villard AM et al (2002) Ammonium-induced impairment of axonal growth is prevented through glial creatine. J Neurosci 22:9810–9820
Brusilow SW (1991) Phenylacetylglutamine may replace urea as a vehicle for waste nitrogen excretion. Pediatr Res 29(2):147–150
Brusilow SW, Valle DL, Batshaw M (1979) New pathways of nitrogen excretion in inborn errors of urea synthesis. Lancet 2(8140):452–454
Feillet F, Leonard JV (1998) Alternative pathway therapy for urea cycle disorders. J Inher Metab Dis 21(Suppl 1):101–111
Kasahara M, Sakamoto S, Shigeta T et al (2010) Living-donor liver transplantation for carbamoyl phosphate synthetase 1 deficiency. Pediatr Transplant 14(8):1036–1040
Leonard JV (2001) The nutritional management of urea cycle disorders. J Pediatr 138(1 Suppl):S40–S44
Maestri N, Brusilow SW, Clissold DB, Bassett SS (1996) Long-term treatment of girls with ornithine transcarbamylase deficiency. N Engl J Med 335:855–859
Matsuda I, Tanase S (1997) The ornithine transcarbamylase (OTC) gene: mutations in 50 Japanese families with OTC deficiency. Am J Med Genet 71:378–383
Matsuda I, Nagata N, Matsuura T et al (1991) Retrospective survey of urea cycle disorders: part 1. Clinical and laboratory observations of thirty-two Japanese male patients with ornithine transcarbamylase deficiency. Am J Med Genet 38:85–89
Morioka D, Kasahara M, Takada Y et al (2005) Current role of liver transplantation for the treatment of urea cycle disorders: a review of the worldwide English literature and 13 cases at Kyoto University. Liver Transpl 11(11):1332–1342
Msall M, Batshaw ML, Suss R, Brusilow SW, Mellits DE (1984) Neurological outcome in children with inborn errors of urea synthesis. Outcome of urea-cycle enzymopathies. N Engl J Med 310:1500–1505
Nagasaka H, Yorifuji T, Murayama K et al (2006) Effects of arginine treatment on nutrition, growth and urea cycle function in seven Japanese boys with late-onset ornithine transcarbamylase deficiency. Eur J Pediatr 165(9):618–624
Nagata N, Matsuda I, Oyanagi K (1991a) Estimated frequency of urea cycle enzymopathies in Japan. Am J Med Genet 39:228–229
Nagata N, Matsuda I, Matsuura T et al (1991b) Retrospective survey of urea cycle disorders: part 2. Neurological outcome in forty-nine Japanese patients with urea cycle enzymopathies. Am J Med Genet 40:477–481
Nassogne MC, Héron B, Touati G, Rabier D, Saudubray JM (2005) Urea cycle defects: management and outcome. J Inherit Metab Dis 28(3):407–414
Nicolaides P, Liebsch D, Dale N, Leonard J, Surtees R (2002) Neurological outcome of patients with ornithine carbamoyltransferase deficiency. Arch Dis Child 86(1):54–56
Schaefer F, Straube E, Oh J, Mehls O, Mayatepek E (1999) Dialysis in neonates with inborn errors of metabolism. Nephrol Dial Transplant 14(4):910–918
Summar M (2001) Current strategies for the management of neonatal urea cycle disorders. J Pediatr 138(1 Suppl):S30–39
Uchino T, Endo F, Matsuda I (1998) Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inher Metab Dis 21(Suppl 1):151–159
Uemoto S, Yabe S, Inomata Y et al (1997) Coexistence of a graft with the preserved native liver in auxiliary partial orthotopic liver transplantation from a living donor for ornithine transcarbamylase deficiency. Transplantation 63(7):1026–1028
Whitington PF, Alonso EM, Boyle JT et al (1998) Liver transplantation for the treatment of urea cycle disorders. J Inher Metab Dis 21(Suppl 1):112–118
Acknowledgments
This study was supported in part by a Grant-in-Aid for the Global COE Program from the Japanese Society for the Promotion of Science and Ministry of Education, Culture, Sports, Science and Technology; a Grant-in-Aid for Pediatric Research from the Ministry of Health, Labor and Welfare; and a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology.
We thank all 668 institutions and, in particular, the 87 institutions that kindly provided us with useful clinical information on patients with urea cycle disorders. We are very grateful to Mari Kimura and Asuka Sakamoto for their help in survey analysis. We express our gratitude to Professor Takahiko Katoh at the Department of Public Health, Kumamoto University for critical analysis of the statistical methods.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Claude Bachmann
Competing interest: None declared.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM. 1
(PDF 61 kb)
Rights and permissions
About this article
Cite this article
Kido, J., Nakamura, K., Mitsubuchi, H. et al. Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis 35, 777–785 (2012). https://doi.org/10.1007/s10545-011-9427-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-011-9427-0