Abstract
Background
In severe neonatal hyperammonemia, extracorporeal dialysis (ECD) provides higher ammonium clearance than peritoneal dialysis (PD). However, there are limited outcome data in relation to dialysis modality.
Methods
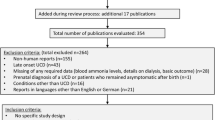
Data from infants with hyperammonemia secondary to inborn errors of metabolism (IEM) treated with dialysis were collected in six Italian centers and retrospectively analyzed.
Results
Forty-five neonates born between 1990 and 2011 were enrolled in the study. Of these, 23 were treated with PD and 22 with ECD (14 with continuous venovenous hemodialysis [CVVHD], 5 with continuous arteriovenous hemodialysis [CAVHD], 3 with hemodialysis [HD]). Patients treated with PD experienced a shorter duration of predialysis coma, while those treated with HD had a shorter ammonium decay time compared with all the other patients (p < 0.05). No difference in ammonium reduction rate was observed between patients treated with PD, CAVHD or CVVHD. Carbamoyl phosphate synthetase deficiency (CPS) was significantly associated with increased risk of death (OR: 9.37 [1.52–57.6], p = 0.016). Predialysis ammonium levels were significantly associated with a composite end-point of death or neurological sequelae (adjusted OR: 1.13 [1.02–1.27] per 100 μmol/l, p = 0.026). No association was found between outcome and dialysis modality.
Conclusions
In this study, a delayed ECD treatment was not superior to PD in improving the short-term outcome of neonates with hyperammonemia secondary to IEM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neonatal hyperammonemia is a severe clinical condition characterized by high ammonium levels and excess glutamine accumulation in astrocytes, inducing cell swelling and brain edema. In most cases, it concerns full-term, healthy-looking neonates showing feeding refusal, seizures, lethargy, coma, and death. Most frequently, it is caused by urea cycle defects (UCD) and organic acidurias (OA). In UCD, partial or complete lack of activity of key enzymes of the urea cycle (carbamoyl phosphate synthetase 1 [CPS1], ornithine transcarbamylase [OTC], argininosuccinate synthetase [ASS], argininosuccinate lyase [ASL], arginase 1 [ARG1], N-acetylglutamate [NAG], ornithine/citrulline antiporter [ORNT1]) induces primary accumulation of ammonium and a secondary increase in glutamine production, owing to the action of intracellular glutamine synthetase in the presence of hyperammonemia [1]. In OA, intramitochondrial accumulation of acyl-CoA esters induces a secondary block of urea cycle enzymes and may result in severe hyperammonemia [2].
Neonatal hyperammonemia is a rare condition (prevalence 1:9,000 live births) [3], but its diagnosis and management involve many competencies (biochemistry labs, metabolism experts, neonatal intensivists, surgeons), because of the multidisciplinary approach that these patients require. The initial management of undiagnosed hyperammonemia includes stopping protein intake, intravenous glucose, initiation of first-line medications: IV L-arginine, nitrogen scavengers, carbamylglutamate, carnitine, vitamin B12 and biotin. A diagnostic workup is simultaneously started and plasma amino acids, blood or plasma acylcarnitines, urinary organic acids, and orotic acid should be urgently requested [1].
In the last four decades, additional artificial ammonium depuration treatment has been introduced in patients not responding to medical and dietary management. After initial experiences with exchange transfusion [4–6], peritoneal dialysis (PD) was performed in these neonates with better results [6–11].
The availability of extracorporeal dialysis (ECD) facilities for neonates allowed more efficient ammonium removal [9, 12–18]. In particular, HD and continuous renal replacement therapy (CRRT) modalities found their application in neonates, given their higher efficacy compared with PD [12, 13, 19]. However, to date, there has been no clear evidence of which dialysis modality is associated with a better outcome [11, 13, 14].
In this multicenter, retrospective, non-controlled study, a large cohort of hyperammonemic neonates treated by dialysis was collected in six Italian pediatric hospitals with the scope of analyzing the possible association between dialysis and the short-term outcome, in terms of both survival and neurological sequelae.
Patients and methods
Data collection
This study was promoted by the Italian Society of Pediatric Nephrology and it was part of a dedicated Study Group. Six Italian Centers of Pediatric Nephrology were asked to provide retrospective information on all patients who were treated with any form of dialysis for neonatal hyperammonemia over the period spanning 1990 to 2011. Diseases included UCD (carbamoyl phosphate synthetase deficiency [CPS]; argininosuccinic aciduria [ASA], and citrullinemia [CIT]) and OA (propionic aciduria [PA] and methylmalonic aciduria [MMA]). In all cases, a final diagnosis was reached based on biochemical investigations, including measurement of plasma, urinary amino acids, urinary organic acids, and orotic acid. Plasma ammonium was measured according to local laboratory methods at the time of diagnosis. Male patients with ornithine transcarbamylase deficiency (OTC) were excluded because of the poor prognosis of this condition, irrespective of treatment in the post-natal period [20]. In general, patients were referred to the neonatal intensive care units of participating centers after a diagnosis of neonatal hyperammonemia. In a minority of cases, patients were transferred after failing to respond to medical treatment in order to begin dialysis.
Medical treatment included avoidance of nitrogen intake and a combination of the following agents: IV L-arginine hydrochloride (250–500 mg/kg/day), IV carnitine (250–500 mg/kg/day), IV sodium benzoate (250–500 mg/kg per day), PO phenylbutyrate (250 mg/kg per day), IV hydroxocobalamin (1 mg/day), and IV biotin (10 mg/day). The timing of the initiation of medical treatment was recorded and refers to the timing of the initiation of the above measures; medications were recorded in the database as dichotomous variables (yes/no) if they had been given at least once, using the above-listed doses for each compound.
The final decision to start dialysis and the choice of dialysis modality was made by local physicians. Dialysis was started when ammonium levels were considered too high to be treated only with medical measures or if patients failed to respond rapidly to medical treatment. Patients responding to medical treatment without the need for dialysis were excluded from the study.
Sequential ammonium levels during dialysis were available in a sub-group of patients. To synchronize levels every 4 h, data were log-transformed, synchronized by linear fitting, and back transformed.
A uniformed retrospective assessment of neurological damage was difficult to achieve. To overcome this limitation, physicians were simply asked to categorize surviving patients as having no, or any, neurological sequelae at day 28 of life. Likewise, a precise evaluation of the duration of coma was also difficult to obtain. Coma was defined as the number of hours of stage III coma (unconsciousness, decerebrated posture, reduced response to painful stimuli) or higher [21]. In general, resolution of coma could be accurately established from medical charts; in several patients. however, the age at which patients entered a comatose stage was more difficult to define; all efforts were made to establish the beginning of coma, including phone interviews with families and with referring physicians. Outcome at 1 month was chosen as the end-point of this study because UCD and OA are known to be diseases characterized by relapsing episodes of metabolic decompensation that frequently result in neurological sequelae and influence the medium- and long-term outcome. Predictors of outcome were analyzed by logistic regression using as primary end-points: death at 28 days of life, or death or neurological sequelae at 28 days of life as a composite end-point. As the primary aim of this study was restricted to evaluating the impact of the dialysis modality on neonatal outcome and survival, all data were censored at 28 days of life. This retrospective analysis was approved by the Ethics Committee of the Bambino Gesù Children′s Hospital (IRCCS).
Statistical analysis
Data were analyzed using SPSS 11.5.1 for Windows software (SPSS, Chicago, IL, USA). Data are expressed as mean±standard deviation if they passed normality tests (Kolmogorov–Smirnov and Shapiro–Wilk test). Otherwise, continuous data are reported as the median value and range. Dichotomous values are indicated as absolute count and percentage. Normal values were compared using a t test, nonparametric distribution data were compared using the Mann–Whitney U test and frequencies using Fisher’s exact test. Outcome values were analyzed using Kaplan–Meier curves. Data were compared using the log-rank test. The impact of covariates was analyzed using the Cox–Mantel test. Multivariate analysis was performed on covariates that reached the p < 0.10 threshold. All p values are two-sided.
Results
Patients’ characteristics and outcomes
Forty-seven patients were included in the study. Of these, 2 patients were excluded because they had been treated with both PD and extracorporeal dialysis (ECD). In the remaining 45 patients, primary diagnosis was CPS deficiency in 7 patients, ASA in 9 patients, CIT in 10 patients, PA in 11 patients, and MMA in 8 patients. Twenty-three infants were treated with PD and 22 with ECD.
Patient characteristics are reported in Table 1. No differences were observed in the distribution of the underlying metabolic defect between the PD and ECD groups, except for CPS deficiency, which was treated more frequently with ECD. General characteristics were also similar, with the exception of the duration of coma before RRT initiation, which was significantly shorter in the PD group. In the ECD group, 14 patients were treated with CVVHD, 5 with CAVHD, and 3 with HD. In all cases, medical treatment was started soon after detecting hyperammonemia and included avoidance of nitrogen intake and administration of IV glucose solutions and/or nasogastric infusions of protein-free formulas. In addition, 45 patients (100 %) received L-arginine hydrochloride, 34 (76 %) L-carnitine, 34 (76 %) sodium benzoate, 12 (27 %) phenylbutyrate, 15 (33 %) hydroxocobalamin, and 9 (20 %) IV biotin.
At 4 weeks of life, 13 patients (29 %) had died, 20 patients (44 %) recovered without substantial sequelae, and 12 patients (27 %) recovered with significant neurological sequelae, including developmental impairment, seizures, hypotonia and/or hypertonia. Outcomes for each disease group are presented in Fig. 1.
Dialysis
Threshold levels of serum ammonium for starting dialysis and modality of dialysis depended on local facilities and expertise. Seventy-five percent of patients (34 out of 45) were referred to one of the tertiary care centers of the present study to start dialysis after the diagnosis of hyperammonemia. Ammonium levels at admission, at the beginning of dialysis, as well as peak ammonium levels during the hospital stay, were similar in the PD and ECD groups (Table 1). The median age for starting dialysis was 4.4 days and did not differ between children treated with PD or ECD (Table 1; log-rank test: p = 0.331). Conversely, children treated with PD continued dialysis for a significantly longer period of time than children treated with extra-corporeal techniques (log-rank test: p < 0.001); the death-censored median duration of dialysis was 0.9 days and 2.2 days in the ECD and PD groups respectively (p < 0.001).
In most cases, ammonium decreased rapidly after beginning dialysis (Fig. 2a, b), except in 4 patients who were excluded from the ammonium decay analysis (Fig. 2c). Of these, 3 patients treated with ECD showed profound hypotension, limiting dialysis efficiency, and 1 treated with PD did not show plasma ammonium reduction because of excessive catabolism.
Ammonium evolution in a subgroup of 31 patients for whom sequential ammonium data were available during dialysis. The upper panels show the ammonium levels of patients treated with a extracorporeal and b peritoneal dialysis. c Illustrates levels of dialysis of 4 patients whose ammonium course was not consistent with an exponential decay and were for this reason discarded from the analysis in d. d Shows the percentage of ammonium decay (mean±SE), according to the modality of dialysis. * p < 0.05
Synchronized ammonium levels showed that patients treated with HD had a significantly faster ammonium reduction rate at 4 h (p = 0.045), compared with all other patients. Ammonium decay tended to be slower in patients treated with PD and intermediate in patients treated with either CAVHD or CVVHD, but differences were not statistically significant (Fig. 2d).
Predictors of outcome
Preliminary analyses on the impact of nonmodifiable variables showed that the year of treatment after 1990 was marginally associated with an improved composite end-point (odds ratio [OR]: 0.87 (0.73–1.02), p = 0.091), and that CPS was significantly associated with an increased risk of death (OR: 9.37 [1.52–57.6], p = 0.016). No association was observed with gender, gestational age, birth weight, Apgar score or dialysis center (see Supplementary Table 1a and 1b). On these bases, all subsequent analyses were adjusted for CPS deficiency and year of treatment (number of years after 1990).
No significant association was observed with the risk of death (Table 2). Marginal associations (p < 0.10) were observed with the age at dialysis (adjusted OR: 1.37 [0.97–1.95] per day, p = 0.074), with pre-dialysis ammonium levels (adjusted OR: 1.10 [0.99–1.23] per 100 μmol/l, p = 0.088) and with the total coma duration (adjusted OR: 4.30 [0.90–20.61] per day, p = 0.068).
For the composite end-point, a significant association was observed with the ammonium levels at the beginning of dialysis (adjusted OR: 1.13 [1.02–1.27] per 100 μmol/l, p = 0.026) and a marginal association was observed with ammonium levels before starting medical treatment (adjusted OR: 1.21 [0.99–1.47] per 100 μmol/l, p = 0.059; Table 2).
No association was observed between the primary or composite end-points and modality of dialysis.
Discussion
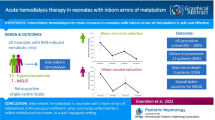
Over the past decades, technical advances and increased expertise in performing dialysis in very small infants has led to treating infants with severe hyperammonemia secondary to inborn errors of metabolism (IEM) with combined medical and dialytic treatment [15, 16]. Studies on neonatal hyperammonemia are scanty and mostly retrospective owing to the rarity of IEM. Despite the lack of rigorous studies, a combined medical and dialytic approach has most likely resulted in improved short-term outcome [12, 13, 18, 19].
Several groups have tried to identify predictors of outcome. In 1984, Msall et al. reported that the neurological outcome of 26 infants with neonatal hyperammonemia was associated with the duration of coma and not with peak ammonium levels [21]. However, at that time diagnosis was often delayed and treatment of hyperammonemia was restricted to decreasing the ammonium generation rate with experimental drugs, protein restriction, and calorie supply. This has led to the establishment of protocols for early diagnosis and treatment in the following years and to the demonstration in the 1990s that peak ammonium levels are also associated with poor outcome [22]. On these bases, dialysis was proposed in infants with very elevated ammonium levels as a means of accelerating ammonium reduction in addition to medical treatment [6, 7, 12, 13, 23–27]. In these patients, ammonium levels rapidly increase after birth as a result of protein introduction, leading to a high ammonium generation rate and poor renal clearance. Dialysis increases the clearance of ammonium, which readily diffuses across synthetic membranes and, to a lesser extent, across the peritoneal membrane [28, 29].
In theory, extracorporeal treatments, in particular HD, should be preferred to PD, because they provide significantly higher ammonium clearances [17, 19, 28]. Thus, HD has been proposed as the optimal choice for fast ammonium removal [12, 29]. In addition, CRRT techniques also allow achievement of satisfactory results [13–15, 18, 19] and are frequently used nowadays in centers where neonatal HD is not available or in order to prevent rebound of ammonium after stopping HD [30]. CRRT offers the advantage of being better tolerated in sick neonates, compared with HD [14]. Nonetheless, PD has recently been used with good results [11]. In particular, PD is easier to perform in neonates, whereas extracorporeal techniques require special skills and are more susceptible to complications such as hypotension, hypothermia, and circuit clotting. In particular, changes in the circuit due to clotting create significant down-times in the treatment, which can invalidate the benefits of higher ammonium clearance by ECD. Moreover, often infant ECD requires neonatal transport to specialized centers, possibly prolonging coma duration. Importantly, we did not observe differences in the age at initiation of dialysis, nor in the ammonium levels at the beginning of dialysis, between the PD and ECD cohorts, although we found a shorter coma duration in patients treated with PD.
The current preferred use of ECD in neonatal hyperammonemia is primarily based on faster ammonium clearance by these techniques; outcome studies, however, are lacking. Arbeiter et al. have retrospectively analyzed data on 21 hyperammonemic neonates treated with CVVHD (n = 17) or with PD (n = 4). The 50 % ammonium reduction time was significantly shorter in infants treated with CVVHD, while no significant differences were observed in the time needed to reach a noncritical value of 200 μg/dl. The survival rate was 14 out of 17 in the CVVHD group and 2 out of 4 in the PD group [19]. In the study by Schaefer et al., the ammonium removal rate by dialysis was the main determinant of outcome in 11 hyperammonemic infants, 6 of whom were treated with CVVHD. Of note, 2 out of 5 patients treated with PD had ammonium decay similar to patients treated with CVVHD. The authors attributed this unexpected result, at least in part, to the use of small catheters limiting CVVHD efficiency [13]. However, the role played by the ammonium removal rate with dialysis in the outcome was not confirmed in other studies. Westrope et al., for example, found no association between ammonium removal efficacy and outcome in 14 neonates treated with continuous venovenous hemofiltration (CVVH); they also failed to observe a prognostic value of pre-dialysis ammonium levels [31]. In 2001, we found no influence of ECD modality in 10 hyperammonemic neonates (CVVHD vs HD); their outcome was equally not related to the rapidity of ammonium level decrease or to the underlying metabolic defect, but was related to the duration of coma before starting dialysis [14]. Finally, Pela et al. reported that patients treated with PD had a good outcome overall, provided that dialysis was started rapidly after the first symptoms of hyperammonemic coma [11].
Taken together, these data are limited by the small number of patients included in each study, but strongly suggest that prevention or fast resolution of hyperammonemic coma is the major determinant of short-term outcome in infants with neonatal hyperammonemia. No decisive conclusion, on the other hand, can be drawn on the relative benefit of specific dialysis modalities.
To overcome limitations due to the rarity of these diseases, we have set up a multicenter study allowing us to recruit a large number of patients and to obtain a balanced cohort of children treated with PD or with ECD. Our main finding is that short-term outcome is not dependent upon dialysis modality, both in terms of patient survival and neurological sequelae. Moreover, ammonium reduction time did not correlate with outcome, regardless of the dialysis modality. A trend was observed in the association between patient outcome and pre-dialysis ammonium levels and between outcome and coma duration. Pre-dialysis ammonium levels were significantly associated with the combined outcome of death and neurological sequelae. As expected, the ammonium reduction rate was fastest in patients treated with HD. Our results suggest that HD has to be performed in neonates with extremely high ammonium levels and in a stable condition, or when ammonium generation induces a rapid increase in plasma levels. No significant differences in the ammonium reduction rate were observed when comparing patients treated with PD, CAVHD or CVVHD. This was in part unexpected, since most studies have reported higher ammonium reduction rates with CVVHD than in PD [13, 19, 28, 32]. In this regard, an important limitation of this study is the lack of data on the prescription of dialysis. We cannot therefore exclude differences in dialysis schedule prescription that may have occurred. Indeed, all available reports show that CRRT provides a two- to ten-fold higher clearance of ammonium [12, 19, 28]. A possible explanation is that the late referral of patients treated with ECD to the centers with dialysis facilities, as suggested by their longer coma duration (see Table 1), induced extremely high ammonium generation, thus affecting the plasma reduction even during dialysis with a more effective modality (i.e., CRRT). Despite enrolling the largest cohort of hyperammonemic infants reported to date, our study has other limitations including the limited number of patients, which restricts the power of statistical analyses, and the retrospective collection of data. In addition, the study period corresponds to the development of continuous dialysis techniques and to their adaptation for the treatment of small infants; therefore, during the study, technology has evolved and operator skills have improved. This limitation is inevitably present in similar retrospective studies that have considered data collected over a period from 8 to 12 years [11, 13, 14, 19, 30, 31]. Nonetheless, it is remarkable that patients treated with PD had a very similar, if not slightly better, outcome. In the study by Pela et al., PD was the only modality used and the outcome was generally good in the presence of a short mean time to PD initiation and a time on PD >200 μmol/L of ammonium not exceeding 36 h in 5 out of 6 patients. In our study, 21 out of 22 patients treated with PD had a substantially longer time to dialysis than those of Pela et al. [11] reaching ammonium levels <200 within 36 h, but showed a worse outcome than those of Pela et al., indicating that patients treated with PD (lowest ammonium clearance) do not necessarily show a bad outcome provided that time to dialysis start is short. This indicates that PD should be performed immediately after admission simultaneously with medical treatment, if this is yet to be started. In the assessment of risk factors, restricting the cohort to patients who required dialysis obviously introduces an important bias by selecting very severe patients. Therefore, the impact of high ammonium levels or prolonged coma duration is likely to be underestimated; thus, these results may apply mainly to dialyzed patients. Moreover, it is possible that the degree of severity of our patients rendered these results applicable only to patients with long coma duration. In agreement with this hypothesis, peak ammonium levels were associated with poor outcome, indicating that timely diagnosis and referral are crucial for successful treatment. In this view, our results question the rationale of systematically transferring newborns to third-level centers that can perform ECD, which inevitably delays initiation of dialysis, rather than performing PD, a technique that is nowadays available in most centers. Another important observation was the lack of substantial rebound in surviving infants, suggesting that ammonium generation was no longer significant when dialysis was stopped and that initiation of medical treatment allowed control of the metabolic decompensation. Another intriguing possibility is that PD has a different impact upon the glucidic metabolism compared with ECD techniques that use isotonic dialysate fluids with physiological concentrations of glucose. Conversely, peritoneal dialysis solutions have very high glucose content (more than 10-fold higher than serum levels) and glucose diffuses directly into the mesenteric circulation through the peritoneal membrane, which is particularly permeable in neonates [33, 34]. Hypothetically, this may result in higher glucose delivery compared with ECD and decreased ammonia generation. Unfortunately, our data cannot address this interesting point because ammonium kinetics were not available. High serum ammonium in neonatal hyperammonemia is the combined result of an increased ammonium generation rate and limited renal clearance. Likewise, decreased ammonium levels during dialysis reflect increased clearance, but also slower generation after initiation of medical treatment. This has been a limitation in previous studies, which have expressed dialysis efficacy by estimating the 50 % ammonium decay time [13, 14, 19], an easy parameter to extrapolate from retrospective data, but one that does not entirely reflect dialysis efficiency. Of note, ammonium generation can be very different according to the type of IEM and to the degree of catabolism [35].
In conclusion, in our series, a delayed ECD treatment was not superior to PD in improving the short-term outcome of hyperammonemic neonates. Under these circumstances, delaying initiation of dialysis in order to transfer patients to centers with expertise in neonatal ECD must be discussed. While other studies are needed to confirm these findings, our data emphasize the importance of early referral for diagnosis, initiation of medical and dialysis treatment, which probably represents the major determinant of neonatal outcome. In these patients dialysis has to be regarded as a means of accelerating the effects of medical treatment by removing excesses of ammonium that accumulated during the early postnatal period.
References
Häberle J, Boddaert N, Burlina A, Chakrapani A, Dixon M, Huemer M, Karall D, Martinelli D, Crespo PS, Santer R, Servais A, Valayannopoulos V, Lindner M, Rubio V, Dionisi-Vici C (2012) Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J Rare Dis 7:32
Coude FX, Sweetman L, Nyhan WL (1979) Inhibition by propionyl coenzyme A of N-acetylglutamate synthetase in rat liver mitochondria. J Clin Invest 64:1544–1548
Dionisi-Vici C, Rizzo C, Burlina AB, Caruso U, Sabetta G, Uziel G, Abeni D (2002) Inborn errors of metabolism in the Italian pediatric population: a national retrospective survey. J Pediatr 140:321–327
Campbell AG, Rosenberg LE, Snodgrass PJ, Nuzum CT (1973) Ornithine transcarbamylase deficiency: a cause of lethal neonatal hyperammonemia in males. N Engl J Med 288:1–6
Snyderman SE, Sansaricq C, Phansalkar SV, Schacht RC, Norton PM (1975) The therapy of hyperammonemia due to ornithine transcarbamylase deficiency in a male neonate. Pediatrics 56:65–73
Francois B, Cornu G, de Meyer R (1976) Peritoneal dialysis and exchange transfusion in a neonate with argininosuccinic aciduria. Arch Dis Child 51:228–231
Wiegand C, Thompson T, Bock GH, Mathis RK, Kjellstrand CM, Mauer SM (1980) The management of life-threatening hyperammonemia: a comparison of several therapeutic modalities. J Pediatr 96:142–144
Gortner L, Leupold D, Pohlandt F, Bartmann P (1989) Peritoneal dialysis in the treatment of metabolic crises caused by inherited disorders of organic and amino acid metabolism. Acta Paediatr Scand 78:706–711
Donn SM, Swartz RD, Thoene JG (1979) Comparison of exchange transfusion, peritoneal dialysis, and hemodialysis for the treatment of hyperammonemia in an anuric newborn infant. J Pediatr 95:67–70
Robert MF, Schultz DJ, Wolf B, Cochran WD, Schwartz AL (1979) Treatment of a neonate with propionic acidaemia and severe hyperammonaemia by peritoneal dialysis. Arch Dis Child 54:962–965
Pela I, Seracini D, Donati MA, Lavoratti G, Pasquini E, Materassi M (2008) Peritoneal dialysis in neonates with inborn errors of metabolism: is it really out of date? Pediatr Nephrol 23:163–168
Summar M, Pietsch J, Deshpande J, Schulman G (1996) Effective hemodialysis and hemofiltration driven by an extracorporeal membrane oxygenation pump in infants with hyperammonemia. J Pediatr 128:379–382
Schaefer F, Straube E, Oh J, Mehls O, Mayatepek E (1999) Dialysis in neonates with inborn errors of metabolism. Nephrol Dial Transplant 14:910–918
Picca S, Dionisi-Vici C, Abeni D, Pastore A, Rizzo C, Orzalesi M, Sabetta G, Rizzoni G, Bartuli A (2001) Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatr Nephrol 16:862–867
Bunchman TE, Barletta GM, Winters JW, Gardner JJ, Crumb TL, McBryde KD (2007) Phenylacetate and benzoate clearance in a hyperammonemic infant on sequential hemodialysis and hemofiltration. Pediatr Nephrol 22:1062–1065
Picca S, Bartuli A, Dionisi-Vici C (2008) Medical management and dialysis therapy for the infant with an inborn error of metabolism. Semin Nephrol 28:477–480
Lai YC, Huang HP, Tsai IJ, Tsau YK (2007) High-volume continuous venovenous hemofiltration as an effective therapy for acute management of inborn errors of metabolism in young children. Blood Purif 25:303–308
Chen CY, Tsai TC, Lee WJ, Chen HC (2007) Continuous hemodiafiltration in the treatment of hyperammonemia due to methylmalonic acidemia. Ren Fail 29:751–754
Arbeiter AK, Kranz B, Wingen AM, Bonzel KE, Dohna-Schwake C, Hanssler L, Neudorf U, Hoyer PF, Büscher R (2010) Continuous venovenous haemodialysis (CVVHD) and continuous peritoneal dialysis (CPD) in the acute management of 21 children with inborn errors of metabolism. Nephrol Dial Transplant 25:1257–1265
Saudubray JM, Touati G, Delonlay P, Jouvet P, Narcy C, Laurent J, Rabier D, Kamoun P, Jan D, Revillon Y (1999) Liver transplantation in urea cycle disorders. Eur J Pediatr 158 [Suppl 2]:S55–S59
Msall M, Batshaw ML, Suss R, Brusilow SW, Mellits ED (1984) Neurologic outcome in children with inborn errors of urea synthesis. N Engl J Med 310:1500–1505
Uchino T, Endo F, Matsuda I (1998) Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inherit Metab Dis 21 [Suppl 1]:151–159
Siegel NJ, Brown RS (1973) Peritoneal clearance of ammonia and creatinine in a neonate. J Pediatr 82:1044–1046
Ring E, Zobel G, Stockler S (1990) Clearance of toxic metabolites during therapy for inborn errors of metabolism. J Pediatr 117:349–350
Thompson GN, Butt WW, Shann FA, Kirby DM, Henning RD, Howells DW, Osborne A (1991) Continuous venovenous hemofiltration in the management of acute decompensation in inborn errors of metabolism. J Pediatr 118:879–884
Sperl W, Geiger R, Maurer H, Guggenbichler JP (1990) Continuous arteriovenous haemofiltration in hyperammonemia of newborn babies. Lancet 336:1192–1193
Falk MC, Knight JF, Roy LP, Wilcken B, Schell DN, O′Connell AJ, Gillis J (1994) Continuous venovenous haemofiltration in the acute treatment of inborn errors of metabolism. Pediatr Nephrol 8:330–333
Wong KY, Wong SN, Lam SY, Tam S, Tsoi NS (1998) Ammonia clearance by peritoneal dialysis and continuous arteriovenous hemodiafiltration. Pediatr Nephrol 12:589–591
Summar M (2001) Current strategies for the management of neonatal urea cycle disorders. J Pediatr 138 [1 Suppl]:S30–S39
McBryde KD, Kershaw DB, Bunchman TE, Maxvold NJ, Mottes TA, Kudelka TL, Brophy PD (2006) Renal replacement therapy in the treatment of confirmed or suspected inborn errors of metabolism. J Pediatr 148:770–778
Westrope C, Morris K, Burford D, Morrison G (2010) Continuous hemofiltration in the control of neonatal hyperammonemia: a 10-year experience. Pediatr Nephrol 25:1725–1730
Semama DS, Huet F, Gouyon JB, Lallemant C, Desgres J (1995) Use of peritoneal dialysis, continuous arteriovenous hemofiltration, and continuous arteriovenous hemodiafiltration for removal of ammonium chloride and glutamine in rabbits. J Pediatr 126:742–746
Fischbach M, Terzic J, Bergère V, Gaugler C, Provot E (1999) The optimal approach to peritoneal dialysis prescription in children. Perit Dial Int 19(Suppl 2):S462–S466
Warady BA, Alexander SR, Hossli S, Vonesh E, Geary D, Watkins S, Salusky IB, Kohaut EC (1996) Peritoneal membrane transport function in children receiving long-term dialysis. J Am Soc Nephrol 7:2385–2391
Batshaw ML (1984) Hyperammonemia. Curr Probl Pediatr 14:1–69
Disclosure
The results presented in this paper have not been published previously in whole or in part.
All the authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Picca, S., Dionisi-Vici, C., Bartuli, A. et al. Short-term survival of hyperammonemic neonates treated with dialysis. Pediatr Nephrol 30, 839–847 (2015). https://doi.org/10.1007/s00467-014-2945-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-014-2945-x