Abstract
Background
Outcomes for severe hyperammonemia treated with renal replacement therapy (RRT) reported in the literature vary widely. This has created differing recommendations regarding when RRT is beneficial for hyperammonemic patients.
Methods
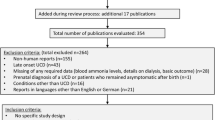
To evaluate our institution’s experience with RRT in pediatric patients with inborn errors of metabolism (IEMs) and potential prognostic indicators of a better or worse outcome, we performed a retrospective chart review of patients who received RRT for hyperammonemia. Our cohort included 19 patients with confirmed IEMs who received RRT between 2000 and 2017. Descriptive statistics are presented as medians with interquartile ranges with appropriate statistical testing assuming unequal variance.
Results
There were 16 males (84%) and 3 females (16%) identified for inclusion in this study. There were 9 survivors (47%) and 10 non-survivors (53%). The average age of survivors was 67 months (age range from 3 days to 15.6 years). The average age of non-survivors was 1.8 months (age range from 2 days to 18.7 months). Peak ammonia, ammonia on admission, and at RRT initiation were higher in non-survivors compared with survivors. Higher ammonia levels and no change in ammonia between admission and RRT initiation were associated with an increased risk of mortality.
Conclusions
Hyperammonemia affects two distinct patient populations; neonates with markedly elevated ammonia levels on presentation and older children who often have established IEM diagnoses and require RRT after failing nitrogen-scavenging therapy. Our experience demonstrates no significant change in mortality associated with neonatal hyperammonemia, which remains high despite improvements in RRT and intensive care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hyperammonemia is a critical metabolic disturbance that is seen in inborn errors of metabolism (IEMs), notably urea cycle defects (UCD) and organic acidemias (OA). Aggressive and expedient treatment is integral to prevent mortality and preserve neurocognition. The risk of neurologic impairment has been well-documented to increase with higher peak ammonia levels and particularly longer durations of hyperammonemia [1,2,3,4,5,6,7,8,9]. Over the past 3 decades, remarkable progress has been made in the treatment of hyperammonemia with the use of sodium phenylacetate and sodium benzoate to lower plasma ammonia levels during acute metabolic decompensations. However, for severe hyperammonemia, renal replacement therapy (RRT) remains the mainstay for rapid clearance of plasma ammonia levels. Despite aggressive treatment, mortality rates for patients with IEMs are high. Previous studies, including our institution’s previous retrospective study for all patients who received RRT for hyperammonemia from 1991 to 2000, found mortality rates of approximately 25–50% in suspected or confirmed IEMs [7, 10,11,12].
The approach to RRT in hyperammonemia has evolved over time. Early treatment options for hyperammonemia included exchange transfusions and peritoneal dialysis (PD); however, there is long-standing evidence showing that these options are less efficient for removal of ammonia [13, 14]. It should be noted that PD remains an option for physicians caring for hyperammonemic neonates who are concerned about the ability to obtain central access in a timely fashion [15, 16]. In the past 3 decades, intermittent hemodialysis (HD) and continuous renal replacement therapy (CRRT) have been primarily used to decrease plasma ammonia levels. HD is the most efficient method to reduce plasma ammonia levels; however, hypotension is often cited as a complication and ammonia levels tend to rebound shortly after discontinuation [11]. In contrast, CRRT can decrease plasma ammonia levels with less risk of hemodynamic instability and less chance of rebound hyperammonemia [17]. Additionally, the ability of newer generations of CRRT now allow clearances comparable to intermittent HD. The exact RRT prescription and prognostic factors for better or worse outcomes in hyperammonemia, particularly in neonates, are unclear [18]. Currently there is general agreement that all treatment options including RRT should be employed to decrease ammonia levels; however, the exact plasma ammonia level that should trigger RRT is debated [7, 12, 17, 18]. The recently updated UCD guidelines suggest assessing the response to nitrogen-scavenging therapy prior to RRT initiation, but the degree of response that would not require RRT is unclear [17]. The risk of prolonging the duration of hyperammonemia and delaying RRT initiation while assessing response to nitrogen-scavenging therapy must be considered as well.
While prognostic indicators do not completely guarantee a specific outcome, they can be an integral component of decision-making between medical teams and patient families. Currently there are few prognostic indicators available to assist providers and families in deciding between curative or comfort care. The lack of clarity on these specific points is likely related to multiple factors including the rarity of hyperammonemia caused by IEM, retrospective nature of previous studies, as well as differences in patient cohorts and institutional practices.
We present our institution’s updated experience with RRT for severe hyperammonemia in patients with UCD and OA from 2000 to 2017. A previous publication from our institution examined outcomes of RRT for hyperammonemia from 1991 to 2000. This cohort had an overall mortality rate of 57% and found that those patients who received HD as the initial RRT modality had improved survival [10]. In this report, we describe our experience with RRT for treatment of hyperammonemia in pediatric patients and examine prognostic factors including well-known factors like peak ammonia, to less frequently examined factors such as use of vasopressors [19] and choice of RRT modality. While most publications on hyperammonemia focus on the management of neonatal UCDs, our patient cohort also includes OA patients and older pediatric patients. We believe our work provides additional meaningful information for medical teams of nephrologists, geneticists, and pediatric intensivists managing severe hyperammonemia and counseling families about their child’s prognosis.
Methods
The University of Michigan Health System institutional review board approved a retrospective chart review of patients who received RRT for hyperammonemia. The patients included in this study were pediatric patients (less than 18 years of age) with confirmed inborn errors of metabolism (UCD or OA) between 2000 and 2017. A total of 17 patients underwent 19 treatments of RRT during this time frame. Treatments were defined by the start of RRT and ending with the discontinuation of RRT and improved ammonia levels, death, or redirection toward comfort care. The first of the two patients who received 2 RRT treatments was 11 days of age and 4 years of age during respective treatments. The other patient who received 2 treatments with RRT underwent a second treatment of RRT 10 days after discontinuation of the first treatment and normalization of ammonia levels; this was considered a separate hyperammonemia episode and RRT treatment. During the course of this study period, our institution implemented clinical practice guidelines regarding when HD versus CRRT should be used based on plasma ammonia levels. Per guidelines, all hyperammonemic patients should receive nitrogen-scavenging medications as soon as possible. Plasma ammonia levels > 500 μmol/L received HD as the initial RRT modality prior to transitioning to CRRT, whereas plasma ammonia levels between 200 and 500 μmol/L were treated with CRRT without a session of HD. Frequency of plasma ammonia concentrations were measured at the discretion of the pediatric nephrology, pediatric genetics, and pediatric intensive care unit teams. Review of medical records for each patient determined basic demographic information (sex, age, weight, length, IEM diagnosis) as well as specifics of medical treatment (use of nitrogen-scavenging medications [sodium phenylacetate and sodium benzoate], use of vasopressors, involvement of spiritual care during admission, completion of neuroimaging and/or EEG for neuro prognostication). RRT records were also reviewed to determine RRT modality, duration of RRT, conversion to second modality of RRT, and RRT-associated complications. Glomerular filtration rate (GFR) for each patient was calculated using the Bedside Schwartz Formula [20], and age-appropriate reference ranges for GFR were obtained from the literature [21]. All plasma ammonia levels obtained during admission (or prior to transfer to our tertiary care center if available) were recorded for each patient to determine peak ammonia, in addition to the plasma ammonia levels that coincided with admission and RRT initiation. Two patients (both non-survivors) had ammonia levels at time of RRT initiation that were reported as > 700 μmol/L. Two patients (both survivors) had ammonia levels only recorded at admission, RRT initiation, and discontinuation. Since the absolute maximum ammonia level of these 4 patients were unknown, these patients were excluded from analyses pertaining to peak ammonia levels. Patient survival was assessed at time of discharge and 18 months after hospital discharge. Redirection toward comfort care and transition to hospice care were considered as non-survival outcomes. Neurologic impairment was determined by review of medical records by medical providers. In our cohort, there were no patients lost to follow-up. Given that all patients who met our inclusion criteria were included and that no patients were lost to follow-up, all efforts to decrease sampling bias were completed.
Descriptive statistics are presented as medians with interquartile ranges. Continuous variables are compared with Mann-Whitney-Wilcoxon U tests for nonparametric data. Chi-squared test of independence is performed for the comparison of discrete variables with p values computed by “MASS” package in R using Pearson’s Chi-squared test [22]. Risk ratios and 95% confidence intervals are calculated in R using the “epitools” package [23]. All analyses were performed using RStudio (Boston, MA). Graphical representations of the data are created in R with the “ggplot2” package [24].
Results
There were 16 males (84%) and 3 females (16%) identified for inclusion in this study (hyperammonemia listed as indication for RRT with confirmed IEM [either UCD or OA]). The high prevalence of males in our cohort is reflective of X-linked ornithine transcarbamylase deficiency being the most common diagnosis within the group. There were a total of 15 patients with UCDs (ornithine transcarbamylase deficiency [n = 9], carbamoyl phosphate synthetase deficiency [n = 4], citrullinemia [n = 2]) and 4 patients with OAs (methylmalonic acidemia [n = 1], propionic acidemia [n = 3]). Ages of the patient cohort ranged from 2 days to 15.6 years, with a median age of 4 days (and reflects the majority of patients were in the neonatal age range). Peak plasma ammonia levels varied greatly from 164 to 3869 μmol/L with a median peak ammonia of 1035 μmol/L. Median plasma ammonia levels at admission and RRT initiation were 680 and 499 μmol/L, respectively. The majority of patients (16 of 19 patients, 84%) received nitrogen-scavenging medications (Ammonul [sodium phenylacetate and sodium benzoate]) or Carbaglu (carglumic acid). Thirteen patients (68%) received HD as their initial RRT modality and 6 patients (32%) received CRRT as the initial modality. Of the 12 patients who survived the initial course of HD, all were transitioned to CRRT. Of the 6 patients initially treated with CRRT, one required transitioning to HD due to worsening hyperammonemia. No patients received peritoneal dialysis.
Comparison of survivors and non-survivors are presented in Table 1, where non-survivors include both patients who died while receiving RRT and those patients whose families redirected care to comfort care and subsequently passed away. There were 9 survivors (47%) and 10 non-survivors (53%). The median age of survivors was 3 years (or 1103 days, age range from 3 days to 15.6 years). The median age of non-survivors was 3.5 days (age range from 2 days to 18.7 months) and was significantly less than the median age of survivors (p value = 0.0167). Peak plasma ammonia, ammonia at admission, and RRT initiation were all significantly higher in non-survivors compared with survivors. Median GFR on admission was lower in the non-survivors, but not statistically significant (28 vs 103 mL/min/1.73 m2, p value = 0.1307). Given the overall predominance of males in our cohort, there was no difference between sex in the survivors and non-survivors. There was no statistically significant difference between use of nitrogen-scavenging medications, RRT modality at initiation, and time to RRT initiation. All patients, who survived RRT treatment and who were not transitioned to hospice care, survived to hospital discharge and at 18 months. Of the 9 surviving patients, 2 were noted to have neurologic impairment (22% of survivors, 10% of total cohort). One organic acidemia patient had a metabolic stroke in late infancy that resulted in hypotonia and an inability to feed or walk. The other survivor with neurologic impairment had cognitive impairment. Of the 10 non-survivors, only 2 patients died while receiving RRT. Eight patients died after the family and medical teams had agreed to redirect goals of care to comfort care only. Comparison of survivors and non-survivors with UCD reveal the same trends as the overall patient cohort with non-survivors having younger age and significantly higher ammonia levels. Additionally, UCD non-survivors had a significantly shorter time from admission to RRT initiation (5.4 vs 26.2 h, p value = 0.0289). This likely reflects that non-survivors had higher ammonia levels compared with survivors who tended to be older, often established IEM patients who were admitted for intravenous nitrogen-scavenging medications and only required RRT after failing medical management.
Given that the majority of our patient cohorts (13 of 19 patients) were neonates presenting with their first hyperammonemic episode, we focused on specific differences between survivors and non-survivors in this group in Table 2. In addition to the parameters outlined in Table 1, we also compared complication rates within the neonatal patients. Four neonates (31%) had complications during RRT (2 had hypotension, 1 had a line malfunction, and 1 had hypotension, line malfunction, and multiple electrolyte disturbances). The rate of complications between survivors and non-survivors was not significantly different. Of the 6 older patients, one developed hypotension as a complication during CRRT. The statistically significant higher ammonia levels at admission, RRT initiation, overall peak ammonia in non-survivors seen in our overall cohort were also significantly higher in the neonatal non-survivors.
Prognostic factors that have been associated with poor outcomes were reviewed between survivors and non-survivors and are presented in Table 3. Several factors were associated with increased risk of non-survival. The term “non-survival” is meant to include patients who died during RRT as well as those who were transitioned to comfort care. Peak plasma ammonia levels greater than or equal to 750 μmol/L (RR 8.1, CI 1.3–52.0) and no change in ammonia from peak to initiation of RRT (RR = 2.8, CI = 1.3–6.0) had significantly higher risk ratios for non-survival compared with survivors. There was no statistically significant increased risk of non-survival for the following parameters: initiation of RRT within 6 h of admission, total duration of RRT ≥ 48 h, HD as the initial RRT modality, nitrogen-scavenging medications prior to RRT, vasopressor use prior to RRT, decreased GFR at admission, EEG performed during admission, or spiritual care involvement during the admission. There were nearly significant increased risk ratios for non-survival associated with head CT/brain MRI performed during admission (RR 2.2, CI 0.998–4.7) and receiving HD as the initial RRT modality for more than 8 h (RR 2.2, CI 0.998–4.7) as compared with those who received CRRT initially or those who were transitioned from HD to CRRT within the first 8 h of RRT. All non-survivors received vasopressors during RRT, which precluded calculation of risk ratio. While some of these clinical features are not prognostic factors per se, the occurrence of these features may be more common in non-survivors.
As highlighted in the demographic tables, there was a wide range of peak plasma ammonia level. The significant difference between the age and peak ammonia levels in our survivors and non-survivors is shown in Fig. 1 a. This plot also highlights that peak ammonia levels greater than 750 μmol/L were associated with non-survival. No survivor had an ammonia greater than 1250 μmol/L. Given that our patient cohort spanned a nearly 2 decades’ time frame, we evaluated the peak plasma ammonia levels and non-survival from 2000 to 2017 as shown in Fig. 1 b. It has recently been proposed that ammonia levels > 300 μmol/L after 12 h of RRT are associated with a worse prognosis [25]. Figure 1 c shows no significant difference in plasma ammonia levels at 8, 12, and 24 h into RRT between survivors and non-survivors. The distribution of patients who received HD as the initial RRT modality > 8 h, those who converted from HD to CRRT, and those that received CRRT as the initial RRT modality > 8 h, is shown in Fig. 1 d. As noted above, the risk ratio for non-survival in patients who received HD > 8 h was nearly significant (RR 2.2, CI 0.998–4.7).
Outcomes based on peak ammonia levels, age, date, and RRT modality. a Comparison of age of patient on x-axis and peak ammonia on y-axis. Triangles denote non-survivors and filled circles denote survivors. b Comparison of admission date on x-axis and peak ammonia on y-axis. c Comparison of response to RRT divided into two panels for survivors and non-survivors; duration of RRT on x-axis and response of ammonia levels on y-axis. Filled circles denote CRRT and filled triangle denote HD. Hashed lines denote a patient with a urea cycle disorder and filled lines denote an organic acidemia. d Bar chart of number of patients who received only HD for at least 8 h, who transitioned from HD to CRRT within 8 h, and those that received only CRRT. Filled bars denote non-survivors, open bars denote survivors
To provide visualization of the range of ammonia levels between survivors and non-survivors, boxplots depicting ranges of ammonia for each patient are plotted in Fig. 2. The percent of ammonia clearance at 8 h was not different between survivors and non-survivors (Fig. 2b). As shown in Table 1, the peak ammonia varied significantly between survivors and non-survivors (Fig. 2a, p value = 0.0021). However, the difference between peak ammonia and ammonia at admission as well as the difference between peak ammonia and ammonia at RRT initiation was not significantly different between survivors and non-survivors (Fig. 2c, d). As shown in Table 3, those patients who had no decrease in ammonia levels from peak to RRT initiation had a higher risk of non-survival compared with those who had a decrease from the peak ammonia to the ammonia collected at the start of RRT initiation.
Boxplots depicting range of ammonia levels for survivors and non-survivors. a Peak ammonia levels, b Percent of ammonia clearance from ammonia level at RRT initiation to 8 h of RRT, c Difference between peak ammonia level and ammonia at admission, d Difference between peak ammonia and ammonia at RRT initiation
Discussion
Here we present a retrospective analysis of patients with IEMs who received RRT for hyperammonemia from 2000 to 2017. Our patient cohort highlights that hyperammonemia affects two distinct patient populations; neonates with markedly elevated ammonia levels on initial presentation and established IEM patients as older children that develop much less severe hyperammonemia who only require RRT after failing medical management. Our experience over the past 17 years demonstrates no significant change in mortality associated with neonatal hyperammonemia, which remains significantly high at 50% despite improvements in RRT and intensive care. We identify several clinical features associated with non-survival including the well-recognized prognostic factor of peak ammonia [1, 5, 7, 12]. Further, we have identified that no change in ammonia between admission and initiation of RRT was a new risk factor for non-survival in our cohort. This finding is consistent with guidelines that RRT should be one component of efficacious management of hyperammonemia in addition to nitrogen-scavenging medications. It may also reflect that non-survivors may have genotypes associated with ammonia production that exceeds the beneficial effects of nitrogen-scavenging medications.
The overall mortality rate from our cohort was 53%, which is consistent with our institution’s previous cohort of patients who received RRT for hyperammonemia [10] almost two decades earlier. The mortality rate within our neonatal cohort was 69% compared to 17% of our older patients. There are several factors that contribute to differences in our mortality rate compared with other recent aggregated neonatal hyperammonemia cohorts [12]. The term “non-survival” is meant to include patients who died during RRT as well as those who were transitioned to comfort care. It should be noted that only 2 patients died while receiving RRT compared to the 8 other non-survivors whose families’ chose to redirect care toward comfort care only. Other published cohorts have not clearly documented whether mortality was a death that occurred while medical teams were attempting curative care compared to a death that occurred as a result of families choosing to redirect care toward comfort care. Factors involved in the decision to redirect care to comfort care only in these situations are usually anecdotal and warrant more systemic investigations. Other published cohorts with higher survival rates also have higher rates of neurologic disabilities [6, 12]. Our cohort only had 2 patients (10% of 19 total patients) with neurologic impairment. This suggests that neurologic outcomes are important considerations for families when determining goals of care. It also reflects our institution’s long-standing history of readiness and willingness to offer palliative care to our patient families.
Previous work has hypothesized that patients with higher trigger/peak ammonia levels are associated with poorer outcomes that would not be improved with RRT [12]. The recently updated guidelines for diagnosis and management of UCD now states that RRT should be started as soon as possible, unless initial medical treatment has already led to sufficient improvement of ammonia levels or based on other specifics of the clinical situation [17]. While there were certainly patients who did not survive or were diverted to comfort care in our cohort, nearly half of our patients survived with a relatively low level of neurocognitive disabilities suggesting that for those individuals, RRT had a powerfully beneficial outcome. Studies like ours and more extensive use of RRT registries for hyperammonemia management will help identify parameters in patients who are less likely to respond to RRT modalities. The degree of improvement in hyperammonemia with nitrogen-scavenging medications alone compared to the faster resolution of hyperammonemia with RRT remains a controversial question. Indeed, it remains unclear if RRT should be used as a last resort (only if nitrogen-scavenging medications have not significantly lowered the plasma ammonia level) or if RRT should be considered as an initial step in management of hyperammonemia while using nitrogen-scavenging medications concurrently and what specific level of hyperammonemia should prompt these decisions. Given recent advances in neonatal RRT, there is reasonable argument for using RRT as a first-line treatment for hyperammonemia in conjunction with nitrogen-scavenging medications.
The data presented has several limitations. Our cohort included only patients who received RRT, which means our patient cohort represents a small patient population with severe hyperammonemia that could not be managed with nitrogen-scavenging medications alone. This study does not include patients with milder hyperammonemia that are admitted and managed with nitrogen scavenger therapy only. Our patient cohort focused on patients receiving RRT for management of hyperammonemia and was identified through dialysis registry records and identification of patients, especially prior to electronic medical records who had severe hyperammonemia and were not treated with dialysis is not known. Over the course of our study period, our institution implemented clinical practice guidelines recommending when RRT should be initiated and which RRT modality should be used based on plasma ammonia levels. This may have skewed our cohort to receiving HD more frequently as the initial RRT modality based on plasma ammonia levels > 500 μmol/L. OTC deficiency is the most common urea cycle disorder and often represents the most common inborn error of metabolism requiring RRT for management of severe hyperammonemia. The poor prognosis associated with OTC deficiency is directly related to ease of management of associated hyperammonemia. Over the course of our study period, molecular testing became far more prevalent. Future studies of hyperammonemia in IEMs, particularly in UCDs, may find genotype-phenotype relationships between specific pathogenic variants and degree of hyperammonemia. The work presented here and in combination with other publications highlights the need for a large, multi-site review of hyperammonemia outcomes in neonates to determine optimal RRT strategies to rapidly decrease plasma ammonia levels while minimizing complications.
Conclusion
In the future, we may see that high-dose CRRT provides better outcomes for RRT given that the logistics and support needs are often easier to coordinate newer equipment that is equally effective in decreasing ammonia levels compared to HD. Additionally as newer devices with lower extracorporeal blood volumes and smaller vascular access requirements become available, shorter times from presentation to RRT initiation may be associated with better outcomes. The management of hyperammonemia in the older pediatric patients in our cohort and other published cohorts reflects that current management strategies are largely successful. However, there are significant improvements to be made in the management and outcomes of neonatal hyperammonemia given the high morbidity and mortality associated with hyperammonemia that has not significantly changed in the two decades since our institution’s previous publication [10] despite improvements in RRT technology and critical care medicine. Additional therapeutic interventions may also focus on earlier detection of hyperammonemia at presumably lower, more readily treatable ammonia levels. Earlier detection may be possible by adding OTC deficiency to the Recommended Uniform Screening Panel with tandem mass spectrometry measurement of orotic acid [26, 27] and EMR alerts to prompt providers to order plasma ammonia levels in patients presenting with neonatal sepsis [28]. As a tertiary center, many of our patients were initially evaluated at referring hospitals. Our data suggests that providing referring hospitals with appropriate hyperammonemia management guidelines and decreasing ammonia levels prior to initiation of RRT is critical for positive outcomes. We believe that the cohort presented here is a valid representation of outcomes in severe hyperammonemia requiring RRT. It also emphasizes the importance of ongoing research to improve these outcomes.
Data availability
The data presented in this submission is available upon request after de-identification beginning 3 months and ending 5 years following article publication. Proposals should be directed to corresponding author. To gain access, data requestors will need to sign a data access agreement and provide a methodologically sound proposal.
Abbreviations
- RRT:
-
Renal replacement therapy
- PD:
-
Peritoneal dialysis
- HD:
-
Hemodialysis
- CRRT:
-
Continuous renal replacement therapy
- IEM:
-
Inborn error of metabolism
- UCD:
-
Urea cycle disorder
- OA:
-
Organic acidemia
- GFR:
-
Glomerular filtration rate
References
Bachmann C (2003) Outcome and survival of 88 patients with urea cycle disorders: a retrospective evaluation. Eur J Pediatr 162(6):410–416
Nassogne MC, Héron B, Touati G, Rabier D, Saudubray JM (2005) Urea cycle defects: management and outcome. J Inherit Metab Dis 28(3):407–414
Msall M, Batshaw M, Suss R, Brusilow S, Mellits ED (1984) Neurologic outcome in children with inborn error of urea synthesis. N Engl J Med 310:1500–1505
Maestri NE, Hauser ER, Bartholomew D, Brusilow SW (1991) Prospective treatment of urea cycle disorders. J Pediatr 119(6):923–928
Unsinn C, Das A, Valayannopoulos V, Thimm E, Beblo S, Burlina A et al (2016) Clinical course of 63 patients with neonatal onset urea cycle disorders in the years 2001-2013. Orphanet J Rare Dis 11(1):1–11
Burgard P, Kölker S, Haege G, Lindner M, Hoffmann GF (2016) Neonatal mortality and outcome at the end of the first year of life in early onset urea cycle disorders—review and meta-analysis of observational studies published over more than 35 years. J Inherit Metab Dis 39(2):219–229
Kido J, Nakamura K, Mitsubuchi H, Ohura T, Takayanagi M, Matsuo M et al (2012) Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis 35(5):777–785
Krivitzky L, Babikian T, Lee HS, Thomas NH, Burk-Paull KLBM (2009) Intellectual, adaptive, and behavioral functioning in children with urea cycle disorders. Pediatr Res 66(1):96–101
Surtees RA, Matthews EE, Leonard JV (1992) Neurologic outcome of propionic acidemia. Pediatr Neurol 8(5):333–337
McBryde KD, Kershaw DB, Bunchman TE, Maxvold NJ, Mottes TA, Kudelka TL et al (2006) Renal replacement therapy in the treatment of confirmed or suspected inborn errors of metabolism. J Pediatr 148(6):770–778
Picca S, Dionisi-Vici C, Abeni D, Pastore A, Rizzo C, Orzalesi M et al (2001) Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatr Nephrol 16(11):862–867
Hediger N, Landolt MA, Diez-Fernandez C, Huemer M, Häberle J (2018) The impact of ammonia levels and dialysis on outcome in 202 patients with neonatal onset urea cycle disorders. J Inherit Metab Dis 41(4):689–698
Donn SM, Swartz RD, Thoene JG (1979) Comparison of exchange transfusion, peritoneal dialysis, and hemodialysis for the treatment of hyperammonemia in an anuric newborn infant. J Pediatr 95(1):67–70
Wong KY, Wong SN, Lam SY, Tam S, Tsoi NS (1998) Ammonia clearance by peritoneal dialysis and continuous arteriovenous hemodiafiltration. Pediatr Nephrol 12(7):589–591
Picca S, Dionisi-Vici C, Bartuli A, De Palo T, Papadia F, Montini G et al (2015) Short-term survival of hyperammonemic neonates treated with dialysis. Pediatr Nephrol 30(5)
Pela I, Seracini D, Donati MA, Lavoratti G, Pasquini E, Materassi M (2008) Peritoneal dialysis in neonates with inborn errors of metabolism: is it really out of date? Pediatr Nephrol 23(1):163–168
Häberle J, Burlina A, Chakrapani A, Dixon M, Karall D, Lindner M et al (2019) Suggested guidelines for the diagnosis and management of urea cycle disorders: first revision. J Inherit Metab Dis 42(6):1192–1230
Cho H (2019) Renal replacement therapy in neonates with an inborn error of metabolism. Korean J Pediatr 62(2):43–47
Demirkol D, Aktuğlu Zeybek Ç, Karacabey BN, Cesur Y, Ataman Y, Soysal E (2019) The role of supportive treatment in the management of hyperammonemia in neonates and infants. Blood Purif:1–8
Schwartz GJ, Haycock GB, Edelmann CM, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics. 58(2):259–263
Su SW, Stonestreet BS (2010) Core concepts: neonatal glomerular filtration rate. Neoreviews. 11(12):e714–e721
Ripley B, Venables B, Bates D, Hornik K, Gebhardt A, Firth D. MASS: Modern Applied Statistics with S [Internet]. R package version 3.5.1. 2019. Available from: https://cran.r-project.org/package=MASS
Aragon T, Fay M, Wollschlaeger D, Omidpanah A. Epitools: Epidemiology Tools [Internet]. R package version 3.5.1. 2017. Available from: https://cran.r-project.org/package=epitools
Wickham H, Chang W, Henry L, Pedersen T, Takahashi K, Wilke C, et al. ggplot2: Create elegant data visualisations using the grammar of graphics [Internet]. R package version 3.5.1. 2019. Available from: https://cran.r-project.org/package=ggplot2
Porta F, Peruzzi L, Bonaudo R, Pieretti S, Busso M, Cocchi E et al (2018) Differential response to renal replacement therapy in neonatal-onset inborn errors of metabolism. Nephrol. 23(10):957–961
Held PK, Haynes CA, De Jesús VR, Baker MW (2014) Development of an assay to simultaneously measure orotic acid, amino acids, and acylcarnitines in dried blood spots. Clin Chim Acta 436:149–154
Janzen N, Terhardt M, Sander S, Demirkol M, Gökçay G, Peter M et al (2014) Towards newborn screening for ornithine transcarbamylase deficiency: fast non-chromatographic orotic acid quantification from dried blood spots by tandem mass spectrometry. Clin Chim Acta 430:28–32
Vergano SA, Crossette JM, Cusick FC, Desai BR, Deardorff MA, Sondheimer N (2013) Improving surveillance for hyperammonemia in the newborn. Mol Genet Metab 110(1–2):102–105
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest for the authors.
Prior presentation of data
Subsets of the data reported in this manuscript have been presented at annual meetings of the Pediatric Academic Society in 2015 and the American College of Medical Genetics in 2018.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ames, E.G., Luckritz, K.E. & Ahmad, A. A retrospective review of outcomes in the treatment of hyperammonemia with renal replacement therapy due to inborn errors of metabolism. Pediatr Nephrol 35, 1761–1769 (2020). https://doi.org/10.1007/s00467-020-04533-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04533-3