Abstract
Hydrocephalus in tuberculous meningitis (TBM) could be obstructive, communicating, or due to combinations of obstructive and communicating variety. Endoscopic third ventriculostomy (ETV) is an established management option for obstructive hydrocephalus in chronic phase. ETV in TBM hydrocephalus could be a demanding surgical procedure especially in acute stage secondary to opaque, thick, and inflamed third ventricle floor. Water-jet dissection is indicated in such patients, while blunt perforation is preferred in thin and transparent third ventricle floor. Intraoperative Doppler or neuronavigation can help in proper planning of the perforation and to prevent neurovascular complications. Choroid plexus coagulation along with ETV could improve success rate especially in infants. Results of ETV are superior in good grade as compared to poor grade. Poor results are described in patients with thick and opaque third ventricle floor, cisternal exudates, malnourished cases, and in acute phase as compared to patients with thin and transparent floor, without cisternal exudates, well-nourished cases, and in chronic phase, respectively. Some of the patients especially in poor grade could show delayed recovery. Failure to improve after surgical procedure could be due to stoma block, complex hydrocephalus, vascular compromise, and in poor grade. Postoperative high intracranial pressure (ICP) has been observed following ETV. Repeated lumbar puncture/external ventricular drainage could help in faster normalization of the ICP after ETV in patients with temporary defect in cerebrospinal fluid absorption, while lumbar peritoneal shunt is required in permanent defect. Repeat ETV is recommended if the stoma is blocked.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Cerebrospinal fluid shunts
- Endoscopic surgical procedure
- Hydrocephalus
- Neuroendoscopy
- Tuberculous meningitis
1 Introduction
Tuberculous meningitis (TBM) involves infection in the lung, regional lymph nodes, and meninges or brain parenchyma. There is development of subpial or subependymal foci of lesions, called Rich foci, which rupture into the subarachnoid space or ventricle. It continues to remain great public health challenge especially in developing world. TBM remains a diagnostic dilemma. There is a need for high index of clinical suspicion and better diagnostic tests for early detection of disease. Cerebrospinal fluid (CSF) studies for detection of organism or biochemical examination helps in diagnosis. CSF centrifugation optimizes the diagnostic performance [1]. The existence of high density within the basal cisterns in non-contrast computed tomography (CT) and basal enhancement after contrast administration is a good sign for the diagnosis of TBM [2]. Polymerase chain reaction (PCR) can be an efficient method for diagnosis of TBM [3]. Presence of tuberculoma on choroid plexus or ventricle wall, though rare, may help in diagnosis [4].
Hydrocephalus is very common in TBM [5,6,7]. Early diagnosis of TBM hydrocephalus should be done by early follow-up CT scan (in first 7 days of first CT scan and at 1 month on one’s discretion) [8]. Hydrocephalus can be categorized as obstructive, communicating, or due to union of both varieties [9]. Effective and early treatment of hydrocephalus can improve prognosis and decrease incidence of infarct. Shunt procedures and endoscopic third ventriculostomy (ETV) are being used to manage hydrocephalus in TBM. Endoscopic techniques are increasingly used in spine [10,11,12,13,14], cranial [15, 16], and skull base lesions [17,18,19,20] in recent times due to the minimally invasive nature, safety, and better outcome. Endoscopic procedures are being used in various types of pathologies such as hematomas [21, 22], congenital lesions [23,24,25], infective pathologies [26, 27], and tumors [28,29,30] with encouraging results.
Although role of ETV is controversial in communicating hydrocephalus and in acute phase of disease, its role is established as an alternative to shunt procedures for obstructive hydrocephalus in TBM [31,32,33,34,35,36,37,38,39,40,41,42,43]. Comparatively poor results of hydrocephalus due to TBM stress the need for early diagnosis and prompt treatment. Although many factors are related to final outcome, clinical stage of disease at diagnosis and presence of hydrocephalus play an important role in prognosis.
2 Indications of Endoscopic Third Ventriculostomy
Although hydrocephalus in early stages of TBM with mild ventriculomegaly may resolve completely in some cases, especially of communicating variety [7], majority of them need some kind of surgery. Modified external ventricular drainage (EVD) and Ommaya reservoir implantation of about 2 weeks can avoid possible complications and long-term indwelling shunt in majority (66%) of patients in early TBM who have mild or moderate hydrocephalus [44, 45].
ETV is indicated in obstructive hydrocephalus in TBM. Although there are reports of ETV being performed in communicating hydrocephalus [35], lumbar peritoneal shunts have been found to be better option in such cases [46, 47]. Selected patients of communicating hydrocephalus with inferior bulging of third ventricle floor or anterior bulging of lamina terminalis can show improvement after ETV. This procedure of ETV not only relieves raised pressure in TBM hydrocephalus (38) but it also helps in making correct diagnosis in suspected cases by detecting tubercles on the wall of the ventricle during surgery. Endoscopy is now treated as the first choice compared to shunt surgery in TBM hydrocephalus especially in chronic stage of disease [40].
Although there was some doubts whether shunt should be done in severe form of TBM hydrocephalus, there are now reports that all patients should be treated with shunts even in poor grades [48,49,50]. Likewise ETV is also indicated in good as well as in poor grades in TBM as some patients in poor grades could show delayed recovery [36, 39]. Although ETV can be done in the presence of thick exudates and even in patients with prepontine suprasellar tuberculoma especially in expert hands [51], it should be avoided in the acute stage especially in untreated patients [31, 52], because of variable success [5]. ETV in subacute and chronic cases looks to be a rationale for first-line treatment [31, 34, 39, 43, 53].
EVD or Ommaya reservoir after ETV may be useful when there is evidence of doubtful functioning of stoma (poor pulsations at stoma margin, exudates in basal cistern, acute phase of TBM, evidence of intraventricular bleed, multiple shunt failure, poor flow of dye across stoma, and poor disappearance of contrast) or cisternal scarring. Intraoperative decision about shunt surgery is indicated in technically difficult case due to thick and inflamed floor with poor differentiation of anatomy, cisternal scarring, poor pulsations of stoma margin, poor flow of dye across stoma, and delayed clearance of contrast from the basal cisterns.
3 Preoperative Workup and Patient Selection
Patients undergoing ETV in TBM hydrocephalus should have sufficiently large lateral or third ventricles and enlarged foramen of Monro to accommodate endoscopic set; otherwise, it could cause injury to ventricle walls or the fornix. It is important to know whether third ventricle floor is thin or thick. Thin third ventricle floor patients are good candidates for ETV, surgery is comparatively simple technically, and the ETV success rate is also good in such cases. Good prepontine space and the absence of basal exudate also favor ETV. There should be sufficient space between brain stem and dorsum sellae and also between basilar artery and dorsum sellae. The distance between midline and posterior communicating artery or third cranial nerve should be known, as small distance predisposes artery or nerve injury during procedure. Presence of large interthalamic adhesions can also create difficulty during the procedure. Although one can observe the presence of any additional membrane such as Liliequist membrane or other membranes after fenestration of third ventricle floor and such membrane can be dealt appropriately intraoperatively, preoperative knowledge prepares surgeon to deal it better. Liliequist membrane if present may be attached to the third nerve, which can risk nerve injury during fenestration. Cistern status is also a critical factor in patient outcome; scarred basal cistern not only adds in the technical difficulty during surgery but also associated with poor outcome.
Patent distal subarachnoid spaces and proper CSF absorption are also necessary for good outcome after ETV. Although it is challenging to measure lumbar outflow resistance preoperatively in a patient requiring ETV, low lumbar outflow resistance suggests good CSF absorption and patent subarachnoid space. Increased outflow resistance could be due to compression of subarachnoid space secondary to dilated ventricle, obliterated subarachnoid space, and/or defective CSF absorption. Although low lumbar outflow resistance generally suggests favorable subarachnoid space, good CSF absorption, and good outcome after ETV, high resistance may not be associated with poor outcome. High resistance could also be due to compression of subarachnoid space secondary to dilated ventricles.
Complex hydrocephalus (combination of both obstructive and communicating hydrocephalus) is quite common in TBM cases [9, 39]. This is due to obliterated basal cisterns or subarachnoid space and/or defective CSF absorption. Cine phase-contrast (PC) magnetic resonance imaging (MRI) can be used for detection of any abnormality in basal cisterns. Detection of early CSF stroke volume in interpeduncular and prepontine cisterns can predict patency of basal cisterns and CSF flow through these cisterns. Good CSF flows in basal cistern alone do not give surety of successful outcome following ETV; distal CSF pathways ahead of the basal cisterns also play crucial role in ETV successfulness [54].
4 Surgical Procedure
TBM hydrocephalus is technically demanding to manage endoscopically as compared to other types and needs good skill and training, especially in acute cases [31, 55]. ETV procedure has been depicted elsewhere in our publication [56]. Although semi-sitting position has been described, ETV is generally operated in supine position with head flexed so that the burr hole site is at the uppermost point. Highest site of burr hole averts excessive drainage of CSF and an entrance of air in the ventricles and subdural space, especially in large ventricles. Although ETV can be done free hand without using any telescope holder, use of scope holder is helpful when procedure is prolonged and during introduction and removal of instruments. It can also give rest to the hand, which is holding the assembly. Telescope holder can be tightened or loosened when required. We used holder in a loose knob position during most of the procedure. Assistant is supporting the holder at tightening knob area and near the joint regions to allow better control and to decrease strain on the hand of the surgeon which is holding endoscope assembly (Fig. 30.1). Excessive drainage of CSF may also precipitate for postoperative subdural hematoma formation. Lateral and third ventricle along with foramen of Monro should be sufficiently large. If there is a slit ventricle secondary to overdrainage in already shunted patient, it is necessary to externalize the shunt to adequately dilate ventricles. Stereotactic guidance along with smaller size of the scope or flexible scope can be used in such patients. Although ETV can be done by flexible scope, we use rigid scope because of better visualization.
Training lab photographs showing (a) assistant supporting joints of telescope holder with loosened knob, which prevents strain on surgeon’s hand. It also prevents time loss in loosening or tightening. (b) Left hand of surgeon holding endoscope sheath while well-supported right hand being used for surgical maneuver. (c) Camera can be supported by body part
A line spanning from interpeduncular cistern and foramen of Monro onto the cranium in preoperative MRI scan accurately determines an exact site of burr hole. Incision just in front to the coronal suture and approximately 2.5–3 cm lateral to the midline on the right side is usually adequate for ETV. Proper direction of brain penetration should be used to reach lateral ventricle at foramen of Monro. Although facility of image guidance can help, marking on the skin near the incision in the direction toward external auditory meatus before patient is draped helps when image guidance facility is not available (Fig. 30.2). Brain cannula is used to perforate ventricle, and then endoscope protected by the sheath is introduced. Peel-away sheath of slightly larger diameter than the endoscope is generally used if the scope does not have sheath. Some systems have sheaths with scope; in such cases peel-away sheath is not required. Peel-away sheath or other sheath avoids lens soiling and brain injury due to repeated scope introduction. It also helps in egress of irrigation fluid and avoids pressure built up. Lactate solution irrigation of normal body temperature implying gravity pressure as against to any pressure procedure is good which avoids any barotraumas to the brain.
Telescope is introduced through the foramen of Monro into the third ventricle after identification of junction of thalamostriate vein, septal vein, and choroid plexus. Perforation in the third ventricle floor is made between mammillary bodies and infundibular recess, at the most translucent site. Identification of basilar artery should be done to avoid trauma and hemorrhage during the procedure. Perforation should be done anterior to the basilar artery or its branches. Trajectory in ETV in sagittal and coronal plane using rigid scope should be properly planned to avoid fornix injury (Fig. 30.3). Although slow and gentle movement up to about 5 mm has been found to be safe [57], such movements generally should be desisted to avoid fornix injury. If working channel is not opposite to the desired site of interest in the floor of third ventricle, rotation of assembly in desired direction should be done (Fig. 30.4). Microvascular Doppler probe could be effective to see basilar artery and its subdivisions if these structures are not visualized endoscopically. Disciplined probing with the round equipment, if the facility of Doppler is not accessible, can identify position of dorsum sellae. Water-jet dissection approach can be utilized to avoid vascular injury or hemorrhage in thick and opaque third ventricle floor [32, 58]. Fenestration in thin third ventricle floor is just behind the dorsum sellae, and in front of basilar artery while in thick floor, it should be made partly on dorsum sellae and partly just posterior to dorsum sellae. Perforation on the bony part in thick floor prevents stretch of third ventricle wall and related complications. Such stretch in already bulging third ventricle wall can cause third cranial nerve injury apart from bleeding from distant site. Blunt instruments should be used preferably to fenestrate third ventricle floor to prevent vascular injury. Although we do not prefer thermal coagulation especially in thin floor, initial use of low bipolar current helps in making fenestration in thick floor and also to avoid excessive stretch on floor. Original perforation is enlarged to about 5 mm or more size by utilizing Fogarty catheter or ventriculostomy forceps. Liliequist membrane or other membrane can be found in some cases, lying below the third ventricle floor. Such membrane should be perforated under endoscopic control. Septum pellucidum perforation along with ETV could be technically difficult as the proper trajectory for ETV and septum perforation is different in coronal plane (Fig. 30.5). Using gentle bipolar coagulation and grasping forceps with one limb side opening can make ETV and septum perforation possible by single trajectory (Fig. 30.6). All the procedure should be done under constant visualization; if any part of the instrument is not seen, it is either due to very high magnification, scope too close to target area, or when scope and the two limbs of instrument are in straight line. Decreasing magnification, slight withdrawal of scope away from target area, and rotation of instrument in such a way that the scope and the two limbs of instrument make triangular orientation allow proper visualization (Fig. 30.7).
Showing (a) correct trajectory in ETV in coronal plane as medial as possible to reach third ventricle floor in midline using rigid scope. (b) Wrong lateral trajectory and (c) entry through contralateral foramen of Monro risking unilateral and bilateral fornix injury, respectively. (d) Correct trajectory in sagittal plane to reach third ventricle floor in between mammillary bodies and infundibular recess. Wrong (e) anterior and (f) posterior trajectory risking fornix injury
Nonvisualization of instrument is due to very high magnification, (a) scope too close to target area, or (b) when scope and the two limbs of instrument are in straight line. Decreasing magnification, (c) slight withdrawal of scope away from target area, and (d) rotation of instrument in such a way that the scope and the two limbs of instrument make triangular orientation allow proper visualization
Good pulsations of stoma margin are a good indicator of stoma opening and cisternal status. If there is any doubt about the patency of stoma or basal cisterns after ETV during surgery, an intraoperative evaluation by ventriculo-stomography can provide valuable information [59]. Contrast flow through the stoma and its disappearance from subarachnoid spaces can be observed. Fast disappearance of contrast is a good indicator of stoma and cisternal patency. This simple and effective method can help in verifying the competency of endoscopic approach, thereby helping in taking decision about further management during surgery, such as requirement for shunt if there is slow disappearance of contrast [59, 60].
ETV is likely to be effective if there is favorable anatomy of third ventricle floor, good pulsations of stoma margins, and good basal cistern without any exudates or scarring. If there is any doubt about stoma or cisternal patency due to not so good stoma pulsations or slow disappearance of dye during intraoperative period, EVD or Ommaya reservoir can be kept which can be used to assess stoma patency in postoperative period. An EVD is also left if there is any small bleeding during procedure. Although some researchers practice use of reservoir routinely, it is useful in certain high-risk patients [61,62,63] for ETV failure with poor stoma pulsations, patients with repeated shunt malfunctions, cisternal scarring, and acute phase of disease if one opt for ETV. Intraoperative decision of shunt placement can be taken if there is unfavorable third ventricle floor anatomy increasing risk of ETV, other technical difficulties due to thick floor, abnormally enlarged interthalamic adhesions, inflamed floor, poor stoma pulsations, prolonged hold of dye in cistern, etc. (Fig. 30.8).
Intraoperative decision of shunt placement can be taken if there is unfavorable third ventricle floor anatomy increasing risk of ETV, other technical difficulties due to thick floor, abnormally enlarged interthalamic adhesions, inflamed floor, poor stoma pulsations, prolonged hold of dye in cistern, poor visualization of third ventricle floor, etc.
Choroid plexus coagulation can improve success rate of ETV especially in infants. Any hemorrhage from cortical surface should be stopped by electrocautery. If there is any bleeding from perforation margin, instrument used for fenestration (Fogarty catheter or ventriculostomy forceps) should be used for tamponade effect. It is not desirable to remove that instrument and bring cautery to stop that bleeding point (by the time cautery forceps is brought near the point, visualization of bleeding point may become difficult). Intermittent closure of outflow channel could help in visualization of bleeding point.
ETV after slit ventricle syndrome in TBM hydrocephalus could be challenging. It is difficult to hit small ventricle; the use of small flexible scope, stereotactic guidance using small scope, dilatation of ventricle by exteriorization, and blockage of shunt tube can be used to help ETV procedure. Endoscopic lamina terminalis fenestration as an alternative site of perforation has been described for treatment of hydrocephalus in TBM when the usual site in third ventricle floor is not favorable for perforation [64]. Endoscopic subfrontal approach to the lamina terminalis fenestration has also been described in cadavers by Spena et al. [65].
4.1 Results of ETV
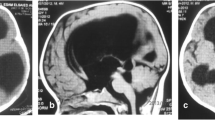
Overall, clinical improvement after ETV alone ranges from 58% to 80% in various series [34, 36, 39, 40, 66]. We reported 58% improvement after ETV alone that improved to 80% when lumbar peritoneal shunt was added [39]. Outcome after ETV is superior in without cisternal exudate patients compared to those with exudates [34, 39]. Good nutritional status patients generally have better outcome compared to poor nutritional status patients [39]. ETV is reasonably effective and safe in full-term normal birth weight infants as compared to low birth weight premature infants [39]. Thin and identifiable third ventricle floor patients have better outcome after ETV as compared to thick and opaque floor (Fig. 30.9) [39, 67]. Although age did not make any difference in clinical outcome in most studies [33, 68], adult patients could fair slightly well compared to children [39]. Outcome is superior in better grade compared to patients in poor grade [34, 39].
Majority of patients show early improvement [36, 39]; delayed improvement is also observed. Patients in superior grades generally improve early as compared to poor grade who show delayed recovery [39]. Outcome after ETV in the chronic phase is superior compared to acute phase [39, 69]. Poor results in acute phase is due to higher incidence of complex hydrocephalus compared to chronic stage [39] which is among significant factor as causes of failure to improve after ETV.
Outcome of ETV in TBM hydrocephalus is poor compared to aqueductal stenosis secondary to congenital cause. The comparatively poor outcome after ETV in TBM compared to aqueductal stenosis is secondary to high prevalence of complex hydrocephalus [9, 39]. The obliteration of CSF pathways and defective absorption of CSF from arachnoid villi can result in persistently elevated intracranial pressure (ICP) in TBM after ETV. Faulty absorption and/or obliteration of CSF pathways in complex hydrocephalus can be temporary or permanent [9]. Most of the patients have temporary defect of absorption, and these patients can be managed by repeated lumbar puncture after ETV before labeling them as failed ETV patients [39, 70]. Repeated lumbar puncture supports by augmenting compliance, improving buffering capacities of the spinal subarachnoid spaces, and decreasing the CSF outflow resistance from the ventricular system. It also promotes reduction in the ventricular volume and allows accelerated permeation of CSF in the intracranial subarachnoid spaces. The chances of complex hydrocephalus in acute phase of disease are more as compared to chronic phase [39]. It is therefore better to do shunt surgery and avoid ETV in acute phase of the disease [31].
The advanced age, neurological status at admission, vaccine status, ischemia, etc. determine prognosis [71]. BCG vaccination might be protective from advance disease as most patients who were vaccinated were seen in early stage of TBM disease [72].
4.2 Radiological Outcome
The size of ventricle does not reduce in 3 weeks in about 50% individuals [39]. There may not be any interrelationship between clinical and radiological recovery. Clinical recovery is earlier than the radiological recovery in most patients. In some individuals there may be clinical recovery without any radiological recovery. On the other hand, there may be radiological recovery without any clinical recovery, in few patients, mainly due to associated ischemic infarcts.
4.3 Causes of Failure to Improve After ETV and Its Management
There can be many causes of failure to improve after ETV such as block stoma, ischemia, complex hydrocephalus, advanced age, poor neurological status at the time of surgery, etc. (Fig. 30.10). Deterioration after ETV does not always imply that the ETV is not working. Stoma patency does not always suggest that the ETV is efficient in decreasing ICP. Complex hydrocephalus is one of the significant causes of failure to improve after surgery. Complex hydrocephalus could be due to temporary or permanent defect in the CSF dynamics. Repeated lumbar puncture can manage temporary defect in CSF dynamic abnormality, while lumbar peritoneal shunt could be required when there is a persistently raised ICP even after repeated lumbar puncture. One should be very careful in selecting lumbar peritoneal shunt surgery in TB as there may be associated TB compression at various levels in the spine [73,74,75,76,77,78]. Repeat ETV is required to treat blocked stoma.
4.4 Complications and Its Avoidance
Although endoscopic techniques are having many advantages, procedure could be associated with many limitations. Such complications should be anticipated to improve results [79, 80]. Although ETV procedure is fairly simple, learning curve of the procedure can be improved by microsurgical skills training, practice on cadaver or models, watching expert surgeons, and visiting other departments [81].
ETV technique could be associated with various complications such as hypothermia or disturbance in temperature regulation, intraventricular bleeding, pneumocephalus, bradycardia, fornix injury, hypothalamic injury, cranial nerve injury, failed ETV, endoscopic blind spot, delayed awakening, block stoma, subdural hematoma, intracerebral hemorrhage, CSF leak, chronic subdural hematoma or subdural hygroma, etc. Although rare, mortalities due to fatal hemorrhage have been reported. Details of these complications are described in Table 30.1 and in our earlier publications [79, 80].
Fornix injury is an important complication in ETV, which should be prevented (Figs. 30.2 and 30.3). Brain injury and bleeding from brain parenchyma or ependymal margin can occur if direction of trajectory toward foramen of Monro is not proper and surgeon tries to enter foramen of Monro by moving the scope (Fig. 30.11). Stroke occurs in about 45% of individuals in TBM both in early and later stage, mainly in the region of basal ganglia. Risk of infarct is high when there is hydrocephalus in TBM [6]. Infarcts are considered to be associated with the involvement of medial striate, thalamotuberal, and thalamostriate arteries that are present in exudates, which are prone to be strained by a coexisting hydrocephalus [82]. Infarct predicts poor outcome at 3 months [83]. Brain ischemia in TBM hydrocephalus is due to vasculitis and raised pressure secondary to hydrocephalus. Ideal management of raised ICP is necessary for improved outcome rather than simply preventing maximum increase in pressure [42].
Showing (a) proper, (b) wrong anterior, and (c) wrong posterior direction of brain penetration to reach foramen of Monro. Brain injury and bleeding from brain parenchyma or ependymal margin can occur if direction of trajectory is not proper and surgeon tries to move from A position of wrong trajectory to B position to reach foramen of Monro
5 Postoperative Imaging and Diagnosis of Stoma Patency
Majority of patients who improve after surgery do not need any investigation. Failure to improve after this surgical procedure can be secondary to the raised ICP (stoma blockage or complex hydrocephalus), vascular compromise, and poor preoperative neurological status. The raised ICP in the early postoperative period could be related to complex hydrocephalus, which could be temporary or permanent.
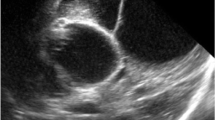
Decrease in the size of the ventricular edema, decrease of periventricular edema, and widening of subarachnoid space after ETV are indirect evidences of stoma patency. These responses continue during the initial few months after ETV. The decrease in size is more marked in acute stage of hydrocephalus and in third ventricle width compared to lateral ventricle width. CSF flow as the flow-void sign could be qualitatively described. This is not very sensitive, as a flow-void sign has been seen in up to 50% of clinical failures. Cine PC MRI could be helpful even in no flow-void situation. This cine PC magnetic resonance (MR) may be helpful in determining the stoma patency and could be of value in follow-up [84]. Three-dimensional constructive interference in steady state (CISS) MR technique has been found to be sensitive to flow [85, 86]. MR ventriculography is useful in determining stoma patency after third ventriculostomy [35]. Ventriculography is helpful in providing accurate assessment of the stoma patency in the early days after surgery if EVD or Ommaya was kept during ETV. It also allows intermittent CSF drainage to relieve raised ICP.
Conclusion
The choice about the best management should be decided by many factors such as surgeon’s expertise, stage and duration of disease, communicating or noncommunicating hydrocephalus, availability of resources for endoscopy, etc. Although most of the patients with hydrocephalus need surgical treatment, small-group patients in early and acute stage with mild hydrocephalus in neurologically intact and in fully conscious state can be observed with early repeat CT scans. Ventriculoperitoneal shunt is a better option in acute phase of TBM hydrocephalus in obstructive hydrocephalus, while ETV is an effective alternative in obstructed hydrocephalus in subacute or chronic phase (Fig. 30.12). Results of lumbar peritoneal shunt are better in communicating hydrocephalus.
Abbreviations
- CISS:
-
Constructive interference in steady state
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- ETV:
-
Endoscopic third ventriculostomy
- EVD:
-
External ventricular drainage
- ICP:
-
Intracranial pressure
- MR:
-
Magnetic resonance
- MRI:
-
Magnetic resonance imaging
- PC:
-
Phase contrast
- PCR:
-
Polymerase chain reaction
- TBM:
-
Tuberculous meningitis
References
Bahr NC, Tugume L, Rajasingham R, Kiggundu R, Williams DA, Morawski B, Alland D, Meya DB, Rhein J, Boulware DR (2015) Improved diagnostic sensitivity for tuberculous meningitis with Xpert(®) MTB/RIF of centrifuged CSF. Int J Tuberc Lung Dis 19:1209–1215
Andronikou S, Smith B, Hatherhill M, Douis H, Wilmshurst J (2004) Definitive neuroradiological diagnostic features of tuberculous meningitis in children. Pediatr Radiol 34:876–885
Nagdev KJ, Bhagchandani SP, Bhullar SS, Kapgate RC, Kashyap RS, Chandak NH, Daginawala HF, Purohit HJ, Taori GM (2015) Rapid diagnosis and simultaneous identification of tuberculous and bacterial meningitis by a newly developed duplex polymerase chain reaction. Indian J Microbiol 55:213–218
Bhattacharyya A, Boruah DK, Handique A, Singh V, Kalita J, Misra UK, Vishnu Phadke RV (2010) Involvement of the choroid plexus in neurotuberculosis: MR findings in six cases. Neuroradiol J 23:590–595
Rajshekhar V (2009) Management of hydrocephalus in patients with tuberculous meningitis. Neurol India 57:368–374
Chan KH, Cheung RT, Fong CY, Tsang KL, Mak W, Ho SL (2003) Clinical relevance of hydrocephalus as a presenting feature of tuberculous meningitis. QJM 96:643–648
Raut T, Garg RK, Jain A, Verma R, Singh MK, Malhotra HS, Kohli N, Parihar A (2013) Hydrocephalus in tuberculous meningitis: incidence, its predictive factors and impact on the prognosis. J Infect 66:330–337
Andronikou S, Wieselthaler N, Smith B, Douis H, Fieggen AG, van Toorn R, Wilmshurst J (2005) Value of early follow-up CT in paediatric tuberculous meningitis. Pediatr Radiol 35:1092–1099
Yadav YR, Mukerji G, Parihar V, Sinha M, Pandey S (2009) Complex hydrocephalus (combination of communicating and obstructive type): an important cause of failed endoscopic third ventriculostomy. BMC Res Notes 2:137
Yadav YR, Parihar V, Namdev H, Agarwal M, Bhatele PR (2013) Endoscopic inter laminar management of lumbar disc disease. J Neurol Surg A Cent Eur Neurosurg 74:77–81
Yadav YR, Parihar V, Kher Y, Bhatele PR (2016) Endoscopic inter laminar management of lumbar disease. Asian J Neurosurg 11:1–7
Yadav YR, Parihar V, Ratre S, Kher Y (2014) Endoscopic anterior decompression in cervical disc disease. Neurol India 62:417–422
Yadav YR, Parihar V, Ratre S, Kher Y, Bhatele P (2014) Endoscopic decompression of cervical spondylotic myelopathy using posterior approach. Neurol India 62:640–645
Yadav YR, Yadav N, Parihar V, Kher Y, Ratre S (2013) Endoscopic posterior decompression of lumbar canal stenosis. Indian J Neurosurg 2:124–130
Yadav YR, Parihar V, Bhatele P (2013) Endoscopic treatment of arachnoid cyst. In: Veerendra Kumar, Mukta Bhatele (eds) Lecture notes in bioengineering 2013. Proceedings of All India Seminar on Biomedical Engineering 2012 (AISOBE 2012). Springer, New Delhi, pp 29–35.
Yadav YR, Parihar V, Pande S, Namdev H (2014) Endoscopic management of colloid cysts. J Neurol Surg A Cent Eur Neurosurg 75:376–380
Yadav YR, Parihar V, Agarwal M, Sherekar S, Bhatele PR (2011) Endoscopic vascular decompression of the trigeminal nerve. Minim Invasive Neurosurg 54:110–114
Yadav YR, Sachdev S, Parihar V, Namdev H, Bhatele PR (2012) Endoscopic endonasal trans-sphenoid surgery of pituitary adenoma. J Neurosci Rural Pract 3:328–337
Yadav YR, Madhariya SN, Parihar VS, Namdev H, Bhatele PR (2013) Endoscopic transoral excision of odontoid process in irreducible atlantoaxial dislocation: our experience of 34 patients. J Neurol Surg A Cent Eur Neurosurg 74:162–167
Yadav YR, Parihar V, Janakiram N, Pande S, Bajaj J, Namdev H (2016) Endoscopic management of cerebro-spinal fluid rhinorrhea. Asian J Neurosurg 11:183–193
Yadav YR, Yadav S, Sherekar S, Parihar V (2011) A new minimally invasive tubular brain retractor system for surgery of deep intracerebral hematoma. Neurol India 59:74–77
Yadav YR, Mukerji G, Shenoy R, Basoor A, Jain G, Nelson A (2007) Endoscopic management of hypertensive intraventricular haemorrhage with obstructive hydrocephalus. BMC Neurol 7:1
Yadav YR, Parihar V, Sinha M, Jain N (2010) Endoscopic treatment of supra sellar arachnoid cyst. Neurol India 58:280–282
Yadav YR, Basoor A, Todorov M, Parihar V (2010) Endoscopic management of large multi compartmental intraventricular arachnoid cyst extending from foramen magnum to foramen monro: case repot and review of literature. Neurol India 58:481–484
Yadav YR, Shenoy R, Mukerji G, Sherekar S, Parihar V (2010) Endoscopic transoral excision of odontoid process in irreducible atlanto-axial dislocation. In: Deepu Banerji, Apoorva Pauranik (ed) Progress in clinical neurosciences, vol 24. Byword Books Private Limited and Neurological society of India, New Delhi. pp 159–169
Gajdhar M, Yadav YR (2005) A case of thalamic abscess treated by endoscopic surgery. Neurol India 53:345–346
Yadav YR, Sinha M, Neha PV (2008) Endoscopic management of brain abscesses. Neurol India 56:13–16
Yadav YR, Yadav N, Parihar V, Khare Y, Ratre S (2015) Management of colloid cyst of third ventricle. Turk Neurosurg 25:362–371
Yadav YR, Nishtha Y, Vijay P, Shailendra R, Yatin K (2015) Endoscopic endonasal trans-sphenoid management of craniopharyngiomas. Asian J Neurosurg 10:10–16
Yadav YR, Bhagwat A, Agarwal M, Parihar V, Chandrakar S, Jain N (2011) Endoscopic treatment of neurocytoma of lateral ventricle: case report and review of literature. Chirurgia 24:173–176
Bhagwati S, Mehta N, Shah S (2010) Use of endoscopic third ventriculostomy in hydrocephalus of tubercular origin. Childs Nerv Syst 26:1675–1682
Yadav YR, Shenoy R, Mukerji G, Parihar V (2010) Water jet dissection technique for endoscopic third ventriculostomy minimizes the risk of bleeding and neurological complications in obstructive hydrocephalus with a thick and opaque third ventricle floor. Minim Invasive Neurosurg 53:155–158
Yadav YR, Jaiswal S, Adam N, Basoor A, Jain G (2006) Endoscopic third ventriculostomy in infants. Neurol India 54:161–163
Chugh A, Husain M, Gupta RK, Ojha BK, Chandra A, Rastogi M (2009) Surgical outcome of tuberculous meningitis hydrocephalus treated by endoscopic third ventriculostomy: prognostic factors and postoperative neuroimaging for functional assessment of ventriculostomy. J Neurosurg Pediatr 3:371–377
Singh I, Haris M, Husain M, Husain N, Rastogi M, Gupta RK (2008) Role of endoscopic third ventriculostomy in patients with communicating hydrocephalus: an evaluation by MR ventriculography. Neurosurg Rev 31:319–325
Singh D, Sachdev V, Singh AK, Sinha S (2005) Endoscopic third ventriculostomy in post-tubercular meningitis hydrocephalus: a preliminary report. Minim Invasive Neurosurg 48:47–52
Jonathan A, Rajshekhar V (2005) Endoscopic third ventriculostomy for chronic hydrocephalus after tuberculous meningitis. Surg Neurol 63:32–34
Figaji AA, Fieggen AG, Peter JC (2003) Endoscopic third ventriculostomy in tuberculous meningitis. Childs Nerv Syst 19:217–225
Yadav YR, Parihar V, Agrawal M, Bhatele PR (2011) Endoscopic third ventriculostomy in tubercular meningitis with hydrocephalus. Neurol India 59:855–860
Husain M, Jha DK, Rastogi M, Husain N, Gupta RK (2005) Role of neuroendoscopy in the management of patients with tuberculous meningitis hydrocephalus. Neurosurg Rev 28:278–283
Tandon V, Mahapatra AK (2011) Management of post-tubercular hydrocephalus. Childs Nerv Syst 27:1699–1707
Figaji AA, Fieggen AG (2013) Endoscopic challenges and applications in tuberculous meningitis. World Neurosurg 79(2 Suppl):S24. e9–14
Yadav YR, Parihar VS, Todorov M, Kher Y, Chaurasia ID, Pande S, Namdev HRole of endoscopic third ventriculostomy in tuberculous meningitis with hydrocephalus. Asian J Neurosurg. doi:10.4103/1793-5482.145100
Lin J, Zhang N, Sheng HS, Yin B, Wang HO, Wang MD (2011) Role of modified external ventricular drainage in the management of children with tuberculous meningitis hydrocephalus. Zhonghua Yi Xue Za Zhi 91:2488–2490
Lin J, Zhou H, Zhang N, Yin B, Sheng HS (2012) Effects of the implantation of Ommaya reservoir in children with tuberculous meningitis hydrocephalus: a preliminary study. Childs Nerv Syst 28:1003–1008
Yadav YR, Parihar V, Sinha M (2010) Lumbar peritoneal shunt. Neurol India 58:179–184
Yadav YR, Pande S, Raina VK, Singh M (2004) Lumboperitoneal shunts: review of 409 cases. Neurol India 52:188–190
Savardekar A, Chatterji D, Singhi S, Mohindra S, Gupta S, Chhabra R (2013) The role of ventriculoperitoneal shunt placement in patients of tubercular meningitis with hydrocephalus in poor neurological grade: a prospective study in the pediatric population and review of literature. Childs Nerv Syst 29:719–725
Peng J, Deng X, He F, Omran A, Zhang C, Yin F, Liu J (2012) Role of ventriculoperitoneal shunt surgery in grade IV tubercular meningitis with hydrocephalus. Childs Nerv Syst 28:209–215
Srikantha U, Morab JV, Sastry S, Abraham R, Balasubramaniam A, Somanna S, Devi I, Bangalore CA, Pandey P (2009) Outcome of ventriculoperitoneal shunt placement in Grade IV tubercular meningitis with hydrocephalus: a retrospective analysis in 95 patients. Clinical article. J Neurosurg Pediatr 4:176–183
Jha D, Khatri P, Choudhary A, Sethi R, Kumar S (2007) Endoscopic third ventriculostomy in prepontine-suprasellar tuberculoma with tuberculous meningitis hydrocephalus: a case report. Pediatr Neurosurg 43:42–46
Misra UK, Kalita J, Prabhakar S, Chakravarty A, Kochar D, Nair PP (2012) Endoscopic third ventriculostomy in tuberculous meningitis needs more evidence. Ann Indian Acad Neurol 15:233
Rajshekhar V (2015) Surgery for brain tuberculosis: a review. Acta Neurochir 157:1665–1678
Di X, Ragab M, Luciano MG (2009) Cine phase-contrast MR images failed to predict clinical outcome following ETV. Can J Neurol Sci 36:643–647
Figaji AA, Fieggen AG, Peter JC (2007) Endoscopy for tuberculous hydrocephalus. Childs Nerv Syst 23:79–84
Yadav YR, Parihar V, Pande S, Namdev H, Agarwal M (2012) Endoscopic third ventriculostomy. J Neurosci Rural Pract 3:163–173
Zhu XL, Gao R, Wong GK, Wong HT, Ng RY, Yu Y, Wong RK, Poon WS (2013) Single burr hole rigid endoscopic third ventriculostomy and endoscopic tumor biopsy: what is the safe displacement range for the foramen of Monro? Asian J Surg 36:74–82
Oertel J, Gen M, Krauss JK, Zumkeller M, Gaab MR (2006) The use of waterjet dissection in endoscopic neurosurgery. Technical note. J Neurosurg 105:928–931
Husain M, Singh DK, Rastogi M, Ojha BK, Chandra A, Gupta RK (2010) Intraoperative ventriculo-stomographic evaluation of endoscopic cerebrospinal fluid diversion and flow restoration procedures. Br J Neurosurg 24:672–678
Singh D, Gupta V, Goyal A, Singh H, Sinha S, Singh AK, Kumar S (2003) Endoscopic third ventriculostomy in obstructed hydrocephalus. Neurol India 51:39–42
Kumar A, Deopujari CE, Biyani N (2011) Utility of ventricular access in an acute deterioration after endoscopic third ventriculostomy. J Postgrad Med 57:123–125
Parikh D, Foroughi M, Nannapaneni R, Hatfield RH (2009) Is the routine placement of a CSF reservoir following endoscopic third ventriculostomy justified? Br J Neurosurg 23:521–523
Xiao B, Roth J, Udayakumaran S, Beni-Adani L, Constantini S (2011) Placement of Ommaya reservoir following endoscopic third ventriculostomy in pediatric hydrocephalic patients: a critical reappraisal. Childs Nerv Syst 27:749–755
Nakao N, Itakura T (2003) Endoscopic lamina terminalis fenestration for treatment of hydrocephalus due to tuberculous meningitis. Case illustration. J Neurosurg 99:187
Spena G, Fasel J, Nd T, Radovanovic I (2008) Subfrontal endoscopic fenestration of lamina terminalis: an anatomical study. Minim Invasive Neurosurg 51:319–323
ul Haq MI, Khan SA, Raja RA, Ahmed E (2012) Efficacy of endoscopic third ventriculostomy in non-communicating hydrocephalus. J Ayub Med Coll Abbottabad 24:144–146
Jha DK, Mishra V, Choudhary A, Khatri P, Tiwari R, Sural A, Kumar S (2007) Factors affecting the outcome of neuroendoscopy in patients with tuberculous meningitis hydrocephalus: a preliminary study. Surg Neurol 68:35–41
Tjemme B, Grotenhuis AJ (2002) Is the success rate of endoscopic age dependent? An analysis of the results of endoscopic third ventriculostomy in young children. Childs Nerv Syst 18:605–608
Kumar A, Singh K, Sharma V (2013) Surgery in hydrocephalus of tubercular origin: challenges and management. Acta Neurochir 155:869–873
Cinalli G, Spennato P, Ruggiero C, Aliberti F, Zerah M, Trischitta V, Cianciulli E, Maggi G (2006) Intracranial pressure monitoring and lumbar puncture after endoscopic third ventriculostomy in children. Neurosurgery 58:126–136
Gu J, Xiao H, Wu F, Ge Y, Ma J, Sun W (2015) Prognostic factors of tuberculous meningitis: a single-center study. Int J Clin Exp Med 8:4487–4493
Güneş A, Uluca Ü, Aktar F, Konca Ç, Şen V, Ece A, Hoşoğlu S, Taş MA, Gürkan F (2015) Clinical, radiological and laboratory findings in 185 children with tuberculous meningitis at a single centre and relationship with the stage of the disease. Ital J Pediatr 41:75
Turgut M, Özcan OE, Özgen T, Bertan V (1993) Intradural extramedullary tuberculoma of the spinal cord -a case report. Zentralbl Neurochir 54:197–199
Turgut M (1997) Pott’s disease. J Neurosurg 87:136–138
Turgut M (1997) Intradural tuberculous granuloma. Br J Neurosurg 11:264–266
Turgut M (2001) Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev 24:8–13
Turgut M (2001) Multifocal extensive spinal tuberculosis (Pott’s disease) involving cervical, thoracic and lumbar vertebrae. Br J Neurosurg 15:142–146
Turgut M, Özcan OE, Özgen T, Sağlam S, Bertan V, Erbengi A (1989) Tuberculomas of the craniospinal axis. Turk Neurosurg 1:34–38
Yadav YR, Parihar V, Kher Y (2013) Complication avoidance and its management in endoscopic neurosurgery. Neurol India 61:217–225
Yadav YR, Parihar V, Ratre S, Kher Y (2015) Avoiding complications in endoscopic third ventriculostomy. J Neurol Surg A Cent Eur Neurosurg 76:483–494
Yadav YR, Parihar V, Ratre S, Iqbal M (2016) Microneurosurgical skills training. J Neurol Surg A Cent Eur Neurosurg 77:146–154
Misra UK, Kalita J, Maurya PK (2011) Stroke in tuberculous meningitis. J Neurol Sci 303:22–30
Kalita J, Misra UK, Nair PP (2009) Predictors of stroke and its significance in the outcome of tuberculous meningitis. J Stroke Cerebrovasc Dis 18:251–258
Faggin R, Calderone M, Denaro L, Meneghini L, d’Avella D (2011) Long-term operative failure of endoscopic third ventriculostomy in pediatric patients: the role of cine phase-contrast MR imaging. Neurosurg Focus 30:E1
Doll A, Christmann D, Kehrli P, Abu Eid M, Gillis C, Bogorin A, Thiebaut A, Dietemann JL (2000) Contribution of 3D CISS MRI for pre and posttherapeutic monitoring of obstructive hydrocephalus. J Neuroradiol 27:218–225
Kurihara N, Takahashi S, Tamura H, Higano S, Furuta S, Jokura H, Umetsu A (2000) Investigation of hydrocephalus with three dimensional constructive interference in steady state MRI. Neuroradiology 42:634–638
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Yadav, Y.R., Yadav, N., Parihar, V., Ratre, S., Bajaj, J. (2017). Role of Endoscopic Third Ventriculostomy in Tuberculous Meningitis with Hydrocephalus. In: Turgut, M., Akhaddar, A., Turgut, A., Garg, R. (eds) Tuberculosis of the Central Nervous System. Springer, Cham. https://doi.org/10.1007/978-3-319-50712-5_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-50712-5_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-50711-8
Online ISBN: 978-3-319-50712-5
eBook Packages: MedicineMedicine (R0)