Abstract
Purpose
Endoscopic third ventriculostomy (ETV) has become standard for obstructive hydrocephalus. Even a successful ETV can obstruct, leading to recurrence of symptoms and even death. A possible solution to this problem is leaving an Ommaya reservoir (OR) following the ETV. OR can be tapped in an emergency and for diagnostic purposes. No specific complications have been attributed to OR in this setting. We present our experience with OR in children undergoing ETV for hydrocephalus.
Materials and methods
A retrospective study was conducted in hydrocephalic children that underwent ETV with OR insertion over 13 years (1997–2010) from a single institution. Data were collected from charts and follow-ups.
Results
Twelve patients (from 200 patients who had an ETV) underwent placement of OR with ETV. OR was reserved for a subgroup of patients in whom we anticipated complications—in children that presented with acute hydrocephalus and were in deteriorating condition, for pathologies believed to have a low predicted ETV success rate, or when the surgeon felt that the ETV procedure was suboptimal. OR was tapped in eight patients. Complications occurred in four patients: two cases of subdural effusion, one case of chronic subdural hematoma, and one CSF leak. Four ORs were removed due to complications, and four were converted to shunts.
Conclusions
OR should be considered in selected patients undergoing ETV. Despite its obvious advantages, OR may be associated with a relatively high risk of extraaxial fluid collections. This association requires further investigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoscopic third ventriculostomy (ETV) is an effective procedure for treating obstructive hydrocephalus in selected patients. Long-term success following ETV in “classic” patients has been well documented [9].
In recent years, neurosurgeons have been trying to further push the envelope of “classic” indications and attempt ETV in patients at a higher risk of failure. In addition, cases of acute deterioration and even death have been documented as late complications following ETV [6, 10]. These life-threatening events may be secondary to acute obstruction of the stoma in the third ventricular floor [22, 25].
The possible advantages of placing an Ommaya reservoir (OR) for potential future urgent access have been discussed previously [1, 12, 17]. Such a device may also provide easy access for tapping, pressure measurement, and other diagnostic purposes when the clinical picture is not sufficient to come to a decision for a specific patient. The use of OR in this context is considered safe.
In the current series, we describe our experience with placing OR in selected cases undergoing ETV. We focus on the indications for OR, its usage, complications, and value in the pediatric population.
Patients and methods
Over a period of 13 years (1997–2010), over 200 pediatric ETVs were performed at the Dana Children's Hospital in Tel Aviv, Israel [19]. An OR system was placed in 12 pediatric patients. Data regarding these patients were collected retrospectively, including: demographics, hydrocephalus history (etiology, symptoms, and previous treatment), indications for ETV, indications for OR, operative notes, postoperative course, and long-term follow-up.
Surgical procedure
Surgical procedures were performed under general anesthesia. Entry burr holes were placed at the precoronal midpupillary point. ETVs were carried out using either a 6.2-mm Minop® rigid endoscope (Aesculap, Inc., Center Valley, PA, USA) with a 19-F peel-away, or a 4.8-mm Karl Storz rigid endoscope (Karl Storz GmbH & Co., Tuttlingen, Germany) with a 15-F peel-away. The third ventricular floor was perforated bluntly with a monopolar probe followed by enlargement with either endoscopic forceps, or using the optics themselves. Following the ETV, a ventricular catheter was placed through the peel-away into the lateral ventricle and connected to a 12-mm Side-Inlet Ommaya® reservoir (Integra NeuroSciences, Plainsboro, NJ, USA). All patients were followed regularly in our clinic with ongoing neurological, ophthalmological, and imaging exams.
We defined ETV success as resolution of the preoperative hydrocephalic-related symptoms as well as no subsequent surgical procedures required to treat the hydrocephalus during the follow-up period.
Statistics
Data were tabulated in an Excel spreadsheet, and basic statistics (mean, standard deviation) were calculated.
Results
Twelve patients (6 male, 6 female) were included in this series. Ages at ETV with OR were between 2 months to 15 years (mean, 4.3 years). All patients had an obstruction at the level of the third or fourth ventricular outlet. Primary hydrocephalus etiologies included: congenital aqueductal stenosis (3 patients), postintraventricular hemorrhage (IVH; 3 patients), aqueductal stenosis associated with neurofibramotosis-1 (NF-1; 2 patients), and one patient each with postmeningitis, Dandy–Walker malformation, myelomeningocele (MM), and a thalamic tumor (Table 1). Four patients presented with a ventriculoperitoneal (VP) shunt malfunction, and three had a previous ETV that failed.
Indications for OR placement
OR placement was planned in advance in ten cases and decided during surgery in two. OR insertion was not a routine procedure, and indications were not rigidly predefined. Rather, the senior surgeon decided, based on clinical instincts. Indications for planned OR placement included:
-
1.
As a safety measure in cases that presented with acute hydrocephalus in a deteriorating condition
-
2.
Anatomical reasons such as in cases of shunt malfunction with relatively small ventricles
-
3.
Cases in which the surgeon estimated the probable success rate of ETV to be relatively poor, including those with post-IVH, postmeningitis, post-MM, repeat ETV, and for a thalamic tumor-related hydrocephalus in which the tumor was suspected of having the future potential to occlude the ETV
In two cases, the placement of OR was decided during the surgery due to the surgeon's assessment of the ETV as suboptimal. In one case, which was post-IVH, multiple intraventricular adhesions were found in addition to mild intraventricular bleeding during the ETV. In the other case, a distorted prepontine anatomy was revealed during surgery. Table 1 summarizes the various OR placement indications.
Usage of the Ommaya reservoir
Fifteen OR-tapping instances were documented in eight out of 12 patients (66.7%). Fourteen events (93.3%) occurred during the first 2 weeks following surgery.
-
1.
Twelve OR taps (80.0%) were for ICP measurement in five patients (cases 1, 4, 6, 10, and 11), in whom increased ICP was suspected. These taps were performed during the first 2 weeks after the ETVs. ICP measurements were marginal (14–20 cm H2O) and led to the performance of lumbar punctures (LP) or CSF aspiration through OR.
-
2.
One prophylactic CSF aspiration through OR was performed on the 11th postoperative day due to subcutaneous fluid collection that threatened the surgical wound (case 3).
-
3.
Two urgent OR taps were performed in two patients, one (case 12) on the third postoperative day and the other (case 7) 3 months after surgery. Both patients presented with acute severe headaches, vomiting, and lethargy. OR taps revealed elevated ICP in both. Urgent CSF aspiration was performed to relieve the elevated pressure, and both cases were followed by shunting.
Complications
There were no infections and no permanent morbidity. Table 2 summarizes complications and outcomes in these patients. There were a total of four complications in this study.
-
1.
Two patients (cases 1 and 10) developed ipsilateral subdural effusions 18 and 9 days after surgery (Fig. 1). The effusion was drained, and the OR was removed in both. Eventually, these two patients underwent placement of a shunt at a later stage (one patient with subduro-peritoneal, the other with VP).
-
2.
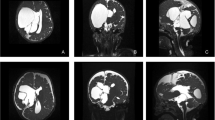
One patient (case 9; Fig. 2) developed a late ipsilateral, chronic, subdural hematoma following a contralateral VP shunt insertion. The blood was drained, and the OR was removed.
-
3.
One child (case 3) suffered from a large subcutaneous CSF collection in the wound site. Unfortunately, attempts to protect the wound by two LPs and one CSF aspiration through OR failed, and a CSF leak appeared 2 weeks after the ETV. This patient was ultimately treated with a new VP shunt and OR removal.
Axial images obtained in case 9. Images 1, 2, and 3 (CT) were taken at postoperative day 1. Images 4, 5, and 6 (MRI flair) were taken 1 month post-ETV and show a slight dilatation of the left ventricle, resulting in the placement of a left occipital shunt; there was no subdural hematoma at that time. Images 7, 8, and 9 (CT) were taken 2 months after shunting and reveal the appearance of an ipsilateral chronic subdural hematoma (white arrows)
When comparing the patients who developed OR-related complications to the others, we did not find any specific risk factors such as younger age, number of OR taps, CSF volume drained, or original size of ventricles.
ETV outcome
Over a follow-up period of 5 months to 13 years (mean; 4.1 years), ETV with OR insertion was successful only in four out of 12 patients (33.3%). In cases which failed, time to failure (as measured from time of ETV with OR placement to the following surgery) ranged from 3 days to 3 months (mean, 25 ± 22 days).
In four patients with complications, OR, including the ventricular catheter, was completely removed. Three of these four patients (cases 1, 3, and 10) needed a shunt, eventually. In another four patients (cases 4, 7, 11, and 12), the OR system was converted to a shunt by removing the reservoir and connecting the proximal catheter to a shunt valve with distal tubing, subsequent to ETV failure.
Discussion
ETV has become a standard treatment for obstructive hydrocephalus, with 70–90% long-term success rate when performed for hydrocephalus secondary to aqueductal stenosis amongst children older than 2 years of age [9]. The main advantages of ETV, compared to standard shunting, are establishing physiological CSF absorption, preventing from hardware implantation, and avoiding shunt-related complications.
Despite the advantages of ETV, several shortcomings do exist, e.g., some pathologies are associated with a lower success rate. An extreme example is, although rare, that acute ETV failure may occur even years after the procedure, resulting in some cases with sudden death [6, 10]. Several authors have suggested routine placement of OR in every ETV procedure as a safety measure, providing an easy access port if an acute deterioration occurs [1, 12, 16]. In a letter to the editor responding to such a suggestion, the senior author of the current series (S. Constantini) advocated against routine placement of OR during ETV, as it increases the infectious risk, requires more financial costs, and compromises the core rationale of ETV—namely, avoiding implantation of a foreign body [4].
Indications for OR placement
With this in mind, we have, in recent years, opted to place OR only in selected patients undergoing ETV. Although not strictly adhered to, the general indications for OR placement included four subgroups:
-
1.
Hydrocephalus secondary to causes presumed to be associated with a lower ETV success rate. For example, posthemorrhagic and postinfectious hydrocephalus have been shown to only have a 60–65% success rate [23, 26]. Similarly, in infants [20], fourth ventricle outlet obstruction [14], hydrocephalus secondary to MM [24, 26], and the Dandy–Walker syndrome [3, 13, 15] are all associated with a lower success rate of ETV. In addition, ETV for treating obstructive hydrocephalus secondary to lesions in the third ventricular wall includes a risk of later obstruction by a growing tumor.
-
2.
Patients presenting with acute shunt malfunction with mild to moderate ventricular enlargement. These patients potentially pose a more urgent clinical deteriorating process once ETV fails, as they typically have poor cerebral compliance.
-
3.
Patients with contraindications for lumbar taps (such as post-MM or deep Chiari malformation). In these patients, OR serves as an alternative, offering the only immediate access to CSF.
-
4.
Patients with anatomical abnormalities (many times associated with MM), such as thickened third ventricular floor and intraventricular or prepontine adhesions [8, 18]. ETV may be more technically challenging in these patients and is associated with a higher failure rate.
OR placement in these subgroups offers several advantages: prompt access to the ventricles in cases with acute deterioration attributed to ETV failure, a port for CSF analysis and intracranial pressure measurement when evaluating patients suspected of elevated ICP, and safely and easily connecting the ventricular catheter with a valve and distal shunt system when subsequent shunting is required.
Complications associated with OR
Three cases (25%) in this current series had subdural fluid collections ipsilateral to OR. All were drained, and OR was removed. Subdural effusions and chronic subdural hematomas have rarely been described following ETV without OR [2, 7] and have not been previously described in series placing routine OR either [1, 16, 17]. The reason for the relatively high rate of extraaxial fluid collections among the current series is unclear. A few possible mechanisms may contribute to this finding: young age, a relatively thin cortical mantle, large volume tapping, and a persistent tract along the catheter. As our described group is small and heterogeneous, it is impossible to come to a conclusion about the exact mechanism. However, this finding raises the need for awareness and screening imaging following ETV and OR placement.
OR insertion may increase the risk of wound breakdown and CSF leak. In our series, one case had wound dehiscence and CSF leak 2 weeks postoperatively, resulting in shunt implantation.
There were no infectious or migration complications associated with OR in this series. Generally, infections associated with OR may be treated in situ without removal of OR [11, 21]. Even if OR is removed, there should be no impact on internal CSF drainage pathways, although the infection itself may lead to an ETV failure. OR migration is a rare complication. Fukuhara reported a case with reservoir migration into the lateral ventricle through the endoscopic tract after a failed ETV [5]. Although these OR complications have been documented, their occurrence seems to be extremely low.
Limitations
The current study has several limitations. In addition to the retrospective nature, the study group was small and heterogeneous, and there was no consistent pattern of indications for OR placement.
This study is not sufficient to draw clear conclusions as to whether a routine use of OR is justified, especially when balanced against the potential complications. However, we believe that in selected cases, an OR should be considered in the same setting as the ETV.
Summary
OR placement is advocated for a small subset of patients undergoing ETV. This includes patients with pathologies linked to a relatively high ETV failure rate and patients with suspected low cerebral compliance presenting in an acute deteriorating condition. Other indications may include intraoperative considerations such as a nonideal anatomy and a suboptimal ETV. Despite its obvious advantages, OR may also be associated with a relatively high complication rate, mainly, extraaxial fluid collections. Surgeons performing ETV and leaving OR are encouraged to perform an early postoperative imaging study to demonstrate these collections.
References
Aquilina K, Edwards RJ, Pople IK (2003) Routine placement of a ventricular reservoir at endoscopic third ventriculostomy. Neurosurgery 53:91–96, discussion 96-97
Beni-Adani L, Siomin V, Segev Y, Beni S, Constantini S (2000) Increasing chronic subdural hematoma after endoscopic III ventriculostomy. Childs Nerv Syst 16:402–405
Buxton N, Macarthur D, Mallucci C, Punt J, Vloeberghs M (1998) Neuroendoscopic third ventriculostomy in patients less than 1 year old. Pediatr Neurosurg 29:73–76
Constantini S, Siomin V (2005) Re: death after late failure of endoscopic third ventriculostomy: a potential solution. Neurosurgery 56:E629
Fukuhara T, Namba Y, Kuyama H (2004) Ventricular reservoir migration into the lateral ventricle through the endoscopic tract after unsuccessful third ventriculostomy. Pediatr Neurosurg 40:186–189
Hader WJ, Drake J, Cochrane D, Sparrow O, Johnson ES, Kestle J (2002) Death after late failure of third ventriculostomy in children. Report of three cases. J Neurosurg 97:211–215
Kamel MH, Murphy M, Aquilina K, Marks C (2006) Subdural haemorrhage following endoscopic third ventriculostomy. A rare complication. Acta Neurochir (Wien) 148:591–593
Kawamura T, Morioka T, Nishio S, Mihara F, Fukui M (2001) Cerebral abnormalities in lumbosacral neural tube closure defect: MR imaging evaluation. Childs Nerv Syst 17:405–410
Kulkarni AV, Drake JM, Mallucci CL, Sgouros S, Roth J, Constantini S (2009) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus. J Pediatr 155(254–259):e251
Lipina R, Palecek T, Reguli S, Kovarova M (2007) Death in consequence of late failure of endoscopic third ventriculostomy. Childs Nerv Syst 23:815–819
Mechleb B, Khater F, Eid A, David G, Moorman JP (2003) Late onset Ommaya reservoir infection due to Staphylococcus aureus: case report and review of Ommaya infections. J Infect 46:196–198
Mobbs RJ, Vonau M, Davies MA (2003) Death after late failure of endoscopic third ventriculostomy: a potential solution. Neurosurgery 53:384–385, discussion 385-386
Mohanty A, Biswas A, Satish S, Praharaj SS, Sastry KV (2006) Treatment options for Dandy-Walker malformation. J Neurosurg 105:348–356
Mohanty A, Biswas A, Satish S, Vollmer DG (2008) Efficacy of endoscopic third ventriculostomy in fourth ventricular outlet obstruction. Neurosurgery 63:905–913, Discussion, 913–914
O'Brien DF, Seghedoni A, Collins DR, Hayhurst C, Mallucci CL (2006) Is there an indication for ETV in young infants in aetiologies other than isolated aqueduct stenosis? Childs Nerv Syst 22:1565–1572
Parikh D, Foroughi M, Nannapaneni R, Hatfield RH (2009) Is the routine placement of a CSF reservoir following endoscopic third ventriculostomy justified? Br J Neurosurg 23:521–523
Paola P, Paola R, Christian FC, Pierpaolo G, Giuseppe C (2007) The role of Ommaya reservoir and endoscopic third ventriculostomy in the management of post-hemorrhagic hydrocephalus of prematurity. Childs Nerv Syst 23:765–771
Pavez A, Salazar C, Rivera R, Contreras J, Orellana A, Guzman C, Iribarren O, Hernandez H, Elzo J, Moraga D (2006) Description of endoscopic ventricular anatomy in myelomeningocele. Minim Invasive Neurosurg 49:161–167
Roth J, Bo X, Beni-Adani L, Elran H, Constantini S (2007) Endoscopic third ventriculostomy–a physiological alternative to shunts as treatment for obstructive hydrocephalus in children. Harefuah 146(660–665):735
Sgouros S, Kulkharni AV, Constantini S (2006) The international infant hydrocephalus study: concept and rational. Childs Nerv Syst 22:338–345
Siegal T, Pfeffer MR, Steiner I (1988) Antibiotic therapy for infected Ommaya reservoir systems. Neurosurgery 22:97–100
Siomin V, Weiner H, Wisoff J, Cinalli G, Pierre-Kahn A, Saint-Rose C, Abbott R, Elran H, Beni-Adani L, Ouaknine G, Constantini S (2001) Repeat endoscopic third ventriculostomy: is it worth trying? Childs Nerv Syst 17:551–555
Siomin V, Cinalli G, Grotenhuis A, Golash A, Oi S, Kothbauer K, Weiner H, Roth J, Beni-Adani L, Pierre-Kahn A, Takahashi Y, Mallucci C, Abbott R, Wisoff J, Constantini S (2002) Endoscopic third ventriculostomy in patients with cerebrospinal fluid infection and/or hemorrhage. J Neurosurg 97:519–524
Teo C, Jones R (1996) Management of hydrocephalus by endoscopic third ventriculostomy in patients with myelomeningocele. Pediatr Neurosurg 25:57–63, discussion 63
Wagner W, Koch D (2005) Mechanisms of failure after endoscopic third ventriculostomy in young infants. J Neurosurg 103:43–49
Warf BC (2005) Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. J Neurosurg 102:1–15
Author information
Authors and Affiliations
Corresponding author
Additional information
Bo Xiao and Jonathan Roth have contributed equally.
Rights and permissions
About this article
Cite this article
Xiao, B., Roth, J., Udayakumaran, S. et al. Placement of Ommaya reservoir following endoscopic third ventriculostomy in pediatric hydrocephalic patients: a critical reappraisal. Childs Nerv Syst 27, 749–755 (2011). https://doi.org/10.1007/s00381-010-1371-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1371-z