Abstract
The treatment of hydrocephalus has changed in recent years with better imaging and introduction of endoscopic procedures as well as enhanced shunts. Indications of endoscopic third ventriculostomy (ETV) are now more refined with better quantification of outcome. This article reviews the current state of neuroendoscopy for infective hydrocephalus in children. The roles of third ventriculostomy as a primary procedure or after shunt malfunction, endoscopic interventions in multiloculated hydrocephalus and introduction of intraventricular lavage to salvage severely infected children are evaluated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoscopic third ventriculostomy (ETV) has been controversial for post-infective hydrocephalus (PIHC). Post-infectious aetiology is a low score criterion in ETV Success Score (ESS) [25]. This seems logical due to the scarring of subarachnoid spaces and arachnoid villi with subsequent defective absorption leading to communicating hydrocephalus in most of these cases. Shunts have, therefore, been traditionally used as a primary surgical treatment for this variety of hydrocephalus. The favourable Ugandan experience [51] with endoscopy, however, has prompted many workers to revisit this indication, and we now have a better understanding of ETV as a primary procedure or after shunt failure. The addition of choroid plexus coagulation (CPC) has improved the outcome of ETV in some reports [50].
An unquestionable additional benefit of endoscopy is to open up CSF pathways in complex, often multiloculated, post-infective hydrocephalus with several procedures viz. septostomy, foraminoplasty, aqueductoplasty and fenestration of various membranes simplifying the hydrocephalus and, thereby, reducing the number of shunt implantations.
Endoscopic ventricular lavage (EVL) is being increasingly performed in severe cases of post-meningitic ventriculitis in some centres, with variable success in avoiding hydrocephalus, shunt implantation and delaying shunt blockage and is currently under investigation.
Pathophysiology of infective hydrocephalus
The effects of a CNS infection on CSF dynamics depend on the period of the primary infection (prenatal, neonatal or post-neonatal) as well as on the infectious agent (bacterial, viral, parasitic) [11]. Leptomeningeal inflammation [7, 24], ependymal erosive necrosis with resultant ventriculomegaly and blockage of aqueduct by intraventricular inflammatory debris are the various causes for hydrocephalus attributed to prenatal toxoplasmosis infection [45]. Cytomegalovirus (CMV) is the other prenatal infection leading to hydrocephalus, though the incidence is much less (10–15%) [7] and is mostly due to encephalomalacia causing volume loss. Leptomeningeal inflammation with thickening also contributes, and it is very rarely due to blockage of the aqueduct [34].
Neonatal infections are primarily bacterial and predominantly caused by coagulase negative staphylococci followed by other gram-positive and gram-negative organisms and result in communicating tetraventricular hydrocephalus frequently (> 50%) in early course of the disease [7, 12]. This may, however, subside with resolving infection, and if this persists, this may result in obstructive hydrocephalus in a delayed fashion due to aqueductal or 4th ventricular outlet blockage [42]. Hydrocephalus is commonly associated with partially treated meningitis, occurring more commonly in neonates and infants, especially with group B streptococcus type III [9]. In gram-negative infections, the ventriculitis and ependymal inflammation is much more common, frequently resulting in multiloculated hydrocephalus. Haemophilus influenzae is the causative agent of post-neonatal infections in most (> 60%) of cases [8], although there has been a decline with progressive vaccination. Hydrocephalus does not commonly follow (approx.10%), as basal meningitis is less common and choroid plexitis results in less CSF production [7]. Gram-negative ventriculitis can progress to obstructive or communicating hydrocephalus in many cases. Tubercular meningitis (TBM) is a very common cause in children in Africa, India and other south Asian countries. Though predominance of basal meningitis commonly results in communicating hydrocephalus, recent reports suggest a large number of them may be obstructive at aqueduct or 4th ventricular outlet level or rarely because of mass effect of a strategically placed tuberculoma [13, 29, 41, 51].
Development of complex, multiloculated hydrocephalus
The pathophysiology of multiloculated hydrocephalus involves denuding of the ependymal cells with protrusion of underlying glial cells into the ventricular lumen. These cells then act as a nidus upon which fibro-glial septations can develop, leading to isolated compartments of CSF [38]. It is a progressive process, with new septae usually continuing to develop, transforming the normal anatomical landscape of the ventricles from a single large system, into multiple non-communicating compartments [43]. Further enlargement of compartments depends on inflammatory exudates with entrapment of CSF. Some loculations may not enlarge if the membranes are still permeable to CSF flow or if the initial insult has involved the choroid plexus, thus impairing CSF production [43]. The chemical ventriculitis which follows intraventricular haemorrhage or post-infectious ventriculitis usually occurs in the neonatal period, and these early insults usually lead to the formation of septations within the ventricular system [1, 38, 43]. Other iatrogenic causes also play an important role, such as shunt infection, direct trauma to the ependymal cells during catheter insertion, over-drainage or even simply decompression of existing loculations which brings chronically inflamed ventricle walls together, allowing adherence and formation of new septae [17, 32, 43]. Multiloculated hydrocephalus may also occur in association with prematurity-related IVH, birth trauma, CNS tumours, head injury and other intracranial surgery [1, 28, 43, 56].
Role of imaging
Ultrasonography
Warf’s findings [51] included a small IV ventricle in 44% cases on pre-operative ultrasound imaging (which has correlated 100% with an obstructed aqueduct in patients undergoing ventriculoscopy) in patients with post-infective hydrocephalus (PIHC). Many patients had intraventricular septations on ultrasound, indicative of prior ventriculitis.
Ultrasound is very useful for evaluating multiloculated hydrocephalus, particularly in infants to demonstrate cysts and loculations as it requires a patent anterior fontanelle. It is non-invasive, allows multiplanar real-time imaging and can be used to confirm adequate fenestration intraoperatively. The main limitation remains operator dependency (Fig. 1).
Pneumoencephalography
A simple technique of prediction of success of ETV was described by Figaji et al., where entry of air in the ventricular system by lumbar puncture route has been considered a negative predictor due to communicating nature of hydrocephalus in tuberculous meningitis patients [15]. Air studies in non-communicating hydrocephalus show air typically trapped in the prepontine cistern; release of this air during an ETV can be helpful to identify entry into the cisternal space as these cases typically have cisterns filled with exudate and obscured anatomy.
CT brain
It is easily available, inexpensive and quick, avoiding the need for sedation or anaesthesia and can be performed even in unstable patients with altered sensorium and is therefore the most common investigation in children. The presence of ventricular dilatation and periventricular ooze will suggest active hydrocephalus with meningeal enhancement on contrast administration, and basal exudates can be well visualised in tubercular meningitis (TBM). It may also demonstrate associated ischemia or infarction, cerebritis with parenchymal enhancement and tuberculoma, if any. However, CT scan cannot always differentiate between communicating and non-communicating hydrocephalus [4].
Dynamic invasive studies like CT scan with air encephalography or CT ventriculogram further aid in the determination of the level of obstruction and differentiation between communicating and non-communicating hydrocephalus. Since it is an invasive procedure, this technique is not widely used, especially due to the wider availability of MR imaging.
Multiloculated hydrocephalus may have a higher prevalence than appreciated and often overlaps with manifestations of shunt malfunction [43]. It is often detected after a shunt revision demonstrating collapse of the drained ventricular compartment with persisting dilatation of the isolated compartments [33]. Contrast CT ventriculography has also been used to assess communication between the various compartments pre- and post-operatively [2, 28].
MRI brain, MR angiogram and Cine MRI
Contrast-enhanced MR imaging demonstrates abnormal meningeal enhancement usually in the basal cisterns and also in other cisterns in severe cases. It also reveals information about hydrocephalus and tuberculomas. Vasculitis in the region of brainstem and basal ganglia is depicted better because of distinction between oedema and infarcts. It can also differentiate between communicating and obstructive hydrocephalus. Chugh et al. strongly advocated use of Cine MRI as a non-invasive tool of assessment and for comparison post-operatively in TBMH (TBM hydrocephalus) [5].
MRI is also considered as the preferred imaging modality for diagnosis of multiloculated hydrocephalus. It provides multiplanar views with higher spatial resolution and better sensitivity for revealing septations. Specific sequences like constant interference steady state (CISS), which is a T2-weighted gradient echo sequence, provide remarkable morphological detail. MR ventriculography (MRV) involves injection of contrast material directly into a cyst cavity to verify communication with the surrounding ventricular system also defining the margins of these compartments. The procedure allows more appropriate treatment planning but is invasive and requires multiple punctures for different compartments to be accessed and rotation of the patient’s head in all directions to spread the contrast material [17].
Endoscopic interventions
Endoscopic third ventriculostomy
It is now a well-established treatment modality for obstructive hydrocephalus with a success rate of 60–85% in most series [14, 23]. Figaji et al., Jonathan et al. and Husain et al. reported the first use of ETV in TBMH [14, 20, 23]. Raouf et al. reported successful outcome of ETV in 55.9% in 35 cases of hydrocephalus secondary to intracranial infection [36].
Warf [51] reported the following frequent findings among patients with PIHC on endoscopy: aqueduct obstruction by a web of tissue; yellow deposits on ependyma (Fig. 2) and choroid plexus; hemosiderin staining on ependyma, floor of 3rd ventricle and periaqueductal areas; intraventricular webbing and anatomic distortion; scarring; and atrophy of choroid plexus. All these findings point towards previous inflammation as the cause of the hydrocephalus in these patients, and it is often non-communicating in nature. In Warf's study of 300 consecutive children with hydrocephalus, 60% of patients had a CSF infection as the aetiology [49]. Later, in his 5-year outcome study of a cohort of 149 patients of PIHC, 56.4% of patients were successfully treated with ETV without the need for a shunt [52].
ETV causes diversion of CSF to previously inaccessible areas and clears exudates from the areas which had impaired absorption [20, 23]. It also decreases the transventricular pressure gradient and the demyelination of periventricular brain parenchyma, which could contribute to some symptoms of hydrocephalus [18, 35]. The improved CSF dynamics facilitate better penetration of antiTB drugs. Alteration in haemodynamics may also allow better drug delivery [20, 35].
Chugh et al. concluded that ETV should be considered as the first surgical option for CSF diversion in patients with TBMH. Cine MRI as a non-invasive tool of assessment and post-operative comparison was strongly recommended by them. They found that patients with chronic disease and longer duration of ATT administration responded well [5]. On the contrary, patients with higher stage of illness and cisternal exudates as observed intraoperatively had a poorer outcome. Singh et al. reported a 77% success rate of ETV—60% early and 17% delayed. They reported the presence of a thin and transparent third ventricular floor to be a favourable prognostic indicator [41].
It appears that favourable cisternal anatomy around the third ventricle and thickness of third ventricular floor is the major determinants of the success of ETV in TBMH [5]. However, TBMH is notorious for thick and fibrous exudates in the interpeduncular and the perimesencephalic cisterns (Fig. 3). This also adds to the difficulty in identifying the anatomical landmarks and increases the risk of complications. ETV in PIHC is thus technically demanding and should be done by an experienced neurosurgeon that has good training and expertise in ETV, typically because the floor is thickened (Fig. 4) and challenging to perforate, and confirmation of cisternal entry is difficult [13]. Variable indications for endoscopy in TBMH have been reported, from ETV used strictly for non-communicating hydrocephalus and medical management or VP shunts for communicating hydrocephalus [13] to a less restricted use of ETV in all patients as a first procedure [5]. The most commonly reported complications of ETV are failure to perform the ETV due to anatomical distortions and CSF leaks [23]. Due to poor results in an acute phase of tubercular meningitis, it is felt that shunt insertion could be advised to start with and the ETV is performed when shunt malfunction occurs [55].
Choroid plexus coagulation to supplement ETV
Choroid plexus coagulation has been thought to be beneficial as it diminishes the CSF production and can thus increase the success rate of ETV. Warf et al. [50] conducted a prospective study in Uganda to determine if the outcome of bilateral CPC + ETV was superior to ETV alone. ETV was accomplished in 550 children of which 266 underwent combined ETV + CPC and 284 underwent ETV alone. Fifty eight percent (320 cases) of the children studied had post-infectious hydrocephalus. Overall, the success rate of ETV + CPC (66%) was superior to that of ETV alone (47%) among infants younger than 1 year of age (p < 0.0001). Although the difference was not significant for PIHC (62% compared with 52% success, p = 0.1607), a benefit was not ruled out (power = 0.3). For patients at least 1 year of age, there was no difference between the two procedures (80% success for each, p = 1.0000). The overall surgical mortality rate was 1.3%, and the infection rate was less than 1%.
Late follow-up analysis of the Ugandan study patients showed that there was no significant difference between the ETV + CPC group and the ventriculoperitoneal-shunt group in BSID-3 motor or language scores, rates of treatment failure (35 and 24%, respectively; hazard ratio, 0.7; 95% CI, 0.3 to 1.5; p = 0.24), or brain volume (z score, − 2.4 and − 2.1, respectively; estimated difference, 0.3; 95% CI, − 0.3 to 1.0; p = 0.12). This single-centre study involving Ugandan infants with post-infectious hydrocephalus showed no significant difference between endoscopic ETV + CPC and ventriculoperitoneal shunting with regard to cognitive outcomes at 12 months [26]. The procedural success rates were not significantly different but failure occurred in 35% of the ETV + CPC group and 24% in the shunt group; there were two deaths, both randomised to the ETV + CPC group. Some improvement with the addition of CPC to ETV has been noted in infants with post-infective hydrocephalus by others as well [53]. Recently, in a North American multicentre prospective study of infant hydrocephalus in which patients treated with ETV + CPC were matched with patients treated with ETV alone or ventriculoperitoneal shunting, the success rate for ETV + CPC was 36%, was significantly lower than for shunted patients and was not significantly different than for ETV alone, although the authors note that the study was not powered to show this [27].
ETV after shunt infection (secondary ETV)
The role of ETV as a primary treatment for hydrocephalus and as an alternative to shunt revision (secondary ETV) in infected and malfunctioning shunts was analysed by O’Brien DF and group [31]. Seventy-four percent of cases in the primary ETV group and 70% in the secondary group had a successful outcome. The success rate of secondary ETV in mechanical shunt malfunction alone was 67% as compared to 79% in infected malfunctioning shunts. The aetiology of hydrocephalus was evaluated as a factor contributing to the success of ETV. In the primary group, infective aetiology led to a poor outcome. However, in the secondary group, 75% cases with infection had a successful outcome. They concluded that the success of secondary ETV, unlike primary ETV, is not origin-specific.
Thirty patients treated with third ventriculostomy for malfunctioning or infected shunts were retrospectively reviewed by Cinalli G et al. 76.7% experienced successful outcomes, resulting in shunt independence. They concluded that ETV is a valuable alternative to shunt revision in patients affected by obstructive hydrocephalus presenting with shunt malfunction or infection [6].
Shimizu et al. suggested that secondary ETV can be used in shunt infections. Although the procedure does not obviate the need for later shunt implantation, it is shown to delay the subsequent procedures [40]. When performing a secondary procedure, some studies recommend removal or blockage of the malfunctioning shunt. This is shown to increase the longevity of the procedure [10].
In our experience, 36 patients underwent secondary ETV from 2004 to 2017, of whom, 15 had an infective aetiology as the cause of shunt malfunction. Our success rate for secondary ETV in these cases was 70%. The most important criterion to guide us to ETV was the radiological anatomy showing the triventricular enlargement as described by Cinalli et al. in 2012 [44].
Endoscopy in Neurocysticercosis
Hydrocephalus due to neurocysticercosis (Fig. 5) usually portends a poor prognosis and shunt failure is a common complication. An early extraction of parasite plus ETV may improve an outcome and reduce shunt failure [19, 48]. ETV and removal of the NCC was found to be better than shunt surgery [21].
Endoscopic strategies in multiloculated hydrocephalus
Multiloculated hydrocephalus is characterised by isolated compartments of CSF within the ventricular system, which progressively enlarge despite the presence of a functioning shunt [56]. Spennato et al. classified multiloculated hydrocephalus morphologically as multiple intraventricular septations isolated lateral ventricle/unilateral hydrocephalus (Fig. 6), entrapped temporal horn, isolated fourth ventricle and expanding cavum septae pellucidi/cavum vergae. Andresen and Juhler also proposed a classification system based on both anatomy and physiology of CSF absorption [3]. Akbari et al. advocated a grading system to guide clinical decision-making regarding treatment choice, the efficacy of treatments and prognosis [1]. A universal classification system for multiloculated hydrocephalus which accounts for supratentorial and infratentorial loculations, which often occur concurrently, would be useful, making uniform analysis possible [3, 56].
Management of multiloculated hydrocephalus remains a challenge. The goal remains to create a single communicating system drained by one ventricular catheter, i.e., simplification of the hydrocephalus [1, 3, 16, 17, 28, 43, 56]. Placement of multiple ventricular catheters may effectively drain non-communicating compartments, but the increasingly complex shunt system required is far from desirable [1, 28, 30, 37, 56]. Wide fenestration of membranes appears to be the more beneficial procedure, and this can be accomplished through open microsurgery or endoscopic surgery [1, 3]. Endoscopic fenestration has demonstrated decreased blood loss, shorter operative time with lower morbidity and decreased length of hospital stay [1, 28]. Placement of shunt catheters under endoscopic guidance may also lower the risk of shunt malposition [38] (Fig. 7a, b). Endoscopic fenestration therefore remains the preferred treatment option for multiloculated hydrocephalus, especially in infants, with open fenestration likely best reserved for severe or refractory cases [1, 16, 28, 56].
Neuroendoscopic experience and good planning are critical. These are often difficult cases—the ventricular anatomy is usually severely distorted and anatomical landmarks are often unclear [38]. Intraoperative decisions about where to create fenestrations are often more difficult in reality than the surgeon expects. Operative morbidity is increased in inexperienced hands by becoming disoriented in the ventricular system. A thorough pre-operative plan is essential, with the goals of the surgery clearly considered. Oftentimes, non-standard entry routes are chosen to maximise access to various compartments. This increases the chance of disorientation. Neuronavigation is invaluable as a pre-operative planning tool. This does however become less accurate with intraoperative brain shift due to CSF movement and real-time intraoperative image guidance with ultrasound or intraoperative MRI have been proven useful [33, 38, 46]. Flexible endoscopy may be valuable in navigating difficult trajectories, but visibility is often not as good, and it is even easier to become disoriented when not operating in a straight line. Intraventricular membranes are often tough to fenestrate and this may require the assistance of sharp dissection, cautery or laser. Wide fenestrations are necessary as the proinflammatory environment often persists for a prolonged time and closure of fenestrations is common. Where possible, it is worthwhile leaving the ventricular catheter traversing the fenestrations, with proximal perforations made on the catheter length where necessary.
The extent of neurological morbidity and developmental delay is determined by the underlying aetiology in multiloculated hydrocephalus, and the goal of surgery is therefore to limit the number of procedures and ideally facilitate insertion of a single ventricular catheter or even avoid catheter placement altogether, where possible [32, 37]. If a shunt is to be placed, it must be remembered that long procedures increase the risk of a shunt infection; therefore, unnecessary fenestrations of questionable benefit may not be in the patient’s best interest if these prolong the procedure unduly.
Intraventricular endoscopic lavage
The treatment of infective hydrocephalus in children, especially infants, remains a great challenge due to difficulty in eradicating the infective materials and inflammatory debris within the CSF pathway in a short period of time. External ventricular drainage (EVD) is frequently not effective and is associated with risks of secondary infection. The subsequent ventriculoperitoneal shunt is often complicated by recurrent blockage, repeated shunt infection and shorter shunt survival due to high level of protein and cell counts. An aggressive approach is therefore needed to facilitate the clearance and restoration of CSF flow [22, 39, 47].
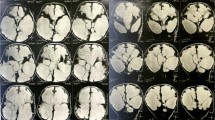
Intraventricular endoscopic lavage (iVEL) was used since 2007 in Kuala Lumpur, Malaysia, to overcome shunt infections, shunt malfunctions and related morbidities among children with infective hydrocephalus treated at the Children’s Hospital. A prospective observational study on 12-month shunt survival among children aged 12 years and less revealed low shunt survival rate at 60%. Forty percent of patients required removal or revision of shunt, of which 23% were due to shunt infection and 18% were due to shunt malfunctions. Four percent of infected shunts developed pyogenic ventriculitis with a 70% mortality. This alarming data triggered the effort to find an alternative approach in treating infective hydrocephalus with ventriculitis (Fig. 8).
The following indications were followed for iVEL: (1) pyogenic ventriculitis, (2) infected shunts, and (3) recurrent shunt malfunction with high cell counts and protein level. Protocol consisted of performing bilateral intraventricular endoscopic lavage (iVEL) combining direct neuroendoscopy with copious irrigation of Ringer’s lactate, removal of the infective debris and replacement of cerebrospinal fluid with physiological solutions. Early attempts on bilateral lavage through a single frontal burr hole and septum pellucidotomy had failed to effectively clear the infective debris within the hidden pocket located on the medial wall of the contralateral ventricle leading to modification of the approach by using bilateral frontal pre-coronal burr holes (Fig. 9).
Surgical approaches: a Unilateral intraventricular endoscopic lavage (iVEL) with septum pellucidotomy has its own limitation and will not be able to remove the hidden pocket of slough (red) located medial to the contralateral occipital horn. b Bilateral iVEL allows direct access and wider view (green triangle) to occipital horn and third ventricle
Pus and infective debris are removed first followed by adherent slough on the ependymal surface. The soft and floating infective materials are removed by continuous gravity feed irrigation with the tip of endoscope directed towards the target area and passive drainage through the outlet of endoscope. Removal of the adherent slough on the floor of ventricle will require specific techniques, which include intermittent “fish-biting” suction aspiration, sweeping with the blunt tip of endoscope and grasping forceps. Gentle sweeping with the blunt tip of endoscope helps to elevate the layer of slough from the underlying ependyma and subsequently removal with the grasping forceps (Figs. 10 and 11). Lavage is done in stepwise fashion within the lateral ventricle starting from frontal horn of the lateral ventricles followed by the septum, lateral wall and occipital horn. Endoscope is then advanced to pass through the foramen of Monroe towards the anterior floor of the third ventricle followed by the posterior floor of the third ventricle, roof of third ventricle and aqueduct of Sylvius (Fig. 12). Special care should be taken when removing the slough on the choroid plexus and veins as it may cause severe haemorrhage if too much suction is used. The underlying inflamed ependymal surface easily bleeds if not handled gently.
Removal of soft and floating infective materials using suction-irrigation technique within the right lateral and third ventricle. a Endoscopic view of right lateral ventricle following ventriculostomy. b Infective materials seen within third ventricle, viewed from the foramen of Monroe. c Aspiration of pus using infant feeding catheter, 8Fr. d Interthalamic mass seen at the margin between clear anterior half and pus within the posterior half floor of the third ventricle. e Left thalamus. f Patent aqueduct of Sylvius seen after lavage (arrow). g View of third ventricle after lavage. h View of right lateral ventricle after lavage
ETV and septum pellucidotomy during lavage
In the case of aqueductal stenosis, endoscopic third ventriculostomy is best avoided at the same setting of lavage as this may contaminate the prepontine space. However, in the presence of the foramen of Monroe stenosis or thick adherent slough which could not be removed safely, endoscopic septum pellucidotomy is performed for access into the contralateral ventricle and creating pathway to communicate both lateral ventricles.
External ventricular drain is inserted on one side of the ventricle if CSF is clear at the end of procedure for post-operative control and subsequently challenge prior to removal. A plain control CT scan is done on day 1 after surgery to exclude complication of lavage and collapsed of ventricles.
Summary
ETV has been able to avoid shunts in selected cases of post-infective hydrocephalus. It has also proved to be quite successful in selected cases of shunt malfunction with infection or previous PIHC. However, the selection of cases is important, and an experienced surgeon is needed to achieve a high degree of success without complications. Other endoscopic interventions have contributed to clear up severe infection in ventricles (iVEL) and have created better chances of shunt survival with simplified insertion of a shunt by endoscopic fenestrations in multiloculated hydrocephalus. The latter has substantially reduced the prevalence of multiple shunt systems in patients. Though its primary use in removal of infective cysts (NCC) is unequivocal, its usefulness in CPC and iVEL is under evaluation. With all of these procedures, it is essential that the surgeon has sufficient neuroendoscopy experience as the anatomy is often difficult, visibility is often poor and stomas and fenestrations may be difficult to create.
Author contribution
Endoscopic third ventriculostomy has been primarily designed and written by Deopujari C and Samantray SK. The material for multiloculated hydrocephalus has been provided by Padayachy L, and the material for Intraventricular Lavage has been provided by Azmi A. Dr. Anthony Figaji has contributed to the manuscript and reviewed the text.
References
Akbari SH, Holekamp TF, Murphy TM, Mercer D, Leonard JR, Smyth MD, Park TS, Limbrick DD Jr (2015) Surgical management of complex multiloculated hydrocephalus in infants and children. Child Nerv Syst 31(2):243–249
Albanese V, Tomasello F, Sampaolo S, Picozzi P (1982) Neuroradiological findings in multiloculated hydrocephalus. Actaneurochirurgica 60(3–4):297–311
Andresen M, Juhler M (2012) Multiloculated hydrocephalus: a review of current problems in classification and treatment (2012). Child Nerv Syst 28(3):357–362
Bruwer GE, Van Der Westhuizen S, Lombard CJ, Schoeman JF (2004) Can CT predict the level of CSF block in tuberculous hydrocephalus? Child Nerv Syst 20:183–187
Chugh A, Husain M, Gupta RK, Ojha BK, Chandra A, Rastogi M (2009) Surgical outcome of tuberculous meningitis hydrocephalus treated by endoscopic third ventriculostomy: prognostic factors and postoperative neuroimaging for functional assessment of ventriculostomy. J Neurosurg Pediatr 3:371–377
Cinalli G, Salazar C, Mallucci C, Yada JZ, Zerah M, Sainte-Rose C (1998) The role of endoscopic third ventriculostomy in the management of shunt malfunction. Neurosurgery 43:1323–1327
Ciurea AV, Coman TC, Mircea D (2004) Postinfectious hydrocephalus in children. In: Cinalli G, Meixner W, Sainte-Rose C (eds) Pediatric Hydrocephalus. Springer-Verlag Italia, Milano, pp 201–218
Daoud AS, Omari H, al-Sheyyab M, Abuekteish F (1998) Indications and benefits of computer tomography in childhood bacterial meningitis. J Trop Pediatr 44:167–169
de Louvois J (1994) Acute bacterial meningitis in the newborn. J Antimicrob Chemother 34(Suppl A):61–73
Deopujari CE, Karmarkar VS, Shaikh ST (2017) Endoscopic third ventriculostomy: success and failure. Korean Neurosurg Soc 60(3):306–314
Di Rocco C, Cinalli G, Massimi L, Spennato P, Cianciulli E, Tamburrini G (2006) Endoscopic third ventriculostomy in the treatment of hydrocephalus in pediatric patients. Adv Tech Stand Neurosurg 31:171–173
Doctor BA, Newman N, Minich NM, Taylor HG, Fanaro AA, Hack M (2001) Clinical outcomes of neonatal meningitis in very low birthweight infant. Clin Pediatr 40:473–480
Figaji AA, Fieggen AG (2013) Endoscopic challenges and applications in tuberculous meningitis. World Neurosurg 79(2 Suppl):S24.e9–S24.14
Figaji AA, Fieggen AG, Peter JC (2003) Endoscopic third ventriculostomy in tuberculous meningitis. Childs Nerv Syst 19:217–225
Figaji AA, Fieggen AG, Peter JC (2005) Air encephalography for hydrocephalus in the era of neuroendoscopy. Child Nerv Syst 21:559–565
Fritsch MJ, Mehdorn M (2002) Endoscopic intraventricular surgery for treatment of hydrocephalus and loculated CSF space in children less than one year of age. Pediatr Neurosurg 36(4):183–188
Gandhoke GS, Frassanito P, Chandra N, Ojha BK, Singh A (2013) Role of magnetic resonance ventriculography in multiloculated hydrocephalus. J Neurosurg Pediatr 11(6):697–703
Ghosh S, Chandy MJ (1992) Intrasellar tuberculoma. Clin Neurol Neurosurg 94:251–252
Goel RK, Ahmad FU, Vellimana AK, Suri A, Chandra PS, Kumar R, Sharma BS, Mahapatra AK (2008) Endoscopic management of intraventricular neurocysticercosis. J Clin Neurosci 15:1096–1101
Husain M, Jha DK, Rastogi M, Husain GRK (2005) Role of neuroendoscopy in the management of patients with tuberculous meningitis hydrocephalus. Neurosurg Rev 28:278–283
Husain M, Rastogi M, Jha DK, Husain N, Gupta RK (2007) Endoscopic transaqueductal removal of fourth ventricular neurocysticercosis with an angiographic catheter. Neurosurgery 60(4 Suppl 2):249–253
Johnson JR, Idris Z, Abdullah JM, Alias A, Haspani MS (2017) Prevalence of shunt dependency and clinical outcome in patients with massive intraventricular haemorrhage treated with endoscopic washout and external ventricular drainage. Malays J Med Sci 24(1):40–46
Jonathan A, Rajshekhar V (2005) Endoscopic third ventriculostomy for chronic hydrocephalus after tuberculous meningitis. Surg Neurol 63:32–34
Kaiser G (1985) Hydrocephalus following toxoplasmosis. Z Kinderkir 40(Suppl. 1):10–11
Kulkarni AV, Riva-Cambrin J, Browd SR (2011) Use of the ETV success score to explain the variation in reported endoscopic third ventriculostomy success rates among published case series of childhood hydrocephalus. J Neurosurg Paediatrics 7:143–146
Kulkarni AV, Schiff SJ, Mbabazi-Kabachelor E et al (2017) Endoscopic treatment versus shunting for infant hydrocephalus in Uganda. N Engl J Med 377:2456–2464
Kulkarni AV, Riva-Cambrin J, Rozzelle CJ, Naftel RP, Alvey JS, Reeder RW, Holubkov R, Browd SR, Cochrane DD, Limbrick DD Jr, Simon TD, Tamber M, Wellons JC III, Whitehead WE, Kestle JRW (2018) Endoscopic third ventriculostomy and choroid plexus cauterization in infant hydrocephalus: a prospective study by the Hydrocephalus Clinical Research Network. J Neurosurg Pediatr 21(3):214–223
Lewis AI, Keiper GL Jr, Crone KR (1995) Endoscopic treatment of loculated hydrocephalus. J Neurosurg 82(5):780–785
Moorthy RK, Rajshekhar V (2011) Endoscopic third ventriculostomy for hydrocephalus: a review of indications, outcomes, and complications. Neurol India 59:848–854
Nowoslawska E, Polis L, Kaniewska D, Mikolajczyk W, Krawczyk J, Szymanski W et al (2003) Effectiveness of neuroendoscopic procedures in the treatment of complex compartmentalized hydrocephalus in children. Childs Nerv Syst 19(9):659–665
O’Brien DF, Javadpour M, Collins DR, Spennato P, Mallucci CL (2005) Endoscopic third ventriculostomy: an outcome analysis of primary cases and procedures performed after ventriculoperitoneal shunt malfunction. J Neurosurg 103(5 Suppl):393–400
Oi S (2011) Classification of hydrocephalus: critical analysis of classification categories and advantages of “multi-categorical hydrocephalus classification” (McHC). Childs Nerv Syst 27:1523–1533
Paraskevopoulos D, Biyani N, Constantini S, Beni-Adani L (2011) Combined intraoperative magnetic resonance imaging and navigated neuroendoscopy in children with multicompartmental hydrocephalus and complex cysts: a feasibility study. J Neurosurg: Peds 8(3):279–288
Pearlman J, Argyle C (1992) Lethal cytomegalovirus infection in preterm infants: clinical, radiological, and neuropathological findings. Ann Neurol 31(1):64–68
Rajsekhar V, Chandy MJ (1997) Tuberculomas presenting as isolated brain stem masses. Br J Neurosurg 11:127–133
Raouf A, Zidan I, Mohamed E (2015) Endoscopic third ventriculostomy for post-inflammatory hydrocephalus in pediatric patients: is it worth a try? Neurosurg Rev 38:149–155
Sandberg DI, McComb JG, Krieger MD (2005) Craniotomy for fenestration of multiloculated hydrocephalus in pediatric patients. Neurosurgery 57(1 Suppl):100–106
Schulz M, Bohner G, Knaus H, Haberl H, Thomale UW (2010) Navigated endoscopic surgery for multiloculated hydrocephalus in children. J Neurosurg Pediatr 5(5):434–442
Schulz M, Buhrer C, Pohl-Schickinger A, Haberl H, Thomale UW (2014) Neuroendoscopic lavage for the treatment of intraventricular hemorrhage and hydrocephalus in neonates. J Neurosurg Pediatr 13(6):626–635
Shimizu T, Luciano MG, Fukuhara T (2012) Role of endoscopic third ventriculostomy at infected cerebrospinal fluid shunt removal. J Neurosurg Pediatr 9:320–326
Singh D, Sachdev V, Singh AK, Sinha S (2005) Endoscopic third ventriculostomy in post tubercular meningitic hydrocephalus: a preliminary report. Minim Invasive Neurosurg 48:47–52
Siomin V, Cinalli G, Grotenhuis A, Golash A, Oi S, Kothbauer K, Weiner H, Roth J, Beni-Adani L, Pierre-Kahn A, Takahashi Y, Mallucci C, Abbott R, Wisoff J, Constantini S (2002) Endoscopic third ventriculostomy for patients with cerebrospinal fluid infections and/or hemorrhage. J Neurosurg 97:519–524
Spennato P, Cinalli G, Ruggiero C, Aliberti F, Trischitta V, Cianciulli E, Maggi G (2007) Neuroendoscopic treatment of multiloculated hydrocephalus in children. J Neurosurg 106(1 Suppl):29–35
Spennato P, Ruggiero C, Aliberti F, Nastro A, Mirone G, Cinalli G (2013) Third ventriculostomy in shunt malfunction. World Neurosurg 79(2 Suppl):S22.e21–S22.e26
Stahl W, Kaneda Y (1997) Pathogenesis of murine toxoplasmic hydrocephalus. Parasitology 114:219–229
Strowitzki M, Keifer M, Steudel W (2002) A new method of ultrasonic guidance of neuroendoscopic procedures. J Neurosurg 96:628–632
Tabuchi S, Kadowaki M (2015) Neuroendoscopic surgery for ventriculitis and hydrocephalus after shunt infection and malfunction: preliminary report of a new strategy. Asian J Endosc Surg 8:180–184
Torres-Corzo JG, Tapia-Pérez JH, Vecchia RR, Chalita-Williams JC, Sánchez-Aguilar M, Sánchez-Rodríguez JJ (2010) Endoscopic management of hydrocephalus due to neurocysticercosis. Clin Neurol Neurosurg 112:11–16
Warf BC (2005) Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. J Neurosurg 102(1 Suppl):1–15
Warf BC (2005) Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age: a prospective study in 550 African children. J Neurosurg Pediatr 103:475–481
Warf BC, MacGowen L (2001) Post infectious hydrocephalus: the most common cause of hydrocephalus in Uganda. Ifhsb (International federation for hydrocephalus and spina bifida)
Warf BC, Dagi AR, Kaaya BN, Schiff SJ (2011) Five-year survival and outcome of treatment for postinfectious hydrocephalus in Ugandan infants. J Neurosurg Pediatr 8(5):502–508
Weil AG, Fallah A, Chamiraju P, Ragheb J, Bhatia S (2016) Endoscopic third ventriculostomy and choroid plexus cauterization with a rigid neuroendoscope in infants with hydrocephalus. J Neurosurg Pediatr 17:163–173
Yadav YR, Jaiswal S, Adam N, Basoor A, Jain G (2006) Endoscopic third ventriculostomy in infants. Neurol India 54:161–163
Yadav YR, Parihar V, Pande S, Namdev H, Agarwal M (2012) Endoscopic third ventriculostomy. J Neurosci Rural Pract 3:163–173
Zuccaro G, Ramos JG (2011) Multiloculated hydrocephalus. Childs Nerv Syst 27(10):1609–1619
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Deopujari, C.E., Padayachy, L., Azmi, A. et al. Neuroendoscopy for post-infective hydrocephalus in children. Childs Nerv Syst 34, 1905–1914 (2018). https://doi.org/10.1007/s00381-018-3901-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3901-z