Abstract
Cardiovascular diseases are major causes of morbidity and mortality in developed countries. Cerebrovascular diseases, especially stroke, represent major burden of disability and economy impact. Major advances in primary and secondary prevention and therapy are needed in order to tackle this public health problem. Our better understanding of pathophysiology is essential in order to develop novel diagnostic and therapeutic tools and strategies. microRNAs are a family of important post-transcriptional regulators of gene expression and their involvement in the pathophysiology of cerebrovascular diseases has already been reported. Moreover, microRNAs may represent above-mentioned potential diagnostic and therapeutic tools in clinical practice. Within this chapter, we briefly describe basic epidemiology, aetiology and clinical manifestation of following cerebrovascular diseases: extracranial carotid atherosclerosis, acute stroke, intracranial aneurysms and cerebral arterio-venous malformations. Further, in each chapter, the current knowledge about the involvement of specific microRNAs and their potential use in clinical practice will be summarized. More specifically, within the subchapter “miRNAs in carotid atherosclerosis”, general information about miRNA involvement in atherosclerosis will be described (miR-126, miR-17-92, miR-155 and others) with special emphasis put on miRNAs affecting carotid plaque progression and stability (e.g. miR-145, miR-146 or miR-217). In the subchapter “miRNAs in acute stroke”, we will provide insight into recent knowledge from animal and human studies concerning miRNA profiling in acute stroke and their expression dynamics in brain tissue and extracellular fluids (roles of, e.g. let-7 family, miR-21, miR-29 family, miR-124, miR-145, miR-181 family, miR-210 and miR-223). Subchapters dealing with “miRNAs and AV malformations” and “miRNAs and intracranial aneurysms” will focus on miR-21, miR-26, miR-29 family and miR-143/145.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- microRNA
- Carotid atherosclerosis
- Ischemic stroke
- Intracranial aneurysms
- Cerebral arterio-venous malformations
Carotid Atherosclerosis
Epidemiology of Carotid Atherosclerosis
Atherosclerosis represents a complex arterial disease characterized by vascular wall inflammation and remodelling in the end resulting in the creation of atherosclerotic plaques [1]. According to the site of plaques occurrence, atherosclerosis clinically presents as coronary artery disease (CAD), carotid atherosclerosis (Fig. 9.1) or peripheral artery disease (PAD) [2]. Carotid arteries represent one of the specific places of plaques accumulation, especially concerning the ostium and bifurcation of common carotid artery, probably due to alteration of blood flow at these locations [3]. Accumulation of atherosclerotic plaques in carotid arteries affects significantly blood supply to the brain and predisposes patients to fainting, syncope and possibly to ischemic stroke. Based on data of Framingham cohort study, the reported prevalence of carotid artery atherosclerosis (defined as stenosis >50 % evaluated by carotid ultrasound) in the study population was 7 % in women and 9 % in men [4–6]. In term of stroke aetiology, the atherosclerotic aetiology accounts for 10–15 % of ischemic strokes and soon revelation of carotid atherosclerosis represents a risk factor for future stroke development [7].
Atherosclerotic plaque in the left internal carotid artery, curved multiplanar reconstruction (MPR). Sagittal (left) and axial (right) CT angiography scans of the neck demonstrating >90 % narrowing of the internal carotid artery behind the common carotid artery bifurcation. Atherosclerotic plaque is represented by a hypodense area in the arterial lumen (black star), open arrows point to the plaque calcifications (the most apparent hyperdense part; on the axial scan forming a hyperdense rim). White arrow on the axial scan (right) shows the residual vascular lumen (diminished by mass of the plaque). CCA common carotid artery, ECA external carotid artery, ICA internal carotid artery, VA vertebral artery
Clinical Evaluation of Carotid Atherosclerosis
Carotid stenosis can be evaluated by various non-invasive methods [8, 9]:
-
B-mode ultrasound (parameters as intima-media thickness (IMT), echogenic quality and 3D volume measurement of plaque characteristics)
-
Transcranial Doppler (microemboli detection used as a marker of plaque instability; detection of intracranial carotid stenosis)
-
Computed tomography angiography/ CTA (assessment of arterial stenosis and basic plaque characteristics)
-
Magnetic resonance imaging/ MRI (evaluating the intraplaque haemorrhage and presence of a fibrous cap, both representing radiological markers of plaque vulnerability)
-
Positron emission tomography/ PET (research imaging technique used for evaluation of vascular wall inflammation)
Periodical carotid plaque evaluation represents a tool for therapy monitoring and carotid plaque evolution. The most important is a proper treatment of vascular risk factors (hypertension, diabetes, dyslipidemia, smoking cessation, etc.), specifically, the therapy of dyslipidemia is typically led by statins which lower serum cholesterol levels, reduce subclinical inflammation inside the plaque, and promote intraplaque stabilization independently of cholesterol lowering as well [10].
Pathophysiology of Atherosclerosis and Roles of miRNAs
From the pathophysiological point of view, atherosclerosis represents a complex process of arterial wall inflammation and remodelling that includes activation of endothelial cells (ECs) by various external stimuli, e.g. disrupted blood-flow [3] or oxidized LDL (oxLDL) presence [11], which further leads to activation/proliferation of vascular smooth muscle cells (VSMCs), vascular wall fibroblasts and also other cell types, such as platelets, adipocytes or macrophages (and their altered form “foam cells”) [1, 11]. All above-mentioned processes results in the end in the creation of atherosclerotic plaques. Predominantly, atherosclerotic plaques are formed at places exposed to disrupted blood flow, in vivo specifically in the aortic arch and arterial bifurcations [12]. Recent advances in our understanding of atherosclerosis pathophysiology revealed that shear stress significantly affects the gene expression of EC exposed to either high or low shear stress, and miRNAs seem to participate even in the flow-regulation of atherosclerosis [12, 13].
Roles of miRNA in atherosclerosis include mainly (a) regulation of gene expression in all aforementioned cells and (b) miRNAs serve as mediators of cell-to-cell communication [13, 14]. From the atherosclerotic point of view, miRNAs (also termed “athero-miRs”) can be divided to several groups concerning their individual characteristics—to mechano-responsive or mechano-irresponsive (depending on the response to shear-stress) or to proatherogenic, antiatherogenic or ambigual (according to their effects on atherosclerosis progression) [15]. Providing the complex overview of miRNAs involved in atherosclerosis is not the main goal in this subchapter—here we will provide just a brief summary of the roles of main atheromiRs, i.e. miR-17-92 cluster, miR-126, miR-143/145 cluster and miR-155, and then we will specifically focus on human studies dealing with carotid atherosclerosis.
AtheromiRs
Concerning the complex pathophysiology of atherosclerosis, from all potential miRNAs involved, we should definitely mention , widespread miR-17-92 cluster [16], endothelium-specific miR-126 [17], vascular-smooth muscle, cell enriched miR-143/145 cluster [18, 19], and also immunity-related miR-155, that is even tightly connected to macrophages function [20].
Members of miR-17-92 cluster (i.e. miR-17, miR-18a, miR-19a, miR-19b, miR-20a and miR-92a) were shown to be downregulated after the exposure of endothelial cells to laminar (≈stable) flow [21], which makes miR-17-92 proatherogenic—we can imagine that by downregulating miR-17-92, endothelium somehow “protects itself” from miR-17-92 effects. miR-17-92 was shown to target Krüppel-like factor (KLF)-2 and KLF-4 and this targeting promoted endothelial inflammation—on the other hand, if miR-17-92 was inhibited, it reduced the expression of proinflammatory markers [22]. Moreover, on the contrary to tumour angiogenesis that is promoted by miR-17-92 increase [23, 24], endothelial sprouting and neovascularization are promoted if miR-17-92 cluster activity is decreased [23, 24] and this may potentially contribute to restenosis occurrence. Concerning other general roles of miR-17-92 cluster in the regulation of cell cycle and apoptosis [25], more studies are needed to shed a light on the precise functions of this cluster in atherosclerotic process; however, inhibition of miR-17-92 cluster may generally be considered atheroprotective.
Endothelial specific miR-126 (and its passenger strand miR-126*) are both known to be highly expressed in endothelium and they are crucial for vascular integrity and the vessel development (by targeting PIK3R2, Spred-1 [17, 26], VEGF [27] or, e.g. by affecting angiopoietin signalling [28]). Their upregulation in endothelial cells generally seems to be atheroprotective. By targeting vascular cell adhesion molecule (VCAM)-1 miR-126 attenuates endothelial inflammation [29]. Similarly, miR-126 packaged in apoptotic bodies enhances endothelial recovery through upregulation of CXCL12 (particularly by inhibiting RGS16, CXCL12 inhibitor [30]), and miR-126* keeps endothelial proliferative reserve by targeting DLK1 [31]. Moreover, circulating levels of miR-126 were shown to be decreased in patients with coronary atherosclerosis and diabetes, which may contribute to the pathophysiology of both diseases [32, 33]. On the other hand, miR-126 transfer into VSMCs was shown to promote VSMCs turnover, thus suggesting a potentially negative role in vascular remodelling [34]. miR-126 functions thus need to be evaluated strictly in the tissue (or cell)-dependent manner.
Focusing now on VSMCs, miR-143/145 should be mentioned. To fulfil their functions in the vessel tone regulation, VSMCs need to remain in so-called contractile (or quiescent) phenotype; during various pathologies, the phenotypic switch to “synthetic” (or “proliferative”) phenotype occurs interfering with VSMCs normal function [35]. miR-143/145 was shown to be one of the crucial regulators of the phenotypic switch—increased levels of miR-143/145 are needed in VSMCs to remain in “contractile” phenotype [18, 36]. Knockout of miR-143/145 leads to incomplete differentiation of VSMCs and results, e.g. in aneurysm development [36]. Interestingly, it was shown that miR-143/145 levels are increased in ECs under the laminar flow [37] and moreover, miR-143/145 is transferred from ECs into VSMCs in order to keep them in “contractile” phenotype [38]. miR-143/145 targeting thus definitely represents a potential therapeutic target in the treatment of atherosclerosis for the future.
Lastly, if talking about atherosclerosis, macrophages need to be mentioned together with miR-155. miR-155 represents a master inflammation-miRNA and the important regulator of the immune system functions [20]. It was repeatedly shown that miR-155 knockout or inhibition in experimental models of atherosclerosis led to reduction of atherosclerotic plaques size and decreased macrophage accumulation [39, 40]. Via targeting of endothelial NO-synthase (eNOS), miR-155 further disrupts endothelial relaxation, which also contributes to the pathophysiology of atherosclerosis [41]. Interestingly, circulating (particularly plasmatic) levels of miR-155 were shown to be increased in experimental models of atherosclerosis [42] and miR-155 was shown as one of the most abundant miRNAs contained within LDL particles. This may partly explain LDL proinflammatory effects [43]. On the contrary, also antiatherogenic effects or miR-155 were described—e.g. absence of miR-155 in the haematopoetic cells in the hyperlipidemic mice increased atherosclerotic plaque formation [44]. Moreover, in human subjects with CAD, circulating levels of miR-155 are reduced [32]. More information about the conflicting role of miR-155 within atherosclerosis development can be found in the recent study performed by Ma et al. [45].
miRNAs in Carotid Atherosclerosis in Humans
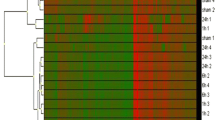
Human studies dealing with carotid atherosclerosis mostly determined expression of miRNAs from carotid atherosclerotic plaques obtained during endarterectomy of carotid arteries in patients with symptomatic stenosis [46–48]. Comparison of carotid plaques miRNA expression revealed a set of differentially expressed miRNAs compared to miRNA expression in normal carotid arteries and within this set, miR-21, miR-34a, miR-146a, miR-146b-5p and miR-210 were found to be upregulated [47]. In the very interesting study by Cipollone et al., the subset of five miRNAs (miR-100, miR-127, miR-145, miR-133a and miR-133b) were further shown to be increased in patients after stroke compared to patients with plaques but without stroke, thus predicting higher plaque instability [46]. In the agreement with Cipollone results, miR-145 expression was shown to be higher in carotid plaques from patients with hypertension [48], who are more prone to develop stroke if hypertension is not properly treated. Higher carotid plaque expression of miR-145 may thus be considered as a risk factor for plaque instability [46, 48]. Interestingly, higher circulating miR-145 levels were shown [49] and at the same time abolished [50] as a potential stroke biomarker (as described further).
Focusing more on circulating miRNAs, levels of miR-21 and miR-221 were shown to be higher in patients with carotid atherosclerosis [50] and urinary levels of miR-29b were shown to correlate with cIMT in patients with type 2 diabetes mellitus (T2DM) [51]. All three miRNAs may thus serve as potential markers of carotid atherosclerosis reflecting the disease severity [50, 51].
Lastly, we would like to point out very interesting role of miR-217 described in the senescence of ECs (using human umbilical vein ECs, aortic ECs and coronary ECs together with endarterectomy samples) [52]. miR-217 was shown to be expressed in human carotid plaques and it was shown to regulate the expression of silent information regulator 1 (Sirt1)—as the cells were ageing, miR-217 levels were increasing with concomitant decrease in Sirt1 levels, a phenomenon known to occur during ageing. Blockade of miR-217 reversed effect of ageing and increased angiogenic activity. miR-217 antagonism may thus represent very interesting strategy to reduce endothelial senescence and prevent the development of age-related diseases.
Summary
Both atherosclerosis in general and particularly carotid atherosclerosis represent risk factor for stroke development. Studies using endarterectomy and plasma/urine samples to reveal biomarkers of plaque instability or disease severity definitely indicate that miRNAs may serve not only as potential diagnostic but also therapeutic targets in carotid atherosclerosis. Further studies on larger cohorts and involving patients with various comorbidities are needed as well as studies using animal models of plaque instability, to reveal the true potential of miRNAs in the carotid atherosclerosis for future clinical practice.
Ischemic Stroke
Epidemiology of Ischemic Stroke
Stroke represents a major cause of disability and the second leading cause of death worldwide (after coronary artery disease), with an incidence of about 17 million per year. It affects both the elderly and the young (in 2010, 31 % of strokes affected adults under 65; more than 83,000 children and youths under 20 have had strokes). Improvements in primary prevention and lifestyle changes have led to a decreased incidence of age-adjusted stroke. Nevertheless, the overall number of strokes has been increasing and is expected to accelerate over the coming decades because of the population ageing. It is predicted that stroke will account for 6.2 % of the total burden of illness in developed countries by 2020. Without major advances in primary and secondary prevention, acute stroke management and treatment, and in post-stroke rehabilitation, the burden and cost of this disease will considerably increase [53–55]. Stroke can be classified as ischemic or haemorrhagic. Ischemic stroke can be either transient ischemic attack (TIA) or cerebral infarction. Haemorrhagic strokes can be either intracerebral or subarachnoid. Figure 9.2 shows the computed tomography (CT) differences between acute ischemic and haemorrhagic strokes.
Ischemic and haemorrhagic stroke on CT. (a) Normal CT (typical baseline finding in patients with acute ischemia); (b) acute ischemia 24 h after stroke onset (hypodense area marked by white arrows); (c) subarachnoid haemorrhage (hyperdense signal marked by white arrows); (d) intracerebral haemorrhage (ICH); (e) intraventricular haemorrhage; (f) cortical vein/dural sinus thrombosis (hyperintensities represents acute clots in cortical vein and superior sagittal sinus)
Brief Aetiology and Pathophysiology of Ischemic Stroke and Intracerebral Haemorrhage
Ischemic strokes represent at least 85 % of all strokes. Sometimes, the cerebral infarctions with a small deficit are called “minor strokes”. Cerebral ischemia represents a consequence of arterial or arteriolar occlusion leading to the blood flow reduction. Possible ischemic stroke mechanisms (aetiologies) include ischemic strokes of atherotrombotic (30 %), lacunar (20 %) or cardioembolic origin (30 %); of other known aetiology, e.g. arterial dissection, vasculitis, hemodynamic infarctions, thrombophilia, cortical vein or dural sinus thrombosis (5–10 %); and 5–10 % are strokes of unknown cause termed cryptogenic strokes [54, 56].
It is important to mention that therapeutic and preventive strategies depend on the proper diagnosis of the stroke cause. Typical example is an indication for anticoagulation versus antiplatelet therapy (secondary prevention) in patients with cardioembolic versus non-cardioembolic strokes. Identification of the exact cause is also important for prognosis and treatment of additional risk factors.
Intracerebral haemorrhages (ICHs) are divided in the primary and secondary. Primary ICHs are caused by a rupture of cerebral artery/arteriole, and are typically associated with uncontrolled hypertension. Based on the localization apparent on neuroimaging methods, they can be divided into two main types: typical and atypical. The typical ICH is located in deep brain structures supplied by perforating arteries. The atypical ICHs are located more superficially (e.g. lobar haemorrhages). Atypical ICHs (20 % of all ICH) are usually secondary to medical conditions different to hypertension, such as coagulopathies, arterio-venous malformations, other vasculopathies, and tumours.
From clinical point of view, presentation of ICH is very similar to acute ischemic stroke, and therefore ICHs cannot be differentiated from acute ischemia based only on clinical examination. ICH manifestation corresponds to its location and volume, and also to the bleeding progression. Because treatments of ischemic and haemorrhagic strokes differ, brain CT or MRI are essential for differential diagnosis and treatment decision-making [57–60].
microRNA in Acute Ischemic Stroke
There are numerous roles of miRNAs in acute ischemic stroke—e.g. intracellular miRNAs participate in pathophysiology of ischemic stroke via affecting the target genes expression involved in atherosclerosis, angiogenesis and/or neuro-inflammation [61]; extracellular miRNAs serve as mediators of cell-to-cell communication affecting pathophysiology and course of the disease. Molecules released into the extracellular space might represent clinically valuable biomarkers. It was shown that almost any ischemic conditions (coronary artery disease, peripheral artery disease) lead to alteration in circulating miRNA levels [62]. The tissue-specific miRNAs are released into the circulation after cell damage or death, and thus indirectly indicate the organ damage [63, 64]. Since the levels of circulating miRNAs are not random and exact mechanisms of miRNA secretion/excretion still need to be clarified, these miRNAs may even reflect the course of disease and bring to clinicians information regarding patients prognosis and outcome (e.g. in myocardial infarction, specific miRNA profile may predict development of heart failure [65]; in stroke, miRNA profiles were shown to be predictive in stroke recurrence [66], etc.).
Within the field of ischemic stroke, miRNAs have been studied both in different animal models and human stroke populations. In terms of miRNAs detection both principal approaches, i.e. studying the expression profiles of many miRNAs at the same time (“miRNA profiling”), as well as candidate-miRNAs approach (i.e. focusing more deeply on a subset of miRNAs, their possible targets and biological roles) have already been employed.
Within the following subchapter, we will focus on profiling studies giving a rationale for further miRNA studies in the field of ischemic stroke.
Animal Models of Stroke
Experimental stroke models used in following studies comprise mainly of cell culture (varying from generally accessible cell cultures such as HEK cells, N2A cells, to the primary cultured cortical neurons) of oxygen-glucose deprivation (OGD) simulating hypoxic-ischemic conditions by restriction of oxygen and glucose or pure hypoxia (e.g. for 30 to 60 min). Otherwise the H2O2 application responsible for simulating the reactive oxygen species (ROS) specific damage has been induced and studied. In studies focused on the roles of progenitor cells after acute ischemia, the subventricular zone (SVZ) cells has been isolated and studied in hypoxic-ischemic conditions.
In animal model studies, models of the middle cerebral artery occlusion (MCAO) have been typically used but with different approaches to the induction of occlusion (usually lasting from 60 to 120 min followed by varying periods of reperfusion and sampling). The way of MCAO technique has been also highly variable (using electro-coagulation, embolic techniques or complete mechanical obstruction, etc.). In terms of animals, spontaneously hypertensive rats (SHR), Wistar rats, Sprague-Dawley rats or C57BL/6J mice have been used.
In human studies, there is no possibility to simulate experimental stroke, thus only patients admitted to hospitals with stroke symptoms might be involved in miRNA sampling from different bodily fluids. So far, only the blood and its derivatives, and/or cerebrospinal fluid have been used in human stroke research.
Profiling microRNA Studies in Acute Ischemic Stroke
Up to date several miRNA profiling studies were performed using both animal model of stroke [67–72] and human stroke patients [73–78], in the animal studies using either brain tissue or blood or both; in the human studies using bodily fluids of patients after ischemic event.
Animal Profiling Studies
The very first miRNA profiling in animal stroke model was performed by Jeyaseelan et al. in 2008. Using MCAO model, they performed screen for 236 various miRNAs in both blood and brain at two different time points (20/106 and 25/82 differentially expressed miRNAs at 24 and 48 h in blood/brain were identified). Moreover, the expression of following miRNAs was detected for the first time in the rat brain: miR-126, miR-129, miR-129*, miR-145, miR-181a/b/c and miR-185.
Focusing on the specific group of miRNAs the authors confirmed several targets: laminin-1 and integrin-1 as targets of miR-124, VSNL1 (neuronal calcium sensor) as a target of miR-290 (and possibly also miR-124a); aquaporin (AQP4) as a target of miR-30a-3p and miR-383, and matrix metalloproteinase 9 (MMP9) as a target of miR-132 and miR-664 [69]. In their following study, they focused on miRNAs expression in later phases of stroke (48–168 h after ischemic stroke) and identified: miR-21, miR-142-3p, miR-142-5p and miR-146a to be increased and miR-196a/b/c, miR-224 and miR-324-3p to be decreased as compared to the acute phase. Moreover, levels of miR-206, miR-290, miR-291a-5p and miR-30c-1* positively correlated with infarct volume [70].
Further, Dharap and colleagues used SHR and extended findings from the first study of Jeyaseelan by sacrificing animals at five different time points (3, 6, 12, 24 and 72 h). It was shown that 49 miRNAs were dysregulated after transient MCAO, 24 miRNAs were upregulated and 25 showed downregulation at least one of these time points. Other subsets of miRNAs were detected at two or more time points showing that expression of some miRNAs (e.g. miR-140, miR-145, miR-260, miR-292-5p) tended to increase and of other miRNAs (e.g. miR-376-5p, miR-153) tended to decrease over time, while other miRNAs were altered only transiently (e.g. miR-29c) or permanently without the specific increase or decrease (e.g. miR-344-3p).
The authors further focused on miR-145 and its target superoxide dismutase (SOD2) using antagomir against miR-145 showing that inhibition of miR-145 led to SOD2 upregulation and consequently protected the neurons from cell death [67]. Similarly to Dharap, Gubern et al. in 2013 also proved the expression change of 32 miRNAs during acute phase of stroke (30 min and 6 h) and late stroke phases (7 and 14 days). Their group further focused on miR-347 and its targets (Acsl4, Bnip31 and Phyhip) showing its importance in regulation of neuronal cell death [68].
Compared to previously mentioned studies, Selvamani et al. [71] focused on stroke from slightly different point of view—studying effect of age and sex on miRNA expression (miR-127-3p, miR-335, miR-543, miR-139-5p, miR-33a, miR-338-3p, miR-222, miR-15b, miR-92a, miR-424, miR-495 and miR-33) in blood and brain at day 2 and 5 after the MCAO. Interestingly, on the day 2, differences in miRNA levels were affected mainly by age, and on the day 5 mainly by sex showing the need to keep in mind the confounding factors.
Animal profiling studies definitely created a great background for the studies mentioned further by identifying a wide range of miRNAs altered in brain tissue after stroke. These studies showed that a large number of miRNAs was altered in rat brain after ischemic event and that this set was not completely the same as the set of blood identified miRNAs. Nowadays, it has been revealed that after stroke, also other organs than brain are involved in the complex body reaction affecting patient outcome. Thus identification of other miRNAs involved, e.g. in inflammation, or being other organ specific (e.g. finding of liver specific miR-122 to be increased in blood after stroke) may further stimulate the research in order to better understand the complex effect of stroke on the organism.
Human Profiling Studies
Unlike the animal profiling studies, where brain tissue is available and enable much deeper focus on molecular biology of stroke, only bodily fluids are available in ischemic stroke in humans for miRNA analysis.
One of the first attempts to identify circulating miRNAs in peripheral blood of 19 patients after stroke was performed by Tan et al. in 2009. Relatively young patients (aged 19–49 years) were enrolled and from 836 miRNAs studied in total, 157 were found to be dysregulated after stroke (138 upregulated, 19 downregulated). Out of these let-7f, miR-126, -1259, -142-3p, -15b, -186, -519e and -768-5p were consistently downregulated in all patients independently of the stroke subtype (according to TOAST classification).
Interestingly, miRNA clustering revealed different expression patterns in patients with good and poor clinical outcome defined as modified Rankin scale (mRS) ≤2 versus mRS >2. Although being a small-sized study enrolling only young individuals, the very promising results definitely identified miRNAs potentially useful as biomarkers of acute stroke and thus much larger studies were performed by the same group in 2013 [76] and 2014 [74].
In the first mentioned study, authors studies no-risk or low-risk patients with stroke, to avoid a potential effect of atherosclerosis, hypertension or diabetes on circulating miRNA profiles and identified 293 miRNAs out of whose 21 miRNAs presented with similar expression in all stroke samples [76]. Four of these, miR-25*, -34b, -483-5p and miR-498, were shown to be downregulated in all cases.
In the latter mentioned study, the authors involved two groups of stroke patients: relatively young (≈45 years) and older cohort (≈60 years) after stroke. The latter cohort displayed a number of age-related comorbidities, which also was a reason to involve healthy control (≈40 years) and patients with metabolic syndrome without the history of stroke as two control cohorts [74]. Out of 314 miRNAs studied, downregulation was observed in 58 and upregulation in 47 miRNAs in acute (24, 48 h up to 7 days) or late phase (from 2 months to 2 years) of stroke. Sixty-three miRNAs were found to be altered at both phases and five upregulated miRNAs, miR-27a*, miR-125b-2*, miR-422a, miR-488 and miR-627, showed high AUCs for patients after stroke, compared to those with metabolic syndrome. Moreover, authors showed that clustering of 32 miRNAs enabled distinguishing among individual stroke subtypes according to TOAST classification.
Another profiling after stroke was performed by Wang et al. [78]. This study group focused on early stroke detection using MRI in 136 stroke patients within 24 h from stroke onset. Based on the MRI finding, MRI(+) and MRI(−) stroke patients were distinguished and profiles were taken for these patients together with 116 healthy subjects. Altogether, 42 miRNAs were chosen for further confirmation and out of these, 13 miRNAs were confirmed as upregulated and 4 miRNAs as being downregulated. miR-106b-5p and miR-4306 showed gradual expression and being the lowest in controls, higher in MRI(−) and the highest in MRI(+) patients. Contrarily, miR-320e and miR-320d showed opposite trend, i.e. being downregulated in MRI(−) and more downregulated in MRI(+) patients, thus being identified as potential biomarkers of acute stroke.
One of the very recent profiling studies of human serum was performed by Li et al. This study identified 115 differentially expressed miRNAs in ischemic stroke patients. Out of whose miR-32-3p, miR-106-5p, miR-1246 and miR-532-5p were identified as potential stroke biomarkers [79].
Another attempt to study specific roles of miRNAs in stroke was performed by Jickling et al. In this study the authors determined miRNA profiles from peripheral blood mononuclear cells, not from plasma or serum [73]. This different approach enables to study leukocytes expression profiles and reveal a potential interconnection between immunity, inflammation and stroke. In conclusion miR-122, miR-148a, let-7i, miR-19a, miR-320d and miR-4429 were decreased and miR-363 and miR-487b increased in the cells of patients with stroke and thus the potential regulation of leukocyte adhesion, extravasation and thrombi formation was proposed [73].
Most recently, Sorensen et al. published interesting paper identifying potential miRNA biomarkers of acute stroke not only from blood but also using the cerebrospinal fluid [75]. At the time of this manuscript preparation, only abstract of this study was available. The authors identified miR-151-3p and miR-140-5p to be upregulated and miR-18b-5p to be downregulated in blood after stroke and miR-523-3p was identified in more than 50 % of patients and in none of the controls in the cerebrospinal fluid. These results, together with results from other research groups mentioned above or further clearly demonstrate a potential of miRNAs as biomarkers of acute ischemic stroke and the need for complex studies taking into account not only the traditional cardiovascular and metabolic risk factors, sex, age but also using control cohorts with other neurological disorders that can resemble stroke.
Candidate microRNA Studies
Following section summarizes up-to-date information regarding animal and human studies in acute stroke with the special emphasis put on the let-7 family, miR-21, miR-29 family, miR-124, miR-145, miR-181 family, miR-210 and miR-223. Roles of other miRNAs are briefly summarized in the last subsection. Overview of below described miRNAs is provided in Tables 9.1 and 9.2, detailed description can be found further in the text.
let-7 Family
let-7 family represents a group of nine miRNAs termed let-7a to let-7i. Being one of the first miRNAs even described with important functions in C. elegans developmental timing [111], its functions in humans has been extensively studied and except of participating in tumorigenesis, angiogenesis and immunity, let-7 family represents one of the most abundant miRNA families in the brain, where it fulfils crucial roles in neurogenesis and differentiation, as recently reviewed [80].
In the pathophysiology of stroke, let-7 may be involved in neurogenesis [111], angiogenesis and inflammation. It is one of the miRNAs transferred via exosomes affecting the gene expression of recipient cells in the atherosclerosis process [112, 113]. Expression of let-7 family members was repeatedly shown to be downregulated in above-mentioned profiling studies [68, 69, 71], and specific blockade of let-7f using antagomir led to increased neuroprotection in the rat model via affecting the insulin like growth factor (IGF-1) signalling pathway [81]. It can be hypothesized that a downregulation of let-7 family members after the stroke leads to activation of neuroprotective mechanisms mediated at least partly by the IGF-1 signalling.
miR-21
In animal brains, miR-21 expression has been reported in profiling studies as increased [69, 77] and being even more dominantly increased in small artery stroke patients [77]. miR-21 is generally known to be involved in ischemia and hypoxia related processes and also has a strong antiapoptotic effect [114].
In the study by Buller and colleagues, expression of miR-21 has been observed to be significantly increased in ischemic boundary zone as compared to contralateral neurons in the MCAO animal model. However, in OGD cultured cortical neurons, no such upregulation of miR-21 has occurred [82]. On the other hand, when miR-21 was introduced to the OGD-cells, much better survival due to decreased apoptosis via downregulation of Fas-Ligand has been proven [82]. In accordance with this, reoxygenation of the N2A cells after OGD increased miR-21 levels and also promoted N2A cells survival [83].
Taking into account that miR-21 is known to be involved not only in cerebral, but also in myocardial ischemia, where it was shown to be produced by fibroblasts in the site of infarction having antiapoptotic effect on surrounding cardiomyocytes [115], strategies leading to increased miR-21 expression may potentially serve as novel future therapeutic strategies in ischemic stroke.
miR-29 Family
miR-29 family is represented by four members: miR-29a, -29b-1, -29b-2 and 29c. With many potential targets of all family members, there is still a controversy, whether miR-29 is pro-survival or pro-apoptotic since the upregulation of miR-29b has been recognized as a neuronal survival factor interfering with apoptosis by affecting Bcl-2 and BH3 pathways [84, 116], while the downregulation of miR-29 protects hearts against ischemia-reperfusion injury [117]. Luciferase target assays have indicated that miR-29 family members target both pro- and anti-apoptotic Bcl-2 family members, and thus it is necessary to evaluate this miRNA family functions in the context of disease and model chosen in particular studies [117].
Focusing more on stroke, both the downregulation [85, 87, 116] and upregulation [86, 88] of miR-29 family members have been observed in animal MCAO models with various interpretation of observed findings. Khanna et al. and Pandi et al. reported miR-29b and miR-29c downregulated in ischemic area. This loss of miR-29b/c participated on ischemic brain damage and can be prevented by oral administration of α-tocotrienol or by re-induction of both mentioned miRNAs in the brain—all these actions resulted in decreased volume of infarct and promoted cell survival. Conversely, recently Huang et al. reported the downregulation of miR-29c after the fastigial nucleus stimulation, which is known to be neuroprotective and indeed, overexpression of miR-29c resulted in increased infarct volume and poor neurological outcomes [87]. In accordance with Huang et al., results of Shi et al. showed that miR-29b was upregulated after ischemic event and promoted neuronal cell death by targeting Bcl2L2 [86].
Slightly different approach was chosen by Dhiraj et al. [88], whose group decided to study miRNA expression in salvageable tissue called penumbra. After the three vessel occlusion followed by 24 h of reperfusion, unilateral hemispheric lesion was induced and comparison of miRNAs expressed in brain ischemic cells and cultivated neuronal cells has been performed. The miR-29b-2, miR-19b, miR-339-5p and miR-341 were found to be dysregulated in both models of ischemic damage suggesting their possible participation in the regulation of gene expression in salvageable ischemic penumbra. The authors suggested also above-mentioned Bcl-2 targeting as one of potential mechanisms [88].
miR-124
miR-124 is almost exclusively expressed in the central nervous system and participates in the regulation of neuronal differentiation and adult neurogenesis [118], which makes this miRNA to be referred as “brain-specific miRNA” [119]. Already in 2009 Laterza et al. showed that brain injury (induced by MCAO) caused miR-124 upregulation in plasma, similarly to elevation of miR-122 after liver injury and miR-133 after muscle injury [119] and suggested this miRNA as possible tissue-specific biomarker. Similarly, Weng et al. using the expression profiling of 671 miRNAs in various tissues (brain, heart, lung, liver, kidney, colon, skin, skeletal muscle and pancreas) confirmed miR-124 to be preferentially expressed in the nervous system, especially in the cerebellum, cerebrum and occipital and temporal lobes, and to be present in serum 6 and 48 h after the MCAO in rats [72]. Later on, elevation of circulating miR-124 was also confirmed in the profiling study by Jeyaseelan and colleagues [69]. Moreover, they reported the visinin like 1 protein (VSNL1) , a neuronal calcium sensor abundantly expressed in the central nervous system as the miR-124 target in animal stroke model [69]. Nowadays, VSNL1 is a protein studied as a potent biomarker of various dementias [120] and also miR-124 is supposed to be involved in pathophysiology of dementia by targeting β-site APP cleaving enzyme 1 (BACE1) [121]. Studies of post-stroke related neuronal damage, post-stroke cognitive decline and dementia development should definitely focus on this possible interconnection. Concerning miR-124, other numerous functions within the brain tissue, several other targets and pathways have already been identified and are summarized in Table 9.1.
Interestingly, results concerning the miR-124 up- or downregulation after ischemic insult are contradictory, which is to our opinion caused by differences among individual studies concerning sample size, MCAO induction technique, sample collection, RNA isolation, choice of internal control and other aspects.
There are two studies reporting miR-124 downregulation after stroke in animal model of MCAO. Zhu et al. reported Ku70 (DNA repair protein), upregulation after MCAO and this upregulation may further be induced via the antagomir-124 application prior to the MCAO resulting in decreased volume of infarction [89]. A slightly different study was performed by Liu and colleagues, where the authors reported miR-124 downregulation 7 days after the MCAO. This was correlated with neuronal progenitor cells proliferation. Artificial administration of miR-124 caused decrease in progenitor cells proliferation and increase in their differentiation, thus also promoting global damage to the brain [90]. Thus, both of these studies have suggested miR-124 downregulation as a protective mechanism for brain tissue repair after stroke.
However, in two other studies, similar properties of miR-124 upregulation, i.e. preventing tissue-injury, were described [91, 92]. In the first study mentioned, miR-124 upregulation after both OGD and MCAO in cell-line and animals, respectively, were confirmed and this prevented neuronal apoptosis. Authors revealed Ups14, (de)ubiquitination-related protein, as a target of miR-124 and revealed that via Ups14 targeting, miR-124 indirectly increases levels of RE1 silencing transcription factor (REST), which upregulation was reported in neurons destined to death [91]. Thus, miR-124 application led to decreased infarct volume size and also to decreased functional impairment, determined by the Rotarod test, tight rope test and modified Morris maze test. In the latter study, miR-124 upregulation in ischemic penumbra was reported and functional studies using miR-124 knockdown/increase led to infarct volume size increase/reduction, respectively. Similarly, in the primary cortical neurons, OGD caused miR-124 upregulation and miR-124 agomir and antagomir delivery reduced or promoted cell death. These effects of miR-124 are probably mediated via Bcl-2 and Bcl-xl pathways [92].
Most recently Liu and colleagues elegantly demonstrated that miR-124 upregulation in infarcted area caused the downregulation of inhibitory member of the apoptosis-stimulating proteins of p53 family (iASPP), and thus affecting the p53-mediated neuronal cell death [93]. Compared to the aforementioned studies by Doeppner and colleagues and Sun and colleagues, who reported upregulation of miR-124, this is not beneficial for neuronal cells—blockage of miR-124 with specific antagomir caused upregulation of iASPP and this resulted in reduced infarct size and reduced neuronal cell death.
It can be concluded that miR-124 is brain-specific microRNA with plentiful roles in the regulation of neuronal cell death, apoptosis and proliferation. Since the results of so far conducted studies are contradictory, more studies are needed to confirm the exact roles of miR-124.
miR-145
miR-145 should be briefly mentioned also in the stroke field, even though it is much more connected with the vessel biology. miR-143/145 cluster is involved in the function of ECs and VSMCs; however, its levels have been reported to be upregulated in brain tissue after ischemic insult [67]. Using bioinformatics prediction, superoxide dismutase 2 (SOD2) was revealed as miR-145 target and application of antagomir against miR-145 led to SOD2 increase, however, without any significant increase in the neuroprotection [67]. Recently, miR-145 was shown to be connected to microglia function and being identified as one of the p53 targets during ROS exposition [122]. Since oxidative stress is connected with reperfusion injury, potential roles for miR-145 in oxidative stress control, exceeding its known roles in vessel biology, may come up in the future.
miR-181 Family
miR-181 family represents a highly conserved group of miRNAs that consists of four members named consecutively miR-181a, -181b, -181c and 181d, and that is highly expressed in mammalian brain [123]. Main roles of this miRNA family was reported in the hematopoiesis and inflammation [124]; however, from the molecular point of view, miR-181 family targets multiple mRNAs of proteins involved in apoptosis (e.g. Bcl-2 family of antiapoptotic proteins [125]) or in tissue protection (e.g. protective proteins of endoplasmatic reticulum or heat shock proteins [94, 126]). Ouyang and colleagues focused repeatedly on various aspects of miR-181 functions in the context of cerebral ischemia concerning regulation of oxidative stress or functions of molecular chaperons [126, 127]. In their very first study, they identified miR-181a to be upregulated in ischemic core and conversely downregulated in the surrounding penumbra corresponding with the potential of the cells to die in core and survive in penumbra [94]. Accordingly, supplementation or inhibition of miR-181 in cultured astrocytes increased and reduced astrocytes cell death, respectively, similarly to effects observed in vivo. One of the targets found to be responsible for observed effect was GRP78, one of the well-known heat shock proteins—if GRP78 levels were maintained stable, miR-181a administration did not promote the cell death [94]. Concerning further delayed neuronal cell death, miR-181 was shown to indirectly regulate the glutamate transporter (GLT-1), which induction is known to prevent the brain from excitotoxicity induced by neurotransmitter glutamate [128].
In agreement with the previous studies, application of miR-181a mimics prior [95] or after [97] the ischemic insult resulted in neuroprotection. Especially the study by Xu and collaborators has shown a great potential of miR-181 application. Since in the clinical practice, clinicians are typically faced with patients after the onset of stroke with no possibility to pretreat them. Xu and colleagues applied miR-181 antagomirs either intravenously (1 h after the MCAO) or intracerebroventricularly (2 h after the MCAO) and interestingly both ways of application have shown reduced infarction volume (at about one third at 48 h after reperfusion). Neurologic deficit was assessed by the Rotarod test and was significantly improved as well as the overall 4-weeks survival (90 % versus 72 % in sham) and neurobehavioural recovery. In conclusion, miR-181 antagomir treatment showed great promises for the future therapeutic applications in the early post-stroke treatment.
miR-210
miR-210 , a master hypoxia-miR, represents a hypoxia-induced and anti-apoptotic miRNA with approximately 35 specific transcripts as its direct or indirect targets [129]. Its overexpression in normoxic human endothelial cells stimulates formation of capillary-like structures, and increases cells migration and differentiation [130]. Consistent with the reported induction under hypoxic conditions via HIF-dependent and independent pathways [129], miR-210 expression was reported to be higher in ischemic brain, where it plays many protective roles against ischemia induced injury [98, 99]. In the setting of cerebral ischemia in rat or mice, increase in miR-210 by lentiviral vector led to increased number of new vessels [99] and progenitor cells in subventricular zone [98], thus resulting in increased angio- and neurogenesis, and preventing mice from ischemia-induced injury. To sum up miR-210 represents another promising target for stroke therapeutics.
miR-223
From the more deeply studied miRNAs, as the last one miR-223 will be mentioned. Together with miR-130a and miR-320, this miRNA was reported to target aquaporin genes, especially aquaporin 4 that is typically expressed in the brain [131]. miR-320a was shown to directly affect the expression of aquaporin 4 and aquaporin 1. Blockade of miR-320a with antagomir led to increase in the aquaporin expression and reduction of infarct volume [131]. Similar results were obtained with the use of antagomir-130a. Reduction in infarct size and increased neuronal recovery were observed after the application [132].
miR-223 is of further interest, since except of its proved aquaporin targeting [69], it was also reported as a platelet-secreted [133] and lipoprotein particle-transferred [134] miRNA, playing one of the central roles in the cholesterol metabolism [135]. Similarly to miR-181 mentioned above and miR-107 mentioned further, miR-223 also has a potential to protect brain from glutamate excitotoxicity by targeting the glutamate receptor subunits GluR2 and NR2B [100]. Moreover, in the study by Duan et al. it was observed that miR-223 levels were lower in patients with diabetes mellitus, which promoted platelet activation and increased the risk of stroke development in DM patients [136].
Other miRNAs in Ischemic Stroke
From the profiling studies mentioned at the beginning of the chapter it is obvious, that more miRNAs are involved in the pathophysiology of acute stroke than those described above. However, information regarding their function still need to be determined or is of a limited extent, thus we provide only basic information regarding their pathophysiologic, diagnostic or therapeutic potentials.
Due to its involvement in general cellular processes, miR-17-92 cluster has been described to be involved in the pathophysiology of almost any disease [137], including stroke [101]. In the subventricular zone of animals after MCAO, miR-17-92 cluster levels were increased and this, via targeting of PTEN, increased a proliferative capacity of neural progenitor cells, as confirmed also in vitro.
Following the numerical order, other miRNA involved in stroke is miR-103 . It is responsible for a regulation of Na+–Ca2+ exchanger (NCX). Its downregulation by a specific antagomir reduced brain damage and neurological deficit in experimental animals [102]. Like above-mentioned miR-181 family, also other miRNAs were shown to affect the glutamate signalling (particularly miR-107 [103]) or target heat-shock proteins (particularly HSPA12), e.g. miR-134 [104, 105]. Another miRNA recently described to promote stroke damage is miR-200c. Its blockade increased levels of Reelin, thus promoting neuronal migration and synaptogenesis, resulting in neuroprotection [107]. Concerning angiogenesis, similar effects to miR-210 were observed in miR-376-5p. This miRNA affects the VEGF/Notch signalling modulating angiogenesis as well [108].
Last but not the least, miR-424 was shown to be downregulated in brain tissue within the profiling studies [69] and it was also shown to be downregulated in peripheral leukocytes in patients after stroke [109, 110]. Restoration of miR-424 activity led to decrease in infarct volume and neuronal cell death, which was associated with decreased microglia activation [109] and reduced oxidative stress [110].
Candidate microRNAs as Biomarkers of Acute Stroke
Using animal models, elevation of serum miR-124 was reported in two independent studies and this upregulation was consistent for at least 48 h after stroke induction [72, 119], which would make miR-124 as a potential stroke biomarker. However, no correlations with outcome of experimental animals or infarct size were observed [72, 119]. Interestingly, in human studies, levels of miR-124 were reported both to be upregulated [138] and downregulated [139] after acute stroke. In the study by Leung et al., upregulation of miR-124 was prominent only in the early phase (below 6 h). In the further sampling, levels of miR-124 were significantly lower compared to acute phase [138]. Leung et al. moreover showed that miR-124 levels were higher in patients with haemorrhagic stroke compared to ischemic stroke only [138]. In another study by Liu et al., miR-124 levels were downregulated and they negatively correlated with infarct volume, CRP levels and levels of matrix metalloproteinase 9 (MMP9), thus somehow reflecting damage of neural tissue and inflammatory activity. However, no correlation with stroke severity defined by NIHSS was observed [139]. Similar properties were observed also for another neuri-miR, miR-9. The true diagnostic potential of miR-124, although being termed as brain specific, needs to be determined in larger multicentric studies since the results of currently conducted studies are contradictory.
Leaving miR-124 and moving further with human studies, let-7, miR-21, miR-30a and miR-126, miR-221 levels were studied as potential diagnostic and prognostic biomarkers.
Concerning let-7, miR-30a and miR-126, altogether 247 patients at different time points after stroke (in the acute phase within 24 h, in the subacute phase within 1 week and in the chronic phases within 48 weeks after stroke) were enrolled. It was observed that let-7 levels were decreased after stroke with a slow restitution after the 24th week. Interestingly, levels of let-7 were more profoundly decreased in patients with stroke of atherosclerotic aetiology [140]. Cut-off value for the let-7 was calculated to 1.675 at 24 h with the sensitivity 92 % and specificity 84 %.
Another larger study was performed in 233 patients (partly patients with ischemic stroke and partly patients with carotid atherosclerosis without ischemic stroke) and 157 controls focusing on miR-21, miR-221 and miR-145 levels in the serum after ischemic stroke [50]. miR-21 and miR-221 showed opposite trends, i.e. miR-21 being upregulated and miR-221 being downregulated in patients compared to the controls. Concerning miR-145, its levels were not detected in more than 50 % of study subjects and its potential for stroke diagnosis is thus not very promising [50]. However, if the whole blood RNA was isolated, miR-145 levels were shown to be upregulated after ischemic stroke in a smaller study by Gan et al. [49] and also in the profiling study performed by Sepramaniam et al. [74]. Gan et al. moreover suggested increase in miR-145 to be predictive for better outcome, due to miR-145 targeting of KLF-4/5 and its effect on reendothelization [49].
Promising results were observed for miR-210, previously mentioned as hypoxia-miR, which levels were reported to be downregulated in peripheral blood leukocytes in patients after stroke. Decrease in miR-210 levels in these patients was continuous and deepened within 2 weeks from stroke onset [141]. Moreover, after the correlation with NIHSS and mRS, patients with higher miR-210 levels had better prognosis, compared to patients with the lowest miR-210 expression. Zeng et al. further determined miR-210 peripheral blood mononuclear cells (PBMC) levels together with the levels of other potential biomarkers, including various cytokines (e.g. IFNγ, IL-1, IL-6, TNFα and others) and haemostatic markers (fibrin and its degradation products FDP, D-dimers, etc.). Combination of miR-210, FDP and IL-6 had even higher sensitivity and specificity for stroke outcome prediction (defined by mRS after 3 months) compared to the use of individual markers alone [142].
Last but not the least, also miR-223 was suggested as a potential biomarker of acute stroke [143]. After dissociation of erythrocytes, RNA was isolated from the remaining cells and miR-223 levels were determined to be increased after stroke with more prominent increase in large and small vessel stroke subtypes. Moreover, a negative correlation with NIHSS (and in animal part of the study with infarct size) and a positive correlation with circulating IGF-1, one of miR-223 targets, were observed. Due to its pleiotropic effect, miR-223 specificity for stroke needs to be tested in other consecutive studies.
Recently, Kim et al. focused on atherosclerosis related miRNAs in the diagnostics of acute stroke. They revealed that miR-126 levels correlated with brain atherosclerotic damage and that levels of miR-17 were increased after acute stroke being also predictive of early stroke recurrence (within the study period, thus probably 1 year—only abstract was available to authors during the manuscript preparation [66]).
Future Directions
In conclusion we would like to point out the tremendous development and progress that has been done regarding the roles of miRNAs in ischemic stroke. Studies above are definitely informative about the involvement of miRNAs in the stroke pathophysiology and also about their potential clinical utilities as diagnostic, prognostic and even therapeutic tools.
For future research, it is needed to define the standardized protocols of miRNAs detection, extraction and isolation. Current studies differ and vary a lot in the source of miRNAs—in animal studies, sometimes ischemic core and sometimes penumbra have been used and this has not been quite often precisely specified; in the human studies, miRNA source ranged from the whole blood through plasma or sera to the isolated cells only. Also, various internal controls are used, sometimes using additive cel-miR-39, sometimes using miR-16 or another defined ubiquitous miRNA. Universal internal control should soon be established to normalize the data from various studies and obtain clearer and more normalized results. Also the need of multicentric studies employing more than 300 subjects is anticipated and this inquires specific needs of proper and universal sample storage protocols.
Last but not the least, the miRNA potential in stroke therapy should be further investigated and focused not only on effects of injected ago- or antagomiRs, but also determining potential side effects, mechanisms of uptake and elimination. Also, the ways of application should be precisely defined in order to increase specific targeting of brain tissue.
Intracranial Aneurysms
Epidemiology of Intracranial Aneurysms
Intracranial aneurysms represent acquired lesions of cerebral arterial wall occurring in 0.5–3 % of general population and accounting for 80–85 % of non-traumatic subarachnoid haemorrhages (i.e. bleeding into subarachnoid space).
These saccular-shaped lesions are typically localized in proximal arterial bifurcations. Typical anatomical localizations are as follows: internal carotid artery (ICA), anterior communicating artery (ACom), middle cerebral artery (MCA), tip of basilar artery (BA) and arteries of the cerebellum.
Risk factors associated with higher occurrence include higher age, female sex, cigarette smoking, hypertension and genetic predisposition (e.g. autosomal dominant polycystic kidney disease, Marfan’s syndrome, Ehlers-Danlos syndrome type IV) [144–147].
Clinicians are faced with a decision regarding an optimal management of intracranial aneurysms; however, there are still many unsolved controversies regarding the risk of rupture and treatment of smaller asymptomatic aneurysms due to lack of randomized control trials. Decisions are thus made regarding patient history data, size and location of aneurysm/s, expert opinion and guidelines.
On the one hand, the particular effect of aneurysms growth on subsequent risk of rupture is not determined; on the other hand, patients with obvious enlargement should be strongly considered for interventional treatment (endovascular coiling or neurosurgical clipping, Fig. 9.3 [148]).
Endovascular coiling of ruptured anterior communicating artery aneurysm, digital subtraction angiography images (DSA images). Seventy-five-year-old female with a ruptured aneurysm as a source of subarachnoid haemorrhage indicated for interventional treatment. (top) Subtracted right internal carotid artery angiograms in antero-posterior (top left) and lateral (top right) view showing aneurysm (open arrow) of the anterior communicating artery of size 12 × 6 mm (bottom). Final control series after the endovascular coiling showing almost total obliteration of the aneurysmal sac. A1 A1 segment of the anterior cerebral artery, ACA A2 and A3 segments of the anterior cerebral artery, ACom anterior communicating artery, ICA internal carotid artery, MCA middle cerebral artery
For those treated conservatively, proper management of hypertension, smoking cessation and repeat CT angiography or MR angiography are strongly recommended (Fig. 9.4) [144].
Management of residual aneurysm sac after endovascular coiling. Forty-two-year-old female with anterior communicating artery aneurysm indicated for endovascular coiling. A tiny residual aneurysm was revealed on MRI control scanning 6 months after the procedure (conservative approach with regular MRI controls was recommended). (top left) CT angiography showing the aneurysm (open arrow) of the right anterior communicating artery (top right) MR angiography revealing a residual filling of the aneurysm (open arrow), size of 2 mm (bottom) MRA angiography reconstruction of the circle of Willis. A1 A1 segment of the anterior cerebral artery, A2 A2 segment of the anterior cerebral artery, ICA internal carotid artery, MCA middle cerebral artery
Biomarkers predicting the clinical course of intracranial aneurysm are still lacking. As long as miRNAs represent potential biomarkers sensitively reflecting the diseases state, maybe their potential role in the monitoring of aneurysms will come up in the near future.
microRNA Profiling Studies and Aneurysms
Animal Studies
Up to date there is only one study using animal model performed by Lee et al. in 2013 [149]. Aneurysms formation was induced by ligation of the left common carotid artery and the posterior branches of both renal arteries in Sprague-Dawley rats. Biological sampling from aneurysms (dissected out of left posterior communicating artery) or from healthy arteries (dissected out of the circles of Willis) were obtained and subsequent miRNA array profiling was done identifying 14 miRNAs upregulated (miR-1, miR-21, miR-22-5p, miR-24-1-5p, miR-26b, miR-29a, miR-29b, miR-29c, miR-101b, miR-140, miR-147, miR-181c, miR-223, miR-451) and 6 miRNAs downregulated (miR-92b, miR-138, miR-181d, miR-433, miR-489, miR-551b) in aneurysmatic vessels. Detected miRNAs are known to be involved in inflammation, apoptosis or angiogenesis and more detailed studies are definitely needed to validate the profiling results and to better understand the intracranial aneurysms development.
Human Studies
Unlike in the case of stroke in human studies biological material other than bodily fluids can be collected when the intracranial aneurysms (IAs) are surgically treated. So far, there were two profiling studies using tissue obtained from patients during the surgery and two studies focusing on detection of intracranial aneurysms using circulating microRNAs.
In the study by Jiang et al. (2013) microarray analysing of full-thickness vessel wall samples from 14 ruptured IA patients and 14 controls was made. Thirty differentially expressed miRNAs were found to be dysregulated and 18 miRNAs were found to be significantly different between IAs and control group (miR-1, miR-7-1-3p, miR-23b-3p, miR-24-1-5p, miR-28-5p, miR-28-3p, miR-29b-2-5p, miR-29c-5p, miR-29c-3p, miR-133a, miR-133b, miR-140-3p, miR-143-5p, miR-143-3p, miR-145-5p, miR-145-3p, miR-455-5p) [150]. One year later, Liu et al. screened IA samples and found 157 differentially expressed (72 upregulated and 85 downregulated) miRNAs. Out of these, let-7a, miR-1, miR-30c and miR-101 were shown to be involved in the regulation of programmed cell death, extracellular matrix organization response to oxidative stress, TGF-β signalling pathway and smooth muscle proliferation [151].
Profiling studies focusing on circulating miRNAs were performed by Jin et al. in 2013 [152] and Lie et al. in 2014 [153]. In the study by Jin et al., blood samples of 24 IA patients were analysed. Patients were divided into four groups according to aneurysm characteristics (including aneurysms with/without daughter aneurysm, ruptured aneurysms and angiography-negative group). Aneurysms were located in the ophthalmic artery, basilar artery, posterior communicating artery and internal carotid artery. Altogether 86 miRNAs (69 upregulated, 17 downregulated) were identified by microarray study. In the larger study by Li et al., authors included 40 IA patients (20 with ruptured IA and 20 with unruptured IA) and 20 healthy volunteers (having neurological symptoms, such as headache, indicated for digital subtraction angiography) [153]. One hundred nineteen miRNAs were significantly changed in patients with unruptured aneurysms and 23 miRNAs in patients with ruptured aneurysms (20 of them in both ruptured and unruptured patients). miR-16 and miR-25 were studied in more detail, because these miRNAs were the most abundant in plasma. Using logistic regression, authors proved hypertension and levels of these two miRNAs, as independent predictors for the presence of IAs.
Candidate miRNA Studies and Intracranial Aneurysms
miR-21
miR-21 , as described in previous chapters dealing with stroke, has very important roles in hypoxia, apoptosis and tumorigenesis. Role in the aneurysm formation was suggested in 2012 in the study by Maegdefessel et al.—authors showed increased miR-21 expression in the developed abdominal aortic aneurysm and this upregulation seemed to be protective since miR-21 blockade caused aneurysm enlargement [154]. Shortly after this pioneering attempt, potential roles of miR-21 were also shown in IAs in profiling studies observing also increase in miR-21 levels suggesting a potential regulatory role for miR-21 in controlling aneurysmal growth [153, 154].
miR-26
miR-26 is known to be involved in programmed cell death and response to oxidative stress, TGF-β signalling pathway and importantly in smooth muscle cell proliferation—it is one of the miRNAs involved in the regulation of phenotypic switch of VSMCs through Smad1 and Smad4 proteins [155]. Within the rat model of abdominal aortic aneurysm, levels of miR-26 were found to be decreased, suggesting a potential failure in the regulatory mechanism, since inhibition of miR-26 expression should promote apoptosis and differentiation [155]. On the contrary, in profiling studies both Lee et al. and Li et al. observed increased level of this miRNA in IA rats and patients, respectively [149, 153]. Distinct roles of miR-26 in aneurysm formation thus still needs to be clarified.
miR-29 Family
All three members of miR-29 family (miR-29a, miR-29b and miR-29c, see above) have been associated with aneurysm formation, as shown mostly on abdominal aortic aneurysms—miR-29 inhibition attenuated and miR-29 overexpression promoted abdominal aneurysm formation in various animal models [156–158]. Concerning IAs, contradictory results are currently present. While two profiling studies revealed that levels of miR-29b are robustly downregulated in IA [150, 151], other two indicated miR-29 upregulation [149, 153]. Since miR-29 is known to be involved in the formation of extracellular matrix and fibrotic processes, its potential involvement in aneurysm formation should be definitely studied into more detail [159].
miR-143 and miR-145
Considering miR-143/145 function in the VSMCs, it is not surprising that it has been studied in the field of intracranial aneurysms. In the profiling performed by Jiang et al., miR-143/145 levels were found to be decreased [150]. Elia et al. further focused on miR-143/145 functions in the development of IAs and also detected downregulation of miR-143/145 levels [36]. Downregulation of this cluster is known to promote VSMCs phenotypic switch to “proliferative” phenotype, which may theoretically results in aneurysm formation, however, since the whole research discovering the roles of miRNAs in IAs is at the beginning, more functional studies are still needed to describe precise mechanism leading to IA formation.
Brain Arteriovenous Malformations
Epidemiology of Brain Arteriovenous Malformation
Brain arteriovenous malformations (AVM) represent a complex (nidus) of abnormal arteries and veins that directly fistualize without an intervening capillary bed (Figs. 9.5 and 9.6). They differ in morphology, size, location, particular clinical symptoms and risk of rupture (and subsequent intracranial bleeding). Narrow incidence is estimated to 1.12–1.42 cases per 100,000 person years.
Diagnostic imaging of brain arteriovenous malformations. (top left) CT angiography, scan showing a hyperdense mass of enlarged feeding arteries (arrow head) supplying the nidus (open white arrow) (top right) MRI, T2 weight image. The nidus appears on the scan as a hypointense mass with a feeding artery (bottom left) MR angiography, scan demonstrating a residual filling (open black arrow pointing to the hyperintense area) of the nidus after endovascular embolization of AVM (hypointense region marked with white open arrow) (bottom right) Digital subtraction angiogram demonstrates a blood supply (feeding arteries) of the AVM (open white arrow) from branches of the middle cerebral artery (arrowheads)
Arteriovenous malformation on digital subtraction angiography (DSA). DSA represents a gold standard in a diagnostic management of AVM. It is widely used to delineate location, number of feeding vessels and pattern of drainage. AVM on the angiogram appears as a packed mass of enlarged feeding arteries (white arrow heads) that supply the central nidus (open arrow). Scans present a 19-year-old patient with AVM in the parieto-occipital region. The nidus is fed by vessels from carotid artery and vertebrobasilar circulation. Dilated veins (black arrow heads) drain the nidus into the superior sagittal sinus and transverse sinus. Abnormal venous opacification in arterial phase of DSA represents evidence for pathological shunting; (left) Lateral view of the AVM showing feeding arteries arising from branches of the middle cerebral artery (anterior circulation); (middle) Lateral view showing draining veins into the superior sagittal and transverse sinus; (right) Anteroposterior view showing feeding arteries arising from the posterior cerebral artery (vertebrobasilar circulation). ACA anterior cerebral artery, BA basilar artery, ICA internal carotid artery, PCA posterior cerebral artery, TR transverse sinus, SAG superior sagittal sinus, SIG sigmoid sinus
The first-ever haemorrhage at presentation range from 38 to 68 %. This clinical symptom represents the most common one followed by seizures and/or headache. Nevertheless, the AVMs natural history and risk of rupture is still largely unknown [160–163].
AVM rupture and subsequent intraparenchymal bleeding account for the most devastating complications with overall annual rate of haemorrhage for non-treated malformations 2.1–4.1 %. Based on several multivariate analyses, the nidus size (large nidus is more predictive of increased risk for future bleeding and re-bleeding), deep brain location and deep vein drainage were determined to be significant in risk for spontaneous haemorrhage [164–166].
Studies regarding angio-architecture features (regarding muscular and elastic laminae and presence of intervening brain parenchyma), risk of rupture and AVM evolution are needed in order to help clinicians in treatment decision-making and management.
miR-18a and Cerebral AVMS
Information regarding the role of miRNAs in AVMs are limited to miR-17-92 cluster and out of this cluster almost entirely on miR-18a. As mentioned before, miR-17-92 cluster is known to play multiple functions in almost any tissue [137]. miR-18a represents an important member of miR-17-92 cluster which is involved in the regulation of angiogenesis. Antiangiogenic activity in AVM progression was particularly influenced by miR-18a (together with miR-17, miR-19a and miR-20a). Overexpression of miR-18a and miR-19a regulated the levels of thrombospondin 1 and the connective tissue growth factor (CTGF) [24, 167, 168].
Furthermore, in 2013 Ferreira et al. used AVM samples from six patients in order to determine the effect of miR-18a introduction on AVM-derived brain endothelial cells (AVM-BECs). miR-18a introduction led to increase in TSP-1 and decrease in inhibitor of DNA-binding protein 1, which resulted into better AVM-BECs function suggesting miR-18a supplementation as a potential AVM treatment [168].
Conclusions
Determining the roles of microRNAs in cerebrovascular diseases is still at its beginning; however, much progress in the field has already been done and much progress is yet to be expected. Better understanding of the post-transcriptional regulation of gene expression in endothelial cells, vascular smooth muscle cells, fibroblasts or even neurons or glia may direct further research and development of new drugs based on RNA interference for the treatment of atherosclerosis, stroke or its complications. Studies focusing on circulating miRNAs may reveal new and unexpected communication pathways among individual tissues and these findings may represent a potential source of new biomarkers, reflecting organ damage, or being predictive of the response to therapy or patients prognosis. We can definitely sum up that miRNA research hold great promises for the future therapeutics, diagnostics and for promotion of personalized medicine.
References
Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999;340:115–26.
Gallino A, Aboyans V, Diehm C, Cosentino F, Stricker H, Falk E, et al. Non-coronary atherosclerosis. Eur Heart J. 2014;35:1112–9.
Nam D, Ni CW, Rezvan A, Suo J, Budzyn K, Llanos A, et al. Partial carotid ligation is a model of acutely induced disturbed flow, leading to rapid endothelial dysfunction and atherosclerosis. Am J Physiol Heart Circ Physiol. 2009;297:H1535–43.
Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. 2012;220:128–33.
Fujihara K, Suzuki H, Sato A, Ishizu T, Kodama S, Heianza Y, et al. Comparison of the Framingham risk score, UK Prospective Diabetes Study (UKPDS) Risk Engine, Japanese Atherosclerosis Longitudinal Study-Existing Cohorts Combine (JALS-ECC) and maximum carotid intima-media thickness for predicting coronary artery stenosis in patients with asymptomatic type 2 diabetes. J Atheroscler Thromb. 2014;21:799–815.
Rockman CB, Hoang H, Guo Y, Maldonado TS, Jacobowitz GR, Talishinskiy T, et al. The prevalence of carotid artery stenosis varies significantly by race. J Vasc Surg. 2013;57:327–37.
Palm F, Dos Santos M, Urbanek C, Greulich M, Zimmer K, Safer A, et al. Stroke seasonality associations with subtype, etiology and laboratory results in the Ludwigshafen Stroke Study (LuSSt). Eur J Epidemiol. 2013;28:373–81.
Rudd JH, Myers KS, Bansilal S, Machac J, Rafique A, Farkouh M, et al. (18)Fluorodeoxyglucose positron emission tomography imaging of atherosclerotic plaque inflammation is highly reproducible: implications for atherosclerosis therapy trials. J Am Coll Cardiol. 2007;50:892–6.
Truijman MT, de Rotte AA, Aaslid R, van Dijk AC, Steinbuch J, Liem MI, et al. Intraplaque hemorrhage, fibrous cap status, and microembolic signals in symptomatic patients with mild to moderate carotid artery stenosis: the Plaque at RISK study. Stroke. 2014;45:3423–6.
Artom N, Montecucco F, Dallegri F, Pende A. Carotid atherosclerotic plaque stenosis: the stabilizing role of statins. Eur J Clin Invest. 2014;44:1122–34.
Maiolino G, Rossitto G, Caielli P, Bisogni V, Rossi GP, Calo LA. The role of oxidized low-density lipoproteins in atherosclerosis: the myths and the facts. Mediators Inflamm. 2013;2013:714653.
Chiu JJ, Chien S. Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiol Rev. 2011;91:327–87.
Sun X, Belkin N, Feinberg MW. Endothelial microRNAs and atherosclerosis. Curr Atheroscler Rep. 2013;15:372.
Loyer X, Vion AC, Tedgui A, Boulanger CM. Microvesicles as cell-cell messengers in cardiovascular diseases. Circ Res. 2014;114:345–53.
Kumar S, Kim CW, Simmons RD, Jo H. Role of flow-sensitive microRNAs in endothelial dysfunction and atherosclerosis: mechanosensitive athero-miRs. Arterioscler Thromb Vasc Biol. 2014;34:2206–16.
Treguer K, Heinrich EM, Ohtani K, Bonauer A, Dimmeler S. Role of the microRNA-17-92 cluster in the endothelial differentiation of stem cells. J Vasc Res. 2012;49:447–60.
Wang S, Aurora AB, Johnson BA, Qi X, McAnally J, Hill JA, et al. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell. 2008;15:261–71.
Boettger T, Beetz N, Kostin S, Schneider J, Kruger M, Hein L, et al. Acquisition of the contractile phenotype by murine arterial smooth muscle cells depends on the Mir143/145 gene cluster. J Clin Invest. 2009;119:2634–47.
Albinsson S, Skoura A, Yu J, DiLorenzo A, Fernandez-Hernando C, Offermanns S, et al. Smooth muscle miRNAs are critical for post-natal regulation of blood pressure and vascular function. PLoS One. 2011;6, e18869.
Vigorito E, Kohlhaas S, Lu D, Leyland R. miR-155: an ancient regulator of the immune system. Immunol Rev. 2013;253:146–57.
Wang KC, Garmire LX, Young A, Nguyen P, Trinh A, Subramaniam S, et al. Role of microRNA-23b in flow-regulation of Rb phosphorylation and endothelial cell growth. Proc Natl Acad Sci U S A. 2010;107:3234–9.
Fang Y, Davies PF. Site-specific microRNA-92a regulation of Kruppel-like factors 4 and 2 in atherosusceptible endothelium. Arterioscler Thromb Vasc Biol. 2012;32:979–87.
Kaluza D, Kroll J, Gesierich S, Manavski Y, Boeckel JN, Doebele C, et al. Histone deacetylase 9 promotes angiogenesis by targeting the antiangiogenic microRNA-17-92 cluster in endothelial cells. Arterioscler Thromb Vasc Biol. 2013;33:533–43.
Doebele C, Bonauer A, Fischer A, Scholz A, Reiss Y, Urbich C, et al. Members of the microRNA-17-92 cluster exhibit a cell-intrinsic antiangiogenic function in endothelial cells. Blood. 2010;115:4944–50.
Petrocca F, Vecchione A, Croce CM. Emerging role of miR-106b-25/miR-17-92 clusters in the control of transforming growth factor beta signaling. Cancer Res. 2008;68:8191–4.
Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, et al. miR-126 regulates angiogenic signaling and vascular integrity. Dev Cell. 2008;15:272–84.
Liu B, Peng XC, Zheng XL, Wang J, Qin YW. MiR-126 restoration down-regulate VEGF and inhibit the growth of lung cancer cell lines in vitro and in vivo. Lung cancer. 2009;66:169–75.
Sessa R, Seano G, di Blasio L, Gagliardi PA, Isella C, Medico E, et al. The miR-126 regulates angiopoietin-1 signaling and vessel maturation by targeting p85beta. Biochim Biophys Acta. 1823;2012:1925–35.
Harris TA, Yamakuchi M, Ferlito M, Mendell JT, Lowenstein CJ. MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc Natl Acad Sci U S A. 2008;105:1516–21.
Zernecke A, Bidzhekov K, Noels H, Shagdarsuren E, Gan L, Denecke B, et al. Delivery of microRNA-126 by apoptotic bodies induces CXCL12-dependent vascular protection. Sci Signal. 2009;2:ra81.
Schober A, Nazari-Jahantigh M, Wei Y, Bidzhekov K, Gremse F, Grommes J, et al. MicroRNA-126-5p promotes endothelial proliferation and limits atherosclerosis by suppressing Dlk1. Nat Med. 2014;20:368–76.
Fichtlscherer S, De Rosa S, Fox H, Schwietz T, Fischer A, Liebetrau C, et al. Circulating microRNAs in patients with coronary artery disease. Circ Res. 2010;107:677–84.
Zampetaki A, Kiechl S, Drozdov I, Willeit P, Mayr U, Prokopi M, et al. Plasma microRNA profiling reveals loss of endothelial miR-126 and other microRNAs in type 2 diabetes. Circ Res. 2010;107:810–7.
Zhou J, Li YS, Nguyen P, Wang KC, Weiss A, Kuo YC, et al. Regulation of vascular smooth muscle cell turnover by endothelial cell-secreted microRNA-126: role of shear stress. Circ Res. 2013;113:40–51.
Owens GK, Kumar MS, Wamhoff BR. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev. 2004;84:767–801.
Elia L, Quintavalle M, Zhang J, Contu R, Cossu L, Latronico MV, et al. The knockout of miR-143 and -145 alters smooth muscle cell maintenance and vascular homeostasis in mice: correlates with human disease. Cell Death Differ. 2009;16:1590–8.
Kohlstedt K, Trouvain C, Boettger T, Shi L, Fisslthaler B, Fleming I. AMP-activated protein kinase regulates endothelial cell angiotensin-converting enzyme expression via p53 and the post-transcriptional regulation of microRNA-143/145. Circ Res. 2013;112:1150–8.
Hergenreider E, Heydt S, Treguer K, Boettger T, Horrevoets AJ, Zeiher AM, et al. Atheroprotective communication between endothelial cells and smooth muscle cells through miRNAs. Nat Cell Biol. 2012;14:249–56.
Nazari-Jahantigh M, Wei Y, Noels H, Akhtar S, Zhou Z, Koenen RR, et al. MicroRNA-155 promotes atherosclerosis by repressing Bcl6 in macrophages. J Clin Invest. 2012;122:4190–202.
Du F, Yu F, Wang Y, Hui Y, Carnevale K, Fu M, et al. MicroRNA-155 deficiency results in decreased macrophage inflammation and attenuated atherogenesis in apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol. 2014;34:759–67.
Sun HX, Zeng DY, Li RT, Pang RP, Yang H, Hu YL, et al. Essential role of microRNA-155 in regulating endothelium-dependent vasorelaxation by targeting endothelial nitric oxide synthase. Hypertension. 2012;60:1407–14.
Tian FJ, An LN, Wang GK, Zhu JQ, Li Q, Zhang YY, et al. Elevated microRNA-155 promotes foam cell formation by targeting HBP1 in atherogenesis. Cardiovasc Res. 2014;103:100–10.
Wagner J, Riwanto M, Besler C, Knau A, Fichtlscherer S, Roxe T, et al. Characterization of levels and cellular transfer of circulating lipoprotein-bound microRNAs. Arterioscler Thromb Vasc Biol. 2013;33:1392–400.
Donners MM, Wolfs IM, Stoger LJ, van der Vorst EP, Pottgens CC, Heymans S, et al. Hematopoietic miR155 deficiency enhances atherosclerosis and decreases plaque stability in hyperlipidemic mice. PLoS One. 2012;7, e35877.
Ma X, Ma C, Zheng X. MicroRNA-155 in the pathogenesis of atherosclerosis: a conflicting role? Heart Lung Circ. 2013;22:811–8.
Cipollone F, Felicioni L, Sarzani R, Ucchino S, Spigonardo F, Mandolini C, et al. A unique microRNA signature associated with plaque instability in humans. Stroke. 2011;42:2556–63.
Raitoharju E, Lyytikainen LP, Levula M, Oksala N, Mennander A, Tarkka M, et al. miR-21, miR-210, miR-34a, and miR-146a/b are up-regulated in human atherosclerotic plaques in the Tampere Vascular Study. Atherosclerosis. 2011;219:211–7.
Santovito D, Mandolini C, Marcantonio P, De Nardis V, Bucci M, Paganelli C, et al. Overexpression of microRNA-145 in atherosclerotic plaques from hypertensive patients. Expert Opin Ther Targets. 2013;17:217–23.
Gan CS, Wang CW, Tan KS. Circulatory microRNA-145 expression is increased in cerebral ischemia. Genet Mol Res. 2012;11:147–52.
Tsai PC, Liao YC, Wang YS, Lin HF, Lin RT, Juo SH. Serum microRNA-21 and microRNA-221 as potential biomarkers for cerebrovascular disease. J Vasc Res. 2013;50:346–54.
Peng H, Zhong M, Zhao W, Wang C, Zhang J, Liu X, et al. Urinary miR-29 correlates with albuminuria and carotid intima-media thickness in type 2 diabetes patients. PLoS One. 2013;8, e82607.
Menghini R, Casagrande V, Cardellini M, Martelli E, Terrinoni A, Amati F, et al. MicroRNA 217 modulates endothelial cell senescence via silent information regulator 1. Circulation. 2009;120:1524–32.
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–57.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010: findings from the global burden of disease study 2010. Lancet. 2014;383:245–54.
Santulli G. Epidemiology of cardiovascular disease in the 21st century: updated numbers and updated facts. J Cardiovasc Dis. 2013;1:1–2.
Menken M, Munsat TL, Toole JF. The global burden of disease study: implications for neurology. Arch Neurol. 2000;57:418–20.
Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–65.
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358:2127–37.
Yuan ZH, Jiang JK, Huang WD, Pan J, Zhu JY, Wang JZ. A meta-analysis of the efficacy and safety of recombinant activated factor VII for patients with acute intracerebral hemorrhage without hemophilia. J Clin Neurosci. 2010;17:685–93.
Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013;382:397–408.
Soreq H, Wolf Y. NeurimmiRs: microRNAs in the neuroimmune interface. Trends Mol Med. 2011;17:548–55.
van Empel VP, De Windt LJ, da Costa Martins PA. Circulating miRNAs: reflecting or affecting cardiovascular disease? Curr Hypertens Rep. 2012;14:498–509.
Saikumar J, Ramachandran K, Vaidya VS. Noninvasive micromarkers. Clin Chem. 2014;60:1158–73.
Heggermont WA, Heymans S. MicroRNAs are involved in end-organ damage during hypertension. Hypertension. 2012;60:1088–93.
Matsumoto S, Sakata Y, Suna S, Nakatani D, Usami M, Hara M, et al. Circulating p53-responsive microRNAs are predictive indicators of heart failure after acute myocardial infarction. Circ Res. 2013;113:322–6.
Kim JM, Jung KH, Chu K, Lee ST, Ban J, Moon J, et al. Atherosclerosis-related circulating microRNAs as a predictor of stroke recurrence. Transl Stroke Res. 2015;6(3):191–7.
Dharap A, Bowen K, Place R, Li LC, Vemuganti R. Transient focal ischemia induces extensive temporal changes in rat cerebral microRNAome. J Cereb Blood Flow Metab. 2009;29:675–87.
Gubern C, Camos S, Ballesteros I, Rodriguez R, Romera VG, Canadas R, et al. miRNA expression is modulated over time after focal ischaemia: up-regulation of miR-347 promotes neuronal apoptosis. FEBS J. 2013;280:6233–46.
Jeyaseelan K, Lim KY, Armugam A. MicroRNA expression in the blood and brain of rats subjected to transient focal ischemia by middle cerebral artery occlusion. Stroke. 2008;39:959–66.
Liu FJ, Lim KY, Kaur P, Sepramaniam S, Armugam A, Wong PT, et al. MicroRNAs involved in regulating spontaneous recovery in embolic stroke model. PloS One. 2013;8:e66393.
Selvamani A, Williams MH, Miranda RC, Sohrabji F. Circulating miRNA profiles provide a biomarker for severity of stroke outcomes associated with age and sex in a rat model. Clin Sci (Lond). 2014;127:77–89.
Weng H, Shen C, Hirokawa G, Ji X, Takahashi R, Shimada K, et al. Plasma miR-124 as a biomarker for cerebral infarction. Biomed Res. 2011;32:135–41.
Jickling GC, Ander BP, Zhan X, Noblett D, Stamova B, Liu D. MicroRNA expression in peripheral blood cells following acute ischemic stroke and their predicted gene targets. PloS One. 2014;9, e99283.
Sepramaniam S, Tan JR, Tan KS, DeSilva DA, Tavintharan S, Woon FP, et al. Circulating microRNAs as biomarkers of acute stroke. Int J Mol Sci. 2014;15:1418–32.
Sorensen SS, Nygaard AB, Nielsen MY, Jensen K, Christensen T. miRNA expression profiles in cerebrospinal fluid and blood of patients with acute ischemic stroke. Transl Stroke Res. 2014;5:711–8.
Tan JR, Tan KS, Koo YX, Yong FL, Wang CW, Armugam A, et al. Blood microRNAs in low or no risk ischemic stroke patients. Int J Mol Sci. 2013;14:2072–84.
Tan KS, Armugam A, Sepramaniam S, Lim KY, Setyowati KD, Wang CW, et al. Expression profile of microRNAs in young stroke patients. PLoS One. 2009;4, e7689.
Wang W, Sun G, Zhang L, Shi L, Zeng Y. Circulating microRNAs as novel potential biomarkers for early diagnosis of acute stroke in humans. J Stroke Cerebrovasc Dis. 2014;23:2607–13.
Li P, Teng F, Gao F, Zhang M, Wu J, Zhang C. Identification of circulating microRNAs as potential biomarkers for detecting acute ischemic stroke. Cell Mol Neurobiol. 2015;35(3):433–47.
Rehfeld F, Rohde AM, Nguyen DT, Wulczyn FG. Lin28 and let-7: ancient milestones on the road from pluripotency to neurogenesis. Cell Tissue Res. 2015;359:145–60.
Selvamani A, Sathyan P, Miranda RC, Sohrabji F. An antagomir to microRNA Let7f promotes neuroprotection in an ischemic stroke model. PLoS One. 2012;7, e32662.
Buller B, Liu X, Wang X, Zhang RL, Zhang L, Hozeska-Solgot A, et al. MicroRNA-21 protects neurons from ischemic death. FEBS J. 2010;277:4299–307.
Zhou J, Zhang J. Identification of miRNA-21 and miRNA-24 in plasma as potential early stage markers of acute cerebral infarction. Mol Med Rep. 2014;10:971–6.
Kole AJ, Swahari V, Hammond SM, Deshmukh M. miR-29b is activated during neuronal maturation and targets BH3-only genes to restrict apoptosis. Genes Dev. 2011;25:125–30.
Pandi G, Nakka VP, Dharap A, Roopra A, Vemuganti R. MicroRNA miR-29c down-regulation leading to de-repression of its target DNA methyltransferase 3a promotes ischemic brain damage. PLoS One. 2013;8, e58039.
Shi G, Liu Y, Liu T, Yan W, Liu X, Wang Y, et al. Upregulated miR-29b promotes neuronal cell death by inhibiting Bcl2L2 after ischemic brain injury. Exp Brain Res. 2012;216:225–30.
Huang LG, Li JP, Pang XM, Chen CY, Xiang HY, Feng LB, et al. MicroRNA-29c correlates with neuroprotection induced by FNS by targeting both Birc2 and Bak1 in rat brain after stroke. CNS Neurosci Ther. 2015;21(6):496–503.
Dhiraj DK, Chrysanthou E, Mallucci GR, Bushell M. miRNAs-19b, -29b-2* and -339-5p show an early and sustained up-regulation in ischemic models of stroke. PloS One. 2013;8:e83717.
Zhu F, Liu JL, Li JP, Xiao F, Zhang ZX, Zhang L. MicroRNA-124 (miR-124) regulates Ku70 expression and is correlated with neuronal death induced by ischemia/reperfusion. J Mol Neurosci. 2014;52:148–55.
Liu XS, Chopp M, Zhang RL, Tao T, Wang XL, Kassis H, et al. MicroRNA profiling in subventricular zone after stroke: MiR-124a regulates proliferation of neural progenitor cells through Notch signaling pathway. PLoS One. 2011;6, e23461.
Doeppner TR, Doehring M, Bretschneider E, Zechariah A, Kaltwasser B, Muller B, et al. MicroRNA-124 protects against focal cerebral ischemia via mechanisms involving Usp14-dependent REST degradation. Acta Neuropathol. 2013;126:251–65.
Sun Y, Gui H, Li Q, Luo ZM, Zheng MJ, Duan JL, et al. MicroRNA-124 protects neurons against apoptosis in cerebral ischemic stroke. CNS Neurosci Ther. 2013;19:813–9.
Liu X, Li F, Zhao S, Luo Y, Kang J, Zhao H, et al. MicroRNA-124-mediated regulation of inhibitory member of apoptosis-stimulating protein of p53 family in experimental stroke. Stroke. 2013;44:1973–80.
Ouyang YB, Lu Y, Yue S, Xu LJ, Xiong XX, White RE, et al. miR-181 regulates GRP78 and influences outcome from cerebral ischemia in vitro and in vivo. Neurobiol Dis. 2012;45:555–63.
Moon JM, Xu L, Giffard RG. Inhibition of microRNA-181 reduces forebrain ischemia-induced neuronal loss. J Cereb Blood Flow Metab. 2013;33:1976–82.
Ouyang YB, Lu Y, Yue S, Giffard RG. miR-181 targets multiple Bcl-2 family members and influences apoptosis and mitochondrial function in astrocytes. Mitochondrion. 2012;12:213–9.
Xu LJ, Ouyang YB, Xiong X, Stary CM, Giffard RG. Post-stroke treatment with miR-181 antagomir reduces injury and improves long-term behavioral recovery in mice after focal cerebral ischemia. Exp Neurol. 2015;264:1–7.
Zeng L, He X, Wang Y, Tang Y, Zheng C, Cai H, et al. MicroRNA-210 overexpression induces angiogenesis and neurogenesis in the normal adult mouse brain. Gene Ther. 2014;21:37–43.
Lou YL, Guo F, Liu F, Gao FL, Zhang PQ, Niu X, et al. miR-210 activates notch signaling pathway in angiogenesis induced by cerebral ischemia. Mol Cell Biochem. 2012;370:45–51.
Harraz MM, Eacker SM, Wang X, Dawson TM, Dawson VL. MicroRNA-223 is neuroprotective by targeting glutamate receptors. Proc Natl Acad Sci U S A. 2012;109:18962–7.
Liu XS, Chopp M, Wang XL, Zhang L, Hozeska-Solgot A, Tang T, et al. MicroRNA-17-92 cluster mediates the proliferation and survival of neural progenitor cells after stroke. J Biol Chem. 2013;288:12478–88.
Vinciguerra A, Formisano L, Cerullo P, Guida N, Cuomo O, Esposito A, et al. MicroRNA-103-1 selectively downregulates brain NCX1 and its inhibition by anti-miRNA ameliorates stroke damage and neurological deficits. Mol Ther. 2014;22:1829–38.
Yang ZB, Zhang Z, Li TB, Lou Z, Li SY, Yang H, et al. Up-regulation of brain-enriched miR-107 promotes excitatory neurotoxicity through down-regulation of glutamate transporter-1 expression following ischaemic stroke. Clin Sci (Lond). 2014;127:679–89.
Chi W, Meng F, Li Y, Li P, Wang G, Cheng H, et al. Impact of microRNA-134 on neural cell survival against ischemic injury in primary cultured neuronal cells and mouse brain with ischemic stroke by targeting HSPA12B. Brain Res. 2014;1592:22–33.
Chi W, Meng F, Li Y, Wang Q, Wang G, Han S, et al. Downregulation of miRNA-134 protects neural cells against ischemic injury in N2A cells and mouse brain with ischemic stroke by targeting HSPA12B. Neuroscience. 2014;277:111–22.
Zhao L, Li H, Guo R, Ma T, Hou R, Ma X, et al. miR-137, a new target for post-stroke depression? Neural Regen Res. 2013;8:2441–8.
Stary CM, Xu L, Sun X, Ouyang YB, White RE, Leong J, et al. MicroRNA-200c contributes to injury from transient focal cerebral ischemia by targeting reelin. Stroke. 2015;46:551–6.
Li LJ, Huang Q, Zhang N, Wang GB, Liu YH. miR-376b-5p regulates angiogenesis in cerebral ischemia. Mol Med Rep. 2014;10:527–35.
Zhao H, Wang J, Gao L, Wang R, Liu X, Gao Z, et al. MiRNA-424 protects against permanent focal cerebral ischemia injury in mice involving suppressing microglia activation. Stroke. 2013;44:1706–13.
Liu P, Zhao H, Wang R, Wang P, Tao Z, Gao L, et al. MicroRNA-424 protects against focal cerebral ischemia and reperfusion injury in mice by suppressing oxidative stress. Stroke. 2015;46:513–9.
Pasquinelli AE, Reinhart BJ, Slack F, Martindale MQ, Kuroda MI, Maller B, et al. Conservation of the sequence and temporal expression of let-7 heterochronic regulatory RNA. Nature. 2000;408:86–9.
Hulsmans M, Holvoet P. MicroRNA-containing microvesicles regulating inflammation in association with atherosclerotic disease. Cardiovasc Res. 2013;100:7–18.
Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–9.
Bienertova-Vasku J, Novak J, Vasku A. MicroRNAs in pulmonary arterial hypertension: pathogenesis, diagnosis and treatment. J Am Soc Hypertens. 2015;9(3):221–34.
Dong S, Cheng Y, Yang J, Li J, Liu X, Wang X, et al. MicroRNA expression signature and the role of microRNA-21 in the early phase of acute myocardial infarction. J Biol Chem. 2009;284:29514–25.
Khanna S, Rink C, Ghoorkhanian R, Gnyawali S, Heigel M, Wijesinghe DS, et al. Loss of miR-29b following acute ischemic stroke contributes to neural cell death and infarct size. J Cereb Blood Flow Metab. 2013;33:1197–206.
Kriegel AJ, Liu Y, Fang Y, Ding X, Liang M. The miR-29 family: genomics, cell biology, and relevance to renal and cardiovascular injury. Physiol Genomics. 2012;44:237–44.
Meza-Sosa KF, Pedraza-Alva G, Perez-Martinez L. MicroRNAs: key triggers of neuronal cell fate. Front Cell Neurosci. 2014;8:175.
Laterza OF, Lim L, Garrett-Engele PW, Vlasakova K, Muniappa N, Tanaka WK, et al. Plasma microRNAs as sensitive and specific biomarkers of tissue injury. Clin Chem. 2009;55:1977–83.
Luo X, Hou L, Shi H, Zhong X, Zhang Y, Zheng D, et al. CSF levels of the neuronal injury biomarker visinin-like protein-1 in Alzheimer’s disease and dementia with Lewy bodies. J Neurochem. 2013;127:681–90.
Fang M, Wang J, Zhang X, Geng Y, Hu Z, Rudd JA, et al. The miR-124 regulates the expression of BACE1/beta-secretase correlated with cell death in Alzheimer’s disease. Toxicol Lett. 2012;209:94–105.
Su W, Hopkins S, Nesser NK, Sopher B, Silvestroni A, Ammanuel S, et al. The p53 transcription factor modulates microglia behavior through microRNA-dependent regulation of c-Maf. J Immunol. 2014;192:358–66.
Miska EA, Alvarez-Saavedra E, Townsend M, Yoshii A, Sestan N, Rakic P, et al. Microarray analysis of microRNA expression in the developing mammalian brain. Genome Biol. 2004;5:R68.
Su R, Lin HS, Zhang XH, Yin XL, Ning HM, Liu B, et al. MiR-181 family: regulators of myeloid differentiation and acute myeloid leukemia as well as potential therapeutic targets. Oncogene. 2015;34(25):3226–39.
Ouyang YB, Giffard RG. MicroRNAs affect BCL-2 family proteins in the setting of cerebral ischemia. Neurochem Int. 2014;77:2–8.
Ouyang YB, Giffard RG. MicroRNAs regulate the chaperone network in cerebral ischemia. Transl Stroke Res. 2013;4:693–703.
Ouyang YB, Stary CM, White RE, Giffard RG. The use of microRNAs to modulate redox and immune response to stroke. Antioxid Redox Signal. 2015;22:187–202.
Ouyang YB, Xu L, Liu S, Giffard RG. Role of astrocytes in delayed neuronal death: GLT-1 and its novel regulation by microRNAs. Adv Neurobiol. 2014;11:171–88.
Chan YC, Banerjee J, Choi SY, Sen CK. miR-210: the master hypoxamir. Microcirculation. 2012;19:215–23.
Fasanaro P, D’Alessandra Y, Di Stefano V, Melchionna R, Romani S, Pompilio G, et al. MicroRNA-210 modulates endothelial cell response to hypoxia and inhibits the receptor tyrosine kinase ligand Ephrin-A3. J Biol Chem. 2008;283:15878–83.
Sepramaniam S, Ying LK, Armugam A, Wintour EM, Jeyaseelan K. MicroRNA-130a represses transcriptional activity of aquaporin 4 M1 promoter. J Biol Chem. 2012;287:12006–15.
Sepramaniam S, Armugam A, Lim KY, Karolina DS, Swaminathan P, Tan JR, et al. MicroRNA 320a functions as a novel endogenous modulator of aquaporins 1 and 4 as well as a potential therapeutic target in cerebral ischemia. J Biol Chem. 2010;285:29223–30.
Pan Y, Liang H, Liu H, Li D, Chen X, Li L, et al. Platelet-secreted microRNA-223 promotes endothelial cell apoptosis induced by advanced glycation end products via targeting the insulin-like growth factor 1 receptor. J Immunol. 2014;192:437–46.
Tabet F, Vickers KC, Cuesta Torres LF, Wiese CB, Shoucri BM, Lambert G, et al. HDL-transferred microRNA-223 regulates ICAM-1 expression in endothelial cells. Nat Commun. 2014;5:3292.
Vickers KC, Landstreet SR, Levin MG, Shoucri BM, Toth CL, Taylor RC, et al. MicroRNA-223 coordinates cholesterol homeostasis. Proc Natl Acad Sci U S A. 2014;111:14518–23.
Duan X, Zhan Q, Song B, Zeng S, Zhou J, Long Y, et al. Detection of platelet microRNA expression in patients with diabetes mellitus with or without ischemic stroke. J Diabetes Complications. 2014;28:705–10.
Mogilyansky E, Rigoutsos I. The miR-17/92 cluster: a comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ. 2013;20:1603–14.
Leung LY, Chan CP, Leung YK, Jiang HL, Abrigo JM, de Wang F, et al. Comparison of miR-124-3p and miR-16 for early diagnosis of hemorrhagic and ischemic stroke. Clin Chim Acta. 2014;433:139–44.
Liu Y, Zhang J, Han R, Liu H, Sun D, Liu X. Downregulation of serum brain specific microRNA is associated with inflammation and infarct volume in acute ischemic stroke. J Clin Neurosci. 2015;22:291–5.
Long G, Wang F, Li H, Yin Z, Sandip C, Lou Y, et al. Circulating miR-30a, miR-126 and let-7b as biomarker for ischemic stroke in humans. BMC Neurol. 2013;13:178.
Zeng L, Liu J, Wang Y, Wang L, Weng S, Tang Y, et al. MicroRNA-210 as a novel blood biomarker in acute cerebral ischemia. Front Biosci (Elite Ed). 2011;3:1265–72.
Zeng L, Liu J, Wang Y, Wang L, Weng S, Chen S, et al. Cocktail blood biomarkers: prediction of clinical outcomes in patients with acute ischemic stroke. Eur Neurol. 2013;69:68–75.
Wang Y, Zhang Y, Huang J, Chen X, Gu X, Zeng L, et al. Increase of circulating miR-223 and insulin-like growth factor-1 is associated with the pathogenesis of acute ischemic stroke in patients. BMC Neurol. 2014;14:77.
Brown Jr RD, Broderick JP. Unruptured intracranial aneurysms: epidemiology, natural history, management options, and familial screening. Lancet Neurol. 2014;13(4):393–404.
Brown Jr RD, Wiebers DO, Forbes GS. Unruptured intracranial aneurysms and arteriovenous malformations: frequency of intracranial hemorrhage and relationship of lesions. J Neurosurg. 1990;73:859–63.
Shiue I, Arima H, Hankey GJ, Anderson CS. Modifiable lifestyle behaviours account for most cases of subarachnoid haemorrhage: a population-based case-control study in Australasia. J Neurol Sci. 2012;313:92–4.
Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, et al. Incidental findings on brain MRI in the general population. N Engl J Med. 2007;357:1821–8.
Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International subarachnoid Aneurysm Trial (ISAT). Lancet. 2015;385(9969):691–7.
Lee HJ, Yi JS, Lee IW, Park KC, Yang JH. Dysregulated expression profiles of microRNAs of experimentally induced cerebral aneurysms in rats. J Korean Neurosurg Soc. 2013;53:72–6.
Jiang Y, Zhang M, He H, Chen J, Zeng H, Li J, et al. MicroRNA/mRNA profiling and regulatory network of intracranial aneurysm. BMC Med Genomics. 2013;6:36.
Liu D, Han L, Wu X, Yang X, Zhang Q, Jiang F. Genome-wide microRNA changes in human intracranial aneurysms. BMC Neurol. 2014;14:188.
Jin H, Li C, Ge H, Jiang Y, Li Y. Circulating microRNA: a novel potential biomarker for early diagnosis of intracranial aneurysm rupture a case control study. J Transl Med. 2013;11:296.
Li P, Zhang Q, Wu X, Yang X, Zhang Y, Li Y, et al. Circulating microRNAs serve as novel biological markers for intracranial aneurysms. J Am Heart Assoc. 2014;3, e000972.
Maegdefessel L, Azuma J, Toh R, Deng A, Merk DR, Raiesdana A, et al. MicroRNA-21 blocks abdominal aortic aneurysm development and nicotine-augmented expansion. Sci Transl Med. 2012;4:122ra22.
Leeper NJ, Raiesdana A, Kojima Y, Chun HJ, Azuma J, Maegdefessel L, et al. MicroRNA-26a is a novel regulator of vascular smooth muscle cell function. J Cell Physiol. 2011;226:1035–43.
Boon RA, Seeger T, Heydt S, Fischer A, Hergenreider E, Horrevoets AJ, et al. MicroRNA-29 in aortic dilation: implications for aneurysm formation. Circ Res. 2011;109:1115–9.
Maegdefessel L, Azuma J, Toh R, Merk DR, Deng A, Chin JT, et al. Inhibition of microRNA-29b reduces murine abdominal aortic aneurysm development. J Clin Invest. 2012;122:497–506.
Merk DR, Chin JT, Dake BA, Maegdefessel L, Miller MO, Kimura N, et al. miR-29b participates in early aneurysm development in Marfan syndrome. Circ Res. 2012;110:312–24.
Tan J, Tong BD, Wu YJ, Xiong W. MicroRNA-29 mediates TGFbeta1-induced extracellular matrix synthesis by targeting wnt/beta-catenin pathway in human orbital fibroblasts. Int J Clin Exp Pathol. 2014;7:7571–7.
Abecassis IJ, Xu DS, Batjer HH, Bendok BR. Natural history of brain arteriovenous malformations: a systematic review. Neurosurg Focus. 2014;37:E7.
Hofmeister C, Stapf C, Hartmann A, Sciacca RR, Mansmann U, terBrugge K, et al. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke. 2000;31:1307–10.
Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 2014;383:614–21.
Stapf C, Mohr JP, Pile-Spellman J, Solomon RA, Sacco RL, Connolly Jr ES. Epidemiology and natural history of arteriovenous malformations. Neurosurg Focus. 2001;11(5):e1.
Gross BA, Du R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg. 2013;118:437–43.
Stefani MA, Porter PJ, terBrugge KG, Montanera W, Willinsky RA, Wallace MC. Large and deep brain arteriovenous malformations are associated with risk of future hemorrhage. Stroke. 2002;33:1220–4.
Stefani MA, Porter PJ, terBrugge KG, Montanera W, Willinsky RA, Wallace MC. Angioarchitectural factors present in brain arteriovenous malformations associated with hemorrhagic presentation. Stroke. 2002;33:920–4.
Ferreira R, Santos T, Amar A, Gong A, Chen TC, Tahara SM, et al. Argonaute-2 promotes miR-18a entry in human brain endothelial cells. J Am Heart Assoc. 2014;3, e000968.
Ferreira R, Santos T, Amar A, Tahara SM, Chen TC, Giannotta SL, et al. MicroRNA-18a improves human cerebral arteriovenous malformation endothelial cell function. Stroke. 2014;45:293–7.
Acknowledgements
J. Novak received a research support from MUNI/A/1326/2014 institutional grant of Masaryk University in Brno, Czech Republic. O. Volny received a research support from European Regional Development Fund—Project FNUSA-ICRC (No.CZ.1.05/1.1.00/02.0123). O. Volny received a student scholarship of city Ostrava in 2014/2015.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Volný, O., Kašičková, L., Coufalová, D., Cimflová, P., Novák, J. (2015). microRNAs in Cerebrovascular Disease. In: Santulli, G. (eds) microRNA: Medical Evidence. Advances in Experimental Medicine and Biology, vol 888. Springer, Cham. https://doi.org/10.1007/978-3-319-22671-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-22671-2_9
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22670-5
Online ISBN: 978-3-319-22671-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)