Abstract
MicroRNAs are small, non-coding RNA molecules that regulate gene expression, and miR-124 is the most abundant miRNA in the brain. Studies have shown that miR-124 is clearly reduced in the ischemic brain after stroke; however, the role of miR-124 after stroke is less well studied. Using TargetScan, MicroCosm Targets version 5, and microRNA.org databases, we identified miR-124 as a possible regulator of the DNA repair protein Ku70. We validated that Ku70 is a target for miR-124 with a luciferase reporter activity assay. Moreover, adult rats subjected to focal cerebral ischemia exhibited a substantial reduction of miR-124 expression, which was inversely upregulated by Ku70 expression. In vivo treatment with miR-124 antagomir effectively enhanced Ku70 mRNA and protein levels in the ischemic region. Furthermore, knockdown of cerebral miR-124 reduced cell death and infarct size and improved neurological outcomes. Our data demonstrate that miR-124 is an endogenous regulator of Ku70 that improves ischemia/reperfusion (I/R)-induced brain injury and dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral ischemia is characterized by insufficient blood flow to the brain that fails to meet the organ’s high metabolic demand (Winters et al. 2012). Minutes after the onset of ischemia, single-strand breaks occur in DNA, and more severe ischemia, even after reperfusion, can cause double-strand DNA breaks (DSBs) (Chen et al. 1997). The major repair mammalian cell repair mechanism for DSBs is nonhomologous end join (NHEJ) (Yano et al. 2009). Ku70 is a 70-kDa protein that has been shown to be involved in multiple cellular pathways, mainly involving NHEJ of DSBs, V(D)J recombination, telomere maintenance, and the regulation of Bax-mediated apoptosis. For all these functions except the last one, Ku70 acts as part of a heterodimer with an approximately 80-kDa protein, Ku80 (Amsel et al. 2008). In mice, Ku70 expression was dramatically reduced 4 h after focal cerebral ischemia and preceded DNA fragmentation (Kim et al. 2001), but upregulation of Ku 70 was observed 1 to 3 days after ischemic preconditioning (Shackelford et al. 1999). Moreover, a Bax-inhibiting peptide designed from the Bax-binding domain of Ku70 has been shown to suppress Bax-mediated apoptosis and improve behavioral deficits following global cerebral ischemia (Rathaus et al. 2009; Sawada et al. 2003). These results suggest that Ku70 may play a role in the regulation of ischemia/reperfusion (I/R)-induced apoptosis.
MicroRNAs (miRNAs) are a newly discovered class of small (∼22 nucleotide), non-coding RNA molecules that negatively regulate protein expression in viruses, plants, and animals (Bartel 2004; Kim 2005). In animals, miRNAs regulate mRNA translation via imperfect pairing with nucleotide sequences within the 3'-untranslated region of targets, and repressed translation is enhanced for those mRNAs targeted by multiple miRNAs (Doench and Sharp 2004). It is now evident that miRNAs are able to regulate the expression of at least one third of the human genome and play a critical role in a variety of normal biological processes, including cell differentiation, apoptosis, development, and metabolism (Bartel 2004; Ketting et al. 2001; Lee et al. 2004).
Using TargetScan (http://www.targetscan.org/) (Betel et al. 2010), MicroCosm Targets version 5 (http://www.ebi.ac.uk/enright-srv/microcosm/cgi-bin/targets/v5/search.pl), and microRNA.org (http://www.microrna.org/microrna/getGeneForm.do) databases (Betel et al. 2008; Friedman et al. 2009), we found that all three miR target prediction software programs identified Ku70 as a potential target of miR-124.
MiR-124 (also called miR-124a) is the most abundant miRNAs in the brain. It is considered neuron specific because it is not expressed by astrocytes. Moreover, miR-124 is downregulated in ischemic brain (Liu et al. 2011). However, the role of miR-124 after stroke is less well studied. Here, we demonstrate that miR-124 is an endogenous regulator of Ku70 in a rat middle cerebral artery occlusion (MCAO) model. We further showed that knockdown of miR-124 attenuates I/R-induced brain injury by negatively regulating Ku70.
Materials and Methods
Plasmid Construction
A 173-bp segment from the 3′UTR of the Ku70 gene containing the miR-124 binding site was amplified by polymerase chain reaction (PCR) from rat genomic DNA and then cloned into the XhoI/NotI site of pmiR-RB-REPORT™ vector (RiboBio, Guangzhou, China). The following primer sets were used to generate specific fragments: forward, 5′-CCGCTCGAGCTAATGATCACACGCCCAGCCACCTTC-3′ and reverse, 5′-GAATGCGGCCGCAATAGTACACAATATAAAGTTAGAGCTCTTTATTC-3′. For mutant construct of Ku70 3′UTR, site-directed mutagenesis was performed with a QuickChange® XL site-directed mutagenesis kit (Stratagene, California, USA). Mutation was performed by replacement of the predicted miR-124 binding site 5′-GUGCCUUA-3′ with 5′-AGACCUUA-3′. Both wild type and mutant inserts were confirmed by sequencing.
Luciferase Assays
HEK293T cells were plated at a density of 4 × 103 cells/well in 96-well plates 1 day before transfection. Cells were co-transfected with 100 ng/ml pmiR-RB-REPORT™ Luciferase vector including the 3′UTR of Ku70 (with either wild-type or mutant-type miR-124 binding sites) and miR mimics or control (RiboBio, Guangzhou, China) at a final concentration of 50 nM using Lipofectamine 2000 (Invitrogen, California, USA) as described by the manufacturer. Luciferase assays were performed with a dual luciferase reporter assay system (Promega, Wisconsin, USA) 48 h after transfection. Renilla luciferase activity was normalized to that of firefly luciferase.
Rat Model of Transient Focal Ischemia
The animals were handled according to the guidelines of the Council for International Organization of Medical Sciences on Animal Experimentation (World Health Organization, Geneva, Switzerland). The animal protocols were approved by the Guangxi Medical University Animal Care and Use Committee. Male Sprague Dawley rats (280–300 g, purchased from Animal Experiment Central of Guangxi Medical University) were intraperitoneally anesthetized with 3.5 % chloral hydrate (1.0 ml/100 g, Sigma, Missouri, USA), and focal cerebral ischemia was produced by 2 h of MCAO using a nylon monofilament suture as described previously (Longa et al. 1989). Rats in the control group only underwent vascular separation without filament insertion. After 24 h of reperfusion, rats were sacrificed, and the ipsilateral brain tissue was dissected for real-time quantitative PCR (RT-qPCR).
RT-qPCR for miR-124 Quantitation
Total RNA was isolated from brain tissue sections (approximately 2-mm thick) dissected from two points in front of and behind the optic chiasm with TRIzol® reagent (Invitrogen, California, USA). Reverse transcription was performed using the One-step PrimeScript® miRNA cDNA synthesis kit (Perfect Real Time; Takara, Dalian, China). Equal amounts of total RNA (1 μg) were reverse-transcribed with 10 μl 2 × miRNA reaction buffer mix (for Real Time), 2 μl 0.1 % bovine serum albumin, 2 μl miRNA PrimeScript® RT enzyme mix, and RNase Free dH2O up to 20 μl at 37 °C for 60 min and at 85 °C for 5 s. PCR reactions were then conducted using the SYBR® Premix Ex TaqTM II (Perfect Real Time, Takara) at 95 °C for 10 s, followed by 40 cycles of 95 °C for 5 s, and 60 °C for 20 s. Each reaction contained 1 μl RT reaction product, 12.5 μl SYBR® Premix Ex TaqTM II (2×), 1 μl miR-124 or U6b (Takara, Dalian, China) qPCR primer mix, and RNase Free dH2O up to 25 μl using Applied Biosystems 7500HT (California, USA). The expression of miR-124 was normalized using U6b as the internal control. Data analyses were performed using the 2−ΔΔCt method.
RT-qPCR for mRNA Quantitation
For Ku70 mRNA detection, 1 μg total RNA was reverse transcribed using the SYBR® Premix Ex TaqTM II (Tli RNase H Plus, Takara) according to the manufacturer’s protocol. Equal amounts of total RNA (1 μg) were mixed with 5× gDNA Eraser buffer 2.0 μl, gDNA Eraser 1.0 μl, and RNase Free dH2O up to 10 μl. The mixtures were incubated at room temperature for 5 min before adding 5 × PrimeScript® buffer 2 (for Real Time) 4.0 μl, PrimeScript® RT enzyme mix I 1.0 μl, RT primer mix 1.0 μl, and RNase Free dH2O up to 20 μl at 37 °C for 15 min and at 85 °C for 5 s. PCR reactions were then conducted using the SYBR® Premix Ex TaqTM II (Tli RNase H Plus, Takara) at 95 °C for 30 s, followed by 40 cycles of 95 °C for 5 s, and 60 °C for 30 s in the Applied Biosystems 7500HT. Ku70 expression was normalized using glyceraldehyde 3-phosphate dehydrogenase (GAPDH) as the internal control. Primer sequences (Takara) were as follows: Ku70: forward 5′-AGCATCGCTGAGGATGAGG-3′, reverse 5′-CACCATGAGTGCTACGTCTTTG-3′, and GAPDH: forward 5′-TATGACTCTACCCACGGCAAGT-3′, reverse 5′-ATACTCAGCACCAGCATCACC-3′.
Intracerebroventricular Infusion of miR-124 Antagomir
MiR-124 antagomir or Ncontrol (RiboBio, Guangzhou, China) was dissolved in artificial CSF (aCSF: 119 mmol/l NaCl, 3.1 mmol/l KCl, 1.2 mmol/l CaCl2, 1 mmol/l MgSO4, 0.50 mmol/l KH2PO4, 25 mmol/l NaHCO3, 5 mmol/l D-glucose, 2.2 mmol/l urea, pH 7.4) at a concentration of 20 nmol/ml (Yin et al. 2010). The following are the structure and sequence of miR-124 antagomir and control (the antagomirs are antisense oligonucleotides for individual miRNA, whose terminal nucleotides at both ends were modified by an O-methyl moiety at the 2'-ribose position and the 5′ end was modified with cholesteryl functionality): miR-124 antagomir: 5′-mUmAmAmGmGmCmAmCmGmCmGmGmUmGmAmAmUmGmCmC-/3chol/-3′; Ncontrol: 5′-mUmUmUmGmUmAmCmUmAmCmAmCmAmAmAmAmGmUmAmCmUmG-/3chol/-3′.
Rats were anesthetized as described above and fixed in a stereotaxic apparatus. The microsyringe (Gaoge, Shanghai, China) was stereotaxically implanted into the right lateral ventricle of the brain (bregma: 0.8 mm posterior, 4.8 mm dorsoventral, 1.5 mm lateral; on the basis of the rat brain atlas of and was affixed to the skull. The miR-124 antagomir or Ncontrol (0.2 nmol/μl, total 5 μl, at a rate of 1 μl/10 min) was continuously infused into the right lateral ventricle of the brain. One day after intracerebroventricular (ICV) infusion, rats were anesthetized and underwent MCAO and reperfusion as For RT-qPCR, Western blotting, and the apoptosis assay; five rats from each group were used for each method. The remaining ten rats from each group were sacrificed for 2,3,5-triphenyltetrazolium chloride (TTC) staining.
Western Blotting Analysis
Total protein was isolated from brain tissue using RIPA lysis buffer (Beyotime, Haimen, China). Equal amounts (20 μg) of protein were loaded and separated by 10 % SDS-polyacrylamide gel electrophoresis, then electrotransferred to polyvinylidene fluoride membranes (Millipore Corp, Massachusetts, USA). The membranes were blocked with a buffer containing 5 % non-fat milk in phosphate-buffered saline with Tween for 1 h and incubated overnight on ice with antibody against Ku70 (1:200, ab2172; Abcam, Cambridge, UK) and GAPDH (1:1,000, AG019, Beyotime, Haimen, China), then washed and incubated with 1:10,000 anti-mouse antibody (042-06-18-06; KPL, Washington, USA). Immunoreactive bands were visualized using the LICOR Odyssey infrared imaging system (LICOR Bioscience, Nebraska, USA), according to the manufacturer’s instructions. Densitometric analysis of bands was performed using LICOR Odyssey software V3.0. Ku70 density values were normalized to those of GAPDH.
Measurement of Infarct Volume and Neurological Deficit
Infarct volume was measured using 2 % TTC (2,3,5-triphenyltetrazolium chloride) (Sangon Biotech, Shanghai, China) staining. Rat brains were removed after 2 h MCAO and 24-h reperfusion and sliced into six 2-mm thick coronal sections on a rat brain matrix. The slices were stained with 2 % TTC for 15 min at 37 °C. The percent of infarct volume was calculated using a derived formula in which infarct volume as a percentage of the contralateral hemisphere was determined as follows: 100 % × (contralateral hemisphere volume − non-infarct ipsilateral hemisphere volume)/contralateral hemisphere volume(Swanson et al. 1990). Following cerebral ischemia, rats were also tested for neurological deficits and scored on a 5-point scale as follows: 0, no observable neurological deficits (normal); 1, failure to extend right forepaw (mild); 2, circling to the contralateral side (moderate); 3, falling to the right (severe); and 4, mice could not walk spontaneously, depressed level of consciousness (very severe) (Vemuganti et al. 2004).
TUNEL Assays
Coronal brain sections (approximately 2-mm thick) were taken immediately from in front of and behind the optic chiasm after intracardial paraformaldehyde perfusion. The brain specimens were individually immersed in 4 % paraformaldehyde fixative for 24 h, dehydrated in alcohol, and embedded in paraffin. They were then cut into slices of 4-μm for TUNEL analysis as described in the commercial kit manual (Roche Applied Science, Mannheim, Germany). Positively labeled nuclei (brown color) were identified from unstained nuclei (blue color). The number of positive nuclei was determined by manually counting (×400 magnification) all the positively labeled nuclei present in five randomly selected fields under a microscope. The percentage of TUNEL-positive nuclei was used as an apoptotic index. The apoptotic cells had the following characteristics: single cells, no inflammation, cell membrane curling, brown particulate, or fragmented nuclei.
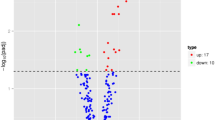
Statistical Analysis
All data reported represent at least three independent experiments, and the numbers of animals are indicated in the figure legends. Data reported are means ± standard deviation. Statistical significance was determined using t tests to compare two groups or analysis of variance, followed by Newman–Keuls posttest for experiments with more than two groups. Values of P < 0.05 were considered significant. “*” indicates P < 0.05, and “**” means P < 0.01.
Results
Ku70 is a Target of miR-124
Ku70 has been widely studied as an important protein in NHEJ, but its regulation of miRNAs is still unknown. To assess the miRNAs that could target Ku70, a bioinformatic search was performed in TargetScan (http://www.targetscan.org/), MicroCosm Targets Version 5 (http://www.ebi.ac.uk/Enright-srv/microcosm/cgi-bin/targets/v5/search.pl), and microrna.org (http://www.microrna.org/microrna/getGeneForm.do) databases. Only miRNAs conserved in mammals were selected for this study. The search yielded 17 miRNAs against Ku70 (Table 1). Interestingly, only miR-124 was identified by three microRNA target prediction software programs, and miR-124 was highly complementary with the Ku70 3′UTR (Fig. 1a). To validate a direct interaction between miR-124 and Ku70 mRNA, its 3′UTR target sites was cloned into a dual luciferase reporter vector (Fig. 1b). We then co-transfected HEK 293T cells with luciferase reporter vector containing the 3′UTR (wild type or mutated type) of Ku70 and miR-124 mimics or Ncontrol. Co-transfection of miR-124 mimics in HEK 293T cells strongly inhibited luciferase activity produced by the reporter construct containing the wild 3′UTR segment of Ku70, whereas no effect was observed with a construct containing a mutated segment of Ku70 3′UTR (miR-124 binding sequence 5′-GUGCCUUA-3′ was mutated to 5′-AGACCUUA-3′). This effect was determined to be specific because no change was seen in luciferase reporter activity when Ncontrol was co-transfected with either reporter construct (Fig. 1c). Collectively, these data indicate that Ku70 is a potential target of miR-124.
Ku70 is a target of miR-124 a predicted binding sites of miR-124 in the 3′UTR of Ku70. The binding sites for rat are indicated. The underlined nucleotides were subsequently mutated (see Fig. 1b legend) for the 3′UTR-miRNA binding studies. b Design of an miR-124 luciferase reporter vector with HSV-driven expression of a luciferase vector fused to a wild Ku70 3′UTR or mutated Ku70 3′UTR. c The 3′UTR of Ku70 mediates miR-124 control of Ku70 expression. HEK 293T cells were transfected with pmiR-RB-REPORT™ Luciferase vector, including the 3′UTR of Ku70 (with either wild-type or mutant-type miR-124 binding sites). The cells were also co-transfected with miR-124 mimics or Ncontrol. Compared to Ncontrol, miR-124 mimics decreased expression of luciferase containing a wild-type miR-124 binding site (right two columns) but not a mutant binding site (left two columns). Data are expressed as mean ± SEM. **P < 0.01 versus mimic control. Results shown are representative of three separate experiments
miR-124 and Ku70 mRNA Levels After Cerebral Ischemia
To explore possible changes in miR-124 and Ku70 mRNA expression in response to cerebral ischemia, transient MCAO was performed. Brain tissue was dissected after 24 h of reperfusion following 2 h MCAO. Although miR-124 levels decreased (Fig. 2a), those of Ku70 mRNA increased (Fig. 2b). To further confirm that miR-124 acts as a negative regulator of Ku70 translation under ischemic conditions, we downregulated miR-124 expression by ICV infusion of miR-124 antagomir (Fig. 2c) and then examined both Ku70 mRNA (Fig. 2d) and protein (Fig. 2e, f) expression. We observed that Ku70 mRNA and Ku70 protein expression levels were significantly increased in rat brain tissue following MCAO and reperfusion. This is consistent with the idea that an ischemia-induced reduction in miR-124 negatively regulates Ku70 expression.
Reciprocal expression of miR-124 and Ku70 after transient focal cerebral ischemia in rat. a, b miR-124 is downregulated and Ku70 mRNA is upregulated after 24 h of reperfusion following 2 h of MCAO. c–f Microsyringe-assisted ICV infusion of a miR-124 antagomir effectively inhibited cerebral miR-124 expression and significantly enhanced Ku70 mRNA and protein levels in rat brain tissue after 2 h of MCAO and 24 h of reperfusion
Downregulation of miR-124 Attenuates Ischemic Brain Damage
To evaluate the biological role of miR-124 in ischemic brain injury in vivo, we altered brain levels by ICV infusion of mir-124 antagomir or Ncontrol. Inhibition of miR-124 alleviated cerebral ischemic damage and decreased infarct volume 24 h after reperfusion subsequent MCAO. We observed that the infarct volume was greatly reduced in miR-124 antagomir-injected rat brains (Fig. 3a, b). Additionally, knockdown of miR-124 effectively reduced abnormal neurological scores relative to Ncontrol group (Fig. 3c). Given the markedly improved recovery of brain function in miR-124 antagomir-injected rats, we next determined the effects of miR-124 on postischemic cellular damage. As shown in (Fig. 3d, e), we observed that the number of TUNEL-positive nuclei was significantly reduced in miR-124 antagomir-injected rat brains relative to Ncontrols. Taken together, these results demonstrate that inhibition of miR-124 protects against I/R-induced cellular damage in vivo.
The effect of miR-124 inhibition after transient focal cerebral ischemia in rat. Rats were pretreated with miR-124 antagomir or Ncontrol for 24 h via microsyringe-assisted ICV infusion and then subjected to 2 h of MCAO and 24 h of reperfusion. a Representative TTC-stained coronal sections demonstrate decreased infarct size in a representative miR-124 antagomir-transfected brain compared with the brain of Ncontrol-infused rat. b The bar graph shows quantitation of % infarct volume by TTC staining in each group. c Knockdown of miR-124 effectively reduced neurological scores relative to the Ncontrol group. d, e The number of TUNEL-positive nuclei was significantly reduced in miR-124 antagomir-infused rat brains after 2 h of MCAO and 24 h of reperfusion (a, b negative control; c, d Ncontrol; e, f miR-124 antagomir; a, c, e ×100 magnification; b, d, f ×400 magnification). Negative control; fixed and permeabilized cells were incubated in 50 μl/well Label solution (without terminal transferase) instead of TUNEL reaction mixture
Discussion
In this study, we established that miR-124 can directly modulate Ku70 gene expression both in vitro and in vivo. Knockdown of endogenous miR-124 protects against I/R-induced brain cell death by upregulating Ku70. For the first time, we demonstrated that Ku70 is a physiological target of miR-124 and that it reduces Ku70 expression at the post-transcriptional level.
In recent years, tremendous efforts have been made to employ an miR microarray screening approach to perform miR expression profiling in infarcted brains from both animal models and human patients (Dharap et al. 2009; Jeyaseelan et al. 2008; Lee et al. 2010; Liu et al. 2011). These reports show that expression levels of specific miRNAs can either increase or decrease after MCAO. However, the role of a specific miR in ischemic cerebral disease is only now emerging. Jeyaseelan et al. reported that miR-124 was upregulated in 24-h-reperfused MCAO rat brains (Jeyaseelan et al. 2007), but Liu et al. showed that miR-124 was decreased in cultured subventricular zone cells in rats 7 days after MCAO (Liu et al. 2011). Therefore, whether miR-124 has a role in stroke pathogenesis and sequelae requires additional investigation. In the present study, we focus on the effects of miR-124 on cell death in the ischemic brain in vivo. We found that continuous delivery of miR-124 antagomir to rat lateral cerebral ventricles effectively reduced I/R-induced apoptosis. Furthermore, knockdown of endogenous miR-124 expression reduced brain infarct size and improved neurological outcomes after focal ischemia. Our data identify miR-124 as a novel antiapoptotic regulator that contributes to the pathogenesis of focal cerebral ischemia.
miRNAs are a class of sophisticated gene expression regulators that inhibit translation and/or degrade target mRNAs by recognizing them through base pairing with short regions near 3′UTRs. In many cases, target recognition by an miRNA only requires a continuous 6-base pair “seed match” between the 5′ end of the miRNA and its target. Therefore, one miRNA can theoretically coordinate the regulation of hundreds of genes. Comparative genomic analyses have predicted that one third of human genes could be miRNA targets (Bartel 2004; Kim 2005). MiR-124 is the most abundant miRNA in the adult brain, and its sequence is completely conserved from worm to human (Aboobaker et al. 2005; Clark et al. 2010; Weng et al. 2011). Conserved seed match sequences to miR-124 are abundant in mammalian genomes; one miRNA target prediction algorithm identified >1,000 potential targets for miR-124 (Lagos-Quintana et al. 2002; Landgraf et al. 2007; Lewis et al. 2005). Using TargetScan, MicroCosm Targets Version 5, and microRNA.org databases (Betel et al. 2008; Betel et al. 2010; Friedman et al. 2009), we identified Ku70 as an important candidate target for miR-124. However, whether the downregulated transcripts represent the physiological targets of miR-124 and whether the findings reflect its in vivo function remain to be tested.
To further validate the computational finding that miR-124 may negatively regulate Ku70, we generated a luciferase construct harboring the 3′UTR fragment of the Ku70-containing binding site of miR-124 and a mutant luciferase construct with an altered binding site. The results showed that miR-124 significantly repressed luciferase activity in the HEK293 T cell line transiently transfected with wide-type Ku70 3′UTR compared to cells transfected with mutated Ku70 3′UTR, suggesting that Ku70 is a genuine target of miR-124.
Our in vivo data showed that adult rats subjected to focal cerebral ischemia followed by reperfusion exhibited a substantial reduction of miR-124 expression, which was inversely upregulated by Ku70 expression. Furthermore, continuous delivery of miR-124 antagomir to rat lateral cerebral ventricles effectively increased Ku70 mRNA and protein expression. These results suggest that miR-124 can directly modulate Ku70 gene expression both in vitro and in vivo.
Ku70 is a DNA repair protein. In addition to its roles in regulating DNA-repair, V(D)J recombination, and telomere maintenance, Ku70 was recently shown to regulate Bax-mediated apoptosis (Amsel et al. 2008). Ku70 overexpressing HEK cells exhibit lower levels of cell death after exposure to apoptotic stimuli, such as staurosporine or ultraviolet radiation. Moreover, overexpression of Ku70 also blocks apoptotic cell death induced by transfection with Bax (Cohen et al. 2004; Lee et al. 2007; Mazumder et al. 2007; Subramanian et al. 2005). Taken together, these results suggest that Ku70 inhibits Bax-mediated apoptosis. We also found that regulation of Ku70 by miR-124 may potentially affect its neuroprotective function in stroke. Specifically, we showed that introduction of anti-miR-124 caused a further increase in Ku70 expression with a consequent reduction in the number of apoptotic cells. Collectively, these results indicate that miR-124 has a critical role in the regulation of ischemic neuronal death via its ability to target Ku70.
In conclusion, our data suggest that Ku70 is a physiological target of miR-124. Knockdown of endogenous miR-124 in vivo protects against I/R-induced neuronal death and apoptosis by targeting Ku70. As Ku70 is a DNA repair protein and antiapoptotic protein that protects against I/R injury in vivo, miR-124 could be a potential therapeutic target to address I/R-triggered cell death after stroke.
References
Aboobaker AA, Tomancak P, Patel N, Rubin GM, Lai EC (2005) Drosophila microRNAs exhibit diverse spatial expression patterns during embryonic development. Proc Natl Acad Sci USA 102:18017–18022
Amsel AD, Rathaus M, Kronman N, Cohen HY (2008) Regulation of the proapoptotic factor Bax by Ku70-dependent deubiquitylation. Proc Natl Acad Sci U S A 105:5117–5122
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Betel D, Koppal A, Agius P, Sander C, Leslie C (2010) Comprehensive modeling of microRNA targets predicts functional non-conserved and non-canonical sites. Genome Biol 11:R90
Betel D, Wilson M, Gabow A, Marks DS, Sander C (2008) The microRNA.org resource: targets and expression. Nucleic Acids Res 36:D149–D153
Chen J, Jin K, Chen M, Pei W, Kawaguchi K, Greenberg DA, Simon RP (1997) Early detection of DNA strand breaks in the brain after transient focal ischemia: implications for the role of DNA damage in apoptosis and neuronal cell death. J Neurochem 69:232–245
Clark AM, Goldstein LD, Tevlin M, Tavare S, Shaham S, Miska EA (2010) The microRNA miR-124 controls gene expression in the sensory nervous system of Caenorhabditis elegans. Nucleic Acids Res 38:3780–3793
Cohen HY, Lavu S, Bitterman KJ, Hekking B, Imahiyerobo TA, Miller C, Frye R, Ploegh H, Kessler BM, Sinclair DA (2004) Acetylation of the C terminus of Ku70 by CBP and PCAF controls Bax-mediated apoptosis. Mol Cell 13:627–638
Dharap A, Bowen K, Place R, Li LC, Vemuganti R (2009) Transient focal ischemia induces extensive temporal changes in rat cerebral microRNAome. J Cereb Blood Flow Metab 29:675–687
Doench JG, Sharp PA (2004) Specificity of microRNA target selection in translational repression. Genes Dev 18:504–511
Friedman RC, Farh KK, Burge CB, Bartel DP (2009) Most mammalian mRNAs are conserved targets of microRNAs. Genome Res 19:92–105
Jeyaseelan K, Herath WB, Armugam A (2007) MicroRNAs as therapeutic targets in human diseases. Expert Opin Ther Targets 11:1119–1129
Jeyaseelan K, Lim KY, Armugam A (2008) MicroRNA expression in the blood and brain of rats subjected to transient focal ischemia by middle cerebral artery occlusion. Stroke 39:959–966
Ketting RF, Fischer SE, Bernstein E, Sijen T, Hannon GJ, Plasterk RH (2001) Dicer functions in RNA interference and in synthesis of small RNA involved in developmental timing in C. elegans. Genes Dev 15:2654–2659
Kim VN (2005) MicroRNA biogenesis: coordinated cropping and dicing. Nat Rev Mol Cell Biol 6:376–385
Kim GW, Noshita N, Sugawara T, Chan PH (2001) Early decrease in DNA repair proteins, Ku70 and Ku86, and subsequent DNA fragmentation after transient focal cerebral ischemia in mice. Stroke 32:1401–1407
Lagos-Quintana M, Rauhut R, Yalcin A, Meyer J, Lendeckel W, Tuschl T (2002) Identification of tissue-specific microRNAs from mouse. Curr Biol 12:735–739
Landgraf P, Rusu M, Sheridan R, Sewer A, Iovino N, Aravin A, Pfeffer S, Rice A, Kamphorst AO, Landthaler M, Lin C, Socci ND, Hermida L, Fulci V, Chiaretti S, Foa R, Schliwka J, Fuchs U, Novosel A, Muller RU, Schermer B, Bissels U, Inman J, Phan Q, Chien M, Weir DB, Choksi R, De Vita G, Frezzetti D, Trompeter HI, Hornung V, Teng G, Hartmann G, Palkovits M, Di Lauro R, Wernet P, Macino G, Rogler CE, Nagle JW, Ju J, Papavasiliou FN, Benzing T, Lichter P, Tam W, Brownstein MJ, Bosio A, Borkhardt A, Russo JJ, Sander C, Zavolan M, Tuschl T (2007) A mammalian microRNA expression atlas based on small RNA library sequencing. Cell 129:1401–1414
Lee Y, Kim M, Han J, Yeom KH, Lee S, Baek SH, Kim VN (2004) MicroRNA genes are transcribed by RNA polymerase II. EMBO J 23:4051–4060
Lee SM, Bae JH, Kim MJ, Lee HS, Lee MK, Chung BS, Kim DW, Kang CD, Kim SH (2007) Bcr-Abl-independent imatinib-resistant K562 cells show aberrant protein acetylation and increased sensitivity to histone deacetylase inhibitors. J Pharmacol Exp Ther 322:1084–1092
Lee ST, Chu K, Jung KH, Yoon HJ, Jeon D, Kang KM, Park KH, Bae EK, Kim M, Lee SK, Roh JK (2010) MicroRNAs induced during ischemic preconditioning. Stroke 41:1646–1651
Lewis BP, Burge CB, Bartel DP (2005) Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell 120:15–20
Liu XS, Chopp M, Zhang RL, Tao T, Wang XL, Kassis H, Hozeska-Solgot A, Zhang L, Chen C, Zhang ZG (2011) MicroRNA profiling in subventricular zone after stroke: MiR-124a regulates proliferation of neural progenitor cells through Notch signaling pathway. PLoS One 6:e23461
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke J Cereb Circ 20:84–91
Mazumder S, Plesca D, Kinter M, Almasan A (2007) Interaction of a cyclin E fragment with Ku70 regulates Bax-mediated apoptosis. Mol Cell Biol 27:3511–3520
Rathaus M, Lerrer B, Cohen HY (2009) Deubiquitylation: a novel DUB enzymatic activity for the DNA repair protein, Ku70. Cell Cycle 8:1843–1852
Sawada M, Sun W, Hayes P, Leskov K, Boothman DA, Matsuyama S (2003) Ku70 suppresses the apoptotic translocation of Bax to mitochondria. Nat Cell Biol 5:320–329
Shackelford DA, Tobaru T, Zhang S, Zivin JA (1999) Changes in expression of the DNA repair protein complex DNA-dependent protein kinase after ischemia and reperfusion. J Neurosci 19:4727–4738
Subramanian C, Opipari AW Jr, Bian X, Castle VP, Kwok RP (2005) Ku70 acetylation mediates neuroblastoma cell death induced by histone deacetylase inhibitors. Proc Natl Acad Sci U S A 102:4842–4847
Swanson RA, Morton MT, Tsao-Wu G, Savalos RA, Davidson C, Sharp FR (1990) A semiautomated method for measuring brain infarct volume. J Cereb Blood Flow Metab 10:290–293
Vemuganti R, Dempsey RJ, Bowen KK (2004) Inhibition of intercellular adhesion molecule-1 protein expression by antisense oligonucleotides is neuroprotective after transient middle cerebral artery occlusion in rat. Stroke 35:179–184
Weng H, Shen C, Hirokawa G, Ji X, Takahashi R, Shimada K, Kishimoto C, Iwai N (2011) Plasma miR-124 as a biomarker for cerebral infarction. Biomed Res (Tokyo, Japan) 32:135–141
Winters A, Taylor JC, Ren M, Ma R, Liu R, Yang SH (2012) Transient focal cerebral ischemia induces long-term cerebral vasculature dysfunction in a rodent experimental stroke model. Transl Stroke Res 3:279–285
Yano K, Morotomi-Yano K, Adachi N, Akiyama H (2009) Molecular mechanism of protein assembly on DNA double-strand breaks in the non-homologous end-joining pathway. J Radiat Res 50:97–108
Yin KJ, Deng Z, Huang H, Hamblin M, Xie C, Zhang J, Chen YE (2010) miR-497 regulates neuronal death in mouse brain after transient focal cerebral ischemia. Neurobiol Dis 38:17–26
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, F., Liu, JL., Li, JP. et al. MicroRNA-124 (miR-124) Regulates Ku70 Expression and is Correlated with Neuronal Death Induced by Ischemia/Reperfusion. J Mol Neurosci 52, 148–155 (2014). https://doi.org/10.1007/s12031-013-0155-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-013-0155-9