Abstract
Data on seasonal differences in stroke incidence are conflicting. Little is known about seasonal variability in etiological stroke subtypes and population-based data on possible trigger factors are lacking. The Ludwigshafen Stroke Study is a prospective population-based stroke registry. All residents of the city of Ludwigshafen who suffer from acute stroke or TIA are registered. Patients with first-ever stroke (FES) were included for the present analysis. Between January 1, 2006 and December 31st, 2010, 1,779 patients (age 71.7 ± 13.4 years (mean + standard deviation; 897 (50.4 %) women) suffered a FES. Incidence for FES was lowest in summer (reference) with significantly higher rates in winter (rate ratio (RR) 1.20, 95 % confidence interval (CI) 1.05–1.37) and spring (RR 1.21 95 % CI 1.06–1.38). First-ever ischemic stroke (FEIS) was more common in winter (RR 1.16, 95 %CI 1.01–1.34) and first-ever intracerebral haemorrhage (FE-ICH) was more frequent in spring (RR 2.0, 95 %CI 1.24–3.22) than in summer. In FES, systolic and diastolic blood pressure on admission (SBP/DBP) showed significant variation with lowest values in summer (SBP: p = 0.02; DBP p = 0.05). In subtypes of FEIS, cardioembolism tended to be more common in winter (p = 0.14). There were no differences in risk factor prevalence between seasons. Leukocyte count on admission was lowest in summer (8.2 ± 1.4/μl) and highest in winter (8.9 ± 1.9/μl; p = 0.008). The hematocrit showed a similar trend (p = 0.06). Our data show higher incidence rates for FES in winter and spring, for FEIS in winter and for FE-ICH in spring. Variations in blood pressure on admission and leukocyte counts were associated with these findings and may possibly contribute to seasonal stroke variability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies investigated the influence of seasonality on stroke incidence. Data are conflicting as some studies found higher stroke incidence during winter and spring and lower incidence during summer and autumn [1–5] while no differences could be observed in other studies [6, 7]. However, several studies were limited by hospital-based study-design [4, 5, 8], low number of observed strokes [7] or age restrictions [2, 5]. Moreover, data on seasonal differences in etiological subtypes of ischemic stroke are rare.
Several trigger factors, such as acute infections, hypercoagulable state and increases in blood pressure due to low ambient temperature, as well as seasonal differences in serum lipids and glucose were discussed as possible explanations for seasonality in vascular diseases [9–11]. However, none of the aforementioned studies on stroke seasonality provides data on such triggers except for traditional risk factors.
Population-based data on stroke incidence represent the most suitable basis for analysing possible seasonal differences in stroke epidemiology. We therefore studied the seasonal influence on incidence of total first-ever stroke (FES), stroke subtypes, stroke etiology in ischemic stroke and risk factors for ischemic stroke in a population-based study. To investigate the possible impact on aforementioned triggers on stroke seasonality we additionally analysed laboratory parameters that serve as markers for inflammation and hypercoagulable state (C-reactive protein (CRP), fibrinogen, leukocyte count, haematocrit) in first-ever ischemic (FEIS) stroke.
Subjects and methods
The “Ludwigshafen Stroke Study” (LuSSt) is a prospective population-based stroke register in the population of the city of Ludwigshafen starting January 1, 2006. LuSSt includes all patients with incident stroke or TIA. A detailed description of LuSSt has been published recently [12]. All patients with FES until December 31st, 2010 were included in the present analysis.
Executive summary of study population, case ascertainment and standard definitions
Ludwigshafen is an industrial city in the state of Rhineland-Palatinate in West Germany. The total source population was 167.657 inhabitants (83.009 males and 84.648 females) on December 31st, 2008. The patients′ postal address accounted for affiliation to the study population. Multiple overlapping methods of patient identification were used to achieve complete case ascertainment as described before [12]. Case ascertainment in hospitalized patients was ensured by collaboration with all hospitals in the city of Ludwigshafen and surrounding hospitals outside the city boundaries that treat stroke patients. To identify patients that have been treated in other hospitals or hospitals abroad and those patients that were non-hospitalized, all general practitioners, specialists in internal medicine and neurologists practicing in Ludwigshafen were regularly contacted and asked to report on such patients. Furthermore, we contacted nursing and residential homes and reviewed death certificates obtained by the local health authority. Patients that were treated at the Klinikum Ludwigshafen and those being treated outside the Klinikum, but who gave written consent by themselves or their legal representatives were examined by a professional member of the study team using a structured questionnaire. Data could be registered including personal data. If informed consent was not available in patients being treated outside Klinikum Ludwigshafen, study data were obtained by the attending physician and transmitted to the study centre in pseudonomized form. In stroke patients that have been identified via death certificates we intensely tried to obtain more information (especially on current stroke symptoms and status of stroke recurrence) by contacting the patients′ general practitioner. The study was approved by the ethics committee of the Landesärztekammer Rhineland-Palatinate and by the data protection commissioner of Rhineland-Palatinate.
Stroke was defined according to the definition of the World Health Organization (WHO) [13]. Stroke subtype classification was based on the results of brain imaging, discriminating between ischemic stroke (IS), intracerebral hemorrhage (ICH) or subarachnoid hemorrhage (SAH). If no brain imaging was available, for example in those patients that died before hospital admission, stroke type was defined as undetermined (UND).
Etiology of ischemic stroke and vascular risk factors
Assignment to etiology in ischemic stroke was performed using modified TOAST-criteria as described in detail before [14, 15]. Stroke due to large artery-atherosclerosis was diagnosed in patients with with stenoses >50 % diameter reduction on Duplex sonography or CT-, MR- or digital subtraction angiography of brain supplying arteries and brain infarcts >1.5 cm in the absence of any source of cardioembolism. Cardioembolism was defined as presence of high- or medium-risk source for cardiac embolism in the absence of other etiologies. Stroke of microangiopathic origin was assigned to patients with typical lacunar syndrome in the absence of brain infarcts >1.5 cm and no evidence of cortical dysfunctions. In patients with rare causes of ischemic stroke, such as hematologic disorders, stroke of other determined etiology was diagnosed. Original TOAST-criteria were modified by inserting the category “stroke of probable atherothrombotic origin”. “Probable atherothrombotic stroke” was diagnosed in patients with stenoses <50 % diameter reduction of brain supplying arteries and brain infarcts >1.5 cm in the absence of any source of cardioembolism. In patients with more than one potential cause for stroke, etiology was assigned to the most likely causative mechanism according to the SSS-TOAST classification [16].
Cardiovascular risk factors were defined according to current national and international guidelines as described in detail before [14, 17]. In brief, hypertension was diagnosed in case of antihypertensive medication on admission, a respective diagnosis by a physician before or if blood pressure was >140/90 mmHg in 2 or more measurements >3 days after stroke. Diabetes mellitus was acknowledged in patients with fasting blood glucose level above 125 mg/dl, with antidiabetics on admission or if a physician had previously made this diagnosis. Hypercholesterolemia was diagnosed in patients with fasting cholesterol levels >200 mg/dl or LDL-cholesterol >140 mg/dl or with cholesterol-lowering medication on admission. AF was ascertained based on ECG or Holter monitoring or in case of a previous respective diagnosis.
Laboratory tests and clinical characteristics on admission
CRP [particle-enhanced immunoturbidimetric assay CRPL3 (cobas®)], fibrinogen (Clauss method on IL Coagulation Systems, Instrumentation Laboratory), blood glucose [enzymatic in vitro test Gluco-quant (cobas®)], leukocyte count and hematocrit (XE analyser XE-2100; Sysmex) were determined shortly after admission. Latency between stroke onset and venipuncture was recorded on daily level. Parameters were assessed in patients with FEIS and patients admitted to the Klinikum Ludwigshafen. About 90 % of all patients with FES in the source population are admitted to this hospital.
Stroke severity was determined using National Institute of Health Stroke Scale (NIHSS) [18]. The first systolic and diastolic blood pressure (SBP, DBP) measured on admission was used for the analyses.
Statistical analyses
We calculated crude incidence rates for FES and stroke dividing numbers of stroke events by the person-years of subjects at risk in the source population. Exact 95 % CIs for the rates based on the Poisson distribution were determined. To assess seasonal trends for FES, we applied a Poisson regression model to model the rate of strokes by month. The accumulated monthly cases for FES were counted and a crude incidence rate was calculated as IR = Ni/M. Here, M is the population times the relative length of the month (e.g. 31/365) times the number of observation years (5) as an approximation of the person-years for each month and Ni is the total number of strokes in month i (i = 1,…,12). The population experienced little change over the observation period from 2006 to 2010, therefore we used a constant population. The monthly crude incidence rates (CIR) were then modelled with a Poisson regression model by:
The underlying model assumption is that the seasonal pattern can be described as a sinusoidal function [19] with 12 months period length. β1 and β2 are regression coefficients to describe seasonal variation over i. In order to test the Null hypothesis that seasonal variation would not contribute to the variation pattern we compared the above model with the base model using a log likelihood ratio (LLR) test. The LLR test was performed calculating the model difference in log likelihood, −2 [log likelihood base model—log likelihood model (1)], which is asymptotically Chi square distributed with 2 degrees of freedom under the null hypothesis. We also fitted more complex models additionally including the covariables age, sex and calendar year. In FES, FEIS and FE-ICH, incidence rates were calculated in total and for each season of the year (winter: December–February; spring: March–May; summer: June–August; autumn: September–November). Month of stroke onset accounted for seasonal assignment.
We calculated incidence rate ratios (RR) between seasons using summer as the baseline season for FES, FEIS and FE-ICH by comparative analysis of rates with 95 % CI proposed by Miettinen and Nurminen [20]. The Χ2-test was used to analyse seasonal differences in binary risk factors for stroke, and the F-test (Analysis of Variance) was used to analyse seasonal differences for laboratory parameters. Leukocyte count, fibrinogen and CRP were log-transformed prior to analysis. Confidence intervals for means were calculated. Log-transformed means and CI values were reconverted by exponentiation.
Correlation between parameters was analysed with Spearman correlation coefficient. All tests were two-sided. Level of significance was set to 5 %. All calculations were performed using SAS 9.2. PROC GENMOD and PROC GLM were used for regression analysis.
Results
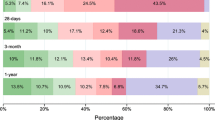
Between 2006 and 2010, 1,779 patients (897 (50.4 %) women, 868 (48.8 %) men, 14 (0.8 %) unknown sex) suffered a FES. Mean age was 71.7 years (SD 13.5). Of all 1,779 patients with FES, 1,547 (87.0 %) suffered FEIS. In 152 (8.5 %) FE-ICH was diagnosed. SAH was assigned in 50 patients (2.8 %). Stroke subtype remained undetermined in 30 patients (1.7 %). Figure 1 presents monthly crude incidence rates for FES (with 95 % CIs) and the results for the Poisson model using the sinusoidal function. We observe a significant seasonal pattern (p < 0.001) with lowest rates at late summer and highest rates in late winter. Further modelling showed that this seasonal pattern was not confounded by age, sex or calendar year. Crude incidence rates for FES, stroke subtypes, and clinical characteristics on admission (NIHSS, SBP, DBP) according to season are presented in Table 1.
As incidence rates were lowest in summer we calculated RR for incidence of FES, FEIS and FE-ICH in each season with reference to summer (Figs. 2, 3, 4). Incidence of FES was significantly higher in winter and spring than in summer whereas difference between summer and autumn was of borderline significance. In FEIS incidence was significantly higher in winter, whereas in FE-ICH, incidence was 100 % higher in spring than in summer (Fig. 4). In total 58 FES (3.3 %) [winter: n = 13 (22.4 %); spring: n = 24 (41.4 %); summer: n = 10 (17.2 %); autumn: n = 11 (19.0 %)] occurred outside the City of Ludwigshafen.
Clinical characteristics on admission showed a trend towards lower NIHSS for FES on admission in spring and summer as compared to winter and autumn. Significant seasonal differences were registered for SBP (p = 0.02) and DBP (p = 0.05) with lowest values in summer. Delay between stroke onset and time point of BP measurement showed no significant differences on daily level (p = 0.47). Correlation between blood pressure and stroke severity (NIHSS) was marginal with a correlation coefficient of 0.08 for SBP (p = 0.003) and 0.06 (p = 0.002) for DBP. There was no seasonal difference regarding the prevalence of stroke risk factors (Table 2).
Stroke etiology in ischemic stroke according to modified TOAST-criteria showed no significant seasonal differences. There was a trend towards higher incidence of stroke due to cardioembolism in winter (p = 0.14).
Results of laboratory tests on admission in patients with FEIS are presented in Table 3. Most blood samples (80 %) were taken within 24 h after stroke. There were no seasonal differences in time delay between stroke onset and venipuncture on daily level (p = 0.47). Significant seasonal differences could be shown for leukocyte count (p = 0.008) on admission, with highest values during winter. A similar, although non-significant difference was seen for hematocrit (p = 0.06). The correlation coefficient between leukocyte count and NIHSS on admission was 0.20 (p < 0.001). There were no seasonal differences for fibrinogen, blood glucose levels or CRP.
Discussion
We analysed seasonal differences in FES incidence in a population-based stroke registry and included stroke subtypes, blood pressure and, especially in ischemic stroke, risk factors, blood glucose and markers of inflammation and coagulation.
The risk of FES showed significant seasonal variations with an about 20 % higher incidence in winter and spring as compared to summer months. This observation is in line with other studies on seasonal variation in stroke incidence [2, 4, 8]. However, some studies reported no seasonal influence on stroke incidence [6, 7]. Analysing seasonal distribution of FES occurring outside study area does not point towards a possible summer bias on stroke seasonality as seasonal pattern was comparable to that of all FES. Furthermore, the majority of cases are beyond retirement age. Different to younger families with school children, this age group can also spend vacation outside peak summer season, when prices are highest. We therefore do not think that seasonal variation of the population present in the study area could have had a major effect.
Considering clinical characteristics on admission, SBP and DBP showed significant seasonal variation in stroke patients with lowest values in summer. This might be a hint towards seasonal differences in blood pressure in the general population of our study as variations in blood pressure have been reported with lower values during summer and higher values in colder months [21]. As multiple trials and meta-analyses have shown that a moderate decrease in SBP and DBP reduces the relative risk for stroke up to 40 %, seasonal variations in blood pressure might partly explain variations in stroke incidence [22, 23]. However, due to descriptive design of our study causality can not be inferred from our data. Several studies have addressed seasonal variation in blood pressure to changes in outdoor temperature as they found an inverse relationship [24, 25]. Additionally, seasonal changes in multiple climate factors such as particulate matter and ozone might also play a role in seasonal variation of blood pressure [26]. Stress induction might be one pathway linking seasonal changes in climatic factors and stroke.
Although NIHSS on admission showed a trend towards lower stroke severity in summer, blood pressure values on admission were likely not influenced by stroke severity as both values showed only marginal correlation. We could not detect seasonal variation for history of arterial hypertension in our study. This might be explained by the fact that history of hypertension is already known for long time in the majority of stroke patients, and therefore seasonal variation might especially influence level of hypertension but not the diagnosis of hypertension per se. Recent data suggesting better control of blood pressure during summer months in hypertensive patients support this thesis [27].
In FEIS, incidence was 16 % higher in winter as compared to summer. This finding is in line with results from the FINMONICA Stroke Register observing comparable seasonal variation of FEIS [2]. We found no seasonal variation for history of risk factors in our study, which is in line with recent studies indicating seasonal differences in stroke incidence being independent of the risk factor profile per se [4]. Laboratory results in FEIS showed significant seasonal differences for leukocyte count and a non-significant trend for hematocrit towards lower values in summer. Leukocyte counts were lowest during summer and highest in winter and spring, which like in blood pressure might point to variation of leukocyte count in our source population. Elevated leukocyte counts have shown to be associated with an elevated risk for future cardiovascular and cerebrovascular events [28–30]. On one hand, leukocyte count might simply represent a marker of inflammation, on the other hand, leukocytes may also be directly involved in complications of atherosclerosis, such as plaque rupture and thrombosis [30]. Acute infections (e.g. acute respiratory infections, influenza) have been shown to temporally increase stroke risk. They show distinctive seasonal patterns with lower incidence in summer and higher incidence in winter and spring. A higher rate of infections during winter months may explain higher leukocyte counts during this season and may partly account for seasonal variations in incidence of FEIS [31]. As a limitation, we did not directly assess pre stroke infection in this study, however. Recent studies have shown leukocytosis on admission to be related to severity of ischemic damage suggesting that NIHSS on admission may confound the relationship between leukocyte count and variability of stroke incidence. However, we found only a weak correlation between stroke severity on admission and leukocyte count [32]. Considering hematocrit, we observed a non-significant trend towards elevated values during winter. Hematocrit is the major contributor to blood viscosity. Highly elevated values have been identified as a risk factor for ischemic stroke [33]. Variation in hematocrit with lowest values in summer has been reported previously [34, 35], suggesting heat acclimatization and intravascular fluid shifts during summer as possible explanation. Seasonal patterns of hematocrit were negatively associated with mean monthly temperature. Hemoconcentration during cold weather might also contribute to seasonality in stroke incidence. In FE-ICH, incidence was significantly higher in spring as compared to summer which is again in line with results from the FINMONICA Stroke Register [2].
Our study has strengths and limitations. We provide data from a population-based stroke registry without age-restrictions. Compared to first 2 years of registration, crude incidence rates remain stable indicating robust quality of case ascertainment. Data analysis is based on a large sample-size. However, due to stroke epidemiology, number of FE-ICH is rather low and results have to be interpreted with caution. As our study design is primarily descriptive we might only describe associations between stroke incidence and possibly interfering factors like leukocyte count or blood pressure. We may therefore only give presumptions of potential causal relationships. Furthermore, laboratory analysis does not include neutrophil counts although neutrophils have been shown to be a better predictor than total leukocyte count for ischemic stroke [28]. Due to population-based study design laboratory results are not complete. However, laboratory results could have been analysed in approximately 90 % of all patients with ischemic stroke.
Conclusion
Our data show significant variations in seasonal incidence for stroke in the city of Ludwigshafen. In FES, FEIS and FE-ICH lowest incidence was observed in summer whereas incidence was elevated in winter for FES and FEIS and in spring for FES and FE-ICH. Seasonal differences in SBP and DBP on admission with lower values during summer and higher values in winter and spring in FES are associated with stroke seasonality and might partly play a role. In FEIS differences in leukocyte count are concomitant and may reflect the impact of infection and inflammation on stroke seasonality.
References
Giroud M, Beuriat P, Vion P, D’Athis PH, Dusserre L, Dumas R. Stroke in a French prospective population study. Neuroepidemiology. 1989;8(2):97–104.
Jakovljevic D, Salomaa V, Sivenius J, Tamminen M, Sarti C, Salmi K, et al. Seasonal variation in the occurrence of stroke in a Finnish adult population. The FINMONICA Stroke Register. Finnish monitoring trends and determinants in cardiovascular disease. Stroke. 1996;27(10):1774–9.
Ricci S, Celani MG, Vitali R, La Rosa F, Righetti E, Duca E. Diurnal and seasonal variations in the occurrence of stroke: a community-based study. Neuroepidemiology. 1992;11(2):59–64.
Turin TC, Kita Y, Murakami Y, Rumana N, Sugihara H, Morita Y, et al. Higher stroke incidence in the spring season regardless of conventional risk factors: Takashima Stroke Registry, Japan, 1988–2001. Stroke. 2008;39(3):745–52. doi:10.1161/STROKEAHA.107.495929.
Wang H, Sekine M, Chen X, Kagamimori S. A study of weekly and seasonal variation of stroke onset. Int J Biometeorol. 2002;47(1):13–20. doi:10.1007/s00484-002-0147-x.
Khan FA, Engstrom G, Jerntorp I, Pessah-Rasmussen H, Janzon L. Seasonal patterns of incidence and case fatality of stroke in Malmo, Sweden: the STROMA study. Neuroepidemiology. 2005;24(1–2):26–31. doi:10.1159/000081046.
Rothwell PM, Wroe SJ, Slattery J, Warlow CP. Is stroke incidence related to season or temperature? The Oxfordshire Community Stroke Project. Lancet. 1996;347(9006):934–6.
Wang Y, Levi CR, Attia JR, D’Este CA, Spratt N, Fisher J. Seasonal variation in stroke in the Hunter Region, Australia: a 5-year hospital-based study, 1995–2000. Stroke. 2003;34(5):1144–50. doi:10.1161/01.STR.0000067703.71251.B6.
Mavri A, Guzic-Salobir B, Salobir-Pajnic B, Keber I, Stare J, Stegnar M. Seasonal variation of some metabolic and haemostatic risk factors in subjects with and without coronary artery disease. Blood Coagul Fibrinolysis. 2001;12(5):359–65.
Tofler GH, Muller JE. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation. 2006;114(17):1863–72. doi:10.1161/CIRCULATIONAHA.105.596189.
Woodhouse PR, Khaw KT, Plummer M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. 1993;11(11):1267–74.
Palm F, Urbanek C, Rose S, Buggle F, Bode B, Hennerici MG, et al. Stroke incidence and survival in Ludwigshafen am Rhein, Germany: the Ludwigshafen Stroke Study (LuSSt). Stroke. 2010;41(9):1865–70. doi:10.1161/STROKEAHA.110.592642.
Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ. 1976;54(5):541–53.
Palm F, Urbanek C, Wolf J, Buggle F, Kleemann T, Hennerici MG, et al. Etiology, risk factors and sex differences in ischemic stroke in the Ludwigshafen Stroke Study, a population-based stroke registry. Cerebrovasc Dis. 2012;33(1):69–75. doi:10.1159/000333417.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Ay H, Furie KL, Singhal A, Smith WS, Sorensen AG, Koroshetz WJ. An evidence-based causative classification system for acute ischemic stroke. Ann Neurol. 2005;58(5):688–97. doi:10.1002/ana.20617.
Balkau B. The DECODE study. Diabetes epidemiology: collaborative analysis of diagnostic criteria in Europe. Diabetes Metab. 2000;26(4):282–6.
Goldstein LB, Bertels C, Davis JN. Interrater reliability of the NIH stroke scale. Arch Neurol. 1989;46(6):660–2.
Kynast-Wolf G, Hammer GP, Muller O, Kouyate B, Becher H. Season of death and birth predict patterns of mortality in Burkina Faso. Int J Epidemiol. 2006;35(2):427–35. doi:10.1093/ije/dyi150.
Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med. 1985;4(2):213–26.
Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J (Clin Res Ed). 1982;285(6346):919–23.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
Collins R, Peto R, Godwin J, MacMahon S. Blood pressure and coronary heart disease. Lancet. 1990;336(8711):370–1.
Kunes J, Tremblay J, Bellavance F, Hamet P. Influence of environmental temperature on the blood pressure of hypertensive patients in Montreal. Am J Hypertens. 1991;4(5 Pt 1):422–6.
Alperovitch A, Lacombe JM, Hanon O, Dartigues JF, Ritchie K, Ducimetiere P, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Intern Med. 2009;169(1):75–80. doi:10.1001/archinternmed.2008.512.
Urch B, Silverman F, Corey P, Brook JR, Lukic KZ, Rajagopalan S, et al. Acute blood pressure responses in healthy adults during controlled air pollution exposures. Environ Health Perspect. 2005;113(8):1052–5.
Fletcher RD, Amdur RL, Kolodner R, McManus C, Jones R, Faselis C, et al. Blood pressure control among US veterans: a large multiyear analysis of blood pressure data from the Veterans Administration health data repository. Circulation. 2012;125(20):2462–8. doi:10.1161/CIRCULATIONAHA.111.029983.
Grau AJ, Boddy AW, Dukovic DA, Buggle F, Lichy C, Brandt T, et al. Leukocyte count as an independent predictor of recurrent ischemic events. Stroke. 2004;35(5):1147–52. doi:10.1161/01.STR.0000124122.71702.64.
Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA. 1998;279(18):1477–82.
Coller BS. Leukocytosis and ischemic vascular disease morbidity and mortality: is it time to intervene? Arterioscler Thromb Vasc Biol. 2005;25(4):658–70. doi:10.1161/01.ATV.0000156877.94472.a5.
Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351(25):2611–8. doi:10.1056/NEJMoa041747.
Nardi K, Milia P, Eusebi P, Paciaroni M, Caso V, Agnelli G. Admission leukocytosis in acute cerebral ischemia: influence on early outcome. J Stroke Cerebrovasc Dis. 2011;. doi:10.1016/j.jstrokecerebrovasdis.2011.04.015.
Gagnon DR, Zhang TJ, Brand FN, Kannel WB. Hematocrit and the risk of cardiovascular disease—the Framingham study: a 34-year follow-up. Am Heart J. 1994;127(3):674–82.
Thirup P. Haematocrit: within-subject and seasonal variation. Sports Med. 2003;33(3):231–43.
Sebok MA, Notari EP, Chambers LA, Benjamin RJ, Eder AF. Seasonal temperature variation and the rate of donor deferral for low hematocrit in the American Red Cross. Transfusion. 2007;47(5):890–4. doi:10.1111/j.1537-2995.2007.01206.x.
Acknowledgments
Data analysis was supported by a grant from the Deutsche Forschungsgemeinschaft (DFG; GR1102/6-1). LuSSt is part of the German Competence Network Stroke.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palm, F., Santos, M.D., Urbanek, C. et al. Stroke seasonality associations with subtype, etiology and laboratory results in the Ludwigshafen Stroke Study (LuSSt). Eur J Epidemiol 28, 373–381 (2013). https://doi.org/10.1007/s10654-013-9772-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-013-9772-4