Abstract
Altered metabolism was first identified in cancer cells by Otto Warburg, who identified a higher reliance on anaerobic glycolysis rather than cellular respiration even in the presence of sufficient oxygen levels, a phenomenon called the Warburg Effect. Deregulated metabolism is now considered a driving hallmark of cancer and an attractive therapeutic target. While a great deal of work is being done to find genetic therapeutic targets that can be used for personalized medicine, current targeted approaches are typically ineffective because tumors are heterogeneous and contain multiple genetic subpopulations. This often precludes a particular targeted molecule from being found on all cells. In contrast to many genetic alterations, dysregulation of metabolism resulting in the need for high amounts of glucose is found in virtually all cancer cells. Targeting metabolism by reducing blood glucose may be a way to inhibit tumor growth since this, to a large extent, should circumvent the inherent problems associated with tumor heterogeneity. Methods that also provide an energy source for normal tissues such as ketones should reduce side effects associated with an overall reduction in blood glucose. The high-fat, low carbohydrate, and protein ketogenic diet (KD) results in reduced blood glucose and increased blood ketones, as does caloric restriction and fasting. In preclinical mouse models of malignant brain tumors, animals fed a KD had increased survival, particularly when used in combination with radiation or chemotherapy. Metabolic modulation through the use of a KD, caloric restriction, or fasting has been found to change the expression of a number of genes and pathways thought to inhibit tumor growth. Metabolic therapy has also recently been explored in other cancer types. In this chapter, we will examine the mechanisms underlying the KD which suggests its potential as an adjuvant therapy for cancer treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Every year, ~14,000 new cases of malignant glioma are diagnosed in the United States. Brain tumors are also the second leading cause of cancer deaths among children and young adults. Glioblastoma (GBM) or grade IV astrocytoma is the most aggressive grade of this disease. The standard of care is surgery followed by radiation and chemotherapy. Like many cancers, brain tumor cells tend to infiltrate adjoining tissue; however, unlike other cancers, complete surgical resection is hampered by the eloquent nature of the brain. While radiation and chemotherapy with alkylating agents such as temozolomide are somewhat effective, again the location can reduce the efficacy of these therapies. Radiation is typically targeted to the tumor to reduce toxicity to normal brain tissue, and the blood–brain barrier limits the number of chemotherapies that are effective. Thus, once a tumor recurs following chemotherapy with temozolomide, there are few additional chemotherapeutic agents with demonstrated efficacy for the treatment of brain tumors. Cells that survive initial therapies typically regrow, and these tumors often recur rapidly. Recurrent tumor is typically resistant to additional chemotherapy and the use of additional radiation can be hazardous due to toxicity to normal brain (Weller et al. 2012). For these reasons, median survival of patients diagnosed with a GBM is 12–18 months and there is less than a 10 % 5-year survival rate (Anton et al. 2012; Bloch et al. 2012). This underscores the need for new therapies for the treatment of malignant brain tumors.
The human genome project has spawned a virtual explosion of tools for the study of the molecular underpinnings of human disease. In-depth molecular analysis of malignant gliomas has been done by The Cancer Genome Atlas consortium (The Cancer Genome Atlas Research Group 2008) and other groups (Brennan et al. 2009; Brennan 2011; Lee et al. 2008; Verhaak et al. 2010). This data has shown that not all GBMs have the same molecular basis. This has fueled the idea that therapies can be tailored to the molecular traits of an individual person’s disease, so-called “personalized medicine.” The ultimate goal of these studies is the identification of therapeutic targets and a better understanding of how to determine the best patients for these specific targeted agents (Masui et al. 2012). While studies such as these may ultimately prove useful, to date they have met with limited success. This is likely due to the heterogeneity seen in most solid tumors. In fact, biopsies taken from different regions of the same tumor can sometimes suggest that the tumor has components of more than one GBM subtype (Gill et al. 2014; Patel et al. 2014). Advances in survival and quality of life rely on new therapeutic strategies, especially those that can enhance the efficacy of current treatment options without damaging the normal brain.
2 Tumor Metabolism
Alterations in the metabolism of cancer cells, what we now call the “Warburg effect” or aerobic glycolysis, were first described by Otto Warburg in 1927 (Warburg et al. 1927). Cancer cells use glycolysis to provide energy and biomolecules regardless of the availability of oxygen. This results in the production of fewer ATP molecules per molecule of glucose, and thus tumor cells require large amounts of glucose. This shift toward increased glycolytic flux in the cytosol and away from the tricarboxylic acid cycle and oxidative phosphorylation in the mitochondria occurs very early in tumorigenesis. This allows for rapid cell proliferation even under conditions of hypoxia and in the presence of dysfunctional mitochondria. Since Warburg’s discovery, metabolism has been of interest in the cancer field, but it often seemed overshadowed by discoveries of oncogenes, tumor suppressor genes, growth factor pathways, molecular subtypes of cancers, etc. There is a resurgence of interest in metabolism as a central theme in cancer, and we continue to find that metabolic pathways intersect and often regulate key components of tumor initiation, progression, and therapy response (Nijsten and van Dam 2009; Wolf et al. 2010). In fact, altered metabolism has been referred to as a hallmark of cancer (Cantor and Sabatini 2012; Ward and Thompson 2012).
The term “metabolic remodeling” has been used to describe some of the metabolic changes that can occur in cancer cells, and a wide variety of oncogenes have been found to be involved in metabolism (Obre and Rossignol 2015). For example, the tumor suppressor protein p53 which plays a pivotal role in the cellular responses to hypoxia, DNA damage, and oncogene activation has recently been found to regulate glycolysis and assist in maintaining mitochondrial integrity (Puzio-Kuter 2011). MYC has been found to activate glutaminolysis and lipid synthesis from citrate (Obre and Rossignol 2015). The overactivation of the stress-responsive PI3K/AKT signaling pathway, typical in many cancers, has also been closely linked to metabolism and under low glucose conditions results in rapid tumor cell death (Marie and Shinjo 2011; Robey and Hay 2009; Yang et al. 2009). Furthermore, Hypoxia-inducible factor 1 (HIF-1) may, at least in part, provide the molecular basis for the Warburg effect. HIF-1 can “reprogram” cellular metabolism in response to oxygen availability. In doing so, it contributes to the cancer cell phenotype in a number of ways. HIF-1 expression is activated by hypoxia, which subsequently activates the transcription of genes involved in angiogenesis (VEGF and other cytokines) in an attempt to improve tissue perfusion. This often results in the formation of abnormal blood vessels that contribute to metastasis in some cancers, and can increase inflammation and edema in brain tumors. Loss of function of phosphatase and tensin homologue (PTEN) or mutation of p53 also increases HIF-1, as does the accumulation of reactive oxygen species (ROS). We now know that cancer cell metabolism is far more complex than originally thought and a number of cancer-associated mutations affect metabolism, and there are numerous reviews on the subject (Cantor and Sabatini 2012; Gatenby and Gillies 2004; Semenza 2013; Vander Heiden et al. 2009; Ward and Thompson 2012). The fact that metabolic dysregulation is seen in virtually all tumor cells has led to suggestions that a promising therapeutic strategy may be to exploit this feature. One potential way to achieve this goal is through the use of the therapeutic ketogenic diet (KD) or physiologically similar methods, such as caloric restriction or intermittent fasting.
3 The Ketogenic Diet
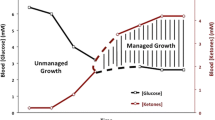
The ketogenic diet (KD) is more correctly referred to as “metabolic therapy” rather than a “diet.” This high-fat low protein/carbohydrate diet is used to treat refractory epilepsy (Cross 2013; Kim and Rho 2008) in children, and more recently in some adults. The diet is not without side effects; however, these are typically readily managed when the patient has appropriate supervision by a registered dietitian skilled in its use. The KD has been shown to have neuroprotective effects and there are now studies to determine its efficacy for a number of neurological disorders, including Alzheimer’s disease, traumatic brain injury, and amyotrophic lateral sclerosis (Maalouf et al. 2009; Stafstrom and Rho 2012). The KD increases blood ketones and decreases blood glucose by simulating the physiological response to fasting, thus leading to high rates of fatty acid oxidation and an increase in the production of acetyl coenzyme A (acetyl-CoA). When the amount of acetyl-CoA exceeds the capacity of the tricarboxylic acid cycle to utilize it, there is an increase in the production of the ketone bodies β-hydroxybutyrate (βHB) and acetoacetate (ACA), which can be used as an energy source in the brain (Cahill and Veech 2003; Morris 2005; Vanitallie and Nufert 2003; Veech et al. 2001). The metabolic alterations found in cancer cells are generally thought to reduce their ability to be “flexible” regarding their primary energy source, and thus they require glucose and are unable to use ketones like normal cells (Fredericks and Ramsey 1978; Maurer et al. 2011; Seyfried et al. 2011; Seyfried 2012; Seyfried and Mukherjee 2005; Tisdale and Brennan 1983; Zhou et al. 2007). Normal cells readily use ketones as an alternate energy source and are thus unaffected by the ketogenic diet. In contrast, the reduction in glucose inhibits the growth of tumor cells. Thus, when used as a therapy, the KD can take advantage of the Warburg effect. In addition, work in the epilepsy field and more recent work in cancer research have shown that the effects of the ketogenic diet extend far beyond the simple growth inhibitory effects of reduced glucose. We used a cell line derived from a recurrent human glioblastoma to demonstrate the in vitro effect of adding ketones to media containing glucose (Scheck et al. 2012). The AO2V4 cell line was derived from a recurrent human glioblastoma and grown in Waymouth’s MAB 87/3 media supplemented with 20 % fetal calf serum. When 10 mM βHB plus ACA was added to complete media, cell growth was significantly inhibited. There was additional growth inhibition when 1,3-bis(2-chloroethyl)-1 nitrosourea (BCNU, carmustine), one of the chemotherapeutic agents given to this patient prior to tumor recurrence, compared to either ketones or BCNU alone. More recent work has shown that the ketones themselves exert antitumor effects separate from the effects of reduced blood glucose (Magee et al. 1979; Scheck et al. 2012; Skinner et al. 2009). This chapter addresses the utility of increasing blood ketones and reducing blood glucose for the treatment of brain tumors.
4 Gene Expression
Studies done in our laboratory using a GL261/C57BL/6 mouse model of malignant glioma demonstrated that the KD exerts a global effect on the aberrant genetic landscape found in tumors (Scheck et al. 2012). We compared gene expression in tumor tissue and tissue from the contralateral non-tumor containing side of the brain using cDNA array technology. This work showed that overall gene expression in tumor from animals fed the KD was shifted more toward the gene expression found in non-tumor containing tissue from animals fed either the KD or standard diet (Stafford et al. 2010) (Fig. 1). Furthermore, the changes in gene expression were different in tumor tissue compared to that seen in the contralateral non-tumor containing side of the brain (Stafford et al. 2010), a finding similar to that of Maurer (Maurer et al. 2011) who demonstrated differential effects of 3-hydroxybutyrate (in vitro) and a non-calorie-restricted ketogenic diet (in vivo) on normal glia versus glioma cells and tumors. Differences in the response of normal cells versus tumor cells are likely to be due to the alterations in metabolism that are a hallmark of cancer. However, the global nature of these differences has been somewhat surprising, and while the underlying mechanism(s) of these pluripotent effects has not been elucidated, it may be based at least in part on epigenetic changes. Epigenetic changes are heritable alterations in gene activity that are not due to DNA sequence changes (Baylin and Jones 2011). These changes include chromatin remodeling, histone modifications, DNA methylation, and alterations in microRNA pathways, all of which have now been linked to gene expression changes and metabolism in many cancers, including brain tumors (Venneti and Thompson 2013; Yun et al. 2012). In fact, the epigenetic changes found in some cancers are now being looked at as potential therapeutic targets. New therapies such as histone deacetylase (HDAC) inhibitors are actively being tested for their ability to reverse the abnormal gene expression patterns inherent to the cancer epigenome and for their ability to enhance other antitumor therapies (Azad et al. 2013; Qureshi and Mehler 2013). Support for the idea that the effects of the ketogenic diet may be due, at least in part, to changes in the genome comes from a recent study demonstrating that β-hydroxybutyrate (βHB), the major ketone elevated in the blood as a result of the ketogenic diet, can also inhibit HDAC, thus altering the epigenetic landscape in much the same way as the HDAC inhibitors currently being tested (Shimazu et al. 2013). While direct effects of the KD on epigenetic changes in brain tumors have not yet been shown, it has been shown to reverse the major epigenetic modifications seen in the brains of epileptic rats (Kobow et al. 2013), thus suggesting that this may indeed be one mechanism through which ketogenic diet exerts its antitumor effect.
The KD alters overall gene expression to more closely resemble that seen in normal brain. Total cellular RNA was isolated from the tumor and the non-tumor containing contralateral side of the brain. Gene expression was analyzed using Affymetrix GeneChip® Mouse Genome 430 2.0 arrays (Affymetrix, Santa Clara, CA). A two-way ANOVA for interaction showed that the data from the tumor sample obtained from mice fed a SD are clearly separate from the data obtained from the other three conditions. This analysis implies that the KD is driving the overall gene expression in the tumor to be more normal, that is, to be more like gene expression seen in the non-tumor containing tissue. Reprinted from (Stafford et al. 2010)
5 Growth Factor Signaling
A number of growth factor signaling pathways are critical to the formation and progression of malignant brain tumors. Insulin-like growth factor 1 (IGF-I) is one such growth factor that supports the growth of the number of cancers including brain tumors (Arcaro 2013; Haisa 2013; Hummel et al. 2013; Negi et al. 2013; Singh et al. 2014; Weroha and Haluska 2012). We have shown that IGF1 expression is markedly reduced in tumors from mice fed a KD compared to those fed a standard diet (Fig. 2). Similar results have been found by others using caloric restriction in a variety of mouse models of malignant brain tumors (Marsh et al. 2008; Seyfried et al. 2003; Shelton et al. 2010). cDNA array analysis also showed a reduction in the expression of RAS p21 protein activator 1 and mitogen-activated protein kinase 8 (c-Jun N-terminal kinase, JNK) in tumors from animals fed a KD (Scheck et al. 2012). These proteins participate in the platelet-derived growth factor and epidermal growth factor receptor tyrosine kinase signaling pathways, suggesting that the KD may act as a “pan-growth factor inhibitor.”
Immunohistochemical analysis of Insulin Growth Factor 1 (IGF1). There is an increase in the expression of IGF1 in tumor tissue relative to non-tumor in animals fed a standard diet. In animals fed a ketogenic diet, the IGF1 expression in tumor tissue is reduced to the level of the adjacent non-tumor tissue. Reprinted from (Scheck et al. 2012)
Growth factor pathways also intersect with metabolism through the PI3K/Akt pathway which can be activated by a number of receptor tyrosine kinase growth factor pathways or activated Ras (Cantor and Sabatini 2012). The PI3K/Akt pathway is also closely linked to glucose metabolism and has been called the “Warburg kinase” (Robey and Hay 2009). Recent studies have shown that the action of Akt is fairly complex and may have different effects on tumor cell survival and growth depending on the genetic background of the cell (such as EGFR amplification, etc.), glucose and oxygen availability, therapy, and other environmental stimuli (Chautard et al. 2010; Elstrom et al. 2004; Eyler et al. 2008; Fan and Weiss 2010; Gallia et al. 2009; Li et al. 2009; Los et al. 2009; Marsh et al. 2008; Rao et al. 2005; Robey and Hay 2009; Vadlakonda et al. 2013). A complete discussion of the role of Akt, HIF-1, and other genes in tumor growth and metabolism is outside the scope of this chapter, but readers are referred to the cited review papers.
6 Reactive Oxygen Species
While the mechanisms underlying the anticancer effects of the KD are not completely understood, the literature regarding the KD in epilepsy has provided some insight. A number of these studies have involved the putative role of changes in the level of reactive oxygen species (ROS) and seizure control. ROS are involved in a variety of cellular processes including autophagic/apoptotic responses to genotoxic stress, pathways involved in the regulation of inflammation, response to hypoxia, and nutrient deprivation—to name a few. Rho and colleagues have shown that ROS production in the brain is reduced in animals fed a ketogenic diet (Kim and Rho 2008; Maalouf et al. 2007). Cancer cells often have increased levels of ROS resulting from a variety of intrinsic and external sources including mitochondrial alterations (Liang and Grootveld 2011), aberrant expression of components of cellular antioxidant systems, chronic inflammation, tobacco, viruses, and environmental pollutants to name just a few (Gupta et al. 2012; Weinberg and Chandel 2009; Fruehauf and Meyskens 2007). They regulate vascular endothelial growth factor (VEGF) and HIF-1 (Weinberg and Chandel 2009) and thus have been implicated in angiogenesis and tumor growth. We have demonstrated a reduction in ROS in tumors from mice fed a KD and changes in the expression of genes involved in oxidative stress pathways (Stafford et al. 2010). Amigo and Kowaltowski (2014) described a similar effect using CR. While the specific downstream effects of this have not yet been fully elucidated, alterations in tumor ROS levels are sure to have profound effects on tumor growth.
7 Anti-angiogenic Effects
One major hallmark of brain tumors is the rapid stimulation of blood vessels that supply the nutrients needed to sustain rapid cellular growth. This vessel growth is favored by the uncontrolled production of angiogenic stimulators and the absence of inhibitors. Vascular endothelial growth factor (VEGF) is considered a driving factor in angiogenesis and has thus become a prime target for anti-angiogenic therapy (El-Kenawi and El-Remessy 2013). To this end, the FDA approved bevacizumab, a monoclonal antibody targeting VEGF, for use in GBMs. While this drug may help to reduce edema, especially following radiation, it often results in adverse effects and it affords little if any improvement in overall survival (Field et al. 2014; Patel et al. 2012).
Studies as far back as 1914 have suggested that restricted food intake can target tumor blood supply and reduce tumor growth (Rous 1914). More recently, it has been suggested that caloric restriction (CR), which also reduces blood glucose and raises blood ketones, reduces growth and angiogenic biomarker expression in prostate cancer and breast cancer (De Lorenzo et al. 2011; Mukherjee et al. 1999; Phoenix et al. 2010; Thompson et al. 2004). Seyfried and colleagues recently showed that CR promoted vessel maturation by preventing vascular VEGF signaling in the CT-2A mouse astrocytoma model (Urits et al. 2012), and they have demonstrated reduced angiogenesis in a number of other mouse glioma models using caloric restriction (Mukherjee et al. 2002, 2004; Seyfried et al. 2011; Shelton et al. 2010; Zhou et al. 2007). Further, CR was shown to normalize a number of factors involved in tumor vessel instability and weakness (including VEGF) as well as reducing peritumoral edema in a mouse model using human U87 glioma cells (Jiang and Wang 2013). In the GL261 mouse glioma model, we found that when fed ad libitum the KD decreased tumor vasculature, reduced peritumoral edema, and altered the expression of genes involved in angiogenesis (Woolf et al. 2015), despite the fact that the expression of VEGF was unchanged (Scheck et al. 2012). Taken together, these results suggest that another effect of metabolic therapy may be to target angiogenesis activity, thus mimicking the beneficial effects of bevacizumab.
8 Anti-inflammatory Effects
The blood vessels formed by rapid angiogenesis in gliomas are often leaky, leading to peritumoral inflammation and edema. Inflammation can also be increased by treatment such as radiation therapy. Inflammation and edema can promote tumor growth, and reduce patient quality of life due to increased pressure-related symptoms and side effects of the high-dose steroids often used for treatment. We have shown that increasing blood ketones affects a number of tumor-related gene networks and alters the expression of genes involved in the cellular response to oxidative stress in tumor tissue, notably cyclooxygenase 2 (COX-2), an important mediator of inflammation (Stafford et al. 2010). A separate study using the KD in combination with radiation therapy in the same mouse model demonstrated reduced expression of both COX-2 and Nf-κB while reducing the production of ROS (Woolf et al. 2013). Similar results have demonstrated reduced expression of pro-inflammatory markers, cyclooxygenase-2 (COX-2), nuclear factor kappa B (NF-κB), and macrophage inflammatory protein (MIP-2) using caloric restriction in mouse models of astrocytoma (Mulrooney et al. 2011) and colon cancer (Harvey et al. 2013).
9 KD as an Adjuvant Therapy
Although evidence suggests that the KD provides antitumor benefits on its own, perhaps the most effective use of the KD is in combination with standard cancer therapies such as radiation and chemotherapy. The KD greatly enhanced survival in a mouse model of malignant glioma when combined with TMZ when compared to either treatment alone (Scheck et al. 2011). In addition, a separate study showed that 9 out of 11 animals maintained on the KD and treated with radiation had complete and sustained remission of their implanted tumors, even after being switched back to a standard rodent diet (Fig. 3) (Abdelwahab et al. 2012). Allen et al. reported similar results when the KD is combined with radiation and chemotherapy in a lung cancer xenograft model (Allen et al. 2013). That is, they found decreased tumor growth rate and increased survival. CR and short-term fasting have also been found to be synergistic with radiation and other anticancer therapeutics in both preclinical and clinical studies (Champ et al. 2013, 2014; Klement and Champ 2014; Lee et al. 2010, 2012; Poff et al. 2013; Raffaghello et al. 2008, 2010; Safdie et al. 2012; Saleh et al. 2013; Seyfried et al. 2012).
Radiation in combination with the ketogenic diet causes tumor regression. On days 3 and 5 postimplantation animals received 4 Gy of radiation. The tumor completely regressed in 9 of the 11 animals fed a ketogenic diet. Animals were switched back to standard diet on day 101 and maintained for an additional 200 days and no tumor regrowth was detected. (a) Kaplan–Meier survival plot; (b) bioluminescence in representative animals treated with radiation and fed a standard diet vs. radiation plus the ketogenic diet; (c) bioluminescent signal plotted as in vivo photon count versus days postimplantation. Reprinted from (Abdelwahab et al. 2012)
The effectiveness of radiation therapy is due to a number of factors including relative damage done to tumor cells versus normal tissue and the ability of normal cells and tumor cells to repair the damage (Klement and Champ 2014). Radiation works, in part, by creating ROS through the radiolysis of water. The ROS damage the DNA and other macromolecules, causing sublethal damage that can become lethal if not repaired. The potentiation of radiation therapy by the KD or caloric restriction seems paradoxical in light of our data demonstrating a reduction in ROS in tumors from animals maintained on a KD (Stafford et al. 2010). However, radiation effects do not only occur through ROS, and radiation can directly damage DNA and other cellular macromolecules. Furthermore, in addition to reactive oxygen species, radiation causes the production of reactive nitrogen species (RNS), a potential source of macromolecular damage following radiation (Saenko et al. 2013). Whether the KD and/or caloric restriction reduces the formation of RNS is as yet unknown. In fact, the main effect of the KD or CR may not be in altering the amount of radiation-induced damage, but may in fact be in modulating the ability of tumor and normal cells to repair radiation-induced damage (Klement and Champ 2014; Santivasi and Xia 2014). Studies have shown that caloric restriction can enhance DNA repair in normal cells (Heydari et al. 2007); however, this may not be the case in tumor cells, and the differential response of tumor cells and normal cells to genotoxic stress may be mediated by reduced IGF1 and glucose in the tumor cells. In fact, a number of studies have shown that reduction of activation of the PI3K/Akt pathway, activation of the adenosine monophosphate-activated protein kinase (AMPK) signaling pathway, and reduction of receptor tyrosine kinase growth factor pathways can all reduce radioresistance in tumor cells (Choi et al. 2014; Danhier et al. 2013; Gil Del Alcazar et al. 2014; Li et al. 2014; Medova et al. 2013; Munshi and Ramesh 2013; Sanli et al. 2014; Wang et al. 2013; Zhang et al. 2014). These reports provide additional support for the use of the KD or caloric restriction as an adjuvant therapy for the treatment of gliomas.
10 Neuroprotection
There is a resurgence of interest in the use of the KD for the treatment of medically refractory epilepsy and increasing interest in the use of this therapy for the treatment of malignant brain tumors. While the majority of the research in this field focuses on slowing tumor growth and enhancing the efficacy of current therapeutic modalities, the KD may have additional benefits for cancer patients. Evidence suggests that the ketogenic diet may also protect normal brain tissue from the genotoxic stress that is a typical “side effect” of radiation and chemotherapy. We have demonstrated that gene expression changes in the tumor tissue from animals fed the KD were not the same as those in the non-tumor containing contralateral side of the brain (Scheck et al. 2012; Stafford et al. 2010). This allows for the hypothesis that while the neuroprotective activity of the KD does not protect the tumor from the therapeutic benefits of radiation and chemotherapy, it may reduce the deleterious side effects of cranial radiation on normal brain. A recent publication showed that fasting, which elevates blood ketones, not only sensitizes many types of cancer cells to standard therapies but may promote the protection of normal tissue from the toxicity associated with radiation and chemotherapy (Lee et al. 2012). Additional studies are needed to support this hypothesis; however, the potential benefit of protecting the normal brain from decreased cognitive function due to radiation toxicity would be of great importance, particularly for the treatment of pediatric brain tumors.
11 KD in Other Cancers
Although much of the research regarding the anticancer benefits of the KD has focused on brain tumors, this type of metabolic therapy has also recently been explored in other cancer types. For example, Gluschnaider et al. used the MMTV-PyMT oncomouse model to demonstrate that a KD suppressed breast tumor growth (Gluschnaider et al. 2014). Likewise, Allen et al. showed that the KD enhanced radiation and chemotherapy responses in a mouse lung xenograft model by increasing oxidative stress in both NCI-H292 and A549 lung xenograft models (Allen et al. 2013). The use of a no carbohydrate ketogenic diet (NCKD) in prostate cancer models has also been examined. A recent study demonstrated that an NCKD significantly slowed tumor growth and prolonged survival in a prostate cancer xenograft model (Freedland et al. 2008). Studies in prostate cancer xenograft models demonstrated that the NCKD significantly reduces tumor volume (Kim et al. 2012) and alters pathways linked to apoptosis, inflammation, and insulin resistance (Mavropoulos et al. 2009). A KD supplemented with omega-3 fatty acids and medium chain triglycerides was shown to delay tumor growth in a mouse xenograft model of gastric cancer. The use of the KD in models of cancer-associated cachexia has also been studied. Shukla et al. showed that a KD reduced glycolytic flux and glutamine uptake in a number of pancreatic cell lines. They identified decreased pancreatic cancer cell growth as well as a dose-dependent induction of apoptosis in the presence of ketone bodies in vitro. Likewise, in the presence of ketones, pancreatic cancer cells had a reduced expression and activity of the oncogene c-Myc and reduced cachexic markers. They also showed a reduction of tumor growth and cachexia in an animal model of pancreatic cancer (Shukla et al. 2014).
Although the mechanisms behind the KD have not been completely identified and extend beyond the reduction in blood glucose and increase in blood ketones, recent studies in cancer research suggest that the KD may provide therapeutic benefits in a variety of cancer types. This demonstrates that more research is warranted to better understand the mechanisms behind the KD as well as the different physiological responses which occur based upon cancer type and location.
12 KD in Humans
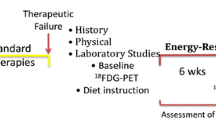
Studies of glucose utilization in cancer go back prior to the 1980s, including studies of metabolism and cancer cachexia (Fearon et al. 1988; Tisdale et al. 1987). These and other studies suggested that the ketogenic diet consisting of a high percentage of medium chain triglycerides (MCT) along with various supplements resulted in weight gain and improved nitrogen balance in both animals and humans. In 1995, Nebeling and colleagues published a case report in which they used a similar ketogenic diet based on MCT oil to treat 2 female pediatric patients with advanced stage malignant brain tumors (Nebeling et al. 1995; Nebeling and Lerner 1995). They demonstrated that dietary-induced ketosis decreased the availability of glucose to the tumor without causing a decrease in patient weight for overall nutritional status. Furthermore, both children had long-term tumor management (Nebeling et al. 1995). The 2nd case report was published in 2010 by Zuccoli and coworkers (2010). This patient was a 65-year-old female with multicentric glioblastoma. She was put on a 4:1 (ratio of fats:carbohydrate plus protein) calorie restricted (600 kcal/day) ketogenic diet during radiation and chemotherapy. During this time her body weight dropped by 20 %, she had reduced blood glucose, increased urinary ketones, and, most importantly, no observable brain tumor by either fluorodeoxyglucose Positron Emission Tomography (FDG-PET) or magnetic resonance imaging (MRI). The tumor recurred 10 weeks after the patient resumed her normal eating habits and she succumbed to her disease less than 2 years after diagnosis. While this patient did not experience long-term tumor control after cessation of the diet, this report demonstrated that the diet could be tolerated, even when used in a calorie-restricted setting. Results of a phase 1 clinical trial were reported in 2011 by a German group. Tolerability of a restricted calorie ketogenic diet was tested in 16 patients with a variety of advanced (end-stage) cancers. There were no severe side effects and 5 of the 16 patients were able to complete the 3-month treatment. These 5 patients had stable disease while on the diet. Two of the 11 remaining patients died early following the beginning of the trial, one was unable to tolerate the diet and dropped out immediately, 2 patients dropped out for personal reasons, one was unable to continue the diet for more than a month, and 3 had disease progression within less than 2 months of starting the diet and one dropped out to resume chemotherapy. While this trail demonstrated tolerability and favorable side-effect profile, the antitumor efficacy could not be assessed due to the variety and severity of disease in the patients. More recently, a number of prospective clinical trials have been initiated. A study in Germany is evaluating the efficacy of a calorie-restricted ketogenic diet and transient fasting during re-irradiation for patients with recurrent GBM (ClinicalTrials.gov NCT01754350). Michigan State University is directing a similar trial evaluating a calorie-restricted KD for recurrent GBM (ClinicalTrials.gov NCT01535911). A third clinical trial is evaluating the KD as adjunctive treatment in refractory/end-stage GBM (ClinicalTrials.gov NCT01865162). The goals for all of these studies are to obtain data on the safety, efficacy, and tolerability of the KD as an adjunctive therapy for patients with GBM. The only study using the KD as an up-front, concurrent therapy has recently been approved and is now open for enrollment at St. Joseph’s Hospital and Medical Center and Barrow Neurological Institute in Phoenix, Arizona (ClinicalTrials.gov NCT02046187). This trial for patients with primary GBM will evaluate the classic 4:1 ketogenic diet therapy during radiation treatment and concurrent temozolomide followed by the modified Atkins Diet (1:1 fat:carbohydrate plus protein) during temozolomide treatment.
The case reports described above along with numerous anecdotal reports suggest that the KD may be a promising anticancer therapy; however, more work is needed to determine how to best utilize this and other metabolic therapies for the treatment of tumors. Most of the information regarding the best way to use the ketogenic diet comes from the epilepsy literature. Further research is needed to determine optimum blood ketone and glucose levels for anticancer effects. In addition, a variety of ketogenic diets are used for seizure control and it is not clear if one or more of the different formulations will provide the best results for cancer patients. Finally, while the KD has a long record of safety in the epilepsy community, side effects that occur when used in combination with cancer therapies may differ in type or severity. This data will come from carefully controlled clinical trials that include input from registered dietitians well-versed in the use of the KD. Patient enrollment into clinical trials requires “buy-in” from the medical community. Physicians must be educated on the therapeutic value of metabolic alteration as an adjuvant therapy, even if it results in a small amount of healthy weight loss, since the current dogma is to avoid weight loss in patients undergoing chemotherapy for fear of increased fatigue and further decline in overall patient health. As with any decision regarding therapy, the patient’s overall condition, including nutritional status, must be taken into account.
Concern about patients’ quality of life is sometimes given as a reason not to employ KD. Compliance can be made more difficult by the use of steroids (prescribed for peritumoral edema) that often increase hunger and raise blood glucose levels. To address this, our clinical trial includes an analysis of both patient and caregiver quality of life. Quality of life measurements are being added to more clinical trials, as the importance of this has become recognized at the national level (Boele et al. 2013; Dirven et al. 2014; van den Bent et al. 2011). While some clinicians are concerned that compliance will reduce quality of life, the patients that do remain on the KD often comment that this allows them to participate in their own therapy. Despite these caveats, the existing preclinical data suggesting antitumor efficacy and a synergistic effect with standard therapies provide a strong impetus to conduct controlled clinical trials, particularly those that will shed light on the interactions between the KD and other therapies.
13 Conclusion
Improvements in the survival and quality of life for patients with malignant brain tumors require the implementation of new therapeutic modalities, especially those that increase the efficacy of current therapies without increasing toxic side effects. While the rapid accumulation of data defining the molecular and genetic aberrations present in these tumors has suggested a host of targets for the development of new therapies, targeted therapies tried to date have met with limited success. This is at least in part due to the molecular heterogeneity of these tumors that prevents any one target from being present on all cells. In contrast, metabolic dysregulation is present in virtually all tumor cells and there is increased interest in using metabolic therapies such as the ketogenic diet for the treatment of various cancers, especially brain tumors. Preclinical data have demonstrated that the antitumor effects of the KD and caloric restriction are multifaceted, and alterations in energy metabolism can inhibit cancer cell growth and increase the tumor’s response to therapy. This provides a strong impetus to continue work designed to elucidate the mechanisms through which the KD exerts its anticancer effects, as well as suggesting the need for the design of controlled clinical trials that will shed light on the most effective way to implement metabolic therapies in combination with standard therapies for the treatment of malignant disease. This is a novel therapeutic paradigm, and we have only begun to scratch the surface of its potential.
References
Abdelwahab MG, Fenton KE, Preul MC, Rho JM, Lynch A, Stafford P, Scheck AC (2012) The ketogenic diet is an effective adjuvant to radiation therapy for the treatment of malignant glioma. PLoS One 7(5), e36197
Allen BG, Bhatia SK, Buatti JM, Brandt KE, Lindholm KE, Button AM, Szweda LI, Smith B, Spitz DR, Fath MA (2013) Ketogenic diets enhance oxidative stress and radio-chemo-therapy responses in lung cancer xenografts. Clin Cancer Res 19(14):3905–3913
Amigo I, Kowaltowski AJ (2014) Dietary restriction in cerebral bioenergetics and redox state. Redox Biol 2:296–304
Anton K, Baehring JM, Mayer T (2012) Glioblastoma multiforme: overview of current treatment and future perspectives. Hematol Oncol Clin North Am 26(4):825–853
Arcaro A (2013) Targeting the insulin-like growth factor-1 receptor in human cancer. Front Pharmacol 4:30
Azad N, Zahnow CA, Rudin CM, Baylin SB (2013) The future of epigenetic therapy in solid tumours--lessons from the past. Nat Rev Clin Oncol 10(5):256–266
Baylin SB, Jones PA (2011) A decade of exploring the cancer epigenome—biological and translational implications. Nat Rev Cancer 11(10):726–734
Bloch O, Han SJ, Cha S, Sun MZ, Aghi MK, McDermott MW, Berger MS, Parsa AT (2012) Impact of extent of resection for recurrent glioblastoma on overall survival: clinical article. J Neurosurg 117(6):1032–1038
Boele FW, Heimans JJ, Aaronson NK, Taphoorn MJ, Postma TJ, Reijneveld JC, Klein M (2013) Health-related quality of life of significant others of patients with malignant CNS versus non-CNS tumors: a comparative study. J Neurooncol 115(1):87–94
Brennan C (2011) Genomic profiles of glioma. Curr Neurol Neurosci Rep 11(3):291–297
Brennan C, Momota H, Hambardzumyan D, Ozawa T, Tandon A, Pedraza A, Holland E (2009) Glioblastoma subclasses can be defined by activity among signal transduction pathways and associated genomic alterations. PLoS One 4(11), e7752
Cahill GF Jr, Veech RL (2003) Ketoacids? Good medicine? Trans Am Clin Climatol Assoc 114:149–161
Cantor JR, Sabatini DM (2012) Cancer cell metabolism: one hallmark, many faces. Cancer Discov 2(10):881–898
Champ CE, Baserga R, Mishra MV, Jin L, Sotgia F, Lisanti MP, Pestell RG, Dicker AP, Simone NL (2013) Nutrient restriction and radiation therapy for cancer treatment: when less is more. Oncologist 18(1):97–103
Champ CE, Palmer JD, Volek JS, Werner-Wasik M, Andrews DW, Evans JJ, Glass J, Kim L, Shi W (2014) Targeting metabolism with a ketogenic diet during the treatment of glioblastoma multiforme. J Neurooncol 117(1):125–131
Chautard E, Loubeau G, Tchirkov A, Chassagne J, Vermot-Desroches C, Morel L, Verrelle P (2010) Akt signaling pathway: a target for radiosensitizing human malignant glioma. Neuro Oncol 12(5):434–443
Choi EJ, Cho BJ, Lee DJ, Hwang YH, Chun SH, Kim HH, Kim IA (2014) Enhanced cytotoxic effect of radiation and temozolomide in malignant glioma cells: targeting PI3K-AKT-mTOR signaling, HSP90 and histone deacetylases. BMC Cancer 14:17
Cross JH (2013) New research with diets and epilepsy. J Child Neurol 28(8):970–974
Danhier P, De Saedeleer CJ, Karroum O, De PG, Porporato PE, Jordan BF, Gallez B, Sonveaux P (2013) Optimization of tumor radiotherapy with modulators of cell metabolism: toward clinical applications. Semin Radiat Oncol 23(4):262–272
De Lorenzo MS, Baljinnyam E, Vatner DE, Abarzua P, Vatner SF, Rabson AB (2011) Caloric restriction reduces growth of mammary tumors and metastases. Carcinogenesis 32(9):1381–1387
Dirven L, Taphoorn MJ, Reijneveld JC, Blazeby J, Jacobs M, Pusic A, La SE, Stupp R, Fayers P, Efficace F (2014) The level of patient-reported outcome reporting in randomised controlled trials of brain tumour patients: a systematic review. Eur J Cancer 50(14):2432–2448
El-Kenawi AE, El-Remessy AB (2013) Angiogenesis Inhibitors in Cancer Therapy: Mechanistic perspective on classification and treatment rationales. Br. J, Pharmacol
Elstrom RL, Bauer DE, Buzzai M, Karnauskas R, Harris MH, Plas DR, Zhuang H, Cinalli RM, Alavi A, Rudin CM, Thompson CB (2004) Akt stimulates aerobic glycolysis in cancer cells. Cancer Res 64(11):3892–3899
Eyler CE, Foo WC, LaFiura KM, McLendon RE, Hjelmeland AB, Rich JN (2008) Brain cancer stem cells display preferential sensitivity to Akt inhibition. Stem Cells 26(12):3027–3036
Fan QW, Weiss WA (2010) Targeting the RTK-PI3K-mTOR axis in malignant glioma: overcoming resistance. Curr Top Microbiol Immunol 347(279-96):279–296
Fearon KC, Borland W, Preston T, Tisdale MJ, Shenkin A, Calman KC (1988) Cancer cachexia: influence of systemic ketosis on substrate levels and nitrogen metabolism. Am J Clin Nutr 47(1):42–48
Field KM, Jordan JT, Wen PY, Rosenthal MA, Reardon DA (2014) Bevacizumab and glioblastoma: Scientific review, newly reported updates, and ongoing controversies. Cancer 10
Fredericks M, Ramsey RB (1978) 3-Oxo acid coenzyme A transferase activity in brain and tumors of the nervous system. J Neurochem 31(6):1529–1531
Freedland SJ, Mavropoulos J, Wang A, Darshan M, Demark-Wahnefried W, Aronson WJ, Cohen P, Hwang D, Peterson B, Fields T, Pizzo SV, Isaacs WB (2008) Carbohydrate restriction, prostate cancer growth, and the insulin-like growth factor axis. Prostate 68(1):11–19
Fruehauf JP, Meyskens FL Jr (2007) Reactive oxygen species: a breath of life or death? Clin Cancer Res 13(3):789–794
Gallia GL, Tyler BM, Hann CL, Siu IM, Giranda VL, Vescovi AL, Brem H, Riggins GJ (2009) Inhibition of Akt inhibits growth of glioblastoma and glioblastoma stem-like cells. Mol Cancer Ther 8(2):386–393
Gatenby RA, Gillies RJ (2004) Why do cancers have high aerobic glycolysis? Nat Rev Cancer 4:891–899
Gil Del Alcazar CR, Hardebeck MC, Mukherjee B, Tomimatsu N, Gao X, Yan J, Xie XJ, Bachoo R, Li L, Habib AA, Burma S (2014) Inhibition of DNA Double-Strand Break Repair by the Dual PI3K/mTOR Inhibitor NVP-BEZ235 as a Strategy for Radiosensitization of Glioblastoma. Clin, Cancer Res
Gill BJ, Pisapia DJ, Malone HR, Goldstein H, Lei L, Sonabend A, Yun J, Samanamud J, Sims JS, Banu M, Dovas A, Teich AF, Sheth SA, McKhann GM, Sisti MB, Bruce JN, Sims PA, Canoll P (2014) MRI-localized biopsies reveal subtype-specific differences in molecular and cellular composition at the margins of glioblastoma. Proc Natl Acad Sci U S A 111(34):12550–12555
Gluschnaider U, Hertz R, Ohayon S, Smeir E, Smets M, Pikarsky E, Bar-Tana J (2014) Long-chain Fatty Acid analogues suppress breast tumorigenesis and progression. Cancer Res 74(23):6991–7002
Group TCGAR (2008) Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455(7216):1061–1068
Gupta SC, Hevia D, Patchva S, Park B, Koh W, Aggarwal BB (2012) Upsides and downsides of reactive oxygen species for cancer: The roles of reactive oxygen species in tumorigenesis, prevention and therapy. Antioxid Redox Signal 16(11):1295–1322
Haisa M (2013) The type 1 insulin-like growth factor receptor signalling system and targeted tyrosine kinase inhibition in cancer. J Int Med Res 41(2):253–264
Harvey AE, Lashinger LM, Otto G, Nunez NP, Hursting SD (2013) Decreased systemic IGF-1 in response to calorie restriction modulates murine tumor cell growth, nuclear factor-kappaB activation, and inflammation-related gene expression. Mol Carcinog 52(12):997–1006
Heydari AR, Unnikrishnan A, Lucente LV, Richardson A (2007) Caloric restriction and genomic stability. Nucleic Acids Res 35(22):7485–7496
Hummel TR, Chow LM, Fouladi M, Franz D (2013) Pharmacotherapeutic management of pediatric gliomas : current and upcoming strategies. Paediatr Drugs 15(1):29–42
Jiang YS, Wang FR (2013) Caloric restriction reduces edema and prolongs survival in a mouse glioma model. J Neurooncol 114(1):25–32
Kim DY, Rho JM (2008) The ketogenic diet and epilepsy. Curr Opin Clin Nutr Metab Care 11(2):113–120
Kim HS, Masko EM, Poulton SL, Kennedy KM, Pizzo SV, Dewhirst MW, Freedland SJ (2012) Carbohydrate restriction and lactate transporter inhibition in a mouse xenograft model of human prostate cancer. BJU Int 110(7):1062–1069
Klement RJ, Champ CE (2014) Calories, carbohydrates, and cancer therapy with radiation: exploiting the five R's through dietary manipulation. Cancer Metastasis Rev 33(1):217–29
Kobow K, Kaspi A, Harikrishnan KN, Kiese K, Ziemann M, Khurana I, Fritzsche I, Hauke J, Hahnen E, Coras R, Muhlebner A, El-Osta A, Blumcke I (2013) Deep sequencing reveals increased DNA methylation in chronic rat epilepsy. Acta Neuropathol 126(5):741–756
Lee Y, Scheck AC, Cloughesy TF, Lai A, Dong J, Farooqi HK, Liau LM, Horvath S, Mischel PS, Nelson SF (2008) Gene expression analysis of glioblastomas identifies the major molecular basis for the prognostic benefit of younger age. BMC Med Genomics 1:52
Lee C, Safdie FM, Raffaghello L, Wei M, Madia F, Parrella E, Hwang D, Cohen P, Bianchi G, Longo VD (2010) Reduced levels of IGF-I mediate differential protection of normal and cancer cells in response to fasting and improve chemotherapeutic index. Cancer Res 70(4):1564–1572
Lee C, Raffaghello L, Brandhorst S, Safdie FM, Bianchi G, Martin-Montalvo A, Pistoia V, Wei M, Hwang S, Merlino A, Emionite L, de Cabo R, Longo VD (2012) Fasting cycles retard growth of tumors and sensitize a range of cancer cell types to chemotherapy. Sci Transl Med 4(124):124ra27
Li HF, Kim JS, Waldman T (2009) Radiation-induced Akt activation modulates radioresistance in human glioblastoma cells. Radiat Oncol 4:43
Li W, Guo F, Wang P, Hong S, Zhang C (2014) miR-221/222 confers radioresistance in glioblastoma cells through activating Akt independent of PTEN status. Curr Mol Med 14(1):185–195
Liang BC, Grootveld M (2011) The importance of mitochondria in the tumourigenic phenotype: gliomas as the paradigm (review). Int J Mol Med 27(2):159–171
Los M, Maddika S, Erb B, Schulze-Osthoff K (2009) Switching Akt: from survival signaling to deadly response. Bioessays 31(5):492–495
Maalouf M, Sullivan PG, Davis L, Kim DY, Rho JM (2007) Ketones inhibit mitochondrial production of reactive oxygen species production following glutamate excitotoxicity by increasing NADH oxidation. Neuroscience 145(1):256–264
Maalouf M, Rho JM, Mattson MP (2009) The neuroprotective properties of calorie restriction, the ketogenic diet, and ketone bodies. Brain Res Rev 59(2):293–315
Magee BA, Potezny N, Rofe AM, Conyers RA (1979) The inhibition of malignant cell growth by ketone bodies. Aust J Exp Biol Med Sci 57(5):529–539
Marie SK, Shinjo SM (2011) Metabolism and brain cancer. Clinics (SaoPaulo) 66(Suppl 1):33–43
Marsh J, Mukherjee P, Seyfried TN (2008) Akt-dependent proapoptotic effects of dietary restriction on late-stage management of a phosphatase and tensin homologue/tuberous sclerosis complex 2-deficient mouse astrocytoma. Clin Cancer Res 14(23):7751–7762
Masui K, Cloughesy TF, Mischel PS (2012) Review: molecular pathology in adult high-grade gliomas: from molecular diagnostics to target therapies. Neuropathol Appl Neurobiol 38(3):271–291
Maurer GD, Brucker DP, Bahr O, Harter PN, Hattingen E, Walenta S, Mueller-Klieser W, Steinbach JP, Rieger J (2011) Differential utilization of ketone bodies by neurons and glioma cell lines: a rationale for ketogenic diet as experimental glioma therapy. BMC Cancer 11(315):315
Mavropoulos JC, Buschemeyer WC III, Tewari AK, Rokhfeld D, Pollak M, Zhao Y, Febbo PG, Cohen P, Hwang D, Devi G, Demark-Wahnefried W, Westman EC, Peterson BL, Pizzo SV, Freedland SJ (2009) The effects of varying dietary carbohydrate and fat content on survival in a murine LNCaP prostate cancer xenograft model. Cancer Prev Res (Phila) 2(6):557–565
Medova M, Aebersold DM, Zimmer Y (2013) The molecular crosstalk between the MET receptor tyrosine kinase and the DNA damage response-biological and clinical aspects. Cancers(Basel) 6(1):1–27
Morris AAM (2005) Cerebral ketone body metabolism. J Inherit Metab Dis 28:109–121
Mukherjee P, Sotnikov AV, Mangian HJ, Zhou JR, Visek WJ, Clinton SK (1999) Energy intake and prostate tumor growth, angiogenesis, and vascular endothelial growth factor expression. J Natl Cancer Inst 91(6):512–523
Mukherjee P, El-Abbadi MM, Kasperzyk JL, Ranes MK, Seyfried TN (2002) Dietary restriction reduces angiogenesis and growth in an orthotopic mouse brain tumour model. Br J Cancer 86(10):1615–1621
Mukherjee P, Abate LE, Seyfried TN (2004) Antiangiogenic and proapoptotic effects of dietary restriction on experimental mouse and human brain tumors. Clin Cancer Res 10(16):5622–5629
Mulrooney TJ, Marsh J, Urits I, Seyfried TN, Mukherjee P (2011) Influence of caloric restriction on constitutive expression of NF-kappaB in an experimental mouse astrocytoma. PLoS One 6(3), e18085
Munshi A, Ramesh R (2013) Mitogen-Activated Protein Kinases and Their Role in Radiation Response. Genes Cancer 4(9-10):401–408
Nebeling LC, Lerner E (1995) Implementing a ketogenic diet based on medium-chain triglyceride oil in pediatric patients with cancer. J Am Diet Assoc 95(6):693–697
Nebeling LC, Miraldi F, Shurin SB, Lerner E (1995) Effects of a ketogenic diet on tumor metabolism and nutritional status in pediatric oncology patients: two case reports. J Am Coll Nutr 14(2):202–208
Negi A, Ramarao P, Kumar R (2013) Recent advancements in small molecule inhibitors of insulin-like growth factor-1 receptor (IGF-1R) tyrosine kinase as anticancer agents. Mini Rev Med Chem 13(5):653–681
Nijsten MW, van Dam GM (2009) Hypothesis: using the Warburg effect against cancer by reducing glucose and providing lactate. Med Hypotheses 73(1):48–51
Obre E, Rossignol R (2015) Emerging concepts in bioenergetics and cancer research: Metabolic flexibility, coupling, symbiosis, switch, oxidative tumors, metabolic remodeling, signaling and bioenergetic therapy. Int J Biochem Cell Biol 59C:167–181. doi:10.1016/j.biocel.2014.12.008
Patel M, Vogelbaum MA, Barnett GH, Jalali R, Ahluwalia MS (2012) Molecular targeted therapy in recurrent glioblastoma: current challenges and future directions. Expert. Opin. Investig, Drugs
Patel AP, Tirosh I, Trombetta JJ, Shalek AK, Gillespie SM, Wakimoto H, Cahill DP, Nahed BV, Curry WT, Martuza RL, Louis DN, Rozenblatt-Rosen O, Suva ML, Regev A, Bernstein BE (2014) Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science 344(6190):1396–1401
Phoenix KN, Vumbaca F, Fox MM, Evans R, Claffey KP (2010) Dietary energy availability affects primary and metastatic breast cancer and metformin efficacy. Breast Cancer Res Treat 123(2):333–344
Poff AM, Ari C, Seyfried TN, D'Agostino DP (2013) The ketogenic diet and hyperbaric oxygen therapy prolong survival in mice with systemic metastatic cancer. PLoS One 8(6), e65522
Puzio-Kuter AM (2011) The role of p53 in metabolic regulation. Genes Cancer 2(4):385–391
Qureshi IA, Mehler MF (2013) Developing epigenetic diagnostics and therapeutics for brain disorders. Trends Mol Med 19(12):732–741
Raffaghello L, Lee C, Safdie FM, Wei M, Madia F, Bianchi G, Longo VD (2008) Starvation-dependent differential stress resistance protects normal but not cancer cells against high-dose chemotherapy. Proc Natl Acad Sci U S A 105(24):8215–8220
Raffaghello L, Safdie F, Bianchi G, Dorff T, Fontana L, Longo VD (2010) Fasting and differential chemotherapy protection in patients. Cell Cycle 9(22):4474–4476
Rao RD, Mladek AC, Lamont JD, Goble JM, Erlichman C, James CD, Sarkaria JN (2005) Disruption of parallel and converging signaling pathways contributes to the synergistic antitumor effects of simultaneous mTOR and EGFR inhibition in GBM cells. Neoplasia 7(10):921–929
Robey RB, Hay N (2009) Is Akt the “Warburg kinase”?-Akt-energy metabolism interactions and oncogenesis. Semin Cancer Biol 19(1):25–31
Rous P (1914) The influence of diet on transplanted and spontaneous mouse tumors. J Exp Med 20(5):433–451
Saenko Y, Cieslar-Pobuda A, Skonieczna M, Rzeszowska-Wolny J (2013) Changes of reactive oxygen and nitrogen species and mitochondrial functioning in human K562 and HL60 cells exposed to ionizing radiation. Radiat Res 180(4):360–366
Safdie F, Brandhorst S, Wei M, Wang W, Lee C, Hwang S, Conti PS, Chen TC, Longo VD (2012) Fasting enhances the response of glioma to chemo- and radiotherapy. PLoS One 7(9), e44603
Saleh AD, Simone BA, Palazzo J, Savage JE, Sano Y, Dan T, Jin L, Champ CE, Zhao S, Lim M, Sotgia F, Camphausen K, Pestell RG, Mitchell JB, Lisanti MP, Simone NL (2013) Caloric restriction augments radiation efficacy in breast cancer. Cell Cycle 12(12):1955–1963
Sanli T, Steinberg GR, Singh G, Tsakiridis T (2014) AMP-activated protein kinase (AMPK) beyond metabolism: a novel genomic stress sensor participating in the DNA damage response pathway. Cancer Biol Ther 15(2):156–169
Santivasi WL, Xia F (2014) 2014. Ionizing radiation-induced DNA damage, response, and repair. Antioxid Redox Signal 21(2):251–9
Scheck AC, Abdelwahab MG, Stafford P, Kim DY, Iwai S, Preul MC, Rho JM (2011) Mechanistic studies of the ketogenic diet as an adjuvant therapy for malignant gliomas. Cancer Res 70(8 Suppl):638, Ref Type: Abstract
Scheck AC, Abdelwahab MG, Fenton K, Stafford P (2012) The ketogenic diet for the treatment of glioma: Insights from genetic profiling. Epilepsy Res 100:327–337
Semenza GL (2013) HIF-1 mediates metabolic responses to intratumoral hypoxia and oncogenic mutations. J Clin Invest 123(9):3664–3671
Seyfried TN (2012) Cancer as a metabolic disease: on the origin, management and prevention of cancer. John Wiley and Sons Inc, Hoboken, NJ
Seyfried TN, Mukherjee P (2005) Targeting energy metabolism in brain cancer: review and hypothesis. Nutr Metab 2:30–38
Seyfried TN, Sanderson TM, El-Abbadi MM, McGowan R, Mukherjee P (2003) Role of glucose and ketone bodies in the metabolic control of experimental brain cancer. Br J Cancer 89(7):1375–1382
Seyfried TN, Kiebish MA, Marsh J, Shelton LM, Huysentruyt LC, Mukherjee P (2011) Metabolic management of brain cancer. Biochim Biophys Acta 1807(6):577–594
Seyfried TN, Marsh J, Shelton LM, Huysentruyt LC, Mukherjee P (2012) Is the restricted ketogenic diet a viable alternative to the standard of care for managing malignant brain cancer? Epilepsy Res 100(3):310–326
Shelton LM, Huysentruyt LC, Mukherjee P, Seyfried TN (2010) Calorie restriction as an anti-invasive therapy for malignant brain cancer in the VM mouse. ASN Neuro 2(3), e00038
Shimazu T, Hirschey MD, Newman J, He W, Shirakawa K, Le MN, Grueter CA, Lim H, Saunders LR, Stevens RD, Newgard CB, Farese RV Jr, de Cabo R, Ulrich S, Akassoglou K, Verdin E (2013) Suppression of oxidative stress by beta-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science 339(6116):211–214
Shukla SK, Gebregiworgis T, Purohit V, Chaika NV, Gunda V, Radhakrishnan P, Mehla K, Pipinos II, Powers R, Yu F, Singh PK (2014) Metabolic reprogramming induced by ketone bodies diminishes pancreatic cancer cachexia. Cancer Metab 2:18
Singh P, Alex JM, Bast F (2014) Insulin receptor (IR) and insulin-like growth factor receptor 1 (IGF-1R) signaling systems: novel treatment strategies for cancer. Med Oncol 31(1):805
Skinner R, Trujillo A, Ma X, Beierle EA (2009) Ketone bodies inhibit the viability of human neuroblastoma cells. J Pediatr Surg 44(1):212–216
Stafford P, Abdelwahab MG, Kim DY, Preul MC, Rho JM, Scheck AC (2010) The ketogenic diet reverses gene expression patterns and reduces reactive oxygen species levels when used as an adjuvant therapy for glioma. Nutr Metab (Lond) 7:74
Stafstrom CE, Rho JM (2012) The ketogenic diet as a treatment paradigm for diverse neurological disorders. Front Pharmacol 3:59
Thompson HJ, McGinley JN, Spoelstra NS, Jiang W, Zhu Z, Wolfe P (2004) Effect of dietary energy restriction on vascular density during mammary carcinogenesis. Cancer Res 64(16):5643–5650
Tisdale MJ, Brennan RA (1983) Loss of acetoacetate coenzyme A transferase activity in tumours of peripheral tissues. Br J Cancer 47(2):293–297
Tisdale MJ, Brennan RA, Fearon KC (1987) Reduction of weight loss and tumour size in a cachexia model by a high fat diet. Br J Cancer 56(1):39–43
Urits I, Mukherjee P, Meidenbauer J, Seyfried TN (2012) Dietary restriction promotes vessel maturation in a mouse astrocytoma. J Oncol 2012:264039
Vadlakonda L, Dash A, Pasupuleti M, Anil KK, Reddanna P (2013) The Paradox of Akt-mTOR Interactions. Front Oncol 3:165
van den Bent MJ, Wefel JS, Schiff D, Taphoorn MJ, Jaeckle K, Junck L, Armstrong T, Choucair A, Waldman AD, Gorlia T, Chamberlain M, Baumert BG, Vogelbaum MA, MacDonald DR, Reardon DA, Wen PY, Chang SM, Jacobs AH (2011) Response assessment in neuro-oncology (a report of the RANO group): assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol 12(6):583–593
Vander Heiden MG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 1029–1033
Vanitallie TB, Nufert TH (2003) Ketones: metabolism's ugly duckling. Nutr Rev 61(10):327–341
Veech RL, Chance B, Kashiwaya Y, Lardy HA, Cahill GF Jr (2001) Ketone bodies, potential therapeutic uses. IUBMB Life 51(4):241–247
Venneti S, Thompson CB (2013) Metabolic modulation of epigenetics in gliomas. Brain Pathol 23(2):217–221
Verhaak RG, Hoadley KA, Purdom E, Wang V, Qi Y, Wilkerson MD, Miller CR, Ding L, Golub T, Mesirov JP, Alexe G, Lawrence M, O'Kelly M, Tamayo P, Weir BA, Gabriel S, Winckler W, Gupta S, Jakkula L, Feiler HS, Hodgson JG, James CD, Sarkaria JN, Brennan C, Kahn A, Spellman PT, Wilson RK, Speed TP, Gray JW, Meyerson M, Getz G, Perou CM, Hayes DN (2010) Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17(1):98–110
Wang Y, Yuan JL, Zhang YT, Ma JJ, Xu P, Shi CH, Zhang W, Li YM, Fu Q, Zhu GF, Xue W, Lei YH, Gao JY, Wang JY, Shao C, Yi CG, Wang H (2013) Inhibition of both EGFR and IGF1R sensitized prostate cancer cells to radiation by synergistic suppression of DNA homologous recombination repair. PLoS One 8(8), e68784
Warburg O, Wind F, Negelein E (1927) The metabolism of tumors in the body. J Gen Physiol 8(6):519–530
Ward PS, Thompson CB (2012) Metabolic reprogramming: A cancer hallmark even Warburg did not anticipate. Cancer Cell 21:297–308
Weinberg F, Chandel NS (2009) Reactive oxygen species-dependent signaling regulates cancer. Cell Mol Life Sci 66(23):3663–3673
Weller M, Stupp R, Hegi M, Wick W (2012) Individualized targeted therapy for glioblastoma: fact or fiction? Cancer J 18(1):40–44
Weroha SJ, Haluska P (2012) The insulin-like growth factor system in cancer. Endocrinol Metab Clin North Am 41(2):335–50, vi
Wolf A, Agnihotri S, Guha A (2010) Targeting metabolic remodeling in glioblastoma multiforme. Oncotarget 1(7):552–562
Woolf EC, Curley KL, Liu Q, Turner GH, Charlton JA, Preul MC, Scheck AC (2015) The ketogenic diet alters the hypoxic response and affects expression of proteins associated with angiogenesis, invasive potential and vascular permeability in a mouse glioma model. PLoS One 10(6):e0130357
Woolf EC, Stafford P, Abdelwahab MG, Fenton KE, Preul MC, Scheck AC (2013) The ketogenic diet potentiates radiation therapy in a mouse model of glioma: effects on inflammatory pathways and reactive oxygen species. Cancer Res 73:4441
Yang C, Sudderth J, Dang T, Bachoo RG, McDonald JG, DeBerardinis RJ (2009) Glioblastoma cells require glutamate dehydrogenase to survive impairments of glucose metabolism or Akt signaling. Cancer Res 69(20):7986–7993
Yun J, Johnson JL, Hanigan CL, Locasale JW (2012) Interactions between epigenetics and metabolism in cancers. Front Oncol 2:163
Zhang H, Gu C, Yu J, Wang Z, Yuan X, Yang L, Wang J, Jia Y, Liu J, Liu F (2014) Radiosensitization of glioma cells by TP53-induced glycolysis and apoptosis regulator knockdown is dependent on thioredoxin-1 nuclear translocation. Free Radic Biol Med 69C:239–248
Zhou W, Mukherjee P, Kiebish MA, Markis WT, Mantis JG, Seyfried TN (2007) The calorically restricted ketogenic diet, an effective alternative therapy for malignant brain cancer. Nutr Metab (Lond) 4:5
Zuccoli G, Marcello N, Pisanello A, Servadei F, Vaccaro S, Mukherjee P, Seyfried TN (2010) Metabolic management of glioblastoma multiforme using standard therapy together with a restricted ketogenic diet: case report. Nutr Metab 7:33–53
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Brooks, K.S., Woolf, E.C., Scheck, A.C. (2016). The Ketogenic Diet as an Adjuvant Therapy for Brain Tumors and Other Cancers. In: Ullah, M., Ahmad, A. (eds) Critical Dietary Factors in Cancer Chemoprevention. Springer, Cham. https://doi.org/10.1007/978-3-319-21461-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-21461-0_5
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21460-3
Online ISBN: 978-3-319-21461-0
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)