Abstract
-
Organic acidemias (OA) are defects in the degradation of leucine, isoleucine, and valine.
-
OA can present as either a severe neonatal onset form (poor feeding, vomiting, lethargy, tachypnea, progressing to acidosis, respiratory distress, coma, death) or late-onset (usually recurrent ketoacidosis or lethargy with catabolic stress).
-
Nutrition treatment involves use of propiogenic amino acid free medical foods and restriction of natural protein in PROP and MMA and protein restriction with or without leucine-free medical food and supplemental glycine in IVA.
-
Outcomes in PROP and MMA have been guarded with frequent neurological complications, renal dysfunction, cardiomyopathy and optic atrophy but are improving with earlier identification and treatment, as well as with liver or liver-kidney transplantation; outcomes in IVA are often normal.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
Organic acidemias (OA) are defects in the degradation of leucine, isoleucine, and valine.
-
OA can present as either a severe neonatal onset form (poor feeding, vomiting, lethargy, tachypnea, progressing to acidosis, respiratory distress, coma, death) or late-onset (usually recurrent ketoacidosis or lethargy with catabolic stress).
-
Nutrition treatment involves use of propiogenic amino acid free medical foods and restriction of natural protein in PROP and MMA and protein restriction with or without leucine-free medical food and supplemental glycine in IVA.
-
Outcomes in PROP and MMA have been guarded with frequent neurological complications, renal dysfunction, cardiomyopathy and optic atrophy but are improving with earlier identification and treatment, as well as with liver or liver-kidney transplantation; outcomes in IVA are often normal.
1 Background
Organic acidemias are disorders of branched chain amino metabolism in which non-amino organic acids accumulate in serum and urine. They are defects in the degradation pathways of leucine, isoleucine, and valine. These conditions are usually diagnosed by examining organic acids in urine with abnormal metabolites also notable on acylcarnitine profile. Organic acidemias comprise a variety of disorders and include methylmalonic acidemia (MMA), propionic acidemia (PROP), isovaleric acidemia (IVA), glutaric acidemia, type 1 (GA-1), 3- methylcrotonyl carboxylase deficiency (3-MCC), 3-methylglutaconic acidemia (3-MGA), methylmalonyl-CoA epimerase deficiency (MCEE), and vitamin B12 uptake, transport, and synthesis defects [1,2,3].
All are autosomal recessive with the exception of the rare, x-linked disorder, 2-methyl-3-hydroxybutyryl-CoA dehydrogenase deficiency (MHBD). The two primary disorders of isoleucine and valine catabolism are propionic acidemia (PROP) and methylmalonic acidemia (MMA) and the primary organic acidemia of leucine catabolism is isovaleric acidemia (IVA). These three disorders will be discussed in detail in this chapter. GA-1 is addressed in Chaps. 19 and 20. The incidence of MMA ranges from 1:83,000 in Quebec to 1:115,000 in Italy to 1:169,000 in Germany and that of PROP from 1:17,400 in Japan to 1:165,000 in Italy to 1:277,000 in Germany [4,5,6,7]. On the basis of newborn screening data, the incidence of IVA has a range of 1:62,500 live births in Germany to ~1:250,000 in the United States [7, 8]. Newborn screening via tandem mass spectrometry has allowed earlier diagnosis and has revealed a higher incidence of these disorders than previously noted based on clinical presentation suggesting a broader phenotype with milder and/or asymptomatic individuals [4, 5, 7, 9,10,11,12,13]. Techniques for newborn screening continue to be refined to aid in increased sensitivity and specificity of screening [14, 15].
The oxidation of threonine, valine, methionine, and isoleucine results in propionyl-CoA, which propionyl-CoA carboxylase converts into L-methylmalonyl-CoA, which is metabolized through methylmalonyl-CoA mutase to succinyl-CoA. Whereas the breakdown of the above amino acids is felt to contribute to ~50% of the propionyl-CoA production, gut bacteria and the breakdown of odd-chain-length fatty acids also substantially contribute to propionyl-CoA production (~ 25% each) with a minimal contribution by cholesterol metabolism [16,17,18,19] (Fig. 18.1).
PROP is caused by a deficiency of the mitochondrial enzyme, propionyl-CoA carboxylase (PCC) [9, 19]. The enzyme is composed of two subunits, an alpha and beta subunit, each encoded by a different gene, PCCA and PCCB, respectively [9]. The enzyme is biotin-dependent with biotin binding to the alpha subunit [19, 20]. Deficiency of the enzyme results in the accumulation of propionyl-CoA and increased concentrations of free propionate in blood and urine. Identification of methylcitrate and 3-hydroxypropionate are the major diagnostic metabolites seen on organic acid analysis [19, 21]. Elevation of propionylcarnitine (C3) can be seen on acylcarnitine profile [9, 21].
Classic MMA is caused by a deficiency of the enzyme, methylmalonyl-CoA mutase, an adenosylcobalamin (AdoCbl)-dependent enzyme consisting of two identical subunits (2α) [9, 19, 21] (Fig. 18.2). About 50% of cases of MMA are due to a defect in the mutase apoenzyme; in others, it is due to a defect in the uptake, transport, or synthesis of its adenosyl-B12 coenzyme causing variant forms of MMA that may or may not be associated with homocystinuria. Individuals who are deficient in mutase activity may be further designated as mut− or mut0 pending residual enzyme activity [19]. There is good correlation between residual enzyme activity and severity of the clinical phenotype [21]. Acquired methylmalonic aciduria can also be seen with acquired deficiency of vitamin B12 in pernicious anemia and in transcobalamin II deficiency [9]. Hence, vitamin B12 deficiency must be excluded in all individuals with elevated methylmalonic acid concentrations [9, 19]. Deficiency of the mutase enzyme results in the accumulation of methylmalonyl-CoA and propionyl-CoA and is reflected in elevations of methylmalonic acid and propionic acid in blood and urine [19, 21]. Methylmalonic acid, methylcitrate, 3-hydroxypropionate, and 3-hydroxyisovalerate are found on urine organic acid analysis [9, 19, 21]. Propionylcarnitine (C3) is also found on acylcarnitine profile in MMA [9, 21].
IVA was initially described in 1966 and was the first organic acidemia described. IVA is caused by a deficiency of the enzyme, isovaleryl-CoA dehydrogenase, an enzyme important in leucine catabolism and also important in the transfer of electrons to the respiratory chain [9, 19]. The consequent accumulating metabolites include isovaleric acid, isovalerylglycine, 3-hydroxyisovaleric acid, and isovalerylcarnitine (C5) [9, 19] (Fig. 18.3). These are easily identified on urine organic acid analysis and the latter on acylcarnitine profile. The excretion of isovalerylglycine and 3-hydroxyisovaleric acid are diagnostic.
2 Clinical Presentation
Organic acidemias may present at any age. In general, they can be divided into two broad groups—a severe, neonatal presentation and a chronic late-onset presentation.
2.1 Severe Neonatal Onset Form
The clinical presentation of the severe, neonatal onset form of these disorders can be quite similar for all three disorders. As is typical with inborn errors of metabolism, the pregnancy and birth history for the child is often unremarkable. Following an initial symptom-free period which may last from hours to weeks, the infant then develops nonspecific symptoms, such as poor feeding, vomiting, dehydration, lethargy, tachypnea, and hypothermia and if unrecognized, quickly progresses to respiratory distress, apnea, bradycardia, coma, cerebral edema, and death [9, 13, 16, 19, 21]. Despite newborn screening, many children are critically ill at the time of initial presentation [13]. At the time of presentation, the physical examination is primarily one of altered mental status and encephalopathy, but dehydration, hepatomegaly, abnormal tone, and seizure-like activity may also be seen [9, 13, 16, 19]. A sweaty feet or dirty sock smell is classically described for IVA secondary to excretion of 3-hydroxyisovaleric acid [9,10,11]. An antenatal presentation of PROP with nephromegaly and acute neonatal kidney injury has also been reported [22].
2.2 Chronic Late Onset Form
The late onset form typically presents after 30 days of age and maybe much later including into adolescence or adulthood [19]. McCrory et al. noted one-third of patients with PROP were ascertained by clinical presentation after one year of age [13]. Individuals may present with recurrent attacks of ketoacidosis with coma or lethargy and ataxia during times of catabolic stress such as during an illness or following a high protein meal [9, 19]. The presentation may mimic diabetic ketoacidosis [23,24,25,26]. Childhood and adolescent onset patients have presented with chronic renal failure [27]. Other individuals may present with acute hemiplegia, hemianopsia, or cerebral edema, or symptoms that mimic a cerebral vascular accident, cerebral tumor, or acute encephalitis [13, 19]. In addition, symptoms may simulate a neurologic disorder presenting with hypotonia, weakness, ataxia, seizures, progressive spasticity, movement disorder, vision loss, or developmental delay. Symptoms may also be misdiagnosed as a gastrointestinal disorder secondary to presenting with failure to thrive, anorexia, chronic vomiting, or a Reye-like presentation [9, 13, 19, 21, 27]. Some individuals may present with hematologic manifestations or present with recurrent infections [9, 19]. Adult presentations have included acute metabolic acidosis with renal and respiratory failure [28] and isolated dilated cardiomyopathy [29].
2.3 Laboratory Studies and Diagnosis
Laboratory studies typically reveal a severe metabolic acidosis with an elevated anion gap, ketosis, and hyperammonemia [9, 16, 19, 21]. Hyperuricemia, hyperlacticacidemia, and hypocalcemia may also be seen. Blood glucose can be reduced, normal, or elevated [16, 19]. Bone marrow involvement as reflected by neutropenia, anemia, thrombocytopenia, or pancytopenia can also be observed and is a rather unique finding of organic acidemias [9, 16, 19]. Diagnostic metabolites, as noted above, are seen on urine organic acid analysis and acylcarnitine profile. Quantitative plasma amino acids and urine amino acids are useful to investigate the possibility of combined MMA and homocystinuria due to vitamin B12 synthesis defects. Striking elevations of glycine and alanine can be seen in blood and urine and may be an early clue to diagnosis and explains the historical descriptive term of “ketotic hyperglycinemias” [9, 21]. The diagnosis may be confirmed by enzyme assay or molecular studies. Organic acidemias are increasingly identified via newborn screening with elevations in propionylcarnitine (C3) for PROP and MMA and elevated isovalerylcarnitine (C5) for IVA.
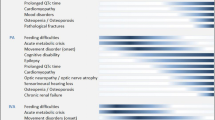
2.4 Complications
Organic acidemias are multisystem disorders with individuals at risk for a variety of complications. Complications arise despite apparent good metabolic control [30,31,32]. Neurologic complications include metabolic stroke with edema evolving into necrosis of the basal ganglia, especially the globus pallidus, and leading to a disabling movement disorder, motor dysfunction, and hypotonia [19, 21, 33,34,35]. Cortical volume loss, basal ganglia lesions, cerebral and vermian atrophy, and delayed myelination may be seen on neuroimaging [9, 19, 21, 34, 36, 37]. Restricted diffusion may be noted during acute events [36]. Clinically, seizures, deafness, optic nerve atrophy, neuropathy, myopathy, developmental delay, attention deficit-hyperactivity disorder (ADHD), and autistic features are seen [33, 35, 38,39,40,41] (Box 18.1). One study reported approximately 50% of affected individuals have an IQ < 80 [33], while another study suggested >70% of individuals with PROP have cognitive deficits [42]. The etiology of this neurologic damage is unclear. Theories include direct toxic effects of methylmalonic acid, propionic acid, and methylcitrate, impairment of energy metabolism as mediated by synergistic inhibition of the Krebs cycle and mitochondrial respiratory chain by the three metabolites, accumulation of decarboxylates in the central nervous system, neuroinflammation, interference of cytoskeleton assembly in neuronal and glial cells, and disruption of signaling pathways that promote apoptosis of neuronal cells [30, 42,43,44,45,46,47,48,49,50]. Elevations in lactate and ammonia in plasma and lactate, glutamine, glycine, and alanine in cerebrospinal fluid have also been detected in a patient with neurologic symptoms but no signs of catabolism suggesting that neurologic abnormalities may be related to localized metabolic derangements [31, 51]. Data suggests a synergistic effect of methylmalonic acid and ammonia disturbing the redox homeostasis and causing morphological brain abnormalities, including vacuolization, ischemic neurons, and pericellular edema in a rat model [52]. Propionate accumulation also results in morphological alterations in cerebral cortex astrocytes [35].
Box 18.1: Neurological Complications of Organic Acidemias
-
Metabolic stroke with edema evolving into necrosis of the basal ganglia and globus pallidus which leads to disabling movement disorder, motor dysfunction and hypotonia
-
Cerebral atrophy and delayed myelination
-
Seizures
-
Optic nerve atrophy, deafness
-
Neuropathy or skeletal myopathy
-
Developmental delay, autistic features
Another complication of organic acidemias is renal tubular acidosis with hyperuricemia leading to chronic renal impairment and eventually to renal failure [9, 19, 40] (Box 18.2). This is especially prominent in individuals with MMA; however, renal disease and failure have also been reported in individuals with propionic acidemia with an age-dependent decline [53,54,55,56]. Renal histology reveals tubulointerstitial nephritis with fibrosis, tubular atrophy, and mononuclear inflammatory infiltrate [55, 57,58,59]. Renal disease is found in the majority of individuals with MMA who are over 6 years of age and may be due to chronic glomerular hyperfiltration secondary to excessive methylmalonic acid excretion [10, 19, 34, 46]. The risk of developing renal failure seems to correlate with methylmalonic acid exposure over time and depends on the disease type with mutase-deficient patients at greater risk than patients with cobalamin defects [58]. Thus, minimizing renal injury may require strict metabolic control to maintain methylmalonic acid concentrations as low as possible [19].
Box 18.2: Complications of Organic Acidemias
-
Renal tubular acidosis (RTA) with hyperuricemia; chronic renal impairment leading to renal failure
-
Superficial desquamation and alopecia due to nutrient or essential amino acid deficiency
-
Cardiomyopathy, long QT syndrome
-
Pancreatitis – acute, chronic and/or recurrent
-
Carnitine deficiency
-
Osteopenia or osteoporosis
-
Ovarian failure
-
Liver disease including nonalcoholic steatohepatitis, fibrosis, and cirrhosis
-
Possible increased risk of infections
Furthermore, cardiomyopathy, more common in PROP than MMA and more commonly dilated than hypertrophic, may occur during acute decompensations or be the presenting feature and may be rapidly fatal [19, 60,61,62,63,64]. The pathogenesis of the cardiomyopathy is unclear—carnitine or micronutrient deficiency, infection, or acute energy deprivation have all been postulated [21, 32, 51]. Cardiomyopathy appears to develop independent of any specific metabolic profile and appears to occur at any age [32, 51, 62]. The mean age of presentation in one series was 7 years [62]. Long QT syndrome (delayed repolarization of the heart) is also reported and may occur in as high as 70% of patients with PROP [32, 65,66,67,68].
A secondary carnitine deficiency due to accumulation of propionyl-CoA and increased concentration of acylcarnitines is also common [19]. Superficial desquamation, alopecia, and corneal ulcerations similar to staphylococcal scalded skin syndrome or acrodermatitis enteropathica-like syndrome, typically associated with diarrhea, may be seen secondary to acute protein malnutrition or essential amino acid deficiency, especially isoleucine deficiency [51, 69,70,71]. Immune dysfunction has also been suggested with an increased risk for viral or bacterial infections, but good studies are lacking [51]. Chronic moniliasis has been described and reflects the effect of propionyl-CoA and methylmalonate on T-cell number and function [9]. Finally, acute, chronic, and recurrent pancreatitis, osteopenia or osteoporosis, ovarian failure, and liver abnormalities including nonalcoholic steatohepatitis, fibrosis, and cirrhosis may also occur; the etiologies of which remain unclear [9, 21, 32, 40, 51, 54, 72,73,74,75,76,77,78,79].
3 Pathophysiology
The pathogenesis of the clinical features of organic acidemias remains complex and incompletely understood. The metabolic blocks cause metabolite accumulation triggering an endogenous intoxication. Propionyl-CoA and its metabolites inhibit the Krebs cycle resulting in reduced GTP and ATP synthesis, inhibit potassium channel flow, and are known to have inhibitory effects on pyruvate dehydrogenase complex, succinyl-CoA synthetase, ATP-citrate lyase, and N-acetyl-glutamate synthetase activities, and on the glycine cleavage system [9, 17, 18, 42, 80, 81]. Furthermore, methylmalonyl-CoA is known to inhibit pyruvate carboxylase [17, 82, 83]. Similarly, isovaleric acid causes marked inhibition of Na(+), K(+) ATPase activity [84]. Methylcitrate, itself, inhibits citrate synthase, aconitase, isocitrate dehydrogenase, and glutamate dehydrogenase activities, disturbs mitochondrial energy homeostasis, decreases ATP generation [42, 81, 85] and has been shown to cause morphologic changes and apoptosis of brain cells [43]. Thus, there is an energy deficit secondary to substrate insufficiency and toxin accumulation [86], as well as a direct impact on Krebs cycle intermediates resulting in secondary effects on other pathways [42, 44]. These inhibitory effects appear to explain some of the clinical signs seen in MMA and PROP, such as the hypoglycemia, lactic acidemia, hyperglycinemia, and hyperammonemia [17].
In addition, it has become increasingly evident that there is significant mitochondrial dysfunction, impairment of the oxidative phosphorylation system, increased production of reactive oxygen species (ROS), and increased autophagy [30, 35, 42, 46, 59, 87,88,89,90,91,92,93,94,95]. The chronic effect of inhibition of mitochondrial energy production leads to oxidative stress, mitochondrial DNA damage, and altered mitochondrial morphology [44, 96]. The oxidative stress is mediated by increased levels of reactive oxygen species (ROS) and reduced ROS-protective levels of glutathione [44]. In addition, there are extensive mitochondrial ultrastructural changes in liver and kidney samples from MMA patients providing more evidence of mitochondrial dysfunction and respiratory chain impairment [59, 87, 89, 92, 97]. Mutase deficiency has been linked to mechanisms that cause mitophagy dysfunction and accumulation of damaged mitochondria that generate epithelial stress and tissue damage [87, 97]. Proteomic studies also suggest disturbances in proteins involved in energy metabolism, cellular detoxification, oxidative stress, cytoskeleton assembly, gluconeogenesis, and Kreb cycle anaplerosis [98, 99]. Finally, Storgaard et al. also suggested involvement of impaired lipolysis, blunted fatty acid oxidation, compensatory increase in carbohydrate utilization, and low work capacity as contributors to the pathophysiology of organic acidemias [100].
The etiology of the hyperammonemia seen in organic acidemias is different than that seen in urea cycle disorders. Recall that in the urea cycle, carbamoyl-phosphate synthesis is activated by N-acetylglutamate (NAG) [101]. Propionyl-CoA, which is accumulating in PROP, and isovaleryl-CoA, accumulating in IVA, are potent inhibitors of N-acetylglutamate synthase (NAGS) [11, 102]. Thus, NAG production is reduced and lack of NAG results in carbamoyl-phosphate synthetase inhibition and elevated ammonia concentrations [102]. It has also been suggested that hyperammonemia may be related to the inability to maintain adequate concentrations of glutamate precursors through a dysfunctional Krebs cycle secondary to accumulating methylcitrate and the decline in citric acid excretion [101].
4 Management
The goal of treatment of an individual with an organic acidemia is to reduce the accumulation of toxic metabolites, maintain normal growth, development, and nutritional status, prevent catabolism, and minimize complications [19, 44]. Therapy is multifaceted and typically involves a diet based on restriction of propiogenic amino acids, medication supplementation, and life-long monitoring [44]. Individualized dietary prescriptions, as prescribed by a metabolic nutritionist, balance the necessary intake of the restricted amino acids, other protein, and energy to provide the recommended daily allowances of nutrients and allow for adequate growth [103]. This is frequently accomplished by the use of special propiogenic amino acid-restricted medical foods combined with a prescribed amount of intact protein provided by breast milk or regular infant formula in infancy and regular solid foods in older children [19]. Provision of total protein intake modestly above the dietary reference intake (DRI) is well-tolerated and can provide a buffer against catabolism [32]. The target plasma range for restricted amino acids in PROP and MMA (isoleucine, valine, methionine, threonine) is low normal to normal [104]. In IVA, it is often sufficient to restrict natural protein to the recommended minimum daily requirements without the use of a leucine-free medical food [19, 104]. The target plasma range for leucine is 50–180 μM or normal range for the laboratory and 200–400 μM for glycine [104].
For all patients, particular attention must be paid to adequate energy intake. Energy requirements have been reported to be lower than predicted for age and sex during the well-fed state secondary to lower energy expenditure [105,106,107]. During illness, however, resting energy expenditure increases, requiring increased caloric intake to prevent catabolism and decompensation [19, 103]. These needs may require the use of additional fat and carbohydrate sources or protein-free modules. Catabolism is the major reason for acute decompensation [32]. If individual amino acids are found to be low, supplementation may be required, but no studies prove the efficiency of consistent supplementation of isoleucine and valine [107]. Nutrition management guidelines have been published by Yannicelli, Knerr et al., and Jurecki et al. [103, 104, 108] and are described in Chap. 21.
Therapy of IVA varies slightly from that of PROP and MMA. Isovaleryl-CoA conjugates with glycine via the enzyme, glycine-N-acylase, forming isovalerylglycine, and also binds with carnitine, via carnitine N-acylase, to form isovalerylcarnitine [109, 110]. Both products, isovalerylglycine and isovalerylcarnitine, are easily excreted in the urine. This feature is exploited for both acute and chronic management. Thus, glycine (150–300 mg/kg/d) and carnitine (50–100 mg/kg/d) are both supplemented in individuals with IVA resulting in excretion of isovaleric acid [9, 11, 16, 19, 82, 83, 104, 109,110,111,112,113,114]. Subsequently, a strict metabolic diet may not be needed.
Supplementation of L-carnitine (100–400 mg/kg/d divided 2–3 times per day) is also an important aspect of the treatment of PROP and MMA [9, 19, 21, 32, 33, 103]. Provision of oral carnitine is effective in preventing carnitine depletion, regenerating the intracellular pool of free coenzyme A (CoA), and allows urinary excretion of propionylcarnitine, thereby reducing propionate toxicity [19, 104]. High doses of carnitine may cause a fishy odor due to overproduction of methylamines and may cause diarrhea [9, 103] but may be particularly helpful in PROP [32].
All patients with MMA should be tested for responsiveness to vitamin B12 [9, 19]. Testing regimes vary, but responsiveness can be determined by monitoring quantitative plasma or urine methylmalonic acid concentrations or by measuring metabolites via urine organic acid analysis. Vitamin B12 responsiveness leads to prompt and sustained decrease of propionyl-CoA byproducts [19]. Results should be confirmed by additional studies. Many vitamin B12-responsive patients may need minimal to no protein or amino acid restriction [19]. In responsive patients, vitamin B12 is supplemented orally once per day or intramuscularly or subcutaneously daily or weekly with a beginning dose of 1 mg [19, 104]. A biotin responsive form of PROP has not been seen, but biotin dosed at 5–20 mg/d is sometimes supplemented in PROP [9, 32, 33, 103, 104].
As propionate production may result from gut bacteria, an intermittent antibiotic regime to reduce gut propionate production is sometimes implemented. The antibiotic, metronidazole, has been reported to be effective in reducing urinary excretion of propionate metabolites when used at a dose of 10–20 mg/kg once per day [16, 19, 103, 104]. The regime of therapy varies, but 7–10 consecutive days each month is a common practice [19, 33, 37, 104]. Some care providers prefer neomycin (50 mg/kg) because it is not absorbed [9]. Care must be taken to avoid complications associated with chronic antibiotic use including leukopenia, peripheral neuropathy, and pseudomembranous colitis. Metronidazole may also cause anorexia and dystonia [32, 103]. There are no studies that evaluate the clinical efficacy of metronidazole in improving clinical outcome, reducing ammonia concentrations, or reducing episodes of acute decompensation [32]. Overall, results of intermittent antibiotic use have been variable as measured by change in metabolite excretion, likely reflecting a variable colonization of gut bacteria by organisms which may or may not produce propionate [9].
Administration of N-carbamylglutamate (100–250 mg/kg/d) with or without ammonia scavengers has been suggested to help restore ureagenesis and improve acute hyperammonemia [18, 32, 44, 115, 116]. Increasing data is beginning to also suggest benefit of chronic use of N-carbamylglutamate (50 mg/kg/d) including a decrease in mean ammonia concentrations and a decrease in acute episodes of decompensation [44, 117]. Similarly, chronic therapy with sodium benzoate (150–250 mg/kg/d) has been proposed to help correct chronic hyperammonemia and hyperglycinemia [33]; however, there is no evidence that supports a role of sodium benzoate in chronic treatment especially given the evidence that higher glycine concentrations may be indicative of good metabolic control [32, 118]. Multivitamins may be given to reduce the risk of micronutrient deficiency. Citric acid and ornithine alpha-ketoglutarate have also been proposed to help sustain Krebs cycle flux and promote anaplerosis during illness and chronic management [96, 101, 119] with citric acid being most efficacious in one study of three agents [120]. In addition, coenzyme Q10 and vitamin E have been suggested as possible therapies for MMA-related optic neuropathy or secondary respiratory chain deficiency [46, 121, 122] and angiotension II inhibition has been suggested to help delay renal disease [123]. The role of growth hormone and supplemental alanine to promote anabolism has been suggested, but experience is limited [9, 32, 124,125,126]. Glutathione deficiency treated with high doses of ascorbate has also been reported [127].
In addition, prompt treatment of intercurrent illnesses, particularly those placing the individual at risk for catabolism (e.g., vomiting, diarrhea, fever), and avoidance of fasting is paramount to reduce the risk of acute decompensations. Many children develop anorexia and feeding difficulties necessitating the placement of a gastrostomy tube to prevent fasting and ensure adequate dietary intake [33, 75, 128]. Patients and families should be provided an emergency medical letter as well as a sick day protocol [32]. A medical alert bracelet or necklace is also recommended [32].
Management of an acute decompensation involves reduction or discontinuation of protein and provision of energy to stop catabolism and promote anabolism by infusion of glucose and intralipid [21]. Fluid recommendations are standard for age. Using a 10% dextrose solution at 120–150 mL/kg/day (or 1.5 times maintenance) often can provide the necessary level of glucose delivery [37, 104]. Rehydration should occur over a 48-hour period to prevent cerebral edema [104]. Additional calories are added by using intralipid at 1–3 gm/kg/day [37, 104]. If hyperglycemia develops, an insulin drip (0.01–0.1 units/kg/h) may be necessary, but the dextrose delivery rate or amount should not be decreased [9, 37, 104]. Bicarbonate supplementation (1–2 mEq/kg) may be necessary to help correct acidosis [104]. If severe hyperammonemia is present, hemodialysis, hemofiltration, continuous chronic renal replacement (CCRT), extracorporeal membrane oxygenation (ECMO), and/or ammonia scavenging medications may be necessary [33, 37, 104, 129, 130]. Sodium benzoate and sodium phenylacetate, however, should be used with caution in patients with organic acidemias because glutamine concentrations can already be low and they may potentiate ammonia toxicity by blocking the urea cycle through sequestration of CoA [44, 115]. Carbamylglutamute (100–250 mg/kg/d) has been demonstrated to be beneficial in controlling the hyperammonemia associated with an acute decompensation [33, 44, 102, 115, 131,132,133,134,135]. Administration of intravenous L-carnitine in relatively high doses (100–400 mg/kg/d) is used in acute illness [37, 104]. Metabolic decompensation in PROP may be complicated by hyperlacticacidemia due to thiamin deficiency, requiring supplementation (10 mg/kg/d) [104, 136, 137]. If the illness is prolonged, total parenteral nutrition may be necessary. Otherwise, reintroduction of protein occurs as tolerated, but should be reintroduced within 24–36 hours of therapy initiation [37, 104]. Frequent monitoring of laboratory studies and for possible complications is required.
For a fragile, medically intractable individual, liver, kidney, or combined liver kidney transplantation may be considered [138,139,140,141,142,143,144,145,146,147,148]. Transplantation is not a cure as it only partially corrects the enzymatic defect, but may result in improved survival, metabolic stability, neurologic function, and quality of life [32, 33, 86, 138,139,140,141, 149,150,151,152,153,154,155]. Perioperative complications, especially vascular complications, however, are common [138]. Liver transplantation has also been shown to improve cardiomyopathy [62, 156, 157], but cardiomyopathy has also recurred following transplantation [158]. Dietary therapy, perhaps liberalized, and L-carnitine supplementation are continued following transplantation [142, 145, 147, 149, 159]. Neurologic dysfunction, including metabolic stroke, and renal disease are not always prevented with transplantation [9, 17, 19, 32, 33, 160, 161]. One-year survival rate following transplantation was 72.2% in a multi-site, retrospective study of 12 individuals with PROP [32, 150] and may be up to 100% at experienced centers [138, 141, 162]. Therapies under investigation include import of transactivation of transcription (TAT) conjugated enzymes, viral vector-mediated gene transfer, systemic messenger RNA therapy, and genome editing [163,164,165,166].
5 Monitoring
Monitoring of patients with organic acidemias will vary according to each clinics’ practice but should occur with some degree of regularity. Patients should be seen routinely in clinic with routine monitoring of laboratory studies. Quantitative plasma amino acids should be obtained at least monthly in all patients managed with a restricted diet, although this practice varies between clinics. Quantitative methylmalonic acid is available in selected laboratories and may be used to follow individuals with MMA [9]. There is no established biomarker for monitoring therapeutic control in IVA [11]. Propionate concentrations may be difficult to obtain for individuals with PROP; some advocate following the methylcitrate to ctirate ratio via quantitative urine organic acid analysis or dried blood spots, if available [167, 168]. Propionylcarnitine has not been demonstrated to correlate with severity or level of control [32]. Ammonia, acid-base balance, and anion gap have been demonstrated to be important biochemical parameters in identifying an impending metabolic decompensation and to assess severity of PROP and MMA patients [169, 170]. The frequency of monitoring laboratory studies varies pending the patient’s age and clinical stability. Laboratory studies to obtain every 6–12 months include complete blood count, complete metabolic panel (to include electrolytes, renal and liver function studies), carnitine, urinalysis, β-type natriuretic peptide, cystatin C, and calculated glomerular filtration rate, as well as annual nutrition monitoring studies to include prealbumin, 25-hydroxyvitamin D, vitamin B12, iron, ferritin, and other micronutrients (thiamin, selenium) [32]. Additional laboratory studies to consider during acute illness include complete blood count, complete metabolic panel (to include electrolytes, renal and liver function studies), amylase, lipase, ammonia, osmolality, lactate, coagulation studies, creatine kinase, and urine ketones. Families can also be taught to test for urine ketones using ketone reagent strips at home as an early warning sign for pending decompensation [9] (Box 18.3).
Box 18.3: Laboratory Monitoring in Organic Acidemiasa
-
Routine:
-
Plasma amino acids
-
Prealbumin
-
Serum methylmalonic acid concentrations (MMA)
-
Urine Organic Acids
-
Urinary methylcitrate to citrate ratio (MC ≤ 2 times citrate in PROP)
-
-
-
Annual
-
Complete blood count
-
Electrolytes, renal and liver function tests
-
Calculated creatinine clearance and glomerular filtration rate (GFR)
-
Carnitine (total, free and esterified)
-
Nutrient adequacy: vitamin D, B12, thiamin, iron studies, minerals (zinc, selenium)
-
β-type naturiuretic peptide
-
Urinalysis
-
Cystatin C
-
-
Acute illness (additional)
-
Amylase, lipase, ammonia, ketones, lactate, coagulation studies, osmolality, CK
-
aFrequency depends on age of patient and clinical status, recommended monthly routine laboratory evaluations.
Recent evidence suggests fibroblast growth factor 21 (FGF21) may be a predictive biomarker for metabolic stress in patients with MMA and PROP [171, 172]. The plasma concentrations of FGF21 appear to correlate with disease subtype and markers of mitochondrial dysfunction and are not affected by nutritional status or renal disease [171, 172]. Molema et al. suggested FGF21 levels >1500 during stable metabolic periods predicted an increase in long-term complications in patients with MMA and PROP [171]. This laboratory study, however, is not yet readily available for clinical use.
In addition to laboratory studies, management of an individual with an organic acidemia often requires the involvement of additional subspecialty services including neurology, nephrology, cardiology, neuropsychology, endocrinology, and ophthalmology. The utilization of these subspecialties is individualized to the clinical presentation of the patient. The patient may be seen yearly if monitoring is only required to assess increased risk or may be seen more frequently if organ system involvement is already noted [32]. Cardiology evaluation, however, with echocardiogram, ECG, and 24-hour Holter monitoring is recommended yearly in individuals with PROP [32] and MMA and during acute illnesses [27]. Schreiber et al. also recommended a baseline electroencephalogram and repeat studies as clinically indicated in all patients with PROP [35]. Long-term and repeated neuropsychological assessment is an excellent tool for tracking developmental progress or decline over time. Early evaluation and, if necessary, intervention are recommended beginning at a young age. Routine bone densitometry (DEXA scan) is also recommended for all patients typically beginning at age 5 years [27, 173]. Baseline endocrinology evaluation should be considered for female patients in late adolescence or thereafter. Nephrotoxic medications and medications that prolong the QT interval should be used with caution [27].
6 Summary
The outcome of individuals with organic acidemias is quite variable. In general for PROP and MMA, late onset forms appear to have a better prognosis as compared with early onset forms, mut− MMA patients appear to do better than mut0 patients, and individuals with vitamin B12 responsive MMA appear to have improved outcome over patients with vitamin B12 unresponsive forms [10, 21, 34, 40, 58, 128, 174, 175]. In MMA, an earlier age of onset, the presence of hyperammonemia at diagnosis, and a history of seizures also predict more severe impairment [176]. The duration of hyperammonemia, abnormal acid–base balance with metabolic acidosis, and coma correlate with poor neurologic outcome [44]. Also, in general, individuals with IVA appear to have a better outcome than those with MMA or PROP; however, in contrast to MMA and PROP, the neurocognitive outcome in patients with a neonatal presentation is more favorable than in patients with a late diagnosis [177, 178]. Mortality has been reported to be >80% in the neonatal onset form of these disorders and as high as 40% before 16 years of age in the late onset forms [33, 179]. Survival has improved [33]. The survival at one year of age in patients with mut0 was 65% in the 1970s but has increased up to 90% in the 1990s [17]. Death may be due to cerebral edema, cerebral or cerebellar hemorrhage, infection, renal failure, heart failure, arrhythmias, cardiomyopathy, pancreatitis, or irreversible metabolic decompensation [9, 51, 63, 68, 179,180,181].
Morbidity is also high with frequent complications, poor growth and nutritional status, poor neurodevelopmental progress with frequent progressive neurocognitive deterioration, abnormal neurologic signs such as chorea and dystonia, and frequent and severe relapses of metabolic decompensation [6, 10, 21, 33, 68]. Overall, developmental outcome is poor in PROP and MMA with the majority of patients demonstrating developmental delay [6, 33, 51, 68, 75, 86, 178]. Martin-Hernandez et al. reported on the long-term needs of adult patients with organic acidemias [40]. In this series of 15 patients, largely with late onset disease, two-thirds of the patients had neurologic or visceral complications, and three-quarters of them required some kind of social support [40]. In contrast, developmental outcome in IVA is normal in 60% or more of the patients [86, 178]. In addition, long-term complications and the risk of metabolic decompensations associated with catabolic stress in individuals with IVA are also much less frequent than compared to PROP and MMA [40, 178]. Evaluation of older patients is beginning to suggest a risk of psychiatric disorders [86].
Outcome and prognosis, however, may be changing and improving with early identification via newborn screening. A benign MMA phenotype has been described and some patients with MMA have remained symptom-free [4, 182, 183]. In addition, infants diagnosed with IVA by newborn screen have also remained asymptomatic with carnitine supplementation and mild or no dietary restriction and retrospectively identified siblings ranging in age from 3 to 11 years were also asymptomatic [7, 11]. Dionisi-Vici et al. compared the outcome of 29 patients with MMA, PROP, or IVA diagnosed clinically to 18 similar patients diagnosed by newborn screening. The newborn screened population demonstrated an earlier diagnosis, significantly reduced mortality (11% compared to 51%) and an increased number of patients with normal development at <1 year of age [10]. A more stable clinical course with less frequent relapses of decompensation was also demonstrated [10]. Similar findings were also found by Grünert et al. in a population of patients with PROP, however, they did not demonstrate a reduction of complications in patients diagnosed by newborn screening [184]. Overall, newborn screening and early diagnosis may result in decreased early mortality, decrease severity of initial symptoms, and improved neurodevelopmental outcome [10]. Outcome data, however, is early and limited and more long-term follow-up studies are needed.
References
Abily-Donval L, Torre S, Samson A, Sudrie-Arnaud B, Acquaviva C, Guerrot AM, et al. Methylmalonyl-CoA epimerase deficiency mimicking propionic aciduria. Int J Mol Sci. 2017;18(11):2294.
Heuberger K, Bailey HJ, Burda P, Chaikuad A, Krysztofinska E, Suormala T, et al. Genetic, structural, and functional analysis of pathogenic variations causing methylmalonyl-CoA epimerase deficiency. Biochim Biophys Acta Mol basis Dis. 2019;1865(6):1265–72.
Waters PJ, Thuriot F, Clarke JT, Gravel S, Watkins D, Rosenblatt DS, et al. Methylmalonyl-coA epimerase deficiency: a new case, with an acute metabolic presentation and an intronic splicing mutation in the MCEE gene. Mol Genet Metab Rep. 2016;9:19–24.
Sniderman LC, Lambert M, Giguere R, Auray-Blais C, Lemieux B, Laframboise R, et al. Outcome of individuals with low-moderate methylmalonic aciduria detected through a neonatal screening program. J Pediatr. 1999;134(6):675–80.
Yorifuji T, Kawai M, Muroi J, Mamada M, Kurokawa K, Shigematsu Y, et al. Unexpectedly high prevalence of the mild form of propionic acidemia in Japan: presence of a common mutation and possible clinical implications. Hum Genet. 2002;111(2):161–5.
Rafique M. Propionic acidaemia: demographic characteristics and complications. J Pediatr Endocrinol Metab. 2013;26(5–6):497–501.
Ensenauer R, Vockley J, Willard JM, Huey JC, Sass JO, Edland SD, et al. A common mutation is associated with a mild, potentially asymptomatic phenotype in patients with isovaleric acidemia diagnosed by newborn screening. Am J Hum Genet. 2004;75(6):1136–42.
Ensenauer R, Fingerhut R, Maier EM, Polanetz R, Olgemoller B, Roschinger W, et al. Newborn screening for isovaleric acidemia using tandem mass spectrometry: data from 1.6 million newborns. Clin Chem. 2011;57(4):623–6.
Nyhan WL, Barshop BA, Ozand PT. Propionic acidemia, methylmalonic acidemia, isovaleric acidemia. In: Atlas of metabolic disease, 2nd ed. London: Hodder Arnold; 2005.
Dionisi-Vici C, Deodato F, Roschinger W, Rhead W, Wilcken B. ‘Classical’ organic acidurias, propionic aciduria, methylmalonic aciduria and isovaleric aciduria: long-term outcome and effects of expanded newborn screening using tandem mass spectrometry. J Inherit Metab Dis. 2006;29(2–3):383–9.
Vockley J, Ensenauer R. Isovaleric acidemia: new aspects of genetic and phenotypic heterogeneity. Am J Med Genet C Semin Med Genet. 2006;142C(2):95–103.
Cappuccio G, Atwal PS, Donti TR, Ugarte K, Merchant N, Craigen WJ, et al. Expansion of the phenotypic spectrum of propionic acidemia with isolated elevated propionylcarnitine. JIMD Rep. 2017;35:33–7.
McCrory NM, Edick MJ, Ahmad A, Lipinski S, Scott Schwoerer JA, Zhai S, et al. Comparison of methods of initial ascertainment in 58 cases of propionic acidemia enrolled in the inborn errors of metabolism information system reveals significant differences in time to evaluation and symptoms at presentation. J Pediatr. 2017;180:200–5 e8.
Monostori P, Klinke G, Richter S, Barath A, Fingerhut R, Baumgartner MR, et al. Simultaneous determination of 3-hydroxypropionic acid, methylmalonic acid and methylcitric acid in dried blood spots: second-tier LC-MS/MS assay for newborn screening of propionic acidemia, methylmalonic acidemias and combined remethylation disorders. PLoS One. 2017;12(9):e0184897.
Peng G, Shen P, Gandotra N, Le A, Fung E, Jelliffe-Pawlowski L, et al. Combining newborn metabolic and DNA analysis for second-tier testing of methylmalonic acidemia. Genet Med. 2019;21(4):896–903.
Ogier de Baulny H, Saudubray JM. Branched-chain organic acidurias. Semin Neonatol. 2002;7(1):65–74.
Tanpaiboon P. Methylmalonic acidemia (MMA). Mol Genet Metab. 2005;85(1):2–6.
Soyucen E, Demirci E, Aydin A. Outpatient treatment of propionic acidemia-associated hyperammonemia with N-carbamoyl-L-glutamate in an infant. Clin Ther. 2010;32(4):710–3.
Ogier de Baulny H, Dionisi-Vici C, Wendel U. Branched-chain organic acidurias/acidemias. In: Saudubray JM, editor. Inborn metabolic diseases. 5th ed. Heidelberg: Springer-Verlag; 2012.
Dionisi-Vici C, Ogier de Baulny H. Emergency treatment. In: Saudubray J-M, van den Berghe G, Walter JH, editors. Inborn metabolic diseases diagnosis and treatment. Berlin: Springer-Verlag; 2012. p. 104–11.
Deodato F, Boenzi S, Santorelli FM, Dionisi-Vici C. Methylmalonic and propionic aciduria. Am J Med Genet C Semin Med Genet. 2006;142C(2):104–12.
Bernheim S, Deschenes G, Schiff M, Cussenot I, Niel O. Antenatal nephromegaly and propionic acidemia: a case report. BMC Nephrol. 2017;18(1):110.
Erdem E, Cayonu N, Uysalol E, Yildirmak ZY. Chronic intermittent form of isovaleric acidemia mimicking diabetic ketoacidosis. J Pediatr Endocrinol Metab. 2010;23(5):503–5.
Dweikat IM, Naser EN, Abu Libdeh AI, Naser OJ, Abu Gharbieh NN, Maraqa NF, et al. Propionic acidemia mimicking diabetic ketoacidosis. Brain Dev. 2011;33(5):428–31.
Joshi R, Phatarpekar A. Propionic acidemia presenting as diabetic ketoacidosis. Indian Pediatr. 2011;48(2):164–5.
Guven A, Cebeci N, Dursun A, Aktekin E, Baumgartner M, Fowler B. Methylmalonic acidemia mimicking diabetic ketoacidosis in an infant. Pediatr Diabetes. 2012;13(6):e22–5.
Fraser JL, Venditti CP. Methylmalonic and propionic acidemias: clinical management update. Curr Opin Pediatr. 2016;28(6):682–93.
Zhao Z, Chu CC, Chang MY, Chang HT, Hsu YL. Management of adult-onset methylmalonic acidemia with hypotonia and acute respiratory failure: a case report. Medicine (Baltimore). 2018;97(25):e11162.
Riemersma M, Hazebroek MR, Helderman-van den Enden A, Salomons GS, Ferdinandusse S, Brouwers M, et al. Propionic acidemia as a cause of adult-onset dilated cardiomyopathy. Eur J Hum Genet. 2017;25(11):1195–201.
de Keyzer Y, Valayannopoulos V, Benoist JF, Batteux F, Lacaille F, Hubert L, et al. Multiple OXPHOS deficiency in the liver, kidney, heart, and skeletal muscle of patients with methylmalonic aciduria and propionic aciduria. Pediatr Res. 2009;66(1):91–5.
Scholl-Burgi S, Haberlandt E, Gotwald T, Albrecht U, Baumgartner Sigl S, Rauchenzauner M, et al. Stroke-like episodes in propionic acidemia caused by central focal metabolic decompensation. Neuropediatrics. 2009;40(2):76–81.
Sutton VR, Chapman KA, Gropman AL, MacLeod E, Stagni K, Summar ML, et al. Chronic management and health supervision of individuals with propionic acidemia. Mol Genet Metab. 2012;105(1):26–33.
de Baulny HO, Benoist JF, Rigal O, Touati G, Rabier D, Saudubray JM. Methylmalonic and propionic acidaemias: management and outcome. J Inherit Metab Dis. 2005;28(3):415–23.
Cosson MA, Benoist JF, Touati G, Dechaux M, Royer N, Grandin L, et al. Long-term outcome in methylmalonic aciduria: a series of 30 French patients. Mol Genet Metab. 2009;97(3):172–8.
Schreiber J, Chapman KA, Summar ML, Ah Mew N, Sutton VR, MacLeod E, et al. Neurologic considerations in propionic acidemia. Mol Genet Metab. 2012;105(1):10–5.
Pfeifer CM, Van Tassel DC, Miller JH. Unique neuroradiological findings in propionic acidemia. Radiol Case Rep. 2018;13(6):1207–11.
Chapman KA, Gropman A, MacLeod E, Stagni K, Summar ML, Ueda K, et al. Acute management of propionic acidemia. Mol Genet Metab. 2012;105(1):16–25.
Sindgikar SP, Shenoy KD, Kamath N, Shenoy R. Audit of organic acidurias from a single centre: clinical and metabolic profile at presentation with long term outcome. J Clin Diagn Res. 2017;11(9):SC11–SC4.
Ianchulev T, Kolin T, Moseley K, Sadun A. Optic nerve atrophy in propionic acidemia. Ophthalmology. 2003;110(9):1850–4.
Martin-Hernandez E, Lee PJ, Micciche A, Grunewald S, Lachmann RH. Long-term needs of adult patients with organic acidaemias: outcome and prognostic factors. J Inherit Metab Dis. 2009;32(4):523–33.
Williams ZR, Hurley PE, Altiparmak UE, Feldon SE, Arnold GL, Eggenberger E, et al. Late onset optic neuropathy in methylmalonic and propionic acidemia. Am J Ophthalmol. 2009;147(5):929–33.
Wongkittichote P, Ah Mew N, Chapman KA. Propionyl-CoA carboxylase - a review. Mol Genet Metab. 2017;122(4):145–52.
Cudre-Cung HP, Zavadakova P, do Vale-Pereira S, Remacle N, Henry H, Ivanisevic J, et al. Ammonium accumulation is a primary effect of 2-methylcitrate exposure in an in vitro model for brain damage in methylmalonic aciduria. Mol Genet Metab. 2016;119(1–2):57–67.
Haberle J, Chakrapani A, Ah Mew N, Longo N. Hyperammonaemia in classic organic acidaemias: a review of the literature and two case histories. Orphanet J Rare Dis. 2018;13(1):219.
Kolker S, Schwab M, Horster F, Sauer S, Hinz A, Wolf NI, et al. Methylmalonic acid, a biochemical hallmark of methylmalonic acidurias but no inhibitor of mitochondrial respiratory chain. J Biol Chem. 2003;278(48):47388–93.
Morath MA, Okun JG, Muller IB, Sauer SW, Horster F, Hoffmann GF, et al. Neurodegeneration and chronic renal failure in methylmalonic aciduria--a pathophysiological approach. J Inherit Metab Dis. 2008;31(1):35–43.
Ballhausen D, Mittaz L, Boulat O, Bonafe L, Braissant O. Evidence for catabolic pathway of propionate metabolism in CNS: expression pattern of methylmalonyl-CoA mutase and propionyl-CoA carboxylase alpha-subunit in developing and adult rat brain. Neuroscience. 2009;164(2):578–87.
Broomfield A, Gunny R, Prabhakar P, Grunewald S. Spontaneous rapid resolution of acute basal ganglia changes in an untreated infant with propionic acidemia: a clue to pathogenesis? Neuropediatrics. 2010;41(6):256–60.
Ribeiro LR, Della-Pace ID, de Oliveira Ferreira AP, Funck VR, Pinton S, Bobinski F, et al. Chronic administration of methylmalonate on young rats alters neuroinflammatory markers and spatial memory. Immunobiology. 2013;218(9):1175–83.
Schuck PF, Alves L, Pettenuzzo LF, Felisberto F, Rodrigues LB, Freitas BW, et al. Acute renal failure potentiates methylmalonate-induced oxidative stress in brain and kidney of rats. Free Radic Res. 2013;47(3):233–40.
Pena L, Burton BK. Survey of health status and complications among propionic acidemia patients. Am J Med Genet A. 2012;158A(7):1641–6.
Viegas CM, Zanatta A, Grings M, Hickmann FH, Monteiro WO, Soares LE, et al. Disruption of redox homeostasis and brain damage caused in vivo by methylmalonic acid and ammonia in cerebral cortex and striatum of developing rats. Free Radic Res. 2014;48(6):659–69.
Shchelochkov OA, Manoli I, Sloan JL, Ferry S, Pass A, Van Ryzin C, et al. Chronic kidney disease in propionic acidemia. Genet Med. 2019;21(12):2830–5.
Lam C, Desviat LR, Perez-Cerda C, Ugarte M, Barshop BA, Cederbaum S. 45-year-old female with propionic acidemia, renal failure, and premature ovarian failure; late complications of propionic acidemia? Mol Genet Metab. 2011;103(4):338–40.
Vernon HJ, Bagnasco S, Hamosh A, Sperati CJ. Chronic kidney disease in an adult with propionic acidemia. JIMD Rep. 2014;12:5–10.
Kasapkara CS, Akar M, Yuruk Yildirim ZN, Tuzun H, Kanar B, Ozbek MN. Severe renal failure and hyperammonemia in a newborn with propionic acidemia: effects of treatment on the clinical course. Ren Fail. 2014;36(3):451–2.
Rutledge SL, Geraghty M, Mroczek E, Rosenblatt D, Kohout E. Tubulointerstitial nephritis in methylmalonic acidemia. Pediatr Nephrol. 1993;7(1):81–2.
Horster F, Baumgartner MR, Viardot C, Suormala T, Burgard P, Fowler B, et al. Long-term outcome in methylmalonic acidurias is influenced by the underlying defect (mut0, mut-, cblA, cblB). Pediatr Res. 2007;62(2):225–30.
Zsengeller ZK, Aljinovic N, Teot LA, Korson M, Rodig N, Sloan JL, et al. Methylmalonic acidemia: a megamitochondrial disorder affecting the kidney. Pediatr Nephrol. 2014;29(11):2139–46.
Massoud AF, Leonard JV. Cardiomyopathy in propionic acidaemia. Eur J Pediatr. 1993;152(5):441–5.
Lee TM, Addonizio LJ, Barshop BA, Chung WK. Unusual presentation of propionic acidaemia as isolated cardiomyopathy. J Inherit Metab Dis. 2009;32 Suppl 1:S97–101.
Romano S, Valayannopoulos V, Touati G, Jais JP, Rabier D, de Keyzer Y, et al. Cardiomyopathies in propionic aciduria are reversible after liver transplantation. J Pediatr. 2010;156(1):128–34.
Prada CE, Al Jasmi F, Kirk EP, Hopp M, Jones O, Leslie ND, et al. Cardiac disease in methylmalonic acidemia. J Pediatr. 2011;159(5):862–4.
Laemmle A, Balmer C, Doell C, Sass JO, Haberle J, Baumgartner MR. Propionic acidemia in a previously healthy adolescent with acute onset of dilated cardiomyopathy. Eur J Pediatr. 2014;173(7):971–4.
Kakavand B, Schroeder VA, Di Sessa TG. Coincidence of long QT syndrome and propionic acidemia. Pediatr Cardiol. 2006;27(1):160–1.
Baumgartner D, Scholl-Burgi S, Sass JO, Sperl W, Schweigmann U, Stein JI, et al. Prolonged QTc intervals and decreased left ventricular contractility in patients with propionic acidemia. J Pediatr. 2007;150(2):192–7, 7 e1.
Jameson E, Walter J. Cardiac arrest secondary to long QT(C )in a child with propionic acidemia. Pediatr Cardiol. 2008;29(5):969–70.
Grunert SC, Mullerleile S, De Silva L, Barth M, Walter M, Walter K, et al. Propionic acidemia: clinical course and outcome in 55 pediatric and adolescent patients. Orphanet J Rare Dis. 2013;8:6.
De Raeve L, De Meirleir L, Ramet J, Vandenplas Y, Gerlo E. Acrodermatitis enteropathica-like cutaneous lesions in organic aciduria. J Pediatr. 1994;124(3):416–20.
Ozturk Y. Acrodermatitis enteropathica-like syndrome secondary to branched-chain amino acid deficiency in inborn errors of metabolism. Pediatr Dermatol. 2008;25(3):415.
Dominguez-Cruz JJ, Bueno-Delgado M, Pereyra J, Bernabeu-Wittel J, Conejo-Mir J. Acrodermatitis enerophatica-like skin lesions secondary to isoleucine deficiency. Eur J Dermatol. 2011;21(1):115–6.
Choe JY, Jang KM, Min SY, Hwang SK, Kang B, Choe BH. Propionic acidemia with novel mutation presenting as recurrent pancreatitis in a child. J Korean Med Sci. 2019;34(47):e303.
Imbard A, Garcia Segarra N, Tardieu M, Broue P, Bouchereau J, Pichard S, et al. Long-term liver disease in methylmalonic and propionic acidemias. Mol Genet Metab. 2018;123(4):433–40.
Sag E, Cebi AH, Kaya G, Karaguzel G, Cakir M. A rare cause of recurrent acute pancreatitis in a child: isovaleric acidemia with novel mutation. Pediatr Gastroenterol Hepatol Nutr. 2017;20(1):61–4.
North KN, Korson MS, Gopal YR, Rohr FJ, Brazelton TB, Waisbren SE, et al. Neonatal-onset propionic acidemia: neurologic and developmental profiles, and implications for management. J Pediatr. 1995;126(6):916–22.
Kahler SG, Sherwood WG, Woolf D, Lawless ST, Zaritsky A, Bonham J, et al. Pancreatitis in patients with organic acidemias. J Pediatr. 1994;124(2):239–43.
Burlina AB, Dionisi-Vici C, Piovan S, Saponara I, Bartuli A, Sabetta G, et al. Acute pancreatitis in propionic acidaemia. J Inherit Metab Dis. 1995;18(2):169–72.
Bultron G, Seashore MR, Pashankar DS, Husain SZ. Recurrent acute pancreatitis associated with propionic acidemia. J Pediatr Gastroenterol Nutr. 2008;47(3):370–1.
Mantadakis E, Chrysafis I, Tsouvala E, Evangeliou A, Chatzimichael A. Acute pancreatitis with rapid clinical improvement in a child with isovaleric acidemia. Case Rep Pediatr. 2013;2013:721871.
Grunert SC, Bodi I, Odening KE. Possible mechanisms for sensorineural hearing loss and deafness in patients with propionic acidemia. Orphanet J Rare Dis. 2017;12(1):30.
Brusque AM, Borba Rosa R, Schuck PF, Dalcin KB, Ribeiro CA, Silva CG, et al. Inhibition of the mitochondrial respiratory chain complex activities in rat cerebral cortex by methylmalonic acid. Neurochem Int. 2002;40(7):593–601.
Ozand PT, Gascon GG. Organic acidurias: a review. Part 2. J Child Neurol. 1991;6(4):288–303.
Ozand PT, Gascon GG. Organic acidurias: a review. Part 1. J Child Neurol. 1991;6(3):196–219.
Ribeiro CA, Balestro F, Grando V, Wajner M. Isovaleric acid reduces Na+, K+-ATPase activity in synaptic membranes from cerebral cortex of young rats. Cell Mol Neurobiol. 2007;27(4):529–40.
Amaral AU, et al. 2-methylcitric acid impairs glutamate metabolism and induces permeability transition in brain mitochondria. J Neurochem. 2016;137(1):62–75.
Nizon M, Ottolenghi C, Valayannopoulos V, Arnoux JB, Barbier V, Habarou F, et al. Long-term neurological outcome of a cohort of 80 patients with classical organic acidurias. Orphanet J Rare Dis. 2013;8:148.
Luciani A, Schumann A, Berquez M, Chen Z, Nieri D, Failli M, et al. Impaired mitophagy links mitochondrial disease to epithelial stress in methylmalonyl-CoA mutase deficiency. Nat Commun. 2020;11(1):970.
Ruppert T, Schumann A, Grone HJ, Okun JG, Kolker S, Morath MA, et al. Molecular and biochemical alterations in tubular epithelial cells of patients with isolated methylmalonic aciduria. Hum Mol Genet. 2015;24(24):7049–59.
Chandler RJ, Zerfas PM, Shanske S, Sloan J, Hoffmann V, DiMauro S, et al. Mitochondrial dysfunction in mut methylmalonic acidemia. FASEB J. 2009;23(4):1252–61.
Wajner M, Goodman SI. Disruption of mitochondrial homeostasis in organic acidurias: insights from human and animal studies. J Bioenerg Biomembr. 2011;43(1):31–8.
Melo DR, Kowaltowski AJ, Wajner M, Castilho RF. Mitochondrial energy metabolism in neurodegeneration associated with methylmalonic acidemia. J Bioenerg Biomembr. 2011;43(1):39–46.
Wilnai Y, Enns GM, Niemi AK, Higgins J, Vogel H. Abnormal hepatocellular mitochondria in methylmalonic acidemia. Ultrastruct Pathol. 2014;38(5):309–14.
Richard E, Alvarez-Barrientos A, Perez B, Desviat LR, Ugarte M. Methylmalonic acidaemia leads to increased production of reactive oxygen species and induction of apoptosis through the mitochondrial/caspase pathway. J Pathol. 2007;213(4):453–61.
Solano AF, Leipnitz G, De Bortoli GM, Seminotti B, Amaral AU, Fernandes CG, et al. Induction of oxidative stress by the metabolites accumulating in isovaleric acidemia in brain cortex of young rats. Free Radic Res. 2008;42(8):707–15.
Fernandes CG, Borges CG, Seminotti B, Amaral AU, Knebel LA, Eichler P, et al. Experimental evidence that methylmalonic acid provokes oxidative damage and compromises antioxidant defenses in nerve terminal and striatum of young rats. Cell Mol Neurobiol. 2011;31(5):775–85.
Collado MS, Armstrong AJ, Olson M, Hoang SA, Day N, Summar M, et al. Biochemical and anaplerotic applications of in vitro models of propionic acidemia and methylmalonic acidemia using patient-derived primary hepatocytes. Mol Genet Metab. 2020;130(3):183–96.
Luciani A, Devuyst O. Methylmalonyl acidemia: from mitochondrial metabolism to defective mitophagy and disease. Autophagy. 2020;16(6):1159–61.
Caterino M, Chandler RJ, Sloan JL, Dorko K, Cusmano-Ozog K, Ingenito L, et al. The proteome of methylmalonic acidemia (MMA): the elucidation of altered pathways in patient livers. Mol Biosyst. 2016;12(2):566–74.
Imperlini E, Santorelli L, Orru S, Scolamiero E, Ruoppolo M, Caterino M. Mass spectrometry-based metabolomic and proteomic strategies in organic acidemias. Biomed Res Int. 2016;2016:9210408.
Storgaard JH, Madsen KL, Lokken N, Vissing J, van Hall G, Lund AM, et al. Impaired lipolysis in propionic acidemia: a new metabolic myopathy? JIMD Rep. 2020;53(1):16–21.
Filipowicz HR, Ernst SL, Ashurst CL, Pasquali M, Longo N. Metabolic changes associated with hyperammonemia in patients with propionic acidemia. Mol Genet Metab. 2006;88(2):123–30.
Gebhardt B, Dittrich S, Parbel S, Vlaho S, Matsika O, Bohles H. N-carbamylglutamate protects patients with decompensated propionic aciduria from hyperammonaemia. J Inherit Metab Dis. 2005;28(2):241–4.
Yannicelli S. Nutrition therapy of organic acidaemias with amino acid-based formulas: emphasis on methylmalonic and propionic acidaemia. J Inherit Metab Dis. 2006;29(2–3):281–7.
Knerr I, Gibson KM. Disorders of leucine, isoleucine and valine metabolism. In: Blau N, editor. Physician’s guide to the diagnosis, treatment and follow-up of inherited metabolic diseases. Berlin: Springer-Verlag; 2014.
Feillet F, Bodamer OA, Dixon MA, Sequeira S, Leonard JV. Resting energy expenditure in disorders of propionate metabolism. J Pediatr. 2000;136(5):659–63.
Thomas JA, Bernstein LE, Greene CL, Koeller DM. Apparent decreased energy requirements in children with organic acidemias: preliminary observations. J Am Diet Assoc. 2000;100(9):1074–6.
Hauser NS, Manoli I, Graf JC, Sloan J, Venditti CP. Variable dietary management of methylmalonic acidemia: metabolic and energetic correlations. Am J Clin Nutr. 2011;93(1):47–56.
Jurecki E, Ueda K, Frazier D, Rohr F, Thompson A, Hussa C, et al. Nutrition management guideline for propionic acidemia: an evidence- and consensus-based approach. Mol Genet Metab. 2019;126(4):341–54.
Roe CR, Millington DS, Maltby DA, Kahler SG, Bohan TP. L-carnitine therapy in isovaleric acidemia. J Clin Invest. 1984;74(6):2290–5.
de Sousa C, Chalmers RA, Stacey TE, Tracey BM, Weaver CM, Bradley D. The response to L-carnitine and glycine therapy in isovaleric acidaemia. Eur J Pediatr. 1986;144(5):451–6.
Chinen Y, Nakamura S, Tamashiro K, Sakamoto O, Tashiro K, Inokuchi T, et al. Isovaleric acidemia: therapeutic response to supplementation with glycine, l-carnitine, or both in combination and a 10-year follow-up case study. Mol Genet Metab Rep. 2017;11:2–5.
Berry GT, Yudkoff M, Segal S. Isovaleric acidemia: medical and neurodevelopmental effects of long-term therapy. J Pediatr. 1988;113(1 Pt 1):58–64.
Naglak M, Salvo R, Madsen K, Dembure P, Elsas L. The treatment of isovaleric acidemia with glycine supplement. Pediatr Res. 1988;24(1):9–13.
Fries MH, Rinaldo P, Schmidt-Sommerfeld E, Jurecki E, Packman S. Isovaleric acidemia: response to a leucine load after three weeks of supplementation with glycine, L-carnitine, and combined glycine-carnitine therapy. J Pediatr. 1996;129(3):449–52.
Valayannopoulos V, Baruteau J, Delgado MB, Cano A, Couce ML, Del Toro M, et al. Carglumic acid enhances rapid ammonia detoxification in classical organic acidurias with a favourable risk-benefit profile: a retrospective observational study. Orphanet J Rare Dis. 2016;11:32.
Ah Mew N, McCarter R, Daikhin Y, Nissim I, Yudkoff M, Tuchman M. N-carbamylglutamate augments ureagenesis and reduces ammonia and glutamine in propionic acidemia. Pediatrics. 2010;126(1):e208–14.
Tummolo A, Melpignano L, Carella A, Di Mauro AM, Piccinno E, Vendemiale M, et al. Long-term continuous N-carbamylglutamate treatment in frequently decompensated propionic acidemia: a case report. J Med Case Reports. 2018;12(1):103.
Al-Hassnan ZN, Boyadjiev SA, Praphanphoj V, Hamosh A, Braverman NE, Thomas GH, et al. The relationship of plasma glutamine to ammonium and of glycine to acid-base balance in propionic acidaemia. J Inherit Metab Dis. 2003;26(1):89–91.
Siekmeyer M, Petzold-Quinque S, Terpe F, Beblo S, Gebhardt R, Schlensog-Schuster F, et al. Citric acid as the last therapeutic approach in an acute life-threatening metabolic decompensation of propionic acidemia. J Pediatr Endocrinol Metab. 2013;26(5–6):569–74.
Longo N, et al. Anaplerotic therapy in propionic acidemia. Mol Genet Metab. 2018;122(1–2):51–9.
Pinar-Sueiro S, Martinez-Fernandez R, Lage-Medina S, Aldamiz-Echevarria L, Vecino E. Optic neuropathy in methylmalonic acidemia: the role of neuroprotection. J Inherit Metab Dis. 2010;33 Suppl 3:S199–203.
Fragaki K, Cano A, Benoist JF, Rigal O, Chaussenot A, Rouzier C, et al. Fatal heart failure associated with CoQ10 and multiple OXPHOS deficiency in a child with propionic acidemia. Mitochondrion. 2011;11(3):533–6.
Ha TS, Lee JS, Hong EJ. Delay of renal progression in methylmalonic acidemia using angiotensin II inhibition: a case report. J Nephrol. 2008;21(5):793–6.
Kelts DG, Ney D, Bay C, Saudubray JM, Nyhan WL. Studies on requirements for amino acids in infants with disorders of amino acid metabolism. I. Effect of alanine. Pediatr Res. 1985;19(1):86–91.
Wolff JA, Kelts DG, Algert S, Prodanos C, Nyhan WL. Alanine decreases the protein requirements of infants with inborn errors of amino acid metabolism. J Neurogenet. 1985;2(1):41–9.
Marsden D, Barshop BA, Capistrano-Estrada S, Rice M, Prodanos C, Sartoris D, et al. Anabolic effect of human growth hormone: management of inherited disorders of catabolic pathways. Biochem Med Metab Biol. 1994;52(2):145–54.
Treacy E, Arbour L, Chessex P, Graham G, Kasprzak L, Casey K, et al. Glutathione deficiency as a complication of methylmalonic acidemia: response to high doses of ascorbate. J Pediatr. 1996;129(3):445–8.
Touati G, Valayannopoulos V, Mention K, de Lonlay P, Jouvet P, Depondt E, et al. Methylmalonic and propionic acidurias: management without or with a few supplements of specific amino acid mixture. J Inherit Metab Dis. 2006;29(2–3):288–98.
Gander JW, Rhone ET, Wilson WG, Barcia JP, Sacco MJ. Veno-venous extracorporeal membrane oxygenation for continuous renal replacement in a neonate with propionic acidemia. J Extra Corpor Technol. 2017;49(1):64–6.
Aygun F, Varol F, Aktuglu-Zeybek C, Kiykim E, Cam H. Continuous renal replacement therapy with high flow rate can effectively, safely, and quickly reduce plasma ammonia and leucine levels in children. Children (Basel). 2019;6(4):53.
Jones S, Reed CA, Vijay S, Walter JH, Morris AA. N-carbamylglutamate for neonatal hyperammonaemia in propionic acidaemia. J Inherit Metab Dis. 2008;31 Suppl 2:S219–22.
Filippi L, Gozzini E, Fiorini P, Malvagia S, la Marca G, Donati MA. N-carbamylglutamate in emergency management of hyperammonemia in neonatal acute onset propionic and methylmalonic aciduria. Neonatology. 2010;97(3):286–90.
Schwahn BC, Pieterse L, Bisset WM, Galloway PG, Robinson PH. Biochemical efficacy of N-carbamylglutamate in neonatal severe hyperammonaemia due to propionic acidaemia. Eur J Pediatr. 2010;169(1):133–4.
Kasapkara CS, Ezgu FS, Okur I, Tumer L, Biberoglu G, Hasanoglu A. N-carbamylglutamate treatment for acute neonatal hyperammonemia in isovaleric acidemia. Eur J Pediatr. 2011;170(6):799–801.
Abacan M, Boneh A. Use of carglumic acid in the treatment of hyperammonaemia during metabolic decompensation of patients with propionic acidaemia. Mol Genet Metab. 2013;109(4):397–401.
Matern D, Seydewitz HH, Lehnert W, Niederhoff H, Leititis JU, Brandis M. Primary treatment of propionic acidemia complicated by acute thiamine deficiency. J Pediatr. 1996;129(5):758–60.
Mayatepek E, Schulze A. Metabolic decompensation and lactic acidosis in propionic acidaemia complicated by thiamine deficiency. J Inherit Metab Dis. 1999;22(2):189–90.
Critelli K, McKiernan P, Vockley J, Mazariegos G, Squires RH, Soltys K, et al. Liver transplantation for propionic acidemia and methylmalonic acidemia: perioperative management and clinical outcomes. Liver Transpl. 2018;24(9):1260–70.
Chu TH, Chien YH, Lin HY, Liao HC, Ho HJ, Lai CJ, et al. Methylmalonic acidemia/propionic acidemia - the biochemical presentation and comparing the outcome between liver transplantation versus non-liver transplantation groups. Orphanet J Rare Dis. 2019;14(1):73.
Jain-Ghai S, Joffe AR, Bond GY, Siriwardena K, Chan A, Yap JYK, et al. Pre-school neurocognitive and functional outcomes after liver transplant in children with early onset urea cycle disorders, maple syrup urine disease, and propionic acidemia: an inception cohort matched-comparison study. JIMD Rep. 2020;52(1):43–54.
Quintero J, Molera C, Juamperez J, Redecillas S, Meavilla S, Nunez R, et al. The role of liver transplantation in propionic acidemia. Liver Transpl. 2018;24(12):1736–45.
Van Calcar SC, Harding CO, Lyne P, Hogan K, Banerjee R, Sollinger H, et al. Renal transplantation in a patient with methylmalonic acidaemia. J Inherit Metab Dis. 1998;21(7):729–37.
van’t Hoff WG, Dixon M, Taylor J, Mistry P, Rolles K, Rees L, et al. Combined liver-kidney transplantation in methylmalonic acidemia. J Pediatr. 1998;132(6):1043–4.
Lubrano R, Scoppi P, Barsotti P, Travasso E, Scateni S, Cristaldi S, et al. Kidney transplantation in a girl with methylmalonic acidemia and end stage renal failure. Pediatr Nephrol. 2001;16(11):848–51.
Nagarajan S, Enns GM, Millan MT, Winter S, Sarwal MM. Management of methylmalonic acidaemia by combined liver-kidney transplantation. J Inherit Metab Dis. 2005;28(4):517–24.
Lubrano R, Elli M, Rossi M, Travasso E, Raggi C, Barsotti P, et al. Renal transplant in methylmalonic acidemia: could it be the best option? Report on a case at 10 years and review of the literature. Pediatr Nephrol. 2007;22(8):1209–14.
Mc Guire PJ, Lim-Melia E, Diaz GA, Raymond K, Larkin A, Wasserstein MP, et al. Combined liver-kidney transplant for the management of methylmalonic aciduria: a case report and review of the literature. Mol Genet Metab. 2008;93(1):22–9.
Clothier JC, Chakrapani A, Preece MA, McKiernan P, Gupta R, Macdonald A, et al. Renal transplantation in a boy with methylmalonic acidaemia. J Inherit Metab Dis. 2011;34(3):695–700.
Yorifuji T, Muroi J, Uematsu A, Nakahata T, Egawa H, Tanaka K. Living-related liver transplantation for neonatal-onset propionic acidemia. J Pediatr. 2000;137(4):572–4.
Barshes NR, Vanatta JM, Patel AJ, Carter BA, O’Mahony CA, Karpen SJ, et al. Evaluation and management of patients with propionic acidemia undergoing liver transplantation: a comprehensive review. Pediatr Transplant. 2006;10(7):773–81.
Kasahara M, Horikawa R, Tagawa M, Uemoto S, Yokoyama S, Shibata Y, et al. Current role of liver transplantation for methylmalonic acidemia: a review of the literature. Pediatr Transplant. 2006;10(8):943–7.
Chen PW, Hwu WL, Ho MC, Lee NC, Chien YH, Ni YH, et al. Stabilization of blood methylmalonic acid level in methylmalonic acidemia after liver transplantation. Pediatr Transplant. 2010;14(3):337–41.
Vara R, Turner C, Mundy H, Heaton ND, Rela M, Mieli-Vergani G, et al. Liver transplantation for propionic acidemia in children. Liver Transpl. 2011;17(6):661–7.
Brassier A, Boyer O, Valayannopoulos V, Ottolenghi C, Krug P, Cosson MA, et al. Renal transplantation in 4 patients with methylmalonic aciduria: a cell therapy for metabolic disease. Mol Genet Metab. 2013;110(1–2):106–10.
Nagao M, Tanaka T, Morii M, Wakai S, Horikawa R, Kasahara M. Improved neurologic prognosis for a patient with propionic acidemia who received early living donor liver transplantation. Mol Genet Metab. 2013;108(1):25–9.
Arrizza C, De Gottardi A, Foglia E, Baumgartner M, Gautschi M, Nuoffer JM. Reversal of cardiomyopathy in propionic acidemia after liver transplantation: a 10-year follow-up. Transpl Int. 2015;28(12):1447–50.
Ou P, Touati G, Fraisse A, Sidi D, Kachaner J, Saudubray JM, et al. A rare cause of cardiomyopathy in childhood: propionic acidosis. Three case reports. Arch Mal Coeur Vaiss. 2001;94(5):531–3.
Berry GT, Blume ED, Wessel A, Singh T, Hecht L, Marsden D, et al. The re-occurrence of cardiomyopathy in propionic acidemia after liver transplantation. JIMD Rep. 2020;54(1):3–8.
Kasahara M, Sakamoto S, Kanazawa H, Karaki C, Kakiuchi T, Shigeta T, et al. Living-donor liver transplantation for propionic acidemia. Pediatr Transplant. 2012;16(3):230–4.
Chakrapani A, Sivakumar P, McKiernan PJ, Leonard JV. Metabolic stroke in methylmalonic acidemia five years after liver transplantation. J Pediatr. 2002;140(2):261–3.
Nyhan WL, Gargus JJ, Boyle K, Selby R, Koch R. Progressive neurologic disability in methylmalonic acidemia despite transplantation of the liver. Eur J Pediatr. 2002;161(7):377–9.
Collard R, Majtan T, Park I, Kraus JP. Import of TAT-conjugated propionyl coenzyme a carboxylase using models of propionic acidemia. Mol Cell Biol. 2018;38(6):e00491–17.
An D, Schneller JL, Frassetto A, Liang S, Zhu X, Park JS, et al. Systemic messenger RNA therapy as a treatment for methylmalonic acidemia. Cell Rep. 2017;21(12):3548–58.
Erlich-Hadad T, Hadad R, Feldman A, Greif H, Lictenstein M, Lorberboum-Galski H. TAT-MTS-MCM fusion proteins reduce MMA levels and improve mitochondrial activity and liver function in MCM-deficient cells. J Cell Mol Med. 2018;22(3):1601–13.
An D, Frassetto A, Jacquinet E, Eybye M, Milano J, DeAntonis C, et al. Long-term efficacy and safety of mRNA therapy in two murine models of methylmalonic acidemia. EBioMedicine. 2019;45:519–28.
Chandler RJ, Venditti CP. Gene therapy for methylmalonic acidemia: past, present, and future. Hum Gene Ther. 2019;30(10):1236–44.
Al-Dirbashi OY, Alfadhel M, Al-Thihli K, Al Dhahouri N, Langhans CD, Al Hammadi Z, et al. Assessment of methylcitrate and methylcitrate to citrate ratio in dried blood spots as biomarkers for inborn errors of propionate metabolism. Sci Rep. 2019;9(1):12366.
Arnold GL, et al. Methylcitrate/citrate ratio as a predictor of clinical control in propionic acidemia. J Inherit Metab Dis. 2003:37.
Zwickler T, Haege G, Riderer A, Horster F, Hoffmann GF, Burgard P, et al. Metabolic decompensation in methylmalonic aciduria: which biochemical parameters are discriminative? J Inherit Metab Dis. 2012;35(5):797–806.
Zwickler T, Riderer A, Haege G, Hoffmann GF, Kolker S, Burgard P. Usefulness of biochemical parameters in decision-making on the start of emergency treatment in patients with propionic acidemia. J Inherit Metab Dis. 2014;37(1):31–7.
Molema F, Jacobs EH, Onkenhout W, Schoonderwoerd GC, Langendonk JG, Williams M. Fibroblast growth factor 21 as a biomarker for long-term complications in organic acidemias. J Inherit Metab Dis. 2018;41(6):1179–87.
Manoli I, Sysol JR, Epping MW, Li L, Wang C, Sloan JL, et al. FGF21 underlies a hormetic response to metabolic stress in methylmalonic acidemia. JCI Insight. 2018;3(23):e124351.
Propionic acidemia: care plan & shared dataset. Mountain States Genetics Regional Collaborative; 2013.
Surtees RA, Matthews EE, Leonard JV. Neurologic outcome of propionic acidemia. Pediatr Neurol. 1992;8(5):333–7.
Nicolaides P, Leonard J, Surtees R. Neurological outcome of methylmalonic acidaemia. Arch Dis Child. 1998;78(6):508–12.
O’Shea CJ, Sloan JL, Wiggs EA, Pao M, Gropman A, Baker EH, et al. Neurocognitive phenotype of isolated methylmalonic acidemia. Pediatrics. 2012;129(6):e1541–51.
Szymanska E, Jezela-Stanek A, Bogdanska A, Rokicki D, Ehmke Vel Emczynska-Seliga E, Pajdowska M, et al. Long term follow-up of polish patients with isovaleric aciduria. Clinical and molecular delineation of isovaleric aciduria. Diagnostics (Basel). 2020;10(10):738.
Grunert SC, Wendel U, Lindner M, Leichsenring M, Schwab KO, Vockley J, et al. Clinical and neurocognitive outcome in symptomatic isovaleric acidemia. Orphanet J Rare Dis. 2012;7:9.
van der Meer SB, Poggi F, Spada M, Bonnefont JP, Ogier H, Hubert P, et al. Clinical outcome of long-term management of patients with vitamin B12-unresponsive methylmalonic acidemia. J Pediatr. 1994;125(6 Pt 1):903–8.
Fischer AQ, Challa VR, Burton BK, McLean WT. Cerebellar hemorrhage complicating isovaleric acidemia: a case report. Neurology. 1981;31(6):746–8.
van der Meer SB, Poggi F, Spada M, Bonnefont JP, Ogier H, Hubert P, et al. Clinical outcome and long-term management of 17 patients with propionic acidaemia. Eur J Pediatr. 1996;155(3):205–10.
Ledley FD, Levy HL, Shih VE, Benjamin R, Mahoney MJ. Benign methylmalonic aciduria. N Engl J Med. 1984;311(16):1015–8.
Treacy E, Clow C, Mamer OA, Scriver CR. Methylmalonic acidemia with a severe chemical but benign clinical phenotype. J Pediatr. 1993;122(3):428–9.
Grunert SC, Mullerleile S, de Silva L, Barth M, Walter M, Walter K, et al. Propionic acidemia: neonatal versus selective metabolic screening. J Inherit Metab Dis. 2012;35(1):41–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Thomas, J.A. (2022). Organic Acidemias. In: Bernstein, L.E., Rohr, F., van Calcar, S. (eds) Nutrition Management of Inherited Metabolic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-94510-7_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-94510-7_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94509-1
Online ISBN: 978-3-030-94510-7
eBook Packages: MedicineMedicine (R0)