Abstract
-
Organic acidemias (OA) are defects in the degradation of leucine, isoleucine, and valine.
-
OA can present either as a severe neonatal-onset form (poor feeding, vomiting, lethargy, tachypnea, progressing to acidosis, respiratory distress, coma, death) or late-onset form (usually recurrent ketoacidosis or lethargy with catabolic stress).
-
Nutrition treatment involves use of propiogenic amino acid-free medical foods and restriction of natural protein in PROP and MMA and protein restriction with or without leucine-free medical foods in IVA.
-
Outcomes in PROP and MMA have been guarded with frequent neurological complications, renal dysfunction, cardiomyopathy, and optic atrophy but are improving with earlier identification and treatment, as well as with liver or liver-kidney transplantation; outcomes in IVA are often normal.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Core Messages-
Organic acidemias (OA) are defects in the degradation of leucine, isoleucine, and valine.
-
OA can present either as a severe neonatal-onset form (poor feeding, vomiting, lethargy, tachypnea, progressing to acidosis, respiratory distress, coma, death) or late-onset form (usually recurrent ketoacidosis or lethargy with catabolic stress).
-
Nutrition treatment involves use of propiogenic amino acid-free medical foods and restriction of natural protein in PROP and MMA and protein restriction with or without leucine-free medical foods in IVA.
-
Outcomes in PROP and MMA have been guarded with frequent neurological complications, renal dysfunction, cardiomyopathy, and optic atrophy but are improving with earlier identification and treatment, as well as with liver or liver-kidney transplantation; outcomes in IVA are often normal.
1 Background
Organic acidemias are disorders of branched-chain amino metabolism in which non-amino organic acids accumulate in serum and urine. They are defects in the degradation pathways of leucine, isoleucine, and valine. These conditions are usually diagnosed by examining organic acids in urine with abnormal metabolites also notable on acylcarnitine profile. Organic acidemias comprise a variety of disorders and include methylmalonic acidemia (MMA), propionic acidemia (PROP), isovaleric acidemia (IVA), glutaric acidemia type 1 (GA-1), 3-methylcrotonyl carboxylase deficiency (3-MCC), 3-methylglutaconic acidemia (3-MGA), and vitamin B12 uptake, transport, and synthesis defects.
All are autosomal recessive with the exception of the rare, X-linked disorder, 2-methyl-3-hydroxybutyryl-CoA dehydrogenase deficiency (MHBD) and the newly described cobalamin X (cblX). The two primary disorders of isoleucine and valine catabolism are propionic acidemia (PROP) and methylmalonic acidemia (MMA), and the primary organic acidemia of leucine catabolism is isovaleric acidemia (IVA). These three disorders will be discussed in detail in this chapter. The incidence of MMA ranges from 1:83,000 in Quebec to 1:115,000 in Italy to 1:169,000 in Germany and that of PROP from 1:17,400 in Japan to 1:165,000 in Italy to 1:277,000 in Germany [1–4]. On the basis of newborn screening data, the incidence of IVA has a range of 1:62,500 live births in Germany to ~1:250,000 in the United States [5, 6]. Newborn screening via tandem mass spectrometry has revealed a higher incidence of these disorders than previously noted based on clinical presentation and suggests a broader phenotype with milder and asymptomatic individuals [1, 2, 5, 7–9].
The oxidation of threonine, valine, methionine, and isoleucine results in propionyl-CoA, which propionyl-CoA carboxylase converts into L-methylmalonyl-CoA, which is metabolized through methylmalonyl-CoA mutase to succinyl-CoA. Whereas the breakdown of the above amino acids is felt to contribute to ~50 % of the propionyl-CoA production, gut bacteria and the breakdown of odd-chain-length fatty acids also substantially contribute to propionyl-CoA production (~25 % each), with a minimal contribution by cholesterol metabolism [10–13] (Fig. 17.1).
PROP is caused by a deficiency of the mitochondrial enzyme, propionyl-CoA carboxylase (PCC) [7, 13]. The enzyme is composed of two subunits, an alpha and beta subunit, each encoded by a different gene, PCCA and PCCB, respectively [7]. The enzyme is biotin dependent with biotin binding to the alpha subunit [13, 14]. Deficiency of the enzyme results in the accumulation of propionyl-CoA and increased concentrations of free propionate in blood and urine. Methylcitrate and 3-hydroxypropionate are the major diagnostic metabolites seen on organic acid analysis [3, 13]. Elevation of propionylcarnitine (C3) can be seen on acylcarnitine profile [3, 7].
Classic MMA is caused by a deficiency of the enzyme methylmalonyl-CoA mutase, an adenosylcobalamin (AdoCbl)-dependent enzyme consisting of two identical subunits (2α) [3, 7, 13] (Fig. 17.2). About 50 % of cases of MMA are due to a defect in the mutase apoenzyme; in others it is due to a defect in the uptake, transport, or synthesis of its adenosyl-B12 coenzyme causing variant forms of MMA that may or may not be associated with homocystinuria. Individuals who are mutase deficient may be further designated as mut− or mut0 pending residual enzyme activity [13]. There is good correlation between residual enzymatic activity and severity of the clinical phenotype [3]. Acquired methylmalonic aciduria can also be seen with acquired deficiency of vitamin B12, in pernicious anemia, and in transcobalamin II deficiency [7]. Hence, vitamin B12 deficiency must be excluded in all individuals with elevated methylmalonic acid levels [7, 13]. Deficiency of the mutase enzyme results in the accumulation of methylmalonyl-CoA and propionyl-CoA and is reflected in elevations of methylmalonic acid and propionic acid in blood and urine [3, 13]. Methylcitrate, 3-hydroxypropionate, and 3-hydroxyisovalerate are found on urine organic acid analysis [3, 7, 13]. Propionylcarnitine (C3) is also found on acylcarnitine profile in MMA [3, 7].
IVA was initially described in 1966 and became the first organic acidemia described. IVA is caused by a deficiency of the enzyme isovaleryl-CoA dehydrogenase, an enzyme important in leucine catabolism and also important in the transfer of electrons to the respiratory chain [7, 13]. The consequent accumulating metabolites include isovaleric acid, isovalerylglycine, 3-hydroxyisovaleric acid, and isovalerylcarnitine (C5) [7, 13] (Fig. 17.3). These are easily identified on urine organic acid analysis and acylcarnitine profile. The excretion of isovalerylglycine and 3-hydroxyisovaleric acid is diagnostic.
2 Clinical Presentation
Organic acidemias may present at any age. In general, they can be divided into two broad groups – a severe, neonatal presentation and a chronic late-onset presentation.
2.1 Severe Neonatal-Onset Form
The clinical presentation of the severe, neonatal-onset form of these disorders can be quite similar for all three disorders. As is typical with inborn errors of metabolism, the pregnancy and birth history for the child is often unremarkable. Following an initial symptom-free period which may last from hours to weeks, the infant then develops nonspecific symptoms, such as poor feeding, vomiting, dehydration, lethargy, tachypnea, and hypothermia and if unrecognized, quickly progresses to respiratory distress, apnea, bradycardia, coma, cerebral edema, and death [3, 7, 10, 13]. At the time of presentation, the physical examination is primarily one of altered mental status and encephalopathy, but dehydration, hepatomegaly, abnormal tone, and seizure-like activity may also be seen [7, 10, 13]. A sweaty feet or dirty sock smell is classically described for IVA secondary to excretion of 3-hydroxyisovaleric acid [7–9].
2.2 Chronic Late-Onset Form
The late-onset form typically presents after a symptom-free period of at least 1 year and maybe much longer (into adolescence or adulthood) [13]. Individuals often present with recurrent attacks of ketoacidosis with coma or lethargy and ataxia during times of catabolic stress such as during an illness or following a high protein meal [7, 13]. The presentation may mimic diabetic ketoacidosis [15–18]. Other individuals may present with acute hemiplegia, hemianopsia, or cerebral edema, or symptoms that mimic a cerebral vascular accident, cerebral tumor, or acute encephalitis [13]. Frequently, symptoms may simulate a neurologic disorder presenting with hypotonia, weakness, ataxia, seizures, abnormal movements, or developmental delay, or symptoms may be misdiagnosed as a gastrointestinal disorder presenting with failure to thrive, anorexia, chronic vomiting, or a Reye-like presentation [3, 7, 13]. Finally, some individuals may present with hematologic manifestations or present with recurrent infections [7, 13].
2.3 Laboratory Studies and Diagnosis
Laboratory studies typically reveal a severe metabolic acidosis with an elevated anion gap, ketosis, and hyperammonemia [3, 7, 10, 13]. Hyperuricemia, hyperlactacidemia, and hypocalcemia may also be seen. Blood glucose levels can be reduced, normal, or elevated [10, 13]. Bone marrow involvement as reflected by neutropenia, anemia, thrombocytopenia, or pancytopenia can also be seen and is a rather unique finding of organic acidemias [7, 10, 13]. Diagnostic metabolites, as noted above, are seen on urine organic acid analysis and acylcarnitine profile. Quantitative plasma amino acids and urine amino acids are useful to investigate the possibility of combined MMA and homocystinuria due to vitamin B12 synthesis defects. Striking elevations of glycine and alanine can be seen in blood and urine and may be an early clue to diagnosis and explains the historical descriptive term of “ketotic hyperglycinemias” [3, 7]. The diagnosis may be confirmed by enzyme assay or molecular studies. Organic acidemias are increasingly identified via newborn screening with elevations in propionylcarnitine (C3) for PROP and MMA and elevated isovalerylcarnitine (C5) for IVA.
2.4 Complications
Organic acidemias are multisystem disorders with individuals at risk for a variety of complications. Neurologic complications include metabolic stroke with edema evolving into necrosis of the basal ganglia, especially the globus pallidus, and leading to a disabling movement disorder, motor dysfunction, and hypotonia [3, 13, 19–21]. Basal ganglia lesions, cerebral atrophy, and delayed myelination may be seen on neuroimaging [3, 7, 13, 20, 22]. Clinically, seizures, deafness, optic nerve atrophy, neuropathy, myopathy, developmental delay, and autistic features are seen [19, 21, 23–25] (Box 17.1). Approximately 50 % of affected individuals have an IQ < 80 [19]. The etiology of this neurologic damage is unclear. Theories include direct toxic effects of methylmalonic acid, propionic acid, and methylcitrate, impairment of energy metabolism as mediated by synergistic inhibition of the Krebs cycle and mitochondrial respiratory chain also by the three metabolites, accumulation of decarboxylates in the central nervous system, and/or neuroinflammation [26–32]. Elevations in plasma lactate and ammonia and in CSF lactate, glutamine, glycine, and alanine have also been detected in a patient with neurologic symptoms, but no signs of catabolism suggesting that neurologic abnormalities may be related to localized metabolic derangements [33, 34]. Newer data indicates a synergistic effect of methylmalonic acid and ammonia disturbing the redox homeostasis and causing morphological brain abnormalities, including vacuolization, ischemic neurons, and pericellular edema in a rat model [35]. Propionate accumulation also results in morphological alterations in cerebral cortex astrocytes [21].
Box 17.1: Neurological Complications of Organic Acidemias
-
Metabolic stroke with edema evolving into necrosis of the basal ganglia and globus pallidus which leads to disabling movement disorder, motor dysfunction, and hypotonia
-
Cerebral atrophy and delayed myelination
-
Seizures
-
Optic atrophy
-
Neuropathy or skeletal myopathy
-
Developmental delay; autistic features
Another complication of organic acidemias is renal tubular acidosis with hyperuricemia leading to chronic renal impairment and eventually to renal failure [7, 13, 24] (Box 17.2). This appears to be especially prominent in individuals with MMA; however, renal disease and failure has been reported in both newborns and adults with propionic acidemia [36–38]. Renal histology reveals tubulointerstitial nephritis with fibrosis, tubular atrophy, and mononuclear inflammatory infiltrate [37, 39–41]. Renal disease is found in the majority of individuals with MMA who are over 6 years of age and may be due to chronic glomerular hyperfiltration secondary to excessive methylmalonic acid excretion [8, 13, 20, 27]. The risk of developing renal failure seems to correlate with methylmalonic acid exposure over time and depends on the disease type, with mutase-deficient patients at greater risk than patients with cobalamin defects [40]. Thus, minimizing renal injury may require strict metabolic control to keep methylmalonic acid concentrations as low as possible [13].
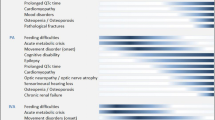
Box 17.2: Complications of Organic Acidemias
-
Renal tubular acidosis (RTA) with hyperuricemia; chronic renal impairment leading to renal failure
-
Superficial desquamation and alopecia due to nutrient or essential amino acid deficiency
-
Cardiomyopathy, long QT syndrome
-
Pancreatitis – acute or chronic
-
Carnitine deficiency
-
Osteopenia or osteoporosis
-
Immune dysfunction
-
Ovarian failure
Further, cardiomyopathy, more common in PROP than MMA and more commonly dilated than hypertrophic, may occur during acute decompensations or may be the presenting feature and may be rapidly fatal [13, 42–46]. The pathogenesis of cardiomyopathy is unclear – carnitine or micronutrient deficiency, infection, or acute energy deprivation have all been postulated [3, 34, 47]. Cardiomyopathy appears to develop independent of any specific metabolic profile and appears to occur at any age [34, 44, 47]. The mean age of presentation in one series was 7 years [44]. Long QT syndrome (delayed repolarization of the heart) is also reported and may occur in as high as 70 % of patients with PROP [47–51].
A secondary carnitine deficiency due to accumulation of propionyl-CoA and increased concentration of acylcarnitines is also common [13]. Superficial desquamation, alopecia, and corneal ulcerations similar to staphylococcal scalded skin syndrome or acrodermatitis enteropathica-like syndrome, typically associated with diarrhea, may be seen secondary to acute protein malnutrition or essential amino acid deficiency, especially isoleucine deficiency [34, 52–54]. Immune dysfunction has also been suggested with an increased risk for viral or bacterial infections, but good studies are lacking [34]. Chronic moniliasis has been described and reflects the effect of propionyl-CoA and methylmalonate on T-cell number and function [7]. Finally, acute and chronic pancreatitis, osteopenia or osteoporosis, and ovarian failure may also occur; the etiologies of which remain unclear [3, 7, 24, 34, 36, 47, 55–59].
3 Pathophysiology
The pathogenesis of the clinical features of organic acidemias remains complex and incompletely understood. Complications arise despite apparent good metabolic control [29, 33, 47]. The metabolic blocks cause metabolite accumulation, triggering an endogenous intoxication. Propionyl-CoA and its metabolites inhibit the Krebs cycle resulting in reduced ATP synthesis and are known to have inhibitory effects on pyruvate dehydrogenase complex, N-acetyl-glutamate synthetase, and on the glycine cleavage system [7, 11, 12]. Further, methylmalonyl-CoA is known to inhibit pyruvate carboxylase [11, 60, 61]. Similarly, isovaleric acid causes marked inhibition of Na(+), K(+) ATPase activity [62]. Thus, there is an energy deficit secondary to substrate insufficiency and toxin accumulation [63]. In addition, these inhibitory effects appear to explain some of the clinical signs seen in MMA and PROP, such as hypoglycemia, lactic acidemia, hyperglycinemia, and hyperammonemia [11].
The etiology of the hyperammonemia seen in organic acidemias is different than that seen in urea cycle disorders. Recall that in the urea cycle, carbamoyl-phosphate synthesis is activated by N-acetylglutamate (NAG) [64]. Propionyl-CoA, which is accumulating in PROP, and isovaleryl-CoA, accumulating in IVA, are potent inhibitors of N-acetylglutamate synthase (NAGS) [9, 65]. Thus, NAG production is reduced, and lack of NAG results in carbamoyl-phosphate synthetase inhibition and elevated ammonia levels [65]. It has also been suggested that hyperammonemia may be related to inability to maintain adequate concentrations of glutamate precursors through a dysfunctional Krebs cycle secondary to accumulating methylcitrate and the decline in citric acid excretion [64].
In addition, it has become increasingly evident that there is significant mitochondrial dysfunction and impairment of the oxidative phosphorylation system [29, 41, 66–69]. This impairment is felt to be secondary to inhibition of the Krebs cycle enzymes citrate synthase, aconitase, and isocitrate dehydrogenase by methylcitrate, inhibition of pyruvate carboxylase by methylmalonic acid, and inhibition of pyruvate dehydrogenase complex, succinyl-CoA synthetase, and ATP citrate lyase by propionic acid [70]. As a consequence, cellular depletion of available CoA occurs which results in impairment of energy metabolism [29]. Hence, oxidative phosphorylation impairment may be an additional mechanism to explain the late complications seen in organic acidemias [27, 29]. In addition, there are extensive mitochondrial ultrastructural changes in liver and kidney samples from MMA patients providing evidence of mitochondrial dysfunction and respiratory chain impairment [41, 66, 69]. Further, it is postulated that free radical production and oxidative damage may also be involved in the pathophysiology of these disorders [21, 27, 71–73].
4 Management
The goal of treatment of an individual with an organic acidemia is to reduce the accumulation of toxic metabolites; maintain normal growth, development, and nutritional status; and prevent catabolism [13]. Therapy is multifaceted and typically involves a diet based on the restriction of propiogenic amino acids combined with medication supplementation. Individualized dietary prescriptions, as prescribed by a metabolic nutritionist, balance the necessary intake of the restricted amino acids, other protein, and energy to provide the recommended daily allowances of nutrients and allow for adequate growth [74]. This is frequently accomplished by the use of special propiogenic amino acid-restricted metabolic formulas combined with a prescribed amount of natural protein provided by breast milk or regular infant formula in infancy and regular solid foods in older children [13]. Provision of protein intake modestly above the recommended daily allowance (RDA) is well tolerated and can provide a buffer against catabolism [47]. Target plasma range for restricted amino acids in PROP and MMA (isoleucine, valine, methionine, threonine) is low normal to normal [75]. In IVA, it is often sufficient to restrict natural protein to the recommended minimum daily requirements without the use of a leucine-free metabolic formula [13, 75]. Goal target plasma range for leucine is 50–180 μM or normal range for the laboratory and 200–400 μM for glycine [75].
For all patients, particular attention must be paid to adequate energy intake. Energy requirements have been reported to be lower than predicted for age and sex during the well-fed state secondary to lower energy expenditure [76–78]. During illness, however, resting energy expenditure increases, requiring increased caloric intake to prevent catabolism and decompensation [13, 74]. These needs may require the use of additional fat and carbohydrate sources or protein-free modules. Catabolism is the major reason for acute decompensation [47]. If individual amino acids are found to be low, supplementation may be required, but no studies prove the efficiency of consistent supplementation of isoleucine and valine [78]. Nutrition management guidelines have been published by Yannicelli and Knerr et al. [74, 75] and are described in Chap. 20.
Therapy of IVA varies slightly from that of PROP and MMA. Isovaleryl-CoA conjugates with glycine via the enzyme glycine-N-acylase, forming isovalerylglycine, and also binds with carnitine, via carnitine N-acylase, to form isovalerylcarnitine [79, 80]. Both products, isovalerylglycine and isovalerylcarnitine, are easily excreted in the urine. This feature is exploited for management. Thus, glycine (150–300 mg/kg/day) and carnitine (50–100 mg/kg/day) are both supplemented in individuals with IVA resulting in excretion of isovaleric acid [7, 9, 10, 13, 60, 61, 75, 79–83]. Subsequently, a strict metabolic diet may not be needed.
Supplementation of carnitine (100–400 mg/kg/day divided two to three times per day) is also an important aspect of the treatment of PROP and MMA [3, 7, 13, 19, 47, 74]. Provision of oral carnitine is effective in preventing carnitine depletion, regenerating the intracellular pool of free coenzyme A (CoA), and allows urinary excretion of propionylcarnitine, thereby reducing propionate toxicity [13, 75]. High doses of carnitine may cause a fishy odor due to overproduction of methylamines and may cause diarrhea [7, 74] but may be particularly helpful in PROP [47].
All patients with MMA should be tested for responsiveness to vitamin B12 [7, 13]. Testing regimes vary but responsiveness can be determined by monitoring quantitative plasma or urine methylmalonic acid levels or by measuring metabolites via urine organic acid analysis. Vitamin B12 responsiveness leads to prompt and sustained decrease of propionyl-CoA by-products [13]. Results should be confirmed by additional studies. Many vitamin B12-responsive patients may need minimal to no protein or amino acid restriction [13]. In responsive patients, vitamin B12 is supplemented orally once per day or intramuscularly or subcutaneously daily or weekly with a beginning dose of 1 mg [13, 75]. A biotin-responsive form of PROP has not been seen, but biotin at 5–20 mg/day is sometimes supplemented in PROP [7, 19, 47, 74, 75].
As propionate production may result from gut bacteria, an intermittent antibiotic regime to reduce gut propionate production is sometimes implemented. The antibiotic metronidazole has been effective in reducing urinary excretion of propionate metabolites when used at a dose of 10–20 mg/kg once per day [10, 13, 74, 75]. The regime of therapy varies, but 7–10 consecutive days each month is a common practice [13, 19, 22, 75]. Some care providers prefer neomycin (50 mg/kg) because it is not absorbed [7]. Care must be taken to avoid complications associated with chronic antibiotic use including leukopenia, peripheral neuropathy, and pseudomembranous colitis [13]. Metronidazole may also cause anorexia and dystonia [47, 74]. There are no studies that evaluate the clinical efficacy of metronidazole in improving clinical outcome, reducing ammonia levels, or reducing episodes of acute decompensation [47]. Overall, results of use have been variable as measured by change in metabolite excretion likely reflecting a variable colonization of gut bacteria by organisms which may or may not produce propionate [7].
Supplementation with N-carbamylglutamate (50–100 mg/kg/day) has been suggested to help restore ureagenesis and improve hyperammonemia; however, limited information is available that supports chronic use of N-carbamylglutamate [12, 47, 84]. Similarly, chronic therapy with sodium benzoate (150–250 mg/kg/day) has been proposed to help correct chronic hyperammonemia and hyperglycinemia [19]; however, there is no evidence that supports a role of sodium benzoate in chronic treatment especially given the evidence that higher glycine levels may be indicative of good metabolic control [47, 85]. Multivitamins may be given to reduce the risk of micronutrient deficiency. Citric acid and ornithine alpha-ketoglutarate have also been proposed to help sustain Krebs cycle flux during illness [64, 86]. In addition, coenzyme Q10 and vitamin E have been suggested as possible therapies for MMA-related optic neuropathy or secondary respiratory chain deficiency [27, 87, 88], and angiotensin II inhibition has been suggested to help delay renal disease [89]. The role of growth hormone and supplemental alanine to promote anabolism has been suggested, but experience is limited [7, 47, 90–92]. Glutathione deficiency treated with high doses of ascorbate has also been reported [93].
In addition, prompt treatment of intercurrent illnesses, particularly those placing the individual at risk for catabolism (e.g., vomiting, diarrhea, fever), and avoidance of fasting are paramount to reduce the risk of acute decompensations. Many children develop anorexia and feeding difficulties necessitating the placement of a gastrostomy tube to prevent fasting and ensure adequate dietary intake [19, 55, 94]. Patients and families should be provided an emergency medical letter as well as a sick-day protocol [47]. A MedicAlert bracelet or necklace is also recommended [47].
Management of an acute decompensation involves reduction or discontinuation of protein and provision of calories to stop catabolism and promote anabolism by infusion of glucose and intralipid [3]. Fluid recommendations are standard for age. Using a 10 % dextrose solution at 120–150 mL/kg/day (or 1.5 times maintenance) often can provide the necessary level of glucose delivery [22, 75]. Rehydration should occur over a 48-h period to prevent cerebral edema [75]. Additional calories are added by using intralipid at 1–3 g/kg/day [22, 75]. If hyperglycemia develops, an insulin drip (0.01–0.1 units/kg/h) may be necessary, but dextrose delivery rate or amount should not be decreased [7, 22, 75]. Bicarbonate supplementation (1–2 mEq/kg) may be necessary to help correct acidosis [75]. If severe hyperammonemia is present, hemodialysis or hemofiltration or ammonia scavenging medications may be necessary [19, 22, 75]. Recently, carbamylglutamate (50–100 mg/kg/day) has been demonstrated to be beneficial in controlling the hyperammonemia associated with an acute decompensation [19, 65, 95–99]. Administration of intravenous L-carnitine in relatively high doses (100–400 mg/kg/day) is used in acute illness [22, 75]. Metabolic decompensation in PROP may be complicated by hyperlacticacidemia due to thiamine deficiency, requiring vitamin supplementation (10 mg/kg/day) [75, 100, 101]. If the illness is prolonged, total parenteral nutrition may be necessary. Otherwise, reintroduction of protein occurs as tolerated, but should be reintroduced within 24–36 h of therapy initiation [22, 75]. Frequent monitoring of laboratory studies and for possible complications is required.
For a fragile, medically intractable individual, liver, renal, or combined liver-kidney transplantation may be considered [102–108]. Transplantation is not a cure as it only partially corrects the enzymatic defect, but may result in improved metabolic stability, neurologic function, and quality of life [19, 47, 63, 109–115]. Liver transplantation has also been shown to improve cardiomyopathy [44, 116]. Dietary therapy, perhaps liberalized, and carnitine supplementation are continued following transplantation [102, 105, 107, 109, 117]. Neurologic dysfunction, including metabolic stroke, and renal disease are not always prevented with transplantation [7, 11, 13, 19, 47, 118, 119]. One-year survival rate following transplant was 72.2 % in a multi-site, retrospective study of 12 individuals with PROP [47, 110].
5 Monitoring
Monitoring of patients with organic acidemias will vary according to each clinics’ practice but should occur with some degree of regularity. Patients should be seen routinely in clinic with routine monitoring of laboratory studies. Quantitative plasma amino acids should be obtained at least monthly in all patients managed with a restricted diet, although this practice varies between clinics. Quantitative methylmalonic acid levels are available in selected laboratories and may be used to follow individuals with MMA [7]. There is no established biomarker for monitoring therapeutic control in IVA [9]. Propionate levels may be difficult to obtain for individuals with PA; some advocate following the citrate-to-methylcitrate ratio via quantitative urine organic acid analysis if available [120]. Propionylcarnitine has not been demonstrated to correlate with severity or level of control [47]. Ammonia, acid-base balance, and anion gap have been demonstrated to be important biochemical parameters in identifying an impending metabolic decompensation and to assess severity of PROP and MMA patients [121, 122]. The frequency of monitoring laboratory studies varies pending the patient’s age and clinical stability. Laboratory studies to obtain every 6–12 months include complete blood count, complete metabolic panel (to include electrolytes, renal and liver function studies), carnitine, urinalysis, β-type natriuretic peptide, and calculated glomerular filtration rate as well as annual nutrition monitoring studies to include prealbumin, 25-hydroxy vitamin D, vitamin B12, iron, ferritin, and other micronutrients (thiamine, selenium) [47]. Additional laboratory studies to consider during acute illness include complete blood count, complete metabolic panel (to include electrolytes, renal and liver function studies), amylase, lipase, ammonia, osmolality, lactate, coagulation studies, creatine kinase, and urine ketones. Families can also be taught to test for urine ketones using Ketostix at home as an early warning sign for pending decompensation [7] (Box 17.3).
Box 17.3: Laboratory Monitoring in Organic Acidemiasa
-
Routine:
-
Plasma amino acids
-
Prealbumin
-
Serum methylmalonic acid concentrations (MMA)
-
Urine organic acids
-
Urinary citrate-to-methylcitrate (MC) ratio (MC ≤ 2 times citrate in PROP)
-
-
-
Annual
-
Complete blood count
-
Electrolytes, renal and liver function tests
-
Carnitine (total, free, and esterified)
-
Nutrient adequacy: (vitamin D, B12, thiamin, iron studies, minerals (zinc, selenium))
-
β-type natriuretic peptide
-
Urine analysis
-
-
Acute illness (additional)
-
Amylase, lipase, ammonia, ketones
-
aFrequency depends on age of patient and clinical status, recommended monthly routine laboratory evaluations.
In addition to laboratory studies, management of an individual with an organic acidemia often requires the involvement of additional subspecialty services including neurology, nephrology, cardiology, neuropsychology, and ophthalmology. The utilization of these subspecialties is individualized to the clinical presentation of the patient. The patient may be seen yearly if only monitoring due to increased risk or may be seen frequently if organ system involvement is already noted [47]. Cardiology evaluation, however, with echocardiogram, ECG, and 24-h Holter monitoring is recommended yearly in individuals with PROP [47]. Schreiber et al. also recommended a baseline EEG and repeat studies as clinically indicated in all patients with PROP [21]. Long-term and repeated neuropsychological assessment is an excellent tool for tracking developmental progress or decline over time. Early evaluation and, if necessary, intervention is recommended beginning at a young age. Routine bone densitometry (DEXA scan) is also recommended for all patients typically beginning at age 5 years [123].
6 Summary
The outcome of individuals with organic acidemias is quite variable. In general for PROP and MMA, late-onset forms appear to have a better prognosis as compared with early-onset forms, mut− MMA patients appear to do better than mut0 patients, and individuals with vitamin B12-responsive MMA appear to have improved outcome over patients with vitamin B12-unresponsive forms [3, 8, 20, 24, 40, 94, 124, 125]. In MMA, an earlier age of onset, the presence of hyperammonemia at diagnosis, and a history of seizures also predicted more severe impairment [126]. Also, in general, individuals with IVA appear to have a better outcome than those with MMA or PROP; however, in contrast to MMA and PROP, the neurocognitive outcome in patients with a neonatal presentation is more favorable than in patients with a late diagnosis [127]. Mortality has been reported to be >80 % in the neonatal-onset form of these disorders and as high as 40 % before 16 years of age in the late-onset forms [19, 128]. Survival has improved [19]. The survival at 1 year of age in patients with mut0 was 65 % in the 1970s but has increased up to 90 % in the 1990s [11]. Death may be due to cerebral edema, cerebral or cerebellar hemorrhage, infection, renal failure, heart failure, arrhythmias, cardiomyopathy, pancreatitis, or irreversible metabolic decompensation [7, 34, 45, 51, 128–131].
Morbidity is also high with frequent complications, poor growth and nutritional status, poor neurodevelopmental progress with frequent progressive neurocognitive deterioration, abnormal neurologic signs such as chorea and dystonia, and frequent and severe relapses of metabolic decompensation [3, 4, 8, 19, 51]. Overall, developmental outcome is poor in PROP and MMA, with the majority of patients demonstrating developmental delay [4, 19, 34, 51, 55, 63, 127]. Martin-Hernandez et al. reported on the long-term needs of adult patients with organic acidemias [24]. In this series of 15 patients, largely with late-onset disease, two-thirds of the patients had neurologic or visceral complications and three-quarters of them required some kind of social support [24]. In contrast, developmental outcome in IVA is normal in 60 % or more of the patients [63, 127]. In addition, long-term complications and the risk of metabolic decompensations associated with catabolic stress in individuals with IVA are also much less frequent than compared to PROP and MMA [24, 127]. Evaluation of older patients is beginning to suggest a risk of psychiatric disorders [63].
Outcome and prognosis, however, may be changing and improving with early identification via newborn screening. A benign MMA phenotype has been described, and some patients with MMA have remained symptom-free [1, 132, 133]. In addition, infants diagnosed with IVA by newborn screen have also remained asymptomatic with carnitine supplementation and mild or no dietary restriction and retrospectively identified siblings ranging in age from 3 to 11 years were also asymptomatic [5, 9]. Dionisi-Vici et al. compared the outcome of 29 patients with MMA, PROP, or IVA diagnosed clinically to 18 similar patients diagnosed by newborn screening. The newborn-screened population demonstrated an earlier diagnosis, significantly reduced mortality (11 % compared to 51 %), and an increased number of patients with normal development at <1 year of age [8]. A more stable clinical course with less frequent relapses of decompensation was also demonstrated [8]. Similar findings were also found by Grünert et al. in a population of PROP patients; however, they did not demonstrate a reduction of complications in patients diagnosed by newborn screening [134]. Overall, newborn screening and early diagnosis may result in decreased early mortality, decreased severity of initial symptoms, and improved neurodevelopmental outcome [8]. Outcome data, however, is early and limited, and more long-term follow-up studies are needed.
References
Sniderman LC, et al. Outcome of individuals with low-moderate methylmalonic aciduria detected through a neonatal screening program. J Pediatr. 1999;134(6):675–80.
Yorifuji T, et al. Unexpectedly high prevalence of the mild form of propionic acidemia in Japan: presence of a common mutation and possible clinical implications. Hum Genet. 2002;111(2):161–5.
Deodato F, et al. Methylmalonic and propionic aciduria. Am J Med Genet C Semin Med Genet. 2006;142C(2):104–12.
Rafique M. Propionic acidaemia: demographic characteristics and complications. J Pediatr Endocrinol Metab. 2013;26(5–6):497–501.
Ensenauer R, et al. A common mutation is associated with a mild, potentially asymptomatic phenotype in patients with isovaleric acidemia diagnosed by newborn screening. Am J Hum Genet. 2004;75(6):1136–42.
Ensenauer R, et al. Newborn screening for isovaleric acidemia using tandem mass spectrometry: data from 1.6 million newborns. Clin Chem. 2011;57(4):623–6.
Nyhan WL, B. B, Ozand PT. Propionic acidemia (Ch 2) Methylmalonic acidemia (Ch 3) Isovaleric Acidemia (Ch 7). In: Atlas of metabolic diseases. 2nd ed. London: Hodder Arnold; 2005.
Dionisi-Vici C, et al. ‘Classical’ organic acidurias, propionic aciduria, methylmalonic aciduria and isovaleric aciduria: long-term outcome and effects of expanded newborn screening using tandem mass spectrometry. J Inherit Metab Dis. 2006;29(2–3):383–9.
Vockley J, Ensenauer R. Isovaleric acidemia: new aspects of genetic and phenotypic heterogeneity. Am J Med Genet C Semin Med Genet. 2006;142C(2):95–103.
Ogier de Baulny H, Saudubray JM. Branched-chain organic acidurias. Semin Neonatol. 2002;7(1):65–74.
Tanpaiboon P. Methylmalonic acidemia (MMA). Mol Genet Metab. 2005;85(1):2–6.
Soyucen E, Demirci E, Aydin A. Outpatient treatment of propionic acidemia-associated hyperammonemia with N-carbamoyl-L-glutamate in an infant. Clin Ther. 2010;32(4):710–3.
Ogier de Baulny H, Dionisi-Vici C, Wendel U. Branched-chain organic acidurias/acidemias. In: van den Berghe G, van den Berghe G, Saudubray J-M, Walter JH, editors. Inborn metabolic diseases. 5th ed. Heidelberg: Springer; 2012.
Dionisi-Vici C, Ogier de Baulny H. Emergency treatment. In: van den Berghe G, Saudubray J-M, Walter JH, editors. Inborn metabolic diseases. Diagnosis and treatment. Berlin: Springer; 2012. p. 104–11.
Erdem E, et al. Chronic intermittent form of isovaleric acidemia mimicking diabetic ketoacidosis. J Pediatr Endocrinol Metab. 2010;23(5):503–5.
Dweikat IM, et al. Propionic acidemia mimicking diabetic ketoacidosis. Brain Dev. 2011;33(5):428–31.
Joshi R, Phatarpekar A. Propionic acidemia presenting as diabetic ketoacidosis. Indian Pediatr. 2011;48(2):164–5.
Guven A, et al. Methylmalonic acidemia mimicking diabetic ketoacidosis in an infant. Pediatr Diabetes. 2012;13(6):e22–5.
de Baulny HO, et al. Methylmalonic and propionic acidaemias: management and outcome. J Inherit Metab Dis. 2005;28(3):415–23.
Cosson MA, et al. Long-term outcome in methylmalonic aciduria: a series of 30 French patients. Mol Genet Metab. 2009;97(3):172–8.
Schreiber J, et al. Neurologic considerations in propionic acidemia. Mol Genet Metab. 2012;105(1):10–5.
Chapman KA, et al. Acute management of propionic acidemia. Mol Genet Metab. 2012;105(1):16–25.
Ianchulev T, et al. Optic nerve atrophy in propionic acidemia. Ophthalmology. 2003;110(9):1850–4.
Martín-Hernández E, et al. Long-term needs of adult patients with organic acidaemias: outcome and prognostic factors. J Inherit Metab Dis. 2009;32(4):523–33.
Williams ZR, et al. Late onset optic neuropathy in methylmalonic and propionic acidemia. Am J Ophthalmol. 2009;147(5):929–33.
Kölker S, et al. Methylmalonic acid, a biochemical hallmark of methylmalonic acidurias but no inhibitor of mitochondrial respiratory chain. J Biol Chem. 2003;278(48):47388–93.
Morath MA, et al. Neurodegeneration and chronic renal failure in methylmalonic aciduria–a pathophysiological approach. J Inherit Metab Dis. 2008;31(1):35–43.
Ballhausen D, et al. Evidence for catabolic pathway of propionate metabolism in CNS: expression pattern of methylmalonyl-CoA mutase and propionyl-CoA carboxylase alpha-subunit in developing and adult rat brain. Neuroscience. 2009;164(2):578–87.
de Keyzer Y, et al. Multiple OXPHOS deficiency in the liver, kidney, heart, and skeletal muscle of patients with methylmalonic aciduria and propionic aciduria. Pediatr Res. 2009;66(1):91–5.
Broomfield A, et al. Spontaneous rapid resolution of acute basal ganglia changes in an untreated infant with propionic acidemia: a clue to pathogenesis? Neuropediatrics. 2010;41(6):256–60.
Ribeiro LR, et al. Chronic administration of methylmalonate on young rats alters neuroinflammatory markers and spatial memory. Immunobiology. 2013;218(9):1175–83.
Schuck PF, et al. Acute renal failure potentiates methylmalonate-induced oxidative stress in brain and kidney of rats. Free Radic Res. 2013;47(3):233–40.
Scholl-Bürgi S, et al. Stroke-like episodes in propionic acidemia caused by central focal metabolic decompensation. Neuropediatrics. 2009;40(2):76–81.
Pena L, Burton BK. Survey of health status and complications among propionic acidemia patients. Am J Med Genet A. 2012;158A(7):1641–6.
Viegas CM, et al. Disruption of redox homeostasis and brain damage caused in vivo by methylmalonic acid and ammonia in cerebral cortex and striatum of developing rats. Free Radic Res. 2014;48(6):659–69.
Lam C, et al. 45-year-old female with propionic acidemia, renal failure, and premature ovarian failure; late complications of propionic acidemia? Mol Genet Metab. 2011;103(4):338–40.
Vernon HJ, et al. Chronic kidney disease in an adult with propionic acidemia. JIMD Rep. 2014;12:5–10.
Kasapkara CS, et al. Severe renal failure and hyperammonemia in a newborn with propionic acidemia: effects of treatment on the clinical course. Ren Fail. 2014;36(3):451–2.
Rutledge SL, et al. Tubulointerstitial nephritis in methylmalonic acidemia. Pediatr Nephrol. 1993;7(1):81–2.
Hörster F, et al. Long-term outcome in methylmalonic acidurias is influenced by the underlying defect (mut0, mut-, cblA, cblB). Pediatr Res. 2007;62(2):225–30.
Zsengellér ZK, et al. Methylmalonic acidemia: a megamitochondrial disorder affecting the kidney. Pediatr Nephrol. 2014;29:2139–46.
Massoud AF, Leonard JV. Cardiomyopathy in propionic acidaemia. Eur J Pediatr. 1993;152(5):441–5.
Lee TM, et al. Unusual presentation of propionic acidaemia as isolated cardiomyopathy. J Inherit Metab Dis. 2009;32 Suppl 1:S97–101.
Romano S, et al. Cardiomyopathies in propionic aciduria are reversible after liver transplantation. J Pediatr. 2010;156(1):128–34.
Prada CE, et al. Cardiac disease in methylmalonic acidemia. J Pediatr. 2011;159(5):862–4.
Laemmle A, et al. Propionic acidemia in a previously healthy adolescent with acute onset of dilated cardiomyopathy. Eur J Pediatr. 2014;173(7):971–4.
Sutton VR, et al. Chronic management and health supervision of individuals with propionic acidemia. Mol Genet Metab. 2012;105(1):26–33.
Kakavand B, Schroeder VA, Di Sessa TG. Coincidence of long QT syndrome and propionic acidemia. Pediatr Cardiol. 2006;27(1):160–1.
Baumgartner D, et al. Prolonged QTc intervals and decreased left ventricular contractility in patients with propionic acidemia. J Pediatr. 2007;150(2):192–7, 197.e1.
Jameson E, Walter J. Cardiac arrest secondary to long QT(C) in a child with propionic acidemia. Pediatr Cardiol. 2008;29(5):969–70.
Grünert SC, et al. Propionic acidemia: clinical course and outcome in 55 pediatric and adolescent patients. Orphanet J Rare Dis. 2013;8:6.
De Raeve L, et al. Acrodermatitis enteropathica-like cutaneous lesions in organic aciduria. J Pediatr. 1994;124(3):416–20.
Oztürk Y. Acrodermatitis enteropathica-like syndrome secondary to branched-chain amino acid deficiency in inborn errors of metabolism. Pediatr Dermatol. 2008;25(3):415.
Domínguez-Cruz JJ, et al. Acrodermatitis enteropathica-like skin lesions secondary to isoleucine deficiency. Eur J Dermatol. 2011;21(1):115–6.
North KN, et al. Neonatal-onset propionic acidemia: neurologic and developmental profiles, and implications for management. J Pediatr. 1995;126(6):916–22.
Kahler SG, et al. Pancreatitis in patients with organic acidemias. J Pediatr. 1994;124(2):239–43.
Burlina AB, et al. Acute pancreatitis in propionic acidaemia. J Inherit Metab Dis. 1995;18(2):169–72.
Bultron G, et al. Recurrent acute pancreatitis associated with propionic acidemia. J Pediatr Gastroenterol Nutr. 2008;47(3):370–1.
Mantadakis E, et al. Acute pancreatitis with rapid clinical improvement in a child with isovaleric acidemia. Case Rep Pediatr. 2013;2013:721871.
Ozand PT, Gascon GG. Organic acidurias: a review. Part 2. J Child Neurol. 1991;6(4):288–303.
Ozand PT, Gascon GG. Organic acidurias: a review. Part 1. J Child Neurol. 1991;6(3):196–219.
Ribeiro CA, et al. Isovaleric acid reduces Na+, K+-ATPase activity in synaptic membranes from cerebral cortex of young rats. Cell Mol Neurobiol. 2007;27(4):529–40.
Nizon M, et al. Long-term neurological outcome of a cohort of 80 patients with classical organic acidurias. Orphanet J Rare Dis. 2013;8:148.
Filipowicz HR, et al. Metabolic changes associated with hyperammonemia in patients with propionic acidemia. Mol Genet Metab. 2006;88(2):123–30.
Gebhardt B, et al. N-carbamylglutamate protects patients with decompensated propionic aciduria from hyperammonaemia. J Inherit Metab Dis. 2005;28(2):241–4.
Chandler RJ, et al. Mitochondrial dysfunction in mut methylmalonic acidemia. FASEB J. 2009;23(4):1252–61.
Wajner M, Goodman SI. Disruption of mitochondrial homeostasis in organic acidurias: insights from human and animal studies. J Bioenerg Biomembr. 2011;43(1):31–8.
Melo DR, et al. Mitochondrial energy metabolism in neurodegeneration associated with methylmalonic acidemia. J Bioenerg Biomembr. 2011;43(1):39–46.
Wilnai Y, et al. Abnormal hepatocellular mitochondria in methylmalonic acidemia. Ultrastruct Pathol. 2014;38(5):309–14.
Brusque AM, et al. Inhibition of the mitochondrial respiratory chain complex activities in rat cerebral cortex by methylmalonic acid. Neurochem Int. 2002;40(7):593–601.
Richard E, et al. Methylmalonic acidaemia leads to increased production of reactive oxygen species and induction of apoptosis through the mitochondrial/caspase pathway. J Pathol. 2007;213(4):453–61.
Solano AF, et al. Induction of oxidative stress by the metabolites accumulating in isovaleric acidemia in brain cortex of young rats. Free Radic Res. 2008;42(8):707–15.
Fernandes CG, et al. Experimental evidence that methylmalonic acid provokes oxidative damage and compromises antioxidant defenses in nerve terminal and striatum of young rats. Cell Mol Neurobiol. 2011;31(5):775–85.
Yannicelli S. Nutrition therapy of organic acidaemias with amino acid-based formulas: emphasis on methylmalonic and propionic acidaemia. J Inherit Metab Dis. 2006;29(2–3):281–7.
Knerr I, V J, Gibson KM. Disorders of leucine, isoleucine and valine metabolism. In: Blau N, editor. Physician’s guide to the diagnosis, treatment and follow-up of inherited metabolic diseases. Berlin: Springer; 2014. p. 103–41.
Feillet F, et al. Resting energy expenditure in disorders of propionate metabolism. J Pediatr. 2000;136(5):659–63.
Thomas JA, et al. Apparent decreased energy requirements in children with organic acidemias: preliminary observations. J Am Diet Assoc. 2000;100(9):1074–6.
Hauser NS, et al. Variable dietary management of methylmalonic acidemia: metabolic and energetic correlations. Am J Clin Nutr. 2011;93(1):47–56.
Roe CR, et al. L-carnitine therapy in isovaleric acidemia. J Clin Invest. 1984;74(6):2290–5.
de Sousa C, et al. The response to L-carnitine and glycine therapy in isovaleric acidaemia. Eur J Pediatr. 1986;144(5):451–6.
Berry GT, Yudkoff M, Segal S. Isovaleric acidemia: medical and neurodevelopmental effects of long-term therapy. J Pediatr. 1988;113(1 Pt 1):58–64.
Naglak M, et al. The treatment of isovaleric acidemia with glycine supplement. Pediatr Res. 1988;24(1):9–13.
Fries MH, et al. Isovaleric acidemia: response to a leucine load after three weeks of supplementation with glycine, L-carnitine, and combined glycine-carnitine therapy. J Pediatr. 1996;129(3):449–52.
Ah Mew N, et al. N-carbamylglutamate augments ureagenesis and reduces ammonia and glutamine in propionic acidemia. Pediatrics. 2010;126(1):e208–14.
Al-Hassnan ZN, et al. The relationship of plasma glutamine to ammonium and of glycine to acid-base balance in propionic acidaemia. J Inherit Metab Dis. 2003;26(1):89–91.
Siekmeyer M, et al. Citric acid as the last therapeutic approach in an acute life-threatening metabolic decompensation of propionic acidaemia. J Pediatr Endocrinol Metab. 2013;26(5–6):569–74.
Pinar-Sueiro S, et al. Optic neuropathy in methylmalonic acidemia: the role of neuroprotection. J Inherit Metab Dis. 2010;33 Suppl 3:S199–203.
Fragaki K, et al. Fatal heart failure associated with CoQ10 and multiple OXPHOS deficiency in a child with propionic acidemia. Mitochondrion. 2011;11(3):533–6.
Ha TS, Lee JS, Hong EJ. Delay of renal progression in methylmalonic acidemia using angiotensin II inhibition: a case report. J Nephrol. 2008;21(5):793–6.
Kelts DG, et al. Studies on requirements for amino acids in infants with disorders of amino acid metabolism. I. Effect of alanine. Pediatr Res. 1985;19(1):86–91.
Wolff JA, et al. Alanine decreases the protein requirements of infants with inborn errors of amino acid metabolism. J Neurogenet. 1985;2(1):41–9.
Marsden D, et al. Anabolic effect of human growth hormone: management of inherited disorders of catabolic pathways. Biochem Med Metab Biol. 1994;52(2):145–54.
Treacy E, et al. Glutathione deficiency as a complication of methylmalonic acidemia: response to high doses of ascorbate. J Pediatr. 1996;129(3):445–8.
Touati G, et al. Methylmalonic and propionic acidurias: management without or with a few supplements of specific amino acid mixture. J Inherit Metab Dis. 2006;29(2–3):288–98.
Jones S, et al. N-carbamylglutamate for neonatal hyperammonaemia in propionic acidaemia. J Inherit Metab Dis. 2008;31 Suppl 2:S219–22.
Filippi L, et al. N-carbamylglutamate in emergency management of hyperammonemia in neonatal acute onset propionic and methylmalonic aciduria. Neonatology. 2010;97(3):286–90.
Schwahn BC, et al. Biochemical efficacy of N-carbamylglutamate in neonatal severe hyperammonaemia due to propionic acidaemia. Eur J Pediatr. 2010;169(1):133–4.
Kasapkara CS, et al. N-carbamylglutamate treatment for acute neonatal hyperammonemia in isovaleric acidemia. Eur J Pediatr. 2011;170(6):799–801.
Abacan M, Boneh A. Use of carglumic acid in the treatment of hyperammonaemia during metabolic decompensation of patients with propionic acidaemia. Mol Genet Metab. 2013;109(4):397–401.
Matern D, et al. Primary treatment of propionic acidemia complicated by acute thiamine deficiency. J Pediatr. 1996;129(5):758–60.
Mayatepek E, Schulze A. Metabolic decompensation and lactic acidosis in propionic acidaemia complicated by thiamine deficiency. J Inherit Metab Dis. 1999;22(2):189–90.
Van Calcar SC, et al. Renal transplantation in a patient with methylmalonic acidaemia. J Inherit Metab Dis. 1998;21(7):729–37.
van’t Hoff WG, et al. Combined liver-kidney transplantation in methylmalonic acidemia. J Pediatr. 1998;132(6):1043–4.
Lubrano R, et al. Kidney transplantation in a girl with methylmalonic acidemia and end stage renal failure. Pediatr Nephrol. 2001;16(11):848–51.
Nagarajan S, et al. Management of methylmalonic acidaemia by combined liver-kidney transplantation. J Inherit Metab Dis. 2005;28(4):517–24.
Lubrano R, et al. Renal transplant in methylmalonic acidemia: could it be the best option? Report on a case at 10 years and review of the literature. Pediatr Nephrol. 2007;22(8):1209–14.
Mc Guire PJ, et al. Combined liver-kidney transplant for the management of methylmalonic aciduria: a case report and review of the literature. Mol Genet Metab. 2008;93(1):22–9.
Clothier JC, et al. Renal transplantation in a boy with methylmalonic acidaemia. J Inherit Metab Dis. 2011;34(3):695–700.
Yorifuji T, et al. Living-related liver transplantation for neonatal-onset propionic acidemia. J Pediatr. 2000;137(4):572–4.
Barshes NR, et al. Evaluation and management of patients with propionic acidemia undergoing liver transplantation: a comprehensive review. Pediatr Transplant. 2006;10(7):773–81.
Kasahara M, et al. Current role of liver transplantation for methylmalonic acidemia: a review of the literature. Pediatr Transplant. 2006;10(8):943–7.
Chen PW, et al. Stabilization of blood methylmalonic acid level in methylmalonic acidemia after liver transplantation. Pediatr Transplant. 2010;14(3):337–41.
Vara R, et al. Liver transplantation for propionic acidemia in children. Liver Transpl. 2011;17(6):661–7.
Brassier A, et al. Renal transplantation in 4 patients with methylmalonic aciduria: a cell therapy for metabolic disease. Mol Genet Metab. 2013;110(1–2):106–10.
Nagao M, et al. Improved neurologic prognosis for a patient with propionic acidemia who received early living donor liver transplantation. Mol Genet Metab. 2013;108(1):25–9.
Ou P, et al. A rare cause of cardiomyopathy in childhood: propionic acidosis. Three case reports. Arch Mal Coeur Vaiss. 2001;94(5):531–3.
Kasahara M, et al. Living-donor liver transplantation for propionic acidemia. Pediatr Transplant. 2012;16(3):230–4.
Chakrapani A, et al. Metabolic stroke in methylmalonic acidemia five years after liver transplantation. J Pediatr. 2002;140(2):261–3.
Nyhan WL, et al. Progressive neurologic disability in methylmalonic acidemia despite transplantation of the liver. Eur J Pediatr. 2002;161(7):377–9.
Arnold GL, et al. Methylcitrate/citrate ratio as a predictor of clinical control in propionic acidemia. J Inherit Metab Dis. 2003;26(suppl 2):37.
Zwickler T, et al. Metabolic decompensation in methylmalonic aciduria: which biochemical parameters are discriminative? J Inherit Metab Dis. 2012;35(5):797–806.
Zwickler T, et al. Usefulness of biochemical parameters in decision-making on the start of emergency treatment in patients with propionic acidemia. J Inherit Metab Dis. 2014;37(1):31–7.
Mountain States Genetics Regional Collaborative Propionic Acidemia: care plan & shared dataset. 2013. 21 Feb 2009 [cited 2014 Oct 2]; Available from: http://www.msgrcc.org/consortium/Propionic_Acidemia/PPA_revison.pdf
Surtees RA, Matthews EE, Leonard JV. Neurologic outcome of propionic acidemia. Pediatr Neurol. 1992;8(5):333–7.
Nicolaides P, Leonard J, Surtees R. Neurological outcome of methylmalonic acidaemia. Arch Dis Child. 1998;78(6):508–12.
O’Shea CJ, et al. Neurocognitive phenotype of isolated methylmalonic acidemia. Pediatrics. 2012;129(6):e1541–51.
Grünert SC, et al. Clinical and neurocognitive outcome in symptomatic isovaleric acidemia. Orphanet J Rare Dis. 2012;7:9.
van der Meer SB, et al. Clinical outcome of long-term management of patients with vitamin B12-unresponsive methylmalonic acidemia. J Pediatr. 1994;125(6 Pt 1):903–8.
Fischer AQ, et al. Cerebellar hemorrhage complicating isovaleric acidemia: a case report. Neurology. 1981;31(6):746–8.
Dave P, Curless RG, Steinman L. Cerebellar hemorrhage complicating methylmalonic and propionic acidemia. Arch Neurol. 1984;41(12):1293–6.
van der Meer SB, et al. Clinical outcome and long-term management of 17 patients with propionic acidaemia. Eur J Pediatr. 1996;155(3):205–10.
Ledley FD, et al. Benign methylmalonic aciduria. N Engl J Med. 1984;311(16):1015–8.
Treacy E, et al. Methylmalonic acidemia with a severe chemical but benign clinical phenotype. J Pediatr. 1993;122(3):428–9.
Grünert SC, et al. Propionic acidemia: neonatal versus selective metabolic screening. J Inherit Metab Dis. 2012;35(1):41–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Thomas, J.A. (2015). Organic Acidemias. In: Bernstein, L., Rohr, F., Helm, J. (eds) Nutrition Management of Inherited Metabolic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-14621-8_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-14621-8_17
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14620-1
Online ISBN: 978-3-319-14621-8
eBook Packages: MedicineMedicine (R0)