Abstract
Protocatechuic acid (PCA) and its precursor protocatechuic aldehyde (PCAL) are widely distributed polyphenols found in edible plants, fruits, and vegetables. PCA is the major human metabolite of cyanidin-glucosides derived from anthocyanins (ACN). Evidence suggests, that both PCA and PCAL influence the profile of the gut microbiota which contributes to the improvement of health benefits for humans. As agents used by plants in the self-defense, they have antibacterial and antiviral activity. Consumption of these substances is associated with lowered risk of some chronic conditions such as cardiovascular diseases. In aging-related states such as neurodegeneration, a reduction in amyloid deposition associated with Alzheimer’s disease was observed. Both PCA and PCAL have been shown to have antioxidant activity in vitro and in vivo, and beneficial effects in chronic inflammation. Both have been shown to be effective in cancer chemoprevention. The preventive effect of PCA in experimental models of the metabolic syndrome is of great importance, thanks to the antidiabetic effect and reducing obesity. PCA and PCAL show antiatherogenic activity; moreover, PCA acts as an anti-aggregating agent, reducing the risk of thrombosis. In preclinical studies, a beneficial effect of PCA in inhibiting osteoporosis has been found. It should be taken into account, that phenolic acids as dietary components, inter alia, show anticancer activity by reversing epigenetics-related changes, that lead to the activation of oncogenes and inactivation of suppressive genes.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Abbreviations
- 3-MT:
-
3-methoxy-4-hydroxyphenethylamine, 3-methoxytyramine
- ABCA1 :
-
ATP-binding cassette transporter A1
- ABCG1:
-
ATP-binding cassette transporter G1
- ACN:
-
Anthocyanins
- AGE:
-
Advanced glycation end products
- Akt (PKB):
-
Protein kinase B
- AMPK:
-
Adenosine 5′-monophosphate-activated protein kinase
- ANF:
-
Atrial natriuretic factor
- ApoE:
-
Apolipoprotein E
- ARE:
-
Antioxidant response element
- ATF:
-
Activating transcription factor
- Bak 1:
-
Bcl-2 homologous antagonist/killer
- Bax:
-
Apoptosis regulator BAX/bcl-2-like protein 4
- Bcl-2:
-
B-cell lymphoma 2
- Bcl-xL:
-
B-cell lymphoma-extra large
- BdNF :
-
Brain-derived neurotrophic factor
- C3G:
-
Cyanidin-3-O-β-glucoside
- Casp:
-
Caspase; cysteine-aspartic acid protease
- CAT:
-
Catalase
- CDK:
-
Cyclin-dependent kinase
- c-Fos:
-
Proto-oncogene c-Fos
- Cmax :
-
Maximum plasma concentration
- COMT:
-
Catechol-O-methyl transferase
- CREB:
-
cAMP-response element binding protein
- c-Src:
-
Proto-oncogene tyrosine-protein kinase Src
- DNA:
-
Deoxyribonucleic acid
- DNMT:
-
DNA methyltransferase
- GPx:
-
Glutathione peroxidase
- GSK:
-
Glycogen synthase kinase
- HDAC:
-
Histone deacetylase
- HMBG 1:
-
High-mobility group box 1 protein
- ICAM-1:
-
Intercellular adhesion molecule 1
- IRE1α:
-
Inositol-requiring enzyme 1 α
- JAK:
-
Janus kinase
- JNK:
-
c-Jun N-terminal kinase
- LC-MS-MS:
-
Liquid chromatography electrospray ionization tandem mass spectrometry
- LDH:
-
Lactic dehydrogenase
- LDL:
-
Low-density lipoprotein
- MAPK:
-
Mitogen-activated protein kinase
- MHCβ:
-
Major histocompatibility complex with β chain
- miRNA:
-
MicroRNA
- MPTP:
-
1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine
- mTOR:
-
Mechanistic target of rapamycin
- NFATc1:
-
Nuclear factor of activated T cells 1
- NFκB:
-
Nuclear factor kappa B
- NO:
-
Nitric oxide
- Nrf2:
-
Nuclear factor erythroid 2-related factor 2
- p27KIP1:
-
Cyclin-dependent kinase inhibitor
- p38:
-
MAPKp38 mitogen-activated protein kinase
- p65:
-
Transcription factor p65
- PARP:
-
Poly (ADP-ribose) polymerase
- PCA:
-
Protocatechuic acid
- PCAL:
-
Protocatechuic aldehyde
- PDGF:
-
Platelet-derived growth factor
- PERK:
-
Protein kinase R-like endoplasmic reticulum kinase
- PI3K:
-
Phosphatidylinositol 3-kinase
- PKC:
-
Protein kinase CRAGE
- PPAR-ϒ:
-
Peroxisome proliferator-activated receptor gamma
- PTX3:
-
Pentraxin-3
- RAGE:
-
Receptor for advanced glycation end products
- RANK:
-
Receptor activator of nuclear factor-κb
- RANKL:
-
Receptor activator of nuclear factor-κb ligand
- RCT:
-
Reverse cholesterol transport
- ROS:
-
Reactive oxygen species
- Sir 2:
-
Silent information regulator 2
- SIRT1:
-
NAD-dependent deacetylase sirtuin-1
- SLC7A5:
-
Large neutral amino acids transporter small subunit 1
- SOD:
-
Superoxide dismutase
- STAT:
-
Signal transducer and activator of transcription
- TNF-α:
-
Tumor necrosis factor alpha
- TRAF6:
-
Tumor necrosis factor receptor-associated factor 6
- TROLOX:
-
Equivalent antioxidant capacity
- α-SMA:
-
α-smooth muscle actin
References
Scalbert A, Manach C, Morand C, Remesy C (2005) Dietary polyphenols and the prevention of diseases. Crit Rev Food Sci Nutr 45:287–306
Williamson G, Manach C (2005) Bioavailability and bioefficacy of polyphenols in humans. II. Review of 93 intervention studies. Am J Clin Nutr 81:243S–255S
Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (2014) Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ:349:g4490. https://doi.org/10.1136/bmj.g4490. Erratum in: BMJ 2014;349:5472
Zhou Z, Liu Y, Miao AD, Wang SQ (2005) Protocatechuic aldehyde suppresses TNF-alpha-induced ICAM-1 and VCAM-1 expression in human umbilical vein endothelial cells. Eur J Pharmacol 513:1–8
Hu J, Webster D, Cao J, Shao A (2018) The safety of green tea and green tea extract consumption in adults – results of a systematic review. Regul Toxicol Pharmacol 95:412–433
García-Cortés M, Robles-Díaz M, Ortega-Alonso A, Medina-Caliz I, Andrade RJ (2016) Hepatotoxicity by dietary supplements: a tabular listing and clinical characteristics. Int J Mol Sci 17:537. https://doi.org/10.3390/ijms17040537
Roytman MM, Poerzgen P, Navarro V (2018) Botanicals and hepatotoxicity. Clin Pharmacol Ther 104:458–469
Satyanarayana U, Kumar AN, Naidu JN, Viswa Prasad DK (2014) Antioxidant supplementation for health – a boon or a bane? J NTR Univ Health Sci 3:221–230
Mursu J, Robien K, Harnack LJ, Park K, Jacobs DR Jr (2011) Dietary supplements and mortality rate in older women: the Iowa Women’s Health Study. Arch Intern Med 171:1625–1633
Bjelakovic G, Nikolova D, Gluud C (2014) Antioxidant supplements and mortality. Curr Opin Clin Nutr Metab Care 17:40–44. https://doi.org/10.1097/MCO.0000000000000009
Xu X, Liu A, Hu S, Ares I, Martínez-Larrañaga MR, Wang X, Martínez M, Anadón A, Martínez MA (2021) Synthetic phenolic antioxidants: metabolism, hazards and mechanism of action. Food Chem 353:129488. https://doi.org/10.1016/j.foodchem.2021.129488
Shen L, Ji HF, Zhang HY (2007) How to understand the dichotomy of antioxidants. Biochem Biophys Res Commun 362:543–545
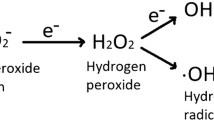
Milkovic L, Cipak Gasparovic A, Cindric M, Mouthuy PA, Zarkovic N (2019) Short overview of ROS as cell function regulators and their implications in therapy concepts. Cells 8:793. https://doi.org/10.3390/cells8080793
Ndhlala AR, Moyo M, Van Staden J (2010) Natural antioxidants: fascinating or mythical biomolecules? Molecules 15:6905–6930. https://doi.org/10.3390/molecules15106905
Tan BL, Norhaizan ME, Liew WP, Sulaiman Rahman H (2018) Antioxidant and oxidative stress: a mutual interplay in age-related diseases. Front Pharmacol 9:1162. https://doi.org/10.3389/fphar.2018.01162
Biswas SK (2016) Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid Med Cell Longev 2016:5698931. https://doi.org/10.1155/2016/5698931
Masella R, Santangelo C, D’Archivio M, Li Volti G, Giovannini C, Galvano F (2012) Protocatechuic acid and human disease prevention: biological activities and molecular mechanisms. Curr Med Chem 19:2901–2917
Kakkar S, Bais S (2014) A review on protocatechuic acid and its pharmacological potential. ISRN Pharmacol 2014:952943. https://doi.org/10.1155/2014/952943
Semaming Y, Pannengpetch P, Chattipakorn SC, Chattipakorn N (2015) Pharmacological properties of protocatechuic acid and its potential roles as complementary medicine. Evid Based Complement Alternat Med 2015:593902. https://doi.org/10.1155/2015/593902
Krzysztoforska K, Mirowska-Guzel D, Widy-Tyszkiewicz E (2017) Pharmacological effects of protocatechuic acid and its therapeutic potential in neurodegenerative diseases: review on the basis of in vitro and in vivo studies in rodents and humans. Nutr Neurosci 22:72–82
Song J, He Y, Luo C, Feng B, Ran F, Xu H, Ci Z, Xu R, Han L, Zhang D (2020) New progress in the pharmacology of protocatechuic acid: a compound ingested in daily foods and herbs frequently and heavily. Pharmacol Res 161:105109. https://doi.org/10.1016/j.phrs.2020.105109
Del Bo’ C, Bernardi S, Marino M, Porrini M, Tucci M, Guglielmetti S, Cherubini A, Carrieri B, Kirkup B, Kroon P, Zamora-Ros R, Liberona NH, Andres-Lacueva C, Riso P (2019) Systematic review on polyphenol intake and health outcomes: is there sufficient evidence to define a health-promoting polyphenol-rich dietary pattern? Nutrients 11:1355. https://doi.org/10.3390/nu11061355
Zamora-Ros R, Knaze V, Rothwell JA, Hémon B, Moskal A, Overvad K, Tjønneland A, Kyrø C, Fagherazzi G, Boutron-Ruault MC, Touillaud M, Katzke V, Kühn T, Boeing H, Förster J, Trichopoulou A, Valanou E, Peppa E, Palli D, Agnoli C, Ricceri F, Tumino R, de Magistris MS, Peeters PH, Bueno-de-Mesquita HB, Engeset D, Skeie G, Hjartåker A, Menéndez V, Agudo A, Molina-Montes E, Huerta JM, Barricarte A, Amiano P, Sonestedt E, Nilsson LM, Landberg R, Key TJ, Khaw KT, Wareham NJ, Lu Y, Slimani N, Romieu I, Riboli E, Scalbert A (2016) Dietary polyphenol intake in Europe: the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Eur J Nutr 55:1359–1375
McGhie TK, Walton MC (2007) The bioavailability and absorption of anthocyanins: towards a better understanding. Mol Nutr Food Res 51:702–713
Manach C, Scalbert A, Morand C, Rémésy C, Jiménez L (2004) Polyphenols—food sources and bioavailability. Am J Clin Nutr 79:727–747
Liu C, Wang W, Lin W, Ling W, Wang D (2016) Established atherosclerosis might be a prerequisite for chicory and its constituent protocatechuic acid to promote endothelium-dependent vasodilation in mice. Mol Nutr Food Res 60:2141–2150
Rashmi HB, Negi PS (2020) Phenolic acids from vegetables: a review on processing stability and health benefits. Food Res Int 136:109298. https://doi.org/10.1016/j.foodres.2020.109298
Juurlink BH, Azouz HJ, Aldalati AM, AlTinawi BMH, Ganguly P (2014) Hydroxybenzoic acid isomers and the cardiovascular system. Nutr J 13:63. https://doi.org/10.1186/1475-2891-13-63
Rossetto M, Lante A, Vanzani P, Spettoli P, Scarpa M, Rigo A (2005) Red chicories as potent scavengers of highly reactive radicals: a study on their phenolic composition and peroxyl radical trapping capacity and efficiency. J Agric Food Chem 53:8169–8175
Buda V, Brezoiu AM, Berger D, Pavel IZ, Muntean D, Minda D, Dehelean CA, Soica C, Diaconeasa Z, Folescu R, Danciu C (2020) Biological evaluation of black chokeberry extract free and embedded in two mesoporous silica-type matrices. Pharmaceutics 12:838. https://doi.org/10.3390/pharmaceutics12090838
Boskou G, Salta FN, Chrysostomou S, Mylona A, Chiou A, Andrikopoulos NK (2006) Antioxidant capacity and phenolic profile of table olives from the Greek market. Food Chem 94:558–564
Takahama U, Oniki T, Hirota S (2001) Phenolic components of brown scales of onion bulbs produce hydrogen peroxide by autooxidation. J Plant Res 114:395–402
Barros L, Duenas M, Ferreira IC, Baptista P, Santos-Buelga C (2009) Phenolic acids determination by HPLC-DAD-ESI/MS in sixteen different Portuguese wild mushrooms species. Food Chem Toxicol 47:1076–1079
Sarikurkcu C, Locatelli M, Tartaglia A, Ferrone V, Juszczak AM, Ozer MS, Tepe B, Tomczyk M (2020) Enzyme and biological activities of the water extracts from the plants Aesculus hippocastanum, Olea europaea and Hypericum perforatum that are used as folk remedies in Turkey. Molecules 5:1202. https://doi.org/10.3390/molecules25051202
Wu X, Pittman HE III, Hager T, Hager A, Howard L, Prior RL (2009) Phenolic acids in black raspberry and in the gastrointestinal tract of pigs following ingestion of black raspberry. Mol Nutr Food Res 53(Suppl 1):S76–S84
Hiemori M, Koh E, Mitchell AE (2009) Influence of cooking on anthocyanins in black rice (Oryza sativa L. japonica var. SBR). J Agric Food Chem 5:1908–1914
Aalim H, Luo Z (2021) Insight into rice (Oryza sativa L.) cooking: phenolic composition, inhibition of α-amylase and α-glucosidase, and starch physicochemical and functional properties. Food Biosci 40:100917. https://doi.org/10.1016/j.fbio.2021.100917
Pojer E, Mattivi F, Johnson D, Stockley CS (2013) The case for anthocyanin consumption to promote human health: a review. CRFSFS 12:483–508
Speciale A, Cimino F, Saija A, Canali R, Virgili F (2014) Bioavailability and molecular activities of anthocyanins as modulators of endothelial function. Genes Nutr 9:404. https://doi.org/10.1007/s12263-014-0404-8
Del Rio D, Costa LG, Lean ME, Crozier A (2010) Polyphenols and health: what compounds are involved? Nutr Metab Cardiovasc Dis 20:1–6
Man AWC, Zhou Y, Xia N, Li H (2020) Involvement of gut microbiota, microbial metabolites and interaction with polyphenol in host immunometabolism. Nutrients 12:3054. https://doi.org/10.3390/nu12103054
Manolescu BN, Oprea E, Mititelu M, Ruta LL, Farcasanu IC (2019) Dietary anthocyanins and stroke: a review of pharmacokinetic and pharmacodynamic studies. Nutrients 11:1479. https://doi.org/10.3390/nu11071479
de Ferrars RM, Czank C, Zhang Q, Botting NP, Kroon PA, Cassidy A, Kay CD (2014) The pharmacokinetics of anthocyanins and their metabolites in humans. Br J Pharmacol 171:3268–3282
Sun YJ, Huang QQ, Li P, Zhang JJ (2015) Catalytic dioxygenation of flavonol by M(II)-complexes (M = Mn, Fe, Co, Ni, Cu and Zn) – mimicking the M(II)-substituted quercetin 2,3-dioxygenase. Dalton Trans 2015(44):13926–11338
Rodriguez-Mateos A, Vauzour D, Krueger CG, Shanmuganayagam D, Reed J, Calani L, Mena P, Del Rio D, Crozier A (2014) Bioavailability, bioactivity and impact on health of dietary flavonoids and related compounds: an update. Arch Toxicol 88:1803–1853
Czank C, Cassidy A, Zhang Q, Morrison DJ, Preston T, Kroon P, Botting NP, Kay CD (2013) Human metabolism and elimination of the anthocyanin, cyanidin-3-glucoside: a 13C-tracer study. Am J Clin Nutr 97(995):1003
Fang J (2014) Some anthocyanins could be efficiently absorbed across the gastrointestinal mucosa: extensive presystemic metabolism reduces apparent bioavailability. J Agric Food Chem 62:3904–3911
Han Y, Xiong Z, Yang C, Liu M, Li F (2007) Determination of protocatechuic acid in rat plasma by high performance liquid chromatography. Se Pu 25:207–210
Tsuda T, Horio F, Osawa T (1999) Absorption and metabolism of cyanidin 3-O-beta-D-glucoside in rats. FEBS Lett 449:179–182
Vitaglione P, Donnarumma G, Napolitano A, Galvano F, Gallo A, Scalfi L, Fogliano V (2007) Protocatechuic acid is the major human metabolite of cyanidin-glucosides. J Nutr 137:2043–2048
Koli R, Erlund I, Jula A, Marniemi J, Mattila P, Alfthan G (2010) Bioavailability of various polyphenols from a diet containing moderate amounts of berries. J Agric Food Chem 58:3927–3932
Mazza G, Kay CD, Cottrell T, Holub BJ (2002) Absorption of anthocyanins from blueberries and serum antioxidant status in human subjects. J Agric Food Chem 50:7731–7737
Galvano F, Vitaglione P, Li Volti G, Di Giacomo C, Gazzolo D, Vanella L, La Fauci L, Fogliano V (2008) Protocatechuic acid: the missing human cyanidins’ metabolite. Mol Nutr Food Res 52:386–387
Pietta PG, Simonetti P, Gardana C, Brusamolino A, Morazzoni P, Bombardelli E (1998) Catechin metabolites after intake of green tea infusions. Biofactors 8:111–118
Nozaki A, Kimura T, Ito H, Hatano T (2009) Interaction of polyphenolic metabolites with human serum albumin: a circular dichroism study. Chem Pharm Bull (Tokyo) 57:1019–1023
Hanske L, Engst W, Loh G, Sczesny S, Blaut M, Braune A (2013) Contribution of gut bacteria to the metabolism of cyanidin 3-glucoside in human microbiota-associated rats. Br J Nutr 109:1433–1441
Braga ARC, de Souza Mesquita LM, Martins PLR, Habu S, Rosso VV (2018) Lactobacillus fermentation of jussara pulp leads to the enzymatic conversion of anthocyanins increasing antioxidant activity. J Food Compos Anal 69:162–170
Keppler K, Humpf HU (2005) Metabolism of anthocyanins and their phenolic degradation products by the intestinal microflora. Bioorg Med Chem 13:5195–5205
Wang D, Xia M, Yan X, Li D, Wang L, Xu Y, Jin T, Ling W (2012) Gut microbiota metabolism of anthocyanin promotes reverse cholesterol transport in mice via repressing miRNA-10b. Circ Res 111:967–981
Lin CY, Tsai SJ, Huang CS, Yin MC (2011) Antiglycative effects of protocatechuic acid in the kidneys of diabetic mice. J Agric Food Chem 59:5117–5124
Wang X, Yan K, Ma X, Li W, Chu Y, Guo J, Li S, Zhou S, Zhu Y, Liu C (2016) Simultaneous determination and pharmacokinetic study of protocatechuic aldehyde and its major active metabolite protocatechuic acid in rat plasma by liquid chromatography-tandem mass spectrometry. J Chromatogr Sci 54:697–705
Farombi EO, Adedara IA, Awoyemi OV, Njoku CR, Micah GO, Esogwa CU, Owumi SE, Olopade JO (2016) Dietary protocatechuic acid ameliorates dextran sulphate sodium-induced ulcerative colitis and hepatotoxicity in rats. Food Funct 7:913–921
Tian X, Schaich KM (2013) Effects of molecular structure on kinetics and dynamics of the Trolox equivalent antioxidant capacity assay with ABTS. J Agric Food Chem 61:5511–5519
Li X, Wang X, Chen D, Chen S (2011) Antioxidant activity and mechanism of protocatechuic acid in vitro. Funct Food Health Dis 7:232–244
Galano A, Pérez-González A (2012) On the free radical scavenging mechanism of protocatechuic acid, regeneration of the catechol group in aqueous solution. Theor Chem Acc 131:1–13
Ueda J, Saito N, Shimazu Y, Ozawa T (1996) A comparison of scavenging abilities of antioxidants against hydroxyl radicals. Arch Biochem Biophys 333:377–384
Zhang Z, Li G, Szeto SSW, Chong CM, Quan Q, Huang C, Cui W, Guo B, Wang Y, Han Y, Michael Siu KW, Yuen Lee SM, Chu IK (2015) Examining the neuroprotective effects of protocatechuic acid and chrysin on in vitro and in vivo models of Parkinson disease. Free Radic Biol Med 84:331–343
Yin X, Zhang X, Lv C, Li C, Yu Y, Wang X, Han F (2015) Protocatechuic acid ameliorates neurocognitive functions impairment induced by chronic intermittent hypoxia. Sci Rep 5:14507. https://doi.org/10.1038/srep14507
Ma L, Wang G, Chen Z, Li Z, Yao J, Zhao H, Wang S, Ma Z, Chang H, Tian X (2014) Modulating the p66shc signaling pathway with protocatechuic acid protects the intestine from ischemia reperfusion injury and alleviates secondary liver damage. Sci World J 2014:387640. https://doi.org/10.1155/2014/387640
Cheng YT, Lin JA, Jhang JJ, Yen GC (2019) Protocatechuic acid-mediated DJ-1/PARK7 activation followed by PI3K/mTOR signaling pathway activation as a novel mechanism for protection against ketoprofen-induced oxidative damage in the gastrointestinal mucosa. Free Radic Biol Med 130:35–47
Crespo I, San-Miguel B, Mauriz JL, Ortiz de Urbina JJ, Almar M, Tuñón MJ, González-Gallego J (2017) Protective effect of protocatechuic acid on TNBS-induced colitis in mice is associated with modulation of the SphK/S1P signaling pathway. Nutrients 9:288. https://doi.org/10.3390/nu9030288
Safaeian L, Emami R, Hajhashemi V, Haghighatian Z (2018) Antihypertensive and antioxidant effects of protocatechuic acid in deoxycorticosterone acetate-salt hypertensive rats. Biomed Pharmacother 100:147–155
Lende AB, Kshirsagar AD, Deshpande AD, Muley MM, Patil RR, Bafna PA, Naik SR (2011) Anti-inflammatory and analgesic activity of protocatechuic acid in rats and mice. Inflammopharmacology 19:255–263
Varì R, D’Archivio M, Filesi C, Carotenuto S, Scazzocchio B, Santangelo C, Giovannini C, Masella R (2011) Protocatechuic acid induces antioxidant/detoxifying enzyme expression through JNK-mediated Nrf2 activation in murine macrophages. J Nutr Biochem 22:409–417
Mandalari G, Bisignano C, D’Arrigo M, Ginestra G, Arena A, Tomaino A, Wickham MS (2010) Antimicrobial potential of polyphenols extracted from almond skins. Lett Appl Microbiol 51:83–89
Jalali O, Best M, Wong A, Schaeffer B, Bauer B, Johnson L (2020) Protocatechuic acid as a topical antimicrobial for surgical skin antisepsis. JBJS Open Access 5:e19.00079. https://doi.org/10.2106/JBJS.OA.19.00079
Jalali O, Best M, Wong A, Schaeffer B, Bauer B, Johnson L (2020) Reduced bacterial burden of the skin surrounding the shoulder joint following topical protocatechuic acid application. JBJS Open Access 5:e19.00078. https://doi.org/10.2106/JBJS.OA.19.00078
Alvarado-Martinez Z, Bravo P, Kennedy N-F, Krishna M, Hussain S, Young AC, Biswas D (2020) Antimicrobial and antivirulence impacts of phenolics on Salmonella enterica serovar typhimurium. Antibiotics 9:668. https://doi.org/10.3390/antibiotics9100668
Bernal-Mercado AT, Gutierrez-Pacheco MM, Encinas-Basurto D, Mata-Haro V, Lopez-Zavala AA, Islas-Osuna MA, Gonzalez-Aguilar GA, Ayala-Zavala JF (2020) Synergistic mode of action of catechin, vanillic and protocatechuic acids to inhibit the adhesion of uropathogenic Escherichia coli on silicone surfaces. J Appl Microbiol 128:387–400
Srivastava N, Tiwari S, Bhandari K, Biswal AK, Rawat AKS (2020) Novel derivatives of plant monomeric phenolics: act as inhibitors of bacterial cell-to-cell communication. Microb Pathog 141:103856. https://doi.org/10.1016/j.micpath.2019.103856
Wu S, Wang Q, Wang J, Duan B, Tang Q, Sun Z, Han J, Shan C, Wang Z, Hao Z (2020) Protocatechuic aldehyde from Salvia miltiorrhiza exhibits an anti-inflammatory effect through inhibiting MAPK signalling pathway. BMC Complement Med Ther 20:347. https://doi.org/10.1186/s12906-020-03090-4
de Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, Serrazanetti DI, Di Cagno R, Ferrocino I, Lazzi C, Turroni S, Cocolin L, Brigidi P, Neviani E, Gobbetti M, O’Toole PW, Ercolini D (2016) High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 65:1812–1821
Zhu B, Wang X, Li L (2010) Human gut microbiome: the second genome of human body. Protein Cell 1:718–725
Duda-Chodak A, Tarko T, Satora P, Sroka P (2015) Interaction of dietary compounds, especially polyphenols, with the intestinal microbiota: a review. Eur J Nutr 54:325–341
Cassidy A, Minihane AM (2017) The role of metabolism (and the microbiome) in defining the clinical efficacy of dietary flavonoids. Am J Clin Nutr 105:10–22
Hair R, Sakaki JR, Chun OK (2021) Anthocyanins, microbiome and health benefits in aging. Molecules 26:537. https://doi.org/10.3390/molecules26030537
Hervert-Hernandez D, Goni I (2011) Dietary polyphenols and human gut microbiota: a review. Food Rev Int 27:154–169
Hidalgo M, Oruna-Concha MJ, Kolida S, Walton GE, Kallithraka S, Spencer JP, de Pascual-Teresa S (2012) Metabolism of anthocyanins by human gut microflora and their influence on gut bacterial growth. J Agric Food Chem 60:3882–3890
Igwe EO, Charlton KE, Probst YC, Kent K, Netzel ME (2019) A systematic literature review of the effect of anthocyanins on gut microbiota populations. J Hum Nutr Diet 32:53–62
Ho L, Zhao D, Ono K, Ruan K, Mogno I, Tsuji M, Carry E, Brathwaite J, Sims S, Frolinger T, Westfall S, Mazzola P, Wu Q, Hao K, Lloyd TE, Simon JE, Faith J, Pasinetti GM (2019) Heterogeneity in gut microbiota drive polyphenol metabolism that influences α-synuclein misfolding and toxicity. J Nutr Biochem 64:170–181
Morais CA, de Rosso VV, Estadella D, Pisani LP (2016) Anthocyanins as inflammatory modulators and the role of the gut microbiota. J Nutr Biochem 33:1–7
Lee S, Keirsey KI, Kirkland R, Grunewald ZI, Fischer JG, de La Serre CB (2018) Blueberry supplementation influences the gut microbiota, inflammation, and insulin resistance in High-Fat-Diet-Fed rats. J Nutr 148:209–219
Ajiboye TO, Habibu RS, Saidu K, Haliru FZ, Ajiboye HO, Aliyu NO, Ibitoye OB, Uwazie JN, Muritala HF, Bello SA, Yusuf II, Mohammed AO (2017) Involvement of oxidative stress in protocatechuic acid-mediated bacterial lethality. Microbiol Open 6:e00472. https://doi.org/10.1002/mbo3.472
Ozdal T, Sela DA, Xiao J, Boyacioglu D, Chen F, Capanoglu E (2016) The reciprocal interactions between polyphenols and gut microbiota and effects on bioaccessibility. Nutrients 8:78. https://doi.org/10.3390/nu8020078
Stevens JF, Maier CS (2016) The chemistry of gut microbial metabolism of polyphenols. Phytochem Rev 15:425–444
Jenner AM, Rafter J, Halliwell B (2005) Human fecal water content of phenolics: the extent of colonic exposure to aromatic compounds. Free Radic Biol Med 38:763–772
Lee YM, Yoon Y, Yoon H, Park HM, Song S, Yeum KJ (2017) Dietary anthocyanins against obesity and inflammation. Nutrients 9:1089. https://doi.org/10.3390/nu9101089
Jeong JB, Lee SH (2013) Protocatechualdehyde possesses anti-cancer activity through downregulating cyclin D1 and HDAC2 in human colorectal cancer cells. Biochem Biophys Res Commun 430:381–386
Lee JR, Lee MH, Eo HJ, Park GH, Song HM, Kim MK, Lee JW, Jeong JB (2014) The contribution of activating transcription factor 3 to apoptosis of human colorectal cancer cells by protocatechualdehyde, a naturally occurring phenolic compound. Arch Biochem Biophys 564:203–210. https://doi.org/10.1016/j.abb.2014.10.005
Choi J, Jiang X, Jeong JB, Lee SH (2014) Anticancer activity of protocatechualdehyde in human breast cancer cells. J Med Food 17:842–848
Zhong S, Li YG, Ji DF, Lin TB, Lv ZQ (2016) Protocatechualdehyde induces S-phase arrest and apoptosis by stimulating the p27(KIP1)-cyclin A/D1-CDK2 and mitochondrial apoptotic pathways in HT-29 cells. Molecules 21:934. https://doi.org/10.3390/molecules21070934
Sankaranarayanan R, Valiveti CK, Kumar DR, Van Slambrouck S, Kesharwani SS, Seefeldt T, Scaria J, Tummala H, Bhat GJ (2019) The flavonoid metabolite 2,4,6-trihydroxybenzoic acid is a CDK inhibitor and an anti-proliferative agent: a potential role in cancer prevention. Cancers (Basel) 11:427. https://doi.org/10.3390/cancers11030427
GBD 2017 Diet Collaborators (2019) Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 393:1958–1972
Habtemariam S, Varghese GK (2014) The antidiabetic therapeutic potential of dietary polyphenols. Curr Pharm Biotechnol 15:391–400
Jamar G, Estadella D, Pisani LP (2017) Contribution of anthocyanin-rich foods in obesity control through gut microbiota interactions. Biofactors 43:507–516
Lee YM, Yoon Y, Yoon H, Park HM, Song S, Yeum KJ (2017) Dietary anthocyanins against obesity and inflammation. Nutrients 9:1089. https://doi.org/10.3390/nu9101089
Adedara IA, Fasina OB, Ayeni MF, Ajayi OM, Farombi EO (2019) Protocatechuic acid ameliorates neurobehavioral deficits via suppression of oxidative damage, inflammation, caspase-3 and acetylcholinesterase activities in diabetic rats. Food Chem Toxicol 125:170–181
Alegbe EO, Teralı K, Olofinsan KA, Surgun S, Ogbaga CC, Ajiboye TO (2019) Antidiabetic activity-guided isolation of gallic and protocatechuic acids from Hibiscus sabdariffa calyxes. J Food Biochem 43:e12927. https://doi.org/10.1111/jfbc.12927
Tagliazucchi D, Martini S, Conte A (2019) Protocatechuic and 3,4-dihydroxyphenylacetic acids inhibit protein glycation by binding lysine through a metal-catalyzed oxidative mechanism. J Agric Food Chem 67:7821–7831
Jia Y, Wu C, Kim YS, Yang SO, Kim Y, Kim J-S, Jeong M-Y, Lee JH, Kim B, Lee S, Kim J, Oh H-S, So M-Y, Yoon YE, Thach TT, Park TH, Lee S-J (2020) A dietary anthocyanin cyanidin-3-O-glucoside binds to PPARs to regulate glucose metabolism and insulin sensitivity in mice. Commun Biol 3:514. https://doi.org/10.1038/s42003-020-01231-6
Scazzocchio B, Varì R, Filesi C, D’Archivio M, Santangelo C, Giovannini C, Iacovelli A, Silecchia G, Li Volti G, Galvano F, Masella R (2011) Cyanidin-3-O-β-glucoside and protocatechuic acid exert insulin-like effects by upregulating PPARγ activity in human omental adipocytes. Diabetes 60:2234–2244
Scazzocchio B, Varì R, Filesi C, Del Gaudio I, D’Archivio M, Santangelo C, Iacovelli A, Galvano F, Pluchinotta FR, Giovannini C, Masella R (2015) Protocatechuic acid activates key components of insulin signaling pathway mimicking insulin activity. Mol Nutr Food Res 59:1472–1481
Leyva-Jiménez FJ, Ruiz-Malagón AJ, Molina-Tijeras JA, Diez-Echave P, Vezza T, Hidalgo-García L, Lozano-Sánchez J, Arráez-Román D, Cenis JL, Lozano-Pérez AA, Rodríguez-Nogales A, Segura-Carretero A, Gálvez J (2020) Comparative study of the antioxidant and anti-inflammatory effects of leaf extracts from four different Morus alba genotypes in high fat diet-induced obesity in mice. Antioxidants (Basel) 9:733. https://doi.org/10.3390/antiox9080733
Wang YH, Han YP, Yu HT, Pu XP, Du GH (2014) Protocatechualdehyde prevents methylglyoxal-induced mitochondrial dysfunction and AGEs-RAGE axis activation in human lens epithelial cells. Eur J Pharmacol 738:374–383
Grzelak-Błaszczyk K, Milala J, Kołodziejczyk K, Sójka M, Czarnecki A, Kosmala M, Klewicki R, Fotschki B, Jurgoński A, Juśkiewicz J (2020) Protocatechuic acid and quercetin glucosides in onions attenuate changes induced by high fat diet in rats. Food Funct 11:3585–3597
Li L, Liu S, Tang H, Song S, Lu L, Zhang P, Li X (2020) Effects of protocatechuic acid on ameliorating lipid profiles and cardio-protection against coronary artery disease in high fat and fructose diet fed in rats. J Vet Med Sci 82:1387–1394
Moon CY, Ku CR, Cho YH, Lee EJ (2012) Protocatechuic aldehyde inhibits migration and proliferation of vascular smooth muscle cells and intravascular thrombosis. Biochem Biophys Res Commun 423:116–121
Zhou Z, Liu Y, Miao AD, Wang SQ (2005) Protocatechuic aldehyde suppresses TNF-alpha-induced ICAM-1 and VCAM-1 expression in human umbilical vein endothelial cells. Eur J Pharmacol 513:1–8
Wang D, Wei X, Yan X, Jin T, Ling W (2010) Protocatechuic acid, a metabolite of anthocyanins, inhibits monocyte adhesion and reduces atherosclerosis in apolipoprotein E-deficient mice. J Agric Food Chem 58:12722–12728
Wang D, Zou T, Yang Y, Yan X, Ling W (2011) Cyanidin-3-O-β-glucoside with the aid of its metabolite protocatechuic acid, reduces monocyte infiltration in apolipoprotein E-deficient mice. Biochem Pharmacol 82:713–719
Liu Y, Wang X, Pang J, Zhang H, Luo J, Qian X, Chen Q, Ling W (2019) Attenuation of atherosclerosis by protocatechuic acid via inhibition of M1 and promotion of M2 macrophage polarization. J Agric Food Chem 67:807–818
Lin MC, Ou TT, Chang CH, Chan KC, Wang CJ (2015) Protocatechuic acid inhibits oleic acid-induced vascular smooth muscle cell proliferation through activation of AMP-activated protein kinase and cell cycle arrest in G0/G1 phase. J Agric Food Chem 63:235–241
Zheng J, Li Q, He L, Weng H, Su D, Liu X, Ling W, Wang D (2020) Protocatechuic acid inhibits vulnerable atherosclerotic lesion progression in older Apoe−/−mice. J Nutr 150:1167–1177
Xiao G, Zhang M, Peng X, Jiang G (2021) Protocatechuic acid attenuates cerebral aneurysm formation and progression by inhibiting TNF-alpha/Nrf-2/NF-kB-mediated inflammatory mechanisms in experimental rats. Open Life Sci 16:128–141
Wei G, Guan Y, Yin Y, Duan J, Zhou D, Zhu Y, Quan W, Xi M, Wen A (2013) Anti-inflammatory effect of protocatechuic aldehyde on myocardial ischemia/reperfusion injury in vivo and in vitro. Inflammation 36:592–602
Guo C, Wang S, Duan J, Jia N, Zhu Y, Ding Y, Guan Y, Wei G, Yin Y, Xi M, Wen A (2017) Protocatechualdehyde protects against cerebral ischemia-reperfusion-induced oxidative injury via protein kinase C epsilon/Nrf2/HO-1 pathway. Mol Neurobiol 54:833–845
Kale S, Sarode LP, Kharat A, Ambulkar S, Prakash A, Sakharkar AJ, Ugale RR (2021) Protocatechuic acid prevents early hour ischemic reperfusion brain damage by restoring imbalance of neuronal cell death and survival proteins. J Stroke Cerebrovasc Dis 30:102207. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105507
Fang X, Liu Y, Lu J, Hong H, Yuan J, Zhang Y, Wang P, Liu P, Ye J (2018) Protocatechuic aldehyde protects against isoproterenol-induced cardiac hypertrophy via inhibition of the JAK2/STAT3 signaling pathway. Naunyn Schmiedeberg’s Arch Pharmacol 391:1373–1385
Wan YJ, Guo Q, Liu D, Jiang Y, Zeng KW, Tu PF (2019) Protocatechualdehyde reduces myocardial fibrosis by directly targeting conformational dynamics of collagen. Eur J Pharmacol 855:183–191
Wan YJ, Wang YH, Guo Q, Jiang Y, Tu PF, Zeng K-W (2020) Protocatechualdehyde protects oxygen-glucose deprivation/reoxygenation-induced myocardial injury via inhibiting PERK/ATF6α/IRE1α pathway. Eur J Pharmacol. https://doi.org/10.1016/j.ejphar.2020.173723
Kim K, Bae ON, Lim KM, Noh JY, Kang S, Chung KY, Chung JH (2012) Novel antiplatelet activity of protocatechuic acid through the inhibition of high shear stress-induced platelet aggregation. J Pharmacol Exp Ther 343:704–711
Ngo T, Kim K, Bian Y, Nam G, Park HJ, Lee K, Cho GS, Ryu JM, Lim KM, Chung JH (2020) Antithrombotic effect of SP-8008, a benzoic acid derivative, through the selective inhibition of shear stress-induced platelet aggregation. Br J Pharmacol 177:929–944
Muley MM, Thakare VN, Patil RR, Bafna PA, Naik SR (2013) Amelioration of cognitive, motor and endogenous defense functions with silymarin, piracetam and protocatechuic acid in the cerebral global ischemic rat model. Life Sci 93:51–57
Kho AR, Choi BY, Lee SH, Hong DK, Lee SH, Jeong JH, Park KH, Song HK, Choi HC, Suh SW (2018) Effects of protocatechuic acid (PCA) on global cerebral ischemia-induced hippocampal neuronal death. Int J Mol Sci 19:1420. https://doi.org/10.3390/ijms19051420
Kangtao Y, Bais S (2018) Neuroprotective effect of protocatechuic acid through MAO-B inhibition in aluminium chloride induced dementia of Alzheimer’s type in rats. Int J Pharmacol 14:879–888
Krzysztoforska K, Piechal A, Blecharz-Klin K, Pyrzanowska J, Joniec-Maciejak I, Mirowska-Guzel D, Widy-Tyszkiewicz E (2019) Administration of protocatechuic acid affects memory and restores hippocampal and cortical serotonin turnover in rat model of oral D-galactose-induced memory impairment. Behav Brain Res 368:111896. https://doi.org/10.1016/j.bbr.2019.04.010
Krzysztoforska K, Piechal A, Blecharz-Klin K, Pyrzanowska J, Joniec-Maciejak I, Mirowska-Guzel D, Widy-Tyszkiewicz E (2020) Effect of protocatechuic acid on cognitive processes and central nervous system neuromodulators in the hippocampus, prefrontal cortex, and striatum of healthy rats. Nutr Neurosci 21:1–12. https://doi.org/10.1080/1028415X.2020.1859728
Scalise M, Galluccio M, Console L, Pochini L, Indiveri C, The Human SLC7A5 (LAT1) (2018) The intriguing histidine/large neutral amino acid transporter and its relevance to human health. Front Chem 6:243. https://doi.org/10.3389/fchem.2018.00243
Kim YS, Seo HW, Lee MH, Kim DK, Jeon H, Cha DS (2014) Protocatechuic acid extends lifespan and increases stress resistance in Caenorhabditis elegans. Arch Pharm Res 37:245–252
Dilberger B, Passon M, Asseburg H, Silaidos CV, Schmitt F, Schmiedl T, Schieber A, Eckert GP (2019) Polyphenols and metabolites enhance survival in rodents and nematodes-impact of mitochondria. Nutrients 11:1886. https://doi.org/10.3390/nu11081886
Dilberger B, Weppler S, Eckert GP (2020) Impact of phenolic acids on the energy metabolism and longevity in C. elegans. bioRxiv. https://doi.org/10.1101/2020.06.23.166314
Sunthonkun P, Palajai R, Somboon P, Suan CL, Ungsurangsri M, Soontorngun N (2019) Life-span extension by pigmented rice bran in the model yeast Saccharomyces cerevisiae. Sci Rep 9:18061. https://doi.org/10.1038/s41598-019-54448-9
Ojeda-Rodríguez A, Zazpe I, Alonso-Pedrero L, Zalba G, Martínez-González MA, Marti A (2020) Higher adherence to an empirically derived Mediterranean dietary pattern is positively associated with telomere length: the Seguimiento Universidad de Navarra (SUN) project. Br J Nutr 124:1–10
Choi JR, Kim JH, Lee S, Cho EJ, Kim HY (2020) Protective effects of protocatechuic acid against cognitive impairment in an amyloid beta-induced Alzheimer’s disease mouse model. Food Chem Toxicol 144:111571. https://doi.org/10.1016/j.fct.2020.111571
Huang L, Zhong X, Qin S, Deng M (2020) Protocatechuic acid attenuates β secretase activity and okadaic acid induced autophagy via the Akt/GSK 3β/MEF2D pathway in PC12 cells. Mol Med Rep 21:1328–1335
Rahman MA, Rahman MS, Rahman MH, Rasheduzzaman M, Mamun-Or-Rashid A, Uddin MJ, Rahman MR, Hwang H, Pang MG, Rhim H (2021) Modulatory effects of autophagy on APP processing as a potential treatment target for Alzheimer’s disease. Biomedicines 9:5. https://dx.doi.org/10.3390
Shi S-h, Zhao X, Liu A, Liu B, Li H, Wu B, K-s B, Jia Y (2015) Protective effect of n-butanol extract from Alpinia oxyphylla on learning and memory impairments. Physiol Behav 139:13–20
Li J, Du Q, Li N, Du S, Sun Z (2020) Alpiniae oxyphyllae fructus and Alzheimer’s disease: an update and current perspective on this traditional Chinese medicine. Biomed Pharmacother 135:111167. https://doi.org/10.1016/j.biopha.2020.111167
Wang Y, Wang M, Fan K, Li T, Yan T, Wu B, Bi K, Jia Y (2018) Protective effects of Alpiniae oxyphyllae fructus extracts on lipopolysaccharide-induced animal model of Alzheimer’s disease. J Ethnopharmacol 217:98–106
Wu T, Fang X, Xu J, Jiang Y, Cao F, Zhao L (2020) Synergistic effects of ginkgolide B and protocatechuic acid on the treatment of Parkinson’s disease. Molecules 25:3976. https://doi.org/10.3390/molecules25173976
Koza LA, Winter AN, Holsopple J, Baybayon-Grandgeorge AN, Pena C, Olson JR, Mazzarino RC, Patterson D, Linseman DA (2020) Protocatechuic acid extends survival, improves motor function, diminishes gliosis, and sustains neuromuscular junctions in the hSOD1G93A mouse model of amyotrophic lateral sclerosis. Nutrients 12:1824. https://doi.org/10.3390/nu12061824
Kaewmool C, Udomruk S, Phitak T, Pothacharoen P, Kongtawelert P (2020a) Cyanidin-3-O-glucoside protects PC12 cells against neuronal apoptosis mediated by LPS-stimulated BV2 microglial activation. Neurotox Res 37:111–125
Yan J, Luo A, Gao J, Tang X, Zhao Y, Zhou B, Zhou Z, Li S (2019) The role of SIRT1 in neuroinflammation and cognitive dysfunction in aged rats after anesthesia and surgery. Am J Transl Res 11:1555–1568
Li Q, Verma IM (2002) NF-kappaB regulation in the immune system. Nat Rev Immunol 2:725–734
Kaewmool C, Kongtawelert P, Phitak T, Pothacharoen P, Udomruk S (2020b) Protocatechuic acid inhibits inflammatory responses in LPS-activated BV2 microglia via regulating SIRT1/NF-κB pathway contributed to the suppression of microglial activation-induced PC12 cell apoptosis. J Neuroimmunol 341:577164. https://doi.org/10.1016/j.jneuroim.2020.577164
Kargar Shouroki F, Neghab M, Mozdarani H, Alipour H, Yousefinejad S, Fardid R (2019) Genotoxicity of inhalational anesthetics and its relationship with the polymorphisms of GSTT1, GSTM1, and GSTP1 genes. Environ Sci Pollut Res Int 26:3530–3541
Neghab M, Kargar-Shouroki F, Mozdarani H, Yousefinejad S, Alipour H, Fardid R (2020) Association between genotoxic properties of inhalation anesthetics and oxidative stress biomarkers. Toxicol Ind Health 36:454–466
Tian Y, Chen KY, Liu LD, Dong YX, Zhao P, Guo SB (2018) Sevoflurane exacerbates cognitive impairment induced by Aβ1-40 in rats through initiating neurotoxicity, neuroinflammation, and neuronal apoptosis in rat hippocampus. Mediat Inflamm 9:3802324. https://doi.org/10.1155/2018/3802324
Gao Y, Ma L, Han T, Wang M, Zhang D, Wang Y (2020) Protective role of protocatechuic acid in sevoflurane-induced neuron apoptosis, inflammation and oxidative stress in mice. Restor Neurol Neurosci 38:323–331
Al Olayan EM, Aloufi AS, AlAmri OD, El-Habit OH, Abdel Moneim AE (2020) Protocatechuic acid mitigates cadmium-induced neurotoxicity in rats: role of oxidative stress, inflammation and apoptosis. Sci Total Environ 723:137969. https://doi.org/10.1016/j.scitotenv.2020.137969
Wei M, Chu X, Gua M, Yang X, Xie X, Liu F, Chen C, Deng X (2013) Protocatechuic acid suppresses ovalbumin-induced airway inflammation in a mouse allergic asthma model. Int Immunopharmacol 15:780–788
Anderson K, Ryan N, Siddiqui A, Pero T, Volpedo G, Cooperstone JL, Oghumu S (2020) Black raspberries and protocatechuic acid mitigate DNFB-induced contact hypersensitivity by down-regulating dendritic cell activation and inhibiting mediators of effector responses. Nutrients 12:1701. https://doi.org/10.3390/nu12061701
Peiffer DS, Zimmerman NP, Wang LS, Ransom BW, Carmella SG, Kuo CT, Siddiqui J, Chen JH, Oshima K, Huang YW, Hecht SS, Stoner GD (2014) Chemoprevention of esophageal cancer with black raspberries, their component anthocyanins, and a major anthocyanin metabolite, protocatechuic acid. Cancer Prev Res (Phila) 7:574–584
Zhang L, Ji Y, Kang Z, Lv C, Jiang W (2015) Protocatechuic aldehyde ameliorates experimental pulmonary fibrosis by modulating HMGB1/RAGE pathway. Toxicol Appl Pharmacol 283:50–56
Jang SA, Song HS, Kwon JE, Baek HJ, Koo HJ, Sohn EH, Lee SR, Kang SC (2018) Protocatechuic acid attenuates trabecular bone loss in ovariectomized mice. Oxid Med Cell Longev 2018:7280342. https://doi.org/10.1155/2018/7280342
Zhang J, Fu B, Chen X, Chen D, Yang H (2020) Protocatechuic acid attenuates anterior cruciate ligament transection-induced osteoarthritis by suppressing osteoclastogenesis. Exp Ther Med 19:232–240
Yang Y, Chi Z, Gao R, Lei Z (2018) The roles of natural compounds in epigenetics. Nat Prod Commun 13:1067–1072
Izzo S, Naponelli V, Bettuzzi S (2020) Flavonoids as epigenetic modulators for prostate cancer prevention. Nutrients 12:1010. https://doi.org/10.3390/nu12041010
Paluszczak J, Krajka-Kuźniak V, Baer-Dubowska W (2010) The effect of dietary polyphenols on the epigenetic regulation of gene expression in MCF7 breast cancer cells. Toxicol Lett 192:119–125
Wang LS, Kuo CT, Cho SJ, Seguin C, Siddiqui J, Stoner K, Weng YI, Huang TH, Tichelaar J, Yearsley M, Stoner GD, Huang YW (2013) Black raspberry-derived anthocyanins demethylate tumor suppressor genes through the inhibition of DNMT1 and DNMT3B in colon cancer cells. Nutr Cancer 65:118–125
Anantharaju PG, Reddy BD, Padukudru MA, Kumari Chitturi CM, Vimalambike MG, Madhunapantula SV (2017) Naturally occurring benzoic acid derivatives retard cancer cell growth by inhibiting histone deacetylases (HDAC). Cancer Biol Ther 18:492–504
Declaration of Interest Statement
The author declare that she has no competing interests. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this entry
Cite this entry
Widy-Tyszkiewicz, E. (2022). Current Evidence for Disease Prevention and Treatment by Protocatechuic Acid (PCA) and Its Precursor Protocatechuic Aldehyde (PCAL) in Animals and Humans. In: Ekiert, H.M., Ramawat, K.G., Arora, J. (eds) Plant Antioxidants and Health. Reference Series in Phytochemistry. Springer, Cham. https://doi.org/10.1007/978-3-030-78160-6_36
Download citation
DOI: https://doi.org/10.1007/978-3-030-78160-6_36
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78159-0
Online ISBN: 978-3-030-78160-6
eBook Packages: Chemistry and Materials ScienceReference Module Physical and Materials ScienceReference Module Chemistry, Materials and Physics