Abstract
Mixed urinary incontinence (MUI) is highly prevalent and associated with a significant impairment in quality of life. The pathogenesis of MUI is unclear, and patients may have stress-predominant MUI, urgency-predominant MUI, or equal stress- and urgency-predominant MUI. There is limited evidence regarding the best initial treatment for women with MUI, though treatment typically begins with conservative therapy for the component of incontinence that is most bothersome to the patient. For women with refractory MUI symptoms, stress incontinence surgery and third-line overactive bladder therapies are reasonable treatment options, and patient factors and urodynamic variables may help guide treatment decisions.
Commentary by Marcio A. Averbeck, Neuro-urology, Video-urodynamics Unit, Moinhos De Vento Hospital, Department of Urology, Porto Allegre, Brazil
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Case Scenario
A 62-year-old woman complains of multiple daily episodes of urinary incontinence that occur with preceding urgency as well as during exertion. She finds the incontinence bothersome. Her examination is within normal limits, and she has not been previously treated for incontinence.
Introduction
Mixed urinary incontinence (MUI) is defined by the International Continence Society (ICS) as “the complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing or coughing” [1]. MUI can also be defined by the presence of both detrusor overactivity (DO) and stress urinary incontinence (SUI) on urodynamics. Data from the Nurses’ Health Study demonstrated that among women with incontinence, 22% experience MUI, 51% experience SUI, and 27% experience urgency urinary incontinence (UUI) [2]. The prevalence of MUI has been shown to increase with age, and clinicians will likely care for more women with MUI as the population ages [3, 4]. MUI can cause a considerable impact on health-care-related quality of life, and research has indicated that women with MUI are actually more bothered by their incontinence compared to women with pure SUI or pure UUI [5, 6].
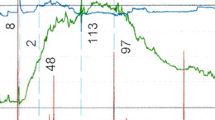
Management of MUI can be challenging for numerous reasons. Women with MUI represent a heterogeneous population and may have stress-predominant symptoms, urgency-predominant symptoms, or equal stress- and urgency-predominant symptoms. In fact, it is hard to universally characterize patients with MUI, and patients may be labeled differently according to the definition of MUI used [7, 8]. Additionally, women with MUI may have varying treatment goals and different comorbidities, such as pelvic organ prolapse, that may complicate management. Furthermore, the pathophysiology of MUI is unclear [9,10,11], and treating one component of MUI (i.e., the urgency component or the stress component) may potentially improve or worsen the other component of the incontinence. Lastly, in comparison to women with either pure SUI or pure UUI, women with MUI appear to have higher rates of surgical treatment failure [12]. For these reasons, MUI patients have often been excluded from treatment trials for SUI- and UUI-directed therapies further limiting the information on therapy effects in the MUI population. Therefore, management of women with MUI is typically performed on a case-by-case basis, with several reasonable treatment strategies available (Fig. 8.1). In this chapter, we review the management of MUI.
Mixed urinary incontinence treatment algorithm from [76]. (Reused with permission © Springer Nature)
How to Approach (Order of Addressing Components)
An appropriate history and physical examination are important first steps in the evaluation of women with MUI. While the evaluation of women with pelvic floor dysfunction was discussed in Chap. 1, as a review, the patient history of women with MUI should capture the timing of incontinence episodes and the degree of bother associated with the incontinence. Specifically, women should be asked whether the incontinence episodes occur during exertional activities, such as laughing or coughing, or are preceded by urgency. Women should also be asked about any incontinence episodes that may occur without awareness (i.e., insensible incontinence) [13]. A thorough history on the situation and triggers of incontinence is critical in this population as many patients find it challenging to differentiate stress and urgency symptoms. Clinicians should ask about the use of protective pads and how many, if any, are used throughout the day. The presence of associated urinary symptoms, such as hematuria, dysuria, and obstructive voiding symptoms, should also be assessed as well as the presence of vaginal bulge/prolapse symptoms and bowel symptoms, such as fecal incontinence. Clinicians should ask about prior treatment history, such as prior midurethral sling placement and/or prolapse repair (and if mesh was used). A bladder diary can be very useful in assessing patients with MUI, and several validated urinary symptom questionnaires, such as the Medical, Epidemiological, and Social Aspects of Aging (MESA), Questionnaire for Urinary Incontinence Diagnosis (QUID), Urinary Distress Inventory-6 (UDI-6) , and 3 Incontinence Questions (3IQ), are available that may help assess patients with MUI.
Physical examination should include both a pelvic and focused neurologic exam. During pelvic examination, the clinician should assess for urethral hypermobility or scarring (i.e., fixed urethra), as well as assess for the presence of pelvic organ prolapse, vaginal atrophy, or other concomitant pelvic pathology. A cough stress test with a full bladder can help clinicians demonstrate SUI. Specifically, leakage associated with hypermobility, leakage in the absence of hypermobility, or cough-induced urgency with delayed leakage may be demonstrated. Urine analysis should be conducted to assess for infection. Measurement of post-void residual (PVR) urine volume is important to assess for the presence of incomplete emptying, which may worsen urinary incontinence.
Ultimately, after the history and physical exam are completed, an attempt should be made to categorize the patient as having stress-predominant MUI, urgency-predominant MUI, or equal stress- and urgency-predominant MUI. Additionally, the clinician should determine which component of incontinence is most bothersome to the patient. Unfortunately, in women with MUI, there is no Level 1 evidence available to guide clinicians in deciding whether to first treat the stress component or the urgency component of MUI [14]; one randomized trial investigating the best first treatment of MUI (surgical versus non-surgical therapy) was stopped prematurely in March 2009 due to poor enrollment (MIMOSA) [15], and a second randomized trial Effects of Surgical Treatment Enhanced with Exercise for Mixed Urinary Incontinence (ESTEEM) was completed, but analyses are not yet available [16]. Therefore, we typically begin treatment by counseling patients with MUI on available treatment options and encouraging them to begin treatment with the most conservative therapy for the component of incontinence that is most bothersome to them.
Conservative treatment for women with MUI includes fluid modification, weight loss, pelvic floor muscle training, and pessary placement. Research has demonstrated that fluid reduction can improve urinary frequency and incontinence episodes [17]. Although it may be difficult for patients to reduce their fluid intake by large volumes, patients may experience a benefit from a 25% reduction in fluid intake [18]. Pelvic floor muscle training is another efficacious treatment for MUI [19] as a Cochrane review specifically demonstrated that pelvic floor muscle training was an effective first-line therapy for all forms of incontinence [20]. Appropriate education from a nurse, the addition of biofeedback, and even virtual reality may be helpful when performing pelvic floor muscle training for women with MUI [21,22,23]. Weight loss is another conservative management option for women with MUI. Subak et al. randomized 338 women with urinary incontinence to a 6-month weight loss program (including diet and exercise along with behavioral modification) or to a structured education program and found that a higher proportion of women assigned to the weight loss program had a clinically relevant reduction in both SUI and UUI episodes [24]. Pessary placement is also a reasonable first-line therapy for women with MUI. Donnelly et al. reviewed the efficacy of a pessary for 239 women with SUI or MUI and found that half of the women fitted with a pessary continued to use it at 6 months [25]. The Ambulatory Treatments for Leakage Associated with Stress Incontinence (ATLAS) trial was a three-arm randomized trial comparing a pessary, behavioral therapy, and combination therapy (pessary and behavioral therapy) for women with SUI (although 54% of women in the trial had MUI). At 12 months of follow-up, 50% of women assigned to the pessary arm were satisfied with the treatment [26].
Pharmacotherapies can also be an effective treatment for women with MUI [27]. For women with MUI who have bothersome urgency, anticholinergic and/or beta-3 agonist therapy can be initiated. Staskin and Te investigated the efficacy of solifenacin in patients with MUI and found a reduction in incontinence episodes in patients taking solifenacin compared to placebo with over 40% of patients taking solifenacin regaining continence after 12 weeks of therapy [28]. Kelleher et al. investigated the efficacy of solifenacin in women with MUI and found that once-daily solifenacin was as effective and as tolerated in women with MUI as compared to pure UUI [29]. This finding was similar to that of a previous trial by Kreder et al. that found that tolterodine was as effective in reducing incontinence episodes in patients with MUI as compared to patients with pure UUI [30]. The MERIT (Mixed Incontinence Effectiveness Research Investigating Tolterodine) trial demonstrated that women with MUI taking tolterodine experienced a considerable improvement in UUI episodes (−12.3) compared to placebo (−8) [31]. Interestingly, data suggests that the presence of SUI does not appear to diminish the efficacy of anticholinergics in patients with overactive bladder (OAB) unless there is more severe SUI [32], and it has been reported that women with MUI taking anticholinergics may overall experience an approximately 50–60% reduction in the urgency component of their incontinence [10].
A trial of vaginal estrogen may be helpful for women with MUI, though research has provided conflicting evidence on the use of vaginal estrogen. One meta-analysis suggested that vaginal estrogen was efficacious for SUI [33], while a different review suggested efficacy for the symptoms of urinary urgency and frequency [34]. Duloxetine is a serotonin-norepinephrine reuptake inhibitor that may be an attractive pharmacotherapy for the treatment of MUI as it has been shown to improve bladder relaxation and also increase outlet resistance. Bent et al. randomized 588 women with MUI to either duloxetine or placebo and found women receiving duloxetine had a larger median reduction in incontinence episode frequency (60% versus 47%) compared to women receiving placebo [35]. It should be noted that duloxetine is not FDA approved for urinary incontinence treatment. Aside from duloxetine, the tricyclic antidepressant, imipramine, is another medication that have been used for MUI treatment but is not FDA approved for this indication [36].
Unfortunately, many patients with MUI may experience bothersome incontinence that is refractory to conservative and oral pharmacotherapies. After the above treatments have been discussed/attempted and more advanced options such as surgery are being considered, it must be decided whether to proceed with treating the stress component of MUI versus the urgency component of MUI. For women with MUI who are mostly bothered by SUI symptoms, surgical therapy using synthetic midurethral sling placement or autologous fascial sling placement appears to be a reasonable treatment option (as discussed below) [37]. Urethral bulking agents also appear to be a reasonable treatment options for women with MUI who have bothersome SUI symptoms and are frail and/or decline urethral sling placement [38]. For women with MUI who are more bothered by refractory urgency and UUI, we discuss all third-line OAB treatment options as described by the AUA OAB guideline including onabotulinumtoxinA, sacral neuromodulation (SNM), and tibial nerve stimulation [39]. In women with equally bothersome stress and urgency symptoms, it can be difficult to determine which component to treat first. We counsel these patients extensively on the goals of each treatment modality and present the advantages and disadvantages of each. We also consider other factors, such as urodynamic findings (as described below), in determining a treatment plan.
Pros and Cons of Each Approach
Treating the Stress Component First
After conservative therapies have been exhausted, addressing the stress component of MUI first is advantageous for several reasons. Research has suggested that stress incontinence events may lead to urgency incontinence events, and, thus, treating SUI may actually improve UUI. In a rat model, Jung et al. showed that urethral perfusion modulated the micturition reflex and suggested that SUI can induce DO [40]. In examining 30-day bladder diary data among 35 women with MUI, Minassian et al. found that a stress activity preceded 52.5% of UUI episodes and that 69% of women reported stress-induced UUI [41]. Therefore, initially treating SUI may potentially help to resolve urgency and UUI in patients with MUI in addition to SUI symptoms.
Numerous trials have demonstrated that SUI surgery is efficacious in women with MUI as it can treat both the SUI and urgency symptoms. Duckett and Tamilselvi reported on 51 women with urodynamic evidence of both DO and SUI who underwent tension-free vaginal tape (TVT) placement and found that 47% were objectively cured of DO, 63% reported subjective cure of urgency symptoms, and SUI was cured in 92% [42]. Abdel-Fattah et al. analyzed data from 83 women with stress-predominant MUI who underwent transobturator tension-free vaginal tape (TOT) placement and found a patient-reported success rate of 75% and an objective cure rate of 90% [43]. Of note, urgency and UUI resolved after TOT placement in over 50% of women in their study. Jain et al. conducted a systematic review examining the effectiveness of midurethral slings specifically in women with MUI [37]. Among the seven prospective studies included in their review, they found an overall subjective cure of 56.4% at 35 months of follow-up. Following midurethral sling placement, they also found an overall cure of urgency and UUI ranging from 30% to 85% and a cure rate of SUI ranging from 85% to 97%. More recently, Zyczynski et al. conducted a secondary analysis of three large multicenter urinary incontinence treatment trials (the Stress Incontinence Surgical Treatment Efficacy Trial, SISTEr; the Trial of Midurethral Slings, TOMUS; and the Value of Urodynamic Evaluations trial, ValUE) in women with stress-predominant MUI who underwent surgical therapy for SUI and found that 50–71% experienced an improvement in OAB symptoms [44].
Burch colposuspension and pubovaginal sling may also effectively treat MUI. Osman performed Burch colposuspensions in 24 women with MUI (with a VLPP of ≥90 cm H2O) and found that 87% of women became completely dry postoperatively [45]. Fulford et al. performed rectus fascial pubovaginal sings in 85 women with SUI and found that 97% were symptomatically cured of SUI and that 69% also experienced resolution of urgency [46]. Interestingly, they conjectured that resolution of urgency was attributable to appropriately tensioning the sling to achieve bladder neck closure.
Treatment of the stress component of MUI using a bulking agent is another reasonable option in women with MUI and may be especially useful in women who decline or are not ideal candidates for midurethral sling placement (e.g., are frail, have underwent prior pelvic radiotherapy, and failed prior midurethral sling placement). Mohr et al. studied periurethral Bulkamid in women with MUI and found considerable improvements for all domains of the King’s Health Questionnaire, pad weights, and visual analogue scores. Complications were low (13%) with the majority being urinary tract infections [38]. Poon and Zimmern also found significant improvement in urinary symptoms (as measured by UDI-6 question scores) in women with MUI who underwent periurethral collagen injection [47]. A Cochrane review however found limited evidence for urethral bulking agents for SUI [48].
Unfortunately, SUI surgery may fail to resolve or even worsen urinary urgency and UUI, and this may be especially problematic for women with MUI who are initially bothered by urgency at baseline. Early studies on SUI therapy suggested higher rates of de novo urgency and worsening urgency and may be related to procedures being performed at the bladder neck rather than the midurethra. Among 754 women with MUI, Lee et al. found that 40% and 32% of women had persistent urgency and UUI, respectively, after midurethral sling placement [49]. Urgency is recognized as a common reason for dissatisfaction after midurethral sling placement [50], and thus, a main disadvantage of treating the SUI component first in women with MUI is the possibility of worsening urgency after anti-incontinence surgery. Needless to say, disadvantages of treating MUI with SUI surgery also include the usual surgical risks of treatment [51].
Treating the Urgency Component First
There are several advantages of treating the urgency component of MUI first in women with MUI. Urgency has been reported to be one of the most bothersome urinary symptoms [52], and, thus, by first treating urgency, one may improve quality of life and eliminate the need for other treatments. In women who fail treatment with an anticholinergic or beta-3 agonist, third-line OAB therapies, including sacral neuromodulation (SNM), tibial nerve stimulation, and onabotulinumtoxinA, can be effective in women with OAB and UUI [39]. Additionally, treatment of urinary urgency with neuromodulation or onabotulinumtoxinA may pose fewer and more reversible surgical complications compared to SUI surgery. Therefore, a patient with MUI and bothersome urgency may opt to try a third-line OAB therapy before proceeding with SUI surgery and consider SUI surgery only if symptoms are not controlled with a third-line OAB therapy.
While third-line OAB therapies have not been extensively studied in women with MUI, they have been demonstrated to improve urgency/urgency incontinence symptoms. In terms of tibial nerve stimulation, the SUmiT trial randomized 220 adults to either percutaneous tibial nerve stimulation or sham treatment for 12 weeks and found that 54% of subjects in the active treatment group reported moderate or marked improvement in bladder symptoms compared to 21% of subjects in the sham group [53]. Numerous studies have supported the efficacy of onabotulinumtoxinA for women with OAB [54]. Recently, Herschorn et al. randomized patients with overactive bladder and urinary incontinence to onabotulinumtoxinA 100 U, solifenacin 5 mg, or placebo and found that both onabotulinumtoxinA 100 U and solifenacin 5 mg were more efficacious than placebo, with a third of patients receiving onabotulinumtoxinA experiencing a 100% reduction in incontinence [55]. Siegel et al. randomized 147 subjects to SNM versus standard medical therapy for OAB and found greater therapeutic success in the SNM group compared to the standard medical therapy group (61% versus 42%) [56]. In the Refractory Overactive Bladder: Sacral Neuromodulation vs Botulinum Toxin Assessment (ROSETTA) trial, which was a randomized trial comparing onabotulinumtoxinA 200 U to sacral neuromodulation in women with UUI, there was a reduction of 3.9 and 3.3 incontinence episodes per day after 6 months in women receiving onabotulinumtoxinA 200 U and SNM, respectively [57].
What Directs Decisions
Multiple factors should be considered when deciding how to treat MUI, including the type of MUI (i.e., stress-predominant MUI, urgency-predominant MUI, and equal stress- and urgency-predominant MUI), patient preferences/goals, physical exam findings (e.g., concomitant prolapse), comorbidities, and urodynamic findings. Of these factors, the role of urodynamics (UDS) in the evaluation of MUI has been widely studied in the literature. Specifically, research has investigated both the correlation between urodynamic findings and urinary symptoms and the urodynamic predictors of success and/or failure after midurethral sling placement in patients with MUI in order to determine what role urodynamics plays in directing MUI treatment.
It is debatable how well urodynamic findings correlate with patient-reported symptoms, and it is, therefore, unclear to what extent urodynamic findings should factor into the treatment approach (i.e., whether to first treat SUI versus UUI) for each patient. For example, many women who report the symptom of urinary urgency, or SUI, do not demonstrate SUI or DO on UDS. A systematic review including 23 studies attempting to classify patients by incontinence type found a poor level of agreement between clinical evaluation and urodynamics [58]. Interestingly, this study found that the reclassification rate of incontinence type was highest among patients with MUI; 46% of patients with a clinical diagnosis of MUI had SUI on UDS, while 21% had DO on UDS. On the other hand, Digesu et al. examined urodynamic findings of 1626 women with MUI symptoms and found reasonable correlation between UDS findings and urinary symptoms [59]. Among women with stress-predominant MUI, 82% demonstrated urodynamic SUI, and among those with urgency-predominant MUI, 64% had DO on UDS. Among women with equal stress- and urgency-predominant MUI, 46% had DO, and 54% demonstrated SUI. Lewis et al. examined the records of 99 women with MUI and also found urodynamic differences that correlated with symptoms [60]. In their study, 100% of women with stress-predominant MUI demonstrated SUI on UDS compared to 61% of women with urgency-predominant MUI, and 70% of women with urgency-predominant MUI demonstrated DO on UDS compared to 26% of women with stress-predominant MUI.
Overall, as the reported correlation between patient symptoms and urodynamic findings has varied in the literature, we rely on the patient history to categorize a patient’s type of MUI (i.e., stress-predominant, urgency-predominant, and equal stress- and urgency-predominant MUI) and consider UDS when the clinical picture is unclear and/or in women who have undergone prior surgery. Additionally, UDS may be advisable in women with MUI prior to surgical intervention [14]. According to AUA guidelines, urodynamics may be performed prior to SUI surgery in women with MUI [61] as well as before any potentially morbid treatment is considered [61]. Additionally, according to AUA guidelines , the absence of DO on UDS in patients with MUI does not exclude it as an etiology for urgency [62].
Several studies have also investigated the role of UDS in predicting midurethral sling or third-line OAB therapy outcomes that may, therefore, be used to help direct decision-making in treating patients with MUI. In women with MUI, Panayi et al. found that the opening detrusor pressure was predicative of postoperative DO after TVT placement [63], and Lee et al. found that preoperative DO was predictive of postoperative urgency after midurethral sling placement [49]. Other studies have found that low maximum urethral closure pressure [64] and low maximum cystometric capacity [65] were associated with persistent urgency and/or detrusor overactivity after midurethral sling placement. Unfortunately, in patients undergoing treatment for urgency and UUI, Cohen et al. did not find any relationship between urodynamic variables and clinical response to onabotulinumtoxinA [66], and Nobrega et al. did not find any relationship between urodynamic variables and SNM outcomes [67].
Patient characteristics may also factor into the decision-making for MUI treatment. Among patient characteristics, the severity of baseline urgency appears to be an important risk factor for poor surgical outcomes after midurethral sling placement in women with MUI. In a study by Kulseng-Hanssen et al., 1113 women with MUI were stratified into 3 groups according to their type of MUI (stress-predominant incontinence group, urgency-predominant incontinence group, and an equal stress- and urgency-predominant incontinence group) [68]. At 38 months of follow-up, objective cure results were 64.2%, 45.2, and 51.3% for women with stress-predominant MUI, urgency-predominant MUI, and equal stress- and urgency-predominant MUI, respectively. Thus, women with stress-predominant MUI symptoms appear to have better outcomes compared to women with urgency-predominant MUI. Preoperative anticholinergic use is another patient characteristic that can be a risk factor for persistent urgency after anti-incontinence surgery and may be useful for patient counseling and decision-making. Kenton et al. investigated risk factors associated with bothersome UUI after Burch colposuspension or midurethral sling placement and found that patients with prior anticholinergic use, preoperative urgency, or DO were more likely to have postoperative UUI [69]. Barber et al. also found that preoperative anticholinergic medication use was associated with recurrent urinary incontinence after midurethral sling placement [70]. Age is another important factor that can be considered in the treatment of MUI, as older women may be at increased risk for urgency after midurethral sling placement. Among 103 women with MUI who underwent TOT, Yoo and Kim found that older women were at high risk of using anticholinergics postoperatively [71].
Choosing the type of midurethral sling is another important decision for patients with MUI who elect to undergo SUI surgery. While overall there does not appear to be a difference in efficacy between retropubic and TOT midurethral slings [72], some data has suggested that TOT slings may have a lower rate of de novo urgency, while retropubic slings may be more efficacious in women with intrinsic sphincter deficiency (ISD). Botros et al. studied 257 women with SUI or MUI who underwent retropubic or TOT slings and found lower rates of de novo UUI in women undergoing TOT (8%) compared to women undergoing retropubic slings (33%) [73]. However, they did not find a difference in resolution of DO, UUI, and de novo DO between the groups. Of note, among patients with preoperative UUI, only 6% who underwent TOT had worsening UUI compared to 14–16% who underwent a retropubic sling placement. Schierlitz et al. compared retropubic sling outcomes to TOT midurethral sling outcomes in women with ISD and found a higher rate of persistent stress urinary incontinence in the TOT group (45%) compared to the retropubic sling group (21%) [74]. Conversely, a meta-analysis examining midurethral sling outcomes for women with MUI found that the odds of overall subjective cure were similar between retropubic and TOT slings [37].
Important Caveats of Counseling
Patients being treated for MUI require extensive counseling. Goals of care should be discussed as this appears to be a major determinant of satisfaction in women undergoing pelvic floor surgery [75]. When considering midurethral sling placement in women with MUI, women should be informed that urgency may not improve and may even potentially worsen after surgery. Mallet et al. found that patients undergoing SUI surgery expect improvement in storage symptoms [76, 77], and in a study by Aigmueller, urgency was reported to be a common reason for dissatisfaction after TVT in women with MUI [50]. Interestingly, a different study found that women with persistent UUI are dissatisfied by midurethral sling placement even if their SUI improves [46]. Additionally, women with MUI undergoing midurethral sling placement should also be counseled that they may be at higher risk of surgical failure compared to women with pure SUI [12] and that they may need combination treatment for their urinary incontinence. The ESTEEM trial, which is being conducted by the Pelvic Floor Disorders Network, is randomizing women with MUI to either midurethral sling placement alone or to midurethral sling placement with perioperative behavioral therapy to see if the addition of pelvic floor muscle therapy will improve MUI (primary aim) and SUI and/or urgency/UUI (secondary aims) symptoms after midurethral sling placement [16]. Pending the results of this trial, women may be counseled on the role of perioperative pelvic floor therapy in addition to midurethral sling placement for the treatment of MUI and the potential role of combination therapy.
Summary
MUI is a very common form of urinary incontinence that can be challenging to treat. Women with MUI should be classified according to the type of their incontinence (i.e., stress-predominant, urgency-predominant, and equal stress- and urgency-predominant MUI), and initial treatment can be targeted to the most bothersome component of their incontinence. Numerous conservative therapies and pharmacotherapies are available to treat MUI, and midurethral sling placement as well as third-line OAB therapies can be effective treatment options for women who have refractory symptoms. Urodynamic factors and patient characteristics may help guide the initial treatment approach, and research has demonstrated that treating one component of MUI may improve or worsen the other component. Women with MUI should be extensively counseled regarding all treatment options and informed that they may require multiple treatments to improve their incontinence.
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002;187(1):116–26.
Minassian VA, Devore E, Hagan K, Grodstein F. Severity of urinary incontinence and effect on quality of life in women, by incontinence type. Obstet Gynecol. 2013;121(5):1083.
Lifford KL, Townsend MK, Curhan GC, Resnick NM, Grodstein F. The epidemiology of urinary incontinence in older women: incidence, progression, and remission. J Am Geriatr Soc. 2008;56(7):1191–8.
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. J Clin Epidemiol. 2000;53(11):1150–7.
Frick AC, Huang AJ, Van Den Eeden SK, Knight SK, Creasman JM, Yang J, et al. Mixed urinary incontinence: greater impact on quality of life. J Urol. 2009;182(2):596–600.
Dooley Y, Lowenstein L, Kenton K, FitzGerald M, Brubaker L. Mixed incontinence is more bothersome than pure incontinence subtypes. Int Urogynecol J. 2008;19(10):1359–62.
Brubaker L, Stoddard A, Richter H, Zimmern P, Moalli P, Kraus SR, et al. Mixed incontinence: comparing definitions in women having stress incontinence surgery. Neurourol Urodyn. 2009;28(4):268–73.
Brubaker L, Lukacz ES, Burgio K, Zimmern P, Norton P, Leng W, et al. Mixed incontinence: comparing definitions in non surgical patients. Neurourol Urodyn. 2011;30(1):47–51.
Myers DL. Female mixed urinary incontinence: a clinical review. JAMA. 2014;311(19):2007–14.
Bandukwala NQ, Gousse AE. Mixed urinary incontinence: what first? Curr Urol Rep. 2015;16(3):9.
Lai HH, Simon M, Boone TB. The impact of detrusor overactivity on the management of stress urinary incontinence in women. Curr Urol Rep. 2006;7(5):354–62.
Gleason JL, Parden AM, Jauk V, Ballard A, Sung V, Richter HE. Outcomes of midurethral sling procedures in women with mixed urinary incontinence. Int Urogynecol J. 2015;26(5):715–20.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. J Assoc Chart Physiother Women Health. 2012;110:33.
Kammerer-Doak D, Rizk DE, Sorinola O, Agur W, Ismail S, Bazi T. Mixed urinary incontinence: international urogynecological association research and development committee opinion. Int Urogynecol J. 2014;25(10):1303–12.
Brubaker L, Moalli P, Richter HE, Albo M, Sirls L, Chai T, et al. Challenges in designing a pragmatic clinical trial: the mixed incontinence—medical or surgical approach (MIMOSA) trial experience. Clin Trials. 2009;6(4):355–64.
Sung VW, Borello-France D, Dunivan G, Gantz M, Lukacz ES, Moalli P, et al. Methods for a multicenter randomized trial for mixed urinary incontinence: rationale and patient-centeredness of the ESTEEM trial. Int Urogynecol J. 2016;27(10):1479–90.
Swithinbank L, Hashim H, Abrams P. The effect of fluid intake on urinary symptoms in women. J Urol. 2005;174(1):187–9.
Hashim H, Abrams P. How should patients with an overactive bladder manipulate their fluid intake? BJU Int. 2008;102(1):62–6.
Sar D, Khorshid L. The effects of pelvic floor muscle training on stress and mixed urinary incontinence and quality of life. J Wound Ostomy Cont Nurs. 2009;36(4):429–35.
Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2010;1(1):CD005654.
Ng S-C, Lin T-L, Chang S-J, Tai H-L, Hu S-W, Chen G-D. Nursing intervention to enhance efficacy of home practice of pelvic floor muscle exercises in treating mixed urinary incontinence. Int Urogynecol J. 2008;19(5):637–42.
Herderschee R, Hay Smith EJC, Herbison GP, Roovers JP, Heineman MJ. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women. Cochrane Library. 2011.
Elliott V, de Bruin ED, Dumoulin C. Virtual reality rehabilitation as a treatment approach for older women with mixed urinary incontinence: a feasibility study. Neurourol Urodyn. 2015;34(3):236–43.
Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, et al. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009;360(5):481–90.
Donnelly MJ, Powell-Morgan S, Olsen AL, Nygaard IE. Vaginal pessaries for the management of stress and mixed urinary incontinence. Int Urogynecol J. 2004;15(5):302–7.
Richter HE, Burgio KL, Brubaker L, Nygaard IE, Ye W, Weidner A, et al. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115(3):609–17.
Hashim H, Abrams P. Pharmacological management of women with mixed urinary incontinence. Drugs. 2006;66(5):591–606.
Staskin DR, Te AE. Short- and long-term efficacy of solifenacin treatment in patients with symptoms of mixed urinary incontinence. BJU Int. 2006;97(6):1256–61.
Kelleher C, Cardozo L, Kobashi K, Lucente V. Solifenacin: as effective in mixed urinary incontinence as in urge urinary incontinence. Int Urogynecol J. 2006;17(4):382–8.
Kreder K, Brubaker L, Mainprize T. Tolterodine is equally effective in patients with mixed incontinence and those with urge incontinence alone. BJU Int. 2003;92(4):418–21.
Khullar V, Hill S, Laval K-U, Schiøtz HA, Jonas U, Versi E. Treatment of urge-predominant mixed urinary incontinence with tolterodine extended release: a randomized, placebo-controlled trial. Urology. 2004;64(2):269–74.
Michel MC, de la Rosette JJ, Piro M, Goepel M. Does concomitant stress incontinence alter the efficacy of tolterodine in patients with overactive bladder? J Urol. 2004;172(2):601–4.
Fantl JA, Cardozo L, McClish DK. Estrogen therapy in the management of urinary incontinence in postmenopausal women: a meta-analysis. First report of the Hormones and Urogenital Therapy Committee. Obstet Gynecol. 1994;83:12–8.
Sultana CJ, Walters MD. Estrogen and urinary incontinence in women. Maturitas. 1994;20(2–3):129–38.
Bent AE, Gousse AE, Hendrix SL, Susan L, Klutke CG, Monga AK, et al. Duloxetine compared with placebo for the treatment of women with mixed urinary incontinence. Neurourol Urodyn. 2008;27(3):212–21.
Hunsballe J, Djurhuus JC. Clinical options for imipramine in the management of urinary incontinence. Urol Res. 2001;29(2):118–25.
Jain P, Jirschele K, Botros SM, Latthe PM. Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2011;22(8):923–32.
Mohr S, Marthaler C, Imboden S, Monga A, Mueller MD, Kuhn A. Bulkamid (PAHG) in mixed urinary incontinence: what is the outcome? Int Urogynecol J. 2017;28(11):1657–61.
Gormley EA, Lightner DJ, Burgio KL, Chai TC, Clemens JQ, Culkin DJ, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol. 2012;188(6):2455–63.
Jung SY, Fraser MO, Ozawa H, Yokoyama O, Yoshiyama M, De Groat WC, et al. Urethral afferent nerve activity affects the micturition reflex; implication for the relationship between stress incontinence and detrusor instability. J Urol. 1999;162(1):204–12.
Minassian VA, Yan XS, Pitcavage J, Stewart WF. Mixed incontinence masked as stress induced urgency urinary incontinence. J Urol. 2016;196(4):1190–5.
Duckett JR, Tamilselvi A. Urogynaecology: effect of tension-free vaginal tape in women with a urodynamic diagnosis of idiopathic detrusor overactivity and stress incontinence. BJOG. 2006;113(1):30–3.
Abdel-Fattah M, Mostafa A, Young D, Ramsay I. Evaluation of transobturator tension-free vaginal tapes in the management of women with mixed urinary incontinence: one-year outcomes. Am J Obstet Gynecol. 2011;205(2):150.e1–6.
Zyczynski HM, Albo ME, Goldman HB, Wai CY, Sirls LT, Brubaker L, et al. Change in overactive bladder symptoms after surgery for stress urinary incontinence in women. Obstet Gynecol. 2015;126(2):423.
Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU Int. 2003;92(9):964–8.
Fulford S, Flynn R, Barrington J, Appanna T, Stephenson T. An assessment of the surgical outcome and urodynamic effects of the pubovaginal sling for stress incontinence and the associated urge syndrome. J Urol. 1999;162(1):135–7.
Poon CI, Zimmern PE. Is there a role for periurethral collagen injection in the management of urodynamically proven mixed urinary incontinence? Urology. 2006;67(4):725–9.
Kirchin V, Page T, Keegan PE, Atiemo K, Cody JD, McClinton S. Urethral injection therapy for urinary incontinence in women. Cochrane Library. 2012.
Lee JS, Dwyer P, Rosamilia A, Lim Y, Polyakov A, Stav K. Persistence of urgency and urge urinary incontinence in women with mixed urinary symptoms after midurethral slings: a multivariate analysis. BJOG. 2011;118(7):798–805.
Aigmueller T, Bjelic-Radisic V, Kargl J, Hinterholzer S, Laky R, Trutnovsky G, et al. Reasons for dissatisfaction ten years after TVT procedure. Int Urogynecol J. 2014;25(2):213–7.
Herschorn S. Midurethral sling complications. Can Urol Assoc J. 2017;11(6Suppl2):S141.
Agarwal A, Eryuzlu LN, Cartwright R, Thorlund K, Tammela TL, Guyatt GH, et al. What is the most bothersome lower urinary tract symptom? Individual-and population-level perspectives for both men and women. Eur Urol. 2014;65(6):1211–7.
Peters KM, Carrico DJ, Perez-Marrero RA, Khan AU, Wooldridge LS, Davis GL, et al. Randomized trial of percutaneous tibial nerve stimulation versus Sham efficacy in the treatment of overactive bladder syndrome: results from the SUmiT trial. J Urol. 2010;183(4):1438–43.
Anger JT, Weinberg A, Suttorp MJ, Litwin MS, Shekelle PG. Outcomes of intravesical botulinum toxin for idiopathic overactive bladder symptoms: a systematic review of the literature. J Urol. 2010;183(6):2258–64.
Herschorn S, Kohan A, Aliotta P, McCammon K, Sriram R, Abrams S, et al. The efficacy and safety of onabotulinumtoxinA or solifenacin compared with placebo in solifenacin naïve patients with refractory overactive bladder: results from a multicenter, randomized, double-blind phase 3b trial. J Urol. 2017;198(1):167–75.
Siegel S, Noblett K, Mangel J, Griebling TL, Sutherland SE, Bird ET, et al. Results of a prospective, randomized, multicenter study evaluating sacral neuromodulation with InterStim therapy compared to standard medical therapy at 6-months in subjects with mild symptoms of overactive bladder. Neurourol Urodyn. 2015;34(3):224–30.
Amundsen CL, Richter HE, Menefee SA, Komesu YM, Arya LA, Gregory WT, et al. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: a randomized clinical trial. JAMA. 2016;316(13):1366–74.
van Leijsen SA, Evert JS, Mol BWJ, Vierhout ME, Milani AL, Heesakkers JP, et al. The correlation between clinical and urodynamic diagnosis in classifying the type of urinary incontinence in women. A systematic review of the literature. Neurourol Urodyn. 2011;30(4):495–502.
Digesu GA, Salvatore S, Fernando R, Khullar V. Mixed urinary symptoms: what are the urodynamic findings? Neurourol Urodyn. 2008;27(5):372–5.
Lewis JB, Ng AV, O’Connor RC, Guralnick ML. Are there differences between women with urge predominant and stress predominant mixed urinary incontinence? Neurourol Urodyn. 2007;26(2):204–7.
Kobashi KC, Albo ME, Dmochowski RR, Ginsberg DA, Goldman HB, Gomelsky A, et al. Surgical treatment of female stress urinary incontinence: AUA/SUFU guideline. J Urol. 2017;198(4):875–83.
Winters JC, Dmochowski RR, Goldman HB, Herndon CA, Kobashi KC, Kraus SR, et al. Urodynamic studies in adults: AUA/SUFU guideline. J Urol. 2012;188(6):2464–72.
Panayi D, Duckett J, Digesu G, Camarata M, Basu M, Khullar V. Pre operative opening detrusor pressure is predictive of detrusor overactivity following TVT in patients with pre operative mixed urinary incontinence. Neurourol Urodyn. 2009;28(1):82–5.
Paick J-S, Ku JH, Kim SW, Oh S-J, Son H, Shin JW. Tension-free vaginal tape procedure for the treatment of mixed urinary incontinence: significance of maximal urethral closure pressure. J Urol. 2004;172(3):1001–5.
Gamble TL, Botros SM, Beaumont JL, Goldberg RP, Miller J-JR, Adeyanju O, et al. Predictors of persistent detrusor overactivity after transvaginal sling procedures. Am J Obstet Gynecol. 2008;199(6):696.e1–7.
Cohen BL, Caruso DJ, Kanagarajah P, Gousse AE. Predictors of response to intradetrusor botulinum toxin-A injections in patients with idiopathic overactive bladder. Adv Urol. 2009;2009:328364.
Nobrega RP, Solomon E, Jenks J, Greenwell T, Ockrim J. Predicting a successful outcome in sacral neuromodulation testing: are urodynamic parameters prognostic? Neurourol Urodyn. 2018;37:1007–10.
Kulseng-Hanssen S, Husby H, Schiøtz HA. Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J. 2008;19(3):391–6.
Kenton K, Richter H, Litman H, Lukacz E, Leng W, Lemack G, et al. Risk factors associated with urge incontinence after continence surgery. J Urol. 2009;182(6):2805–9.
Barber MD, Kleeman S, Karram MM, Paraiso MFR, Ellerkmann M, Vasavada S, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol. 2008;199(6):666.e1–7.
Yoo E-H, Kim D. Predictors of postoperative antimuscarinics in women with mixed urinary incontinence after transobturator surgery. Int Urogynecol J. 2013;24(3):401–6.
Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid urethral sling operations for stress urinary incontinence in women. Cochrane Library. 2017.
Botros SM, Miller JJR, Goldberg RP, Gandhi S, Akl M, Beaumont JL, et al. Detrusor overactivity and urge urinary incontinence following trans obturator versus midurethral slings. Neurourol Urodyn. 2007;26(1):42–5.
Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstet Gynecol. 2008;112(6):1253–61.
Elkadry EA, Kenton KS, FitzGerald MP, Shott S, Brubaker L. Patient-selected goals: a new perspective on surgical outcome. Am J Obstet Gynecol. 2003;189(6):1551–7.
Mallett VT, Brubaker L, Stoddard AM, Borello-France D, Tennstedt S, Hall L, et al. The expectations of patients who undergo surgery for stress incontinence. Am J Obstet Gynecol. 2008;198(3):308.e1–6.
Lee EW, Kobashi KC. Mixed incontinence: what takes precedence in its management? Curr Urol Rep. 2014;15(12):461.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Commentary
Commentary
The chapter entitled “Mixed Urinary Incontinence: Strategic Approach” deals with a highly relevant subject in the clinical practice. Dr. Steven J. Weissbart and Dr. Ariana L. Smith adeptly described the strategic approach to mixed incontinence, in a comprehensive fashion, starting with the importance of diagnostic workup and then addressing the pros and cons of treatment options, including conservative measures and minimally invasive procedures for refractory cases.
Medical history and physical examination remain the cornerstones of medical assessment of women with mixed urinary incontinence (MUI). As mentioned by the authors, conservative treatments comprise fluid modification, weight loss, pelvic floor muscle training, and pessary placement. Despite the lack of high level evidence to propose specific regimens, conservative treatment should always be offered to the patients, since minimally invasive procedures may be associated with inherent complications. Thus, precise guidance on the risks and benefits of all available treatments is truly important to effectively manage patients’ expectations and avoid future frustrations. Retrieving clear information on the most bothersome component of female urinary incontinence may be challenging sometimes. In this context, urodynamics (UDS) represent a valid tool to reproduce the patients’ urinary complaints. The authors described honestly the role of UDS in predicting midurethral sling or third-line OAB therapy outcomes for those patients refractory to behavioral and medical treatments. Although UDS should not be seen as a panacea in the assessment of such difficult cases, this method sheds a light toward decision-making.
This chapter certainly brings valuable insights not only to the initial management but also to the third-line treatments of refractory MUI patients.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Weissbart, S.J., Smith, A.L. (2021). Mixed Urinary Incontinence: Strategic Approach. In: Kobashi, K.C., Wexner, S.D. (eds) Female Pelvic Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-54839-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-54839-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-54838-4
Online ISBN: 978-3-030-54839-1
eBook Packages: MedicineMedicine (R0)