Abstract
Mixed urinary incontinence (MUI) is the involuntary loss of urine associated with the sensation of urgency and also with exertion, effort, sneezing, or coughing. The underlying cause of MUI is poorly understood. Without clearly understanding the pathophysiological and anatomical changes associated with MUI, treatment is often misdirected. This review presents an analysis of the most recent studies and pathophysiological mechanisms thought to be associated with MUI-related voiding dysfunction. A suggested algorithm is provided for the workup of these women with a review of medical and surgical treatment options used to treat MUI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Continence Society (ICS)-International Urogynecological Association defines urinary incontinence as any involuntary loss of urine [1••]. Urinary incontinence is subcategorized into three groups according to the ICS: (1) stress urinary incontinence (SUI), which is defined as involuntary leakage of urine on effort or exertion or on sneezing or coughing; (2) urge urinary incontinence (UUI), which is the involuntary leakage of urine immediately preceded by urgency; and (3) mixed urinary incontinence (MUI) defined as the involuntary loss of urine associated with the sensation of urgency and also with exertion, effort, sneezing, or coughing [2]. There are other types of incontinence that are beyond the scopes of this paper including continuous urinary leakage seen in fistula patients, coital incontinence, and insensible urinary incontinence [3••].
Mixed urinary incontinence (MUI) is a term that applies to both urinary incontinence symptoms and urodynamic findings in the same individual [4]. MUI with a prevalence rate as high as 35 % in the nearly 15 million women with urinary incontinence is fairly common in everyday clinical practice [5, 6•]. Estimates of MUI vary. Studies from China report a rate as low as 6 % in Chinese women with urinary incontinence while other studies have found a prevalence rate as high as 61 % [6•, 7–9]. MUI affects women more than men and women of all ages. Multiple studies comparing health-related quality of life (HRQoL) have found that patients with MUI have a greater negative impact on quality of life than either SUI or UUI [6•, 10•, 11, 12].
Incontinence symptoms do not always reveal the true etiology behind an individual’s incontinence. Symptomatology is often inconsistent with urodynamic findings, which are in turn often not reflective of MUI. Physical exam and urodynamic findings will often reveal either SUI or detrusor over-activity (DO) consistent with UUI [4]. These findings were demonstrated in studies by Cardozo and Stanton. Fifty percent of women with mixed symptomatology were found to have only SUI and 40 % of women were found to have only detrusor over-activity during urodynamic testing [13]. Similar findings were reported by Sandvik who found that only half of the patients with MUI symptoms had an identifiable mixed condition [4, 9, 14].
There is an abundance of literature on MUI as well as many developing treatment options for MUI. However, we are still plagued with the same clinical problems today as nearly a decade ago. Conservative treatment aimed at the most bothersome component of a patient’s MUI can improve subjective and objective measures on validated questionnaires, patient-reported symptom improvement, and urodynamic testing. The group of women that do not respond to traditional treatments poses a serious challenge that we have yet to effectively treat. Furthermore, while some studies are based on incontinence symptoms, others are based on urodynamic findings, which render effective comparison of the available results very difficult if not impossible [3••, 4]. The goal of this paper is to review the current literature on MUI and provide a MUI treatment algorithm for clinicians.
Pathophysiology
Parity, vaginal delivery, obesity, diabetes, constipation, family history, and increasing age predispose women to incontinence. Genetic differences in extracellular matrix proteins and androgen receptors may also play a role in the development of mixed urinary incontinence [15].
A separate theory behind the etiology of mixed urinary incontinence is attributed to two separate disease processes, which cumulatively contribute to more bothersome symptoms. Another theory describes behavioral changes in voiding habits in women with MUI. These women retrain the bladder by urinating more frequently to avoid leakage associated with SUI. The patient may rush to the restroom to urinate at the first sensation or first desire. This patterned behavior to avoid stress-induced leakage may lead to a “pseudo-urgency syndrome” [4, 16].
Anatomical changes corresponding to theories accounting for SUI include the following: alterations in the urethrovesical axis, intrinsic sphincter deficiency, hammock theory, and integral theory [10•]. It has also been postulated that accumulation of urine in the proximal urethra can lead to urethral relaxation and detrusor contraction. Additionally, urethral instability and fluctuation in urethral pressure lead to detrusor overactivity and change in the urethrodetrusor reflexes that can lead to a heightened micturition reflex [4].
Workup
Clinicians should focus on medical, neurological, and genitourinary history; explore symptoms in terms of duration, frequency, and most bothersome symptoms; and explore precipitants and treatments. Investigations include a urine dipstick, post void residual, voiding diary, and a thorough physical exam assessing rectal tone, tightness of the perineal body, vaginal mucosa, urethral mobility, and presence of prolapse. Anatomical changes leading to a lax pelvic floor have been found to contribute to MUI symptoms. Quality of life (QOL) questionnaires assessing the impact of urinary incontinence symptoms are useful tools utilized in evaluating MUI. These tools can aid physicians in their assessment and monitoring of a patient’s progress posttreatment [3••, 15]. The 3 Incontinence Questions (3IQ), The Questionnaire for Female Urinary Incontinence Diagnosis (QUID), Stress and Urge Incontinence Quality of Life Questionnaire (SUIQQ), and the International Consultation on Incontinence Questionnaire-short form have received high grade A recommendations from the International Consultation on Incontinence and can be used to diagnose MUI [17].
Although a detailed history and physical exam are important in diagnosing patients with MUI, subjective symptoms are often a poor indicator of the final diagnosis. Secondary testing including cystourethroscopy and urine cytology to rule out pathologic conditions of the bladder are also recommended.
Urodynamics is an important tool in determining the underlying etiology of a patient’s incontinence especially when symptomology is unclear or potentially misleading. The literature however has varying recommendations regarding urodynamics. Digesu et al. state the initial symptom and most bothersome component are more predictive of a patient’s response to a particular treatment than urodynamics findings [18]. Conversely, detrusor overactivity (DO) can be detected on urodynamics in a significantly higher proportion of women with urge urinary incontinence as the predominant component and is helpful in providing guidance in the clinical scenario in which the symptomatic diagnosis is unclear [19]. Recently released SUFU and AUA guidelines on urodynamics state that urodynamics can be utilized to diagnose MUI but is not absolutely necessary to confirm the diagnosis of MUI given that it is a symptomatic diagnosis. The AUA guidelines specifically state that (1) clinicians may perform multi-channel filling cystometry when it is important to determine if altered compliance, DO, or other urodynamic abnormalities are present (or not) in patients with urgency incontinence in whom invasive, potentially morbid, or irreversible treatments are considered. (2) Clinicians may perform pressure flow studies (PFS) in patients with urgency incontinence after bladder outlet procedures or to evaluate for bladder outlet obstruction. (3) Clinicians should counsel patients with urgency incontinence and mixed incontinence that the absence of DO on a single urodynamic study does not exclude it as a causative factor for their symptoms [20••, 21•, 22•].
Videourodynamics, which utilizes fluoroscopy, allows simultaneous assessment of structure and function and is the preferred method for evaluation of mixed symptomatology. Urodynamics is especially important in patients with MUI as it provides information on bladder compliance. Poorly compliant bladders with high pressures can lead to detrimental upper tract damage of the kidneys and ureters. Poor compliance can result from a variety of causes including neurological disease, prolonged catheter drainage, long standing obstruction of the urinary tract, radiation therapy, prior genitourinary surgeries, and interstitial cystitis. Urodynamics should therefore be performed in any patient at risk for poor bladder compliance. Anti-incontinence procedures and medications to correct MUI can risk damaging the upper tracts due to elevated bladder pressures [4]. Urodynamics is routinely performed in patients with MUI symptoms in the authors’ clinical practice prior to proceeding with invasive procedures.
Treatment
MUI treatment is addressed in a stepwise fashion. MUI utilizes either monotherapy or a combination therapy of conservative management, pharmacotherapy, and surgery [10•]. Table 1 reviews the summary of evidence for treatment of MUI.
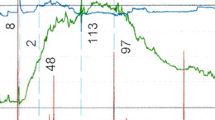
Conservative management includes lifestyle interventions such as weight loss and decreased fluid intake, bladder retraining, anti-incontinence devices such as pessaries, biofeedback, and pelvic floor muscle exercises (PFME). It is the responsibility of the physician to work with the patient in identifying which component of MUI is most bothersome—stress or urge. Based on this assessment, a physician can offer the appropriate initial treatment [10•]. See Fig. 1 for determining which is the most bothersome component.
Pharmacological therapy consists of topical hormone replacement; antimuscarinic drugs (oxybutynin, tolterodine, solifenacin, fesoterodine, darifenacin, trospium); Beta 3 adrenergic agonists (mirabegron); and serotonin/norepinephrine reuptake inhibitors [15, 30]. A typical clinical scenario in MUI patients on anticholinergic therapy is resolution of the urge component in 50–60 % of patients but little to no improvement in the stress component [4, 16].
Multiple trials have been conducted comparing anticholinergic therapy to placebo and surgery. The Mixed Incontinence Effective Research Investigating Tolterodine (MERIT) study, a multinational, double-blinded, placebo controlled trial, evaluated the efficacy of antimuscarinic therapy in patients with urge-predominant MUI. In total, 854 patients with MUI were studied, 634 (74.5 %) with UUI as their initial or predominant symptom. After 8 weeks of treatment 76 % in the drug group reported improvement compared with 53 % in the placebo group [4, 23]. Karram and Bhatia found no significant difference in cure rates in either the SUI or UUI component of 52 MUI patients treated with surgery or medical therapy [5]. Osman et al. compared patients with MUI who received anticholinergic versus either a Burch colposuspension or pubovaginal sling. Persistent UUI was seen in 43 % of patients who received anticholinergic therapy compared to 13 and 12 % in the Burch and sling groups [16].
Surgical treatment of urinary incontinence is planned according to the dominant component of urinary incontinence. If SUI is the dominant symptom, according to the AUA guidelines on surgical treatment of female stress urinary incontinence, one might offer pelvic floor muscle exercise with or without physical therapy and biofeedback, midurethral sling (MUS), peri-urethral bulking injections, or colposuspension. If the above fails, re-evaluate the patient and re-enter the algorithm at the appropriate stage. Consider second-line surgery for SUI if applicable [31]. Conversely, in cases of urge-predominant MUI, in accordance with the AUA/SUFU OAB guidelines, the patient may be offered behavioral and dietary adjustment with physical therapy, pharmacotherapy, intradetrusor botulinum toxin A injection, sacral neurostimulation, percutaneous tibial nerve stimulation, bladder augmentation, or urinary diversion in extreme cases [21•].
As mentioned earlier in this article, mixed symptomatology does not always correlate with a mixed condition. As shown in a handful of studies, surgical correction in patients who underwent either a Burch colposuspension, pubovaginal sling, tension free vaginal tape (TVT), or transobturator tape (TOT) procedure can lead to resolution of urge incontinence and urgency in a majority of patients with MUI symptoms. Scotti and colleagues demonstrated an overall resolution of urgency incontinence in 56.5 % of the 46 MUI patients after Burch colposuspension [32]. Langer and colleagues studied 127 women with MUI who underwent a Burch colposuspension, 33 % had preoperative UUI, and 55 % had urinary urgency. Only 9 % of the patients with preoperative UUI and 25 % of the patients with urgency were still complaining at 1 year postoperatively [33]. Another study by Serels et al. evaluated 36 patients with DO on urodynamics who underwent various pubovaginal sling procedures. Sling procedures included in situ vaginal wall slings, free swing vaginal wall slings, rectus fascia slings, cadaveric fascia slings, and synthetic slings. Preoperatively, 21 (58 %) patients had MUI. SUI was cured in 92 % of these patients with 75 % having resolution of their UUI [34]. Other studies by McGuire, Fulford, and Osman report resolution of urge incontinence in 69–83 % of their patients who had undergone a pubovaginal sling operation [4, 16] . A meta-analysis conducted in 2011 reviewed the effectiveness of mid urethral slings on mixed urinary incontinence. Six randomized trials (RCTs) and seven prospective studies were reviewed. The overall subjective cure from seven prospective non-randomized studies that included patients with symptomatic ± urodynamically proven MUI was found to be 56.4 %. The overall cure of urgency and the UUI component was 30–85 % at a follow-up of a few months to up to 5 years. Most of the studies described found this cure does not persist over time. The cure rate of SUI following MUS varies from 85 to 97 %. On meta-analysis of five RCTs that included women with MUI symptoms, the odds of overall subjective cure with TVT versus TOT tapes are similar at 6–33 months follow-up. This was true when a subgroup analysis was performed on women with MUI who did not demonstrate DO on UDS [28]. A more recent study in 2014 by Abdel Fattah et al. found that transobturator tape procedures are associated with a good (73.8 %) patient reported success rate at a minimum of 3 years of follow up in the surgical management of MUI in women with predominant SUI symptoms. Nearly half of the women reported cure of their urgency and UUI [29•]. A Cochrane review analysis of urethral bulking agents for SUI found limited benefit for MUI [35].
There are a few studies that address the etiology behind the resolution of MUI by fixing the SUI component; however, this resolution can be attributed to preoperative mixed symptomatology rather than a true MUI. Most studies suggest that women with stress-predominant MUI have significantly better cure rates than women with equal stress-urge and urge-predominant MUI. Women with urge-predominant MUI have more postoperative bother [4].
De Novo Urgency and Other Voiding Dysfunctions After Anti-Incontinence Therapy
Existing reports indicates that up to 40 % of patients develop voiding dysfunction after anti-incontinence procedures. Voiding dysfunction discussed here includes persistent or worsening urinary urgency, urethral obstruction, and de novo urgency.
Persistent urinary urgency is symptomatic urgency that does not resolve after anti-incontinence therapy. Persistent urgency can also be manifested with DO on UDS prior to surgery that continues post operatively. It is estimated to be up to 40 % after synthetic sling surgery and ranges from 13.6 to 74 % in women with a history of MUI. Postulated risk factors for persistent urgency are the presence of DO on preoperative urodynamics, increasing age, and increased baseline severity [36•]. These patients have the lowest satisfaction with the procedure and should be appropriately counseled on the data of persistent urgency and urgency incontinence preoperatively.
De novo urgency, on the other hand, is urinary urgency that develops after sling placement and includes new symptoms of frequency, nocturia, urgency, and or UUI. Contributing factors in the development of de novo urgency include postoperative urinary tract infection, urethral obstruction, perforation of the urinary tract and idiopathic urgency. Other theories include increased urethral resistance during voiding, denervation causing detrusor super-sensitivity and over-activity, failed repair of SUI, and intrinsic sphincter deficiency (ISD) [4]. The Ingleman-Sundberg procedure in which there is intentional division of the terminal branches of the pelvic nerves could also cause these symptoms. Urinary tract infections in a large Medicare study have been reported to be as high as 33.6 % in the first 3 months after sling placement [36•]. Urethral obstruction is uncommon with an incidence in the literature ranging from 1 to 19 %. Higher rates of urethral obstruction and repeat surgery have been reported following retropubic sling placement compared to transobturator sling placement [4, 36•, 37]. Urinary tract perforation is a rare complication and the estimated prevalence ranges from 0.5 to 24 % after sling placement. Higher rates are reported in retropubic sling placement with blind passage of trocars [38].
It is especially important to note that there is no preoperative urodynamic parameter that directly correlates with de novo urgency [4, 36•].
Evaluation of Postoperative Voiding Dysfunction
The normal healing process can take up to 6 weeks and it is prudent that the clinician and patient wait this time period postoperatively prior to performing further invasive tests and procedures. It is critical to rule out urinary retention in patients with postoperative voiding dysfunction. Urinary retention can be diagnosed via assessment of the post void residual (PVR). Some authors suggest that a PVR value greater than 60 mL may be suggestive of obstruction in a patient who has undergone a sling without a history of elevated residuals preoperatively [36•]. Evaluation should begin with a thorough history and physical exam. History can clarify the initial onset and bother of symptoms and differentiate between persistent and de novo urgency. A detailed history will also identify any irritative or obstructive voiding symptoms such as gross hematuria, dysuria, pain, urinary tract infections, incomplete emptying, hesitancy, dribbling, or decreased urinary stream. This is also an appropriate time to re-administer QoL and voiding questionnaires to determine any changes post operatively. Voiding diaries can also be helpful in assessing the severity of symptoms.
Physical examination should assess the anterior vaginal wall for the appearance and position of the bladder neck and proximal urethra. Palpation of this same region can also assess for mobility, scarring, pelvic prolapse, and sling extrusion. A catheter or urethral sound placed in the urethra can demonstrate the degree of urethral mobility and allow the examiner to assess for urethral stenosis or obstruction. Cystourethroscopy can rule out a foreign body such as sutures, stones or sling extrusion. Cystoscopy can also evaluate for any neoplasms.
Urodynamics can be done for the same indications mentioned in the workup section of MUI earlier in the body of this paper. Urodynamics can evaluate for any DO and or new altered compliance. Videourodynamics can evaluate the bladder neck for any obstruction. High-pressure low-flow voiding is suggestive of bladder outlet obstruction. While specific data points for females with obstruction on urodynamic testing are lacking, it has been stated that a detrusor pressure greater than 30 cm H20 and peak flow less than 15 mL/s are suggestive of an obstructive voiding pattern. Blavias and Groutz proposed values of detrusor pressure greater than 20 cm H20 and peak flow less than 12 mL/s as suggestive of female bladder outlet obstruction [4, 36•, 39]. A multimodal approach utilizing the aforementioned recommendations is advised in the evaluation of voiding dysfunction after anti-incontinence surgery.
Treatment of Postoperative Voiding Dysfunction
In cases of obstructive uropathy following an anti-incontinence surgery, treat the underlying cause. If there is excessive sling tension, the sling can be incised/excised or urethrolysis can be performed [36•].
If obstruction has been ruled out, treatment similar to idiopathic urgency including bladder-retraining exercises, pharmacotherapy, and limitation of bladder irritants is recommended. If conservative therapy fails, intradetrusor onabotulinumtoxin A injections or xylocaine mixed with steroids injected periurethrally have also been used to treat external sphincter spasticity and dysfunctional voiding [4]. Starkman et al. reported on the success of sacral neuromodulation (SNM) in the management of refractory overactive bladder after urethrolysis for bladder outlet obstruction. On retrospective review, six of eight patients that underwent SNM had a favorable response to SNM with three patients being dry and three patients having one to two urgency incontinence episodes per week [40].
Conclusion
High-quality evidence is lacking for the treatment of mixed urinary incontinence. There is no consensus as to which component to treat first: urge or stress. Most clinicians opt to treat the most bothersome component. It is the authors’ opinion when choosing treatment options, to start with conservative treatment of the urge component before considering surgical therapy for SUI. This can bypass un-needed surgery in a group of patients who respond to non-operative treatment.
There is no sound data suggesting which patients will have success or failure with each treatment option. We have provided a stepwise algorithm from our practice. Although this algorithm has not been validated, it has translated into effective clinical outcomes. There are many new treatment options in development for women with MUI including new pharmacologic agents including potassium channel agonists, calcium channel blockers, phosphdiesterase-5 inhibitors, and neurokinin receptor antagonists [15, 41, 42]. Randomized trials in women with mixed urinary incontinence are needed to validate these treatment options. Only then will we be able to improve the overall cure rates and offer sustained relief to those complex and challenging cases of MUI refractory to standard treatment options. In the meantime, it is best to start with non-operative and conservative treatment of the most bothersome component of a given individual’s MUI.
Abbreviations
- MUI:
-
Mixed urinary incontinence
- SUI:
-
Stress urinary incontinence
- UUI:
-
Urge urinary incontinence
- DO:
-
Detrusor overactivity
- MUS:
-
Midurethral sling
- UTI:
-
Urinary tract infection
- ICS:
-
International Continence Society
- TVT:
-
Transvaginal tape
- TOT:
-
Transobturator tape
- ISD:
-
Intrinsic sphincter deficiency
- SNM:
-
Sacral neuromodulation
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;1(1):5–26. This is the main reference for current terminology regarding voiding dysfunction, female sexual dysfunction and pelvic floor dysfunction.
Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–40.
Myers DL. Female mixed urinary incontinence: a clinical review. JAMA. 2014;311(19):2007–14. This review provides a good case presentation and clinical review of mixed urinary incontinence presented at a obsteretic and gynecology grand rounds prsentation. It also includes a summary of the evidence of mixed, urge and stress urinary incontinence trials mainly from the last decade.
Smith Karen E, McGuire Edward J. Mixed urinary incontinence. In: Rodriguez SR, Larissa V, editors. Female urology third edition. Philadelphia: ELSEVIER SAUNDERS; 2008. p. 477–85.
Karram MM, Bhatia NN. Management of coexistent stress and urge urinary incontinence. Obstet Gynecol. 1989;73(1):4–7.
Sensoy N, Dogan N, Ozek B, Kaaaslan L. Urinary incontinence in women: prevalence rates, risk factors and impact on quality of life. Pak J Med Sci. 2013;29(3):818–22. This study reviews the prevalence of mixed urinary incontinence and its impact on quality of life using multiple health related quality of life tools.
Kogan MI, Zachoval R, Ozyurt C, Schäfer T, Christensen N. Epidemiology and impact of urinary incontinence, overactive bladder, and other lower urinary tract symptoms: results of the EPIC survey in Russia, Czech Republic, and Turkey. Curr Med Res Opin. 2014;30(10):2119–30.
Liu B, Wang L, Huang SS, Wu Q, Wu DL. Prevalence and risk factors of urnary incontinence among Chinese women in Shanghai. Int J Clin Exp Med. 2014;7(3):686–96.
Sandvik H, Hunskaar S, Vanvik A, et al. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. J Clin Epidemiol. 1995;48(3):339–43.
Porena M, Costantini E, Lazzeri M. Mixed incontinence: how best to manage it? Curr Bladder Dysfunct Rep. 2013;8(1):7–12. This article reviews the pathophysiology behind mixed urinary incontinence and new pharmocotherapy trials in progress for the treatment of mixed urinary incontinence.
Petros PE. Mixed urinary incontinence—time to uncouple urgency from stress? Int Urogynecol J. 2011;22(8):919–21.
Milsom I, Coyne KS, Nicholson KM, Cl C, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2014;65(1):79–95.
Cardozo LD, Stanton SL. Genuine stress incontinence and detrusor instability: a review of 200 patients. Br J Obstet Gynecol. 1980;87(3):184–90.
Weidner AC, Myers AG, Ag V, et al. Which women with stress incontinence require urodynamics? Am J Obstet Gynecol. 2001;184(2):20–7.
Grimshaw R, Jain P, Latthe P. Management of mixed urinary incontinence. Womens Health (Lond Engl). 2012;8(5):567–77.
Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU Int. 2003;92(9):964–8.
Corcos J. Outcomes in urinary incontinence: reconciling clinical relevance with scientific rigour. Eur Urol. 2008;53(1):1151–61.
Digesu GA, Derpapas A, Hewett S, Tubaro A, Puccini F, Fernando R, et al. Does the onset or bother of mixed urinary incontinence symptoms help in the urodynamic diagnosis? Eur J Obstet Gynecol Reprod Biol. 2013;171(2):381–4.
Kulseng-Hanssen S, Moe K, Schiotz HA. How often does detrusor overactivity cause urinary leakage during a stress test in women with mixed urinary incontinence? Int Urogynecol J. 2013;24(9):1537–41.
Collins CW, Winters JC. American urological association; society of urodynamics female pelvic medicine and urogenital reconstruction. Urol Clin N Am. 2014;41(3):353–62. This article guides clinicians in the role of urodynamics in the evaluation and management of complex lower urinary tract conditions. It examines each guideline statement and provides a clinical context for each statement.
Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA SUFU guideline. J Urol. 2012;188(6):2455–63. These guideliens detail the evaluation for overactive bladder and the various tretament options avialable. Beta agonists and botulinum toxin are excluded in these guidelines however were approved by the FDA for idiotpathic overactive bladder after publication of these guidelines.
Patel BN, Kobashi KC. Practical use of the new American Urological Association adult urodynamics guidelines. Curr Urol Rep. 2013;14(3):240–6. Reviews the recently published AUA urodynamics guidelines and its application in everyday clinical practice.
Khullar V, Hill S, Laval KU, et al. Treatment of urge-predomnant mixed urinary incontinence with tolterodine extended release: a randomized, placebo-controlled trial. Urology. 2004;64(2):269–74.
Staskin DR, Te AE. Short and long term efficacy of solifenacin treatment in patients with symptoms of mixed urinary incontinence. BJU Int. 2006;97(6):1256–61.
Kulseng-Hansen S, Husby H, Schiotz HA. The tension free vaginal tape operation for women with mixed incontinence: do preoperative variables predict the outcome? Neurourol Urodyn. 2007;26(1):115–21.
Kulseng-Hansen S, Husby H, Schiotz HA. Follow-up of TVT operations in 1113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):391–6.
Townsend MK, Jura YH, Curhan GC, et al. Fluid intake and risk of stress, urgency and mixed urinary incontinence. Am J Obstet Gynecol. 2011;205(1):e1–6.
Jain P, Jirschele K, Botros SM, Latthe PM. Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2011;22(8):923–32.
Abdel-Fattah M, Hoppstafa A. Evaluation of transobturator tension-free vaginal tapes in the surgical management of mixed urinary incontinence: 3-year outcomes of a randomized controlled trial. J Urol. 2014;191(1):114–9. This is the most recent prospective, single blind, randomized controlled trial reporting favorable outcomes of transobturator tape procedure in the surgical management of women with mixed urinary incontinence in 3 years of follow up.
Bump RC, Norton PA, Zinner NR, et al. Mixed urinary incontinence symptoms: urodynamic findings; incontinence severity, and treatment response. Obstet Gynecol. 2003;102:76–83.
Dmochowski RR, Blavias JM, Gormely EA, Juma S, Karram MM, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010;183(5):1906–14.
Scotti RJ, Angell G, Flora R, et al. Antecedent history as a predictor of surgical cure of urgency symptoms in mixed incontinence. Obstet Gynecol. 1998;91:51–4.
Langer R, Lipshitz Y, Halperin R, et al. Long term (10-15 years)follow-up after Burch colposuspension for urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:1290–1.
Serels SR, Rackley RR, Appell RA. Surgical treatment for stress urinary incontinence associated with Valsalva induced detrusor instability. J Urol. 2000;163:884–7.
Ayeleke RO, Hay-Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database Syst Rev. 2013;20:11.
Abraham N, Vasavada S. Urgency after a sling: review of the management. Curr Urol Rep. 2014;15(4):400. This review summarizes the workup and treatment of de novo urgency after a sling - a common occurrence in women with mixed urinary incontinence.
Richter HE, Albo ME, Zyczynski HM, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;3629(22):2066–76.
Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: important outcomes for future clinical trials. J Urol. 2008;180(5):1890–7.
Blavias JG, Groutz A. Urinary incontinence: pathophysiology, evaluation, and management overview. In: Walsh PC, Retik A, Vaughan ED, Wein AJ, editors. Campbell's urology, 8th ed. Philadelphia: Saunders; 2002. p. 1027–52.
Starkman JS, Duffy III JW, Wolter CE, et al. Refractory overactive bladder after urethrolysis for bladder outlet obstruction: management with sacral neuromodulation. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(2):277–82.
Petkov GV. Role of potassium ion channels in detrusor smooth muscle function and dysfunction. Nat Rev Urol. 2012;9(1):30–40.
Andersson KE. Prospective pharmacologic therapies for the overactive bladder. Ther Adv Urol. 2009;1(2):71–83.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Nazia Q. Bandukwala declares no potential conflicts of interest. Dr. Angelo E. Gousse is a consultant and investigator for Allergan.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Female Urology
Rights and permissions
About this article
Cite this article
Bandukwala, N.Q., Gousse, A.E. Mixed Urinary Incontinence: What First?. Curr Urol Rep 16, 9 (2015). https://doi.org/10.1007/s11934-015-0483-0
Published:
DOI: https://doi.org/10.1007/s11934-015-0483-0