Abstract
Introduction and hypothesis
The study sought to identify the risk factors of postoperative use of antimuscarinics after transobturator surgery in women with mixed urinary incontinence (MUI) displaying both urodynamic stress urinary incontinence (SUI) and involuntary detrusor contraction (IDC) with leakage in urodynamic study.
Methods
The clinical data of 103 patients with MUI who underwent transobturator tape (TOT) sling surgery were retrospectively reviewed. The patients were followed at least a year. To determine risk factors for postoperative use of antimuscarinics, variables of only those with P values < 0.05 on univariate analysis were included in the multivariate logistic regression analysis with forward stepwise building.
Results
Eight-four (81.6 %) of 103 patients were included in this study. The cure rate of urge urinary incontinence (UUI) was 69.0 % (58/84). Antimuscarinics were prescribed postoperatively in 22 (26.2 %) of 84 patients. Variables affecting postoperative use of antimuscarinics were age, parity, episode of any UUI, preoperative use of antimuscarinics, predominant urgency incontinence type, detrusor pressure at maximum flow, and Urogenital Distress Inventory 6. Increasing age and preoperative use of antimuscarinics increased the odds of postoperative use of antimuscarinics following TOT surgery.
Conclusion
Patients who were older and had taken antimuscarinics preoperatively were significantly associated with postoperative use of antimuscarinics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mixed urinary incontinence (MUI) is therapeutically challenging due to the heterogenous nature of symptoms, signs, and urodynamic observations. Conditions such as urodynamic stress urinary incontinence (SUI) and urgency, or urodynamic SUI and detrusor overactivity (DO), or urodynamic SUI and involuntary detrusor contraction (IDC) with leakage are classified as MUI. There has been some evidence of persistent and good cure of the stress component following midurethral sling surgery in women with MUI [1, 2]. The cure rate of urgency or urge urinary incontinence (UUI) is variable, and the postoperative course of UUI can unpredictably resolve, persist, or worsen [3–7]. There is no consensus as to what patient or surgical factors contribute to the success of anti-incontinence procedures in resolving the urge or UUI component. Similarly, no consistent predictors of persistent urgency or UUI after midurethral sling surgery have been identified. The purpose of this study was to elucidate risk factors of postoperative use of antimuscarinics following midurethral sling surgery in patients with MUI whose urodynamic study showed both urodynamic SUI and IDC with leakage
Methods
This study assessed a retrospective cohort of 103 women who underwent transobturator (TOT) sling surgery (Monarc; American Medical Systems, Minnetonka, MN, USA) between April 2008 and August 2010. Preoperatively, all women underwent routine assessment, including gynecologic history, physical examination with Pelvic Organ Prolapse Quantification (POP-Q) system, urinalysis, postvoid residual volume, uroflowmetry, and multichannel urodynamic evaluation. Patients also completed a Urinary Distress Inventory (UDI)-6 questionnaire. The terminology was consistent with the joint report of the International Urogynecological Association (IUGA)/International Continence Society (ICS) [8]. The methods and units used in the urodynamic study were followed to the standards recommended [9, 10].
In all patients, MUI was confirmed by urodynamic study, where the coexistence of SUI and UUI was demonstrated by leakage of urine with the Valsalva maneuver or cough in the absence of detrusor contraction, and involuntary urinary leakage combined with DO or secondary uninhibited detrusor contraction. The predominant type of MUI was determined by more severe and bothersome incontinence based on history, UDI-6, and urodynamic findings. Urge-predominant MUI was managed initially with pelvic floor muscle training (PFMT) and antimuscarinics. The stress-predominant MUI was managed with PFMT or surgery. Surgery was recommended for patients with urge-predominant MUI who did not respond to treatment with antimuscarinics after 8–12 weeks.
TOT sling surgery was performed in the standard manner, as previously described [11]. Under spinal anesthesia, helical needles were passed from a groin incision into the labiocrural folds at the superior medial border of the obturator foramen to the vagina incision beneath the midurethra under the guidance of the operator’s ipsilateral index finger bilaterally. Intraoperative cystourethroscopy was routinely performed. Concomitant gynecologic surgery was done in 59.5 % of patients, posterior colporrhaphy in 29.8 %, uterosacral vaginal-vault suspension surgery in 8.3 %, laparoscopic hysterectomy in 7.1 %, laparoscopic adnexal surgery in 4.8 %, laparoscopic myomectomy in 2.4 %, open sacrocolpopexy in 2.4 %, and laparoscopic sacrocolpopexy in 2.4 %. Anterior and posterior colporrhaphy and vaginal hysterectomy were each done in 1.2 % of patients.
Postoperative evaluations were scheduled at 6 weeks, 6 months, 12 months, and annually thereafter. At follow-up, patients were evaluated using supine stress test, uroflowmetry, and postvoid residual urine volume; completed the UDI-6 questionnaire; and were asked about the use of antimuscarinics following surgery [12]. Telephone interviews were attempted with women who missed follow-up. The subjective cure was assessed by UDI-6 scores and nonuse of postoperative antimuscarinics. Objective cure was assessed by no leakage on cough stress test.
Patients were divided into user and nonuser groups based on antimuscarinics after TOT surgery. Institutional review board approval was obtained prior to performing the chart review. Statistical analyses were done using SAS statistical software (SAS Institute, Cary, NC, USA) and R(version 2,2,0). Chi-square tests and independent t tests were used to compare baseline characteristics and parameters of the postoperative use/nonuse of antimuscarinics. To determine the possible affecting factors for postoperative use of antimuscarinics after TOT surgery, variables of only those with P values < 0.05 on univariate analysis were included in the multivariate logistic model. The multivariate logistic regression analysis with a forward stepwise building of an optimal model for prediction was built up for maximum likelihood estimates of the odds ratio (OR) and 95 % confidence intervals (CIs).
Results
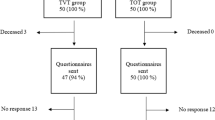
Eighty-four (81.6 %) of 103 women were followed up at 12 months after surgery. Nineteen patients who missed follow-up could not be contacted because of death (n = 1) and change of telephone number (n = 18). Baseline characteristics and parameters of the 84 patients are summarized in Table 1. All women expressed bothersome urgency, and 61.3 % of women had experienced episodes of UUI. All patients showed both SUI and IDC with leakage in the urodynamic study. Preoperatively, antimuscarinics were prescribed in 20 (24 %) of the 84 women. The median postoperative follow-up was 23 (range 12–40) months.
The objective and subjective cure rate for SUI was 96.4 % (81 of 84) and 86.9 % (73 of 84), respectively. The cure rate of UUI was 69.0 % (58 of 84). The scores of UDI-6 significantly improved postoperatively from 55.4 to 11.8 (p < 0.01). The proportion of postoperative non-use of antimuscarinics was 73.8 %. Among women who reported any UUI after surgery, 22 (84.6 %) of 26 had taken antimuscarinics postoperatively. They started to take antimuscarinics from as early as 1 month to 6 months following surgery. The reasons the remaining four women who did not take antimuscarinics were that the bladder problem would be solved by frequent voiding (n = 2), did not like taking any medications (n = 1) and no reasons reported (n = 1). Eleven (55 %) of 20 women who had taken antimuscarinics preoperatively did not take antimuscarinics after surgery.
Table 2 shows the characteristics and parameters of the user or nonuser of postoperative antimuscarinics groups. The proportion of those who took antimuscarinics postoperatively was 26.2 % (22 of 84). Women who took postoperative antimuscarinics were older and showed more predominant UUI type. Their parity was higher, and they displayed a higher detrusor pressure at maximum flow. They were more likely to complain of bothersome daytime frequency and nocturia and had higher UDI-6 scores; however, these differences were not statistically significant. They were more likely to complain of any UUI (89.5 % vs 41.1 %, p = 0.001) and take antimuscarinics preoperatively (40.9 % vs 18.0 %, p = 0.043).
Variables affecting postoperative use of antimuscarinics were examined using multivariate logistic regression analysis with a forward stepwise building of an optimal model for prediction: age, parity, episode of any UUI, preoperative use of antimuscarinics, predominant UUI type, detrusor pressure at maximum flow, and UDI-6 scores. Table 3 shows the results of the independent risk factors for users of postoperative antimuscarinics. Older age and preoperative use of antimuscarinics increased the odds of postoperative antimuscarinic use following TOT (OR:1.08, p = 0.0043 and OR:3.938, p = 0.0206, respectively).
Discussions
MUI remains a complex clinical condition representing diverse groups with symptom- and urodynamics-based diagnosis. The variances in the definition and outcome measures of MUI contributed to the wide variation of cure rate of urinary incontinence following surgery in MUI. In this study, we selected cases whose urodynamic study showed both stress and IDC with leakage. The validated UDI-6 questionnaire and postoperative use of antimuscarinics were used as outcome measures with a minimum follow-up of 12 months instead of objective parameters of UUI, such as urodynamic study or voiding diary. UDI-6 questionnaire is a relevant way to assess patient perception of incontinence severity in women with MUI [13]. Limitations of our study are retrospective design and relatively short-term follow-up.
The cure rate of SUI and UUI following surgery has been reported to be 83–97 % and 40–85 %, respectively [2, 14–16]. Our study revealed that the objective and subjective cure rate for SUI was 96.4 % and 86.9 %, respectively. The cure rate of UUI was 69 % and the proportion of nonuse of postoperative antimuscarinics was 73.8 %. Two patients (2.4 %) showed aggravation of urgency or UUI after surgery. In a prospective study of midurethral retropubic sling surgery [transvaginal tape (TVT)] with follow-up of 4 years where coexistence of stress and IDC with leakage was confirmed urodynamically, a higher cure rate of both SUI and UUI (85 %) was shown, and treatment failure rate was 11 % [3]. Of the cured or improved group, 25 % had urgency without incontinence. Contrary to this, Duckett et al. reported a higher cure rate of SUI (97 %) and lower cure rate of UUI (30 %) in a prospective study of 77 women who showed urodynamically proven MUI after TVT [16]. A retrospective study demonstrated a 44 % resolution rate of UUI in 457 women with urodynamically proven MUI after transvaginal sling surgery. The only predictor of persistent UUI was sling type (OR: TOT 1.00, bladder-neck sling 4.06, SPARC 2.25, TVT 1.77; p < 0.001) [17]. In a symptomatic MUI group, the resolution rate of urgency or UUI was not consistent according to the type of midurethral sling surgery. Botros et al. reported a significantly higher deterioration rate of preoperative UUI (14–16 %) after midurethral retropubic sling surgery, such as TVT or SPARC, compared with 6 % after TOT [6]. However, Shierlitz et al. showed that the rate of resolution and new development of overactive bladder symptoms were not significantly different between TVT and TOT [18]. To date, there is a lack of controlled studies showing whether type of midurethral sling surgery predicts persistent urgency/UUI.
We also tried to elucidate specific urodynamic parameters associated with an increased risk for postoperative use of antimuscarinics. Women showing lower maximum cystometric capacity and higher detrusor pressure at maximum urinary flow were more likely to be postoperative users of antimuscarinics. However, these differences disappeared in multivariate analysis. The postoperative use of antimuscarinics tended to be associated with predominant UUI type, bothersome daytime frequency, nocturia, more episodes of UUI, higher UDI-6 score, and more relaxed vaginal wall. These differences also disappeared in the multivariate analysis. In some studies, low maximal urethral closure pressure, lower maximum cystometric capacity, or high-pressure motor UUI have been reported to be associated with persistent UUI in women with MUI [17, 19, 20]. No consistent urodynamic parameters or preoperative risk factors predicting persistent urgency/UUI have been identified in women with MUI following surgery
Our study showed that 55 % of women who had taken antimuscarinics preoperatively did not take antimuscarinics after surgery, and the proportion of postoperative users of antimuscarinics was 26.2 %. Segal et al. reported that 57.7 % of those who used antimuscarinics preoperatively no longer took antimuscarinics after TVT surgery in a retrospective study of 98 women with urodynamic SUI, symptomatic UUI, and overactive bladder [5]. Our results concerning discontinuation or postoperative use of antimuscarinics may be clinically helpful and can be used in preoperative counseling of patients with MUI who need to surgery. Our multivariate analysis showed that age and preoperative use of antimuscarinics in women with urodynamically proven MUI undergoing TOT sling surgery were independent risk factors for postoperative use of antimuscarinics. This was not different from our expectation. SUI and UUI may be not independent but could be a pathophysiologically linked condition associated with bladder control problems [21, 22]. With advancing age, these changes are evident from epidemiologic and clinical evidence [23–25]. Significant improvement of UUI in women with MUI treated with surgery may suggest that the UUI component of MUI comes from a severe and advanced stage of SUI. The condition of poor pelvic floor support, incompetent bladder neck, and urethral hypermobility in cases of severe SUI could allow urine to be forced into the proximal urethra during physical activity, causing urethrodetrusor facilitative reflexes and triggering an IDC with leakage [21, 22, 26]. The stabilized and competent urethra with anti-incontinence surgery can correct both SUI and UUI. Patients who used antimuscarinics preoperatively would be more likely to be in the predominant UUI group and if they have ever experienced resolution of overactive symptoms with antimuscarinics and would be willing to add medications following surgery. Further prospective studies with longer follow-up are necessary to explore the risk factors predicting either resolution or persistence of urgency/UUI in women with urodynamically proven MUI following midurethral sling surgery.
Conclusion
The incidence of postoperative use of antimuscarinics was 26.2 % in women with MUI defined as coexistence of SUI and IDC with leakage by urodynamic study after TOT at 1-year follow-up. Those who were older and had used antimuscarinics preoperatively were significantly associated with postoperative use of antimuscarinics.
References
But I, Faganelj M (2008) Complications and short-term results of two different transobturator techniques for surgical treatment of women with urinary incontinence: a randomized study. Int Urogynecol J 19:857–861
Kulseng-Hamssen K, Husby H, Schiotz HA (2008) Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J 19:391–396
Rezapour M, Ulmsten U (2001) Tension-free vaginal tape (TVT) in women with mixed urinary incontinence - a long-term follow up. Int Urogynecol J 12(Supp 2):S15–S18
Kershen RT, Appell RA (2002) De novo urge syndrome and detrusor instability after anti-incontinence surgery: current concepts, evaluation and treatment. Curr Urol Rep 3:345–353
Segal JL, Vassallo B, Kleeman S, Silva WA, Karram MM (2004) Prevalence of persistent and de novo overactive bladder symptoms after the tension-free vaginal tape. Obstet Gynecol 104:1263–1269
Botros SM, Miller JJ, Goldberg RP et al (2007) Detrusor overactivity and urge urinary incontinence following trans obturator versus midurethral slings. Neurourol Urodyn 26:42–45
Tahseen S, Reid P (2009) Effect of transobturator tape on overactive bladder symptoms and urge urinary incontinence in women with mixed urinary incontinence. Obstet Gynecol 113:617–623
Haylen BT, Dd R, Freeman RM et al (2010) An international urogynecological association (IUGA)/international continence society(ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20
Schafer W, Abrams P, Liao L et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21:261–274
Roiser PF, Gajewski JB, Sand PK, Szabo L, Capewell A, Hosker GL (2010) Executive summary: the international consultation on incontinence 2008-Commitee on “dynamic testing” for urinary incontinence and for incontinence. Part 1: innovations in urodynamic techniques and urodynamic testing for signs and symptoms of urinary incontinence in female patients. Neurourol Urodyn 29:140–145
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193:103–113
Lowenstein L, Kenton K, FitzGerald MP, Brubaker L (2008) Clinically useful measures in women with mixed urinary incontinence. Am J Obstet Gynecol 198:664.e1–664.e4
Richter HE, Albo ME, Zyczynski HM et al (2010) Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 362:2066–2076
Meschia M, Bertozzi R, Pifarotti P et al (2007) Peri-operative morbidity and early results of a randomized trial comparing TVT and TVT-O. Int Urogynecol J 18:1257–1261
Duckett J, Aggarwal I, Patil A, Vella M (2008) Effect of tension free vaginal tape position on the resolution of irritative bladder symptoms in women with mixed incontinence. Int Urogynecol J 19:237–239
Gamble TL, Botors SM, Beaumont JL, Goldberg RP, Miller JR, Adeyanju OA, Sand PK (2008) Predictors of persistent detrusor overactivity after transvaginal sling procedures. Am J Obstet Gynecol 199:696.e1–696.e7
Schierlitz L, Dwyer PL, Rosamilia A et al (2008) A prospective analysis of the effect of TVT retropubic and Monarc trans-obturator sling on lower urinary tract symptoms (LUTS) in women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD). Int Urogynecol J Pelvic Floor Dysfunct 19:S43
Paick J-S, Ku JH, Kim SW, Oh S-J, Son H, Shin JW (2004) Tension-free vaginal tape procedure for the treatment of mixed urinary incontinence:significance of maximal urethral closure pressure. J Urol 172:1001–1005
Schrepferman CG, Griebling TL, Nygaard IE, Kreder KJ (2000) Resolution of urge symptoms following sling cystourethropexy. J Urol 164:1628–1631
Jung SY, Fraser MO, Ozawa H et al (1999) Urethral afferent nerve activity affects the micturition reflex; implication for the relationship between stress incontinence and detrusor instability. J Urol 162:204–212
Bump RC, Norton PA, Zinner NR, Yalcin I, Duloxetine Urinary Incontinence Study Group (2003) Mixed urinary incontinence symptoms: urodynamic findings, incontinence severity, and treatment response. Obstet Gynecol 102:76–83
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S, Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trondelag (2000) A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trondelag. J Clin Epidemiol 53:1150–1157
Townsend MK, Danforth KN, Lifford KL et al (2007) Incidence and remission of urinary incontinence in middle-aged women. Am J Obstet Gynecol 197:e1–e5
Holmgren C, Nilsson S, Lanner L, Hellberg D (2005) Long-term results with tension-free vaginal tape on mixed and stress urinary incontinence. Obstet Gynecol 106:38–43
Serels SR, Rackley RR, Appell RA (2000) Surgical treatment for stress urinary incontinence associated with Valsalva induced detrusor instability. J Urol 163:884–887
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoo, EH., Kim, D. Predictors of postoperative antimuscarinics in women with mixed urinary incontinence after transobturator surgery. Int Urogynecol J 24, 401–406 (2013). https://doi.org/10.1007/s00192-012-1880-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1880-2