Abstract
For young patients with irreparable meniscal tears or previously meniscectomized knees, meniscal allograft transplantation (MAT) has been established as a safe and effective method to increase the tibiofemoral contact area, decrease contract stress, and restore the physiologic mechanics of the knee. Appropriately sized allografts are implanted using either the bridge-in-slot or bone plug technique for bony fixation, and any associated ligamentous or chondral pathologies are addressed concomitantly. Following rehabilitation, patients generally experience significant improvements in pain and function, and most patients are able to return to physical activity or sport within 6–9 months postoperatively. While animal models have demonstrated that meniscal transplantation slows the rate of degenerative cartilage changes, the chondroprotective effect of MAT in humans remains unclear.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
I. S. Smillie, the Scottish surgeon who pioneered the operative treatment of meniscus injuries, wrote that “treatment consists of excision of the meniscus; and the sooner the torn degenerate structure is removed, the better is the immediate and long-term result.” [1] Yet, well before Smillie performed his 6500th total meniscectomy in 1965, T. J. Fairbank’s radiographic analysis of meniscectomized patients revealed evidence that removing the meniscus leads to unintended consequences [2]. Fairbank described flattening of the femoral condyle, formation of a ridge on the femoral condyle, and joint space narrowing, suggesting that meniscectomy alters the biomechanics of the knee in such a way that the articular surfaces are overloaded [2]. The early progression of arthritic changes observed in early meniscus-deficient patients were then supported by long-term studies that showed unsatisfactory functional outcomes and a high risk of eventual total knee arthroplasty [3,4,5].
Although patients often report good clinical outcomes following surgery, meniscectomy leads to degeneration of the cartilage and subchondral bone in as little as 5 years, due to the disruption of normal knee kinematics [6,7,8,9]. As increasingly large amounts of meniscus are removed from the knee, the contact area between the tibia and femur decreases, causing a subsequent increase in tibiofemoral contact stress [10]. Biomechanical studies have demonstrated that intra-articular contact stresses double following medial meniscectomy and triple following lateral meniscectomy [11,12,13,14,15]. Peak contact pressure increases proportionally to the percentage of meniscus removed and damage to articular cartilage occurs at the area of peak contact pressure, illustrating the impaired ability of meniscus deficient knees to accommodate stress [10, 16, 17].
The intact meniscus plays several roles related to the overall health and function of the knee. Removing the meniscus in whole or part weakens the ability of the meniscus to perform each of these roles optimally. In addition to increasing the contact area of the tibiofemoral joint and diminishing the intra-articular shock absorption [10], meniscectomy destabilizes the knee joint. The native meniscus acts an important secondary stabilizer to protect against anterior–posterior motion of the joint, and medial meniscectomy yields a significant increase in anterior tibial translation, especially in ACL-deficient knees [18]. The meniscus also assists with lubrication of the knee joint and contains mechanoreceptors that provide proprioception, both of which are compromised following meniscectomy [19, 20].
The end result of altered knee mechanics, excessive contact forces, and impaired joint stability is a significantly increased risk of osteoarthritis in meniscus deficient knees [21]. Forty years after undergoing total meniscectomy with Dr. Smillie, a cohort of 53 of his patients were evaluated in what is the longest available follow-up duration of meniscus-deficient patients to date. Clinical and radiographic evaluation revealed that meniscectomy was associated with a fourfold increase in risk of developing osteoarthritis and a 132-fold increase in the rate of total knee arthroplasty compared to a matched cohort [5].
Despite the deleterious effects of meniscectomy, the procedure clearly continues to play an important role in the treatment of symptomatic meniscus injuries. While the management of meniscus injuries has shifted away from total meniscectomy in favor of preserving tissue or repairing tears whenever possible, there are situations in which meniscectomy is warranted. For patients with symptomatic meniscus tears that are poor candidates for repair, meniscectomy remains the best option. However, given the association between meniscus deficiency and osteoarthritis, there is an obvious role for a procedure that protects the articular cartilage from future degradation.
Several of the first recorded attempts to replace an injured meniscus occurred in 1916 and 1933 by several surgeons who performed autologous fat flap interpositional arthroplasties [22]. In the early 1900s, complete knee transplantations included meniscal allografts [23]. In the 1980s, surgeons attempted to repair tibial plateau fractures with large osteochondral allografts that included the meniscus [24]. The first meniscal allograft transplants (MAT) resembling modern techniques were reported by Milachowski in 1989. The author concluded that MAT is a safe and effective procedure for restoring stability and function to meniscus deficient knees [22].
Roughly 30 years after Milachowski presented his cohort of successful MATs, the procedure has become an established method of optimizing knee function and protecting against the long-term consequences of meniscectomy. Animal models have demonstrated that MAT, whether performed immediately after meniscectomy or in delayed fashion, slows the rate of degenerative chondral changes but does not cease articular degeneration completely [25, 26]. The same chondroprotective benefits have yet to be definitively demonstrated in humans. However, for young patients with irreparable meniscal tears or who have previously undergone meniscectomy in the setting of maintained articular surfaces, MAT can be used to successfully increase the tibiofemoral contact area, decrease contract stress, and restore the physiologic mechanics of the knee [13, 27,28,29].
Indications and Contraindications
Indications
In general, meniscal allograft transplantations are performed in young patients who present with symptomatic meniscal deficiency [30, 31]. The deficiency in this patient population is typically the result of a recurrent tear, failed attempt at repair, or a complex meniscal injury leading to total or subtotal meniscectomy. Patients will often present with a history of multiple ipsilateral knee injuries with associated ligament or cartilage pathology, as well as a failed trial of nonoperative management. MAT is most often performed in patients that are deemed too young for unicondylar or total knee arthroplasty who want to restore normal knee mechanics.
The indications for the procedure include an absent or nonfunctioning meniscus causing activity-related pain in nonobese patients less than 50 years of age. Although ideally patients selected for MAT have Outerbridge grade II articular changes or less in the affected compartment, there is evidence to suggest that patients with advanced articular cartilage degradation should not be excluded from MAT [32, 33]. While MAT is thought to be chondroprotective, prophylactic transplantation in asymptomatic meniscus-deficient patients is not currently an accepted indication.
Contraindications
Contraindications for MAT include age greater than 50 years, flattening of the femoral condyle or tibial plateau (Fairbank changes on plain radiographs), osteophytes or other architectural changes, inflammatory arthritis, synovial disease, preoperative loss of knee extension greater than 5°, preoperative flexion less than 125°, and obesity due to concern that the elevated level of stress would increase risk of graft failure [30, 31, 34,35,36,37]. As discussed above, advanced articular disease with Outerbridge grade III or IV changes has typically been used as a contraindication to MAT, although this may not be necessary, as concomitant cartilage repair procedures can be performed [32, 33]. It should be noted that many of the generally accepted contraindications for MAT are theoretical and there is no objective data demonstrating inferior outcomes with these comorbidities.
Although intact ligaments, normal lower extremity alignment, and pristine cartilage make preoperative planning for the MAT more straightforward, combinations of associated knee pathology do not exclude patients from transplantation. However, these associated injuries must be addressed either concurrently with MAT or in a staged fashion. When malalignment, ligamentous instability, and focal chondral defects are not corrected, the success of the MAT is limited. When these pathologies are addressed simultaneously, clinical outcomes are not different than performing the procedures in isolation [38,39,40,41,42,43,44,45,46,47].
Patients with meniscus deficiency and abnormal lower extremity alignment should have corrective osteotomy performed at the time of meniscus transplant or in a staged fashion with osteotomy preceding the MAT by several months [48, 49]. Similarly, patients with injuries of both the meniscus and one or more ligaments should undergo simultaneous meniscal transplant and ligament reconstruction [50]. An isolated chondral lesion is also not a contraindication for surgery, provided that a cartilage-restoring procedure, such as an osteochondral allograft transplantation or autologous chondrocyte implantation, is also performed [45, 51, 52].
Graft Preparation
Processing and Preservation
There are a variety of methods for processing and preserving meniscal allografts prior to implantation. As MAT becomes more common, optimizing this process will become critical in order to ensure that allografts are readily available in a variety of sizes that can be matched with the recipient’s anatomy.
There are four methods currently available for preservation of meniscal allografts. Lyophilization, in which grafts are dehydrated and frozen in a vacuum, has been associated with a greater risk of effusion and synovitis compared to alternative methods of graft preservation [22, 53]. The process destroys the viable cell population, and after implantation these grafts undergo remodeling which causes the meniscus to shrink [54,55,56]. This process is no longer recommended for MAT.
Cryopreservation involves freezing the grafts using dimethyl sulfide or glycerol. This process preserves viable chondrocytes, but metabolic activity of the cells decreases with longer storage times [57]. In vitro studies have demonstrated that the process of cryopreservation does not affect the ultrastructure of the meniscus and likely does not alter the biomechanical properties, but the population of viable cells is highly variable and unpredictable at the time of implantation [58]. Further studies of cryopreservation have shown that the preservation process induces an apoptosis-mediated decreased in the cell population [59]. The clinical implications of these findings are not currently well understood.
Fresh allografts must be harvested within 12 hours of cold ischemia time, and can then be stored at 4 °C for 7 days before there is loss of viable cells. These grafts contain the greatest number of viable cells, which is thought to help maintain the mechanical integrity of the graft [23, 56].
The most easily available, and generally most cost-effective, type of graft is the fresh-frozen allograft [60, 61]. These menisci are harvested and stored at −80 °C. Animal models have shown that at 4 weeks after implantation, there are no appreciable donor fibrochondrocytes remaining in fresh-frozen allografts, but host cells have populated the graft by this time point [62].
Irradiation of the graft was previously recommended, but is no longer performed due to studies demonstrating deleterious effects on the mechanical properties of the graft [40, 63,64,65,66]. Furthermore, immune-matching of the donor and recipient was originally performed in early cases of MAT, but was eventually found to provide no additional benefit, and is therefore no longer required [18, 67]. Rejection of the allograft is rare, as the meniscus is believed to be immune-privileged, perhaps because the chondrocytes are embedded in a dense proteoglycan network and less accessible to host immune cells [23, 68].
Sizing
Graft sizing is one of the most critical aspects of MAT because the size of the graft is closely associated with the resulting biomechanics, and suboptimal contact forces can negatively affect functional outcomes. The meniscus allograft should be sized to closely match the native meniscus, with meniscus width being the most important dimension. A study of lateral meniscus allografts demonstrated that oversized grafts prevent compressive forces from being appropriately distributed across the joint and may lead to excessive stress on the cartilage. Conversely, undersized grafts lead to excessive forces across the meniscus allograft itself, increasing the risk of postoperative tearing and failure [69]. Most studies conclude that mismatches of graft size within 10% of the native meniscus size are acceptable [69].
Until recently, the most common method of preoperative allograft sizing was performed using plain radiographs and the Pollard technique, originally described by Matthew Pollard in 1995 [70]. With this technique, the medial meniscus width is determined from the AP radiograph as the distance between one vertical line that runs tangent to the most medial aspect of the tibial metaphysis and another vertical line that runs through the peak of the medial tibial spine. Lateral meniscus width is measured using corresponding points on the lateral tibial metaphysis and lateral tibial spine (Fig. 9.1). The lines used for width sizing should be perpendicular to the joint line and parallel to each other. Basing meniscal width on the edge of the metaphysis, rather than the joint space, helps to avoid measurement errors associated with osteophytes in patients with arthritis [70].
Meniscus length is determined on a lateral radiograph as the distance between most anterior point of the tibia superior to the tuberosity and a line tangent to the posterior aspect of the tibia at the level of the joint line. These lines should be parallel and, if the knees are extended, posteriorly tilted approximately 7° to align with the normal anatomic orientation of the tibial joint surface in the sagittal plane. Because the true length of the meniscus does not extend to these bony landmarks, the measured distance is then multiplied by 0.8 for medial meniscus sizing or 0.7 for lateral meniscus sizing [70].
While the method outlined by Pollard continues to be a useful technique for graft sizing in situations where the surgeon must rely on radiographs, follow-up studies have often failed to reproduce the reported level of accuracy originally associated with this technique [71, 72]. As a result, MRI sizing has become more common and is now generally regarded as the gold standard due to its superior accuracy [73,74,75,76]. In a direct comparison of several meniscal allograft–sizing techniques, the Pollard technique was found to significantly overestimate the width and length of the lateral meniscus. The Pollard technique is therefore not recommended for lateral meniscus sizing. If a plain radiograph must be used (e.g., MRI is not available), a mathematical correction to the Pollard technique has been developed and found to yield more accurate measurements [77, 78]. For the medial meniscus, the Pollard technique was found to be comparable to MRI sizing [77]. However, it is important to note that deviation from true AP and lateral views on the radiograph significantly decreases the accuracy of measurements [76].
Regardless of the method used to size the allograft, each dimension should be measured independently as length cannot be used to accurately predict width of the meniscus [79]. If a patient has already undergone meniscectomy and the native ipsilateral meniscus cannot be measured, the size can be approximated using the contralateral meniscus, although there are often differences between meniscus sizes within individuals [80]. One group developed a formula based on patient height, weight, and gender to mathematically predict meniscus dimensions. Although likely less reliable than MRI measurements, this remains an option for patients with bilateral meniscal deficiency, making imaging-based measurements difficult [81]. Measurements are sent to the tissue bank and an offer for a size-matched allograft is returned to the physician (Fig. 9.2).
Surgical Technique
When first introduced, MAT was performed through an arthrotomy and involved splitting the collateral ligament. In 1994, Shelton first described the arthroscopic approach that eventually replaced the open approach and remains in use today [82]. Following the approach and introduction of the graft into the joint, the meniscus is fixated using one of several techniques. The method used to fixate the meniscal allograft is thought to be closely associated with the resultant biomechanical alterations and postoperative outcomes [29, 83].
Historically, stabilization of the graft was often achieved by suturing the donor meniscus to the recipient meniscal remnant without fixation of the anterior and posterior horns, or with stabilization of the horns with suture tied over a button or bone bridge [56, 84]. The soft tissue fixation technique , however, is no longer recommended as studies have demonstrated that securing both meniscal horns is required to achieve intra-articular contact pressures that most closely approximate the load-bearing function of an intact meniscus [85]. Without any form of bony fixation, the load transmission profile of the knee after MAT resembles the meniscus-deficient knee, and any biomechanical advantage provided by meniscus transplant is lost [29]. Cadaveric studies have also suggested that bone plug fixation provides greater strength than soft-tissue fixation [29, 86].
Bony fixation of the allograft, therefore, is thought to be an essential component of a successful MAT. There are currently two techniques that are used to achieve bony, anatomic fixation of the horns. In the bridge-in-slot technique, the meniscal horns remain attached to a single bone block. This allows the original anatomic orientation of the meniscal horns to be maintained during implantation, which is believed to optimize the ability of the meniscus to accommodate hoop stresses [15]. The bone plug technique involves bone tunnels drilled in the proximal tibia to accept bone plugs attached to the anterior and posterior meniscal horns. This technique is more technically demanding given the additional challenge of achieving proper tunnel placement. The bridge-in-slot technique is most commonly used for isolated lateral MATs. Although the bridge-in-slot can also be used for isolated medial MATs and has been shown to yield the same biomechanical results as the bone plug technique [13], the proximity of the ACL insertion often requires debridement of ACL fibers to achieve bridge-in-slot fixation. Therefore, bony fixation using bone plugs is often preferred for medial MATs.
As discussed previously, when meniscus insufficiency is accompanied by an associated ligament or focal chondral injury, both pathologies should be addressed appropriately. When meniscal transplantation is performed with a concomitant ACL reconstruction, the bone plug technique is preferred for both medial and lateral allografts in order to avoid interference between the bone bridge and the tibial ACL tunnel. For patients that require an alignment-correcting osteotomy, the operation is typically performed in a staged fashion. The surgeon should first correct the valgus or varus deformity and allow the patient to recover for 4 to 6 months before returning to the operating room for the MAT. Patients presenting with both meniscal deficiency and focal osteochondral defects should undergo concomitant MAT and cartilage restoration procedure. Autologous chondrocyte implantation and osteochondral allograft implantation can be performed simultaneously with the MAT and do not dictate which method of bony fixation is used.
Bridge-in-Slot Technique for Lateral MAT
Positioning
With the patient in the supine position on the table, the operative leg is placed in a circumferential leg holder and the foot of the table is dropped (Fig. 9.3). This allows the leg to be maneuvered during the procedure to provide unobstructed access to the posteromedial and posterolateral aspects of the knee for the allograft repair portion of the procedure. A folded blanket is placed under the proximal thigh of the contralateral leg to bring the hip into slight flexion and prevent any tension on the femoral nerve. A tourniquet is placed on the thigh of the operative leg, which is prepped and draped in a sterile fashion . Appropriate anatomic landmarks are then marked on the operative knee, including the site of the posterolateral incision.
Diagnostic Arthroscopy and Meniscus Debridement
Using anterolateral and anteromedial portal sites , a diagnostic arthroscopy is performed. For lateral meniscal transplantations, the anteromedial portal site should be 1 mm to 2 mm superior to the standard anteromedial portal site to facilitate access to the lateral compartment over the tibial spines. The meniscal deficiency is confirmed and the condition of the articular cartilage is assessed before proceeding.
If the diagnostic arthroscopy reveals the presence of meniscus remnant, an arthroscopic biter and standard 4.5 mm shaver are used to debride the native meniscus down to a 1 mm to 2 mm peripheral rim until punctate bleeding occurs (Fig. 9.4). In cases where there is no remnant meniscus, a rasp is used to abrade the capsule until a bleeding bed is created to encourage tissue healing.
Graft Preparation
As the arthroscopy and debridement are being performed, the allograft is prepared on the back table (Fig. 9.5). The attachment sites of the meniscus graft to the bone block are first identified. A cutting block, bridge-sizing guide, and sagittal saw are used to create a bone bridge that measures 7 mm in width by 10 mm in depth and connects the anterior and posterior meniscal horns. The lateral tibial spine is removed using a saw or rongeur. A #2 nonabsorbable suture is then passed through the meniscus at the point where the body of the allograft meets the posterior horn. This suture will be used to facilitate introduction of the meniscus into the knee. After being prepared, the allograft is placed in a basin with wet gauze until it is ready to be inserted.
Approach
The biceps femoris tendon is palpated and a posterolateral incision is made anterior to the tendon insertion to prevent injuring the common peroneal nerve (Fig. 9.6). The incision should be 3 inches in length with one-third of the incision above the joint line and two-thirds of the incision below the joint line. The interval between the posterior aspect of the iliotibial band and the biceps femoris tendon is identified with dissection. Through the identified interval, the lateral head of the gastrocnemius is palpated while plantarflexing and dorsiflexing the foot to confirm appropriate positioning. A space is created deep to the gastrocnemius to allow for an interval between the lateral head of the gastrocnemius and the posterolateral capsule. A spoon or Henning retractor is then inserted to protect the neighboring neurovascular structures during the repair portion of the procedure.
Slot Preparation
The bridge-in-slot technique aims to create a tibial slot based on the native meniscal attachment sites. Using a spinal needle to aid with localization, an anterolateral accessory portal is created in line with the anterior and posterior root insertions of the lateral meniscus (Fig. 9.7). A 4 mm bone-cutting shaver is inserted through the anterolateral accessory portal and used to create a superficial preliminary reference slot that connects the centers of the anterior and posterior horn attachment sites (Fig. 9.8). The reference slot should run parallel to the sagittal slope of the tibial plateau and reach a depth of 4 mm.
A hooked depth gauge is inserted through the anterolateral accessory portal and placed into the reference slot (Fig. 9.9). The hooked tip of the gauge should engage the posterior tibial cortex. A guide pin is inserted through the drill guide into the posterior tibial cortex, ensuring that the pin does not over-penetrate the cortex . Proper depth can be confirmed with direct palpation of the cortex through the posterolateral portal. Although not required, intraoperative fluoroscopy can also be used to confirm appropriate drill depth. The drill guide is removed and the pin is over-reamed with an 8 mm cannulated reamer. The drill bit and guide pin are then removed. Any remaining debris can be removed using an arthroscopic shaver or basket.
The final tibial slot is created using an 8 mm slot-cutting chisel (Fig. 9.10). The box chisel is gently impacted with a mallet along the course of the premade tunnel to the level of the posterior tibial cortex. The tines of the box chisel should be continuously visualized arthroscopically to ensure no damage to the surrounding tissue or opposing femoral articular cartilage (Fig. 9.11). The box chisel creates a rectangular slot measuring 8 mm in width and 10 mm in depth, matching the prepared bone bridge. To facilitate easy placement of the bone bridge, 7 and 8 mm rasps are used to enlarge the recipient slot until the 8 mm rasp sits flush with the tibial plateau (Fig. 9.12). The recipient slot is now complete.
Graft Introduction and Fixation
To prepare for introduction of the graft into the knee, the anterolateral accessory portal should first be extended into an arthrotomy large enough to permit passage of the graft. A zone-specific cannula is then placed into the medial portal. A meniscal repair needle is passed through the remnant of the native meniscus slightly anterior and lateral to the popliteus tendon. The needle is then retrieved through the posterolateral incision. The second needle is removed and the suture is retrieved through the enlarged anterolateral accessory portal site. This suture is tied into a loop and used to shuttle the graft passage sutures placed in the prepared meniscus allograft through the posterolateral incision. Gentle traction is maintained on the graft passage sutures while the allograft is passed through the arthrotomy and aligned with the recipient slot. Two army–navy retractors are used to maintain clear visualization of the recipient slot through the arthrotomy (Fig. 9.13). While applying varus stress to the knee, the bone bridge is reduced into the slot using gentle digital pressure and traction on the passage sutures. The knee can be cycled to aid with proper placement of the meniscus between the tibiofemoral articulation.
Once the allograft is in position, the meniscus is secured peripherally with 2–0 nonabsorbable sutures using multiple inside-out vertical mattress sutures (Fig. 9.14). Placing sutures on both the superior and inferior aspects of the meniscus allows the periphery of the graft to be closely approximated to the capsule in a balanced fashion . As the periphery is being secured, the sutures are retrieved through the posterolateral incision. An all-inside technique is then used to secure the graft directly posterior to the popliteus tendon and for fixation of the posterior horn.
After confirming that the periphery of the meniscus has been secured, the bone bridge is stabilized in the slot. A nitinol guide wire is first placed central to the bone bridge, and then a 7 × 23 mm bioabsorbable interference screw is used to achieve the final fixation of the bridge in the slot (Fig. 9.15).
The knee is placed in full extension and the meniscus repair sutures are tied. Maintaining visualization of the meniscus arthroscopically ensures that the sutures are placed directly on the capsule. Fixation of the most anterior aspect of the meniscus is performed with 2–0 sutures placed through the anterolateral arthrotomy. The graft is then probed to confirm adequate stabilization.
The posterolateral approach and anterolateral arthrotomy are irrigated and closed in layers. The portals are closed subcuticularly, skin adhesive is applied to the incisions, and sterile dressings are applied. The knee is then placed in hinged brace that is locked in extension.
Bone Plug Technique for Medial MAT
Graft Preparation
Patient positioning, diagnostic arthroscopy , and meniscal debridement are first performed using the methods described for the bridge-in-slot technique. As the arthroscopy and debridement are being performed, the allograft is prepared on the back table (Fig. 9.16). Any excess soft tissue is dissected away and the anterior and posterior horn insertion sites are isolated. A 2.4 mm guide pin is placed in the center of each horn attachment site. A collared reamer is placed over the guide pins and used to create the bone plugs, which are then sized to 8 mm in width by 10–12 mm in depth. Sutures are passed through each bone plug, first incorporating the horn attachment site, and then exiting through the central hole of the plug (Fig. 9.17). These sutures will be used to seat the donor plugs into the recipient tunnels. An additional suture is passed through junction of the meniscal body and the posterior horn to facilitate graft passage and reduction (Fig. 9.18). After being prepared, the allograft is placed in a basin with wet gauze to prevent drying.
Approach
The approach for a medial MAT utilizes a posteromedial incision similar to the approach for an inside-out meniscus repair. The MCL is palpated and the incision is made just posterior to the ligament, with one-third of the incision above the joint line and two-thirds of the incision below the joint line. The interval between the medial head of the gastrocnemius and the semimembranosus is identified. Palpating the gastrocnemius while plantarflexing and dorsiflexing the foot will confirm the appropriate positioning. Blunt dissection is then used to create an interval between the medial head of the gastrocnemius and the posteromedial capsule. A spoon or Henning retractor can be inserted into this space to protect the surrounding neurovascular structures during the remainder of the procedure.
Tunnel Preparation, Graft Introduction, and Fixation
The posterior tunnel is created first. An ACL tibial drill guide is used to pass a retrograde reamer into the location of the native meniscal posterior insertion site. An 8.5 mm diameter tunnel is reamed to a depth of 12–15 mm. A looped passing suture is then placed through the posterior tunnel and retrieved through the anteromedial portal (Fig. 9.19). This will be used to facilitate passing of the posterior bone plug.
The anteromedial portal is extended to create an arthrotomy large enough to pass the allograft. The graft passage sutures placed in the donor meniscus during preparation are passed through the arthrotomy and retrieved through the posteromedial incision (Fig. 9.20). The posterior bone plug sutures are placed through the posterior tunnel passing suture placed previously. After the posterior bone plug sutures are passed through the posterior tunnel, gentle traction on the sutures is used to reduce the bone plug into the tunnel. A Freer elevator or another blunt instrument can be used to guide the bone plug into place. The meniscus graft is then reduced under the medial femoral condyle. Arthroscopic visualization is used to confirm appropriate placement of the posterior bone plug and the meniscus allograft.
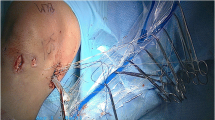
The allograft is introduced into the knee by feeding the passing sutures into the arthrotomy and through the posteromedial incision. Note: This image was obtained during a combined medial MAT and bone–patellar tendon–bone ACL reconstruction, explaining the large anterior incision. (Source: Jazrawi, Laith. 2014)
Following placement of the posterior bone plug, the meniscal repair portion of the procedure is performed. Zone-specific cannulas are used for an inside-out medial meniscus repair with sutures passed in the vertical mattress fashion. Sutures are placed on both the superior and inferior aspects of the allograft to ensure that the meniscus remains in an anatomic position.
The anterior bone tunnel is then created by first placing a guide pin at the site of the native anterior meniscus insertion site through the anteromedial arthrotomy. An 8.5 mm tunnel is reamed over the guide pin to a depth of 15 mm. Starting 2 cm distal to the joint line, a 2.5 mm drill bit is used to drill superiorly into the anterior tunnel. A Hewson suture passer is then used to shuttle the anterior bone plug sutures through the anterior tunnel. The anterior bone plug is then reduced into the tunnel.
With the periphery of the meniscus secured and the bone plugs seated in their tunnels, the bone plugs are fixed by tying their sutures over cortical buttons. The knee is placed in full extension and the meniscal repair sutures are tied through the posteromedial approach (Fig. 9.21). The incisions are closed as described for the bridge-in-slot technique and the knee is placed in a hinged brace locked in extension.
Postoperative Rehabilitation
To date, there is no well-established postoperative rehabilitation protocol that has been shown to provide superior outcomes compared to other protocols. Most studies that describe the postoperative rehabilitation involve bracing, restricted range of motion, and limited weight-bearing following surgery. A hinged brace should be used for 6–8 weeks following the procedure to protect against flexion of the knee past 90° and prevent excessive translation of the meniscus relative to the tibia. Tibial rotation should also be avoided for 8 weeks. Early joint exercises and progressive advancement of weight-bearing are typically recommended with the goal of achieving full range of motion within 2–3 months, use of a stationary bike at 2 months, light jogging at 3–4 months, and athletic activity at 6–9 months postoperatively [44, 50, 87, 88].
During the first 2 weeks following MAT, the patient is typically encouraged to proceed with toe-touch weightbearing with the knee locked in full extension. Carefully controlled stress placed on recently transplanted allografts is believed to stimulate collagen synthesis and enhance graft strength [89]. After 2 weeks, the patient can progress to weight-bearing as tolerated with the use of crutches [90,91,92]. However, weight-bearing with the knee flexed greater than 90° should be avoided until 8 weeks after surgery. Although one study found no difference in outcomes after MAT between a rehabilitation protocol involving restricted weight-bearing and range of motion and another protocol without any restrictions, further studies are needed to determine the optimal protocol that will allow patients to return to work or sport as quickly and safely as possible [93]. A recommended postoperative rehabilitation protocol is provided in Table 9.1.
Outcomes
As meniscal transplantation has become a more common solution for young patients with symptomatic meniscal deficiency, there have been a large number of studies that have shown MAT to be a safe and effective procedure with satisfactory outcomes. However, the conclusions that can be drawn from the existing outcomes studies are limited by heterogeneity in graft preservation technique, surgical technique, bony fixation method, and the rehabilitation protocol utilized. Additionally, surgical technique has evolved since meniscus transplants were first introduced, making it difficult to compare studies over time. Nevertheless, the overall positive outcomes demonstrated by the literature have helped solidify MAT as beneficial treatment for appropriately selected patients (Table 9.2).
The initial evidence that helped establish MAT as an effective treatment option was provided by a series of small cohort studies. In 2001, Rath et al. reported the outcomes of 22 cryopreserved meniscal allografts implanted in 18 patients [87]. At a mean follow-up of 4.5 years following surgery, there was an overall improvement in both pain and function. Repeat radiographs taken at the latest follow-up time demonstrated no significant difference in the joint space compared to preoperative radiographs. Eight of the 22 transplanted menisci tore during the study period requiring repeat meniscectomy. Histologic examination of the removed meniscal tissue revealed revascularization of the periphery, consistent with prior studies [39, 53, 94]. However, the torn allografts contained fewer fibrochondrocytes and lower levels of growth factors compared to torn native menisci. The authors postulated that reduced biologic activity of the allograft may be associated with the increased rate of tears [87].
Further studies demonstrated clinical improvements similar to those reported by Rath et al. [88, 95,96,97,98] In an evaluation of 40 cryopreserved allografts, the percentage of patients experiencing pain with daily activities decreased from 79% preoperatively to 11% at 3.3 years after MAT [88]. In another cohort, 77.5% of patients were mostly satisfied or completely satisfied with the outcomes of the procedure [95]. In addition to improved pain and function, analysis of 32 allografts found no significant difference in joint space loss between involved and uninvolved knees [98]. Kim et al. presented a group of 110 MAT cases with improved function in 94.5% of patients at a minimum of 2 years after surgery [97]. Despite the low level of evidence provided by these initial investigations, they served as an early description of the short- and intermediate-term efficacy of MAT.
Verdonk evaluated a cohort of 100 allografts preserved in culture, transplanted either in isolation or with concomitant high tibial osteotomy, with a mean follow-up time of 7.2 years [99]. Overall, MAT resulted in significant improvements in both pain and function. Failure, defined as moderate or severe occasional pain, persistent pain, or poor knee function, occurred in 28% of medial allografts at a mean of 6 years and 16% of lateral allografts at a mean of 4.8 years. For medial meniscal allografts, mean survival rate was 86.2% at 5 years, 74.2% at 10 years, and 52.8% at 14.5 years. For lateral allografts, mean survival rate was 90.2% at 5 years, 69.8% at 10 years, and 69.8% at 14 years. There was no difference in survival between medial and lateral grafts. The level of cartilage degeneration at the time of surgery did not affect the risk of failure, in contrast to previous studies which have suggested that failure rate is higher with advanced degeneration [36, 40]. The difference can perhaps be due to the study’s utilization of nonirradiated, fresh allografts, which may be more resistant to failure in patients with moderate or severe preexisting cartilage damage compared to the irradiated, cryopreserved allografts used in contradicting studies.
An additional study of graft survival was carried out by McCormick et al. [100] This cohort consisted of 172 patients who received fresh-frozen, nonirradiated allografts using the bridge-in-slot technique or, if concomitant ACL reconstruction was performed, a modified bridge technique. At a mean follow-up of 4.9 years, 4.7% of patients had experienced graft failure requiring revision MAT or TKA. Despite a greater than 95% graft survival rate, 32% of the cohort required re-operation during the study period. The most common reason for re-operation was arthroscopic debridement of scar tissue, with an average time to reoperation of 21 months. Patients requiring reoperation had graft survival rate of 88%, although they were at an increased risk of failure compared to patients who did not require reoperation [100]. This investigation suggests that although roughly one in three MAT patients will undergo reoperation, there is still a high likelihood of graft survival.
Verdonk also reported on a cohort of patients consisting of 39 culture-maintained allografts in 38 patients with a mean follow-up time of 12.1 years [101]. Like this group’s earlier results, pain and function improved significantly for both medial and lateral allografts. Despite the noted improvements, patients continued to experience functional impairment and symptoms at the time of follow-up. Eighteen percent of the study group had undergone total knee arthroplasty after a mean of 6.5 years due to progression of pain and functional limitation. There was no additional change in joint space narrowing in 41% of the patients at the time of follow-up, suggesting that MAT may attenuate progression of cartilage degradation and provide a chondroprotective effect. Similar to other existing studies [102, 103], MRI outcomes (including femoral and tibial cartilage degeneration, meniscus signal intensity, meniscus position, extrusion, and tears) did not correlate with subjective clinical outcomes. The authors conclude that the evaluation of patient outcomes should rely primarily on clinical measures rather than radiographic measures [101]. This is consistent with a later study which found that although significant meniscus shrinkage occurred by 1 year postoperatively, the morphologic changes were not associated with clinical outcomes [104].
Saltzman performed a longitudinal study of patient satisfaction following MAT with the most recent update consisting of 22 allografts at a mean follow-up time of 8.5 years [105]. There were significant improvements in pain, functional outcomes, and quality of life with no difference between medial allografts and lateral allografts. At the time of follow-up, the patients reported an average satisfaction score of 8.8 out of 10. Eight of the 22 patients were completely satisfied with the results of the procedure, and the remaining 14 patients reported being mostly satisfied. This same cohort of patients was evaluated at 2 and 4 years postoperatively, and it was found that that pain, severity of symptoms, and function were generally consistent from the earlier follow-up times to the most recent evaluation [105]. This suggests that the benefits achieved shortly after rehabilitation are maintained for at least 8 years following MAT.
A 2011 meta-analysis examined 44 trials consisting of 1136 total grafts in 1068 patients with a mean age of 34.8 years [106]. Although the included studies differed in their outcome measures, they consistently demonstrated an improvement in clinical outcomes with MAT. Of the studies that specified, only 36% of MATs were isolated, while the remainder were performed with another procedure. Among all included studies, 84% of patients described their knee function as normal or nearly normal, and 89% were satisfied with their results. The overall complication rate was 21.3%, with the most common adverse events being tearing of the graft and adhesions requiring MUA. There was a failure rate of 10.6% when defined as destruction or removal of the graft with or without conversion to arthroplasty. Of the studies that included radiographic or MRI follow-up, most noted little to no progression of joint space narrowing at last follow-up. The chondroprotective effect of MAT has been demonstrated in animal models [107], and while this analysis provides additional support for a similar effect in humans, definitive evidence is still lacking. Despite the unknown efficacy in terms of cartilage preservation, the consistent clinical improvement and low rate of serious complications found in this analysis suggest that MAT is a safe and effective procedure in carefully selected patients.
A similarly large 2018 meta-analysis included 38 studies consisting of 1637 MATs with a mean age of 34 years [108]. There was overall tear rate of 9% and a failure rate of 12.6%, when defined as requiring revision, removal of the graft, or persistent knee pain. Interestingly, there was no difference in graft tears, failure rates, functional improvement, or pain improvement between bony fixation and soft tissue fixation. This contrasts the biomechanical studies which have largely concluded that bony fixation is superior to soft tissue fixation [29, 86]. In another study comparing suture-only MAT and bone plug MAT, there was similarly no difference in functional outcomes, although the suture-only technique was associated with higher risk of extruded meniscal body at 40 months postoperatively [83]. While the measured functional outcomes may be similar between the two different methods of securing the meniscus, soft-tissue fixation has largely fallen out of favor among surgeons.
Bin et al. performed a meta-analysis comparing the mid-term and long-term outcomes of medial MAT versus lateral MAT [109]. The analysis included nine studies consisting of 287 medial MATs and 407 lateral MATs. At 5 to 10 years postoperatively, the graft survival rate was 85.8% for medial allografts and 89.2% for lateral allografts. Greater than 10 years following transplantation, the graft survival rate was 52.6% for medial allografts and 56.6% for lateral allografts. At both mid-term follow-up and long-term follow-up, there was no significant difference in graft survival rate between medial and lateral MATs. However, lateral MAT was found to be associated with greater improvement in pain and function. The authors suggested that lateral MAT may be more successful because patients with lateral meniscus injuries tend to have shorter intervals between meniscectomy and transplantation, perhaps leading to less cartilage damage accumulation [99]. Further studies are needed to explain this difference.
Early studies initially suggested that meniscal extrusion was associated with poorer outcomes [110]. However, subsequent studies found that graft extrusion did not affect the progression of joint space narrowing at 5 years [64]. Additionally, although lateral menisci tend to extrude to a greater extent than medial menisci, neither was associated with clinical outcomes [64, 111].
A 2019 systematic review and meta-analysis examined the rate of return to physical activity following MAT [112]. Based on the nine included studies, 77% of patients were able to return to any level of sport or physical activity at minimum 2-year follow-up, with 67% returning to the same level of preinjury activity. One of the included studies specifically analyzed 13 high-level athletes (nine collegiate athletes, three high school varsity athletes, and one professional athlete) who had undergone prior partial or total meniscectomies and had been undeniable to return to their preinjury level of play [113]. In this study, 10 athletes (77%) returned to their previous level of play after a mean of 16.5 months and nine (70%) returned to their desired level of play after MAT. The existing data regarding return to sport after MAT is generally low-level, making it difficult to draw conclusions, especially related to high-impact sports and activities.
Conclusion
Within the relatively short history of meniscal allograft transplantation, the techniques used to preserve and implant the grafts have advanced dramatically. While the procedure in its current state is not capable of entirely eliminating the sequelae associated with the meniscectomized knee, MAT does represent an opportunity to restore the mechanics of the knee joint, improve function, and alleviate pain. As the body of data surrounding meniscal transplantation grows, the surgical techniques will continue to be refined and the lifespan of the allografts will likely improve, offering even greater benefits for patients with symptoms related to meniscus insufficiency.
References
Smillie IS. The current pattern of internal derangements of the knee joint relative to the menisci. Clin Orthop Relat Res. 1967;51:117–22.
Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg. 1948;30b(4):664–70.
Tapper EM, Hoover NW. Late results after meniscectomy. J Bone Joint Surg Am. 1969;51(3):517–526 passim.
Johnson RJ, Kettelkamp DB, Clark W, Leaverton P. Factors effecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56(4):719–29.
Pengas IP, Assiotis A, Nash W, Hatcher J, Banks J, McNicholas MJ. Total meniscectomy in adolescents: a 40-year follow-up. J Bone Joint Surg. 2012;94(12):1649–54.
Bolano LE, Grana WA. Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at five years. Am J Sports Med. 1993;21(3):432–7.
Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13(6):673–9.
Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38(9):1907–16.
Williams RJ 3rd, Warner KK, Petrigliano FA, Potter HG, Hatch J, Cordasco FA. MRI evaluation of isolated arthroscopic partial meniscectomy patients at a minimum five-year follow-up. HSS J. 2007;3(1):35–43.
Lee SJ, Aadalen KJ, Malaviya P, et al. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34(8):1334–44.
Bai B, Shun H, Yin ZX, Liao ZW, Chen N. Changes of contact pressure and area in patellofemoral joint after different meniscectomies. Int Orthop. 2012;36(5):987–91.
McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg. 2006;88(12):1549–56.
Verma NN, Kolb E, Cole BJ, et al. The effects of medial meniscal transplantation techniques on intra-articular contact pressures. J Knee Surg. 2008;21(1):20–6.
Van Thiel GS, Frank RM, Gupta A, et al. Biomechanical evaluation of a high tibial osteotomy with a meniscal transplant. J Knee Surg. 2011;24(1):45–53.
Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14(4):270–5.
Bullough P, Goodfellow J. The significance of the fine structure of articular cartilage. J Bone Joint Surg. 1968;50(4):852–7.
Korkala O, Karaharju E, Gronblad M, Aalto K. Articular cartilage after meniscectomy. Rabbit knees studied with the scanning electron microscope. Acta Orthop Scand. 1984;55(3):273–7.
Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–8.
Mac CM. The movements of bones and joints; the synovial fluid and its assistants. J Bone Joint Surg. 1950;32-b(2):244–52.
Aagaard H, Verdonk R. Function of the normal meniscus and consequences of meniscal resection. Scand J Med Sci Sports. 1999;9(3):134–40.
Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50(9):2811–9.
Milachowski KA, Weismeier K, Wirth CJ. Homologous meniscus transplantation. Experimental and clinical results. Int Orthop. 1989;13(1):1–11.
Rijk PC. Meniscal allograft transplantation--part I: background, results, graft selection and preservation, and surgical considerations. Arthroscopy. 2004;20(7):728–43.
Locht RC, Gross AE, Langer F. Late osteochondral allograft resurfacing for tibial plateau fractures. J Bone Joint Surg Am. 1984;66(3):328–35.
Cummins JF, Mansour JN, Howe Z, Allan DG. Meniscal transplantation and degenerative articular change: an experimental study in the rabbit. Arthroscopy. 1997;13(4):485–91.
Aagaard H, Jorgensen U, Bojsen-Moller F. Reduced degenerative articular cartilage changes after meniscal allograft transplantation in sheep. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):184–91.
Andrish JT, Kambic HE, Valdevit ADC, et al. Selected knee osteotomies and meniscal replacement: effects on dynamic intra-joint loading. J Bone Joint Surg Am. 2001;83-A Suppl 2 Pt 2:142–50.
Alhalki MM, Hull ML, Howell SM. Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft. A human cadaveric study. Am J Sports Med. 2000;28(3):370–6.
Paletta GA Jr, Manning T, Snell E, Parker R, Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med. 1997;25(5):692–8.
Sekiya JK, Ellingson CI. Meniscal allograft transplantation. J Am Acad Orthop Surg. 2006;14(3):164–74.
Trentacosta N, Graham WC, Gersoff WK. Meniscal allograft transplantation: state of the art. Sports Med Arthrosc Rev. 2016;24(2):e23–33.
Kempshall PJ, Parkinson B, Thomas M, et al. Outcome of meniscal allograft transplantation related to articular cartilage status: advanced chondral damage should not be a contraindication. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):280–9.
Stone KR, Pelsis JR, Surrette ST, Walgenbach AW, Turek TJ. Meniscus transplantation in an active population with moderate to severe cartilage damage. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):251–7.
Lee AS, Kang RW, Kroin E, Verma NN, Cole BJ. Allograft meniscus transplantation. Sports Med Arthrosc Rev. 2012;20(2):106–14.
Jarit GJ, Bosco JA 3rd. Meniscal repair and reconstruction. Bull NYU Hosp Jt Dis. 2010;68(2):84–90.
de Boer HH, Koudstaal J. Failed meniscus transplantation. A report of three cases. Clin Orthop Relat Res. 1994;306:155–62.
Mascarenhas R, Yanke AB, Frank RM, Butty DC, Cole BJ. Meniscal allograft transplantation: preoperative assessment, surgical considerations, and clinical outcomes. J Knee Surg. 2014;27(6):443–58.
Harris JD, Cavo M, Brophy R, Siston R, Flanigan D. Biological knee reconstruction: a systematic review of combined meniscal allograft transplantation and cartilage repair or restoration. Arthroscopy. 2011;27(3):409–18.
van Arkel ER, de Boer HH. Human meniscal transplantation. Preliminary results at 2 to 5-year follow-up. J Bone Joint Surg. 1995;77(4):589–95.
Cameron JC, Saha S. Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop Relat Res. 1997;337:164–71.
Getgood A, Gelber J, Gortz S, De Young A, Bugbee W. Combined osteochondral allograft and meniscal allograft transplantation: a survivorship analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):946–53.
Lee BS, Kim HJ, Lee CR, et al. Clinical outcomes of meniscal allograft transplantation with or without other procedures: a systematic review and meta-analysis. Am J Sports Med. 2018;46(12):3047–56.
Sekiya JK, Giffin JR, Irrgang JJ, Fu FH, Harner CD. Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(6):896–906.
Ryu RK, Dunbar VW, Morse GG. Meniscal allograft replacement: a 1-year to 6-year experience. Arthroscopy. 2002;18(9):989–94.
Abrams GD, Hussey KE, Harris JD, Cole BJ. Clinical results of combined meniscus and femoral osteochondral allograft transplantation: minimum 2-year follow-up. Arthroscopy. 2014;30(8):964–970.e961.
Farr J, Rawal A, Marberry KM. Concomitant meniscal allograft transplantation and autologous chondrocyte implantation: minimum 2-year follow-up. Am J Sports Med. 2007;35(9):1459–66.
Kazi HA, Abdel-Rahman W, Brady PA, Cameron JC. Meniscal allograft with or without osteotomy: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):303–9.
Bonasia DE, Amendola A. Combined medial meniscal transplantation and high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):870–3.
Amendola A. Knee osteotomy and meniscal transplantation: indications, technical considerations, and results. Sports Med Arthrosc Rev. 2007;15(1):32–8.
Graf KW Jr, Sekiya JK, Wojtys EM. Long-term results after combined medial meniscal allograft transplantation and anterior cruciate ligament reconstruction: minimum 8.5-year follow-up study. Arthroscopy. 2004;20(2):129–40.
Rue JP, Yanke AB, Busam ML, McNickle AG, Cole BJ. Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair: minimum 2-year follow-up. Am J Sports Med. 2008;36(9):1770–8.
Gomoll AH, Kang RW, Chen AL, Cole BJ. Triad of cartilage restoration for unicompartmental arthritis treatment in young patients: meniscus allograft transplantation, cartilage repair and osteotomy. J Knee Surg. 2009;22(2):137–41.
Garrett JC, Steensen RN. Meniscal transplantation in the human knee: a preliminary report. Arthroscopy. 1991;7(1):57–62.
Milachowski KA, Kohn D, Wirth CJ. [Transplantation of allogeneic menisci]. Der Orthopade. 1994;23(2):160–3.
Weismeier K, Wirth CJ, Milachowski KA. [Transplantation of the meniscus. Experimental study]. Revue de chirurgie orthopedique et reparatrice de l’appareil moteur. 1988;74(2):155–9.
Siegel MG, Roberts CS. Meniscal allografts. Clin Sports Med. 1993;12(1):59–80.
Arnoczky SP, McDevitt CA, Schmidt MB, Mow VC, Warren RF. The effect of cryopreservation on canine menisci: a biochemical, morphologic, and biomechanical evaluation. J Orthop Res. 1988;6(1):1–12.
Gelber PE, Gonzalez G, Torres R, Garcia Giralt N, Caceres E, Monllau JC. Cryopreservation does not alter the ultrastructure of the meniscus. Knee Surg Sports Traumatol Arthrosc. 2009;17(6):639–44.
Villalba R, Pena J, Navarro P, et al. Cryopreservation increases apoptosis in human menisci. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):298–303.
Lubowitz JH, Verdonk PC, Reid JB 3rd, Verdonk R. Meniscus allograft transplantation: a current concepts review. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):476–92.
Rodeo SA. Meniscal allografts–where do we stand? Am J Sports Med. 2001;29(2):246–61.
Jackson DW, Whelan J, Simon TM. Cell survival after transplantation of fresh meniscal allografts. DNA probe analysis in a goat model. Am J Sports Med. 1993;21(4):540–50.
Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D. Long-term results of meniscal allograft transplantation. Am J Sports Med. 2002;30(2):174–81.
Lee DH, Kim SB, Kim TH, Cha EJ, Bin SI. Midterm outcomes after meniscal allograft transplantation: comparison of cases with extrusion versus without extrusion. Am J Sports Med. 2010;38(2):247–54.
Noyes F. Irradiated meniscus allografts in the human knee: a two to five years follow-up study. Revue de chirurgie orthopedique et reparatrice de l’appareil moteur. 1995;81(2):207–8.
Yahia L, Zukor D. Irradiated meniscal allotransplants of rabbits: study of the mechanical properties at six months postoperation. Acta Orthop Belg. 1994;60(2):210–5.
von Lewinski G, Milachowski KA, Weismeier K, Kohn D, Wirth CJ. Twenty-year results of combined meniscal allograft transplantation, anterior cruciate ligament reconstruction and advancement of the medial collateral ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1072–82.
Goble EM, Kohn D, Verdonk R, Kane SM. Meniscal substitutes--human experience. Scand J Med Sci Sports. 1999;9(3):146–57.
Dienst M, Greis PE, Ellis BJ, Bachus KN, Burks RT. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med. 2007;35(1):34–42.
Pollard ME, Kang Q, Berg EE. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11(6):684–7.
Wilmes P, Pape D, Kohn D, Seil R. The reproducibility of radiographic measurement of lateral meniscus horn position. Arthroscopy. 2007;23(10):1079–86.
Wilmes P, Anagnostakos K, Weth C, Kohn D, Seil R. The reproducibility of radiographic measurement of medial meniscus horn position. Arthroscopy. 2008;24(6):660–8.
Haut TL, Hull ML, Howell SM. Use of roentgenography and magnetic resonance imaging to predict meniscal geometry determined with a three-dimensional coordinate digitizing system. J Orthop Res. 2000;18(2):228–37.
Prodromos CC, Joyce BT, Keller BL, Murphy BJ, Shi K. Magnetic resonance imaging measurement of the contralateral normal meniscus is a more accurate method of determining meniscal allograft size than radiographic measurement of the recipient tibial plateau. Arthroscopy. 2007;23(11):1174–1179.e1171.
Huang A, Hull ML, Howell SM, Haut DT. Identification of cross-sectional parameters of lateral meniscal allografts that predict tibial contact pressure in human cadaveric knees. J Biomech Eng. 2002;124(5):481–9.
Shaffer B, Kennedy S, Klimkiewicz J, Yao L. Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med. 2000;28(4):524–33.
Kaleka CC, Netto AS, Silva JC, et al. Which are the most reliable methods of predicting the meniscal size for transplantation? Am J Sports Med. 2016;44(11):2876–83.
Yoon JR, Kim TS, Lim HC, Lim HT, Yang JH. Is radiographic measurement of bony landmarks reliable for lateral meniscal sizing? Am J Sports Med. 2011;39(3):582–9.
Yoon JR, Kim TS, Wang JH, Yun HH, Lim H, Yang JH. Importance of independent measurement of width and length of lateral meniscus during preoperative sizing for meniscal allograft transplantation. Am J Sports Med. 2011;39(7):1541–7.
Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy. 1995;11(4):386–94.
Van Thiel GS, Verma N, Yanke A, Basu S, Farr J, Cole B. Meniscal allograft size can be predicted by height, weight, and gender. Arthroscopy. 2009;25(7):722–7.
Shelton WR, Dukes AD. Meniscus replacement with bone anchors: a surgical technique. Arthroscopy. 1994;10(3):324–7.
Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40(7):1591–6.
Stone KR, Rosenberg T. Surgical technique of meniscal replacement. Arthroscopy. 1993;9(2):234–7.
Chen MI, Branch TP, Hutton WC. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12(2):174–81.
Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med. 1999;27(3):320–8.
Rath E, Richmond JC, Yassir W, Albright JD, Gundogan F. Meniscal allograft transplantation. Two- to eight-year results. Am J Sports Med. 2001;29(4):410–4.
Noyes FR, Barber-Westin SD, Rankin M. Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am. 2004;86-a(7):1392–404.
Krippaehne WW, Hunt TK, Jackson DS, Dunphy JE. Studies on the effect of stress on transplants of autologous and homologous connective tissue. Am J Surg. 1962;104:267–72.
Hannon MG, Ryan MK, Strauss EJ. Meniscal allograft transplantation a comprehensive historical and current review. Bull Hosp Jt Dis (2013). 2015;73(2):100–8.
Fritz JM, Irrgang JJ, Harner CD. Rehabilitation following allograft meniscal transplantation: a review of the literature and case study. J Orthop Sports Phys Ther. 1996;24(2):98–106.
Kohn D, Aagaard H, Verdonk R, Dienst M, Seil R. Postoperative follow-up and rehabilitation after meniscus replacement. Scand J Med Sci Sports. 1999;9(3):177–80.
Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy. 1994;10(2):206–10.
Arnoczky SP, Warren RF, McDevitt CA. Meniscal replacement using a cryopreserved allograft. An experimental study in the dog. Clin Orthop Relat Res. 1990;252:121–8.
Cole BJ, Dennis MG, Lee SJ, et al. Prospective evaluation of allograft meniscus transplantation: a minimum 2-year follow-up. Am J Sports Med. 2006;34(6):919–27.
Vundelinckx B, Bellemans J, Vanlauwe J. Arthroscopically assisted meniscal allograft transplantation in the knee: a medium-term subjective, clinical, and radiographical outcome evaluation. Am J Sports Med. 2010;38(11):2240–7.
Kim JM, Lee BS, Kim KH, Kim KA, Bin SI. Results of meniscus allograft transplantation using bone fixation: 110 cases with objective evaluation. Am J Sports Med. 2012;40(5):1027–34.
Sekiya JK, West RV, Groff YJ, Irrgang JJ, Fu FH, Harner CD. Clinical outcomes following isolated lateral meniscal allograft transplantation. Arthroscopy. 2006;22(7):771–80.
Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R. Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87(4):715–24.
McCormick F, Harris JD, Abrams GD, et al. Survival and reoperation rates after meniscal allograft transplantation: analysis of failures for 172 consecutive transplants at a minimum 2-year follow-up. Am J Sports Med. 2014;42(4):892–7.
Verdonk PC, Verstraete KL, Almqvist KF, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):694–706.
Verstraete KL, Verdonk R, Lootens T, Verstraete P, De Rooy J, Kunnen M. Current status and imaging of allograft meniscal transplantation. Eur J Radiol. 1997;26(1):16–22.
van Arkel ER, Goei R, de Ploeg I, de Boer HH. Meniscal allografts: evaluation with magnetic resonance imaging and correlation with arthroscopy. Arthroscopy. 2000;16(5):517–21.
Lee BS, Chung JW, Kim JM, Cho WJ, Kim KA, Bin SI. Morphologic changes in fresh-frozen meniscus allografts over 1 year: a prospective magnetic resonance imaging study on the width and thickness of transplants. Am J Sports Med. 2012;40(6):1384–91.
Saltzman BM, Bajaj S, Salata M, et al. Prospective long-term evaluation of meniscal allograft transplantation procedure: a minimum of 7-year follow-up. J Knee Surg. 2012;25(2):165–75.
Elattar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P. Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):147–57.
Kelly BT, Potter HG, Deng XH, et al. Meniscal allograft transplantation in the sheep knee: evaluation of chondroprotective effects. Am J Sports Med. 2006;34(9):1464–77.
Jauregui JJ, Wu ZD, Meredith S, Griffith C, Packer JD, Henn RF 3rd. How should we secure our transplanted meniscus? A meta-analysis. Am J Sports Med. 2018;46(9):2285–90.
Bin SI, Nha KW, Cheong JY, Shin YS. Midterm and long-term results of medial versus lateral meniscal allograft transplantation: a meta-analysis. Am J Sports Med. 2018;46(5):1243–50.
Potter HG, Rodeo SA, Wickiewicz TL, Warren RF. MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology. 1996;198(2):509–14.
Koh YG, Moon HK, Kim YC, Park YS, Jo SB, Kwon SK. Comparison of medial and lateral meniscal transplantation with regard to extrusion of the allograft, and its correlation with clinical outcome. J Bone Joint Surg. 2012;94(2):190–3.
Grassi A, Bailey JR, Filardo G, Samuelsson K, Zaffagnini S, Amendola A. Return to sport activity after meniscal allograft transplantation: at what level and at what cost? A systematic review and meta-analysis. Sports Health. 2019;1941738118819723
Chalmers PN, Karas V, Sherman SL, Cole BJ. Return to high-level sport after meniscal allograft transplantation. Arthroscopy. 2013;29(3):539–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kingery, M.T., Strauss, E.J. (2020). Meniscal Allograft Transplantation: Indications, Techniques, and Outcomes. In: Strauss, E.J., Jazrawi, L.M. (eds) The Management of Meniscal Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-49488-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-49488-9_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-49487-2
Online ISBN: 978-3-030-49488-9
eBook Packages: MedicineMedicine (R0)