Abstract
Meniscus allotransplantation represents the biological solution for the symptomatic, meniscus-deficient patient who has not developed advanced osteoarthritis. A growing body of evidence suggests that pain relief and functional improvement may reliably be achieved at short- and medium-term follow-up, and even, in some cases, at long-term (>10 years) follow-up. Future research must address the issue of optimal timing of the procedure and whether meniscal transplantation results in demonstrable long-term benefits, especially with regard to protection of articular cartilage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscus allograft transplantation (allotransplantation) represents a potential biological solution for the symptomatic meniscus-deficient patient who has not developed advanced osteoarthritis. A growing body of evidence suggests that pain relief and functional improvement may reliably be achieved at short- and medium-term follow-up when applying appropriate indications and techniques. Refining best indications, howevening best indications, however, is complicated by a dilemma regarding optimal timing of the procedure in order to maximize the chance of a successful outcome. In addition, the long-term effects of meniscal allograft transplantation, especially with regard to protection of articular cartilage and prevention of arthrosis, remain to be proven.
In this current concepts review, we consider the significance of the meniscus macroscopically, microscopically, and biomechanically. After evaluation of meniscal allograft processing, preservation, and biology, we review current indications and contraindications for meniscal replacement including patient selection. Surgical considerations such as graft selection and sizing, implantation techniques, complications, and rehabilitation are discussed. In vitro and clinical outcomes, including potential long-term effects on articular cartilage, alternative treatments, and future directions are finally considered.
Understanding the meniscus
In 1948, Fairbank [1] described three specific radiological changes in the meniscectomized knee. These alterations, now classically known as “Fairbank’s changes”, include: (1) formation of a ridge on the femoral condyle, (2) flattening of the femoral condyle, and (3) joint space narrowing.
Fairbank’s report resulted in an era of increasing appreciation of the role of menisci. Over the last few decades, the understanding of meniscal functions and, consequently, the management of meniscal injuries has continued to evolve, with increasing commitment among orthopedists to preserve the meniscus whenever possible. The natural history of a meniscus-deficient knee has been persuasively shown to involve poor outcomes over time, including disruption of load-sharing and shock absorption, diminution of joint stability and nutrition, and deterioration of articular cartilage with progression to arthrosis [2].
When meniscal repair is not possible, the issue of meniscal replacement arises. In the early 1980s, Locht et al. [3] reported encouraging results following the transplantation of meniscal allografts in combination with proximal osteochondral allografts in the treatment of tibial plateau fractures. Milachowski et al. [4] reported in 1984, the first attempt at meniscal allograft transplantation in humans.
Anatomy and function of the menisci
The menisci perform many functions in the normal and injured knee. Both the medial and lateral menisci bear weight, help stabilize the tibiofemoral joint (with the medial meniscus particularly acting to restrain anterior translation of the tibia in the ACL-deficient knee [5]), transmit load, improve joint congruency, enhance rotation of the opposing articular surfaces, and augment lubrication and nutrition of the articular cartilage [6–10].
The lateral meniscus is the more mobile of the two. The lateral meniscal posterior attachments are supplemented, posteriorly, by the (variable) meniscofemoral ligaments of Humphrey and Wrisberg. Centrally, the popliteus hiatus represents a gap in the lateral meniscal peripheral attachment. About the hiatus, attachment is supplemented anteroinferiorly and posterosuperiorly by popliteomeniscal fasciculi [11, 12]. Lateral meniscus transplantation may not restore the meniscofemoral ligaments or the popliteomeniscal fasciculi; the biomechanical consequences of this eventuality, is unknown [2]. In contrast to the more mobile, lateral meniscus, the medial meniscus is attached firmly both to the coronary (meniscotibial) ligaments and the deep medial collateral ligament, and, in addition, is circumferentially attached to the capsule [13].
Load bearing and transmission
When the knee is in extension, the menisci transmit approximately 50% of the joint reactive force; in flexion, this force increases up to 90% [10]. The lateral meniscus bears 70% of the load transmitted across the lateral compartment, while the transmission of load across the medial compartment is evenly distributed between the medial meniscus and the articular cartilage [2]. The greater contribution of the lateral meniscus to load sharing may explain why lateral (as compared to medial) meniscectomy results in earlier and more rapid degeneration of the articular surfaces [10].
Vascularity and perfusion
The menisci are centrally avascular, relying on diffusion from synovial fluid for their nutrition. Peripherally, the menisci are nourished by a perimeniscal capillary plexus originating in the knee’s capsular and synovial tissues from the superior and inferior medial and lateral geniculate arteries. These vessels are oriented circumferentially, with radial branches directed towards the central regions. These radial branches penetrate between 10 and 30% of the width of each meniscus [14, 15]. Integral to the healing response after meniscus transplantation is a peripheral, vascular synovial fringe that may extend up to 3 mm over the tibial and femoral meniscal surfaces [2].
Material properties
During loading of the normal knee joint, high compressive forces are resisted by intrameniscal distension pressures exerted as water within the meniscal tissue flows through the solid but porous and permeable matrix proteins [2, 16, 17]. Compressive loading of the joint also results in radial displacement of the menisci by the femoral condylar surfaces, which is enhanced by the concave, wedge shape of each menisci. Together with its ligamentous attachments, the menisci convert joint axial load into tensile strain and shearing forces, which are well transmitted and tolerated by virtue of its meniscal cellular and histological architecture [18].
Histology
Menisci possess collagen fibers oriented circumferentially. These circumferential fibers are bound by radially oriented fibers. In sum, this architecture is designed to convert joint load to hoop or shear stress, which the meniscus is designed to tolerate well. In addition, the resistance to hoop stress may inhibit extrusion of the menisci from their position between the tibial and femoral surfaces [18]. A prerequisite for this protective feature is secure anchoring of the anterior and posterior horns of the menisci, and many believe that these attachments must be replicated in meniscal transplantation in order to sustain this function. Data from one MRI study has indicated that graft extrusion is more likely in knees with advanced arthrosis; this is likely associated with increased risk for graft failure [19].
Anterior and posterior horn-insertions contain type I and II neuroreceptors with possible propioceptive and mechanoreceptive capacities [20, 21]. Larger concentrations of these nerve cells exist in the horn insertions and the outer third of the menisci than in the central regions. One hypothesis for this distribution is that at extremes of flexion and extension, there is a greater need for afferent information in order to generate protective or postural muscular reflex arcs [22]. Functional reinnervation following meniscal transplantation has not been determined.
Graft processing
There are four types of meniscal allograft processing with which the clinician should be familiar: cryopreserved, deep-frozen (fresh-frozen), fresh, and lyophilized (freeze-dried.) The most commonly implanted menisci are either deep-frozen (fresh-frozen) or cryopreserved [2], though currently there is a lack of evidence to justify the increase in logistical difficulties and expense that arise with the use of cryopreserved (or fresh) tissue [2]. The various means of graft processing are distinct; each presenting pros and cons. The first variable is whether or not viable donor cells are preserved in the transplanted tissue. This occurs only in fresh grafts and to a lesser extent, in cryopreserved grafts. One animal study has indicated that the donor cells in a fresh graft are completely replaced by host cells within a matter of weeks, raising the question of the significance of donor cell viability [23]. Other data, however, suggest that donor cells in fact do persist in the allograft, over time [24, 25]. Some research results support the concept that viable meniscus cells in the graft may enhance the maintenance of the extracellular matrix and, thus, the allograft’s mechanical integrity following transplantation [26, 27].
A second significant variable is whether the allograft can be secondarily sterilized to reduce risk of disease transmission. Sterilization generally kills viable cells and is not performed on fresh or cryopreserved grafts. The third factor is whether the processing method affects a graft’s immunogenicity. Deep freezing may denature histocompatibility antigens [28], though not all data support this understanding [29]. While deep freezing may make a graft less immunogenic, its clinical significance is uncertain. A fourth variable regarding how material properties of a graft may be altered by processing, must also be considered. Though the material properties of deep frozen grafts are, purportedly, not significantly altered by the freezing process, some animal data indicate reduced tensile strength as a result of freezing over time [30]. Lyophilized grafts may also be prone to reduced tensile strength, graft shrinkage [4], poor rehydration [27], post-transplantation joint effusion [4, 31], and synovitis [32], and are therefore no longer used in the clinical setting.
Allograft biology, success, and failure
Most of the available information regarding graft biology has been generated from animal studies. It is worth remembering, however, that animal studies cannot be directly compared with clinical trials for the following reasons: small animals, in general, manifest a more robust healing response than humans. In addition, most animal transplantations are performed immediately after graft harvest; in humans, post-harvest transplantation is typically delayed. Finally, differing kinematics of the quadruped knee joint render direct comparisons with the biped knee problematic [33].
With these caveats in mind, what has been suggested by research thus far is as follows: allografts become repopulated with cells that appear to be derived from the host synovial membrane [34], and the graft incorporates from the periphery towards the center [33]. Long-term ability of these graft-repopulating cells to generate and maintain the extracellular matrix is unclear [2]. In one study, reduced glycosaminoglycan content was revealed in an animal recipient of the allograft [35]. New capillaries from the capsular and synovial attachments have been shown to revascularize the graft gradually and incompletely [35]. Deep-frozen grafts have been shown to repopulate least completely, with the central region of the graft tending to remain hypocellular or acellular [20].
Graft revascularization and cellular repopulation are intrinsically associated with remodeling of the matrix structure, but perhaps in a disordered fashion [19]. Effects on the material properties of the graft are unclear, though it is suspected that this remodeling may lead to tears and failure of the graft. On the other hand, it is clear that the phenotype of the allograft-repopulating cell ultimately determines the biomechanical behavior of the graft. In one human study, which examined biopsy specimens from both intact and failed deep-frozen meniscal transplants, repopulating cells consisted of several phenotypes: fibroblasts, fibrochondrocytes, and mononuclear/synovial cells [34]. This study also indicated that in the majority of cases only partial repopulation of the allograft was observed. Another clinical study of failed meniscal transplant biopsies indicated that fibroblastic cells predominated over fibrochondrocytic ones [36].
In cases of allograft failure, it is likely that both biological and biomechanical factors act in consort [19]. The most common region of allograft failure due to tearing and degeneration is adjacent to the posterior horn attachment of the medial meniscus; it is in this location that the medial meniscus experiences the highest contact stresses [19]. Critically, hoop stress transmission and functional load transmission across the knee depend upon correct position and fixation of the anterior and posterior horn attachment sites [19]. When the allograft’s posterior horn attachment is fixed in an excessively posterior position, proper load sharing will not be reestablished [37]. On the other hand, an excessively anterior position of a medial meniscal transplant may result in excessive compressive forces and meniscal damage [38].
Sizing of the allograft also plays a role in the ultimate success or failure of the implant. Undersized grafts result in poor congruity with the femoral condyle and may experience excessive loads [19]. Oversized grafts may be predisposed to extrude from the compartment, resulting in inadequate transmission of compressive loads across the knee [19]. In addition to the biomechanical aspects of sizing, which will be considered below, improper sizing may exacerbate biological or immune responses, which have the potential to undermine the eventual outcome of the allograft [19]. Additional research on how to characterize the biological and biomechanical interactions underlying meniscal allograft incorporation may assist in the understanding of factors relevant to improved clinical outcomes [2].
Allograft risks
The use of allografts is not without special risks, which must be well understood by both clinician and patient. These include a potential for immune reactions and the risk of disease transmission.
Immunologic concerns
Meniscal allografts have been demonstrated to express Class I and II histocompatibility antigens, which confer potential for host immune response [29]. Bone grafts are well known to be immunogenic, so the presence of bone plugs attached to the meniscal graft may increase the risk of immune reaction. [39, 40] One study of fresh meniscal allografts in animals compared immunosuppressed rats to normal counterparts. This investigation demonstrated increased graft survival up to 21 weeks in the immunosuppressed population, while in the normal rats, histologic evidence of rejection was noted [41].
On the other hand, it has been reported that fresh meniscal allografts in conjunction with osteochondral allografts in humans did not elicit any significant immune response at a mean follow-up of 4.5 years [42]. Thus far, there has been only one report of frank immunologic rejection of a cryopreserved, non-tissue-antigen-matched meniscal allograft in a human, based on histologic and clinical evidence [43]. Though immune response of this magnitude is apparently rare, more subtle immune responses may be at work.
One human study demonstrated sensitization to HLA class I and II antigens among cryopreserved graft recipients [44], while another study documented B lymphocyte and cytotoxic T cell presence in nine of 12 deep-frozen graft recipients [34]. The effects of such subclinical immunoreactivity on graft health and outcome are unknown, though it has been proposed that healing, incorporation, and revascularization may be unfavorably altered [2].
Disease transmission
Because meniscal transplantation is not a life-saving measure, a significant risk of graft-related disease transmission could not be acceptable [18]. Given the pitfalls associated with graft processing techniques, stringent donor selection and screening is an essential first step in procurement of healthy allograft tissue [2]. Criteria for selection of donors and methods of tissue screening and processing may vary considerably among tissue banks, and the surgeon should be familiar with the protocols of the tissue bank he or she is using [38]. For example, there is a risk of negative serologic results in the span of time between HIV infection and development of detectable antibodies. Thus, tissue banks should perform polymerase chain reaction (PCR) testing for HIV. The data of 1990, estimate the risk of HIV transmission by frozen connective tissue allografts as 1/8,000,000 [45].
Different types of allograft processing, including ethanol to denature proteins, ultrasonic washing, debridement, or freezing, lower the risk of infection; but HIV can survive washing, freezing, and freeze-drying [46]. Secondary sterilization techniques are, thus, a consideration in an attempt to decrease transmission of HIV and other pathogens. These techniques, which include gamma irradiation, chemical sterilization, and ethylene oxide treatment, are applicable to fresh-frozen or lyophilized grafts only, as they would disrupt cell viability in fresh or cryopreserved tissues. Such methods may, therefore, be impractical in certain situations.
Gamma irradiation is the most common method of secondary sterilization but not without potentially serious drawbacks. A dose of 2.4 mrad destroys nearly all pathogens except HIV; HIV requires more than 3.6 mrad to inactivate all but 1/1,000,000 HIV-infected bone cells [47]. The problem is that at doses at and above 2.5 mrad, the mechanical properties of meniscal tissue may be significantly and adversely altered [48]. Doses below 2.0 mrad are useful for bacterial sterilization [2].
Chemical secondary sterilizations are performed with appropriate bactericidal or virucidal solutions.
Ethylene oxide, with a history of use on lyophilized grafts, is not recommended, because of the risk of inducing synovitis [49].
Indications for meniscal allograft transplantation
The indications for meniscal allograft transplantation have yet to be comprehensively defined. Current recommendations suggest that the procedure is indicated in three clinical scenarios:
-
1.
Young patients with a history of meniscectomy who have pain localized to the meniscus-deficient compartment, a stable knee joint, no malalignment, and articular cartilage with only minor evidence of osteochondral degenerative changes (no more than grade 3 according to the International Cartilage Repair Society classification system (Table 1)) are considered ideal candidates for this procedure. Because of the more rapid deterioration in the lateral compartment [10], a relatively common indication for meniscal transplantation would be a symptomatic, meniscus-deficient, lateral compartment.
-
2.
ACL-deficient patients who have had prior medial meniscectomy (who might benefit from the increased stability afforded by a functional medial meniscus) in conjunction with concomitant ACL reconstruction. In one series, such patients exhibited significantly better KT-1000 arthrometer results as compared with patients who underwent isolated ACL reconstruction with continuing medial meniscal deficiency [50].
-
3.
A third context for meniscal transplantation has also been advocated by some. In an effort to avert early joint degeneration, young, athletic patients who have had complete meniscectomy might be considered as meniscal transplantation candidates prior to symptom onset [51]. This much said, prophylactic meniscal transplantation is not routinely recommended at the present time. The inherent dilemma is that meniscus transplantation is not without risks, and current evidence has yet to demonstrate long-term prevention of arthrosis. However, better graft outcomes do occur in knees with less degenerative change. Earlier surgery may yield superior results. At present, young, athletic, meniscectomized patients may be educated about symptoms of ipsilateral compartment pain and followed up on an yearly basis with 45° PA radiographs or three-phase technetium bone scans to assess progression of joint space narrowing [2, 52]. In an attempt to develop objective indicators for the identification of early articular cartilage changes following meniscectomy, MRI may represent another modality and has been shown to detect fibrillation and early softening of hyaline cartilage [53].
Finally, these may represent ideal indications, but we do not live in an ideal world and indications are rarely perfect for a given patient. As discussed in the next section, patients who meet criteria for meniscus allograft but have instability, malalignment or focal cartilage defects, may be candidates for transplantation as well as procedures to correct associated pathology. Such major interventions must, at present, be considered salvage procedures, and we do not recommend that they be performed casually or by surgeons without extensive experience and expertise in complex knee reconstruction.
Contraindications to meniscal allograft transplantation
The most common contraindication to meniscus allotransplantation is advanced chondral degeneration arthritis. Wear, greater than early grade 3 according to the International Cartilage Repair Society (ICRS) classification system or radiographic evidence of significant osteophyte formation or femoral condyle flattening, is associated with inferior postoperative results [2]. Generally, patients aged over 50 years, have excessive cartilage disease and are suboptimal candidates. The proposed etiology of graft failures in arthritic knees is the joint milieu of destructive enzymes, eroded articular surfaces, and pathological biomechanics [54–56]. The location of chondral lesions is probably as important as their size and depth [19]. Full-thickness articular cartilage lesions greater than 10–15 mm in any dimension that exist in the proximity of the posterior aspect of the transplanted meniscus (specifically the flexion weight bearing zones of the femoral condyle or tibia) should contraindicate the procedure, as it is the degeneration of this posterior meniscal region that most often accounts for graft failure [19]. Localized chondral defects may be treated concomitantly—the meniscus transplant and the cartilage repair or restoration may benefit each other in terms of healing and outcome [19]. Generally, chondrocyte transplantation or osteochondral grafting procedures should be performed after completion of the meniscal transplant in order to prevent accidental damage to the patch or graft meniscal allograft insertion [57].
Axial malalignment tends to exert abnormal pressure on the allograft leading to loosening of the graft, degeneration, and failure [18]. A corrective osteotomy should be considered for greater than 2° of deviation toward the involved compartment, as compared with the contralateral limb mechanical axis [2, 58]. Varus or valgus deformity may be managed with either staged or concomitant high tibial or distal femoral osteotomy [2]. However, as in any situation in which procedures are thus combined, it becomes unclear as to which aspect of the procedure is implicated in symptom resolution, such as relief of pain [18].
Other contraindications to meniscal allotransplantation include: obesity, skeletal immaturity, instability of the knee joint (which may be addressed in conjunction with transplantation as above), synovial disease, inflammatory arthritis, previous joint infection, lack of symptoms (which remains controversial, as above), or symptoms not attributable to the meniscal deficiency.
Patient selection for meniscal allograft transplantation
History
The clinician should elicit a focused history, in order to document the history of injury and ensuing meniscectomy. Often, there will then be an interval of adequate knee function (2–15 years) followed by complaints of relevant compartment pain, swelling, and/or mechanical symptoms exacerbated by physical activity.
Physical examination
In addition to a thorough knee examination, a targeted physical examination must be performed. The surgeon must evaluate patient height and weight, as obesity and graft sizing play important roles in surgical decision making. When examining range of motion, the acceptable extension is within 5° of normal, and flexion must exceed 125° . Compromised range of motion of the knee is likely to be exacerbated postoperatively. If an effusion exists in the absence of activity, this may suggest advanced degeneration of the compartment [58]. Angular alignment and mechanical axis of the involved lower extremity requires evaluation to determine if an osteotomy is required in conjunction with the meniscus transplantation. Ligamentous stability must also be assessed. Any deficit noted preoperatively should also be addressed in a staged fashion or at the time of meniscal transplantation. Location of pain and tenderness should be isolated to the ipsilateral compartment. The patient may be asked to jump, squat, or run to evaluate exertional compartment pain. Quadriceps strength with recording of circumferential measurements should be noted, as this may be reduced in the affected limb secondary to chronic pain.
Diagnostic imaging
Standard plain films are required as part of the preoperative evaluation. These should include weight-bearing AP radiographs of bilateral knees in full extension, a non-weight bearing 45° flexion lateral radiograph, and an axial radiograph of the patellofemoral joint [2]. To disclose potentially subtle narrowing of the joint space that may be overlooked on traditional extension views, a 45° flexion weight-bearing PA radiograph is also recommended [59].
Depending upon the clinical scenario, special imaging studies may be indicated, such as long-cassette mechanical axis radiography in cases of clinical malalignment and possibly bone scan or high-resolution MRI to evaluate for chondral injury (unless joint-space narrowing on the 45° flexion weight-bearing PA radiograph preempts the need).
Current MRI techniques include two-dimensional fast spin-echo and three-dimensional fat suppression with and without intra-articular gadolinium [53]. Some authors report that MRI should be reserved for difficult cases with an elusive diagnosis, in particular, those which demonstrate no radiographic abnormalities or those lacking previous operative reports to verify the extent of prior meniscectomy or the condition of the articular cartilage [2]. Others feel that routine MRI may be useful for documentation of articular cartilage defects and the status of subchondral bone, as well as any remaining meniscus [19, 60].
A three-phase technetium bone scan may be obtained if questions remain about the source of symptoms, in order to look for increased uptake in the involved compartment [2].
Allograft sizing and selection
Meniscal allografts are specific to compartment and side. Certain grafts are unacceptable for transplantation, and the surgeon should be aware of these. Medial menisci with a hypoplastic, narrow anterior horn attachment that inserts distal to the medial tibial surface (i.e., Type III) [63] are not appropriate allograft material [38]. A lateral meniscus with a shortened anteroposterior dimension, less than what is calculated on the recipient’s sagittal radiograph, is another example of an unsuitable graft [38]. Medial or lateral menisci with a width of 8–10 mm in the middle one-third can only be used in small patients [38]. Correct size of the allograft is likely to be critical to successful healing and functionality and to maximize the graft’s potential capacity to be chondroprotective [62]. Knee joint tolerance for size mismatch is not completely understood although some estimate that graft size should be within 5% of the original meniscus [48, 63]. Small size mismatches may be managed with minor modifications [2, 62] however, reduction of meniscus size may damage the collagen structure and may well interfere with the mechanical properties of the graft [64].
Different techniques have been employed in an attempt to match meniscal allografts with host size requirements. Use of the contralateral meniscus for sizing, remains controversial in view of numerous cases of demonstrated anatomic variability and asymmetry between left and right knees [63, 65]. MRI has both been described as producing excessively low estimates of the size of menisci [66, 67], and as having somewhat improved accuracy over radiography as a means of preoperative sizing [68, 69].
Currently, plain radiographs appear to serve as the gold standard of preoperative graft sizing [68]. The most common method at present, has been developed by Pollard et al. [70]. Using this approach: (1) correct for magnification; (2) in the coronal plane, calculate the width of the meniscus on the AP radiograph by measuring from the medial or lateral tibial metaphyseal margin, disregarding marginal osteophyte, to the peak of the respective tibial eminence; (3) calculate the length of the lateral meniscus as 70% of the tibial plateau sagittal length on the lateral radiograph, and calculate the length of the medial meniscus as 80% of this measurement (the sagittal length of the tibial plateau is defined as the distance measured at the joint line between a line running parallel to the tibia’s anterior and posterior margins).
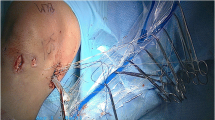
Surgical techniques
[Author’s preferred methods: the senior authors prefer different methods of meniscal allotransplantation surgical technique. Currently, author JHL (Taos, New Mexico, USA), prefers to implant fresh-frozen allografts using an arthroscopic trough technique for both the medial and lateral menisci. Author RV (Ghent, Belgium), prefers to implant viable meniscal allografts using open technique using soft tissue fixation without bone plugs both medially and laterally. In the following, we attempt to review, in an unbiased fashion, the surgical techniques reported in the published literature. The review is concise and incomplete; review of surgical technique guides or textbooks which could supplement continuing medical education courses or residency or fellowship training is required as a part of careful pre-operative planning prior to performing meniscal allograft transplantation surgery.]
Similar outcomes have been reported following both open and arthroscopic-assisted techniques (other than cosmetic differences) [19, 58]. However, some believe that an open surgical procedure, especially on the medial side, may enable more secure peripheral suturing or bony fixation of the graft allowing greater precision and stability [58]. Proponents of the open method assert that the post-operative period for patients undergoing open allotransplantation is similar to that of patients having arthroscopic transplantation, specifically reporting that patients require no more analgesics, can be discharged on the same day (as outpatients), enjoy immediate functioning of all muscle groups and require no special modifications to rehabilitation other than an initial need to protect the medial collateral ligament [58]. On the other hand, while greater technical proficiency may be required with arthroscopic techniques, some experts feel that a positive trend is toward arthroscopically based procedures [2, 18], citing reduced surgical morbidity, avoidance of collateral ligament disruption, and earlier rehabilitation.
Whether an arthroscopic or open technique is chosen, the correct anatomic positioning and peripheral fixation of the graft is of primary importance. Though it may be easier to secure the graft by soft tissue alone, cadaver model research indicates that superior transmission of load occurs when securing the graft with bone [71–73].
For all techniques
In the preparation for transplantation, it is of crucial importance not to remove completely nor to transect the remnant meniscal rim. This rim is deemed an important envelope encapsulating the compartment, limiting extrusion of the graft and providing an excellent bed for meniscal suturing and fixation.
Open technique: medial double bone plug
The open approach to medial meniscal transplantation, as described by Goble [58], may be summarized as follows: the knee is supported by a proximal thigh leg-holder device in 80° of flexion. A medial curvilinear incision is performed, starting just medial to the patellar tendon at the joint line and extending proximally to a point just proximal and posterior to the medial femoral epicondyle. An interval is developed from the anteromedial joint line along the patellar tendon to a point proximal and medial to the patella. An incision is made in the synovium deep to this interval; with posterior retraction, one should be able to visualize, distally, the medial gutter, including the medial articular border of the medial femoral condyle, and proximally, the anterior, inferior, and superior edges of the medial epicondyle, as well as its soft tissue attachments.
The origin of the medial collateral ligament on the medial epicondyle is removed from anterior to posterior and distal to proximal, using a curved 1 inch osteotome. The bone is scored both posterior and distal to the medial epicondyle, in order to forestall extension of the osteotomy to the margin of the femoral articular border. The medial compartment is exposed using valgus stress after elevating the medial epicondyle from anterior to posterior and using the curved osteotome to sharply dissect the posterior capsular attachment from the posteromedial femur. Sharp excision of any medial meniscal remnants is performed.
Two 10 mm holes are then prepared directly at the anatomic site of each horn’s bony insertion. The middle of each of the graft’s bone plugs is secured with a 20 mm long, 4 mm cancellous screw. This permits compression of each plug within its recipient hole, using a lag screw technique (instead of fixation by transosseous suture. An alternative is to insert a bioabsorbable 7 mm diameter interference screw alongside the bone block). The meniscal edge (not the surface of the meniscus) is sutured to the joint capsule. Reattachment of the medial epicondyle to the femur is achieved by staple or screw and washer technique. Standard closure is performed.
Open technique: lateral or trough
A lateral double bone plug technique could be performed in a similar manner, but lateral meniscal allotransplantation is usually performed using the trough technique. A lateral (or medial) open trough technique could be performed with arthrotomy and the trough method as described below.
Open technique: medial or lateral, with soft tissue fixation
Medial and lateral meniscal allotransplantation can be performed using only soft tissue fixation (no bony fixation). The collateral ligament is released with a bone plug from the epicondyle to open up either affected compartment. This allows for all-inside suture fixation of the allograft to the meniscal rim. In addition, the meniscal soft tissue at the anterior and posterior horns may be fixed in tibial tunnels with interference or biotenodesis screw fixation or transosseous suture Anterior horn fixation may be augmented using suture anchors [74]. Alternatively, surgeons may eliminate tibial tunnels and tibial fixation entirely.
Arthroscopic techniques
The most common arthroscopic methods are the trough or “Bridge in Slot” techniques for lateral (much more commonly than medial) meniscal transplantation, and the double bone plug technique for medial meniscal transplantation. (The “Keyhole” technique is a variation of the trough technique in which the shapes of the bone block and recipient slots are keyhole shaped).
The trough technique is the preferred method for lateral meniscus transplantation because the distance between the anterior and posterior horns of the lateral meniscus is small (1 cm or less), and a single block of bone is ideal [2, 58]. The double bone plug technique is most common for the medial meniscus because the anterior and posterior horns are more widely spaced and because a trough may compromise the tibial attachment of the anterior cruciate ligament. Those supporting use of the trough technique (single bone block) on the medial side emphasize that the anatomic relationship between anterior and posterior horns is preserved; in addition, there may be improved ease of insertion with this method [2]. Furthermore, “tight” knees with a limited amount of medial joint opening may benefit from the trough technique as the surgeon is thereby, able to circumvent disruption of the medial collateral ligament [38]. Otherwise, partial detachment of the distal aspect of the medial collateral ligament or partial division of the midsubstance of the MCL (judiciously, using an arthroscopic knife while applying valgus stress to create a Grade I MCL lesion) may be required, to prevent articular cartilage scuffing during meniscal allotransplantation in tight knees. On the other hand, those favoring use of bone plugs on the medial side highlight the anterior horn attachment site’s variability and extol the utility of being able to make minor positional adjustments [61, 75].
For all arthroscopic techniques, positioning of the patient is according to the surgeon’s preference, for arthroscopy combined with mini-arthrotomy. Examination under anesthesia is performed both to verify absence of ligamentous laxity and to confirm range of motion. Exsanguination and use of a tourniquet may be postponed during the initial arthroscopic portions of the case until bleeding impedes visualization. This may allow reduction of total tourniquet time or allow adequate time to complete the entire case without exceeding the maximum time recommended for a single period of tourniquet inflation.
Modifications for concomitant ACL reconstruction
When ACL reconstruction is undertaken concomitantly with double bone plug (medial) meniscal transplantation, the ACL tibial tunnel’s starting point is adjusted to be in a slightly more medial and proximal position so as to fall between the tunnels for the bone plugs [18]. For the trough technique, drilling of the ACL tibial tunnel follows the implementation of the bone–bone block. Though the bone block may be partially violated by the ACL tibial tunnel, the slot’s integrity generally remains intact [19].
Combination medial and lateral meniscal transplantation
In this scenario, an arthrotomy is used. The allografts can be implanted with a common bone bridge that contains both meniscal attachments [19]. The authors have no experience with this technique.
Complications of human meniscal allograft transplantation
In addition to the usual potential complications of surgery and anesthesia and the risks of allograft tissue (considered above), complications after meniscus allotransplantation are rare and include arthrofibrosis, loss of bone plug or bone block fixation, detachment of the meniscus from the bone block, meniscal allograft tear or failure to heal to the periphery (requiring re-repair or partial meniscectomy of the graft), continued or progressive pain or progression of degenerative joint disease, and as a result (or due to infection or persistent synovitis), need for allograft removal. [4, 18, 42, 76–80].
Rehabilitation
The effects of loading on a new meniscal allograft are not well understood. Though there is still some lack of consensus on best rehabilitation, it is generally similar to meniscal repair.
The lack of controlled studies and absence of consensus have yielded a variety of approaches. In animal studies, immediate full weight bearing did not appear to undermine healing of the grafts, [35, 81, 82], and one human study indicated that immediate full range of motion with unlimited weight bearing could produce good results [83]. At the other extreme, some recommend maintaining the lower limb in full extension, non-weight bearing for 6 weeks [84].
Recent articles have suggested that, in theory, it is prudent to implement a fairly conservative rehabilitation protocol because in a joint with early degenerative changes, there are higher loads associated with a new meniscal implant [2]. With this in mind, limiting flexion initially may be warranted because the meniscus remains relatively fixed on the tibia through the first 60° of flexion [13] at which point, anterior translation of the meniscus with displacement from the capsule and increased stress on a posterior repair begins. Early weight bearing may be allowed; some restriction is recommended (i.e., protected weight bearing in a hinged knee immobilizer for the first 4–6 weeks) due to concerns regarding damage to the graft or compromise of graft fixation and healing during early postoperative revascularization [82, 83]. One of us, (JHL), allows full weight bearing with the knee locked in extension for the first 6 weeks, and unrestricted motion while non-weight bearing. The senior author (RV) advocates a postoperative rehabilitation comprising 3 weeks of non-weight bearing with mobilization of the knee within pain limits and limitation of flexion to 60°. After 3 weeks, patients are allowed to flex the knee to 90° and to start partial weightbearing. At 6 weeks, patients are permitted to walk with one crutch, which may be discontinued after two more weeks.
Regardless of weight bearing, an early goal of the rehabilitation protocol is to gain full extension. Some authors stress on isometric exercises to prevent muscle atrophy, as well as commencement of closed-chain kinetic exercises with weight bearing (around week 3–4), avoidance of forced flexion and pivoting, and postponement of any return to strenuous activity and sports until patients demonstrate strength and proprioception close to normal [2]. The expected time frame for this goal is said to range from 4 to 12 months, with running at four to 6 months and return to full activity at 6–9 months [2].
Though survival of transplanted menisci after high-impact activity is unknown, many patients attempt such activities despite recommended restrictions. Further research is required to understand the loads experienced by a meniscal allograft and graft fixation sites during various rehabilitation activities, as well as to describe the types of stress and the magnitude of such stress required to either promote or compromise healing of the implant [85, 86].
Findings from meniscal transplantation studies
Meniscal allotransplantation literature is confounded by diverse patient- and surgeon-specific variables [2], including degree of arthrosis, type of graft processing, surgical technique, concomitant procedures, and outcome measures. Clinical evaluation, using physical examination or subjective symptoms may not reliably correlate with the condition of the allograft [54]. Both MRI and second-look arthroscopy have been used to obtain objective evaluation of the status of meniscal allografts post-transplantation [18, 33]. Although more invasive, arthroscopy may correlate better with outcome than MRI [87]. In the future, advanced MRI techniques, such as weight bearing MRI and dynamic MRI, may improve noninvasive assessment post-meniscal implantation [33]. Finally, neither gross nor microscopic appearance of the transplant necessarily correlate with its biomechanical functionality.
Selected human outcome studies from the last decade are summarized in Table 2. Over the last several years, the trend is of increasingly successful outcomes, perhaps as a result of refinement in selection of patients, graft processing and preparation, and surgical technique. Overall, the literature describes good or excellent results (as defined by admittedly diverse outcome measures) in approximately 85% of meniscal allograft transplantations [88].
While most studies with early and mid-term follow-up describe healing of the allograft to the periphery and symptomatic improvement, long-term results regarding pain relief and reduction or slowing of arthrosis have yet to be clearly established [18]. However, series with long-term follow-up are beginning to be published. Verdonk et al. [89] describe 100 procedures in 96 patients; survival analysis shows that pain relief and functional improvement persist in approximately 70% of patients at ten-year follow-up. An additional finding is that medial and lateral meniscal transplantations have similar longevity unless the transplanted knee is lacking a functional ACL, in which case the survival of medial implants tends to be compromised [89, 90].
Potential long-term effects on articular cartilage
In all meniscal allograft studies, the lack of a control group consisting of conservatively treated symptomatic postmeniscectomy patients limits the power to detect a chondroprotective effect. In addition, there is a scarcity of published data beyond ten years of follow-up. Though meniscal deficiency correlates with articular cartilage degeneration as confirmed by MRI [91], it has not yet been shown that meniscal transplantation forestalls or reverses this process over time. Moreover, clinical outcome may not correlate with the condition of the allograft [54].
Macroscopic findings
As noted, diverse study designs make comparison of data difficult. Some studies are descriptive while others lack controls; others employ various grading systems to quantify (or qualify) articular cartilage changes. However, certain concepts are supported by animal investigations. Outcome following immediate transplantation may be superior to outcome post-chronic meniscal deficiency [55]. In addition, there is some evidence that following meniscal transplantation, the articular cartilage underlying the graft appears “more normal” than the adjacent articular surface after weeks or months [42, 92, 93]. However, degeneration of the articular surface does continue to be observed post-transplantation, although some describe less deterioration in the short-term after transplantation than in meniscectomized controls [33].
Histological evaluation
Mixed results are reported; some animal studies show protection of articular cartilage in immediately transplanted knees [92, 94, 95]. Others demonstrate microscopic evidence of chondroprotection after both immediate and delayed transplantation or even suggest that degenerative changes may be reversed [96] Yet, others counter that such reversals may be transient [94, 95], and others, still, show no significant histological differences between transplanted and meniscectomized subjects [97]. In general, available histological data in animals supports the concept that immediate meniscal transplantation is associated with a greater degree of articular cartilage protection as compared with delayed transplantation [33].
Radiographic evaluation
Radiographic follow-up in the short to mid-term describes few significant changes in articular cartilage post-meniscal allotransplantation [33]. A recently published long-term study observed no progression of joint space narrowing in a considerable number of allograft patients [98]. However, X-rays are not sensitive to early degenerative changes [99, 100].
Scintigraphic evaluation
Although infrequently used as a routine imaging technique, scintigraphy may offer an advantage over routine radiography regarding ability to sensitively detect early changes as shown in a rabbit model [101]. However, this finding has been questioned [95, 102]. One study described a non-statistically significant chondroprotective effect of meniscal allotransplantation and reported the negative result of greater degenerative change in articular cartilage (in cases of delayed meniscal transplantation) than after meniscectomy alone in rabbits [102].
MRI
This imaging modality is becoming increasingly important in assessing the condition of articular cartilage and the meniscus allograft, and it is expected that more sophisticated MRI techniques will aid in long-term evaluation of meniscal transplantation [33]. Current long-term data in the literature suggests a potential chondroprotective effect over 10 years in a subset of patients [98].
Biomechanical studies
Some animal studies suggest that transplanted menisci manifest inferior biomechanical function as compared to normals [103]. One study states that after both meniscectomy or meniscal transplantation, femoral articular cartilage manifests a significantly lower tensile modulus as compared with non-operated controls [97]. It is unclear whether meniscal allografts improve weight distribution throughout the joint [33], although some authors do suggest improvement [104–107].
Potential alternative treatments
Alternative treatments to meniscal allograft transplantation have been investigated in an attempt to maximize functionality and minimize risks in the meniscus-deficient knee. Alternatives include meniscal regeneration [108–110] which seems to result in inferior and disorganized tissue structure, autogenous grafts [92, 111–114] which do not seem feasible in humans, resorbable scaffolds [23, 93, 115–117] which have precedent in human skin replacement and as nerve conduits and hold great promise, xenografts which currently do not seem feasible due to sizing and immunorejection issues, and meniscal prostheses. With the exception of resorbable scaffolds [118, 119], none of these options has yet seemed clinically feasible [33].
Future directions
There seems to be an evolving consensus regarding the importance of early detection of degenerative changes in the post-meniscectomized knee. This could resolve the dilemma of optimal timing of meniscal allotransplantation. Strategies include greater clinical surveillance of these patients, high-resolution MRI [53], scintigraphy, and synovial fluid analysis (to assess indices of degeneration, such as collagen or proteoglycan breakdown products or metalloproteinase activity) [33]. In the future, bioactive scaffolds, tissue engineering, gene therapy, and combinations thereof may also prove an alternative to meniscal allografts.
Conclusion
Although published studies are often difficult to compare, meniscal allograft transplantation appears to reliably result in pain relief and improved function. Future research must determine if the beneficial effects will persist beyond an intermediate range of follow up. Nevertheless, “typical” meniscal allograft patients may find intermediate-term gains acceptable and a priority in the final analysis. Additional and long-term studies are needed to evaluate the optimal timing of meniscal allotransplantation in humans and to evaluate the actual function and condition of the allografts. An ultimate question is whether or not this procedure provides long-term prevention or delay of articular cartilage degeneration and osteoarthritis. In addition, other approaches to the meniscus-deficient knee may continue to develop.
References
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30B:664–670
Cole BJ, Carter TR, Rodeo SA (2003) Allograft meniscal transplantation: background, techniques, and results. Instr Course Lect 52:383–396
Locht RC, Gross AE, Langer F (1984) Late osteochondral resurfacing for tibial plateau fractures. J Bone Joint Surg Am 66:328–335
Milachowski KA, Weismeier K, Wirth CJ (1989) Homologous meniscal transplantation: Experimental and clinical results. Int Orthop 13:1–11
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Helfet AJ (1959) Mechanism of derangements of the medial semilunar cartilage and their management. J Bone Joint Surg Br 41:319–336
Levy IM, Torzilli PA, Gould JD, Warren RF (1989) The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am 71:401–406
MacConaill MA (1931) The function of intra-articular fibrocartilages, with special reference to the knee and inferior radiolunar joints. J Anat 66:210–227
Simon WH, Friedenberg S, Richardson S (1973) Joint congruence: a correlation of joint congruence and thickness of articular cartilage in dogs. J Bone Joint Surg Am 55:1614–1620
Walker PS, Erkman MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop 109:184–192
Simonian PT, Sussmann PS, van Trommel M, Wickiewicz TL, Warren RF (1997) Popliteomeniscal fasciculi and lateral meniscal stability. Am J Sports Med 25:849–853
Staubli HU, Birrer S (1990) The popliteus tendon and its fascicles at the popliteal hiatus: gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy 6:209–220
Thompson WO, Thaete FL, Fu FH, Dye SF (1991) Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med 19:210–216
Arnoczky SP, McDevitt CA (2000) The meniscus: structure, function, repair and replacement. In: Buckwalter JA, Einhorn TA, Simon SR (eds) Orthopaedic basic science: biology and biomechanics of the musculoskeletal system. 2nd ed American Academy of Orthopaedic Surgeons, Rosemont, pp 531–545
Arnoczky SP, Warren RF (1982) Microvasculature of the human meniscus. Am J Sports Med 10:90–95
Fithian DC, Kelly MA, Mow VC (1990) Material properties and structure–function relationships in the menisci. Clin Orthop 252:19–31
Favenesi JA, Shaffer JC, Mow VC (1983) Biphasic mechanical properties of knee meniscus. Trans Orthop Res Soc 7:264–265
Rijk PC (2004a) Meniscal allograft transplantation—part I: background, results, graft selection and preservation, and surgical considerations. Arthroscopy 20:728–743
Rodeo SA (2001) Meniscal allografts—where do we stand? Am J Sports Med 29:246–261
Arnoczky SP, DiCarlo EF, O’Brien SJ, Warren RF (1992) Cellular repopulation of deep-frozen meniscal autografts: an experimental study in the dog. Arthroscopy 8:428–436
Day B, Mackenzie WG, Shim SS, Leung G (1985) The vascular and nerve supply of the human meniscus. Arthroscopy 1:58–62
Zimny ML, Albright DL, Dabeziew E (1988) Mechanoreceptors in the human medial meniscus. Acta Anat 133:35–40
Jackson DW, Whelan J, Simon TM (1993) Cell survival after transplantation of fresh meniscal allografts: DNA probe analysis in a goat model. Am J Sports Med 21:540–550
Verdonk R (1997) Alternative treatment for meniscal injuries. J Bone Joint Surg 79B:866–873
Verdonk R, Van Daele P, Claus B et al (1994) Viable meniscus transplantation (in German). Orthopade 23(2):153–159
Arnoczky SP, Milachowski KA (1990) Meniscal allografts: where do we stand? In: Ewing JW (ed) Articular cartilage and knee joint function: basic science and arthroscopy. Raven, New York, pp 129–136
Siegel MG, Roberts CS (1993a) Meniscal allografts. Clin Sports Med 12:59–80
Brown KL, Cruess RL (1982) Bone and cartilage transplantation in orthopaedic surgery. A review. J Bone Joint Surg Am 64:270–279
Khoury MA, Goldberg VM, Stevenson S (1994) Demonstration of HLA and ABH antigens in fresh and frozen human menisci by immunohistochemistry. J Orthop Res 12:751–757
Milachowski KA, Weismeier K, Erhardt W, Remberger K (1987) Transplantation of the meniscus: an experimental study in sheep. Sportverletzung Sportschaden 1:20–24
Garrett JC, Stevensen RN (1991) Meniscal transplantation in the human knee. A preliminary report. Arthroscopy 7:57–62
Jackson DW, Windler GE, Simon TM (1990a) Intraarticular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone-patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med 18:1–11
Rijk PC (2004b) Meniscal allograft transplantation—part II: alternative treatments, effects on articular cartilage, and future directions. Arthroscopy 20:851–859
Rodeo SA, Seneviratne A, Suzuki K, Felker K, Wickiewicz TL, Warren RF (2000) Histological analysis of human meniscal allografts: a preliminary report. J Bone Joint Surg Am 82:1071–1082
Jackson DW, McDevitt CA, Simon TM, Arnoczky SP, Atwell EA, Silvino NJ (1992) Meniscal transplantation using fresh and cryopreserved allografts: an experimental study in goats. Am J Sports Med 20:644–656
Noyes FR, Barber-Westin SD (1995) Irradiated meniscus allografts in the human knee: a two to five year follow-up study. Orthop Trans 19:417
Alhalki MM, Hull ML, Howell SM (2000a) Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft. A human cadaveric study. Am J Sports Med 28:370–376
Noyes FR, Barber-Westin SD, Rankin M (2005) Meniscal transplantation in symptomatic patients less than fifty-years old. J Bone Joint Surg Am 87:149–165
Bos GD, Goldberg VM, Zika JM, Heiple KG, Powell AE (1983) Immune responses of rats to frozen bone allografts. J Bone Joint Surg Am 65:239–246
Stevenson S (1987) The immune response to osteochondral allografts in dogs. J Bone Joint Surg Am 69:573–582
Wada Y (1993) Meniscal transplantation using fresh and cryopreserved allografts. An experimental study in the genetically defined rat. J Jpn Orthop Assoc 67:677–683
Zukor DJ, Cameron JC, Brooks PJ et al (1990) The fate of human meniscal allografts. In: Ewing JW (ed) Articular cartilage and knee joint function. Raven, New York, pp 147–152
Hamlet W, Liu SH, Yang R (1997) Destruction of a cryopreserved meniscal allograft: a case for acute rejection. Arthroscopy 13:517–521
van Arkel ERA, van den Berg-Loonen EM, van Wersch JW, de Boer HH (1997) Human leukocyte antigen sensitization after cryopreserved human meniscal transplantations. Transplantation 64:531–533
Buck BE, Resnick L, Shah SM, Malinin TI (1990) Human immunodeficiency virus cultured from bone. Implications for transplantation. Clin Orthop 251:249–253
Nemzek JA, Arnoczky SP, Swenson CL (1994) Retroviral transmission by the transplantation of connective-tissue allografts: an experimental study. J Bone Joint Surg Am 76:1036–1041
Conway B, Tomford W, Mankin HJ, Hirsch MS, Schooley RT (1991) Radiosensitivity of HIV-I: potential application to sterilization of bone allografts. AIDS 5:608–609
Yahai L, Zukor D (1994) Irradiated meniscal allotransplants of rabbits: study of the mechanical properties at six months post-operation. Acta Orthop Belg 60:210–215
Jackson DW, Windler GE, Simon TM (1990b) Intra-articular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med 18:1–11
Barber FA (1994) Accelerated rehabilitation for meniscus repairs. Arthroscopy 10:206–210
Johnson DL, Bealle D (1999) Meniscal allograft transplantation. Clin Sports Med 18:93–108
Dye SF, Chew MH (1993) The use of scintigraphy to detect increased osseous metabolic activity about the knee. J Bone Joint Surg Am 75:1388–1406
Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB (1998a) Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am 81:1349–1350
Garrett JC (1993) Meniscal transplantation: a review of 43 cases with 2- to 7- year follow-up. Sports Med Arthrosc Rev 1:164–167
Aagaard H, Jorgenssen U, Bojsen-Moller F (1999) Reduced degenerative articular cartilage changes after meniscal allograft transplantation in sheep. Knee Surg Sports Traumatol Arthrosc 7:184–191
Siegel MG, Roberts CS (1993b) Meniscal allografts. Clin Sports Med 12:59–80
Cole BJ, Cohen B (2000) Chondral injuries of the knee. A contemporary view of cartilage restoration. Orthop Spec Ed 6:71–76
Goble EM (2004) Arthroscopic meniscus transplantation: plug and slot technique. In: Miller M, Cole BJ (eds) Textbook of arthroscopy. WB Saunders, Philadelphia, pp 536–546
Rosenberg TD, Paulos LE, Parker RD et al (1988) The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am 70:1479–1483
Potter HG, Linklater JM, Allen AA et al (1998b) Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am 80:1276–1284
Berlet GC, Fowler PJ (1998) The anterior horn of the medial meniscus. An anatomic study of its insertion. Am J Sports Med 26:540–543
Verdonk R, Kohn D (1999) Harvest and conservation of meniscal allografts. Scand J Med Sci Sports 9:158–159
Wilcox TR, Goble EM, Doucette SA (1996) Goble technique of meniscus transplantation. Am J Knee Surg 9:37–42
Kohn D (1994) Meniscus transplantation. In: Fu FH (ed) Advances in operative orthopaedics. Mosby-Year Book, Chicago, 2:49–76
Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD (1995) Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 11:386–394
Garrett JC (1992) Meniscal transplantation. In: Aichroth PC, Canon WD, Patel DV (eds) Knee surgery: current practice. Raven, New York, pp 95–103
Johnson DL, Swenson TM, Harner CD (1994) Meniscal reconstruction using allograft tissue: an arthroscopic technique. Oper Tech Sports Med 2:223–231
Shaffer B, Kennedy S, Klimkiewicz J, Yao L (2000) Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med 28:524–533
Haut TL, Hull ML, Howell SM (2000) Use of roentgenography and magnetic resonance imaging to predict meniscal geometry determined with a three-dimensional coordinate digitizing system. J Orthop Res 18:228–237
Pollard ME, Kang Q, Berg EE (1995) Radiographic sizing for meniscal transplantation. Arthroscopy 11:684–687
Chen MI, Branch TP, Hutton WC (1996) Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 12:174–181
Paletta GA Jr, Manning T, Snell E, Parker R, Bergfeld J (1997) The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee: a biomechanical study. Am J Sports Med 25:692–698
Alhalki MM, Howell SM, Hull ML (1999) How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med 27:320–328
Verdonk PCM, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R (2006) Transplantation of viable meniscal allograft. J Bone Joint Surg Am 88(1 Suppl 1):109–118
Kohn D, Moreno B (1995) Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy 11:96–103
Kuhn JE, Wojtys EM (1996) Allograft meniscal transplantation. Clin Sports Med 15:537–556
Goble EM, Kohn D, Verdonk R, Kane SM (1999) Meniscal substitutes-human experience. Scand J Med Sci Sports 9:146–157
Cameron JC, Saha S (1997) Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop 337:164–171
Rath E, Richmond JC, Yassir W, Albright JD, Gundogan F (2001) Meniscal allograft transplantation. Two-to-eight-year results. Am J Sports Med 29:410–414
Shelton WR, Dukes AD (1994) Meniscus replacement with bone anchors: a surgical technique. Arthroscopy 10:324–327
Mikic ZD, Brankov MZ, Tubic MV, Lazetic AB (1993) Allograft meniscus transplantation in the dog. Acta Orthop Scand 64:329–332
Rijk PC, Van Noorden CJF (2002) Structural analysis of meniscal allografts after immediate and delayed transplantation in rabbits. Arthroscopy 18:995–1001
Stollsteimer GT, Shelton WR, Dukes A, Bomboy AL (2000) Meniscal allograft transplantation: a 1-to-5 year follow-up of 22 patients. Arthroscopy 16:343–347
Fritz JM, Irrgang JJ, Harner CD (1996) Rehabilitation following allograft meniscal transplantation: a review of the literature and case study. J Orthop Sports Phys Ther 24:98–106
Anderson DR, Gershuni DH, Nakhostine M, Danzig LA (1993) The effects of non-weight-bearing and limited motion on the tensile properties of the meniscus. Arthroscopy 9:440–445
Dowdy PA, Miniaci A, Arnoczky SP, Fowler PJ, Boughner DR (1995) The effect of cast immobilization on meniscal healing: an experimental study in the dog. Am J Sports Med 23:721–728
Van Arkel ERA, Goei R, de Ploeg I, de Boer HH (2000) Meniscal allografts: evaluation with magnetic resonance imaging and correlation with arthroscopy. Arthroscopy 16:517–521
Alford W, Cole BJ (2005) The indications and technique for meniscal transplant. Orthop Clin N Am 36:468–484
Verdonk PCM, Demurie A, Almqvist KF, Veys EM, Verbruggen, Verdonk R (2005) Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am 87:715–724
Van Arkel ERA, De Boer HH (2002) Survival analysis of human meniscal transplantation. J Bone Joint Surg Br 84:227–231
Potter HG, Rodeo SA, Wickiewicz TL et al (1996) MR imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology 198:509–514
Szomor ZL, Martin TE, Bonar F, Murrell GAC (2000) The protective effects of meniscal transplantation on cartilage: an experimental study in sheep. J Bone Joint Surg Am 82:80–88
Messner K (1999) Meniscal regeneration or meniscal transplantation? Scand J Med Sci Sports 9:162–167
Aagaard H, Jorgensen U, Bojsen-Moller F (2003) Immediate versus delayed meniscal allograft transplantation in sheep. Clin Orthop 406:218–227
Rijk PC, Tigchelaar-Gutter W, Bernoski FP, Van Noorden CJF (2004) Histologic changes of articular cartilage after meniscus replacement in rabbits. Arthroscopy 20:911–917
Cummins JF, Mansour JN, Howe Z, Allan DG (1997) Meniscal transplantation and degenerative articular change: an experimental study in the rabbit. Arthroscopy 13:485–491
Elliott DM, Jones R, Setton LA, Sully SP, Vail TP, Guilak F (2002) Joint degeneration following meniscal allograft transplantation in a canine model: mechanical properties and semiquantitative histology of articular cartilage. Knee Surg Sports Traumatol Arthrosc 10:109–118
Verdonk PCM, Verstraete KL, Almqvist KF, De Cuyper K, Veys EM, Verbruggen G, Verdonk R (2006) Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc (Epublication ahead of print)
Messner K, Fahlgren A, Persliden J, Andersen BM (2001) Radiographic joint space narrowing and histologic changes in a rabbit meniscectomy model of early knee osteoarthrosis. Am J Sports Med 2:151–160
Thomas RH, Resnick D, Alazraki NP, Daniel D, Greenfield R (1975) Compartmental evaluation of osteoarthritis of the knee. A comparative study of available diagnostic modalities. Radiology 116:585–594
Christensen SB (1983) Localization of bone-seeking agents in developing experimentally induced osteoarthritis in the knee joint of the rabbit. Scand J Rheumatology 12:343–349
Rijk PC, Van Eck-Smit BLF, Van Noorden CJF (2003) Scintigraphic assessment of rabbit knee joints after meniscal allograft transplantation. Arthroscopy 19:506–510
Bylski-Austrow DI, Meade T, Malumed J et al (1992) Irradiated meniscal allografts: mechanical and histological studies in the goat. Trans Orthop Res Soc 17:175
Paletta GA Jr, Manning T, Snell E, Parker R, Bergfeld J (1997) The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med 25(5):692–698
Alhalki MM, Hull ML, Howell SM (2000) Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft: a human cadaveric study. Am J Sports Med 28:370–376
Chen MI, Branch TP, Hutton WC (1996b) Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 12(2):174–81
von Lewinski G, Hurschler C, Allmann C, Wirth CJ (2006) The influence of pre-tensioning of meniscal transplants on the tibiofemoral contact area. Knee Surg Sports Traumatol Arthrosc 14(5):425–436
Moon MS, Woo YK, Kin YI (1988) Meniscal regeneration and its effects on articular cartilage in rabbit knees. Clin Orthop 227:298–304
Elmer RM, Moskowitz RW, Frankel VH (1977) Meniscal regeneration and postmeniscectomy degenerative joint disease. Clin Orthop 124:304–310
Ghosh P, Taylor TKF, Pettit GD, Horsburgh BA, Bellanger CR (1983) Effect on postoperative immobilization of the regrowth of the knee joint semilunar cartilage: an experimental study. J Orthop Res 1:153–164
Stone KR, Rodkey WG, McKinney LA, Steadman JR (1995) Autogenous replacement of the meniscal cartilage: analysis of results and mechanics of failure. Arthroscopy 11:395–400
Bruns J, Kahrs J, Kampen J, Behrens P, Plitz W (1998) Autologous perichondral tissue for meniscal replacement. J Bone Joint Surg Br 80:918–923
Kohn D, Wirth CJ, Reiss G, Plitz W, Maschek H, Erhardt W, Wulker N (1992) Medial meniscus replacement by a tendon autograft. Experiments in sheep. J Bone Joint Surg Br 74(6):910–917
Pressel T, v Lewinski G, Kohn D, Wirth CJ (2005) Der Meniskusersatz mit autologer Quadrizepssehne - eine Langzeitanalyse. Z Orthop Ihre Grenzgeb 143(1):42–47
Yannas IV (1992) Tissue regeneration by use of collagen-glycosaminoglycan copolymers. Clin Mater 9:179–187
Yannas IV, Burke JF (1980) Design of artificial skin: 1. design principles. J Biomed Mater Res 14:65–81
Klompmaker J, Veth RP, Jansen HW, Nielsen HK, De Groot JH, Penning AJ (1996) Meniscal replacement using a porous polymer prosthesis: a preliminary study in the dog. Biomaterials 17:1169–1175
Stone KR, Rodkey WG, Webber R, McKinney L, Steadman JR (1992) Meniscal regeneration with copolymeric collagen scaffolds. In vitro and in vivo studies evaluated clinically, histologically, and biochemically. Am J Sports Med 20:104–111
Steadman JR, Rodkey WG (2005) Tissue-engineered collagen meniscus implants: 5- to 6-year feasibility study results. Arthroscopy 21(5):515–525
Van Arkel ERA, De Boer HH (1995) Human meniscal transplantation: preliminary results at 2 to 5-year follow-up. J Bone Joint Surg Br 77:589–595
Carter TR (1999) Meniscal allograft transplantation. Sports Med Arthrosc Rev 7:51–62
Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D (2002) Long-term results of meniscal allograft transplantation. Am J Sports Med 30:174–181
Ryu RK, Dunbar VWH, Morse GG (2002) Meniscal allograft replacement: a 1-year to 6-year experience. Arthroscopy 18:989–994
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lubowitz, J.H., Verdonk, P.C.M., Reid , J.B. et al. Meniscus allograft transplantation: a current concepts review. Knee Surg Sports Traumatol Arthrosc 15, 476–492 (2007). https://doi.org/10.1007/s00167-006-0216-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0216-5