Abstract
This chapter summarizes data in the current literature regarding return to sports (RTS) after patellofemoral realignment surgery from 52 studies encompassing 1892 patients. There were 1408 patients in 36 studies that underwent medial patellofemoral ligament (MPFL) reconstruction or repair and 484 patients in 16 studies that underwent a variety of patellar proximal and/or distal realignment procedures that did not involve MPFL reconstruction or repair (such as Fulkerson and Elmslie-Trillat). Following MPFL reconstruction, a mean of 70% of patients returned to preinjury sports activity levels, a mean of 83% returned to any sport, and the approximate mean postoperative Tegner score was 5.2 points. After other proximal/distal procedures, the mean values for return to preinjury sports (provided in only 5 studies) ranged from 22% to 97% and the mean postoperative Tegner score was 4.1 points. The mean time patients were usually allowed to RTS was provided in 28 studies and varied from 3 to 9 months postoperatively. Almost no objective criteria were provided to determine when patients could be safely released to either sports-specific training or unrestricted athletic activities. The failure rates were <10% in the majority of studies. The Cincinnati Sports Medicine and Orthopedic Center postoperative rehabilitation program and return to sport criteria are provided.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Patellofemoral surgery and sports
- Proximal-distal realignment
- MPFL reconstruction
- Patellofemoral rehabilitation
1 Introduction
Injuries and disorders of the patellofemoral joint are some of the most common causes of knee pain and frequently include inflammation of the parapatellar soft tissues, damage to the articular cartilage of the patella and/or femoral sulcus, and instability (subluxation or dislocation) [1]. The terminology used to describe patellofemoral disorders can be confusing. Patellar malalignment is a translational or rotational deviation of the patella relative to any axis caused by an abnormal relationship between the patella, the soft tissues surrounding the patella, and the femoral and tibial osseous structures. The abnormalities may be caused by congenital issues, such as peripatellar tissue tightness or laxity, a shallow or convex trochlear groove, bony abnormalities of the patella, rotational malalignment of the femur and tibia, patella alta, or patella baja, and may be exacerbated by inflexibility or weakness of the lower extremity musculature. Patellar malalignment may also arise from an injury that disrupts soft tissue stabilizers, especially the medial tissues restraints, including the medial patellofemoral ligament (MPFL). Patellar dislocations and patellofemoral instability are common problems in young athletic individuals. In a study that analyzed factors associated with patellar dislocations in 40,544 injured knees in the United States, Waterman et al. [2] reported that 52% of the injuries occurred during athletics. The peak incidence of dislocations occurred between 15 and 19 years of age. Redislocation rates of first-time patella dislocations treated conservatively range from 36% to 71% in pediatric populations [3, 4] and from 14% to 57% in adult populations [5, 6].
While many patients who sustain patellar dislocations may be successfully treated with conservative measures, surgery is required to prevent recurrent dislocations and the subsequent patellofemoral cartilage damage that occurs. Patients with distinct anatomical abnormalities described in detail elsewhere are more likely to undergo repetitive dislocations unless there is surgical intervention. Many surgical procedures have been described for realignment or stabilization of the patellofemoral mechanism including proximal realignment, distal realignment, or a combination of both (Fig. 28.1). Proximal realignment procedures alter the medial-lateral position of the patella through balancing of soft tissue restraints proximal to its inferior pole and include MPFL repair or reconstruction (Fig. 28.2), medial retinacular capsular and medial patellomeniscal plication, vastus medialis obliquus advancement, and lateral retinacular release. Distal realignment procedures modify the medial-lateral, anterior-posterior, rotations, and proximal-distal positions of the patella by transfer of the tibial tubercle. Included in this category are anterior (Maquet [7]), medial (Elmslie-Trillat [8]), and anteromedial (Fulkerson [9]) transfer of the tibial tubercle. Literally, hundreds of articles have been written on these operative procedures regarding their indications, technique, and clinical outcomes [4, 10,11,12,13,14,15,16,17,18,19,20]. However, information regarding the ability of patients to return to sports (RTS) and previous activity levels after these operations is more difficult to determine and, as of the time of writing, no formal systematic review had been conducted on this topic.
Proximal-distal realignment procedure. (a) The medial retinaculum and vastus medialis obliquus 2 cm above the patella are advanced in line of their insertions to restore patellar stability. (b) The millimeters of tibial tubercle medial displacement requires are measured at surgery. (c) A dovetail tibial tubercle osteotomy has been performed, maintaining the distal and medial soft tissues. (d) Postoperative radiograph (From Noyes and Barber-Westin [1])
Medial patellofemoral ligament (MPFL) reconstruction with quadriceps tendon. (a) A medial full-thickness quadriceps tendon graft, 60 mm × 8 mm wide (measured to the superior edge of the patella) is harvested with the patellar attachment retained. In some knees, a partial-thickness autograft provides a suitably sized graft. Two to 3 mm of the remaining quadriceps tendon is left attached to the vastus medialis obliquus (VMO) for later closure. (b) Dissection deep to the medial retinaculum and above synovial pouch and MPFL, medial patellomeniscal ligament (MPML). (c) Puncture of the medial retinaculum, posterior to the medial femoral epicondyle at the native MPFL attachment just anterior to the adductor tendon, with the passage of graft beneath the retinaculum. Setting of the normal tension of the medial soft tissues. (d) Imbrication of the VMO, medial retinaculum, MPFL, and MPML. (e) Suturing of the quadriceps graft to the MPFL native femoral attachment, with a backup suture to the adductor tendon. The graft and medial tissues are not overtensioned and should allow a normal lateral translation (glide) of 25% patellar width (From Noyes and Barber-Westin [1])
Few detailed postoperative rehabilitation guidelines specific for RTS after patellofemoral realignment operations are available. In 2018, Zaman et al. [21] reviewed 53 studies to determine criteria for RTS after MPFL reconstruction. The authors reported that although 35 studies (66%) provided an expected timeline for RTS, only eight included objective criteria in the rehabilitation protocol, such as sufficient quadriceps or general muscle strength, range of motion (ROM), and patellar stability. However, none of the eight studies provided numerical values for these criteria. Fisher et al. [18] reviewed the literature to determine the ability of an MPFL reconstruction to return patients to sports activities. Of 21 studies included in the investigation, only six provided sports activity level ratings (Tegner scores) and the authors concluded that there was very limited RTS information available.
Menetrey et al. [22] reviewed the literature to devise a RTS protocol after patellar dislocation or surgery for patellofemoral instability. These authors also concluded that available evidence regarding the functional capacity of patients, including rehabilitation and testing protocols, that allowed for a safe RTS was sparse. They provided the following criteria from a consensus meeting from the ISAKOS Sports Medicine Committee held in 2013 on RTS after patellofemoral instability: (1) postoperative complete radiographic healing of bone, (2) no knee pain, effusion, or instability, (3) full or nearly full ROM, (4) completion of neuromuscular training and proprioception, (5) satisfactory core strength and endurance, (6) acceptable dynamic control (Star Excursion Balance Test, SEBT), (7) limb symmetry index >85% on hop tests, (8) adequate performance with physiotherapist during sport-specific drills simulating the intensity and movement patterns of the athlete’s sport, and (9) psychological readiness to RTS (Single Assessment Numerical Evaluation [SANE] score > 80/100). The authors recommended consideration of several videotaped tests to determine dynamic control, including the single-leg squat, the drop-jump, the side-hop, and the SEBT.
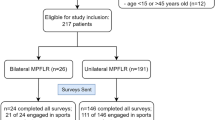
We have published elsewhere a complete description of the management of active patients with patellofemoral malalignment and instability, including a review of the biomechanics of patellofemoral restraints, indications, and contraindications for surgery, and postoperative management [1]. This chapter summarizes data from 52 studies regarding RTS after MPFL reconstruction and proximal/distal realignment procedures that did not involve MPFL reconstruction (Table 28.1). Data regarding return to preinjury sport and return to any type of sport, as well as Tegner activity scores and failure rates are provided. An analysis of the postoperative rehabilitation criteria for RTS described by each study is presented. Our postoperative rehabilitation protocol is detailed, along with our criteria to initiate sports training and for final RTS release.
2 Return to Sport After MPFL Reconstruction
Our review located 36 studies that provided RTS percentages (Table 28.2) and/or Tegner activity scores (Table 28.3) after MPFL reconstruction in 1408 patients [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. The mean age was approximately 22.8 years (range, 10.3–56) and the gender breakdown, provided in 31 studies, was 717 females and 481 males. The mean follow-up was 3.2 years (range, 0.3–13 years).
The MPFL was reconstructed in all patients in 30 studies and hamstring tendon autografts were used in the majority (23 studies). MPFL reconstruction or repair was selected based on indications in one investigation [38] or in a randomized trial design in two studies [46, 52]. MPFL suture repair was used in acute ruptures in two studies [26, 28] and for chronic recurrent dislocations in one [29]. Associated procedures were described in 12 studies, with the most common including tibial tuberosity transfer, lateral release, and trochleoplasty.
Return to preinjury sports activity levels, provided in 14 studies encompassing 387 patients, averaged 70% (range, 22–100%, Fig. 28.3). Data regarding return to any sport, found in 15 studies, averaged 83% (range, 43–100%). The mean postoperative Tegner score, calculated from 29 studies (Fig. 28.4), was 5.2 points.
The mean time patients were usually allowed to RTS was found in 21 studies (Table 28.4). Almost no criteria were provided to determine when patients could be released safely to either sports-specific training or unrestricted activities. Carnesecchi et al. [23] allowed RTS “depending on the analytical and functional recovery” of the patient. Drez et al. [25] allowed RTS when full ROM and normal quadriceps strength had been achieved. Tompkins et al. [38] released patients to full sports once they passed a “functional assessment”; however, no information regarding tests used or passing criteria was provided.
Ambrozic et al. [35] described sports activity levels in 29 patients (14 females, 15 males, mean age, 26.2 years) who underwent isolated MPFL gracilis autograft reconstruction for recurrent dislocation. RTS was permitted 6 months postoperatively. Twenty-six patients were active in sports before surgery and three never participated. An average of 6.4 years postoperatively, 23 patients had RTS, with 16 obtaining their preinjury level. The most common sports patients returned to were soccer, cycling, and skiing. There were no complications or failures.
Lippacher et al. [28] also focused on the ability of a MPFL reconstruction to return patients to sports activities. These authors followed 68 patients (44 females, 24 males, mean age, 18.3 years) a mean of 2 years postoperatively. Sixty-two patients participated in sports before surgery and all were able to return; 53% at the same or higher level and 47% at lower levels. Common sports patients returned to included soccer, volleyball/handball, cycling, and swimming. Recurrent dislocations occurred in two patients and five patients had 1–2 episodes of subluxation. All of these individuals underwent further rehabilitation and none required revision surgery.
3 Return to Sport After Patellar Realignment Procedures
We found 16 studies that provided RTS data after patellar realignment procedures (that did not include MPFL repair or reconstruction) in 484 patients [39, 58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. The mean age was approximately 22.2 (range, 5–56) and the gender numbers, provided in 13 studies, were 264 females and 116 males. The mean follow-up was approximately 7 years (range, 0.5–46 years). The operative procedures included Elmslie-Trillat in four studies, Elmslie-Trillat-Roux in two studies, Fulkerson in two studies, Roux-Goldthwait in one study, Grammont in one study, and a variety of procedures offered in six studies. Associated procedures were described in nine studies and most frequently included lateral release. Trochleoplasty was done in two studies in select patients.
Return to preinjury sports activity levels was provided in only five studies involving 173 patients (Table 28.5). Percentages ranged from 22% to 97%. Postoperative Tegner activity scores were found in 13 studies (Table 28.6) and averaged 4.1 points (Fig. 28.5).
The mean time patients were usually allowed to RTS was provided in seven studies (Table 28.4). Criteria for RTS was sparse. Tjoumakaris et al. [71] required “adequate” quadriceps strength and ROM. Luhmann et al. [67], in a study involving 27 children (aged 8.8–18.3 years), cited adequate radiographic healing, knee ROM, and near normal leg strength as criteria. Barber and McGarry [59] had similar requirements for RTS.
Liu et al. [66] specifically analyzed RTS after a Fulkerson tibial tubercle anteromedialization for a primary diagnosis of patellofemoral pain or osteoarthritis. A total of 57 patients (48 females, 9 males, mean age, 29.6 years) were followed a mean of 4.6 years postoperatively. Patients were typically allowed to RTS between 6 and 8 months but had to demonstrate “quality movement strategies on a sports-specific return-to-play assessment” similar to the authors’ anterior cruciate ligament patients. Contact sports involving extensive cutting and/or pivoting were prohibited until 9 months postoperatively. Overall, 70% returned to any sport and 54% returned to preinjury levels. The authors noted that 48 patients had participated in sports within 3 years of surgery and of these, 40 were able to return to at least one sport after surgery. Activities most commonly resumed included weightlifting, cycling, soccer, running, and yoga. There was no correlation between age, number of prior surgical procedures, smoking status, patellar Outerbridge grade, or the presence of trochlear lesions and the ability to RTS. There were no failures, although 47% had chronic pain and only 58% felt their knee was normal during sports.
Tjoumakaris et al. [71] followed 34 athletes (30 females, 4 males, mean age, 20 years) who underwent a Fulkerson procedure for a primary diagnosis of recurrent patellar instability. There were 14 high school, 12 collegiate, and 8 recreational athletes. Patients were allowed to RTS by 4–5 months after surgery if “adequate quadriceps strength and ROM” had been achieved. At follow-up, a mean of 3.8 years postoperatively, 97% had returned to their preinjury sport. The authors did not provide data related to any problems patients may have experienced while participating. The one patient who failed and had recurrent instability tested positive for Ehlers–Danlos syndrome.
4 Failure Rates
Twenty-three studies of MPFL reconstruction or repair reported no failures or recurrent dislocations resulting in the need for further surgery (Fig. 28.6). Hopper et al. [37] reported that all seven patients who had severe trochlear dysplasia (Dejour classification C and D) failed, suffering recurrent dislocations, compared with 7.4% of 54 patients with mild dysplasia. Xie et al. [40] found that patients in whom a semitendinosus MPFL reconstruction was augmented with polyester suture (n = 42) had a recurrent dislocation rate of just 2.4% compared with 23.3% of patients who did not have suture augmentation (n = 43). Zhao et al. [46] in a level 2 randomized study reported postoperative rates of redislocation and/or multiple episodes of instability of 9% after MPFL reconstruction (n = 45, mean age 25.0 ± 6.6) and 26% after medial retinaculum plication (n = 43, mean age 23.9 ± 5.8). At the 5-year follow-up, patients in the MPFL-reconstructed group had a significantly higher mean Tegner score (5.7 ± 1.7 and 4.0 ± 1.4, respectively; P < 0.001).
Four studies involving other proximal and/or distal procedures reported no failures or recurrent dislocations resulting in the need for further surgery. Sillanpaa et al. [5] reported that 14% of 21 knees failed after a Roux-Goldthwait procedure. Vivod et al. [72] followed 54 patients a mean of 22.5 years postoperatively and reported failures (recurrent dislocations) in 36% after isolated proximal realignment, 32% after proximal-distal realignment, and 20% after isolated distal realignment. Kreuz et al. [65] followed three surgical groups in a nonrandomized study an average of 6.3 years postoperatively and found recurrent dislocations in 31% after isolated Green proximal realignment, in 29% after Green proximal and Roux-Goldthwait distal realignment, and in 12.5% after a combined proximal realignment and tubercle transfer (P < 0.05).
5 Advances in Operative Techniques for RTS
The RTS data summarized in this chapter reflect, for the most part, studies that failed to include modern objective testing of knee function, including strength and agility, as well as postoperative advanced neuromuscular retraining that is now recognized as vitally important after ACL surgery. Recent literature has demonstrated changes in surgical procedures recommended to correct patellofemoral instability that allows earlier restoration of ROM and muscle strength. These continued advances in both surgery and rehabilitation should, we believe, result in improved RTS data and lower failure rates. These include the following:
-
1.
A better appreciation of the role of trochlear dysplasia which, when present, indicates a lack of a normal trochlear groove to provide patella stability and control patellar kinematics. Patients with trochlear dysplasia have a higher failure rate and rely to a greater extent on soft tissue ligament restraints and muscle control mechanisms. This also applies to patella alta cases, in which tibial tubercle distalization is required to position the patella within a normal patellar-trochlear relationship.
-
2.
An understanding of the role of the MPFL in conjunction with other medial retinacular restraints (medial patellar meniscal and tibia restraints). MPFL surgery must restore a checkrein for abnormal lateral patellar translation, particularly from 0° to 20° of knee motion. The femoral attachment of the MPFL graft requires careful positioning from a proximal-to-distal direction to function at low knee flexion angles and avoid overtightening with knee flexion.
-
3.
The indications for distal tibial tubercle medialization or elevation are now highly select and many knees do not require these procedures.
-
4.
Proximal realignment procedures require early knee motion exercises to prevent abnormal scarring and disuse effects. For example, we reported that immediate ROM from 0° to 90° and full weight-bearing in extension is possible and encouraged immediately after surgery [73]. Previous rehabilitation protocols may have been overprotective regarding the allowance of immediate motion and weight-bearing.
-
5.
Proximal MPFL grafts placed into the patella through drills holes risk patellar fracture. Docking of the graft at adjacent patella soft tissues avoids this complication. In the MPFL quadriceps turndown procedure advocated by the authors (Fig. 28.2) [1], the attachment of the quadriceps graft is performed entirely by soft tissue sutures at both the patella and femoral anatomic attachment sites, thereby avoiding the necessity for rigid fixation implants and their potential complications.
6 Postoperative Rehabilitation Concepts
Our postoperative rehabilitation protocol is summarized in Table 28.7. This protocol is used in patients undergoing proximal and distal extensor mechanism realignment procedures, with or without MPFL reconstruction. Patients are placed into a postoperative long-leg brace for the first 4 weeks. ROM exercises and patellar mobilization in superior-inferior and medial-lateral directions are begun immediately after surgery to prevent parapatellar contractures. The goal for the first week is to obtain 0–90° of motion. Knee flexion is gradually increased to 110° by the fourth week and then a full motion of at least 135° is allowed by the eighth week. This limitation of flexion in the first 4 weeks is designed to protect the suture lines and the repair when a proximal realignment procedure is performed. The therapist should be aware of the potential for a knee motion complication and, if 0–110° is not obtained by the end of the fourth week, the patient should undergo a local anesthetic nerve block or a gentle ranging of motion under anesthesia as previously discussed. The early treatment and avoidance of an arthrofibrotic response to surgery are critical in these cases.
After isolated MPFL reconstruction, patients are allowed to bear 100% of their body weight with the knee at full extension using crutches for support. For patients who undergo a concurrent tibial tubercle medialization procedure, 50% weight-bearing is used for 2 weeks for protection and full weight-bearing is allowed by the fourth week.
Radiographs are taken the first and the fourth postoperative weeks to ensure adequate position and healing of the osteotomy. Weight-bearing may be delayed if problems are detected in bony healing or in quadriceps control. Flexibility exercises including stretching of hamstrings, gastrocnemius-soleus, quadriceps and iliotibial band are started the first week. The strengthening program for the quadriceps mechanism is begun during the first week and gradually progressed. Straight leg raises are allowed immediately after isolated MPFL reconstruction and at the fourth week after concurrent tibial tubercle procedures. Open kinetic chain exercises are begun immediately after isolated MPFL reconstruction but are delayed until the fourth to sixth week after concurrent tibial tubercle procedures at which time the osteotomy is usually healed.
Unfortunately, the majority of patients that undergo the operative procedures described in this chapter have marked joint deterioration from chronic patellofemoral malalignment or recurrent dislocation/subluxation episodes. In these patients, the goal of surgery is to return to light, low-impact activities only. In select patients (without articular cartilage damage) wishing to resume more strenuous activities, sports training is begun with a running program when the patient demonstrates at least 70% of the strength of the noninvolved limb for quadriceps and hamstrings on isometric testing, is at least 3 months postoperative, has normal patellar stability and tracking, and has no pain or joint effusion. Our running program is described in detail in Chap. 14. The program includes agility drills, cutting, and sharp directional change movement patterns. In select patients wishing to resume sports involving pivoting and cutting, a basic plyometric training program may be initiated upon completion of the running and agility program (see also Chap. 14). Final release to unrestricted sports is based on successful completion of training and achievement of normal indices shown in Table 28.8. Testing includes quadriceps and hamstrings isokinetic [78,79,80,81,82,83,84,85,86,87,88], isometric [89,90,91], or 1-repetition maximum bench press and leg press [92, 93]; two single-leg hops [74, 78, 80, 81, 94,95,96,97]; video drop-jump [75, 98,99,100], single-leg squat [101,102,103,104], and plant and cut [77, 105,106,107] tests. Other tests to consider before the patient is released to unrestricted athletic activities include the multi-stage fitness test to estimate VO2max [108] and the 60-s sit-up test or other core strength measures [109].
A trial of function is encouraged in which the patient is monitored for knee swelling, pain, overuse symptoms, and instability episodes. Upon successful return to activity, the patient is encouraged to continue with a maintenance program. During the in-season, a conditioning program of two workouts a week is recommended. In the off-season or preseason, this program should be performed three times a week to maximize gains in flexibility, strength, and cardiovascular endurance.
References
Noyes FR, Barber-Westin SD. Operative options for extensor mechanism malalignment and patellar dislocation. In: Noyes FR, Barber-Westin SD, editors. Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes. 2nd ed. Philadelphia, PA: Elsevier; 2017. p. 970–1013. https://doi.org/10.1016/b978-0-323-32903-3.00035-4.
Waterman BR, Belmont PJ Jr, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25(1):51–7.
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–70.
Hennrikus W, Pylawka T. Patellofemoral instability in skeletally immature athletes. Instr Course Lect. 2013;62:445–53.
Sillanpaa P, Mattila VM, Iivonen T, Visuri T, Pihlajamaki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–11.
Smith TO, Davies L, Chester R, Clark A, Donell ST. Clinical outcomes of rehabilitation for patients following lateral patellar dislocation: a systematic review. Physiotherapy. 2010;96(4):269–81. https://doi.org/10.1016/j.physio.2010.02.006.
Maquet P. Valgus osteotomy for osteoarthritis of the knee. Clin Orthop Relat Res. 1976;120:143–8.
Trillat A, Dejour H, Couette A. Diagnosis and treatment of recurrent dislocations of the Patella. Rev Chir Orthop Reparatrice Appar Mot. 1964;50:813–24.
Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18(5):490–6; discussion 496-497
Sanchis-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg. 2014;22(3):175–82. https://doi.org/10.5435/JAAOS-22-03-175.
Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30(8):1018–25. https://doi.org/10.1016/j.arthro.2014.02.044.
Buckens CF, Saris DB. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med. 2010;38(1):181–8. https://doi.org/10.1177/0363546509353132.
Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007;35(3):484–92. https://doi.org/10.1177/0363546507299237.
Amis AA. Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc. 2007;15(2):48–56.
Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM. Surgical biomechanics of the patellofemoral joint. Arthroscopy. 2007;23(5):542–53.
Mihalko WM, Boachie-Adjei Y, Spang JT, Fulkerson JP, Arendt EA, Saleh KJ. Controversies and techniques in the surgical management of patellofemoral arthritis. Instr Course Lect. 2008;57:365–80.
Smith TO, Walker J, Russell N. Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2007;15(11):1301–14.
Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384–94. https://doi.org/10.1016/j.arthro.2010.04.005.
Singhal R, Rogers S, Charalambous CP. Double-bundle medial patellofemoral ligament reconstruction with hamstring tendon autograft and mediolateral patellar tunnel fixation: a meta-analysis of outcomes and complications. Bone Joint J. 2013;95-B(7):900–5. https://doi.org/10.1302/0301-620X.95B7.31417.
Vavken P, Wimmer MD, Camathias C, Quidde J, Valderrabano V, Pagenstert G. Treating patella instability in skeletally immature patients. Arthroscopy. 2013;29(8):1410–22. https://doi.org/10.1016/j.arthro.2013.03.075.
Zaman S, White A, Shi WJ, Freedman KB, Dodson CC. Return-to-play guidelines after medial patellofemoral ligament surgery for recurrent patellar instability: a systematic review. Am J Sports Med. 2018;46(10):2530–9. https://doi.org/10.1177/0363546517713663.
Menetrey J, Putman S, Gard S. Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2320–6. https://doi.org/10.1007/s00167-014-3172-5.
Carnesecchi O, Philippot R, Boyer B, Farizon F, Edouard P. Recovery of gait pattern after medial patellofemoral ligament reconstruction for objective patellar instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):123–8. https://doi.org/10.1007/s00167-014-3347-0.
Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58–63. https://doi.org/10.1177/0363546512463683.
Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298–306.
Nelitz M, Dreyhaupt J, Lippacher S. Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med. 2013;41(5):1005–12. https://doi.org/10.1177/0363546513478579.
Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647–55. https://doi.org/10.1177/0363546511420079.
Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: clinical outcomes and return to sports. Am J Sports Med. 2014;42(7):1661–8. https://doi.org/10.1177/0363546514529640.
Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38(11):2248–54. https://doi.org/10.1177/0363546510376230.
Ahmad CS, Stein BE, Matuz D, Henry JH. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation. A review of eight cases. Am J Sports Med. 2000;28(6):804–10.
Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37(9):1735–42. https://doi.org/10.1177/0363546509333482.
Mariani PP, Liguori L, Cerullo G, Iannella G, Floris L. Arthroscopic patellar reinsertion of the MPFL in acute patellar dislocations. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):628–33. https://doi.org/10.1007/s00167-010-1315-x.
Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2470–6. https://doi.org/10.1007/s00167-014-3132-0.
Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):318–24. https://doi.org/10.1007/s00167-012-2015-5.
Ambrozic B, Novak S. The influence of medial patellofemoral ligament reconstruction on clinical results and sports activity level. Phys Sportsmed. 2016;44(2):133–40. https://doi.org/10.1080/00913847.2016.1148561.
Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD. Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Joint Surg. 2012;94(9):1202–8. https://doi.org/10.1302/0301-620X.94B9.28738.
Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42(3):716–22. https://doi.org/10.1177/0363546513518413.
Tompkins M, Kuenze CM, Diduch DR, Miller MD, Milewski MD, Hart JP. Clinical and functional outcomes following primary repair versus reconstruction of the medial patellofemoral ligament for recurrent patellar instability. J Sports Med (Hindawi Publ Corp). 2014;2014:702358. https://doi.org/10.1155/2014/702358.
Lim AK, Chang HC, Hui JH. Recurrent patellar dislocation: reappraising our approach to surgery. Ann Acad Med Singap. 2008;37(4):320–3.
Xie G, Zhao J, Huangfu X, He Y. Medial patellofemoral ligament reconstruction using semitendinosus tendons: polyester suture augmentation versus nonaugmentation. Am J Sports Med. 2012;40(6):1365–74. https://doi.org/10.1177/0363546512441324.
Blond L, Haugegaard M. Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2484–90. https://doi.org/10.1007/s00167-013-2422-2.
Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K, Imhoff AB, Schottle PB. Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2591–8. https://doi.org/10.1007/s00167-013-2603-z.
Li J, Li Y, Wei J, Wang J, Gao S, Shen Y. A simple technique for reconstruction of medial patellofemoral ligament with bone-fascia tunnel fixation at the medial margin of the patella: a 6-year-minimum follow-up study. J Orthop Surg Res. 2014;9:66. https://doi.org/10.1186/s13018-014-0066-7.
Berruto M, Ferrua P, Uboldi F, Usellini E, Gala L, Tassi A, Marelli B. Medial patellofemoral ligament reconstruction with bioactive synthetic ligament is an option. A 3-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2419–25. https://doi.org/10.1007/s00167-014-2970-0.
Calanna F, Pulici L, Carimati G, Quaglia A, Volpi P. Medial patello-femoral ligament (MPFL) reconstruction using suture anchors fixation: preliminary results. Muscles Ligaments Tendons J. 2016;6(1):64–70. https://doi.org/10.11138/mltj/2016.6.1.064.
Zhao J, Huangfu X, He Y. The role of medial retinaculum plication versus medial patellofemoral ligament reconstruction in combined procedures for recurrent patellar instability in adults. Am J Sports Med. 2012;40(6):1355–64. https://doi.org/10.1177/0363546512439193.
Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37(10):2021–7. https://doi.org/10.1177/0363546509336261.
Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27(2):139–46. https://doi.org/10.1055/s-0033-1360652.
Becher C, Kley K, Lobenhoffer P, Ezechieli M, Smith T, Ostermeier S. Dynamic versus static reconstruction of the medial patellofemoral ligament for recurrent lateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2452–7. https://doi.org/10.1007/s00167-014-3020-7.
Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–61.
Hinterwimmer S, Imhoff AB, Minzlaff P, Saier T, Rosenstiel N, Hawe W, Feucht MJ. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2147–54. https://doi.org/10.1007/s00167-013-2498-8.
Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy. 2013;29(5):891–7. https://doi.org/10.1016/j.arthro.2013.01.030.
Song SY, Kim IS, Chang HG, Shin JH, Kim HJ, Seo YJ. Anatomic medial patellofemoral ligament reconstruction using patellar suture anchor fixation for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2431–7. https://doi.org/10.1007/s00167-013-2730-6.
Kohn LM, Meidinger G, Beitzel K, Banke IJ, Hensler D, Imhoff AB, Schottle PB. Isolated and combined medial patellofemoral ligament reconstruction in revision surgery for patellofemoral instability: a prospective study. Am J Sports Med. 2013;41(9):2128–35. https://doi.org/10.1177/0363546513498572.
Suganuma J, Mochizuki R, Sugiki T, Inoue Y, Kitamura K, Akutsu S, Ono H. Reconstruction of the medial patellofemoral ligament using a synthetic graft with arthroscopic control of patellofemoral congruence. Arthroscopy. 2016;32(11):2259–68. https://doi.org/10.1016/j.arthro.2016.02.004.
Matthews JJ, Schranz P. Reconstruction of the medial patellofemoral ligament using a longitudinal patellar tunnel technique. Int Orthop. 2010;34(8):1321–5. https://doi.org/10.1007/s00264-009-0918-7.
Christiansen SE, Jacobsen BW, Lund B, Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–7.
Sillanpaa P, Mattila VM, Visuri T, Maenpaa H, Pihlajamaki H. Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res. 2008;466(6):1475–84. https://doi.org/10.1007/s11999-008-0207-6.
Barber FA, McGarry JE. Elmslie-Trillat procedure for the treatment of recurrent patellar instability. Arthroscopy. 2008;24(1):77–81.
Berruto M, Uboldi FM, Ferrua P, Vergottini G, Manunta A. Surgical treatment of objective patellar instability: long-term results. Joints. 2018;6(1):33–6. https://doi.org/10.1055/s-0038-1636949.
Carney JR, Mologne TS, Muldoon M, Cox JS. Long-term evaluation of the Roux-Elmslie-Trillat procedure for patellar instability: a 26-year follow-up. Am J Sports Med. 2005;33(8):1220–3. https://doi.org/10.1177/0363546504272686.
Endres S, Wilke A. A 10 year follow-up study after roux-elmslie-Trillat treatment for cases of patellar instability. BMC Musculoskelet Disord. 2011;12:48. https://doi.org/10.1186/1471-2474-12-48.
Karataglis D, Green MA, Learmonth DJ. Functional outcome following modified elmslie-Trillat procedure. Knee. 2006;13(6):464–8. https://doi.org/10.1016/j.knee.2006.08.004.
Kraus T, Lidder S, Svehlik M, Rippel K, Schneider F, Eberl R, Linhart W. Patella re-alignment in children with a modified Grammont technique. Acta Orthop. 2012;83(5):504–10. https://doi.org/10.3109/17453674.2012.736168.
Kreuz PC, Peterson L, van der Werf-Grohmann N, Vohrer M, Schwering L. Clinical and electromyographic results of proximal and distal realignment procedures in young patients with recurrent patellar dislocations. Am J Sports Med. 2013;41(7):1621–8. https://doi.org/10.1177/0363546513488869.
Liu JN, Wu HH, Garcia GH, Kalbian IL, Strickland SM, Shubin Stein BE. Return to sports after tibial tubercle osteotomy for patellofemoral pain and osteoarthritis. Arthroscopy. 2018;34(4):1022–9. https://doi.org/10.1016/j.arthro.2017.09.021.
Luhmann SJ, O’Donnell JC, Fuhrhop S. Outcomes after patellar realignment surgery for recurrent patellar instability dislocations: a minimum 3-year follow-up study of children and adolescents. J Pediatr Orthop. 2011;31(1):65–71. https://doi.org/10.1097/BPO.0b013e318202c42d.
Marcacci M, Zaffagnini S, Lo Presti M, Vascellari A, Iacono F, Russo A. Treatment of chronic patellar dislocation with a modified Elmslie-Trillat procedure. Arch Orthop Trauma Surg. 2004;124(4):250–7. https://doi.org/10.1007/s00402-003-0511-2.
Rillmann P, Dutly A, Kieser C, Berbig R. Modified elmslie-Trillat procedure for instability of the patella. Knee Surg Sports Traumatol Arthrosc. 1998;6(1):31–5. https://doi.org/10.1007/s001670050069.
Sillanpaa PJ, Mattila VM, Maenpaa H, Kiuru M, Visuri T, Pihlajamaki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am. 2009;91(2):263–73. https://doi.org/10.2106/JBJS.G.01449.
Tjoumakaris FP, Forsythe B, Bradley JP. Patellofemoral instability in athletes: treatment via modified Fulkerson osteotomy and lateral release. Am J Sports Med. 2010;38(5):992–9. https://doi.org/10.1177/0363546509357682.
Vivod G, Verdonk P, Drobnic M. Long-term clinical and radiographic outcome of patello-femoral realignment procedures: a minimum of 15-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2747–55. https://doi.org/10.1007/s00167-013-2637-2.
Parikh SN, Albright J, Noyes FR. Proximal and distal extensor mechanism realignment: the surgical technique. Tech Knee Surg. 2006;5:27–38.
Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–8.
Noyes FR, Barber-Westin SD, Fleckenstein C, Walsh C, West J. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. Am J Sports Med. 2005;33(2):197–207.
Ireland ML, Bolgla LA, Noehren B. Gender differences in core strength and lower extremity function during static and dynamic single-leg squat tests. In: Noyes FR, Barber-Westin SD, editors. ACL injuries in the female athlete. Causes, impacts, and conditioning programs. 2nd ed. Berlin Heidelberg, New York: Springer-Verlag; 2018. p. 239–57.
Pollard CD, Sigward SM, Powers CM. Gender differences in hip joint kinematics and kinetics during side-step cutting maneuver. Clin J Sport Med. 2007;17(1):38–42. https://doi.org/10.1097/JSM.0b013e3180305de8.
Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):390–7. https://doi.org/10.1007/s00167-010-1225-y.
Choi NH, Lee JH, Son KM, Victoroff BN. Tibial tunnel widening after anterior cruciate ligament reconstructions with hamstring tendons using rigidfix femoral fixation and intrafix tibial fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):92–7. https://doi.org/10.1007/s00167-009-0951-5.
Landes S, Nyland J, Elmlinger B, Tillett E, Caborn D. Knee flexor strength after ACL reconstruction: comparison between hamstring autograft, tibialis anterior allograft, and non-injured controls. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):317–24. https://doi.org/10.1007/s00167-009-0931-9.
Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–54. https://doi.org/10.2519/jospt.2010.3168.
Isberg J, Faxen E, Brandsson S, Eriksson BI, Karrholm J, Karlsson J. Early active extension after anterior cruciate ligament reconstruction does not result in increased laxity of the knee. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1108–15. https://doi.org/10.1007/s00167-006-0138-2.
Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34(12):1933–40.
Poehling GG, Curl WW, Lee CA, Ginn TA, Rushing JT, Naughton MJ, Holden MB, Martin DF, Smith BP. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: allograft versus autograft. Arthroscopy. 2005;21(7):774–85.
Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med (Auckland, NZ). 2004;34(4):269–80.
Beynnon BD, Johnson RJ, Fleming BC, Kannus P, Kaplan M, Samani J, Renstr m P. Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts: a prospective, randomized study. J Bone Joint Surg Am. 2002;84-A(9):PG-1503-13.
Henriksson M, Rockborn P, Good L. Range of motion training in brace vs. plaster immobilization after anterior cruciate ligament reconstruction: a prospective randomized comparison with a 2-year follow-up. Scand J Med Sci Sports. 2002;12(2):73–80.
Moller E, Forssblad M, Hansson L, Wange P, Weidenhielm L. Bracing versus nonbracing in rehabilitation after anterior cruciate ligament reconstruction: a randomized prospective study with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):102–8.
Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3(5):472–9. https://doi.org/10.1016/j.pmrj.2010.10.025.
Toonstra J, Mattacola CG. Test-retest reliability and validity of isometric knee-flexion and -extension measurement using 3 methods of assessing muscle strength. J Sport Rehabil. 2013;22(7)
Whiteley R, Jacobsen P, Prior S, Skazalski C, Otten R, Johnson A. Correlation of isokinetic and novel hand-held dynamometry measures of knee flexion and extension strength testing. J Sci Med Sport. 2012;15(5):444–50. https://doi.org/10.1016/j.jsams.2012.01.003.
Kraemer WJ, Patton JF, Gordon SE, Harman EA, Deschenes MR, Reynolds K, Newton RU, Triplett NT, Dziados JE. Compatibility of high-intensity strength and endurance training on hormonal and skeletal muscle adaptations. J Appl Physiol. 1995;78(3):976–89.
Reiman MP, Manske RC. Functional testing in human performance. Champaign: Human Kinetics; 2009.
Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990;255(255):204–14.
Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593–601. https://doi.org/10.1016/j.arthro.2010.05.014.
Logerstedt D, Grindem H, Lynch A, Eitzen I, Engebretsen L, Risberg MA, Axe MJ, Snyder-Mackler L. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40(10):2348–56. https://doi.org/10.1177/0363546512457551.
Logerstedt D, Di Stasi S, Grindem H, Lynch A, Eitzen I, Engebretsen L, Risberg MA, Axe MJ, Snyder-Mackler L. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: a Delaware-Oslo ACL cohort study. J Orthop Sports Phys Ther. 2014;44(12):914–23. https://doi.org/10.2519/jospt.2014.4852.
Sigward SM, Havens KL, Powers CM. Knee separation distance and lower extremity kinematics during a drop land: implications for clinical screening. J Athl Train. 2011;46(5):471–5.
Nilstad A, Andersen TE, Kristianslund E, Bahr R, Myklebust G, Steffen K, Krosshaug T. Physiotherapists can identify female football players with high knee valgus angles during vertical drop jumps using real-time observational screening. J Orthop Sports Phys Ther. 2014;44(5):358–65. https://doi.org/10.2519/jospt.2014.4969.
Pollard CD, Sigward SM, Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech (Bristol, Avon). 2010;25(2):142–6. https://doi.org/10.1016/j.clinbiomech.2009.10.005.
Ireland ML, Durbin T, Bolgla LA. Gender differences in core strength and lower extremity function during the single-leg squat test. In: Noyes FR, Barber-Westin SD, editors. ACL injuries in the female athlete: causes, impacts, and conditioning programs. Berlin Heidelberg: Springer-Verlag; 2012. p. 203–19.
Ageberg E, Bennell KL, Hunt MA, Simic M, Roos EM, Creaby MW. Validity and inter-rater reliability of medio-lateral knee motion observed during a single-limb mini squat. BMC Musculoskelet Disord. 2010;11:265. https://doi.org/10.1186/1471-2474-11-265.
Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22(1):41–50.
Ireland ML. The female ACL: why is it more prone to injury? Orthop Clin North Am. 2002;33(4):637–51.
Cortes N, Onate J, Van Lunen B. Pivot task increases knee frontal plane loading compared with sidestep and drop-jump. J Sports Sci. 2011;29(1):83–92. https://doi.org/10.1080/02640414.2010.523087.
Jones PA, Herrington LC, Munro AG, Graham-Smith P. Is there a relationship between landing, cutting, and pivoting tasks in terms of the characteristics of dynamic valgus? Am J Sports Med. 2014;42(9):2095–102. https://doi.org/10.1177/0363546514539446.
Nagano Y, Ida H, Akai M, Fukubayashi T. Biomechanical characteristics of the knee joint in female athletes during tasks associated with anterior cruciate ligament injury. Knee. 2009;16(2):153–8. https://doi.org/10.1016/j.knee.2008.10.012.
Ramsbottom R, Brewer J, Williams C. A progressive shuttle run test to estimate maximal oxygen uptake. Br J Sports Med. 1988;22(4):141–4.
Okada T, Huxel KC, Nesser TW. Relationship between core stability, functional movement, and performance. J Strength Cond Res. 2011;25(1):252–61. https://doi.org/10.1519/JSC.0b013e3181b22b3e.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Noyes, F.R., Barber-Westin, S. (2019). Return to Sport After Patellofemoral Realignment and Stabilization Procedures. In: Noyes, F., Barber-Westin, S. (eds) Return to Sport after ACL Reconstruction and Other Knee Operations. Springer, Cham. https://doi.org/10.1007/978-3-030-22361-8_28
Download citation
DOI: https://doi.org/10.1007/978-3-030-22361-8_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-22360-1
Online ISBN: 978-3-030-22361-8
eBook Packages: MedicineMedicine (R0)