Abstract
Purpose
To compare clinical and radiological outcomes of static and dynamic medial patellofemoral ligament (MPFL) reconstruction techniques.
Methods
In a retrospective, matched-paired, cohort analysis, 30 patients surgically treated for recurrent lateral patellar dislocation were divided into two groups of 15 patients matched for inclusion and exclusion criteria. The static technique group underwent rigid fixation of the gracilis tendon at the anatomic femoral MPFL insertion and the superomedial border of the patella; the dynamic technique group underwent detachment of the gracilis tendon at the pes anserinus with fixation to the proximal medial patellar margin via tunnel transfer obliquely through the patella. Kujala, Lysholm, and Tegner scores; pain level; and pre- and postoperative radiographic changes of patellar height, patellar tilt, and bisect offset were compared.
Results
No significant between-group differences were found in mean Kujala, Tegner, Lysholm, or visual analogue scale scores or radiographic parameters. One case of resubluxation was observed in the dynamic group. All but one patient in each group would have been willing to undergo the procedure again.
Conclusions
Both techniques provided satisfactory short-term outcomes.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patellar instability is often multifactorial, with osseous and soft tissue abnormalities leading to recurrent lateral dislocations. Patients without severe osseous abnormalities who are prone to dislocations within the first 30 degrees of flexion are usually candidates for repair of medial soft tissue constraints [4].
Because the medial patellofemoral ligament (MPFL) is the primary passive restraint to lateral patellar translation at 0–30 degrees of knee flexion [5, 15], reconstruction of the MPFL has become a popular treatment option for recurrent lateral patellar dislocations. Various techniques have been described in the literature, with differences among the techniques including choice of graft, graft fixation and tension, and static versus dynamic reconstruction [6, 11–13, 17, 22, 24, 29, 34, 35]. Reconstruction of the MPFL with a static, anatomic, double-bundle, gracilis tendon has evolved as a reliable treatment option [17, 29, 32]. However, because the graft is stronger and stiffer than the native MPFL [1], malpositioning and over-tensioning of the graft may result in increased retropatellar forces, and an increased medial tilt moment may lead to degeneration of the patellofemoral joint [1, 9, 33]. Dynamic MPFL reconstruction has been proposed as an alternative to static reconstruction [6, 24, 26]. The first description of a dynamic reconstruction technique dates to 1904, when Lanz described detaching the gracilis tendon at its insertion at the pes anserinus and fixing it to the medial patella with sutures after tunnelling the tendon through the medial capsule [19]. A possible drawback is that the reconstruction is non-anatomic; however, the major theoretical advantages include protection against malpositioning and over-tensioning the graft.
There has been only one matched-paired study comparing static and dynamic reconstruction techniques, in which either adductor magnus rigid or semitendinosus tendon dynamic femoral fixation was used for reconstruction of the MPFL in two groups of 12 patients [12]. The findings suggested that a more dynamic femoral fixation had advantages over the rigid alternative, although statistically significant differences were not found.
The purpose of this analysis was to compare the clinical and radiological outcomes of static versus dynamic MPFL reconstruction, hypothesizing more favourable outcomes for dynamic reconstruction.
Materials and methods
The databases of two hospitals were used to identify patients who had undergone reconstruction of the MPFL using either static or dynamic reconstruction for the treatment of recurrent lateral patellar dislocations. The patients were divided into two similar groups, matched according to the variables listed in Table 1. Preoperative magnetic resonance imaging (MRI) or computed tomography (CT) scan and radiographs, surgical reports, and patient files were available for all patients. Inclusion criteria were isolated reconstruction of the MPFL, age >16 years, and a minimum of two lateral patellar dislocations. Exclusion criteria were Dejour type D trochlear dysplasia [7], Caton-Deschamps index >1.3 measured on a lateral non-weight-bearing radiograph [2], tibial tubercle–trochlear groove distance >20 mm measured on a preoperative CT scan or MRI [8, 28], frontal plane malalignment >7° measured on a long leg standing weight-bearing X-ray (if clinically suspected), a Q-angle >15°, cartilage defects > Outerbridge grade III as determined from the operative report [8, 25], arthritis > Iwano stage 2 determined from preoperative X-rays [16], instability of the cruciate or collateral ligaments, body mass index >35 kg/m2, and known significant musculoskeletal disease.
Surgical technique and postoperative protocol
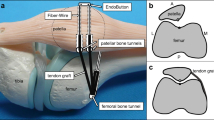
Static reconstruction of the MPFL (Fig. 1)
Static reconstruction was performed according to the description of Schoettle et al. [31]. Briefly, the gracilis tendon is harvested, and both ends are whip-stitched with an absorbable braided suture. After performing a skin incision from the superomedial corner to the end of the medial margin of the patella, the central part of the vastus medialis obliquus (VMO) is identified and scissors used to cut down to the medial femoral epicondyle between the VMO and the joint capsule. The bony insertion of the MPFL is prepared, and a 2-cm bony rim is created. The tendon is embedded in the rim after placing two suture anchors at the proximal and the distal ends of the rim and fixed to the anchors under slight tension with non-resorbable sutures. After performing another skin incision in the area of the medial epicondyle and the adductor tubercle, the medial epicondyle and the adductor tubercle are palpated and a guide wire with an eyelet is placed slightly posterior to the midpoint of these two points under image intensification on a straight lateral view. A drill hole is created up to the contralateral cortex. The free tendon ends are pulled between the prepared second and third layers to the femoral insertion site and pulled into the femoral tunnel. Fixation of the graft is performed using a biodegradable interference screw with the knee in 30 degrees of flexion.
Illustration of the static reconstruction technique according to Schoettle et al. [29]. The graft is attached by two suture anchors at the superomedial border of the patella and tendon-to-bone tunnel fixation with an interference screw at the adductor tubercle
Dynamic reconstruction of the MPFL (Fig. 2)
The technique was performed according to the description by Ostermeier et al. [24]. Briefly, the gracilis tendon is detached at its insertion at the pes anserinus after opening the sartorius fascia. Instead of transferring the tendon through a subligamentous tunnel of the medial collateral ligament, as detailed in the original description of the technique, the tendon was passed around the incised sartorius fascia to the medial patellar margin, allowing the fascia to act as a pulley for the transferred tendon. Fixation of the tendon is achieved by passing it through an oblique transpatellar drill hole extending from the proximal medial patellar margin to the lateral patellar margin. The tendon is then tensioned with the knee in 30 degrees of flexion and fixed with non-resorbable sutures placed subperiosteally, with additional single resorbable sutures joining the distal part of the VMO and the medial patellar margin.
Illustration of the dynamic reconstruction technique according to Ostermeier et al. [24]. The distal part of the gracilis tendon is detached from its tibial insertion and transferred to the medial margin of the patella
Clinical outcome measures
Data collection was performed at the follow-up examination and according to patient records. Two board-certified orthopaedic surgeons not involved in the surgical procedures conducted all the postoperative follow-up examinations.
Rating of the results was performed using the Kujala score as the primary outcome measure [18]. Secondary outcome measures were the Lysholm score [20], Tegner [36] score, and pain level using a visual analogue scale (VAS) score (10 cm, 0 = no pain, 10 = severe pain). General satisfaction with treatment outcomes was evaluated by questionnaire (1 = excellent, 2 = very good, 3 = good, 4 = fair, 5 = poor) and by asking patients whether they would undergo the procedure again and would recommend this procedure. Furthermore, recurrence of dislocation, reoperation, and other postoperative complications was recorded.
Radiological outcome measures
All patients underwent a standardized radiographic evaluation at the follow-up visit, including conventional plain anteroposterior (standing weight bearing), straight lateral, and axial views. Patellar height, patellar tilt, and patellar shift were compared with preoperative radiographs. Patellar height was assessed on the lateral radiographs using the Caton-Deschamps index [2]. Patellar tilt angle [14] and patellar shift [37] were determined on axial views.
Institutional review board approval (ID 4433) was obtained from the ethics committee of Hannover Medical School prior to the study.
Statistical analysis
Sample size calculation was performed according to published results of the techniques [24, 29] with different score results by nine points with a standard deviation of 10 % using the Kujala score as the primary variable. The dropout rate was assumed to be 10 %. A power calculation was performed with a confidence level of 95 % (a = 0.05) and a power (1 − b) of 90 %, resulting in a minimum requirement of 14 patients per group.
PASW Statistics for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA), was used for all analyses. Descriptive statistics (means and standard deviation values) were calculated. The Kolmogorov–Smirnov test was used to test the normality of the distributions. To determine differences between groups, a two-tailed Student’s t test was used. A P value ≤0.05 was considered significant.
Results
Mean follow-up was 26 ± 0.6 months (range 20–34 months). No significant between-group differences were observed in demographic data and pathology-determining parameters (Table 1).
No intraoperative or early postoperative complications were observed. Two patients underwent further operative treatment of the affected knee. One patient from the static group underwent arthroscopic partial meniscectomy independent of the prior patella-stabilizing procedure. One patient from the dynamic group underwent another patellar-stabilizing procedure because of continued lateral patellar dislocations. No other recurrences were noted in either group.
No scores were taken from the two reoperated patients, leaving 14 patients for analysis. However, the patient with resubluxations was rated as a surgical failure, and the patient’s general satisfaction with the treatment was rated as poor.
No significant differences were observed between groups with respect to the Kujala, Lysholm, and Tegner scores and the VAS pain score (Table 2). All but one patient in each group indicated they would undergo the procedure again. Surprisingly, only 12 patients from the static group and 11 patients from the dynamic group would recommend the procedure. When compared with the contralateral side, a flexion deficit of 5° was found in one patient and a flexion deficit of 10° in three patients (all from the static group).
No significant differences were observed between groups in radiological outcome parameters of patellar height, patellar tilt, and patellar shift (Table 3). Comparison of changes between pre- and postoperative findings also revealed no significant differences. Slight decreases in mean values were found in all parameters in the dynamic group, whereas in the static group, patellar shift and patellar height remained almost unchanged (Table 3).
Discussion
The most important finding of this study is that both techniques resulted in satisfactory clinical outcomes. The complication rate was low, with subjectively satisfied patients in most cases. No significant differences were observed in score and radiological outcome parameters. However, one patient in the dynamic reconstruction group needed revision surgery because of recurrent lateral patellar dislocations, whereas no static reconstruction patient had a new dislocation after MPFL reconstruction.
The hypothesis that dynamic reconstruction leads to a favourable clinical and radiological outcome over static reconstruction could not be confirmed. In the present study, whether protection against malpositioning or over-tensioning of the graft was achieved by using the dynamic reconstruction remains unclear. However, the flexion deficit in 4 of 14 patients in the static reconstruction group might be an indicator of malposition or over-tension, although none of these patients reported major complaints or were found to have an inferior outcome compared with other patients with a range of motion equivalent to that of the contralateral knee.
Although it did not reach statistical significance, there was a slight tendency toward better average Kujala, Lysholm, and Tegner scores in the dynamic group than in the static reconstruction group. However, compared with previously published scores after MPFL reconstruction [10, 32, 34], scores in both groups were rather low. Comparison of our results with those previously reported is difficult because of differing study protocols, outcome criteria, and pathologies treated. In the original publication reporting the technique used for this study, Schoettle et al. [29] reported an average postoperative Kujala score of 85.7 points compared with 82 points in this series. Mean Kujala scores in the original publication of Ostermeier et al. [24] (95 points) were better than those in this study (84 points). The reasons for the inferior findings among the patients in this study remain unclear. Possible explanations could be the different follow-up periods; abbreviations of the techniques used, with different surgeons performing the procedures; and a possible bias from non-independent follow-up examinations. Furthermore, in both original studies, the semitendinosus tendon was used for reconstruction. However, both authors recommended use of the gracilis tendon in later publications [23, 30, 31], consistent with other publications on reconstruction of the MPFL [3, 21, 27].
Radiological evaluation revealed only slight changes compared with preoperative findings in both groups. This is not surprising, because reconstruction of the MPFL treats lateral instability in the first 30 degrees of knee flexion. Axial views are performed in 45 degrees of flexion and in many instances show normal values with respect to the patellar tilt angle and patellar shift. Interestingly, although the mean Δ values were almost comparable between the two groups, the standard deviation was higher in the dynamic reconstruction group, probably because of less rigid fixation of the graft.
The major limitations of this study are the short follow-up and the small number of patients being evaluated. However, power analysis with sample size calculation was performed according to published results of the techniques, and the mean follow-up time of over 2 years appears sufficient to obtain meaningful results. The strengths of this study are that patients were matched, providing comparable study groups, and that two observers not involved in the surgical procedures independently examined all patients. The interpretations of the radiological outcomes should be regarded cautiously because the preoperative radiographs were performed in two different hospitals, whereas the follow-up examination was performed in the same hospital.
Conclusion
The findings of this study suggest that both techniques result in satisfactory, comparable short-term outcomes with low complication rates.
References
Beck P, Brown NA, Greis PE, Burks RT (2007) Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med 35:1557–1563
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Christiansen SE, Jakobsen BW, Lund B, Lind M (2008) Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 24:881–887
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg Am 90:2751–2762
Conlan T, Garth WP Jr, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75:682–693
Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M (2005) A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc 13:522–528
Dejour D, Saggin PRMX, Tavernier T (2010) Standard X-ray examination: patellofemoral disorders. In: Zaffagnini S, Dejour D, Arendt EA (eds) Patellofemoral pain, instability, and arthritis. Springer, Heidelberg, pp 51–60
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 34:1478–1485
Frosch S, Balcarek P, Walde TA, Schuttrumpf JP, Wachowski MM, Ferleman KG, Sturmer KM, Frosch KH (2011) The treatment of patellar dislocation: a systematic review. Z Orthop Unfall 149:630–645
Giordano M, Falciglia F, Aulisa A, Guzzanti V (2011) Patellar dislocation in skeletally immature patients: semitendinosus and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:1784–1786
Gomes JE (2008) Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy 24:430–435
Goyal D (2013) Medial patellofemoral ligament reconstruction: the superficial quad technique. Am J Sports Med 41:1022–1029
Grelsamer RP, Bazos AN, Proctor CS (1993) Radiographic analysis of patellar tilt. J Bone Joint Surg Br 75:822–824
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res 252:190–197
Kang H, Cao J, Yu D, Zheng Z, Wang F (2013) Comparison of 2 different techniques for anatomic reconstruction of the medial patellofemoral ligament: a prospective randomized study. Am J Sports Med 41:1013–1021
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Lanz (2013) Sehnenplastik bei habitueller Luxation der Patella. Zbl Chir 31:829
Lysholm J, Nordin M, Ekstrand J, Gillquist J (1984) The effect of a patella brace on performance in a knee extension strength test in patients with patellar pain. Am J Sports Med 12:110–112
Nelitz M, Dreyhaupt J, Lippacher S (2013) Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med 41:1005–1012
Nomura E, Inoue M (2003) Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy 19(5):E47
Ostermeier S, Becher C (2010) Vorderes Knieschmerzsyndrom. Deutscher Ärzte-Verlag, Köln
Ostermeier S, Stukenborg-Colsman C, Wirth CJ, Bohnsack M (2007) Reconstruction of the medial patellofemoral ligament by tunnel transfer of the semitendinosus tendon. Oper Orthop Traumatol 19:489–501
OUTERBRIDGE RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43:752–757
Panagopoulos A, van Niekerk l, Triantafillopoulos IK (2008) MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med 29:359–365
Quirbach S, Smekal V, Rosenberger RE, El AR, Schottle PB (2012) Anatomical double-bundle reconstruction of the medial patellofemoral ligament with a gracilis autograft. Oper Orthop Traumatol 24:131–139
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Schottle PB, Fucentese SF, Romero J (2005) Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 13:516–521
Schottle PB, Hensler D, Imhoff AB (2009) Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc 18:147–151
Schottle PB, Romero J, Schmeling A, Weiler A (2008) Technical note: anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 128:479–484
Singhal R, Rogers S, Charalambous CP (2013) Double-bundle medial patellofemoral ligament reconstruction with hamstring tendon autograft and mediolateral patellar tunnel fixation: a meta-analysis of outcomes and complications. Bone Joint J 95:900–905
Smith TO, Song F, Donell ST, Hing CB (2011) Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc 19:988–998
Smith TO, Walker J, Russell N (2007) Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 15:1301–1314
Steiner TM, Torga-Spak R, Teitge RA (2006) Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med 34:1254–1261
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Urch SE, Tritle BA, Shelbourne KD, Gray T (2009) Axial linear patellar displacement: a new measurement of patellofemoral congruence. Am J Sports Med 37:970–973
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becher, C., Kley, K., Lobenhoffer, P. et al. Dynamic versus static reconstruction of the medial patellofemoral ligament for recurrent lateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc 22, 2452–2457 (2014). https://doi.org/10.1007/s00167-014-3020-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3020-7