Abstract
Purpose
Various techniques for reconstruction of the medial patellofemoral ligament (MPFL) have been developed. In this article, a modified technique for anatomical two-bundle MPFL reconstruction with hardware-free patellar graft fixation is described and the preliminary results of this technique are presented.
Methods
A modified surgical technique for MPFL reconstruction with a gracilis tendon autograft and hardware-free patellar graft fixation using two short oblique bone tunnels is described in detail. Complications and preliminary results of this procedure were assessed in 19 patients at a mean follow-up of 16 ± 3 months using the Kujala score, Tegner scale, and Insall score.
Results
No postoperative patellar dislocation or subluxation was reported. Eighty-nine per cent of the patients were either satisfied or very satisfied with the overall outcome. The mean Kujala score was 92 ± 7 (range 69–100), and the median Tegner scale was 5 (range 3–7). According to the Insall score, the results of 18 patients (95 %) were rated as good or excellent. Postoperative complications occurred in 3 patients (16 %), with two of them persisting only temporary.
Conclusions
The described technique for anatomical two-bundle MPFL reconstruction is a safe and effective surgical procedure for the treatment of lateral patellar instability, with several methodical advantages compared to similar techniques. Further evaluation in a larger patient cohort with a longer follow-up is necessary to confirm these short-term results.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous surgical procedures with variable results have been described to treat lateral patellar instability [8, 38]. Since biomechanical studies have highlighted the crucial role of the medial patellofemoral ligament (MPFL) in maintaining patellar stability [2, 12, 31], and radiographic studies as well as open surgical exploration have shown that rupture of the MPFL is the main pathoanatomical finding after lateral patellar dislocation [40, 49], reconstruction of the MPFL has become a widely accepted and successful treatment method for lateral patellar instability [3, 16].
Various techniques for MPFL reconstruction have been described, including tendon transfers to the patella or femur [4, 10, 23, 34, 50], and reconstruction of the ligament with free tendon autografts, allografts, or synthetic material [14, 33, 36, 42, 44].
In order to more closely replicate the native anatomy of the MPFL, several authors have proposed a two-bundle technique with free tendon grafts [5, 7, 18, 25, 32, 36, 39, 42–44, 47]. It is believed that an anatomical reconstruction more likely restores physiologic patellofemoral loads and kinematics [2, 42, 44].
One of the major controversies with the use of free tendon grafts is the ideal graft fixation. Whereas most authors use interference screws for femoral graft fixation [5, 7, 18, 32, 36, 39, 42, 44], patellar graft fixation remains controversial, and several techniques have been described. Most of these techniques require hardware such as suture anchors [42, 43], tenodesis screws [44], suture buttons [21, 25, 56], or different suture materials [1, 47]. However, the use of hardware has several disadvantages such as soft tissue irritation, implant pain, foreign body reactions, and higher costs [6, 13, 46, 53]. Therefore, hardware-free patellar graft fixation might be a favourable alternative.
Different techniques for anatomical two-bundle MPFL reconstruction with hardware-free patellar graft fixation have been described [5, 7, 18, 29, 32, 36, 39]. However, each of these techniques has its specific shortcomings, which is why we have developed a modified technique. The purpose of this study is therefore (1) to describe a modified technique for anatomical two-bundle MPFL reconstruction with hardware-free patellar graft fixation and (2) to present the preliminary results of this technique.
Materials and methods
Preceding reconstruction of the MPFL, an arthroscopy is performed routinely. The gracilis tendon is harvested in a standard fashion. Both ends of the graft are prepared with non-absorbable sutures (e.g. No. 2 Ethibond, Ethicon, Somerville, NJ, USA) in a whip-stitch fashion over a length of 15 mm. The length of the graft should be at least 18 cm. To allow for easier passage of the graft through the patellar tunnels, the thinner end of the graft is prepared tapered.
Next, the medial and anteromedial aspect of the patella is prepared. A 3-cm vertical skin incision reaching from the superomedial corner to the midpoint of the medial margin of the patella is made [51]. After subcutaneous preparation, the periosteum of the proximomedial patella is carefully elevated off the medial and anterior patellar surface. In order not to jeopardize the blood supply of the patella, this step should be done sparingly.
A 2.4-mm threaded guidewire is drilled from the anterior surface of the patella, starting approximately 10 mm central of the superomedial corner, to the superior margin of the MPFL on the medial wall of the patella (Figs. 1a, 2a). In the axial view, this creates an oblique course of the guidewire, running from antero-central to infero-medial (Fig. 2b). A second guidewire is drilled parallel to the first guidewire with its entry point 10–15 mm more distal. By gently tilting the rotating guidewires, the diameter of the drill holes is increased to about 3 mm. This diameter is usually large enough to enable passage of the gracilis graft. If necessary, the guidewires can be overdrilled with a 4.0-mm cannulated drill. A bony rim is created between both tunnels on the anterior surface of the patella (Fig. 1b). The thinner end of the graft is passed through the superior bone tunnel from medial to central and back through the inferior tunnel from central to medial (Fig. 3). The midportion of the looped graft is placed in the bony rim on the patellar surface.
Creation of the patellar tunnels. a The first guidewire is drilled from the anterior surface of the patella, approximately 10 mm central of the superomedial corner to the superior margin of the MPFL insertion on the medial wall of the patella. The second guidewire is drilled parallel to the first one, about 10–15 more distal, b a bony rim is created between both entry points on the anterior surface of the patella
To create the femoral tunnel, the knee is placed in 90° of flexion. Because anatomical femoral tunnel placement is crucial for successful MPFL reconstruction [2, 51, 54], we routinely use a picture intensifier to identify the anatomical femoral insertion point using the radiographic landmarks described by Schottle et al. [45]. A guidewire with an eyelet is drilled through the femur from postero-medial to antero-lateral and subsequently is overdrilled to the contralateral cortex.
The free ends of the graft are passed through the second layer of the medial capsular–ligamentous complex. A nitinol wire is placed in the femoral tunnel, and both ends of the graft are pulled into the tunnel. In 30° of flexion, a bioabsorbable interference screw is inserted over the nitinol wire. While manually tensioning the graft, femoral fixation is performed when the lateral border of the patella is in line with the margin of the lateral trochlea. After confirming patellar stability and full range of motion, the detached periosteum is sutured back to the patella with absorbable sutures, covering the graft loop on the anterior patellar surface.
Postoperative management
Postoperative rehabilitation involves partial weight bearing for 2 weeks and a hinged knee brace for 6 weeks. Range of motion is not restricted. Low-impact sports (running, cycling) are allowed after 6 weeks, and full return to sports is allowed after 3 months.
Patient evaluation
Inclusion criteria for this study were as follows: isolated MPFL reconstruction using the described technique, closed femoral physis, minimum follow-up of 12 months, and informed consent of the patient to participate in this study.
Indications for isolated MPFL reconstruction were as follows: symptomatic lateral patellar instability with recurrent patellar dislocations or subluxations, failure of conservative treatment, increased lateral patellar translation with a positive lateral patellar apprehension sign, and a tear or sprain of the MPFL on preoperative magnetic resonance imaging (MRI). Contraindications for isolated MPFL reconstruction were as follows: osteoarthritis > grade 1 according to Kellgren and Lawrence [24], focal chondral defects > grade 2 according to Outerbridge [35], trochlear dysplasia > grade B according to Dejour [11], valgus deviation >5 [20], tibial tuberosity–trochlear groove distance >20 mm [41], and pathologic rotational alignment (femoral anteversion >20°, tibial torsion >40°) [20, 52]. Indications and contraindications were confirmed by history, clinical evaluation, plain radiographs, and MRI in all patients. Additional weight-bearing full-leg radiographs and computer tomography scans were obtained in patients with suspected abnormal limb alignment.
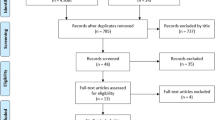
Between April 2011 and November 2011, 28 patients with symptomatic lateral patellar instability were treated by use of the above-described technique. Nine of these patients fulfilled at least one contraindication for isolated MPFL reconstruction, for which reason MPFL reconstruction was combined with concomitant procedures (distal femoral osteotomy, deepening trochleoplasty, matrix-associated chondrocyte implantation, lateral retinacular lengthening, lateral patellar facetectomy). These patients were excluded from further clinical evaluation, except for the assessment of postoperative patellar fracture. The final study population therefore consisted of 19 patients with an average follow-up of 16 ± 3 months. The detailed patient characteristics are provided in Table 1. All operations were performed or directly supervised by the first author.
Postoperative complications, patient satisfaction, knee function, and activity level were retrospectively assessed using a self-designed questionnaire, Kujala score [26], and Tegner scale [55]. The overall outcome was rated according to the Insall score [22] (Table 2).
Results
All patients were available for follow-up evaluation. No patient suffered recurrent patellar dislocation or subluxation. Eighty-nine per cent of the patients were either satisfied (32 %) or very satisfied (58 %) with the overall outcome of the operation. Two patients (11 %) were partially satisfied because of persistent pain during squatting, stair climbing, and sporting activities. No patient was dissatisfied with the outcome of the operation. All patients stated that they would undergo the surgery again. The mean Kujala score was 92 ± 7 (range 69–100), and the median Tegner scale was 5 (range 3–7). According to the Insall score [22], the results of 18 patients (95 %) were rated as good or excellent (Table 2).
Postoperative complications occurred in 3 patients (16 %). Two patients could not flex the knee beyond 90° at 6 weeks postoperatively and therefore required a prolonged rehabilitation program with intensified physical therapy. Three months postoperatively, full range of motion was achieved in both patients. One other patient suffered a displaced fracture of the superomedial quadrant of the patella during a high-velocity motorbike accident 3 months after MPFL reconstruction. The fracture ran through the inferior bone tunnel and was treated by open reduction and internal fixation using two small fragment screws. The MPFL was stable attached to the fragment and could be retained. At final follow-up, the fracture had healed completely and knee function as well as sporting activity was not impaired (Kujala score: 100, Tegner scale: 7, Insall grading: excellent).
Discussion
The main finding of the present study was that anatomical two-bundle MPFL reconstruction with a gracilis tendon autograft and hardware-free patellar graft fixation using two short oblique bone tunnels is an effective and save technique to treat patients with symptomatic lateral patellar instability.
Various techniques for MPFL reconstruction have been described, and to date, no technique is considered to represent the “gold standard”. Some authors have proposed a transfer of the quadriceps tendon [34, 50], patellar tendon [4], semitendinosus tendon [10], or adductor magnus tendon [48] as a single-bundle graft. Other authors placed a free tendon graft in a single patellar tunnel [1, 15, 21]. These techniques, however, must be considered as non-anatomical because the native anatomy of the MPFL with its broad patellar attachment and two-bundle structure is not replicated [2]. Non-anatomical MPFL reconstruction can cause non-physiologic loads and kinematics of the patellofemoral joint [2, 44]. Therefore, several authors have proposed a two-bundle technique using free tendon grafts [5, 7, 18, 25, 32, 36, 39, 42, 44]. Potential advantages of a two-bundle technique are as follows: more close reconstruction of the anatomical and biomechanical properties, less patellar rotation during flexion–extension movement because of a two-point fixation at the patella, and higher stability throughout a greater range of motion [18, 32, 44]. To date, it is not clear whether a two-bundle technique is superior compared to a single-bundle technique. However, similar to ACL reconstruction, we believe that anatomical reconstruction of the MPFL is one of the major keys to success.
Using free tendon grafts, patellar fixation remains an issue of debate. Several authors have used hardware for patellar fixation, such as suture anchors [42], tenodesis screws [44], suture buttons [21, 25, 56], or different suture material [1, 47]. However, hardware-free patellar graft fixation has the advantage of lower risk for soft tissue irritation, implant pain, and foreign body reactions [6, 13, 37, 46, 53]. Furthermore, this method makes the operation more cost effective.
The concept of anatomical two-bundle MPFL reconstruction with hardware-free patellar graft fixation has been reported before [5, 7, 18, 29, 32, 36, 39]. Christiansen et al. [7] described a technique in which the gracilis tendon was looped through two transverse 4.5-mm drill holes in the patella (transpatellar drill holes) (Fig. 4c). Other authors described a similar technique using the semitendinosus tendon [5, 18, 39]. Panni et al. [36] proposed to drill two 5-mm diverging transpatellar tunnels in order to more closely replicate the course of the inferior-straight and superior-oblique bundle (Fig. 4d). Nelitz et al. [32] looped a gracilis graft through a V-shaped tunnel at the superomedial half of the patella (Fig. 4e). LeGrand et al. [27] described a technique with two oblique tunnels, comparable to our technique (Fig. 4b). However, these authors used the semitendinosus tendon, which required tunnel diameters of 5–6 mm. Furthermore, the exit points of the tunnels on the patellar surface were located markedly more laterally, between the midpoint and the lateral third of the patella.
Different techniques for anatomical two-bundle MPFL reconstruction with hardware-free patellar graft fixation. a Technique presented in this article (drill hole diameter usually 3 mm), b technique according to LeGrand et al. [27] (drill hole diameter 5–6 mm), c technique according to Christiansen et al. [7] (drill hole diameter 4.5 mm), d technique according to Panni et al. [36] (drill hole diameter 5 mm), e technique according to Nelitz et al. [32] (drill hole diameter 4 mm)
In clinical follow-up studies, several of these techniques have demonstrated to achieve good to excellent results in most patients with mean postoperative Kujala scores of 83–92, median Tegner scores of 4–5, and redislocation rates of 0–11 % [7, 18, 32, 36, 39]. However, each of these techniques has its specific shortcomings, for which reason we have developed a modified technique.
Using two transpatellar tunnels requires a long graft; therefore, the semitendinosus tendon is a common used graft source [5, 18, 39]. A semitendinosus graft, however, requires larger tunnel diameters (usually 5–6 mm [27]) with a higher risk of violating the anterior cortex or cartilage. These tunnels might create stress risers with increased risk for patellar fracture [37]. Furthermore, long tendon grafts combined with long tunnels increase the risk of micromotion of the graft within the tunnel, possibly leading to tunnel widening or abrasion of the graft at the tunnel aperture. The oblique bone tunnels used in our modified technique are considerably shorter compared to transpatellar tunnels, avoiding the disadvantages associated with long tunnels. To keep donor side morbidity as low as possible, we prefer to use the gracilis tendon. The mean tensile strength of the MPFL has been reported to be 208 N [31], whereas the mean strength of a single strand gracilis graft is 837 N [17], indicating that there is no need to use the semitendinosus tendon. In our experience, the length of a gracilis graft has always been sufficient for our technique. Using the gracilis tendon moreover enables to drill smaller tunnels. We usually drill two tunnels of 3 mm in diameter, which is considerably smaller compared to other techniques [7, 36]. Smaller patellar tunnels might lower the risk of joint penetration or patellar fracture. If the graft is looped around the lateral cortex of the patella, exposure of the lateral patellar wall is necessary. Therefore, some authors used an additional lateral incision or a longer midline incision [5, 18, 36, 39]. Our technique for patellar graft passage requires only one incision of about 3 cm lengths at the medial patellar border, making this technique less invasive and cosmetically more appealing.
The preliminary results of the described technique demonstrate a high patient satisfaction and good to excellent functional results at a mean follow-up of 15 months with no redislocation. The mean Kujala score and median Tegner scale at final follow-up were 92 and 5, respectively, which is comparable or even superior compared to other studies reporting on the results of anatomical two-bundle MPFL reconstruction with hardware-free patellar graft fixation [7, 18, 32, 36, 39].
A systematic review of 25 studies found a mean complication rate of 26 % after reconstruction of the MPFL [46]. A major complication after MPFL reconstruction is a fracture of the patella [46, 53]. Patellar fractures have been reported after MPFL reconstruction using bone tunnels [7, 14, 30, 36, 37], tenodesis screws [28], and suture anchors [37]. Most of these fractures occurred during activities of daily living or minor traumas, especially transverse bone tunnels traversing the entire width of the patella, and long oblique tunnels are believed to create stress risers with a considerable risk of patellar fracture [37]. By using shorter tunnels with smaller diameters, we thought to minimize the risk of patellar fracture. However, during the study period, a displaced fracture of the superomedial quadrant through the inferior patellar tunnel was seen in one of 28 patients. The fracture occurred 3 months after MPFL reconstruction during a high-velocity motorbike accident. After the study period, the described technique was used in more than 30 additional patients without the occurrence of a patellar fracture. We therefore believe that the risk of fracture is minimal without a high-impact trauma. However, this issue needs further attention in a larger study group.
To avoid patellar drill holes, suture fixation of the graft might be an alternative technique [9, 30, 47]. However, because of less initial fixation strength, range of motion and full weight bearing are usually restricted for the first 3–6 weeks postoperatively. Our technique provides high initial fixation strength [19], enabling immediate full range of motion and faster rehabilitation.
Shortcomings of this study are the retrospective study design, small sample size, and short-term follow-up. Furthermore, no statistical analysis was performed because preoperative scores were not available. However, the main intention of this article was to describe and discuss a modified technique for anatomical MPFL reconstruction, which we believe has several advantages compared to current methods. Because of the lack of a control group, this article cannot answer the question whether this technique is superior compared to other techniques. Further evaluation in a larger patient cohort with a longer follow-up is necessary to confirm the safety and effectiveness of this technique.
Conclusions
Compared to similar techniques, the described modification of an anatomical MPFL reconstruction with hardware-free patellar graft fixation has the advantage of short and small tunnels, less donor side morbidity, reduced risk of graft micromotion, minimal invasiveness, and more appealing cosmesis. The preliminary results of this technique are encouraging and comparable to those of other MPFL reconstruction techniques. Complications and results of this technique, including the risk for patellar fracture, have to be further evaluated in a larger patient cohort with longer follow-up.
References
Ahmad CS, Brown GD, Stein BS (2009) The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med 37(10):2021–2027
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10(3):215–220
Buckens CF, Saris DB (2010) Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med 38(1):181–188
Camanho GL, Bitar AC, Hernandez AJ, Olivi R (2007) Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy 23(1):108 e101–108 e104
Carmont MR, Maffulli N (2007) Medial patellofemoral ligament reconstruction: a new technique. BMC Musculoskelet Disord 8:22
Carr BJ, Ochoa L, Rankin D, Owens BD (2009) Biologic response to orthopedic sutures: a histologic study in a rabbit model. Orthopedics 32(11):828
Christiansen SE, Jacobsen BW, Lund B, Lind M (2008) Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy 24(1):82–87
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg Am 90(12):2751–2762
Deie M, Ochi M, Adachi N, Shibuya H, Nakamae A (2011) Medial patellofemoral ligament reconstruction fixed with a cylindrical bone plug and a grafted semitendinosus tendon at the original femoral site for recurrent patellar dislocation. Am J Sports Med 39(1):140–145
Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M (2005) A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc 13(7):522–528
Dejour H, Walch G, Neyret P, Adeleine P (1990) Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 76(1):45–54
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26(1):59–65
Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ (2012) Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med 40(6):1424–1430
Ellera Gomes JL (1992) Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: a preliminary report. Arthroscopy 8(3):335–340
Ellera Gomes JL, Stigler Marczyk LR, de Cesar Cesar P, Jungblut CF (2004) Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy 20(2):147–151
Fisher B, Nyland J, Brand E, Curtin B (2010) Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy 26(10):1384–1394
Hamner DL, Brown CH Jr, Steiner ME, Hecker AT, Hayes WC (1999) Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81(4):549–557
Han H, Xia Y, Yun X, Wu M (2011) Anatomical transverse patella double tunnel reconstruction of medial patellofemoral ligament with a hamstring tendon autograft for recurrent patellar dislocation. Arch Orthop Trauma Surg 131(3):343–351
Hapa O, Aksahin E, Ozden R, Pepe M, Yanat AN, Dogramaci Y, Bozdag E, Sunbuloglu E (2012) Aperture fixation instead of transverse tunnels at the patella for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20(2):322–326
Hinterwimmer S, Rosenstiel N, Lenich A, Waldt S, Imhoff AB (2012) Femoral osteotomy for patellofemoral instability. Unfallchirurg 115(5):410–416
Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD (2012) Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Joint Surg Br 94(9):1202–1208
Insall JN, Aglietti P, Tria AJ Jr (1983) Patellar pain and incongruence. II: clinical application. Clin Orthop Relat Res 176:225–232
Jacobi M, Reischl N, Bergmann M, Bouaicha S, Djonov V, Magnussen RA (2012) Reconstruction of the medial patellofemoral ligament using the adductor magnus tendon: an anatomic study. Arthroscopy 28(1):105–109
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kita K, Horibe S, Toritsuka Y, Nakamura N, Tanaka Y, Yonetani Y, Mae T, Nakata K, Yoshikawa H, Shino K (2012) Effects of medial patellofemoral ligament reconstruction on patellar tracking. Knee Surg Sports Traumatol Arthrosc 20(5):829–837
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9(2):159–163
LeGrand AB, Greis PE, Dobbs RE, Burks RT (2007) MPFL reconstruction. Sports Med Arthrosc 15(2):72–77
Lippacher S, Reichel H, Nelitz M (2010) Patellar fracture after patellar stabilization. Orthopade 39(5):516–518
Matthews JJ, Schranz P (2010) Reconstruction of the medial patellofemoral ligament using a longitudinal patellar tunnel technique. Int Orthop 34(8):1321–1325
Mikashima Y, Kimura M, Kobayashi Y, Miyawaki M, Tomatsu T (2006) Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg 72(1):65–71
Mountney J, Senavongse W, Amis AA, Thomas NP (2005) Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 87(1):36–40
Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S (2012) Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med 41(1):58–63
Nomura E, Inoue M (2003) Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy 19(5):E47
Noyes FR, Albright JC (2006) Reconstruction of the medial patellofemoral ligament with autologous quadriceps tendon. Arthroscopy 22(8):904e901–904e907
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43-B:752–757
Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N (2011) Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med 39(12):2647–2655
Parikh SN, Wall EJ (2011) Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am 93(17):97e91–97e98
Redziniak DE, Diduch DR, Mihalko WM, Fulkerson JP, Novicoff WM, Sheibani-Rad S, Saleh KJ (2009) Patellar instability. J Bone Joint Surg Am 91(9):2264–2275
Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N (2009) Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 37(9):1735–1742
Sallay PI, Poggi J, Speer KP, Garrett WE (1996) Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med 24(1):52–60
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13(1):26–31
Schottle P, Schmeling A, Romero J, Weiler A (2009) Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 129(3):305–309
Schottle PB, Fucentese SF, Romero J (2005) Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 13(7):516–521
Schottle PB, Hensler D, Imhoff AB (2010) Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc 18(2):147–151
Schottle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35(5):801–804
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C (2012) A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 40(8):1916–1923
Siebold R, Chikale S, Sartory N, Hariri N, Feil S, Passler HH (2010) Hamstring graft fixation in MPFL reconstruction at the patella using a transosseous suture technique. Knee Surg Sports Traumatol Arthrosc 18(11):1542–1544
Sillanpaa PJ, Maenpaa HM, Mattila VM, Visuri T, Pihlajamaki H (2009) A mini-invasive adductor magnus tendon transfer technique for medial patellofemoral ligament reconstruction: a technical note. Knee Surg Sports Traumatol Arthrosc 17(5):508–512
Spritzer CE, Courneya DL, Burk DL Jr, Garrett WE, Strong JA (1997) Medial retinacular complex injury in acute patellar dislocation: MR findings and surgical implications. AJR Am J Roentgenol 168(1):117–122
Steensen RN, Dopirak RM, Maurus PB (2005) A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy 21(3):365–370
Steensen RN, Dopirak RM, McDonald WG III (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32(6):1509–1513
Strecker W, Keppler P, Gebhard F, Kinzl L (1997) Length and torsion of the lower limb. J Bone Joint Surg Br 79(6):1019–1023
Tanaka MJ, Bollier MJ, Andrish JT, Fulkerson JP, Cosgarea AJ (2012) Complications of medial patellofemoral ligament reconstruction: common technical errors and factors for success: AAOS exhibit selection. J Bone Joint Surg Am 94(12):e87
Tateishi T, Tsuchiya M, Motosugi N, Asahina S, Ikeda H, Cho S, Muneta T (2011) Graft length change and radiographic assessment of femoral drill hole position for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19(3):400–407
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Toritsuka Y, Amano H, Mae T, Uchida R, Hamada M, Ohzono K, Shino K (2011) Dual tunnel medial patellofemoral ligament reconstruction for patients with patellar dislocation using a semitendinosus tendon autograft. Knee 18(4):214–219
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hinterwimmer, S., Imhoff, A.B., Minzlaff, P. et al. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc 21, 2147–2154 (2013). https://doi.org/10.1007/s00167-013-2498-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2498-8