Abstract
Nearly two decades after the first successful endovascular aortic repair (EVAR), steady advancements in device technology, deployment techniques, and imaging capabilities have allowed this treatment modality to replace traditional open aortic repair as the treatment of choice for patients undergoing elective abdominal aortic aneurysm (AAA) repair. EVAR now accounts for greater than half of all AAA repairs; however, certain challenges to EVAR remain including anatomic limitations and graft durability. These limitations are now being addressed with new technology and deployment modalities. Surveillance and surgical repair remain the primary focus of therapy for AAA, and this chapter aims to discuss developments in disease surveillance, interventional techniques, and the evolution of endograft devices for EVAR.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Abdominal aortic aneurysm
- Endovascular aortic repair
- Aneurysm
- Stent graft
- Endograft
- Aneurysm surveillance
Introduction
Abdominal aortic aneurysms (AAA) affect approximately 5 % of men and 1 % of women over the age of 60 years, and multiple epidemiological studies indicate that the incidence is increasing despite improved medical management of certain risk factors [1]. Weakening of the aortic wall due to systemic and local pathology combined with a genetic predisposition results in progressive wall stress and aneurysm dilation. Most AAAs remain asymptomatic and undetected, and unfortunately without intervention, rupture may occur [2]. In the USA, AAAs are estimated as the tenth most common cause of mortality and are responsible for approximately 2 % of all deaths [3].
Since the first open AAA repair nearly 60 years ago, surveillance and surgical repair of AAAs remain the mainstay of therapy, with maximum aneurysm diameter between 5 and 5.5 cm the accepted threshold for repair in average risk patients [4]. It has been nearly two decades since Parodi and colleagues pioneered the first successful endovascular aortic aneurysm repair (EVAR) in humans, and with steady advances in device technology, deployment techniques, and imaging capabilities, this treatment modality has now replaced open aortic repair as the treatment of choice for patients undergoing elective AAA repair [5]. This evolution has been buoyed by large, randomized controlled trials that compared morbidity and mortality rates for EVAR vs. open AAA repair and demonstrated superior outcomes for EVAR (Table1.1) [6–10].
EVAR now accounts for more than half of all AAA repairs, and despite the favorable clinical outcomes and patient demand for this less invasive approach to AAA repair, certain challenges to EVAR including anatomic limitations and graft durability remain and limit its potential applicability to some patients [11]. These limitations are now being addressed with new technology and deployment techniques. This chapter aims to discuss recent advances in the diagnosis and management of AAAs including developments in diagnosis and surveillance, EVAR devices and techniques, and medical management of AAAs.
Latest Developments in Diagnosis and Screening
Indications for open aortic repair were originally derived from the calculated risk of rupture rates based on aneurysm diameter, and this remains the mainstay of diagnosis and treatment algorithms for AAA. In a review published by the Society for Vascular Surgery, compiled data from multiple studies demonstrates very little risk of rupture for AAAs less than 5 cm in diameter. Once an AAA grows beyond 5.5 cm, however, the increase in annual rupture risk rises exponentially to 9.4 % [12,13]. Therefore, current practice mandates elective repair for all symptomatic aneurysms and AAAs greater than 5.5 cm in diameter [4].
Aneurysm Screening and Imaging
Ultrasonography (US) is the preferred diagnostic technique for screening of AAAs as it detects the presence of an aneurysm at low cost with sensitivity and specificity approaching 100 % [14,15]. Computed tomography (CT) surpasses US in reproducibility but its use for routine screening and surveillance should be limited due to radiation exposure and expense [16]. While serial CT scanning of AAAs has demonstrated a marginal shortening in proximal neck length and a small increase in neck diameter as the aneurysm grows during surveillance [17–19], early screening with CT instead of US fails to capture more patients anatomically suitable for EVAR. Therefore, many centers forgo CT evaluation until the aneurysm size approaches the indications for repair, and CT should be primarily used as an imaging modality for preoperative planning to evaluate the morphology of the AAA, iliofemoral access characteristics, device sizing, and also to detect anomalous or unusual arterial anatomy.
Asymptomatic patients who should be screened for AAA include those with risk factors including increasing age, male gender, white race, long history of smoking, personal or family history of AAA or other vascular aneurysms, hypertension, atherosclerotic disease, and hypercholesterolemia [4,20]. Frequency of surveillance for patients with AAA depends on aneurysm size, with 12-month intervals for AAA 3.5–4.4 cm in diameter and 6-month intervals for AAA 4.5–5.4 cm in diameter [21]. These recommendations are based primarily on findings from the UK Small Aneurysm Trial which also showed that growth rate was greatest among smokers, lowest in patients with a lower ankle-brachial index and diabetes, and was unaffected by lipids and blood pressure. A recent European meta-analysis has demonstrated a significant decrease in aneurysm-related mortality and a 50 % reduction in the number of emergency operations for ruptured AAA after 3–5 years of US screening [22]. Additionally, a multicenter study in the United Kingdom by Kim et al. found sustained cost-effectiveness and improved survival rates in male patients participating in a 7-year US screening program [23]. Recognizing these developments, the USA implemented the Screening Abdominal Aortic Aneurysms Very Efficiently (SAAAVE) Act in 2007, which provides Medicare coverage of screening US for men 65–75 years of age who have ever smoked or men and women who have a family history of AAA [24].
Repair of Small AAA
Whether patients benefit from prophylactic repair of smaller aneurysms (i.e., 4–5 cm range) has been an area of much debate. Two randomized prospective clinical trials, the United States Aneurysm Detection and Management Study (ADAM) and the United Kingdom Small Aneurysm Trial (UKSAT), have determined surveillance alone every 3 or 6 months for AAA 4.0–5.4 cm in diameter is as effective as elective open surgical repair in reducing mortality risk. Most patients, however, did eventually require intervention as demonstrated by a 10-year follow-up report in which 74 % of patients from the surveillance cohort had undergone surgical repair [12,25–28].
Despite the lack of evidence to support early open repair of small AAA, an endovascular approach may offer additional benefits. Smaller AAAs may be more anatomically amenable to EVAR, and in fact, studies have shown AAAs less than 5.5 cm in diameter have longer infrarenal necks, less angulation, less tortuosity, and longer iliac landing zones than larger aneurysms [18,29]. In a prospective clinical series of 206 patients, Arko et al. found no significant difference in proximal neck diameter, but that larger aneurysms (>6 cm) had 27 % shorter and 15 % more angulated proximal necks than smaller aneurysms (<5 cm) [30]. Furthermore, two randomized clinical trials were initiated to evaluate EVAR outcomes vs. surveillance for small AAAs: (1) the European-based Comparison of Surveillance vs. Aortic Endografting for Small Aneurysm Repair (CAESAR) trial and (2) the United States’ Positive Impact of Endovascular Options for Treating Aneurysm Early (PIVOTAL) trial [31–33].
The CAESAR trial enrolled 360 (of a planned 740) patients before the trial ended prematurely due to lack of funding and delay in patient enrollment. There was no difference in mortality between EVAR and surveillance at 3 years, but a surprising 58.2 % of patients required repair even at this short surveillance interval [34]. The PIVOTAL trial results demonstrated that in the 728 (of a planned 1,050) patients with AAA (4–5 cm) randomized to receive EVAR vs. ultrasound surveillance, mortality did not differ (4.1 % in each group) at a mean follow-up of 20 months. Aneurysm-related death and time to rupture were negligible (0.6 %) in both groups, and this led to the early discontinuation of enrollment in the study. The patients in the surveillance arm underwent a rigorous schedule of ultrasound or CT scan every 6 months, and nearly one third of this group subsequently underwent repair [33]. The number of patients in this study who “crossed over” from the surveillance to the treatment arm is consistent with the other large randomized controlled trials comparing early vs. late repair, with crossover rates ranging from 27 to 60 % [35].
Most of the surveillance patients in PIVOTAL who crossed over to intervention did so due to an enlarging aneurysm [33]. However, 11 % cited anxiety as the primary reason for pursuing treatment. Other studies have documented much higher rates: in the ADAM and UKSAT trials, as many as 26 and 23 % of patients requested early treatment due to “symptoms” or “increased anxiety,” respectively [35]. The role that quality of life measures play in appropriate treatment selection remains an area of investigation. In summary, current recommendations provided by the Society for Vascular Surgery state that for aneurysms in the range of 4.0–5.4 cm, surveillance followed by selective repair is recommended for older males with significant comorbidities; some young healthy patients, particularly women, may see benefit from early repair between 5.0 and 5.4 cm [4]. Future long-term data on these patients should help elucidate the benefit vs. risk ratio for small aneurysm EVAR.
Development in EVAR Devices
Stent grafts are classified based on body characteristics (i.e., tube vs. bifurcated, unibody vs. modular), means of deployment (i.e., self-expanding vs. balloon-inflated), and mode of fixation (i.e., active vs. passive). They are produced from a combination of stainless steel, cobalt chromium, or nickel alloys with a durable graft material such as Dacron or PTFE [36]. The ideal aortic stent graft is hemostatic, user-friendly, and contains a low-profile delivery system which is flexible when maneuvering yet rigid enough to resist kinking. The graft material must be thin to facilitate a lower profile yet maintain low porosity and demonstrate strength and durability. Finally, the metal frame supporting the graft must provide a high column strength and durability, maintain resistance to external compression, corrosion and fatigue, and importantly, be radiopaque [37].
Current FDA-Approved Devices
The aforementioned requirements, combined with the stringent scrutiny of the Food and Drug Administration, have led to only 6 of 16 devices developed in the past two decades achieving approval, one of which was taken off the market in March 2001 [38]. Current Food and Drug Administration (FDA)-approved EVAR devices and their characteristics are listed in Table1.2. Due to potential problems with distal attachment site failure, all current devices are bifurcated endografts which allow for distal attachment at the level of the iliac arteries. Unibody bifurcated grafts (i.e., the Powerlink, Endologix, Irvine, CA) are placed as a whole, requiring subsequent retraction of the second iliac limb via contralateral access. Modular bifurcated grafts are composed of a main body with a short contralateral limb and provide customized intraoperative deployment [39].
The AneuRx (Medtronic, Santa Rosa, CA) bifurcated, modular stent graft is composed of a nitinol frame and polyester graft material and contains no barbs or hooks for main body attachment. Bilateral femoral or iliac access is required for the main body and contralateral limb through a 21-French (F) and 16–19-F catheter, respectively. The device is currently in its sixth generation and has the largest cumulative clinical experience, with greater than 80,000 endoprostheses deployed worldwide as of 2010. Though the Aneuryx device has certain favorable characteristics such as the potential to treat the smallest aortic diameter, concerns for a higher risk of device migration remains due to the lack of an active proximal fixation mechanism [39]. The Talent (Medtronic, Santa Rosa, CA) abdominal stent graft is a modular, bifurcated stent of similar material that was designed to treat a larger range of aortic and iliac diameters, extending its indications to include AAA with aortic necks from 18 to 32 mm and iliac arteries from 7 to 22 mm in diameter. Long-term follow-up data of the most recent generation Talent graft demonstrates comparable results to other stent grafts, and its use in AAA with short necks (10–15 mm) has provided encouraging results at 5-year follow-up [40,41].
The Excluder (W.L. Gore, Flagstaff, AZ) graft is also a bifurcated, modular stent graft composed of a nitinol frame and PTFE graft material with active fixation facilitated by anchoring barbs. Delivery of the main body and contralateral limbs is made through 18-F and 12-F sheaths for the standard diameter grafts. A significant advantage of this device is its relatively low profile, flexibility, and uncomplicated deployment system. The first-generation Excluder graft has been implicated in a substantial percentage of patients demonstrating aneurysm growth; however, later modifications of the graft with addition of a lower permeability membrane has demonstrated success in arresting AAA expansion and facilitating AAA sac regression [39,42]. Furthermore, the latest version of this device (C3 delivery system) incorporates a unique feature for added deployment control which allows the surgeon/interventionalist to partially deploy and reposition the device. This feature may prove to revise EVAR techniques altogether and certainly will expand the anatomic inclusion criteria for most operators.
The Zenith Flex (Cook Inc., Bloomington, IN) endoprosthesis provides suprarenal fixation with an uncovered proximal stent and fixation barbs and is available in a wide range of sizes. Due to its ferromagnetic exoskeleton, this stent is unsafe for magnetic resonance (MR) imaging. Deployment is staged, with partial deployment of the main body preceding the barbed suprarenal fixation stent, and is completed with contralateral iliac limb followed by full release of the main body. Additional steps include removal of the top cap, adding the ipsilateral iliac limb, and inflating the balloon to secure sealing. The Zenith Flex provides flexibility with suprarenal fixation to abrogate stent migration and for the potential treatment of AAAs with shorter necks. The Powerlink device has been available since 2004 and is a unibody, bifurcated, self-expanding stent graft with infrarenal and suprarenal extensions available. Its deployment from a distal to proximal fashion, with fixation of the aortic bifurcation preceding suprarenal fixation, has the potential to prevent device migration and subsequent endoleak. Graft migration rates vary from 4.2 to 7 % and limb occlusion rates ranged from 1 to 2 %, with improvement once primary deployment at the aortic bifurcation was implemented [43–45]. A distinct advantage is the low-profile (9F) contralateral limb.
While all FDA-approved devices have unique features, little significant difference in EVAR outcomes, including endoleak, device migration, and graft occlusion rates, have been definitively determined [46]. The following section describes newer technology currently pending FDA approval in the USA but that may be available in Europe and elsewhere. These devices are considered “next-generation” devices aimed at expanding the anatomic inclusion criteria for EVAR.
Next-Generation Devices: Expanding the Anatomic Inclusion Criteria
EVAR requires certain aortoiliac anatomic criteria for adequate aneurysm exclusion and prevention of complications. On-label use of current FDA-approved devices would limit EVAR anatomical inclusion criteria to AAAs with a 10–15-mm infrarenal neck length, aortic diameter ≤32 mm, angulation <60°, and 7-mm iliac access diameter [4]. Mounting experience with the current devices, recognized need to expand therapy, and patient demand for this less invasive approach to AAA repair have driven industry to develop novel “next-generation” devices that either improve on the current prototypes or expand the anatomic inclusion criteria (Fig.1.1). The most frequent anatomic features limiting potential EVAR are short and angulated proximal aortic necks [47]. The Anaconda (Vascutek, Terumo, Inchinnan, Scotland) and Aorfix (Lombard Medical, Oxfordshire, UK) stent grafts are designed to address AAAs with hostile neck anatomy, and both are currently in phase II US clinical trials.
The Anaconda is a unique tri-modular, repositionable stent graft composed of woven polyester with multiple independent ring stents that provide device flexibility. The main body size ranges from 19.5 to 34 mm for treatment of AAA from 16 to 32 mm in diameter. The Anaconda graft can be employed in AAAs with highly angulated proximal necks due to a saddle shape of the proximal stents: the apex of the convexity lies anteriorly-posteriorly and the concavity lies laterally. Fixation relies on the radial forces of two overlapping proximal components and four pairs of hooks, and during the implantation phase, the stents spread and flatten, moving proximally, therefore requiring adequate distance from the takeoff of the renal arteries. Two-year follow-up in patients with the Anaconda graft has shown no correlation of clinical or technical success or survival with degree of angulation of the proximal necks and no incidences of graft migration. Rates of proximal endoleak remain relatively high at up to 14 % [48–50].
Introduced in Europe in 2004, the Aorfix stent graft is a bifurcated or aorto-uni-iliac device developed with increased flexibility in order to acquire greater seal in proximal necks angulated greater than 45°. Four double hooks at the proximal end enhance fixation, and during deployment, pushrods maintain positioning of the proximal end of the graft and upon completion, the stent graft has a “fish-mouth” shape. Initial midterm results in a few small trials from Europe have demonstrated acceptable results in hostile neck anatomy, and results from the larger US PIVOTAL trial are pending [51,52].
Iliac artery anatomy must facilitate passage of the stent graft delivery system, and iliac tortuosity, calcification, and size are all potential limitations to EVAR. Even with adequate preoperative imaging and planning, 8–15 % of patients have iliac anatomy unsuitable for EVAR [53,54]. Women and patients of Asian ancestry represent two particularly problematic populations for iliofemoral access [4,55,56]. Two novel devices that have a reduced profile to address access challenges, while maintaining characteristics of durability and flexibility, are the Endurant (Medtronic, Santa Rosa, CA) and Ovation (TriVascular, Santa Rosa, CA) stent grafts.
The Endurant is Medtronic’s next-generation device which, similar to the Aneuryx and Talent devices, is composed of a nitinol polyester fabric and nitinol frame but also incorporates a suprarenal stent with barbs for active fixation. The device is highly flexible, designed to treat challenging neck anatomy, and also reduces the delivery profile to 18–20-F outer diameter. It has been approved in Europe since 2008 and has been recently approved in the USA. The TriVascular Ovation stent graft is a tri-modular, suprarenal device composed of nitinol stents encapsulated in PTFE and maintains the smallest profile of any device (14–15-F outer diameter delivery system). This device also has a novel seal technology which features two inflatable rings in the proximal seal zone that are filled with a polymer to enhance aortic wall apposition. The TriVascular device recently received its CE mark in Europe and is currently in a phase II nonrandomized multicenter trial in the USA.
Advances in EVAR Techniques
As medical device companies forge ahead with significant research and development of next-generation devices, physicians have gained significant experience with EVAR techniques over the past decade. While feasibility of this technology remains limited by some anatomical constraints, certain challenges such as difficult iliac access, hostile proximal aortic neck anatomy, and associated iliac aneurysms can be managed with currently available devices and some appropriate technical maneuvers.
Dealing with Challenging Iliac Artery Access
As previously mentioned, a substantial proportion of potential EVAR candidates has iliac artery anatomy not ideally suited for delivery of large-profile devices. Frequently encountered problems such as excessive vessel calcification, occlusive disease, and tortuosity may be overcome with adjunctive procedures such as iliac artery balloon angioplasty, endoluminal conduit construction (endoconduit), buddy wire techniques, external iliac artery straightening via manual extracorporeal compression or even retroperitoneal dissection and traction, and, occasionally, iliofemoral bypass conduit construction.
For patients with small diameter external iliac arteries (i.e., <7 mm), one should use the lowest possible profile device, and at times, the use of components from different manufacturers may be necessary to achieve aneurysm exclusion with the minimum profile. Several maneuvers may facilitate passage through small, calcified vessels including placement of mineral oil on the outer sheath (though the advent of hydrophilic sheaths makes this less necessary), sequential vessel expansion with gradual dilators, and balloon angioplasty. When performing balloon angioplasty, only the smallest profile necessary to facilitate passage of the main body of the graft is needed (usually an 8 mm balloon), and this vessel segment can often be covered with the stent graft or an adjunctive self-expanding stent following device deployment. Though more commonly needed for thoracic EVAR (TEVAR), an endoconduit may occasionally be the best option for safe delivery of the endograft [57,58]. In this scenario, a covered stent or a contralateral limb of the device (greater radial force) is deployed in the ipsilateral external and common iliac artery in a primary fashion, and the graft is then balloon dilated to facilitate passage of the device (Fig.1.2).
Endoconduit for challenging iliac access. (a) Primary stent graft placement followed by balloon angioplasty of a circumferentially calcified stenosis at the iliac artery bifurcation; (b) balloon angioplasty of the common and small diameter external iliac arteries; (c) completion angiogram demonstrating endoconduit
Extremely tortuous iliac vessels may be difficult to cross with a stiff wire, even when attempting exchange through a catheter, and in these scenarios, a “buddy wire” technique may be helpful. In this case, leaving a floppy wire and catheter in the proximal thoracic aorta will often provide enough stability to advance a stiff wire through a separate catheter which will straighten the tortuous iliac and facilitate passage of the device into the aorta. One must be mindful of the potential complications caused by the change in anatomical configuration after vessel straightening, including upward (i.e., cephalad) torque and device migration, and iliac limb kinking and occlusion.
Management of the Hostile Aortic Neck
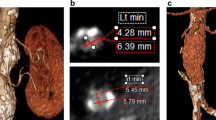
As mentioned previously, the most frequent anatomic features limiting potential EVAR are short and angulated proximal aortic necks, and there is no substitute for length with respect to preventing endoleak and potential device migration [59]. Greater neck length provides increased seal potential, and one of the best ways to maximize seal is optimizing graft positioning. This is facilitated by the use of preoperative 3D imaging for case planning with intraoperative magnification and appropriate adjustment of the fluoroscopy image intensifier to facilitate placement of the device as close to the renal arteries as possible. Future EVAR procedures may be enhanced by the use of novel imaging systems such as the Artis zeego (Siemens, Erlangen, Germany) which is the first robotically controlled multi-axis imaging system that provides simultaneous angiography and large volume 3D DynaCT imaging capacity (Fig.1.3).
Another technique to maximize the proximal seal zone, termed the “endo-wedge,” places wires into the renal artery via a proximal brachial approach and takes advantage of the proximal scalloped 4 mm of the Excluder device to maximize seal and achieve aneurysm exclusion [60]. For persistant proximal endoleaks, other options include placement of zero-extension aortic cuffs and/or balloon-expandable Palmaz (Cordis Corporation, Miami Lakes, FL) stents.
Iliac Artery Aneurysms
AAA-associated common iliac artery aneurysm occurs in 35 % of patients evaluated for EVAR, and these aneurysms may prevent a suitable seal zone in the distal common iliac artery [61,62]. For aneurysms that require unilateral extension to the external iliac artery for adequate seal, coil embolization of the ipsilateral hypogastric artery to prevent endoleak is generally safe [4,53,62]. While erectile dysfunction and buttock claudication may occur in up to 40 % of patients, symptoms usually improve with time [63–65]. Bilateral iliac aneurysms present a greater challenge because bilateral coil embolization, even in a staged fashion, is not as well tolerated as unilateral embolization [65,66]. Options in this setting include internal iliac artery bypass, endovascular repair with an iliac branched device (IBD), or endovascular repair using a “snorkel” technique (Fig.1.4). This later approach is attractive because it can be performed with the current commercially available devices, but its durability remains unknown.
Percutaneous EVAR
Percutaneous EVAR (PEVAR) is emerging as a feasible approach to endograft repair of AAA, particularly with advancements in both delivery and closure device technology [67]. EVAR device delivery systems range in size from 18 to 24 Fr and generally require external and common iliac artery diameters to be at least 7 mm [68]. Typically this is accessed via a femoral cutdown procedure in which an oblique incision is made in the groin to expose the femoral artery and ensure secure closure of the arteriotomy. Complications contributed to the groin wound, include pain, paresthesias, lymphoceles, wound infection, and scarring, which may greatly impact future interventions via the groin [69]. In keeping with the minimally invasive approach, percutaneous access for EVAR has been used to minimize these postsurgical complications and promote earlier ambulation and shorter procedure time.
The ideal candidate for PEVAR is a nonobese patient with noncalcified femoral arteries >7 mm in diameter. Femoral access is obtained through an ultrasound-guided puncture in the common femoral artery at least 1 cm proximal to the origin of the profunda femoris artery [67]. Some authors note successful PEVAR in suboptimal femoral artery anatomy, including obese patients and those with heavily calcified femoral arteries [70]. The procedure is performed using a “pre-close” technique in which the arteriotomy sutures are placed prior to placement of the large-diameter sheath or delivery catheter. This can be achieved with off-label use of one Prostar XL (Abbott Vascular, Abbott Park, Ill) or two Perclose Proglide (Abbott Vascular, Abbott Park, Ill) percutaneous closure devices, and safe closure of femoral artery defects as large as 24F has been demonstrated [71].
Several moderate-sized single center studies have been published demonstrating acceptable outcomes with PEVAR (Table1.3). A prospective, randomized controlled pilot study by Torsello et al. compared percutaneous closure with the 10-F Prostar XL to conventional cutdown technique. In one patient (of 30 total), conversion to an open groin incision was necessary due to bleeding after Prostar device deployment, and three devices initially failed (one due to needle deflection off calcified arterial wall, two due to failure of needles to grasp the arterial wall in obese patients), yet a second device was deployed without complication in all three cases. Postoperative arterial thrombosis occurred in one patient from each study group; however, mean operative time and time to ambulation were significantly shorter in the percutaneous closure group [69].
Aneurysm Surveillance Following EVAR
Postoperative surveillance is required after EVAR to detect and monitor potential complications such as endoleak or endotension, persistent flow inside the aneurysm sac. Endoleak is the most commonly detected complication of EVAR [85,86]. While the gold standard for post-EVAR surveillance currently relies on contrast-enhanced CT at 1, 6, and 12 months postoperatively with subsequent annual follow-up, other less invasive imaging modalities as well as protocols are emerging [86,87].
Color duplex US (CDUS) is frequently used for post-EVAR surveillance, but its potential limitations included high false-negative and false-positive results due to reflection from the metallic graft, calcifications, slow-flowing endoleaks, and obesity. Recent prospective studies have shown contrast-enhanced US (CEUS) to be superior to CDUS and a successful alternative to contrast-enhanced CT with the advantage of no additional radiation exposure [86]. CEUS relies on contrast agents composed of microbubbles which resonate upon interrogation with ultrasound and the recent introduction of second-generation agents has greatly improved their diagnostic accuracy. Advantages of CEUS over CT include increased detection capability despite high attenuation caused by extensive calcification and, occasionally, increased sensitivity to slow-flowing leaks [85].
CTA will likely remain a necessary post-EVAR evaluation in order to ensure accurate graft anchoring and integrity, post-repair aneurysm regression, and visceral vessel patency, but CEUS may well serve as an adequate surveillance tool and certainly diminish the number of surveillance CTs required.
Cardiomems Sac Pressure Monitoring
Intra-aneurysm sac pressure is one of the primary determinants of arterial wall stress and subsequent aneurysm expansion or shrinkage. The development of minimally invasive implantable telemetric sensors such as the FDA-approved EndoSure Wireless AAA Pressure Sensor (CardioMems, Atlanta, GA) allows for direct measurement of sac pressure without the added radiation or contrast exposure. The EndoSure sensor responds to changes in surrounding pressure by changing capacitance, and this resonance frequency is detected by an external antenna via radiofrequency impulse [88]. The device is delivered over a super stiff guidewire in the contralateral iliac artery during EVAR and positioned inside the aneurysm sac, held in place by its surrounding wire basket. In the Acute Pressure Measurement to Confirm Aneurysm Sac Exclusion (APEX) trial, the EndoSure sensor demonstrated a sensitivity of 0.939 and specificity of 0.800 for the detection of type I or III endoleaks when compared to intraoperative angiography [89]. The Cardiomems is an exciting new technology and holds the potential to significantly alter our current post-EVAR surveillance protocols, but its exact role in clinical practice remains to be seen.
Medical Management
The current medical management of AAA focuses on pathophysiologic contributors to aneurysmal disease, specifically hemodynamics, inflammation, and proteolytic enzymes. First-line therapy always includes smoking cessation due to its independent association with increased aneurysm growth rate [20]. Unfortunately, beta blockade with propranolol has failed to provide conclusive evidence for attenuated aneurysm growth rate [90,91]. Statin therapy, despite a lack of association between cholesterol levels and the expansion rate of AAAs, remains a promising and important component of therapy due to a proposed reduction in C-reactive protein levels, matrix metalloproteinase-9 (MMP-9) concentration, and infiltrating inflammatory cells [92–96]. Additionally, tetracycline antibiotics such as doxycycline hold much hope for becoming a mainstay of treatment due to their ability to inhibit MMP activity and attenuate elastin degradation, leading to dose-dependent prevention of aneurysm expansion [97,98]. In summary, when combined with US surveillance, optimum medical management for patients with small AAA provides a continuum of care prior to definitive repair.
Conclusion
AAAs remain underdiagnosed and a significant killer of the elderly population. Since the introduction of EVAR, the incidence of aneurysm-associated deaths has substantially decreased, correlating with an increase in elective AAA repair and decrease in repair of ruptured AAAs. As device technology and operative experience continue to improve, EVAR-related complications can be expected to decrease. Ultimately, improvements in AAA detection and advances in medical management to retard aneurysm growth remain the greatest potential for the next breakthrough in AAA therapy.
References
Best VA, Price JF, Fowkes FG. Persistent increase in the incidence of abdominal aortic aneurysm in Scotland, 1981–2000. Br J Surg. 2003;90(12):1510–5.
Nordon IM, Hinchliffe RJ, Holt PJ, Loftus IM, Thompson MM. Review of current theories for abdominal aortic aneurysm pathogenesis. Vascular. 2009;17(5):253–63.
Golledge J, Muller J, Daugherty A, Norman P. Abdominal aortic aneurysm: pathogenesis and implications for management. Arterioscler Thromb Vasc Biol. 2006;26(12):2605–13.
Chaikof EL, Brewster DC, Dalman RL, et al. The care of patients with an abdominal aortic aneurysm: the society for vascular surgery practice guidelines. J Vasc Surg. 2009;50(4 Suppl):S2–49.
Joels CS, Langan 3rd EM, Daley CA, et al. Changing indications and outcomes for open abdominal aortic aneurysm repair since the advent of endovascular repair. Am Surg. 2009;75(8):665–9; discussion 669–70.
De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1881–9.
Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet. 2004;364(9437):843–8.
Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D, Sculpher MJ. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1863–71.
Lederle FA, Freischlag JA, Kyriakides TC, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302(14):1535–42.
Prinssen M, Verhoeven EL, Buth J, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351(16):1607–18.
Giles KA, Pomposelli F, Hamdan A, Wyers M, Jhaveri A, Schermerhorn ML. Decrease in total aneurysm-related deaths in the era of endovascular aneurysm repair. J Vasc Surg. 2009;49(3):543–50; discussion 550–1.
Brewster DC, Cronenwett JL, Hallett Jr JW, Johnston KW, Krupski WC, Matsumura JS. Guidelines for the treatment of abdominal aortic aneurysms. Report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery. J Vasc Surg. 2003;37(5):1106–17.
Lederle FA, Johnson GR, Wilson SE, et al. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA. 2002;287(22):2968–72.
Lederle FA, Wilson SE, Johnson GR, et al. Variability in measurement of abdominal aortic aneurysms. Abdominal Aortic Aneurysm Detection and Management Veterans Administration Cooperative Study Group. J Vasc Surg. 1995;21(6):945–52.
Wilmink AB, Forshaw M, Quick CR, Hubbard CS, Day NE. Accuracy of serial screening for abdominal aortic aneurysms by ultrasound. J Med Screen. 2002;9(3):125–7.
Zhou W. Radiation exposure of vascular surgery patients beyond endovascular procedures. J Vasc Surg. 2011;53:39S–43. Epub 2010 Sept 16.
Lederle FA. The natural history of abdominal aortic aneurysm. Acta Chir Belg. 2009;109(1):7–12.
Propper BW, Rasmussen TE, Jones WT, Gifford SM, Burkhardt GE, Clouse WD. Temporal changes of aortic neck morphology in abdominal aortic aneurysms. J Vasc Surg. 2010;51(5):1111–5.
Schlosser FJ, Tangelder MJ, Verhagen HJ, et al. Growth predictors and prognosis of small abdominal aortic aneurysms. J Vasc Surg. 2008;47(6):1127–33.
Baxter BT, Terrin MC, Dalman RL. Medical management of small abdominal aortic aneurysms. Circulation. 2008;117(14):1883–9.
Brady AR, Thompson SG, Fowkes FG, Greenhalgh RM, Powell JT. Abdominal aortic aneurysm expansion: risk factors and time intervals for surveillance. Circulation. 2004;110(1):16–21.
Eckstein HH, Bockler D, Flessenkamper I, Schmitz-Rixen T, Debus S, Lang W. Ultrasonographic screening for the detection of abdominal aortic aneurysms. Dtsch Arztebl Int. 2009;106(41):657–63.
Kim LG, P Scott RA, Ashton HA, Thompson SG. A sustained mortality benefit from screening for abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):699–706.
Lee ES, Pickett E, Hedayati N, Dawson DL, Pevec WC. Implementation of an aortic screening program in clinical practice: implications for the Screen for Abdominal Aortic Aneurysms Very Efficiently (SAAAVE) Act. J Vasc Surg. 2009;49(5):1107–11.
Lederle FA, Wilson SE, Johnson GR, et al. Immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002;346(19):1437–44.
Brady AR, Brown LC, Fowkes FG, et al. Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002;346(19):1445–52.
Powell JT, Brady AR, Brown LC, et al. Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. The UK Small Aneurysm Trial Participants. Lancet. 1998;352(9141):1649–55.
Powell JT, Brown LC, Forbes JF, et al. Final 12-year follow-up of surgery versus surveillance in the UK Small Aneurysm Trial. Br J Surg. 2007;94(6):702–8.
Welborn 3rd MB, Yau FS, Modrall JG, et al. Endovascular repair of small abdominal aortic aneurysms: a paradigm shift? Vasc Endovascular Surg. 2005;39(5):381–91.
Arko FR, Filis KA, Hill BB, Fogarty TJ, Zarins CK. Morphologic changes and outcome following endovascular abdominal aortic aneurysm repair as a function of aneurysm size. Arch Surg. 2003;138(6):651–5; discussion 655–6.
Cao P. Comparison of surveillance vs aortic endografting for small aneurysm repair (CAESAR) trial: study design and progress. Eur J Vasc Endovasc Surg. 2005;30(3):245–51.
Ouriel K. Randomized clinical trials of endovascular repair versus surveillance for treatment of small abdominal aortic aneurysms. J Endovasc Ther. 2009;16 Suppl 1:I94–105.
Ouriel K, Clair DG, Kent KC, Zarins CK. Endovascular repair compared with surveillance for patients with small abdominal aortic aneurysms. J Vasc Surg. 2010;51(5):1081–7.
Cao P, De Rango P, Verzini F, Parlani G, Romano L, Cieri E. Comparison of surveillance versus aortic endografting for small aneurysm repair (CAESAR): results from a randomised trial. Eur J Vasc Endovasc Surg. 2011;41:13–25. Epub 2010 Sept 25.
Buckley CJ, Rutherford RB, Diethrich EB, Buckley SD. Inherent problems with randomized clinical trials with observational/no treatment arms. J Vasc Surg. 2010;52(1):237–41.
Soor GS, Chakrabarti MO, Abraham JR, et al. Aortic stent grafts. J Clin Pathol. 2008;61(7):794–801.
Gowda RM, Misra D, Tranbaugh RF, Ohki T, Khan IA. Endovascular stent grafting of descending thoracic aortic aneurysms. Chest. 2003;124(2):714–9.
Rutherford RB, Krupski WC. Current status of open versus endovascular stent-graft repair of abdominal aortic aneurysm. J Vasc Surg. 2004;39(5):1129–39.
Tan JWC, Yeo KK, Laird JR. Food and drug administration-approved endovascular repair devices for abdominal aortic aneurysms: a review. J Vasc Interv Radiol. 2008;19(6 Suppl 1):S9–17.
Jim J, Sanchez LA, Rubin BG, et al. A 5-year evaluation using the talent endovascular graft for endovascular aneurysm repair in short aortic necks. Ann Vasc Surg. 2010;24(7):851–8.
Turnbull IC, Criado FJ, Sanchez L, et al. Five-year results for the talent enhanced low profile system abdominal stent graft pivotal trial including early and long-term safety and efficacy. J Vasc Surg. 2010;51(3):537–44, 544 e531–532.
Haider SE, Najjar SF, Cho JS, et al. Sac behavior after aneurysm treatment with the gore excluder low-permeability aortic endoprosthesis: 12-month comparison to the original excluder device. J Vasc Surg. 2006;44(4):694–700.
Albertini JN, Lahlou Z, Magnan PE, Branchereau A. Endovascular repair of abdominal aortic aneurysms with a unibody stent-graft: 3-year results of the French Powerlink Multicenter Trial. J Endovasc Ther. 2005;12(6):629–37.
Carpenter JP. Midterm results of the multicenter trial of the powerlink bifurcated system for endovascular aortic aneurysm repair. J Vasc Surg. 2004;40(5):849–59.
Qu L, Raithel D. From clinical trials to clinical practice: 612 cases treated with the Powerlink stent-graft for endovascular repair of AAA. J Cardiovasc Surg (Torino). 2009;50(2):131–7.
Ouriel K, Clair DG, Greenberg RK, et al. Endovascular repair of abdominal aortic aneurysms: device-specific outcome. J Vasc Surg. 2003;37(5):991–8.
Simons P, van Overhagen H, Nawijn A, Bruijninckx B, Knippenberg B. Endovascular aneurysm repair with a bifurcated endovascular graft at a primary referral center: influence of experience, age, gender, and aneurysm size on suitability. J Vasc Surg. 2003;38(4):758–61.
Stella A, Freyrie A, Gargiulo M, Faggioli GL. The advantages of Anaconda endograft for AAA. J Cardiovasc Surg (Torino). 2009;50(2):145–52.
Freyrie A, Gargiulo M, Rossi C, et al. Preliminary results of Anaconda aortic endografts: a single center study. Eur J Vasc Endovasc Surg. 2007;34(6):693–8.
Saratzis N, Melas N, Saratzis A, et al. Anaconda aortic stent-graft: single-center experience of a new commercially available device for abdominal aortic aneurysms. J Endovasc Ther. 2008;15(1):33–41.
Albertini JN, Perdikides T, Soong CV, Hinchliffe RJ, Trojanowska M, Yusuf SW. Endovascular repair of abdominal aortic aneurysms in patients with severe angulation of the proximal neck using a flexible stent-graft: European Multicenter Experience. J Cardiovasc Surg (Torino). 2006;47(3):245–50.
Perdikides T, Georgiadis GS, Avgerinos ED, et al. The Aorfix stent-graft to treat infrarenal abdominal aortic aneurysms with angulated necks and/or tortuous iliac arteries: midterm results. J Endovasc Ther. 2009;16(5):567–76.
Henretta JP, Karch LA, Hodgson KJ, et al. Special iliac artery considerations during aneurysm endografting. Am J Surg. 1999;178(3):212–8.
Cotroneo AR, Iezzi R, Giancristofaro D, et al. Endovascular abdominal aortic aneurysm repair: how many patients are eligible for endovascular repair? Radiol Med. 2006;111(4):597–606.
Velazquez OC, Larson RA, Baum RA, et al. Gender-related differences in infrarenal aortic aneurysm morphologic features: issues relevant to Ancure and Talent endografts. J Vasc Surg. 2001;33(2 Suppl):S77–84.
Masuda EM, Caps MT, Singh N, et al. Effect of ethnicity on access and device complications during endovascular aneurysm repair. J Vasc Surg. 2004;40(1):24–9.
Hinchliffe RJ, Ivancev K, Sonesson B, Malina M. “Paving and cracking”: an endovascular technique to facilitate the introduction of aortic stent-grafts through stenosed iliac arteries. J Endovasc Ther. 2007;14(5):630–3.
Peterson BG, Matsumura JS. Creative options for large sheath access during aortic endografting. J Vasc Interv Radiol. 2008;19(6 Suppl):S22–6.
Leurs LJ, Kievit J, Dagnelie PC, Nelemans PJ, Buth J. Influence of infrarenal neck length on outcome of endovascular abdominal aortic aneurysm repair. J Endovasc Ther. 2006;13(5):640–8.
Minion DJ, Yancey A, Patterson DE, Saha S, Endean ED. The endowedge and kilt techniques to achieve additional juxtarenal seal during deployment of the Gore Excluder endoprosthesis. Ann Vasc Surg. 2006;20(4):472–7.
Vallabhaneni SR, Harris PL. Lessons learnt from the EUROSTAR registry on endovascular repair of abdominal aortic aneurysm repair. Eur J Radiol. 2001;39(1):34–41.
Lee C, Dougherty M, Calligaro K. Concomitant unilateral internal iliac artery embolization and endovascular infrarenal aortic aneurysm repair. J Vasc Surg. 2006;43(5):903–7.
Mehta M, Veith FJ, Ohki T, et al. Unilateral and bilateral hypogastric artery interruption during aortoiliac aneurysm repair in 154 patients: a relatively innocuous procedure. J Vasc Surg. 2001;33(2 Suppl):S27–32.
Lee WA, O’Dorisio J, Wolf YG, Hill BB, Fogarty TJ, Zarins CK. Outcome after unilateral hypogastric artery occlusion during endovascular aneurysm repair. J Vasc Surg. 2001;33(5):921–6.
Rayt HS, Bown MJ, Lambert KV, et al. Buttock claudication and erectile dysfunction after internal iliac artery embolization in patients prior to endovascular aortic aneurysm repair. Cardiovasc Intervent Radiol. 2008;31(4):728–34.
Morrissey NJ, Faries PL, Carrocio A, et al. Intentional internal iliac artery occlusion in endovascular repair of abdominal aortic aneurysms. J Invasive Cardiol. 2002;14(12):760–3.
Haas PC, Krajcer Z, Diethrich EB. Closure of large percutaneous access sites using the prostar XL percutaneous vascular surgery device. J Endovasc Surg. 1999;6(2):168–70.
Berland TL, Cayne NS, Veith FJ. Access complications during endovascular aortic repair. J Cardiovasc Surg (Torino). 2010;51(1):43–52.
Torsello GB, Kasprzak B, Klenk E, Tessarek J, Osada N, Torsello G. Endovascular suture versus cutdown for endovascular aneurysm repair: a prospective randomized pilot study. J Vasc Surg. 2003;38(1):78–82.
Smith ST, Timaran CH, Valentine RJ, Rosero EB, Clagett GP, Arko FR. Percutaneous access for endovascular abdominal aortic aneurysm repair: can selection criteria be expanded? Ann Vasc Surg. 2009;23(5):621–6.
Morasch MD. Percutaneous techniques for aneurysm repair. J Vasc Surg. 2006;43(Suppl a):69A–72.
Krajcer Z, Gregoric I. Totally percutaneous aortic aneurysm repair: methods and outcomes using the fully integrated IntuiTrak endovascular system. J Cardiovasc Surg (Torino). 2010;51(4):493–501.
Malkawi AH, Hinchliffe RJ, Holt PJ, Loftus IM, Thompson MM. Percutaneous access for endovascular aneurysm repair: a systematic review. Eur J Vasc Endovasc Surg. 2010;39(6):676–82.
Eisenack M, Umscheid T, Tessarek J, Torsello GF, Torsello GB. Percutaneous endovascular aortic aneurysm repair: a prospective evaluation of safety, efficiency, and risk factors. J Endovasc Ther. 2009;16(6):708–13.
Jahnke T, Schafer JP, Charalambous N, et al. Total percutaneous endovascular aneurysm repair with the dual 6-F Perclose-AT preclosing technique: a case-control study. J Vasc Interv Radiol. 2009;20(10):1292–8.
Lee WA, Brown MP, Nelson PR, Huber TS, Seeger JM. Midterm outcomes of femoral arteries after percutaneous endovascular aortic repair using the Preclose technique. J Vasc Surg. 2008;47(5):919–23.
Jean-Baptiste E, Hassen-Khodja R, Haudebourg P, Bouillanne PJ, Declemy S, Batt M. Percutaneous closure devices for endovascular repair of infrarenal abdominal aortic aneurysms: a prospective, non-randomized comparative study. Eur J Vasc Endovasc Surg. 2008;35(4):422–8.
Starnes BW, Andersen CA, Ronsivalle JA, Stockmaster NR, Mullenix PS, Statler JD. Totally percutaneous aortic aneurysm repair: experience and prudence. J Vasc Surg. 2006;43(2):270–6.
Quinn SF, Kim J. Percutaneous femoral closure following stent-graft placement: use of the Perclose device. Cardiovasc Intervent Radiol. 2004;27(3):231–6.
Morasch MD, Kibbe MR, Evans ME, et al. Percutaneous repair of abdominal aortic aneurysm. J Vasc Surg. 2004;40(1):12–6.
Rachel ES, Bergamini TM, Kinney EV, Jung MT, Kaebnick HW, Mitchell RA. Percutaneous endovascular abdominal aortic aneurysm repair. Ann Vasc Surg. 2002;16(1):43–9.
Teh LG, Sieunarine K, van Schie G, et al. Use of the percutaneous vascular surgery device for closure of femoral access sites during endovascular aneurysm repair: lessons from our experience. Eur J Vasc Endovasc Surg. 2001;22(5):418–23.
Howell M, Doughtery K, Strickman N, Krajcer Z. Percutaneous repair of abdominal aortic aneurysms using the AneuRx stent graft and the percutaneous vascular surgery device. Catheter Cardiovasc Interv. 2002;55(3):281–7.
Traul DK, Clair DG, Gray B, O’Hara PJ, Ouriel K. Percutaneous endovascular repair of infrarenal abdominal aortic aneurysms: a feasibility study. J Vasc Surg. 2000;32(4):770–6.
Carrafiello G, Recaldini C, Lagana D, Piffaretti G, Fugazzola C. Endoleak detection and classification after endovascular treatment of abdominal aortic aneurysm: value of CEUS over CTA. Abdom Imaging. 2008;33(3):357–62.
Iezzi R, Basilico R, Giancristofaro D, Pascali D, Cotroneo AR, Storto ML. Contrast-enhanced ultrasound versus color duplex ultrasound imaging in the follow-up of patients after endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2009;49(3):552–60.
Back MR. Surveillance after endovascular abdominal aortic aneurysm repair. Perspect Vasc Surg Endovasc Ther. 2007;19(4):395–400; discussion 401–2.
Springer F, Gunther RW, Schmitz-Rode T. Aneurysm Sac pressure measurement with minimally invasive implantable pressure sensors: an alternative to current surveillance regimes after EVAR? Cardiovasc Intervent Radiol. 2008;31(3):460–7.
Ohki T, Ouriel K, Silveira PG, et al. Initial results of wireless pressure sensing for endovascular aneurysm repair: the APEX Trial–Acute Pressure Measurement to Confirm Aneurysm Sac EXclusion. J Vasc Surg. 2007;45(2):236–42.
Propanolol Aneurysm Trial Investigators. Propranolol for small abdominal aortic aneurysms: results of a randomized trial. J Vasc Surg. 2002;35(1):72–9.
Lindholt JS, Vammen S, Juul S, Henneberg EW, Fasting H. The validity of ultrasonographic scanning as screening method for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 1999;17(6):472–5.
Gotto Jr AM. Role of C-reactive protein in coronary risk reduction: focus on primary prevention. Am J Cardiol. 2007;99(5):718–25.
Evans J, Powell JT, Schwalbe E, Loftus IM, Thompson MM. Simvastatin attenuates the activity of matrix metalloprotease-9 in aneurysmal aortic tissue. Eur J Vasc Endovasc Surg. 2007;34(3):302–3.
Nagashima H, Aoka Y, Sakomura Y, et al. A 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, cerivastatin, suppresses production of matrix metalloproteinase-9 in human abdominal aortic aneurysm wall. J Vasc Surg. 2002;36(1):158–63.
Schouten O, van Laanen JH, Boersma E, et al. Statins are associated with a reduced infrarenal abdominal aortic aneurysm growth. Eur J Vasc Endovasc Surg. 2006;32(1):21–6.
Sukhija R, Aronow WS, Sandhu R, Kakar P, Babu S. Mortality and size of abdominal aortic aneurysm at long-term follow-up of patients not treated surgically and treated with and without statins. Am J Cardiol. 2006;97(2):279–80.
Baxter BT, Pearce WH, Waltke EA, et al. Prolonged administration of doxycycline in patients with small asymptomatic abdominal aortic aneurysms: report of a prospective (Phase II) multicenter study. J Vasc Surg. 2002;36(1):1–12.
Prall AK, Longo GM, Mayhan WG, et al. Doxycycline in patients with abdominal aortic aneurysms and in mice: comparison of serum levels and effect on aneurysm growth in mice. J Vasc Surg. 2002;35(5):923–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag London
About this chapter
Cite this chapter
White, L.E., Hassoun, H.T. (2012). Infrarenal Aortic Aneurysms: New Technologies. In: Hoballah, J., Lumsden, A. (eds) Vascular Surgery. New Techniques in Surgery Series, vol 6. Springer, London. https://doi.org/10.1007/978-1-4471-2912-7_1
Download citation
DOI: https://doi.org/10.1007/978-1-4471-2912-7_1
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-2911-0
Online ISBN: 978-1-4471-2912-7
eBook Packages: MedicineMedicine (R0)