Abstract
The choice between an open surgical and an endovascular approach for abdominal aortic aneurysm (AAA) repair remains an individualized clinical decision. As the technology and applications of endovascular aortic aneurysm repair (EVAR) continue to evolve, so does the literature investigating its outcomes. Multiple high-quality, randomized controlled trials comparing EVAR to open surgical repair (OSR) have now been published with long-term follow-up. Experience with ruptured aneurysms and the use of complex endografts is growing as well. This review is an up-to-date compilation of pertinent clinical trials for practitioners placed in the context of individual patient considerations to guide the choice of an optimal approach to the management of AAAs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The surgical approach to aneurysmal disease has changed radically since Parodi’s first report of endovascular aortic aneurysm repair (EVAR) [1]. Reports of early experience with EVAR included significant complications but showed promise to eventually supplant open surgical repair (OSR) in appropriately selected patients [2, 3]. In the two decades since its introduction, EVAR has become widely popularized. In the USA, three quarters of elective abdominal aortic aneurysm (AAA) repairs are now performed via an endovascular approach [4]. Despite the growth in popularity of EVAR, the decision between surgical and endovascular repair is individualized based on anatomic considerations accompanying the aneurysm and its accessibility for repair, comorbidities that may further impact the risks of either approach, and patient preferences regarding follow-up and potential for complications. High-quality evidence exists to guide practitioners and patients in choosing the optimal approach. This article seeks to summarize the most up-to-date evidence comparing OSR to EVAR. This includes comparisons of both elective and ruptured aneurysm repair. We also discuss the latest evidence addressing treatment of complex abdominal aneurysms utilizing branched or fenestrated endografts.
Elective Repair of Infrarenal AAA (Standard EVAR versus Open Surgical Repair)
The common indications for elective repair of AAA are to prevent rupture or to eliminate symptoms attributed to the aneurysm. In the preoperative evaluation of a patient for AAA repair, the expected morbidity and mortality of the operative intervention are weighed against the risk of rupture and other impact upon quality of life the aneurysm carries when recommending repair. The evidence comparing EVAR to OSR for multiple clinical considerations is summarized in this section.
Size
The generally accepted size threshold for repair is greater than 5.4 cm or expansion greater than 1 cm in 12 months [5]. This was established for open repair by the United Kingdom Small Aneurysm Trial (UKSAT) and the Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative study. These studies randomized patients with aneurysms between 4.0 and 5.4 cm to immediate OSR versus surveillance and found no statistical difference in long-term survival [6–8]. Two additional trials, the Comparison of Surveillance versus Endografting for Small Aneurysm Repair (CAESAR) and Positive Impact of Endovascular Options for Treating Aneurysm Early (PIVOTAL) trials demonstrated similar results for EVAR as compared to the open repair results described above, despite the lower perioperative mortality of EVAR [9, 10]. A systematic Cochrane review of these trials showed no advantage to immediate repair for aneurysms 4.0–5.4 cm when pooled analysis was performed [11]. A practical limitation of the trial data pertinent to clinicians is that it includes a low proportion of women and non-white individuals, while there are data to suggest women may be at greater risk for rupture [12, 13]. Fillardo and colleagues demonstrated no difference in survival when the UKSAT and ADAM trial participants were combined and assessed via proportional hazard models that accounted for gender and AAA size [14]. Unfortunately, the EVAR trials lack the long-term follow-up of the OSR trials and are underpowered to detect differences by age subgroup or differences in AAA size within the 4.0–5.4 cm range. Thus, the existing data favor surveillance over early repair, particularly for open repair. However, some uncertainty exists given risk of early rupture in women, making repair >5.0 cm acceptable [15].
Anatomic Considerations
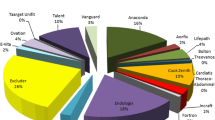
If a patient’s aneurysm meets criteria for repair because of size or symptoms, anatomic considerations guide the operative planning. Some considerations are of particular importance for determining eligibility for EVAR. The first criterion assessed is aortic neck characteristics, including diameter, length, and angulation. A proximal landing zone of 1.0–1.5 cm with less than 60° of angulation is generally required for the majority of currently available devices. The vessel caliber, presence of calcific disease, tortuosity and presence of aneurysmal disease in the iliac arteries also determine the choice of endograft and technical challenges with the approach. Endografts are sized and FDA approved for various neck diameters as well as native iliac diameters, as demonstrated in Table 1.
Perioperative and Long-Term Outcomes
In patients anatomically appropriate for EVAR, the perioperative morbidity and mortality as well as the rate of long-term complications as compared to OSR should be taken into account when planning the operative approach. There are four large randomized controlled trials comparing EVAR to OSR that provide the best basis for this discussion with patients. The Dutch Randomised Endovascular Aneurysm Management (DREAM) trial [25, 26], the Anevrysme de l’aorte abdominale: Chirurgie versus Endoprothese (ACE) trial [27], the U.K. Endovascular Aneurysm Repair 1 trial (EVAR1) [28–30], and the Open Versus Endovascular Repair (OVER) Veterans Affairs Cooperative study [31, 32] all demonstrated decreased short-term mortality for EVAR compared with OSR, similar rates of intermediate and long-term survival, and increased re-intervention rates during follow-up for EVAR. The trials are detailed in Table 2. A systematic review of these studies confirms the major findings in a pooled analysis with similar rates between EVAR and OSR for cardiac death (RR = 1.13, 95 % CI = 0.87–1.46, p = 0.36) and fatal stroke (RR = 0.91, 95 % CI = 0.49–1.72, p = 0.79); OSR resulted in slightly higher pulmonary complication rates (RR = 2.67, 95 % CI = 1.31–5.42, p = 0.001) [33•]. A large propensity-score-matched cohort study of 39,996 paired Medicare beneficiaries from 2001 to 2008 demonstrated an improving trend of complications related to EVAR across this time interval [34••]. Notably, mortality decreased by 0.8 % (p = 0.001), open conversions decreased from 2.2 to 0.3 % (p < 0.001), and re-intervention rates at 2 years decreased from 10.4 to 9.1 % (p < 0.001) [34••]. Perioperative mortality remained lower in EVAR patients (1.6 versus 5.2 % in OSR, p < 0.001) with a difference persisting until the third postoperative year; however, EVAR was associated with a higher risk of late aneurysm rupture after repair (5.4 versus 1.4 % in OSR, p < 0.001) [34••]. This study provides evidence of the improving outcomes with EVAR in a large database while also confirming the findings of the trial data.
Follow-Up/Ultrasound Surveillance
Both EVAR and OSR are associated with long-term complications that can require re-intervention. Some of these present clinically and would be difficult to reduce with routine surveillance; these include incisional complications, graft infections, graft occlusions, and formation of aortoenteric fistula. Complications from the repair associated with aneurysmal enlargement that predispose to a complication of late rupture are routinely diagnosed and followed with imaging to determine the need for re-intervention. In OSR, para-anastomotic aneurysm development is evaluated with non-contrast CT at 5-year intervals after OSR [15]. Compared to OSR, EVAR requires more rigorous follow-up in the absence of clinically apparent complications to evaluate for endoleak, graft migration, or evidence of device failure. Initial surveillance practice included obtaining a contrast-enhanced CT at 1 month, 6 months, 1 year, and annually thereafter [35]. The exposure to radiation, potential for contrast-associated injury, and cost of this surveillance raised significant concerns. Fortunately, experience with the use of color duplex ultrasonography (CDU) has suggested that CDU is an acceptable alternative means for surveillance in the absence of findings of endoleak or aneurysmal enlargement [36–38]. Additionally, CT at the 6-month postoperative time point is now only recommended if abnormalities are detected on the initial 1-month CT [39]. The frequency of surveillance and possibility for re-intervention can impact patient preference for the type of repair. Younger patients who would be subjected to a high frequency of follow-up or patients who may otherwise have difficulty with adherence to the recommended follow-up may prefer an open approach.
Elective Repair of Complex or Inflammatory AAA
Approximately 15 % of AAAs originate in close proximity to the renal arteries and require suprarenal aortic cross-clamping during open repair; these are termed juxtarenal aortic aneurysms [40]. This class of aneurysms is associated with an increased risk of perioperative morbidity and mortality, especially postoperative renal dysfunction, secondary to unavoidable renal and/or visceral ischemia from aortic cross-clamping as well as technical challenges of the surgical dissection when compared to infrarenal aneurysms [41]. Similar to OSR, treatment of this class of aneurysms with EVAR presents unique technical challenges requiring advanced technology to obtain aneurysm coverage by the endograft without endoleak while maintaining flow to the renal and visceral arteries. The development of endografts with fenestrations or branched stents and early experience in patients deemed at high risk for open repair has paved the way for treatment of increasingly complex aneurysms via an endovascular approach [42]. These devices were initially custom-made with a manufacturing period of several weeks, but there is growing experience with commercially available “off the shelf” endografts with excellent technical success [43].
Comparisons of Complex EVAR with OSR
Unfortunately, no randomized data exists comparing fenestrated or branched stent EVAR (FEVAR) and OSR; however, publications of experience with FEVAR are increasing. The GLOBALSTAR registry in the UK provided nationwide data on the early experience with FEVAR quoting a 99 % likelihood of primary procedure technical success, 7 % rate of 30-day re-intervention, and an associated 4.1 % perioperative mortality [44]. In 2015, Rao and colleagues published a systematic review and meta-analysis examining 35 existing case series of OSR and fenestrated EVAR (FEVAR) totaling 2326 patients (751 FEVAR, 1575 OSR) since 1990 [45•]. The review demonstrated no significant difference in short-term survival for FEVAR versus OSR (4.1 % for both, p = 0.82) or postoperative renal dysfunction (11.4 versus 13.9 % OSR, p = 0.54); however, FEVAR had higher rates of secondary re-intervention (12.7 versus 4.9 % in OSR, p < 0.001), progression to renal failure (19.7 versus 7.7 % in OSR, p < 0.001) during the 1–5-year follow-up periods from included series, and a decreased 5-year survival (55 versus 73 % in OSR, p = 0.09) in series with sufficient follow-up [44]. The review’s comparisons are limited by significant heterogeneity in the series included. Moreover, FEVAR patients were 5 years older on average, with higher frequencies of preoperative renal impairment, diabetes, as well as cardiopulmonary disease, reflective of FEVAR’s initial use in patients deemed high risk for OSR [45•]. A prospective multicenter registry (WINDOW registry) from France demonstrated a 6.7 % 30-day mortality rate, 10.1 % in-hospital mortality rate, and 22 % combined rate of mortality or severe complication defined as renal failure, spinal cord ischemia, or re-intervention within 30 days for FEVAR [46]. When the WINDOW registry was compared to a matched control group of OSR patients extracted from a national hospital database, there was no difference in 30-day mortality and a lower rate of permanent hemodialysis for FEVAR (5.6 versus 20.8 % in OSR, p < 0.001); FEVAR was associated with a higher rate of paraplegia (4.1 versus 1.0 % in OSR, p < 0.001), myocardial infarction (3.1 versus 1.2 % in OSR, p = 0.019), stroke (4.2 versus 0.7 % in OSR, p < 0.001), and re-interventions in the first 30-days (15.3 versus 10.3 % in OSR, p = 0.017) [47]. However, it should be noted that the patients receiving FEVAR were deemed to be at high risk for OSR and different methodologies were used to evaluate clinical outcomes in the registry versus the control database, which may importantly bias the results [48]. A retrospective analysis of well-matched patients with complex AAAs taken from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database between 2005 and 2010 included 1091 OSR and 264 FEVAR patients; the study demonstrated FEVAR had lower 30-day mortality (0.8 versus 5.4 % in OSR, p = 0.001), significantly lower rates of renal complications (1.5 versus 9.9 % in OSR, p < 0.001), pulmonary complications (2.3 versus 21.3 % in OSR, p < 0.001), and cardiovascular complications (1.9 versus 7.4 % in OSR, p = 0.001), as well as a 1-week decreased length of stay (p < 0.001), when compared to OSR [49]. The above studies represent the initial publications within an evolving area of investigation and should be interpreted with great caution. Taken collectively, the studies demonstrate that complex EVAR can be performed with adequate technical results and with similar or lower 30-day mortality when compared to OSR. However, long-term follow-up and data on re-interventions are lacking. The NSQIP data stands in contrast to the other studies in suggesting lower morbidity for FEVAR, presumably due to the high-risk population included in studies of FEVAR from Europe.
Inflammatory Aneurysms
Another important category of aneurysms, which accounts for 5–10 % of patients with AAA, is the inflammatory aneurysm (IAAA) [50]. These aneurysms have a characteristic perianeurysmal fibrosis that is often adherent to surrounding bowel, renal vessels, or ureter and makes the dissection in OSR technically challenging, with a higher incidence of perioperative complications [51]. For this reason, EVAR is the recommended approach for these aneurysms in the Society for Vascular Surgery practice guidelines [15]. A recent retrospective comparative study of OSR and EVAR in the Greek population by Kakkos and colleagues demonstrated lower rates of transfusion, operating times, and length of stay for EVAR but was underpowered to detect differences in morbidity and mortality given a 27 patient sample size [52]. Paravastu and colleagues performed the most recent large systemic review of existing data comparing approaches to IAAA in 2009; the study included 1020 patients (999 OSR, 121 EVAR) and demonstrated lower all-cause mortality at 1 year for EVAR (2 versus 14 % in OSR, p = 0.02) [53]. A recent Cochrane review highlighted the lack of randomized and prospective evidence for IAAA and called for studies to better characterize the perioperative and long-term complication rates [54].
Ruptured Aneurysm
Another important population of patients with AAA is those who present with rupture and require emergent repair. Yusuf and colleagues reported the first use of EVAR in a patient with a leaking AAA in 1994, drawing attention to the potential of a minimally invasive approach to improve outcomes in a population with a perioperative mortality approaching 50 % [55]. Since the initial report, the application of EVAR in the ruptured population has grown significantly and multiple randomized trials have been performed. The first trial was conducted at a single center in Nottingham, UK, between 2002 and 2004 and included 32 patients; the study was underpowered to detect differences in the study groups but nonetheless reported an equivalent 30-day mortality of 53 % percent in each group (RR = 1.01, 95 % CI = 0.52–1.93, p = 0.98) and greater than 75 % rates of moderate to severe postoperative complications in the two arms as well [56]. This trial laid the groundwork for three larger trials that have since followed. These trials are the Amsterdam Acute Aneurysm (AJAX) trial, the Endovasculaire versus Chirurgie dans les Anévrismes Rompus (ECAR) trial, and the Immediate Management of the Patient with Ruptured Aneurysm (IMPROVE) trial [57–59]. AJAX randomized 116 patients anatomically suitable for EVAR after CT scan between 2004 and 2011; there was no difference in the primary outcome of 30-day mortality (21 versus 25 % in OSR, p = 0.66) [57]. ECAR randomized 107 patients in a similar fashion between 2008 and 2012, also demonstrating no difference in the primary endpoint of 30-day mortality (18 versus 24 % in OSR, p = 0.47) [58]. IMPROVE randomized 613 patients between 2009 and 2013 to an endovascular versus open strategy at the time of clinical diagnosis of ruptured aneurysm and prior to CT scan; there was again no significant difference in 30-day mortality between the groups (36 versus 41 % in OSR strategy, p = 0.62) despite the difference in design and larger number of patients [59]. Pooled meta-analysis of the patients suitable for EVAR following the publication of the latest three trials demonstrated no survival difference between EVAR and OSR at 90 days (RR = 0.98, 95 % CI = 0.81–1.17, p = 0.78) and 1 year (RR = 0.84, 95 % CI = 0.63–1.11), p = 0.24) [60•, 61]. The trial data are in contrast to recent large-scale observational studies in the USA that suggest early mortality benefit of EVAR [62–64] but are supported by a review of the Swedish Vascular Registry [65]. The differences between observational and randomized data may be explained in part by a selection bias driven by short aneurysm necks, which will preclude standard EVAR and adversely impact outcomes of OSR as previously discussed [66]. While the initial reported data in ruptured aneurysms focused heavily on survival, the AJAX collaborators recently published 5-year observational data demonstrating a higher re-intervention rate for EVAR in patients who survive the initial hospital stay (33 versus 10 % in OSR, p < 0.01), similar to the difference in elective repair [67]. In summary, the randomized trial data in rupture differs from that of elective repair; there is no benefit seen in early mortality with EVAR when compared to OSR in patients who are candidates for both interventions. This makes both options acceptable and the approach will often be dependent on hospital capabilities and surgeon preference.
Conclusion
Selection of the optimal approach for aneurysm repair should remain an individualized clinical decision. Each aneurysm can present a unique combination of anatomic variation, clinical symptoms, associated comorbidities, and patient preference for consideration before a given intervention. Fortunately, there is a large body of evidence with a focus on meaningful clinical outcomes to guide practitioners in this process. Experience with complex EVAR will continue to grow and represent the next opportunity for high-quality prospective comparisons to open repair in an attempt to improve outcomes in these patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991;5(6):491–9.
Nasim A, Thompson MM, Sayers RD, Bolia A, Bell PR. Endovascular repair of abdominal aortic aneurysm: an initial experience. Br J Surg. 1996;83(4):516–9.
Edwards Jr WH, Naslund TC, Edwards Sr WH, Jenkins JM, McPherson K. Endovascular grafting of abdominal aortic aneurysms. A preliminary study. Ann Surg. 1996;223(5):568–75.
Kent KC. Clinical practice. Abdominal aortic aneurysms. N Engl J Med. 2014;371(22):2101–8.
Brewster DC, Cronenwett JL, Hallett Jr JW, Johnston KW, Krupski WC, Matsumura JS, et al. Guidelines for the treatment of abdominal aortic aneurysms. Report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery. J Vasc Surg. 2003;37(5):1106–17.
The UK Small Anuerysm Trial Participants. Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet. 1998;352(9141):1649–55.
Powell JT, Brown LC, Forbes JF, Fowkes FG, Greenhalgh RM, Ruckley CV, et al. Final 12-year follow-up of surgery versus surveillance in the UK Small Aneurysm Trial. Br J Surg. 2007;94(6):702–8.
Lederle FA, Wilson SE, Johnson GR, Reinke DB, Littooy FN, Acher CW, et al. Immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002;346(19):1437–44.
Cao P, De Rango P, Verzini F, Parlani G, Romano L, Cieri E, et al. Comparison of surveillance versus aortic endografting for small aneurysm repair (CAESAR): results from a randomised trial. Eur J Vasc Endovasc Surg. 2011;41(1):13–25.
Ouriel K, Clair DG, Kent KC, Zarins CK, Positive Impact of Endovascular Options for treating Aneurysms Early (PIVOTAL) Investigators. Endovascular repair compared with surveillance for patients with small abdominal aortic aneurysms. J Vasc Surg. 2010;51(5):1081–7.
Filardo G, Powell JT, Martinez MA, Ballard DJ. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2015;2:CD001835.
Brown PM, Zelt DT, Sobolev B. The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J Vasc Surg. 2003;37(2):280–4.
Lo RC, Bensley RP, Hamdan AD, Wyers M, Adams JE, Schermerhorn ML, et al. Gender differences in abdominal aortic aneurysm presentation, repair, and mortality in the Vascular Study Group of New England. J Vasc Surg. 2013;57(5):1261–8. 1268.e1-5.
Filardo G, Lederle FA, Ballard DJ, Hamilton C, da Graca B, Herrin J, et al. Immediate open repair vs surveillance in patients with small abdominal aortic aneurysms: survival differences by aneurysm size. Mayo Clin Proc. 2013;88(9):910–9.
Chaikof EL, Brewster DC, Dalman RL, Makaroun MS, Illig KA, Sicard GA, et al. The care of patients with an abdominal aortic aneurysm: the Society for Vascular Surgery practice guidelines. J Vasc Surg. 2009;50(4 Suppl):S2–49.
Makaroun MS. The Ancure endografting system: an update. J Vasc Surg. 2001;33(2 Suppl):S129–34.
Peterson BG, Matsumura JS, Brewster DC, Makaroun MS, Excluder Bifurcated Endoprosthesis Investigators. Five-year report of a multicenter controlled clinical trial of open versus endovascular treatment of abdominal aortic aneurysms. J Vasc Surg. 2007;45(5):885–90.
Mertens J, Houthoofd S, Daenens K, Fourneau I, Maleux G, Lerut P, et al. Long-term results after endovascular abdominal aortic aneurysm repair using the Cook Zenith endograft. J Vasc Surg. 2011;54(1):48–57.
Qu L, Raithel D. From clinical trials to clinical practice: 612 cases treated with the Powerlink stent-graft for endovascular repair of AAA. J Cardiovasc Surg (Torino). 2009;50(2):131–7.
Criado FJ, Wilson EP, Fairman RM, Abul-Khoudoud O, Wellons E. Update on the Talent aortic stent-graft: a preliminary report from United States phase I and II trials. J Vasc Surg. 2001;33(2 Suppl):S146–9.
van Keulen JW, de Vries JP, Dekker H, Gonçalves FB, Moll FL, Verhagen HJ, et al. One-year multicenter results of 100 abdominal aortic aneurysm patients treated with the Endurant stent graft. J Vasc Surg. 2011;54(3):609–15.
Trellopoulos G, Georgakarakos E, Pelekas D, Papachristodoulou A, Kalaitzi A, Asteri T. Initial single-center experience with the Ovation stent-graft system in the treatment of abdominal aortic aneurysms: application to challenging iliac access anatomies. Ann Vasc Surg. 2015;29(5):913–9.
Oderich GS, Greenberg RK, Farber M, Lyden S, Sanchez L, Fairman R, et al. Results of the United States multicenter prospective study evaluating the Zenith fenestrated endovasculargraft for treatment of juxtarenal abdominal aortic aneurysms. J Vasc Surg. 2014;60(6):1420–8.
Sbarzaglia P, Grattoni C, Oshoala K, Castriota F, D’Alessandro G, Cremonesi A. Aorfix™ device for abdominal aortic aneurysm with challenging anatomy. J Cardiovasc Surg (Torino). 2014;55(1):61–70.
Blankensteijn JD, de Jong SE, Prinssen M, van der Ham AC, Buth J, van Sterkenburg SM, et al. Two-year outcomes after conventional or endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2005;352(23):2398–405.
De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, Cuypers PW, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1881–9.
Becquemin JP, Pillet JC, Lescalie F, Sapoval M, Goueffic Y, Lermusiaux P, et al. A randomized controlled trial of endovascular aneurysm repair versus open surgery for abdominal aortic aneurysms in low- to moderate-risk patients. J Vasc Surg. 2011;53(5):1167–1173.e1.
Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG, EVAR trial participants. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet. 2004;364(9437):843–8.
United Kingdom EVAR Trial Investigators, Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D, et al. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1863–71.
Brown LC, Thompson SG, Greenhalgh RM, Powell JT, Endovascular Aneurysm Repair trial participants. Incidence of cardiovascular events and death after open or endovascular repair of abdominal aortic aneurysm in the randomized EVAR trial 1. Br J Surg. 2011;98(7):935–42.
Lederle FA, Freischlag JA, Kyriakides TC, Matsumura JS, Padberg Jr FT, Kohler TR, et al. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med. 2012;367(21):1988–97.
Lederle FA, Freischlag JA, Kyriakides TC, Padberg Jr FT, Matsumura JS, Kohler TR, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302(14):1535–42.
• Paravastu SC, Jayarajasingam R, Cottam R, Palfreyman SJ, Michaels JA, Thomas SM. Endovascular repair of abdominal aortic aneurysm. Cochrane Database Syst Rev. 2014;1:CD004178. Systematic review of the trials comparing standard EVAR with OSR.
•• Schermerhorn ML, Buck DB, O’Malley AJ, Curran T, McCallum JC, Darling J, et al. Long-term outcomes of abdominal aortic aneurysm in the Medicare population. N Engl J Med. 2015;373(4):328–38. Medicare level data on EVAR that demonstrates improving long-term outcomes as experience with this technique improves.
Sapirstein W, Chandeysson P, Wentz C. The Food and Drug Administration approval of endovascular grafts for abdominal aortic aneurysm: an 18-month retrospective. J Vasc Surg. 2001;34(1):180–3.
Tomlinson J, McNamara J, Matloubieh J, Hart J, Singh MJ, Davies MG, et al. Intermediate follow-up after endovascular aneurysm repair: can we forgo CT scanning in certain patients? Ann Vasc Surg. 2007;21(6):663–70.
Sternbergh WC, Greenberg RK, Chuter TA, Tonnessen BH. Redefining postoperative surveillance after endovascular aneurysm repair: recommendations based on 5-year follow-up in the US Zenith multicenter trial. J Vasc Surg. 2008;48(2):278–84.
Chaer RA, Gushchin A, Rhee R, Marone L, Cho JS, Leers S, et al. Duplex ultrasound as the sole long-term surveillance method post-endovascular aneurysm repair: a safe alternative for stable aneurysms. J Vasc Surg. 2009;49(4):845–50.
Go MR, Barbato JE, Rhee RY, Makaroun MS. What is the clinical utility of a 6-month computed tomography in the follow-up of endovascular aneurysm repair patients? J Vasc Surg. 2008;47(6):1181–87.
Jongkind V, Yeung KK, Akkersdijk GJ, Heidsieck D, Reitsma JB, Tangelder GJ, et al. Juxtarenal aortic aneurysm repair. J Vasc Surg. 2010;52(3):760–7.
Sarac TP, Clair DG, Hertzer NR, Greenberg RK, Krajewski LP, O’Hara PJ, et al. Contemporary results of juxtarenal aneurysm repair. J Vasc Surg. 2002;36(6):1104–11.
Chuter TA. Fenestrated and branched stent-grafts for thoracoabdominal, pararenal and juxtarenal aortic aneurysm repair. Semin Vasc Surg. 2007;20(2):90–6.
Farber MA, Vallabhaneni R, Marston WA. “Off-the-shelf” devices for complex aortic aneurysm repair. J Vasc Surg. 2014;60(3):579–84.
British Society for Endovascular Therapy and the Global Collaborators on Advanced Stent-Graft Techniques for Aneurysm Repair (GLOBALSTAR) Registry. Early results of fenestrated endovascular repair of juxtarenal aortic aneurysms in the United Kingdom. Circulation. 2012;125(22):2707–15.
• Rao R, Lane TR, Franklin IJ, Davies AH. Open repair versus fenestrated endovascular aneurysm repair of juxtarenal aneurysms. J Vasc Surg. 2015;61(1):242–55. The largest analysis of observational data in FEVAR which will form the basis for future prospective data comparing open and endovascular repair of juxtarenal aneurysms.
Marzelle J, Presles E, Becquemin JP, WINDOWS trial participants. Results and factors affecting early outcome of fenestrated and/or branched stent grafts for aortic aneurysms: a multicenter prospective study. Ann Surg. 2015;261(1):197–206.
Michel M, Becquemin JP, Clément MC, Marzelle J, Quelen C, Durand-Zaleski I, et al. Editor’s choice—thirty day outcomes and costs of fenestrated and branched stent grafts versus open repair for complex aortic aneurysms. Eur J Vasc Endovasc Surg. 2015;50(2):189–96.
Ricco JB, Schneider F. Commentary on ‘thirty day outcomes and costs of fenestrated and branched stent grafts versus open repair for complex aortic aneurysms’: an innovative but expensive tool requiring further evaluation. Eur J Vasc Endovasc Surg. 2015;50(2):197–8.
Tsilimparis N, Perez S, Dayama A, Ricotta 2nd JJ. Endovascular repair with fenestrated-branched stent grafts improves 30-day outcomes for complex aortic aneurysms compared with open repair. Ann Vasc Surg. 2013;27(3):267–73.
Pennell RC, Hollier LH, Lie JT, Bernatz PE, Joyce W, Pairolero PC, et al. Inflammatory abdominal aortic aneurysms: a thirty-year review. J Vasc Surg. 1985;2(6):859–69.
Nitecki SS, Hallett Jr JW, Stanson AW, Ilstrup DM, Bower TC, Cherry Jr KJ, et al. Inflammatory abdominal aortic aneurysms: a case–control study. J Vasc Surg. 1996;23(5):860–9.
Kakkos SK, Papazoglou KO, Tsolakis IA, Lampropoulos G, Papadoulas SI, Antoniadis PN. Open versus endovascular repair of inflammatory abdominal aortic aneurysms: a comparative study and meta-analysis of the literature. Vasc Endovasc Surg. 2015;49(5–6):110–8.
Paravastu SC, Ghosh J, Murray D, Farquharson FG, Serracino-Inglott F, Walker MG. A systematic review of open versus endovascular repair of inflammatory abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2009;38(3):291–7.
Capoccia L, Riambau V. Endovascular repair versus open repair for inflammatory abdominal aortic aneurysms. Cochrane Database Syst Rev. 2015;4:CD010313.
Yusuf SW, Whitaker SC, Chuter TA, Wenham PW, Hopkinson BR. Emergency endovascular repair of leaking aortic aneurysm. Lancet. 1994;344(8937):1645.
Hinchliffe RJ, Bruijstens L, MacSweeney ST, Braithwaite BD. A randomised trial of endovascular and open surgery for ruptured abdominal aortic aneurysm—results of a pilot study and lessons learned for future studies. Eur J Vasc Endovasc Surg. 2006;32(5):506–15.
Reimerink JJ, Hoornweg LL, Vahl AC, Wisselink W, van den Broek TA, Legemate DA, et al. Endovascular repair versus open repair of ruptured abdominal aortic aneurysms: a multicenter randomized controlled trial. Ann Surg. 2013;258(2):248–56.
Desgranges P, Kobeiter H, Katsahian S, Bouffi M, Gouny P, Favre JP, et al. Editor’s Choice—ECAR (Endovasculaire ou Chirurgie dans les Anévrysmes aorto-iliaques Rompus): a French randomized controlled trial of endovascular versus open surgical repair of ruptured aorto-iliac aneurysms. Eur J Vasc Endovasc Surg. 2015;50(3):303–10.
IMPROVE Trial Investigators, Powell JT, Sweeting MJ, Thompson MM, Ashleigh R, Bell R, et al. Endovascular or open repair strategy for ruptured abdominal aortic aneurysm: 30 day outcomes from IMPROVE randomised trial. BMJ. 2014;348:f7661.
• Sweeting MJ, Balm R, Desgranges P, Ulug P, Powell JT, Ruptured Aneurysm Trialists. Individual-patient meta-analysis of three randomized trials comparing endovascular versus open repair for ruptured abdominal aortic aneurysm. Br J Surg. 2015;102(10):1229–39. Recent individual patient level meta-analysis of the ruptured aneurysm trials.
Sweeting MJ, Ulug P, Powell JT, Desgranges P, Balm R, Ruptured Aneurysm Trialists. Ruptured aneurysm trials: the importance of longer-term outcomes and meta-analysis for 1-year mortality. Eur J Vasc Endovasc Surg. 2015;50(3):297–302.
Edwards ST, Schermerhorn ML, O’Malley AJ, Bensley RP, Hurks R, Cotterill P, et al. Comparative effectiveness of endovascular versus open repair of ruptured abdominal aortic aneurysm in the Medicare population. J Vasc Surg. 2014;59(3):575–82.
Speicher PJ, Barbas AS, Mureebe L. Open versus endovascular repair of ruptured abdominal aortic aneurysms. Ann Vasc Surg. 2014;28(5):1249–57.
Park BD, Azefor N, Huang CC, Ricotta JJ. Trends in treatment of ruptured abdominal aortic aneurysm: impact of endovascular repair and implications for future care. J Am Coll Surg. 2013;216(4):745–55.
Gunnarsson K, Wanhainen A, Djavani Gidlund K, Björck M, Mani K. Endovascular versus open repair as primary strategy for ruptured abdominal aortic aneurysm: a national population-based study. Eur J Vasc Endovasc Surg. 2016;51(1):22–8.
IMPROVE Trial Investigators. The effect of aortic morphology on peri-operative mortality of ruptured abdominal aortic aneurysm. Eur Heart J. 2015;36(21):1328–34.
van Beek SC, Vahl A, Wisselink W, Reekers JA, Legemate DA, Balm R, et al. Midterm re-interventions and survival after endovascular versus open repair for ruptured abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2015;49(6):661–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Theodore Hart declares no conflict of interest.
Ross Milner declares to have done consulting for Cook Medical, Endospan, Medtronic, and WL Gore.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Clinical Trials and Their Interpretations
Rights and permissions
About this article
Cite this article
Hart, T., Milner, R. Surgical Versus Endovascular Aortic Aneurysm Repair: Evidence to Guide the Optimal Approach for the Individual Patient. Curr Atheroscler Rep 18, 76 (2016). https://doi.org/10.1007/s11883-016-0621-2
Published:
DOI: https://doi.org/10.1007/s11883-016-0621-2