Abstract
Since the first use of insulin 100 years ago, there have been marked improvements in diabetes therapy including, but not limited to, the development of oral antidiabetic agents (OADs), incretin mimetics and insulin analogues. Still, there are substantial shortcomings in diabetes therapy: the blood-glucose lowering effect of OADs is often limited, incretin mimetics often induce gastrointestinal side effects and insulins still induce hypoglycaemia and weight gain in many patients.
This review evaluates on-going developments of antidiabetic drugs for their potential for future therapy focussing on injectable therapies. Recent data from dual agonists, in particular tirzepatide, a combination of GIP- and GLP-1 receptor agonists, show unprecedented reductions in HbA1c, body weight and cardiovascular risk factors. Once-weekly administrations of incretin mimetics open up the potential of a combination with once-weekly insulins that have been shown to have low peak-to-trough fluctuations. Eventually, it might be feasible to administer incretins and insulins (combinations) orally. While this has already been achieved for incretins, there are still some challenges for the oral application of insulin. Nevertheless, many promising data of novel antidiabetic drugs clearly indicate that therapy of people with diabetes will become easier, safer and more efficacious in the next years.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Pharmacological diabetes therapy started with the first use of insulin 100 years ago. Since then, there have been quite a number of additions to the therapeutic armamentarium, such as oral antidiabetic agents (OADs) and incretin mimetics. Notably, SGLT-2 inhibitors and GLP-1 receptor agonists have been shown to reduce the excess cardiovascular risk of people with diabetes compared to non-diabetic people (Buse et al. 2020). The insulin molecule itself and insulin formulations have also been optimised for therapeutic use, e.g., by purification of insulin formulations reducing antibody formation, by adding mechanisms to slow down insulin absorption for basal insulin coverage and by modifications to accelerate insulin absorption for prandial insulin therapy (Home 2021; Heise 2021a).
Nevertheless, there are still major shortcomings in diabetes therapy. OADs often have limited blood-glucose lowering properties or are associated with side effects including hypoglycaemia and body weight gain. The therapeutic potential of incretin mimetics can often not fully exploited because of gastrointestinal side effects (Hayes et al. 2021). Despite all refinements, insulin formulations are still associated with the highest risk of hypoglycaemia among all available antidiabetic therapies, in particular in people with type 1 diabetes and long-standing type 2 diabetes (UK Hypoglycaemia Study Group 2007). In addition, the rather inconvenient subcutaneous route of administration (which also applies to most incretin mimetics) in combination with adverse effects like body weight gain and other psychosocial factors makes many patients and clinicians reluctant to initiate insulin therapy (Khunti and Millar-Jones 2017).
Looking at the growing number of patients with diabetes and the still unsatisfactory control in many patients (Kazemian et al. 2019), there is a clear unmet need for novel drugs facilitating and improving diabetes therapy. This review will describe some on-going developments of blood-glucose lowering drugs focussing on injectables. Indeed, there are a number of promising developments on-going for incretin mimetics with even higher efficacy, in particular dual combinations of either glucose-dependent insulin releasing polypeptide (GIP) or glucagon receptor agonists and glucagon-like peptide-1 (GLP-1) mimetics. Likewise, first data have been provided for improved insulin formulations, making insulin initiation easier and reducing undesired side effects of insulin therapy. These include but are not limited to insulin for once-weekly application and orally administered insulins. These two insulin developments seem to be the most promising, not only because they have already entered at least phase 2 of the clinical development stage, but also because they could possibly be combined with incretin mimetics or incretin combinations.
In contrast, other insulin developments such as hepato-preferential insulin primarily acting on the liver or glucose-responsive insulins that only act when blood glucose levels are high are still in early development stage with only few clinical data available that mostly show the high challenges that have to still to be overcome for these developments (Heise 2021a).
Likewise, there do not seem to be too many oral agents in late-stage development that might enter the diabetes market soon (Bailey and Day 2018). Small molecule agonists of G-protein-coupled fatty acid receptors GPR40 and GPR119 have been shown to increase insulin secretion or decrease glucagon secretion, but have not entered late-stage clinical developments yet or have been discontinued due to hepatic side effects (Bailey and Day 2018). Glucokinase activators are very potent insulin secretion enhancers that, however, often lead to hypoglycaemia and also show tachyphylaxis (Nakamura and Terauchi 2015). The development of other oral drug candidates, such as inhibitors of the 11ß-hydroxysteroid-dehydrogenase, were stopped because of lack of efficacy (Bailey and Day 2018; Bianzano et al. 2021).
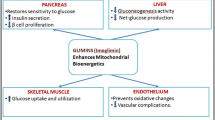
Currently, the only OAD in late-stage development seems to be imeglimin, a tetrahydrotriazine-containing compound that improves both insulin secretion and insulin action due to modulation of mitochondrial function according to a recent review co-authored by staff of Poxel, the manufacturer of imeglimin (Hallakou-Bozec et al. 2021). Imeglimin has been approved in Japan, but not yet in the EU or the USA. Phase 2b and phase 3 clinical trials with 74–107 patients per arm showed good tolerability and an HbA1c-lowering effect of about 0.9% with 1,000 mg imeglimin versus placebo (Dubourg et al. 2021a, b). There were no differences with regard to body weight. Full publications with active comparators have not yet been provided. Most importantly, there are no cardiovascular outcome data available for imeglimin, and it has to be applied twice daily in contrast to SGLT-2 inhibitors that are mostly applied once daily. Due to these limitations, a wide-spread use of imeglimin seems unlikely in view of the competition with SGLT-2 inhibitors with proven cardiovascular benefits.
2 GLP-1 Receptor Co-agonists
2.1 Background
Undoubtedly, GLP-1 mimetics have substantially changed diabetes therapy. Robust improvements in both glycaemic control and body weight in combination with proven cardiovascular benefits have moved GLP-1 mimetics to the first-line injectable antidiabetic therapy (Buse et al. 2020). Moreover, the availability of the first GLP-1 mimetic for oral administration might further increase the popularity of this class of compounds.
However, GLP-1 mimetics still have some limitations. Because of rather frequent gastrointestinal side effects, the dose has to be up-titrated over weeks to achieve the maximum tolerated dose. But even at this dose level GLP-1 mimetics do not yet achieve the efficacy of bariatric surgery for body weight reduction and remission of type 2 diabetes (Baggio and Drucker 2021). In physiology, most peptide-secreting cells in the gut are plurihormonal, so that the gut secretes several peptide hormones in addition to GLP-1 to control body weight and glucose levels (Drucker 2016). It might therefore make sense to look into combinations of GLP-1 (mimetics) with other gut-secreted hormones like glucagon and GIP. Indeed, both pre-clinical studies and data from patients after bariatric surgery showing sustained increases in the circulating levels of multiple gut hormones indicate a high therapeutic potential of such combinations (Baggio and Drucker 2021; Finan et al. 2015).
2.2 Combinations of GLP-1 Agonists and Glucagon
While glucagon is usually regarded as a hormone with insulin-counterregulatory action increasing glucose levels, it also inhibits food intake and induces weight loss similar to the actions of GLP-1 (Henderson et al. 2016). Also, the naturally occurring 37 amino acid peptide oxyntomodulin contains the amino acid sequence of glucagon (GCG) and an 8 amino acid carboxy terminal extension and binds to the glucagon and GLP-1 receptors (Baggio and Drucker 2021). It has been shown that the weight-sparing effect of oxyntomodulin is mediated by both the glucagon and GLP-1 receptor (Kim et al. 2018a) inducing appetite suppression and satiety, but also increasing energy expenditure (Wynne et al. 2006). Therefore, a glucagon/GLP-1 co-agonist is an attractive candidate for treatment of diabetes and obesity (Baggio and Drucker 2021). Indeed, several of such co-agonists have been investigated, at least pre-clinically, however, the optimal ratio of glucagon and GLP-1 receptor activation (i.e., the affinity to each receptor) has not been easy to find.
While there are a number of glucagon/GLP-1 co-agonists in development (Hope et al. 2021), the most promising data seem to come from cotadutide which shows a balanced activity towards the glucagon and GLP-1 receptors (Ambery et al. 2018). In a placebo-controlled study in people with type 2 diabetes cotadutide showed a placebo-corrected decrease in postprandial glucose levels of 22% and reduced body weight by more than 2 kg in 41 treatment days (Ambery et al. 2018). In addition, a subset of patients was investigated with MRI-based proton-density fat-fraction analysis and showed a significantly stronger decline from baseline in liver fat (−6.0% vs. −3.2%), subcutaneous adipose tissue and visceral adipose tissue (p = 0.052) with cotadutide than with placebo.
The glucose-lowering effects of cotadutide were confirmed in a 4-week treatment study in overweight subjects with type 2 diabetes treated with dapagliflozin and metformin. Cotadutide showed significantly larger improvements versus placebo in both postprandial glucose levels (a difference of 22%) and mean glucose levels assessed by CGM (difference of 34 mg/dl) (Flor et al. 2021). The glucose-lowering properties of cotadutide seem to be primarily mediated by enhanced insulin secretion and delayed gastric emptying (Parker et al. 2020). Pre-clinical studies indicated that the effects of cotadutide to reduce body weight, food intake and improve glucose control are predominantly mediated through the GLP-1 signalling (Boland et al. 2020). In contrast, its action on the liver to reduce lipid content is directly mediated through glucagon signalling (Boland et al. 2020).
In a phase 2b-study in patients with type 2 diabetes inadequately controlled with metformin, cotadutide (investigated in doses of 100 μg, 200 μg and 300 μg q.d.) again led to significant reductions in body weight and HbA1c versus placebo over a treatment duration of 54 weeks (Nahra et al. 2021). There were no significant differences in HbA1c or body weight between the cotadutide arms versus liraglutide 1.8 mg q.d. with the exception of a slightly, but significantly higher body weight loss in the 300 μg cotadutide arm (−5.01 kg vs. −3.44 kg with liraglutide, p = 0.001). Patients in this treatment arm also showed greater reductions in liver enzymes, i.e. ALT (p = 0.023), whereas lower doses only showed significant reductions in liver enzymes (AST, ALT and GGT) versus placebo. However, the results of this study are difficult to interpret as cotadutide treatment was associated with significantly higher rates of treatment-emergent adverse events (TEAEs) across all doses. The most commonly reported TEAEs with cotadutide treatment were gastrointestinal disorders, including diarrhoea, nausea and vomiting. While a marked decrease in the event rate of these gastrointestinal events was observed over time, cotadutide showed lower study completion rates compared with placebo or liraglutide (73–77% cotadutide, 94% liraglutide, 81% placebo). Additional data are therefore needed to evaluate cotadutide’s tolerability and its efficacy in comparison with more potent glucose-lowering therapies than liraglutide (e.g., semaglutide).
2.3 Combinations of GLP-1 Agonists and GIP
The most prominent candidate of the combination of a GLP-1 mimetic and GIP is tirzepatide for which the phase 3 programme has already been completed. In contrast, most other GIP/GLP-1 co-agonists are still in pre-clinical development (Burade et al. 2021), however, some clinical data were published for an acylated GLP-1/GIP co-agonist demonstrating good tolerability at doses of up to 3.6 mg in healthy people and people with type 2 diabetes (Portron et al. 2017; Schmitt et al. 2017) as well as significant reductions in HbA1c and body weight over 12 weeks in people with type 2 diabetes (Frias et al. 2017). However, these improvements (in contrast to those seen with tirzepatide) did not exceed those observed with the GLP-1 agonist liraglutide alone.
Tirzepatide is a 39 amino acid linear peptide attached to a C20 fatty diacid moiety allowing binding to albumin thereby achieving a mean half-life of ~5 days (116.7 h), enabling once-weekly dosing (Coskun et al. 2018). Its molecular structure is based on the native GIP peptide sequence, but was modified to bind to both GIP and GLP-1 receptors. In vitro, tirzepatide has a higher potency to native GIP and has an about 5 times lower affinity to the GLP-1 receptor than native GLP-1 (Coskun et al. 2018; Papachristou et al. 2021). The higher affinity to the GIP-receptor might be surprising as even very high doses of GIP were ineffective as an insulinotropic agent in subjects with type 2 diabetes. In addition, GIP receptor knockout mice were protected from weight gain induced by high fat-feeding, suggesting that GIP might induce rather than prevent weight gain (Nauck et al. 2021).
Still, GIP is an attractive candidate for the combination with GLP-1 as both incretins have important physiological effects that are only partly overlapping. GLP-1 improves glucose-dependent insulin secretion, reduces glucagon secretion, slows down gastric emptying and leads to weight loss mainly through reducing appetite (Nauck and Meier 2016). GIP has also been demonstrated to have glucose-dependent effects on insulin and glucagon secretion, with a potentiation of glucagon secretion at hypoglycaemic and euglycaemic conditions but no effect on glucagon secretion at hyperglycaemic conditions where it potentiates the glucose-induced insulin secretion (Christensen et al. 2011). GIP was shown to increase glucose uptake, but also to promote the activity of lipoprotein lipase and of lipogenesis leading to increased triglyceride storage in adipose tissue (Nauck et al. 2021). In addition, GIP is involved in meal-associated bone remodelling (Nauck et al. 2021).
Overall, the effects of GIP alone are difficult to study in humans because of its short half-life. While a long-acting GIP receptor agonist has been developed for rodent studies (Zhang et al. 2021), such a tool is not available for human research. Potential benefits of the combination of GLP-1 and GIP can therefore only be derived from studies with co-agonists such as tirzepatide. Tirzepatide has been shown to suppress fasting glucagon more than the GLP-1 receptor agonist dulaglutide, even after adjusting for ambient plasma glucose concentrations (Nauck et al. 2021). In addition, it was recently demonstrated in a glucose clamp study that tirzepatide improves both insulin secretion and insulin sensitivity to a significantly larger extent than does the GLP-1 receptor agonist semaglutide (Heise 2021b). While these studies clearly indicate a high therapeutic potential for GLP-1/GIP-receptor co-agonists in diabetes and obesity, they cannot answer the question how and to what extent GIP contributes to the overall effects of these co-agonists. Based on pre-clinical findings (Borner et al. 2021) it has also been proposed that GIP acts as an anti-emetic, thereby improving the tolerability of GLP-1 receptor agonists (Hayes et al. 2021). Indeed, gastrointestinal side effects limit the efficacy of GLP-1 receptor agonists and it has been suggested that more than 20% of patients with type 2 diabetes cannot benefit fully from existing GLP-1 therapeutics because of these adverse events (Hayes et al. 2021). Improving gastrointestinal tolerability may therefore allow for using higher doses of GLP-1 receptor agonists to further enhance weight loss and glycaemic control.
While the exact contribution of GIP is still unclear, there is no question that tirzepatide shows unprecedented effects on glycaemia and body weight. This was impressively shown in the SURPASS-studies, the phase 3 programme of tirzepatide (Rosenstock et al. 2021; Frias et al. 2021a; Ludvik et al. 2021; Del Prato et al. 2021; Dahl et al. 2021). Design and results of these studies are summarised in Table 1 and Fig. 1. Overall, tirzepatide was investigated in people with type 2 diabetes in different treatment modalities (treatment-naïve, metformin monotherapy or in combination with other oral antidiabetic drugs, basal insulin therapy) and compared to placebo, semaglutide, insulin degludec or insulin glargine over 40 or 52 weeks. Tirzepatide was administered at once-weekly doses of 5 mg, 10 mg and 15 mg. To improve tolerability, tirzepatide treatment was initiated at 2.5 mg once per week, and increased by 2.5 mg every 4 weeks until the randomised dose was achieved. In case of intolerable gastrointestinal adverse events, the tirzepatide dose could be reduced to a lower, tolerated maintenance dose on which participants remained for the remainder of the study. Dose de-escalation was allowed only once. Despite this up-titration schedule, gastrointestinal adverse events were rather high with tirzepatide, in particular at the start of treatment. Up to 26.4% of patients exposed to tirzepatide discontinued study participation or treatment (Fig. 1, lower panel), although not all these discontinuations were due to adverse events. Nevertheless, study or treatment discontinuation was often higher with tirzepatide than with comparators, often even in the 5 mg once-weekly study arm.
Results of the Tirzepatide SURPASS Phase 3 Programme. The figure shows mean changes from baseline in HbA1c (upper panel) and body weight (middle panel) for the different tirzepatide doses and the comparators. The lower panel shows the percentage of randomised patients not completing the study or the full treatment duration. MET metformin, SGLT-2i SGLT-2 inhibitor, OADs oral antidiabetic drugs, TZP tirzepatide
On the other hand, tirzepatide showed impressive reductions in HbA1c and body weight (Fig. 1, upper and middle panel) which were significantly higher than active comparators or placebo. Importantly, treatment effects were significantly higher than those achieved with semaglutide (Frias et al. 2021a) which in previous studies had shown superior effects versus other GLP-1 receptor agonists (Capehorn et al. 2020; Pratley et al. 2018). Up to 87% of patients achieved HbA1c-levels ≤6.5% and up to 51% even showed normal HbA1c-levels below 5.7% (Frias et al. 2021a). Body weight losses were also impressive with up to 43% of patients achieving a weight loss of at least 15% (Ludvik et al. 2021). In a CGM-substudy of SURPASS-3, patients on 10 mg or 15 mg Tirzepatide once weekly showed 91% of CGM-values to be in target range (70–180 mg/dl) with only 1% or less values in the hypoglycaemic range (Battelino et al. 2021). Hypoglycaemia did not substantially increase in the combination with insulin glargine with annual rates of level 2 hypoglycaemia (blood glucose <54 mg/dl) of 0.43–0.50 events versus 0.44 events with insulin glargine alone (Dahl et al. 2021). Furthermore, Tirzepatide reduced liver enzymes (ALT and AST) by up to 32% of baseline values and liver fat content by 8.1% versus 3.4% with degludec (absolute changes from baseline) (Gastaldelli et al. 2021). Abdominal visceral adipose tissue was lowered by up to 1.65 l from baseline compared to a subtle increase (0.38 l) with insulin degludec.
Overall, these results clearly indicate that tirzepatide and potentially other GLP-1/GIP receptor co-agonists will achieve major improvement in patients with type 2 diabetes, at least in those who can tolerate at least weekly doses of 5 mg or 10 mg. Data on the impact of tirzepatide on hard cardiovascular endpoints are still pending (a cardiovascular outcome trial has been started, https://clinicaltrials.gov/ct2/show/NCT04255433, access 4th Jan 2022). However, a post-hoc analysis of the phase 2 data with tirzepatide showed improvements in cardiovascular biomarkers of insulin resistance, inflammation, endothelial dysfunction and cellular stress biomarkers (Wilson et al. 2020, 2021). Nevertheless, the results of the on-going cardiovascular outcome trial are certainly will have to be awaited before being able to evaluate the potential cardiovascular benefit of tirzepatide, in particular as it (like GLP-1 receptor agonists alone) significantly increases heart rate, but lowers systolic and diastolic blood pressure (Del Prato et al. 2021).
2.4 Other Dual- or Triple Agonists with GLP-1
Other co-agonists with GLP-1 receptor agonists are still early in development and are discussed in excellent previous reviews (Baggio and Drucker 2021). One promising development is the combination of amylin and GLP-1 receptor agonists. Amylin acts as both a neuropeptide and circulating endocrine hormone co-secreted with insulin from islet beta-cells and seems to be involved in the control of energy homeostasis, encompassing locomotor activity, energy expenditure and food intake (Baggio and Drucker 2021). Co-administration of a long-acting amylin analogue and semaglutide led to greater body weight reductions (15.7–17.1%) than semaglutide alone (9.8%) in a multiple-ascending dose, phase 1b trial in healthy overweight or obese people (Enebo et al. 2021). Large and long-term clinical trials including people with type 2 diabetes are outstanding.
Further promising candidates for the combination with GLP-1 receptor agonists are fibroblast growth factors (FGFs) as they decrease food intake, enhance thermogenesis, increase hepatic glucose uptake, reduce hepatic fat accumulation and liver inflammation and also enhance insulin action (Baggio and Drucker 2021). In pre-clinical studies, even single administrations of FGF1 (peripherally or into the brain) led to remissions of experimental diabetes (Bentsen et al. 2020). Clinical studies with analogues of FGF19 or FGF 21 showed some promising results such as reduction in liver fat and body weight, but not necessarily in blood glucose levels (Gaich et al. 2013; Harrison et al. 2018). Co-agonists of GLP-1 and FGF21 receptor agonists have only been studied pre-clinically so far. A fusion protein of the two agonists improved body weight and glucose control to a greater extent than the single components without inducing hypoglycaemia in rodents (Gilroy et al. 2020).
Finally, triple co-agonists have been investigated, although still pre-clinically. In view of the impressive efficacy of tirzepatide, GLP-1/GIP/glucagon triple agonists might be of particular interest. One of these triple agonists, HM15211, showed potent weight loss and HbA1c-improvements in obese animal models, either alone or in combination with a once-weekly insulin (Kim et al. 2018b). In addition, HM15211 reduced both body weight and liver fat content in obese subjects with non-alcoholic fatty liver disease (Abdelmalek et al. 2020).
Another GLP-1/GIP/glucagon triple agonist in development, LY3437943, has some similarities to tirzepatide as it is a single peptide derived from a GIP backbone and has an activity ratio between the GIP-receptor and GLP-1 receptor alike tirzepatide (Coskun et al. 2021). The glucagon receptor activity is similar to that of native glucagon. LY3437943 led to a significantly greater weight loss than cotadutide, liraglutide and tirzepatide, stimulated glucose-dependent insulin secretion and improved insulin sensitivity in DIO male C57/Bl6 mice (Coskun et al. 2021). It also reduced liver triglycerides and liver enzymes (ALT) in doses of 1 nmol/kg or higher in obese mice. A first in human study in healthy people showed good tolerability and safety, although (as expected) gastrointestinal adverse events were more frequent with LY3437943 (Urva et al. 2021). While no changes in fasting plasma glucose levels were observed in this single dose study, there were significant reductions in body weight with higher doses of LY3437943 (4.5 and 6.0 mg) which were sustained over the 43 days observation period and were most likely due to appetite suppression (Urva et al. 2021).
In summary, GLP-1 dual and triple receptor agonists show very promising results, in particular with regard to improvements in glucose control and body weight. While many of these agonists are still early in development, the GLP-1/GIP co-agonist tirzepatide has already completed phase 3 and is expected to get regulatory approval in the USA and Europe in 2022.
3 Novel Insulin Preparations
3.1 Once-Weekly Insulins
Obviously, one advantage of insulins that can be applied once weekly is the reduction in the number of necessary injections. Indeed, patients’ fear of needles or social embarrassment associated with injecting in public is a major reason for omitting insulin doses or for initiating insulin therapy with negative implications for glycaemic control (Ross 2013). But the potential of once-weekly insulins goes beyond reducing needle anxiety or mere convenience. Because of their long half-life once-weekly insulins should have low peak-to-trough fluctuations, thereby potentially avoiding hypoglycaemia and/or improving glycaemic control (Heise and Meneghini 2014). On the other hand, short-term adaptations of insulin dose will not be possible with very long-acting insulins which may trigger concerns about potential periods of over- or under-insulinisation with high risks of hypoglycaemia or hyperglycaemia (Heise 2021a).
3.1.1 Insulin Icodec
To date, clinical data of two once-weekly insulins in development have been published. One is insulin icodec which differs from the human insulin molecule in three positions (A14E, B16H and B25H) and contains a C20 fatty diacid containing side chain at B29K which is attached via a hydrophilic linker (Nishimura et al. 2020). These modifications lead to strong, but reversible albumin binding (10 times stronger than the albumin binding properties of insulin detemir), reduced enzymatic degradation and attenuated insulin receptor binding and clearance. Once insulin icodec binds to the insulin receptor, it elicits the same metabolic effects as human insulin. The in vitro mitogenic effects of icodec were found to be lower than that of human insulin (Nishimura et al. 2020).
3.1.2 Basal Insulin Fc (BIF)
The other development is Basal Insulin Fc (BIF), a fusion protein that combines a novel single-chain variant of insulin with a human IgG2Fc domain (Heise et al. 2021). BIF exhibits reduced insulin receptor (IR) potency with full agonism, and selectivity against human insulin-like growth factor-1 receptor (hIGF-1R) and has a mitogenic potential like native human insulin but with reduced potency (Moyers et al. 2021).
3.1.3 Pharmacology
Obviously, a long half-life is essential to make insulins suited for once-weekly dosing. A longer half-life will reduce peak-trough fluctuations, but will also be associated with more time to reach steady state after insulin initiation or dose changes. In general, it takes more than 3 half-lives to reach clinical steady state defined as trough concentrations exceeding 90% of the final plateau level (Heise et al. 2016).
For insulin icodec, a half-life of 196 h (~8.2 days) was presented (Hövelmann et al. 2020), whereas the reported half-life of BIF of 17 days was more than twice as long (Heise et al. 2021). In fact, the half-life of BIF might be even longer considering its peak-to-trough ratio of 1.14 over 1 week (Heise et al. 2021). As there is a direct correlation between half-life, peak-to-trough interval and peak-to-trough ratio (\( \mathrm{half}-\mathrm{life}=\ln (2)\bullet \frac{\mathrm{peak}-\mathrm{to}-\mathrm{trough}\ \mathrm{interval}}{\ln \left(\mathrm{peak}-\mathrm{to}-\mathrm{trough}\ \mathrm{ratio}\right)} \)), it is easy to calculate that the half-life of BIF is in the range of 3 weeks. The half-life of insulin icodec would then translate into a peak-to-trough ratio of 1.81 in a one-week treatment interval, which is very comparable to the peak-to-trough ratio of insulin glargine U100 over 24 h (Fig. 2) (Becker et al. 2015).
PK-simulations of insulin icodec with and without loading dose and BIF (with loading dose). Simulated pharmacokinetic profiles of insulin icodec when started with and without a loading dose at first administration (panel a) and of insulin icodec and basal insulin Fc BIF with a loading dose (panel b). A double dose has been simulated as loading dose for insulin icodec, and a triple dose for BIF. The grey shaded area shows the simulated peak-trough fluctuations at steady state with once-daily injected insulin glargine U100
With these reported pharmacological characteristics, both insulins should be suited for once-weekly dosing. BIF with its longer half-life will have very low changes in its glucose-lowering effect over 1 week, but will certainly require a loading dose to reach steady state in a reasonable time frame (without loading dose, it will take more than 3 months to reach “clinical” steady state). In contrast, insulin icodec will reach steady state much faster (in a bit more than 3 weeks without a loading dose), but will have higher fluctuations in its metabolic action over 1 week (Fig. 2, lower panel) (Heise 2021a). While this might be less important for patients with type 2 diabetes, the variability in basal insulin effect might be more difficult to cope with for patients with type 1 diabetes who might have to use lower bolus insulin doses in the first days post-dosing and higher doses towards the end of the dosing interval.
3.1.4 Clinical Data
Several phase 2 clinical studies demonstrated the potential of insulin icodec in patients with type 2 diabetes (data in people with type 1 diabetes have not yet been presented). The first study with a randomised double-blind design was done in insulin-naïve patients who received either once-weekly subcutaneous icodec or once-daily subcutaneous glargine U100 over 26 weeks (Rosenstock et al. 2020). The starting dose of insulin icodec was 70U once weekly, comparable to the 10U once-daily starting dose of insulin glargine. All insulin doses were adjusted once a week with the aim to achieve a pre-breakfast self-measured plasma glucose of 70–108 mg/dl (3.9–6.0 mmol/l). Starting from baseline HbA1c-levels of about 8% mean end of treatment (EOT) levels were 6.69% with icodec and of 6.87% with glargine with a trend of statistical superiority for insulin icodec (p = 0.08). In line with these HbA1c-results the mean self-measured plasma glucose levels were lower with icodec than with glargine (difference −7.9 mg/dl, 95% confidence interval −14.10 to −1.62 mg/dl) as was the time with glucose level in range of 70–140 mg/dl in the last 2 weeks of treatment (66.1% vs. 60.7%). While the incidence and rates of confirmed level 1 hypoglycaemia (blood glucose level <70 mg/dl or <3.9 mmol/l) were significantly higher with icodec than with glargine, the incidence and rates of the clinically more relevant level 2 hypoglycaemia (blood glucose level <54 mg/dl or <3.0 mmol/l) were similar. Weekly insulin doses were 19% lower with icodec during the last 2 weeks of treatment than with glargine, however, this finding could not be replicated in other studies. Both insulins were well tolerated and no unexpected safety findings occurred. A body weight gain of about 1.5 kg was observed in either treatment group.
These results are comparable to those obtained in patients already treated with basal insulin and at least one oral antidiabetic agent (Bajaj et al. 2020). In this study, a 100% loading dose was used in one icodec arm (icodec+LD, i.e., the first icodec dose was doubled) which resulted in better outcomes compared with the icodec arm with no loading dose (icodec NLD). In particular, time in range measured with continuous glucose monitoring (CGM) during the last 2 weeks of the 16 week treatment period was significantly higher for icodec+LD than that achieved with the comparator daily glargine U100 (72.9% vs. 65.0%, p = 0.01) and numerically higher than with icodec NLD (66.0%, p = 0.75). Similar to the results in insulin-naïve patients, HbA1c-values trended to be lower with icodec+LD vs. glargine (EOT difference −0.23%, p = 0.08), whereas hypoglycaemia incidence and rates as well as insulin doses and adverse event rates were similar across treatment arms. As expected a transient elevation of fasting plasma glucose was observed in the icodec NLD arm. This increase could be avoided with the loading dose.
The question how to best titrate doses of a once-weekly insulin was investigated in a third study which compared several titration algorithms for insulin icodec in insulin-naïve patients with type 2 diabetes (Lingvay et al. 2020). The algorithm with the lowest target fasting plasma glucose (FPG) target (3.9–6.0 mmol/l vs. 4.4–7.2 mmol/l with the other algorithms) resulted in better HbA1c-levels, but also in considerably higher rates of hypoglycaemia. Perhaps the best results were seen with algorithm B where weekly icodec doses were adjusted by ±28U based on the three most recent FPG values. This algorithm led to numerically higher time in range and lower HbA1c with comparable hypoglycaemia rates versus algorithm A where icodec dose changes were limited to 21U.
The only published clinical study with BIF was done in patients with type 2 diabetes treated with oral antidiabetic drugs and basal insulin (Frias et al. 2021b). Patients were randomised to two BIF-groups (with different dosing algorithms targeting relatively high fasting serum glucose (FSG) concentrations of ≤140 mg/dl and ≤120 mg/dl) or to insulin degludec once daily (target FSG ≤100 mg/dl). The treatment duration was 32 weeks. Both BIF-arms achieved non-inferior HbA1c levels to degludec, although mean FSG-concentrations were higher (by study design). Importantly, hypoglycaemic events ≤70 mg/dL (3.9 mmol/L) occurred less often with BIF than with degludec (a relative risk reduction of 25–26%), particularly nocturnal events (where the relative risk reduction was 33–43%). However, level 2 hypoglycaemic rates were not significantly different between treatment arms, although slightly lower in the BIF-arms. The number of adverse events including serious adverse events was comparable across treatments.
While these first clinical study data certainly demonstrate that the use of once-weekly insulins is feasible and safe in people with type 2 diabetes, clinical advantages are limited to non-significant trends towards slightly improved HbA1c-levels (icodec) and reduction in (nocturnal) level 1 hypoglycaemia (BIF). Several analyses showed that the duration of hypoglycaemic events was not different between once-weekly insulins and once-daily insulins (Heise et al. 2021; Silver et al. 2021), however, clinically significant (level 2) hypoglycaemia was not reduced versus once-daily insulins. Clearly, phase 3 data will have to be awaited before a fair evaluation of the clinical potential of once-weekly insulins will be possible. It is easy to predict, though, that a mere reduction in the number of insulin predictions will not suffice in most countries for coverage of once-weekly insulins by public health insurance (unless costs will be on par with once-daily insulins). Furthermore, it remains to be seen whether or not once-weekly insulins are suitable at least for a subset of patients with type 1 diabetes.
Despite these current limitations, there seems to be a future of once-weekly insulins in combination with once-weekly incretins which would certainly facilitate treatment intensification in people with type 2 diabetes. For both BIF and icodec a combination with dulaglutide and semaglutide, respectively, has been proposed to be feasible. A study with the combination of insulin icodec and semaglutide (IcoSema) has been started (https://clinicaltrials.gov/ct2/show/NCT05013229, access of 15th Oct 2021), but results have not yet been available.
3.2 Oral Insulins
3.2.1 Background
While once-weekly insulins might be preferred over once-daily injections, it clearly is the oral administration route that is the preferred way of drug intake. For insulins, the advantage of oral administration goes even beyond mere convenience and ease of therapy. The oral absorption of insulin, similar to endogenous insulin, will achieve high insulin concentration in the portal vein before reaching peripheral tissues. Thus, orally absorbed insulin will have a hepato-preferential action avoiding over-insulinisation of peripheral tissues and thereby potentially reducing the risk of hypoglycaemia (Heise 2021a). And as semaglutide is already available as oral preparation, an oral combination of incretin and insulin might also be feasible, provided that oral insulin administration works.
Indeed, oral application of insulin was tested very soon after its first subcutaneous administration in humans. The first publication was published in 1923 and was the first of many testimonials of the major challenges of oral insulin administration, in particular high variability in insulin absorption and poor bioavailability (Harrison 1923).
Nevertheless, oral insulin absorption has been shown to be feasible. A glucose clamp study in patients with type 2 diabetes demonstrated a bioavailability of 26% in the first hour post-dosing, whereas bioavailability over the 6 h of the experiment was only 2%. This difference between early and total bioavailability of oral insulin was due to a fast onset of absorption with high peak serum insulin levels and a considerably shorter duration of action compared with s.c. regular human insulin (Kapitza et al. 2010). This pharmacokinetic (PK)/pharmacodynamics (PD) profile with a fast onset and short duration of action would predestine oral insulin for prandial insulin coverage, perhaps even allowing postprandial intake. Unfortunately, however, oral insulin preparations have a pronounced “food effect”, so that absorption is considerably lower when given with or shortly after a meal (Khedkar et al. 2020; Halberg et al. 2019a). Therefore, a dosing-meal interval has to be used with prandial oral insulin formulations, and it has been shown that insulin absorption improves with increasing duration of such an interval. However, a longer administration-meal interval also bears a risk of early hypoglycaemia (due to a strong early insulin effect before oral glucose absorption) and of late postprandial hyperglycaemia (because of declining insulin absorption, but on-going glucose absorption) (Heise 2021a; Khedkar et al. 2020).
3.2.2 Prandial Oral Insulins
Prandial oral insulin formulations have been described in excellent previous reviews (Zijlstra et al. 2014). One such formulation is IN-105 or insulin tregopil, an insulin analogue with a polyethylene glycol side chain at position B29 and sodium caprate as absorption enhancer (Khedkar et al. 2010). Due to its rapid absorption, short duration of action and its food effect (Khedkar et al. 2019), insulin tregopil should be administered 10–30 min before meal intake (Khedkar et al. 2010, 2020). However, this did not suffice to achieving a placebo-adjusted HbA1c reduction of 0.7%, the predefined primary efficacy endpoint in an early phase 3 clinical trial in patients with type 2 diabetes. Insulin tregopil did induce significant improvements in early postprandial glucose levels, though (Zijlstra et al. 2014). In another 24-week treatment study in 91 people with type 2 diabetes comparing 30 and 45 mg of insulin tregopil (to be administered 10 min before meal intake) with s.c. insulin aspart (injected within 5 min before meal intake) insulin tregopil even showed numerical deteriorations in HbA1c (increase by 0.11–0.15%), whereas insulin aspart improved HbA1c by 0.78% (https://clinicaltrials.gov/ct2/show/results/NCT03430856, access 11 Oct 2021). Hypoglycaemia incidence was comparable across treatment groups (83–87% of patients). A study in people with type 1 diabetes is on-going (https://clinicaltrials.gov/ct2/show/NCT04141423, access 11 Oct 2021).
Another oral insulin in development is ORMD-0801, formulated in an enteric-coated capsule with further unspecified adjuvants that shall both protect the insulin from degradation in the gastrointestinal tract and enhance its absorption (Zijlstra et al. 2014). While the number of clinical trials with ORMD-0801 registered on https://clinicaltrials.gov is quite impressive (to date 7 completed, 5 recruiting and 3 not yet recruiting), only one of the more recently completed studies has been published (Eldor et al. 2021). Like most other published studies with ORMD-0801, this study only compared to placebo rather than to a s.c. insulin, which makes it quite difficult to evaluate clinical efficacy. Nevertheless, the results of this publication (the “largest Phase II, placebo-controlled study conducted with ORMD-0801 to date” in 188 patients with type 2 diabetes) raise some doubts that ORMD-0801 will become a viable treatment option for people with diabetes. The pooled results of patients randomised to 16 mg or 24 mg ORMD-0801 (administered at bedtime, at least 2 h after the last evening meal and at least 6 h before the next meal) in addition to pre-exiting metformin therapy did not show any meaningful improvements in HbA1c or baseline weighted mean night-time CGM readings, even though the observed small increase in the latter parameter was significantly lower than the increase observed with placebo (Eldor et al. 2021). The absence of nocturnal hypoglycaemic events in the study might rather be a sign of insufficient insulin absorption than a safety feature. Poor absorption was also indicated by a glucose clamp study comparing two 8 mg ORMD-0801 capsules with three 8 mg capsules and one 16 mg capsule under euglycaemic clamp conditions with tritiated glucose to assess hepatic glucose production (HGP) in 11 people with type 1 diabetes (https://clinicaltrials.gov/ct2/show/results/NCT02535715, access 11 Oct 2021). None of the ORMD-0801 formulations showed increases from baseline plasma insulin concentrations over a period of 240 min, and suppression of HGP was modest in all three treatment arms. In addition, other clinical studies have also only shown modest effects on glycaemic control. In small studies using CGM over 1 or 2 weeks in people with type 1 or type 2 diabetes, ORMD-0801 slightly reduced daytime and night-time glucose levels (by 1.0–1.5 mmol/l or less) and basal insulin doses (in type 1 diabetes) versus placebo (https://clinicaltrials.gov/ct2/show/results/NCT01889667 and https://clinicaltrials.gov/ct2/show/results/NCT02094534, access 11 Oct 2021). Despite these shortcomings FDA approved several phase 3 studies in people with type 2 diabetes which are currently on-going.
Overall, these results show that the challenges of developing prandial oral insulin have not changed since 1923. Variability preventing a clear dose-response relationship in combination with low bioavailability, in particular when given in close temporal proximity with food, limits the clinical efficacy of prandial oral insulin (Heise 2021a).
3.2.3 Basal Oral Insulins
A basal oral insulin would solve all issues about the food effect of oral insulin absorption as a basal insulin could be taken far before or after a meal. However, achieving a basal, constant insulin supply from an orally administered insulin is a major challenge. This challenge was addressed with the long-acting basal insulin analogue 338 (I338) formulated with a gastrointestinal permeation enhancer (GIPET I) and an absorption enhancer (sodium caprate) (Halberg et al. 2019b; Kjeldsen et al. 2021). I338 contains an 18-carbon fatty diacid which is attached via a linker to the insulin molecule and allows reversible binding to albumin. Thus, I338 is absorbed quickly but released only slowly from the albumin pool resulting in a half-life of up to 70 h at steady state (Kjeldsen et al. 2021). This allows meal-independent dosing of I338 which, however, also shows a food effect I338 (Halberg et al. 2019a). A double-blind, double-dummy phase 2 clinical study compared oral I338 with insulin glargine U100 s.c. once daily for 8 weeks in insulin-naïve patients with type 2 diabetes on metformin therapy with or without other oral antidiabetic agents. I338 was given in a fasted state and patients were asked to refrain from fluid and food intake for 1 h. At the end of treatment, fasting plasma glucose (FPG) levels (the primary endpoint) and 10-point plasma glucose profiles were not significantly different between treatment arms (Fig. 3), neither were HbA1c-levels (although they were numerically lower (with a difference of 0.3%) s.c. insulin glargine. Interestingly, within-patient variability in FPG concentration was higher by 52% in the I338 group than in the insulin glargine group, but again this difference did not reach statistical significance and was already present at baseline.
Glucose control with oral insulin. 10-point plasma glucose concentration profiles at baseline and after 8 weeks of treatment with oral insulin I338 or subcutaneous insulin glargine U100 (IGlar). Data are arithmetic mean (SD). Reprinted from Halberg et al. (2019b) with permission
Overall, this study was the first demonstrating that oral insulin therapy might be feasible, at least in people with type 2 diabetes when using a basal oral insulin with a long half-life. While food effect and high variability of oral insulins could be successfully overcome with this approach, the issue of a low bioavailability remained (I338 doses were approximately 58 times higher than insulin glargine doses at the end of treatment). While this bioavailability was still higher than that of oral semaglutide (Buckley et al. 2018), it led to discontinuation of the development of I338 as “production of the required quantities of I338 for wide public use was deemed not commercially viable” (Halberg et al. 2019b).
Therefore, despite having shown proof of concept, the further development of oral basal insulin seems unclear. Approaches to increase bioavailability have not yet reached clinical stage (Abramson et al. 2019). Likewise, new strategies, e.g. using oral insulin early in type 2 diabetes to improve beta-cell dysfunction and insulin sensitivity or even achieve remission (Kramer et al. 2013) have not been investigated to date.
4 Summary and Conclusions
It is easy to predict that future diabetes therapy will comprise of tirzepatide and once-weekly insulins in the nearer future, whereas it will take much more time before other co-agonists or triple agonists or other insulin developments (like hepato-preferential, oral or glucose-responsive insulins) will be part of a clinical routine. Many other developments have not been addressed in this paper because clinical data are still outstanding. Although pharmacological diabetes therapy was introduced with the discovery of insulin 100 years ago (Banting et al. 1922), the development of antidiabetic drugs is still on-going. Many promising data of novel antidiabetic drugs clearly indicate that therapy of people with diabetes will become easier, safer and more efficacious in the next years.
References
Abdelmalek MF, Choi J, Kim Y, Seo K, Hompesch M (2020) HM15211, a novel GLP-1/GIP/glucagon triple-receptor co-agonist significantly reduces liver fat and body weight in obese subjects with non-alcoholic fatty liver disease: a phase 1b/2a, multi-center, randomized, placebo-controlled trial. J Hepatol 73(Suppl. 1):S124
Abramson A, Caffarel-Salvador E, Khang M, Dellal D, Silverstein D, Gao Y et al (2019) An ingestible self-orienting system for oral delivery of macromolecules. Science 363(6427):611–615
Ambery P, Parker VE, Stumvoll M, Posch MG, Heise T, Plum-Moerschel L et al (2018) MEDI0382, a GLP-1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double-blind, ascending dose and phase 2a study. Lancet 391(10140):2607–2618
Baggio LL, Drucker DJ (2021) Glucagon-like peptide-1 receptor co-agonists for treating metabolic disease. Mol Metab 46:101090
Bailey CJ, Day C (2018) Treatment of type 2 diabetes: future approaches. Br Med Bull 126(1):123–137
Bajaj H, Isendahl J, Gowda A, Stachlewska K, Rosenstock J (2020) Efficacy and safety of switching to insulin icodec, a once-weekly basal insulin, vs insulin glargine U100 in patients with type 2 diabetes inadequately controlled on OADs and basal insulin. Diabetologia 63(Suppl. 1):657
Banting FG, Best CH, Collip JB, Campbell WR, Fletcher AA (1922) Pancreatic extracts in the treatment of diabetes mellitus. Can Med Assoc J 12(3):141–146
Battelino T, Bergenstal R, Rodriguez A, Fernandez Lando L, Bray R, Tong Z et al (2021) Effect of tirzepatide versus insulin degludec on glycaemic control captured with continuous glucose monitoring in patients with type 2 diabetes (SURPASS-3 CGM). Diabetologia 64(Suppl. 1):S244
Becker RH, Nowotny I, Teichert L, Bergmann K, Kapitza C (2015) Low within- and between-day variability in exposure to new insulin glargine 300 U/ml. Diabetes Obes Metab 17(3):261–267
Bentsen MA, Rausch DM, Mirzadeh Z, Muta K, Scarlett JM, Brown JM et al (2020) Transcriptomic analysis links diverse hypothalamic cell types to fibroblast growth factor 1-induced sustained diabetes remission. Nat Commun 11(1):4458
Bianzano S, Heise T, Jungnik A, Schepers C, Scholch C, Grafe-Mody U (2021) Safety, tolerability, pharmacokinetics and pharmacodynamics of single oral doses of BI 187004, an inhibitor of 11beta-hydroxysteroid dehydrogenase-1, in healthy male volunteers with overweight or obesity. Clin Diabetes Endocrinol 7(1):16
Boland ML, Laker RC, Mather K, Nawrocki A, Oldham S, Boland BB et al (2020) Resolution of NASH and hepatic fibrosis by the GLP-1R/GcgR dual-agonist Cotadutide via modulating mitochondrial function and lipogenesis. Nat Metab 2(5):413–431
Borner T, Geisler CE, Fortin SM, Cosgrove R, Alsina-Fernandez J, Dogra M et al (2021) GIP receptor agonism attenuates GLP-1 receptor agonist-induced nausea and emesis in preclinical models. Diabetes 70(11):2545–2553
Buckley ST, Baekdal TA, Vegge A, Maarbjerg SJ, Pyke C, Ahnfelt-Ronne J et al (2018) Transcellular stomach absorption of a derivatized glucagon-like peptide-1 receptor agonist. Sci Transl Med 10(467). https://doi.org/10.1126/scitranslmed.aar7047
Burade VS, Garcia-Ozana A, Pratley RE, Rutter GA, Vilsboll T, Thorens B et al (2021) A novel, long-acting dual agonist for GIPR/GLP-1R, HISHS-2001, demonstrates effects on HbA1c and weight loss in the db/db mouse model of type 2 diabetes. Diabetes 70(Suppl. 1):638
Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C et al (2020) 2019 Update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 43(2):487–493
Capehorn MS, Catarig AM, Furberg JK, Janez A, Price HC, Tadayon S et al (2020) Efficacy and safety of once-weekly semaglutide 1.0mg vs once-daily liraglutide 1.2mg as add-on to 1-3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab 46(2):100–109
Christensen M, Vedtofte L, Holst JJ, Vilsboll T, Knop FK (2011) Glucose-dependent insulinotropic polypeptide: a bifunctional glucose-dependent regulator of glucagon and insulin secretion in humans. Diabetes 60(12):3103–3109
Coskun T, Sloop KW, Loghin C, Alsina-Fernandez J, Urva S, Bokvist KB et al (2018) LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab 18:3–14
Coskun T, Moyers JS, Roell W, O'Farrell L, Regmi A, Ruan X et al (2021) The novel GIP, GLP-1, and glucagon triple receptor agonist LY3437943 exhibits robust efficacy in preclinical models of obesity and diabetes. Diabetes 70(Suppl 1):679
Dahl D, Onishi Y, Norwood P, Huh R, Patel H, Rodriguez A (2021) Tirzepatide, a dual GIP/GLP-1 receptor agonist, is effective and safe when added to basal insulin for treatment of type 2 diabetes (SURPASS-5). Diabetes 70(Suppl 1):80
Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J et al (2021) Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet
Drucker DJ (2016) Evolving concepts and translational relevance of enteroendocrine cell biology. J Clin Endocrinol Metab 101(3):778–786
Dubourg J, Ueki K, Grouin JM, Fouqueray P (2021a) Efficacy and safety of imeglimin in Japanese patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled, dose-ranging phase 2b trial. Diabetes Obes Metab 23(3):800–810
Dubourg J, Fouqueray P, Thang C, Grouin JM, Ueki K (2021b) Efficacy and safety of Imeglimin monotherapy versus placebo in Japanese patients with type 2 diabetes (TIMES 1): a double-blind, randomized, placebo-controlled, parallel-group, multicenter phase 3 trial. Diabetes Care 44(4):952–959
Eldor R, Neutel J, Homer K, Kidron M (2021) Efficacy and safety of 28-day treatment with oral insulin (ORMD-0801) in patients with type 2 diabetes: a randomized, placebo-controlled trial. Diabetes Obes Metab 23(11):2529–2538
Enebo LB, Berthelsen KK, Kankam M, Lund MT, Rubino DM, Satylganova A et al (2021) Safety, tolerability, pharmacokinetics, and pharmacodynamics of concomitant administration of multiple doses of cagrilintide with semaglutide 2.4 mg for weight management: a randomised, controlled, phase 1b trial. Lancet 397(10286):1736–1748
Finan B, Yang B, Ottaway N, Smiley DL, Ma T, Clemmensen C et al (2015) A rationally designed monomeric peptide triagonist corrects obesity and diabetes in rodents. Nat Med 21(1):27–36
Flor A, Petrone M, Sanchez J, Petrohoy T, Jermutus L, Hansen L et al (2021) Efficacy, safety and tolerability of cotadutide as an add-on therapy in overweight subjects with type 2 diabetes treated with dapagliflozin and metformin. Diabetologia 64(Suppl. 1):S247
Frias JP, Bastyr EJ 3rd, Vignati L, Tschop MH, Schmitt C, Owen K et al (2017) The sustained effects of a dual GIP/GLP-1 receptor agonist, NNC0090-2746, in patients with type 2 diabetes. Cell Metab 26(2):343–52 e2
Frias JP, Davies MJ, Rosenstock J, Perez Manghi FC, Fernandez Lando L, Bergman BK et al (2021a) Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med 385(6):503–515
Frias JP, Chien J, Zhang Q, Chigutsa E, Landschulz W, Wullenweber P et al (2021b) Once weekly basal insulin Fc (BIF) is safe and efficacious in patients with type 2 diabetes mellitus (T2DM) previously treated with basal insulin. J Endocr Soc 5(Suppl 1):A448–A449
Gaich G, Chien JY, Fu H, Glass LC, Deeg MA, Holland WL et al (2013) The effects of LY2405319, an FGF21 analog, in obese human subjects with type 2 diabetes. Cell Metab 18(3):333–340
Gastaldelli A, Cusi K, Fernandez Lando L, Bray R, Brouwers B, Rodriguez A (2021) Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in patients with type 2 diabetes (SURPASS-3 MRI). Diabetologia 64(Suppl. 1):S219–SS20
Gilroy CA, Capozzi ME, Varanko AK, Tong J, D'Alessio DA, Campbell JE et al (2020) Sustained release of a GLP-1 and FGF21 dual agonist from an injectable depot protects mice from obesity and hyperglycemia. Sci Adv 6(35):eaaz9890
Halberg IB, Lyby K, Wassermann K, Heise T, Plum-Morschel L, Zijlstra E (2019a) The effect of food intake on the pharmacokinetics of oral basal insulin: a randomised crossover trial in healthy male subjects. Clin Pharmacokinet 58(11):1497–1504
Halberg IB, Lyby K, Wassermann K, Heise T, Zijlstra E, Plum-Morschel L (2019b) Efficacy and safety of oral basal insulin versus subcutaneous insulin glargine in type 2 diabetes: a randomised, double-blind, phase 2 trial. Lancet Diabetes Endocrinol 7(3):179–188
Hallakou-Bozec S, Vial G, Kergoat M, Fouqueray P, Bolze S, Borel AL et al (2021) Mechanism of action of Imeglimin: a novel therapeutic agent for type 2 diabetes. Diabetes Obes Metab 23(3):664–673
Harrison GA (1923) Insulin in alcoholic solution by the mouth. Br Med J 2(3286):1204–1205
Harrison SA, Rinella ME, Abdelmalek MF, Trotter JF, Paredes AH, Arnold HL et al (2018) NGM282 for treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 391(10126):1174–1185
Hayes MR, Borner T, De Jonghe BC (2021) The role of GIP in the regulation of GLP-1 satiety and nausea. Diabetes 70(9):1956–1961
Heise T (2021a) The future of insulin therapy. Diabetes Res Clin Pract 175:108820
Heise T (2021b) Tirzepatide mechanism of action: effects on endocrine function and insulin resistance in patients with type 2 diabetes. A clamp study. EASD virtual meeting. https://www.easd.org/virtualmeeting/home.html#!resources/b-tirzepatide-mechanism-of-action-effects-on-endocrine-function-and-insulin-resistance-in-patients-with-type-2-diabetes-b. Accessed 14 Nov 2021
Heise T, Meneghini LF (2014) Insulin stacking versus therapeutic accumulation: understanding the differences. Endocr Pract 20(1):75–83
Heise T, Korsatko S, Nosek L, Coester HV, Deller S, Roepstorff C et al (2016) Steady state is reached within 2-3 days of once-daily administration of degludec, a basal insulin with an ultralong duration of action. J Diabetes 8(1):132–138
Heise T, Chien J, Beals J, Benson C, Klein O, Moyers JS et al (2021) Basal insulin FC (BIF), a novel insulin suited for once weekly dosing for the treatment of patients with diabetes mellitus. J Endocr Soc 5(Suppl. 1):A329
Henderson SJ, Konkar A, Hornigold DC, Trevaskis JL, Jackson R, Fritsch Fredin M et al (2016) Robust anti-obesity and metabolic effects of a dual GLP-1/glucagon receptor peptide agonist in rodents and non-human primates. Diabetes Obes Metab 18(12):1176–1190
Home P (2021) The evolution of insulin therapy. Diabetes Res Clin Pract 175:108816
Hope DCD, Vincent ML, Tan TMM (2021) Striking the balance: GLP-1/Glucagon Co-Agonism as a treatment strategy for obesity. Front Endocrinol (Lausanne) 12:735019
Hövelmann U, Brøndsted L, Kristensen NR, Ribel-Madsen R, DeVries JH, Heise T et al (2020) Insulin icodec: an insulin analog suited for once-weekly dosing in type 2 diabetes. Diabetes 69(Suppl 1):237
Kapitza C, Zijlstra E, Heinemann L, Castelli MC, Riley G, Heise T (2010) Oral insulin: a comparison with subcutaneous regular human insulin in patients with type 2 diabetes. Diabetes Care 33(6):1288–1290
Kazemian P, Shebl FM, McCann N, Walensky RP, Wexler DJ (2019) Evaluation of the cascade of diabetes care in the United States, 2005-2016. JAMA Intern Med 179(10):1376–1385
Khedkar A, Iyer H, Anand A, Verma M, Krishnamurthy S, Savale S et al (2010) A dose range finding study of novel oral insulin (IN-105) under fed conditions in type 2 diabetes mellitus subjects. Diabetes Obes Metab 12(8):659–664
Khedkar A, Lebovitz H, Fleming A, Cherrington A, Jose V, Athalye SN et al (2019) Impact of insulin Tregopil and its permeation enhancer on pharmacokinetics of metformin in healthy volunteers: randomized, open-label, placebo-controlled, crossover study. Clin Transl Sci 12(3):276–282
Khedkar A, Lebovitz H, Fleming A, Cherrington A, Jose V, Athalye SN et al (2020) Pharmacokinetics and pharmacodynamics of insulin Tregopil in relation to Premeal dosing time, between meal interval, and meal composition in patients with type 2 diabetes mellitus. Clin Pharmacol Drug Dev 9(1):74–86
Khunti K, Millar-Jones D (2017) Clinical inertia to insulin initiation and intensification in the UK: a focused literature review. Prim Care Diabetes 11(1):3–12
Kim T, Holleman CL, Nason S, Arble DM, Ottaway N, Chabenne J et al (2018a) Hepatic glucagon receptor signaling enhances insulin-stimulated glucose disposal in rodents. Diabetes 67(11):2157–2166
Kim JK, Lee JS, Choi J, Jung SY, Lee SH, Choi IY et al (2018b) Novel combination of a long-acting GLP-1/GIP/glucagon triple agonist (HM15211) and once-weekly basal insulin (HM12460a) offers improved glucose sowering and weight loss in a diabetic animal model. Diabetes 67(Suppl 1):77
Kjeldsen TB, Hubalek F, Tagmose TM, Pridal L, Refsgaard HHF, Porsgaard T et al (2021) Engineering of orally available, ultralong-acting insulin analogues: discovery of OI338 and OI320. J Med Chem 64(1):616–628
Kramer CK, Choi H, Zinman B, Retnakaran R (2013) Determinants of reversibility of beta-cell dysfunction in response to short-term intensive insulin therapy in patients with early type 2 diabetes. Am J Physiol Endocrinol Metab 305(11):E1398–E1407
Lingvay I, Koefoed M, Stachlewska K, Hansen M, Rosenstock J (2020) Effect of three different titration algorithms of insulin icodec vs insulin glargine U100 on time in range in patients with type 2 diabetes inadequately controlled on OADs. Diabetologia 63(Suppl. 1):658
Ludvik B, Giorgino F, Jodar E, Frias JP, Fernandez Lando L, Brown K et al (2021) Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet 398(10300):583–598
Moyers JS, Hansen RJ, Day JW, Dickinson CD, Zhang C, Kahl SD et al (2021) Preclinical characterization of once weekly basal insulin Fc (BIF). J Endocr Soc 5(Suppl 1):A442
Nahra R, Wang T, Gadde KM, Oscarsson J, Stumvoll M, Jermutus L et al (2021) Effects of cotadutide on metabolic and hepatic parameters in adults with overweight or obesity and type 2 diabetes: a 54-week randomized phase 2b study. Diabetes Care 44(6):1433–1442
Nakamura A, Terauchi Y (2015) Present status of clinical deployment of glucokinase activators. J Diabetes Investig 6(2):124–132
Nauck MA, Meier JJ (2016) The incretin effect in healthy individuals and those with type 2 diabetes: physiology, pathophysiology, and response to therapeutic interventions. Lancet Diabetes Endocrinol 4(6):525–536
Nauck MA, Quast DR, Wefers J, Pfeiffer AFH (2021) The evolving story of incretins (GIP and GLP-1) in metabolic and cardiovascular disease: a pathophysiological update. Diabetes Obes Metab 23(Suppl 3):5–29
Nishimura E, Kjeldsen T, Glendorf FH, Stidsen CE, Hansen BF et al (2020) Molecular and biological properties of insulin icodec, a new insulin analog designed to give a long half-life suitable for once-weekly dosing. Diabetes 69(Suppl 1):236
Papachristou S, Popovic DS, Papanas N (2021) The new dual gastric inhibitory peptide/glucagon-like peptide 1 agonist tirzepatide in type 2 diabetes: is the future bright? Diabetes Metab Res Rev 37(8):e3503
Parker VER, Robertson D, Wang T, Hornigold DC, Petrone M, Cooper AT et al (2020) Efficacy, safety, and mechanistic insights of Cotadutide, a dual receptor glucagon-like peptide-1 and glucagon agonist. J Clin Endocrinol Metab 105(3)
Portron A, Jadidi S, Sarkar N, DiMarchi R, Schmitt C (2017) Pharmacodynamics, pharmacokinetics, safety and tolerability of the novel dual glucose-dependent insulinotropic polypeptide/glucagon-like peptide-1 agonist RG7697 after single subcutaneous administration in healthy subjects. Diabetes Obes Metab 19(10):1446–1453
Pratley RE, Aroda VR, Lingvay I, Ludemann J, Andreassen C, Navarria A et al (2018) Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol 6(4):275–286
Rosenstock J, Bajaj HS, Janez A, Silver R, Begtrup K, Hansen MV et al (2020) Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med 383(22):2107–2116
Rosenstock J, Wysham C, Frias JP, Kaneko S, Lee CJ, Fernandez Lando L et al (2021) Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet 398(10295):143–155
Ross SA (2013) Breaking down patient and physician barriers to optimize glycemic control in type 2 diabetes. Am J Med 126(9 Suppl 1):S38–S48
Schmitt C, Portron A, Jadidi S, Sarkar N, DiMarchi R (2017) Pharmacodynamics, pharmacokinetics and safety of multiple ascending doses of the novel dual glucose-dependent insulinotropic polypeptide/glucagon-like peptide-1 agonist RG7697 in people with type 2 diabetes mellitus. Diabetes Obes Metab 19(10):1436–1445
Silver R, Asong M, Begtrup K, Heller SR, Liu L, Rosenstock J (2021) Similar hypoglycaemia duration with once-weekly insulin icodec vs insulin glargine U100 in insulin naive or experienced patients with type 2 diabetes. Diabetologia 64(Suppl. 1):S73
UK Hypoglycaemia Study Group (2007) Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 50(6):1140–1147
Urva S, Du Y, Thomas MK, Milicevic Z, Coskun T, Benson CT et al (2021) Novel GIP/GLP-1/glucagon receptor agonist LY3437943: a first in human dose study in healthy participants. Diabetes 70(Suppl 1):104
Wilson JM, Nikooienejad A, Robins DA, Roell WC, Riesmeyer JS, Haupt A et al (2020) The dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist, tirzepatide, improves lipoprotein biomarkers associated with insulin resistance and cardiovascular risk in patients with type 2 diabetes. Diabetes Obes Metab 22(12):2451–2459
Wilson JM, Lin Y, Luo MJ, Considine G, Cox AL, Bowsman LM et al (2021) The dual glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist tirzepatide improves cardiovascular risk biomarkers in patients with type 2 diabetes: a post hoc analysis. Diabetes Obes Metab
Wynne K, Park AJ, Small CJ, Meeran K, Ghatei MA, Frost GS et al (2006) Oxyntomodulin increases energy expenditure in addition to decreasing energy intake in overweight and obese humans: a randomised controlled trial. Int J Obes (Lond) 30(12):1729–1736
Zhang Q, Delessa CT, Augustin R, Bakhti M, Collden G, Drucker DJ et al (2021) The glucose-dependent insulinotropic polypeptide (GIP) regulates body weight and food intake via CNS-GIPR signaling. Cell Metab 33(4):833–44 e5
Zijlstra E, Heinemann L, Plum-Mörschel L (2014) Oral insulin reloaded: a structured approach. J Diabetes Sci Technol 8(3):458–465
Conflict of Interest
TH is shareholder of the private research institute Profil which received research funds from Adocia, Afon Technology, Astra Zeneca, Biocon, Boehringer Ingelheim, Eli Lilly, Gan Lee Pharmaceuticals, Johnson & Johnson, Julphar, Mylan, Nestlé, Neuraly, Nordic Bioscience, Novo Nordisk, Sanofi and Zealand Pharma. TH received speaker honoraria and travel grants from Eli Lilly and Novo Nordisk, and was a paid member of advisory panels for Novo Nordisk and Valbiotis.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Heise, T. (2022). Novel Drugs for Diabetes Therapy. In: Eckel, J., Clément, K. (eds) From Obesity to Diabetes. Handbook of Experimental Pharmacology, vol 274. Springer, Cham. https://doi.org/10.1007/164_2021_574
Download citation
DOI: https://doi.org/10.1007/164_2021_574
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-99994-0
Online ISBN: 978-3-030-99995-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)