Abstract
Five subtypes of muscarinic acetylcholine receptors denoted M1 through M5 have been cloned. Muscarinic receptors mediate a wide array of physiological functions and impairment of muscarinic signaling is involved in numerous pathological conditions including Alzheimer’s disease and schizophrenia. Reliable radioligand binding techniques allow study of involvement of individual muscarinic receptor subtypes in the physiology and pathology of muscarinic signaling, and study of the structure of muscarinic receptors and structure-activation relationship of muscarinic ligands. Here we discuss the current state of knowledge of radioligand binding experiments at muscarinic receptors from the perspective of available radioligands and selective unlabeled muscarinic ligands. We relate binding properties of muscarinic ligands to experimental design (e.g., nonspecific binding determination, incubation conditions, buffers, temperature). We also list tissue/cell sources of muscarinic receptors suitable for radioligand binding studies and describe procedures of cell and tissue preparation for radioligand binding experiments. We also describe several techniques of receptor-bound ligand separation applicable at muscarinic receptors and provide basic information for binding data analysis.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
1 Historical Background
Radioligand binding methods are a cornerstone of receptor pharmacology, taking muscarinic acetylcholine receptors as an example. The main principle of the method is to allow a radiolabeled compound specific to a given receptor to incubate with a biological sample enriched with that receptor, and then separate the bound and free radioligand. Many radiolabeled muscarinic ligands with high affinity and specific activity are currently available. Development of reliable radioligand binding technique at muscarinic receptors cleared the way for identification, purification, and subsequent sequencing of the first muscarinic receptor [1] that enabled ensuing cloning of five subtypes of muscarinic receptors (M1 through M5) [2] that revolutionized the field of research of muscarinic receptor pharmacology. Furthermore, radioligand binding played a key role in identifying the orthosteric ligand-binding site that is located in a pocket formed by transmembrane helices [3, 4], receptor subtype-specific ligands, allosteric modulators, and structure-activation relationship. Radioligand binding may also be employed in sophisticated experiments to study kinetics of drug-receptor interactions or in a combination with site-directed mutagenesis to determine the role of specific residues and domains in ligand binding. Similar to other receptor targets, radioligand binding studies at muscarinic receptors are simple and if performed correctly are very sensitive and highly accurate.
2 Principles of Ligand Binding
2.1 Ligand Binding Definition
Interaction of a small molecule (ligand) with a protein (receptor) is mediated by four chemical forces: electrostatic force, hydrogen bonding, van der Waals interactions, and hydrophobic bonds. Electrostatic force mediates attraction between opposed charged groups or repulsion between similarly charged groups that is proportional to the net sum of charges and inversely proportional to the square of distance between charges (as described by Coulomb’s law). van der Waals interactions are attractive and repulsive forces between dipoles approximated by Lennard-Jones function that has its minimum (strongest attraction) at certain distance of the components. A hydrogen bond is a special case of the electrostatic attractive interaction between polar molecules, in which hydrogen is bound to a highly electronegative atom like nitrogen or oxygen. A hydrogen bond is weaker than electrostatic force but stronger than a van der Waals interaction. Hydrophobic bonds are entropy-driven interactions between nonpolar groups to avoid interaction with polar groups, mainly water. Hydrophobic bonds are stronger than van der Waals interaction. Because these forces vary in their strength and dependence on the distance between components, the combination of all these forces directs the positioning of a ligand on the receptor-binding site with minimal free energy. A measure of attraction of the ligand to the binding site is termed affinity. Thermodynamic movement does not allow ligands to sit still in the binding site and makes them associate and dissociate from the receptor, even at equilibrium. Thus, the probability with which a ligand is bound to (stays at) the binding site of a receptor is given by ligand concentration, temperature, and strengths of interactions. Dependence of the ligand binding on its concentration (Fig. 1 black curve) is defined by Langmuir isotherm:
where square brackets designate concentration and K D is the equilibrium dissociation constant that is equal to concentration at which the binding site is occupied with 50 % probability (for [L] = K D expression is equal to 1/2 while for [L] ≫ K D it limits to 1).
2.2 Radioligands
The aim of binding experiments is to quantify ligand binding to the receptor under given conditions. Labeling the ligand with a radioactive isotope allows easy and sensitive quantification of binding and (unlike fluorescent labeling) does not interfere with ligand binding. High specific radioactivity is required, so ligand binding translates to high signal. Low nonspecific binding is required for high signal-to-noise ratio. Finally, a good radioligand should have high affinity for the receptor to prevent ligand dissociation from the receptor during the separation of free and bound radioligand. High affinity also affords the use of low concentrations of expensive radioligands.
2.3 Ligand-Specific Binding
Ligand binding to a receptor is a dynamic process of attraction mediated by chemical forces and disruption of binding by thermal movement of molecules. As a result a ligand incessantly associates with and dissociates from the receptor with time. Ligand (L) binding to the receptor (R) and formation of ligand-receptor complexes (LR) can be described as a reversible bimolecular reaction:
where k On is the association rate constant and k Off is the dissociation rate constant. The observed rate of association is directly proportional to the concentration of receptor, ligand, and k On. While the rate of dissociation of a ligand from the receptor (k Off) is only a property of the affinity of binding, the amount of remaining ligand-receptor complex at any moment is dependent on the starting amount of the complexes prior to the onset of dissociation. Thus, for any given moment the magnitude of change of the concentration of the ligand-receptor complex is given by the difference between formation and decay of ligand-receptor complexes:
Under binding equilibrium the change in LR is nil and formation of LR happens at the same rate as its decay:
The ratio of k On and k Off defines ligand affinity. Affinity (also known as equilibrium association constant) is a measure of attraction between ligand and receptor and thus is directly proportional to k On and inversely proportional to k Off. Equilibrium dissociation constant K D is the reciprocal value of equilibrium association constant and defines the ligand concentration necessary to occupy 50 % of receptors (see Eq. (1)). Restating Eq. (3) gives K D as
At any time the total number of receptors [RT] is the sum of free receptors and receptors in complex with the ligand:
or
Substitution of R in Eq. (4) according Eq. (5b) gives Eq. (6a):
or
or
or
and finally
that is actually Eq. (1) of specific binding related to concentration (or number) of binding sites RT.
2.4 Ligand Nonspecific Binding
Apart from the specific binding site on the receptor a ligand may also bind to other sites on the biological sample by nonspecific interaction that is by orders of magnitude weaker than specific binding. Nonspecific binding is linearly proportional to ligand concentration and in principle has infinite binding capacity (non-saturable) (Fig. 1, red curve). Nonspecific binding is not only given by chemical properties of the radioligand but also by arrangement of the experiment (e.g., sample washing, removal of tissue components that do not express the receptor). The magnitude of nonspecific binding is determined in the presence of excess of a highly specific non-labeled ligand sufficient to fully occupy the receptor. For example 1 μM atropine is commonly used for determination of nonspecific binding of muscarinic ligands. Higher concentrations should be avoided as it may slow down tracer dissociation [5] and so lead to overestimation of nonspecific binding. A ligand from the same pharmacological class but different from the radiolabeled ligand is preferred. A non-labeled ligand of the same chemical structure may bind to the same nonspecific sites and protect them from tracer binding so that these nonspecific binding sites are erroneously counted as specific binding sites. Ideally, several different unlabeled competitors should all yield statistically indistinguishable estimates of nonspecific binding. The ratio of nonspecific to specific binding should be as low as possible (less then 1 % of total added radioactivity to the sample and less than 10 % of total binding in case of muscarinic receptors). Washing is the least accurate step in the radioligand binding assay. Since nonspecific binding is affected by washing, variations in washing lead to variations in nonspecific binding. Thus, nonspecific binding should be determined in each filtration.
3 Radioligand Binding Experiments at a Glance
A radioligand binding experiment consists of these steps: (1) preparation of samples from tissues, cell cultures, or cell lines; (2) incubation of samples with radioligand; (3) separation of free radioligand from the bound one; (4) scintillation counting to determine radioactivity of individual samples; and (5) data analysis. Therefore, two pieces of specialized devices (besides common laboratory equipment) are needed to conceive radioligand binding experiments: first, an apparatus for separation of free and bound radioligand for which purpose cell harvesters are most commonly used; second, a scintillation counter compatible with the format of apparatus used for separation of free and bound radioligand. For example, a scintillation counter that can read filtration plates is needed when filtration plates are used in the cell harvester.
4 Available Radioligands
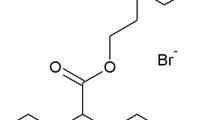
Nowadays available muscarinic radioligands cover almost all experimenter needs. Available radioligands include both reversible antagonists and agonists as well as covalent ligands, antagonists with fast as well as slow kinetics, and antagonists selective to M1, M2, and M3 subtypes. A list of common muscarinic radioligands is shown in Table 1. Their structures and chemical names are depicted in Fig. 2.
4.1 Antagonist Radioligands
Muscarinic receptor antagonists are preferred over agonists as tracers because of their higher affinity (Table 1). The most commonly used tracers are N-methylscopolamine (NMS) and quinuclidinyl benzilate (QNB). NMS exhibits slightly lower affinity at M2 and M5 receptor subtypes (Table 1). Tritiated NMS is commercially available at high specific radioactivity (80 Ci/mmol). The half-life of ligand-receptor complex is around 15 min at M1, M3, and M4 receptors, 3 min at the M2 receptor, and 53 min at the M5 receptor [6]. Combined with a rather fast rate of association, NMS is suitable for most common radioligand binding studies. Half-life of the complexes is short enough to reach equilibrium and slow enough for ligand separation by simple filtration. The advantage of QNB over NMS is its higher affinity and lower nonspecific binding (mainly to glass-fiber filters thanks to the absence of the positive charge). However, commercially available tritiated QNB has lower specific radioactivity (50 Ci/mmol). Moreover, QNB has extremely slow kinetics. Half-life of QNB in complex with muscarinic receptors is around 100 min, at M5 receptors even 180 min [6]. Slow kinetics of QNB may be problematic when attaining the equilibrium quickly is needed but may be of advantage when samples are washed from free radioligand (e.g., washing tissues for radioimaging) or ligand separation is slow (e.g., gel filtration, see Protocol F). Finally, the lipophilic nature of QNB results in its uptake into cells, which causes significantly high levels of nonspecific binding in intact cell studies. Pirenzepine is M1-selective antagonist (Table 1) that is commonly used for selective labeling of M1 receptors in samples with mixture of receptor subtypes. The use of other selective as well as nonselective radiolabeled antagonists has been reported; however, they have in general lower affinity than NMS (Table 1) and thus are less suitable for routine radioligand binding experiments.
4.2 Agonist Radioligands
There are two commercially available tritiated muscarinic agonists, the nonselective acetylcholine and the M2 preferring oxotremorine. In general, muscarinic agonists are not good tracers because of their low affinity (Table 1). Moreover, only receptors in high-affinity states (receptors in complexes with GDP-free G-protein) [7] can be detected by radiolabeled agonists. Thus agonists as tracers are employed only when specific effects on agonist binding have to be determined [8]. The use of acetylcholine as a tracer at muscarinic receptors is limited by several factors. First, acetylcholine binds both to muscarinic and nicotinic types of acetylcholine receptors. Second, acetylcholine is readily cleaved by cholinesterases (acetylcholinesterase and butylcholinesterase) that are omnipresent in animal tissues either in a free form in body fluids or anchored to plasma membranes [9]. To use acetylcholine as a tracer samples has to be devoid of cholinesterases (e.g., membrane preparations of non-neural cell lines) or activity of cholinesterases has to be blocked by specific inhibitors. However, many of acetylcholinesterase inhibitors are allosteric modulators of muscarinic receptors [10] and affect binding of muscarinic ligands. Moreover, the ester bond of acetylcholine is not chemically stable and acetylcholine decays spontaneously in aqueous solution to acetate and choline. Commercially available tritiated acetylcholine is radiolabeled either at acetate or choline group. It is easier (and cheaper) to label acetylcholine to high specific radioactivity at the choline group. However, acetylcholine labeled in this manner has high nonspecific binding due to traces of labeled choline from acetylcholine chemical decay that is hard to wash from nonspecific sites due to its positive charge. In contrast, radiolabeling of acetylcholine at the acetate group gives low nonspecific binding. Carbachol may be considered as an alternative to acetylcholine. It is similar to acetylcholine in structure, has similar affinity, and is resistant to cholinesterases. Unfortunately, radiolabeled carbachol is not commercially available. Unlike acetylcholine oxotremorine is chemically stable, is not a substrate for cholinesterases, and is specific for the muscarinic type of acetylcholine receptors. However, oxotremorine has much lower affinity than acetylcholine (Table 1).
4.3 Irreversible Radioligands
Two radiolabeled ligands, the agonist acetylcholine mustard (ACM) [4] and the antagonist propylbenzilyl choline mustard (PBCM) [3], form covalent bonds with muscarinic receptors. The advantage of covalently bound, practically irreversible tracers is that binding withstands long-lasting sample manipulation (like receptor isolation, electrophoresis, or immunoprecipitation) without ligand dissociation. The disadvantage of these tracers is that their nonspecific reactivity (binding) cannot be prevented by reversible antagonists (irreversible ligand always wins over reversible one in competition for binding) nor removed by washing (because tracer is bound irreversibly). Thus these tracers are suitable only for at least partly purified receptors.
5 Source of Muscarinic Receptors
5.1 Tissues
Muscarinic receptors are expressed throughout the body at the central nervous system, peripheral neurons, as well as target tissues innervated by cholinergic neurons (primarily parasympathetic neurons) [11] (Table 2). Almost all tissues express a mixture of subtypes of muscarinic receptors; for example smooth muscles express M2 and M3 receptors, and lungs express M2 and M4 receptors. Natural expression of M5 receptor is limited only to certain parts of brain like the ventral tegmental area and substantia nigra [12, 13]. Muscarinic receptors were also reported in non-neuronal non-innervated cells like lymphocytes [14]. Tissues may serve as a source of membranes or purified receptors (Sections 5.3 and 5.4) or used in binding experiments in whole, as slices, dissipated cells, or tissue culture.
5.2 Cell Lines
Besides expressing a mixture of muscarinic receptors another drawback of animal tissues as a source of muscarinic receptors is the relatively low density of receptor expression (less than 1 pmol of binding sites per mg of membrane proteins). Since cloning of all five subtypes of muscarinic receptors CHO cell lines stably expressing individual subtypes of muscarinic receptors in high density have become available and widely used [15]. Although muscarinic receptors were detected in naive CHO-K1 cells by highly sensitive second messenger assays [16] they cannot be detected in binding studies. Thus CHO cell lines are a widely used source of individual subtypes of muscarinic receptors in radioligand binding studies. Currently CHO cells stably expressing individual subtypes are available also from commercial sources (e.g., Perkin Elmer; Missouri S&T cDNA Resource Center). Muscarinic receptors are also routinely transiently expressed in COS-7 or HEK-293 cell lines [17, 18]. Since these cells have to be prepared anew for each binding experiment, stable transfection is usually used for studies of native receptors. Transiently transfected cells become quite useful for studying the binding characteristics of a large number of engineered receptor constructs, e.g., in receptor mutagenesis studies.
5.3 Membranes
The use of membranes instead of whole tissue or cells in binding experiments facilitates separation of bound and free radioligand and eliminates nonspecific binding to tissues and cellular components that do not express the receptor. The use of membranes rather than intact cells removes GTP that uncouples the receptor from G proteins. This increases agonist affinity and enables the use of radiolabeled agonist. Protocols A and B yield a mixture of plasma membranes, light membrane vesicles, and mitochondria, and are a practical compromise between purity of sample and receptor yield. Membrane preparation according to Protocol A results in 10–30 % of high-affinity sites for agonists (receptors in complex with GDP-free G-protein). Protocol B is modification of Protocol A that facilitates GDP dissociation [19] and subsequent formation of high-affinity complexes of receptor. This makes membranes suitable for experiments with radiolabeled agonists.
5.4 Purified Receptors
Isolation of purified muscarinic receptors may be desired for specific purposes (like determination of effects of membrane or membrane composition on receptor binding properties). Preparation of purified muscarinic receptors is described in Protocol C. It should be noted that a source with high expression density of muscarinic receptors like transfected Sf9 cells [20] has to be used. Purified receptors can be reconstituted in artificial lipid vesicles [21]. Protocol D describes reconstitution of purified receptors into artificial vesicles with a simplified composition of common membranes (cholesteryl hemisuccinate:phosphatidyl choline:phosphatidyl inositol, 4:48:48) that can be varied as desired [22] and optionally purified G-proteins may be added [23].
Protocol A: Preparation of membranes for general use
-
1.
Put tissue or cells of your choice in ice-cold homogenization medium (e.g., 100 mM NaCl, 10 mM EDTA, 20 mM HEPES buffer pH = 7.4). Keep on ice during steps 1 and 2. Homogenization medium should contain EDTA to stop calcium-dependent proteases. Protease inhibitors should be used with caution as they may modify muscarinic receptors and affect their binding properties [ 24 , 25 ]. Homogenization medium should have more or less normal ionic strength for steps 3 and 4 to work. If for any reason low ionic strength medium has to be used centrifugal force and duration of centrifugation in steps 3 and 4 need to be increased and extended because low ionic strength improves membrane dispersion that results in increased membrane flotation and thus greater centrifugal forces and longer times are needed to sediment the membranes.
-
2.
Homogenize the sample by the method of your choice (e.g., in Ultra-Turrax homogenizer by two 30-s strokes with 30-s pause between strokes) while cooling them on ice.
-
3.
To remove unbroken cells, cell nuclei, cytoskeleton, and extracellular matrix proteins spin down the samples at 1000 × g for 5 min and take the supernatant for the next step. During preparation of certain tissues rich in lipids (like brain cortex) the lipid foam that forms on top of the water phase needs to be discarded.
-
4.
To remove the cytosolic fraction spin down the supernatant from step 3 at 30,000 × g for 30 min. Remove the supernatant and dissolve pellet in incubation medium (e.g., 100 mM NaCl, 10 mM MgCl 2 , 20 mM HEPES buffer pH = 7.4).
-
5.
Leave samples for 30 min at 4 °C.
-
6.
Spin down samples at 30,000 × g for 30 min and discard supernatant.
-
7.
Pellets may be stored for limited time (couple of months) frozen at −20 °C or below.
Protocol B: Preparation of membranes for experiments with radiolabeled agonists
Steps 1–3 are the same as in Protocol A.
-
4.
To remove the cytosolic fraction spin down supernatant from step 3 at 30,000 × g for 30 min. Remove supernatant and dissolve pellet in 1 M ammonium sulfate.
-
5.
Allow samples to denature for 3 h at 4 °C.
-
6.
Spin down samples at 60,000 × g for 60 min, discard supernatant, and dissolve pellet in incubation medium containing 20 % glycerol.
-
7.
Leave samples for 1 h at 4 °C to renaturate.
-
8.
Spin down samples at 60,000 × g for 60 min, discard supernatant, and dissolve pellet in incubation medium.
Continue with steps 5–7 from Protocol A.
Protocol C: Preparation of purified muscarinic receptors
-
1.
Harvest Sf9 cells by centrifugation at 1500 × g for 10 min.
-
2.
Prepare crude membranes according to steps 1–4 of Protocol A.
-
3.
Dilute crude membranes in 20 mM HEPES buffer pH = 7.4, 5 mM imidazole, 1 mM EDTA, 1 % digitonin, and 0.1 % sodium cholate to a protein concentration of 1 mg/ml.
-
4.
Incubate stirred for 1 h at 4 °C.
-
5.
Centrifuge at 100,000 × g for 90 min at 4 °C and take the supernatant fraction.
-
6.
Apply 1 l of supernatant fraction from step 5 to ABT-agarose [ 26 ] column (300 ml) at 4 °C at a flow rate of 70 ml/h.
-
7.
Wash the column with 15 l of washing medium (0.2 M NaCl, 20 mM potassium phosphate buffer (pH 7.0), 0.1 % digitonin).
-
8.
Connect hydroxyapatite column (1 ml) to the outflow of ABT-agarose column.
-
9.
Apply 700 ml of the washing medium supplemented with 0.1 mM carbachol (to dissociate receptors from affinity column) to the ABT-agarose column at the same rate as above (carbachol is preferred over atropine in this step for easier removal in step 11).
-
10.
Disconnect hydroxyapatite column from ABT-agarose column and elute purified receptors with 0.5 M potassium phosphate buffer (pH = 7.0) containing 0.1 % digitonin.
-
11.
Prior to performing the radioligand binding experiment remove bound carbachol by 50-fold dilution in 0.5 M potassium phosphate buffer (pH = 7.0) containing 0.1 % digitonin. Allow carbachol dissociate for 1 h at 4 °C and then concentrate receptors by centrifugation through Centricon-30 membranes (Amicon Co., Ltd.).
Protocol D: Reconstitution of receptors into artificial vesicles
Steps 10 and 11 are optional.
-
1.
Prepare 4 mg of lipids by combining 16 μl of cholesteryl hemisuccinate (10 mg/ml in methanol), 48 μl of phosphatidyl choline (20 mg/ml in chloroform), and 48 μl of phosphatidyl inositol (20 mg/ml in chloroform) in glass tube.
-
2.
Form lipid film on the wall of tube by evaporation with N 2 .
-
3.
Add 1 ml of solution A (100 mM NaCl, 1 mM ETDA, 20 mM HEPES pH = 7.4) supplemented with 1 % sodium cholate.
-
4.
Sonicate on ice for 20 min.
-
5.
Combine 66 μl of receptors (300 pmol/ml), 32 μl of solution A, and 100 μl of lipid vesicles from step 4. Vortex vigorously and leave on ice for 30 min.
-
6.
Wash 2 ml Sephadex G-50 fine-grade columns with 5 ml of solution A.
-
7.
Apply mixture from step 5 to Sephadex G-50 column.
-
8.
Wash column three times with 0.2 ml of solution A.
-
9.
Add 0.4 ml of solution A and collect.
-
10.
Mix 0.2 ml of receptor vesicles (~10 pmol of receptors) from step 9 with 28 μl of G-proteins (~50 pmol), 1.25 μl of 2 M MgCl 2 , 1.25 μl of 1 M dithiothreitol, and 19.5 μl of solution A and vortex vigorously.
-
11.
Leave on ice for 60 min.
-
12.
Dilute with 5 volumes of solution A and use 50 μl per sample in binding assay.
6 Incubation Conditions
6.1 Buffers
Many types of buffers may be used for radioligand binding experiments. However, it should be noted that buffer composition influences ligand affinity. Low concentrations of sodium (low ionic strength in general) lead to higher affinity and slower dissociation of the tracer [27]. This is desired in experiments with tracers with low affinity and fast dissociation like agonists. Agonists bind to complexes of receptor and GDP-free G-protein. Formation of these complexes is conditioned by the presence of magnesium ions [23]. For routine measurements on membranes thus simple buffer consisting of 100 mM NaCl, 5 mM MgCl2, and 20 mM HEPES buffer pH = 7.4 is suitable for a wide range of tracers. For binding experiments on whole cells iso-osmotic buffer (like Krebs-HEPES buffer: 138 mM NaCl, 4 mM KCl, 1.3 mM CaCl2, 1 mM MgCl2, 1.2 mM NaH2PO4, 10 mM glucose, 20 mM HEPES pH = 7.4; 340 mOsm/l) has to be used. An advantage of Krebs-HEPES buffer is that many functional assays like accumulation of inositol phosphates, inhibition of cAMP synthesis, or microfluorometric determination of intracellular calcium can be conducted in it. This allows the comparison of ligand affinity in binding and functional studies under similar conditions [28].
Another consideration is the addition of chelating agents for their beneficial effects. Chelating agents may inhibit possible contamination with proteases. Chelating agents in combination with low ionic strength promote membrane dispersion and thus improve handling properties of membrane preparations. On the other hand chelating agents significantly perturb ligand interactions by removing multivalent ions. As stated above magnesium ions are essential for agonist high-affinity binding.
6.2 Sample Size
For radioactivity of the sample to be counted accurately it should be about 1000 cpm (about 2000 dpm for tritiated ligands on the assumption of 50 % efficiency of counting). Typical specific radioactivity of tritiated commercial grade muscarinic radioligand is 160 dpm/fmol that translates to 12.5 fmol radioligand occupied sites per sample to achieve 2000 dpm of specific binding. The best ratio of specific to nonspecific binding is observed around ligand K D. When radioligand in concentration equal to K D is used 50 % of binding sites are occupied by radioligand. Thus 25 fmol of receptors per sample is needed to get 2000 dpm of specific binding. Membranes prepared according to Protocol A from CHO cells stably expressing muscarinic receptors usually have 1–10 fmol of receptors per microgram of proteins; thus 10–20 μg of protein per sample is generally used. However, agonists bind with high affinity only to receptors in complex with GDP-free G-protein that represent only a fraction of total receptors. Thus, up to five times more membranes are needed in comparison to antagonist binding. The capacity limit of filtration on 96-well plates (filter diameter 5 mm) is 100 μg of protein per sample. This means that only membranes from high-expression systems like cell lines or brain cortex (0.5 fmol/μg of protein) can be used in this compact and economic assay. Tissue homogenates or preparations from low-expressing systems (0.1 fmol/μg of protein or lower) like lung [29] have to be filtered through filters with higher capacity like 24-tube cell harvester (filter diameter 15 mm) which maximum capacity is about 1 mg of proteins.
6.3 Incubation Volume
Incubation volume is determined by the method of separation of bound and free radioligand. In separation on gel filter the incubation volume is equal to the loading volume, which is dependent on the volume of the column (e.g., for 2 ml G-50 Sephadex column 50 μl of loading volume is required). In scintillation proximity assay the incubation volume is only limited by the size of well or tube. In separation on filters the incubation volume is related to the size of the filter. Larger filters require larger washing volumes and thus larger incubation volumes. The larger the area of the filter, the higher the capacity and more membranes, cells, or tissue can be and should be used. Large filters (like in 24-tube Brandel cell harvester) are thus suitable for preparations with low receptor density, and therefore require a large amount of biological sample, e.g., non-neural tissues. For 24-tube filtration (filter diameter 15 mm) the optimal incubation volume is about 3 ml; for 96-well filtration (filter diameter 5 mm) the optimal incubation volume is about 0.4 ml.
Another aspect that influences the size of incubation volume is the combination of tracer amount, tracer affinity, and number of binding sites in the sample. If the amount of the tracer in relation to the tracer affinity and the number of binding sites is low a substantial part (>10 %) of the tracer is bound to the receptors. Such conditions are termed tracer depletion and may happen usually in saturation binding experiments. Tracer depletion complicates data analysis because the free tracer concentration is significantly lower than that inferred from the amount of added tracer (radioactivity) and final incubation volume. The incubation volume should be increased if it is estimated that there is a risk of tracer depletion. For such cases 1.2 ml 96-well plates are available. When the incubation volume of samples intended for gel filtration is increased the volume of the gel column has to be proportionally increased. On the other hand when tracers with low affinity (like agonists) are used the incubation volume can be reduced to save expensive radioligand. However, in a 96-well plate Brandel cell harvester samples with volume smaller than 0.2 ml are difficult to apply and wash reliably. In case of gel filtration a smaller incubation volume can be diluted with ice-cold buffer to the desired volume and applied to the gel column of the standard size.
6.4 Temperature
As explained above in Section 2 temperature affects ligand binding. An increase in temperature potentiates thermal movement of molecules including the receptor and the ligand but the strength of intermolecular forces remains the same. Temperature dependence of the affinity constant K A and equilibrium dissociation constant K D is described by the Van’t Hoff equation:
where ΔG is free binding energy, ΔH is enthalpy of binding, ΔS is entropy of binding, and R and T are gas constant and absolute temperature, respectively. Enthalpy contribution to equilibrium ligand binding is small. The major contribution to the thermodynamics of ligand binding is change in entropy (mainly ligand desolvation on association with receptor). Temperature dependence of equilibrium constants is thus relatively small; however it is still about twofold change over 10 °C (the difference between room temperature and body temperature). An increase in temperature usually leads to a decrease in affinity unless hydrophobic effects (which strengthen with temperature) contribute to ligand binding substantially [30]. Thanks to relatively low temperature dependence of equilibrium binding incubation temperature can be often chosen to be the same as in other types of assays in the conducted study (e.g., 37 °C as in study of functional response). For study of agonist binding 30 °C appears to be optimal as the fraction of high-affinity sites for agonists is at its maximum [31].
Temperature dependence of the association rate constant k On is described by the Arrhenius equation:
where k B and ħ are Boltzmann’s and Planck’s constants, respectively. Usually there is large enthalpic contribution to kinetics of ligand association with receptor that gives it large temperature sensitivity. Thus thermodynamics of ligand binding may be inferred by assessing temperature dependence of the rate of association. For muscarinic ligands a 10 °C increase in temperature may lead to a tenfold increase in the rate of association. Thus, time of incubation of a radioligand with the receptor source in equilibrium binding studies must be increased if a lower temperature is employed. For tracers with fast kinetics like muscarinic agonists the very short time steps required to accurately determine the rate of association may be unattainable by available technique and lowering incubation temperature to slow down the rate of association may be considered.
7 Radioligand Separation
As stated above separation of free radioligand from the bound one is the most crucial step of the procedure. Separation, on the one hand, must not disturb the formed ligand-receptor complex (has to be quick). On the other hand it has to be complete (since any remains of free radioligand counts as nonspecific binding). Thus optimization of separation step is about finding a balance between the duration of separation and intensity of washing.
7.1 Radioligand Binding in Cell Membranes
The simplest method to separate free radioligand from the bound one is filtration through glass-fiber filters (Protocol E) where due to difference in the size membranes with bound radioligand are retained on the filter and free radioligand passes through it. Tracer nonspecific binding is reduced in the filtration assay by washing the filters. Nonspecific binding should be determined for each filtration as it may vary among filtrations due to variations in the process of washing (that is the step with lowest precision and main source of variation). Solubilized receptors and purified receptors reconstituted in artificial lipid vesicles are small enough to pass through glass-fiber filters. For radioligand separation either gel filtration (Protocol F) or scintillation proximity assay (Protocol G) can be used. Filtration times on gel filter are long; thus radioligands with slow dissociation (e.g., QNB) have to be used. Although filtration on gel filters can be expedited by centrifugation of gel columns it is not suitable for radioligands with fast kinetics like agonists and certain antagonists. In gel filtration free radioligand is trapped in the gel pores and receptors while bound radioligand is eluted in void volume. In scintillation proximity assays receptors with bound radioligand are coprecipitated with scintillation beads by antibodies, so only bound radioligand is close enough to scintillation beads and scintillates.
Protocol E: Filtration through glass-fiber filters in a 96-well plate setup
-
1.
If the used radioligand has positive charge (e.g., NMS, NMQNB, acetylcholine) soak filters in 0.5 % solution of polyethylenimine to lower radioligand adsorption to filters.
-
2.
Place GF/C filter or filtration plate into Brandel filtration apparatus and wash it with ice-cold deionized water to remove bubbles from tubing.
-
3.
Place incubation 96-well plate on Brandel filtration apparatus, harvest the samples, and immediately wash the samples with the ice-cold deionized water (QNB and NMQNB for 9 s, other antagonists for 6 s, agonists for 3 s).
-
4.
Let harvest vent open for at least 30 s to remove excess moisture from filter.
-
5.
Take filter or filter plate out of Brandel filtration apparatus and dry it in microwave oven at maximum power for 2 min.
-
6.
For glass-fiber filters, melt on Metltilex A solid scintillator for 90 s on 105 °C hot plate. For filtration plates, seal the bottom of the plate with transparent tape, add 50 μl of liquid scintillator to each well, and seal top of the plate with transparent tape.
Protocol F: Gel filtration
-
1.
Prepare 2 ml Sephadex G-50 fine-grade columns and wash them with 5 ml of washing solution (100 mM NaCl, 1 mM EDTA, 20 mM HEPES buffer pH = 7.4, 0.05 % Lubrol PX).
-
2.
Add 0.2 ml of washing solution to samples (incubation volume 50 μl) and apply to column immediately.
-
3.
Add 0.1 ml of washing solution to columns.
-
4.
Place 6 ml scintillation vials under the columns. Elute with 1 ml of washing solution.
-
5.
Add 4 ml of water-compatible scintillation cocktail (e.g., EcoLite, Rotiszint, OptiPhase) to scintillation vials.
Protocol G: Scintillation proximity assay
-
1.
If membranes were incubated solubilize them by the addition of 20 μl of 10 % Nonidet P-40 and shake the samples for 20 min.
-
2.
Add 10 μl of rabbit polyclonal IgG antibody against muscarinic receptor in a final dilution of 1:5000 and incubate for 1 h.
-
3.
Dilute one batch of anti-rabbit IgG-coated scintillation beads in 40 ml of incubation medium. Add 50 μl of the scintillation bead suspension to each sample and incubate for 3 h.
-
4.
Centrifuge samples for 15 min at 1000 × g and count samples using the scintillation proximity assay protocol. If the background radioactivity due to scintillation of free ligand is too high filter samples through GF/C filter plate according to Protocol E.
7.2 Radioligand Binding in Intact Cells
For separation of free and bound radioligand in case of the cells in suspension (e.g., Sf9 cells, detached CHO cells, dissociated tissues, or tissue cultures) filtration through glass-fiber filters with large pores (Whatman GF/A) according to Protocol D is the most straightforward approach. Alternatively cells may be centrifuged for 3 min at 250 × g. This method does not allow complete removal of the free radioligand and is therefore associated with high nonspecific binding. It is preferred for radioligands with very fast dissociation that does not allow washing that is necessary in case of filtration.
Protocol H: Processing of attached cells grown on 24-well plate
-
1.
Remove cell culture media and wash the cells with 0.5 ml of Krebs-HEPES buffer (KHB; final concentrations in mM: NaCl 138; KCl 4; CaCl 2 1.3; MgCl 2 1; NaH 2 PO 4 1.2; Hepes 20; glucose 10; pH adjusted to 7.4).
-
2.
Incubate cells with radioligand in 0.5 ml (final volume) of KHB for 20 min (NMS) or 12 h (QNB).
-
3.
Remove incubation medium and quickly wash cells twice with 0.5 ml of KHB removing it immediately.
-
4.
Dissolve cells in 0.4 ml of 1 M NaOH and shake the plate for 15 min at room temperature.
-
5.
Pipet 0.2 ml aliquot to 4 ml scintillation vials and add 3 ml of water-compatible scintillation cocktail (e.g., EcoLite, Rotiszint, OptiPhase).
8 Experimental Arrangement
Arrangement of the binding experiment must conform to the specific parameters intended to be determined. In so-called kinetic experiments time of incubation varies while other parameters remain constant and the association rate constant k On or dissociation rate constant k Off is determined. In so-called equilibrium experiments time of incubation is constant and long enough to achieve binding equilibrium and the concentration of ligand is varied to determine the equilibrium dissociation constant K D and number of receptors RT.
8.1 Measurement of the Rate of Association
Usually association experiments are performed first to determine the time needed to achieve equilibrium that is a prerequisite for dissociation and equilibrium binding experiments. In association experiments samples are incubated with a constant concentration of tracer for different periods of time and dependence of ligand binding on time is evaluated. Association is usually started by the addition of tracer to free receptor and terminated by tracer removal. When tracer is added to free receptors the concentration of ligand-receptor complexes rises according to Eq. (9) that is the integral of Eq. (2) over time:
[LREq] is the concentration of LR under equilibrium according to Eq. (6e). In association experiments the tracer both associates with and dissociates from the receptors. Thus neither k On nor k Off can be determined. Instead the observed rate association constant k Obs is calculated according Eq. (10):
Theoretical association curves are shown in Fig. 3. The association rate constant k On is calculated after subtraction of k Off determined in dissociation experiments and division by ligand concentration. Association of muscarinic antagonists is easy to measure as NMS reaches equilibrium within minutes and QNB in hours [5]. However, the logarithmic shape of the association curve dictates that the initial time intervals of measurement should be in the fractions of minute for NMS. Kinetics of muscarinic agonists are much faster than kinetics of antagonists. Acetylcholine reaches equilibrium from within 1 (M5 receptors) to 3 min (M3 receptors) [8]. Thus time steps should be as short as possible. With the aid of pipetting robots the initial steps can be as short as 2 s. The association rate is strongly dependent on the temperature, so lowering incubation temperature to slow down association may be considered. Due to the rushed nature of association experiments samples of nonspecific binding should be preincubated with unlabeled ligand to allow association with all specific sites. When atropine is used for determination of nonspecific binding 30-min preincubation is sufficient. Formation of nonspecific binding is instant and is not time dependent. Thus determination of nonspecific binding at a single time point is sufficient. In determination of nonspecific binding a non-labeled, chemically distinct, highly specific ligand is used at a receptor saturating concentration (e.g., 1 μM atropine). Much higher concentrations should not be used to avoid blockade of nonspecific binding sites. The latter appears as a fraction of binding sites with extremely fast rate of association.
Theoretical association curves. Abscissa, time. Ordinate, tracer binding expressed as a fraction of total receptor RT. Upper graph: Relationship between the association rate constants k On (indicated in legend as the ratio to equilibrium dissociation constant K D) on the association of L in a concentration equal to K D. When L is equal to K D equilibrium binding represents 50 % of total receptors regardless of the association rate. Increasing k On accelerates association and equilibrium is achieved earlier. Lower graph: Effects of changing the concentration of L (indicated in legend as ratio to equilibrium dissociation constant K D) for ligand with k On equal to 0.25 × K D. Increasing concentration of L both accelerates association and increases equilibrium binding
8.2 Measurement of Dissociation
In dissociation experiments samples are first preincubated with tracer. Equilibrium binding should be reached prior to initiation of dissociation. To safely reach equilibrium preincubation should last at least 5 min for acetylcholine, 20 min for NMS or atropine, and 3 h for QNB or NMQNB. Dissociation of tracer can be achieved by one of the two ways: (1) by removal of the tracer and (2) by addition of the excess of unlabeled ligand that prevents tracer association. The unlabeled ligand used for detection of nonspecific binding should be of a different chemical nature not to protect nonspecific binding sites that would appear as extremely fast dissociating sites. Tracer can be removed either by replacement of incubation medium with tracer-free medium (that is easily achievable by centrifugation or suction in case of whole tissues, cells in suspension, attached cell lines, and the like) or by dilution of incubation medium to lower tracer concentration substantially (at least 100 times). Medium for replacement or dilution should have the same temperature as preincubation medium to prevent temperature effects on dissociation. When dissociation is initiated binding starts to decline according to Eq. (11) that is a modification of Eq. (9) for zero concentration of L:
where [LR0] is tracer binding in the start of dissociation and is equal to [LREq] in Eq. (10) and [LR] in Eq. (6e) if equilibrium was reached. As is apparent from Eq. (11) the rate of dissociation is independent from used concentration of the tracer.
8.3 Measurement of Binding Saturation
Equilibrium dissociation constant K D and the number of binding sites in sample RT can be determined in saturation binding experiment where samples are incubated with various concentrations of the tracer. Under equilibrium tracer-specific binding depends on tracer concentration according to Eq. (6e). It should be stressed that Eqs. (6a), (6b), (6c), (6d), and (6e) were derived on the assumption that the concentration of tracer is much higher than the concentration of receptors and thus there is no ligand depletion. Therefore the concentration of free tracer is constant during the experiment. In practice this is not always true and free tracer concentration has to be calculated by subtraction of ligand binding from initial ligand concentration that is calculated as total radioactivity added to the sample divided by specific radioactivity of the tracer. It should be noted that this simple correction does not work for large tracer depletion that takes place at concentrations of the radioligand significantly below its K D. In such case the incubation volume has to be increased. Theoretical curves of saturation binding are shown in Fig. 4.
Theoretical saturation binding curves. Abscissa, concentration of free tracer. Ordinate, concentration of ligand-receptor complexes. Upper graph: Effects of tracer equilibrium dissociation constant K D (indicated in legend) on tracer binding for RT equal to 1. Lower graph: Effects of total receptor number RT (indicated in legend) on binding of tracer with equilibrium dissociation constant K D equal to 1
Because tracer nonspecific binding also depends on the concentration of the tracer it must be determined for each tracer concentration used and subtracted from total binding (Fig. 1). For K D and RT to be defined and reliably used the concentrations of tracer should be evenly distributed around K D. Using only high concentrations of the tracer leads to erroneous estimates of K D (usually underestimation) and using only low concentrations of the tracer leads to erroneous estimates of RT (usually overestimation). Extremely low and high concentrations of the tracer (far from K D) should be avoided as the ratio of specific to nonspecific binding is unfavorable (Fig. 1). If only RT is of interest a single saturating (several times K D) concentration of the tracer can be used (e.g., 1 nM NMS) as at concentrations saturating for tracer variation in K D has small effect on tracer binding. However, equilibrium time and K D should be determined in preliminary experiment. In typical saturation experiment eight concentrations of NMS ranging from 58 pM to 1 nM (starting with 1 nM and diluting it 3:2 in each step) are used.
8.4 Displacement (Competition) Binding
As shown in Table 1 the number of available radiolabeled muscarinic ligands is limited. However, there are means to determine the binding affinity of non-labeled ligands. For this purpose the ability of a non-labeled ligand to compete for specific binding of a radioligand and decrease tracer binding is utilized. In practice binding of the tracer at a fixed concentration is measured in the presence of various concentrations of the non-labeled ligand. If the binding of the non-labeled ligand X and tracer L is mutually exclusive then the amount of tracer-receptor complexes is given by Eq. (12) that is a combination of two equations (Eq. 6e) (one for tracer L and one for competitor X):
where K X is the equilibrium dissociation constant of non-labeled ligand X. For practical purposes the tracer binding can be expressed as its fraction in the absence of X:
where [LR0] is the tracer binding in the absence of X. Equation (13) can be further simplified for practical purposes by the introduction of IC50 value that represents the concentration of X that decreases the tracer binding to 50 %:
Equation (13) then becomes Eq. (15):
Theoretical curves of competitive binding are shown in Fig. 5, upper graph. As can be inferred from Eq. (14) IC50 is dependent on the ratio of L to K D. As the K D is constant IC50 depends on the concentration of L. The higher the concentration of L the higher the IC50; in other words the bigger is the ratio of the IC50 and K X. Equation (14) dictates that the ratio of IC50 to K X is equal to the ratio of L to K D plus 1 (Fig. 5, lower graph). Nonlinearity of the dependence of IC50 on K X on the ratio of L to K D implies that the interaction between the tracer and non-labeled ligand is not competitive, for example allosteric (see Chap. 6) or irreversible.
Competition binding. Upper graph: Competition binding of tracer L and competitor X. Abscissa, logarithm of ratio of competitor concentration [X] to its equilibrium constant [KX]. Ordinate, tracer binding [LR] expressed as fraction of total receptors [RT]. Ratio of the tracer concentration [L] to its equilibrium dissociation constant K D is indicated in the legend. Circles are IC50 at individual binding curves. Increasing tracer concentration leads to higher binding in the absence of competitor and to increase in IC50. Lower graph: Dependence of IC50 on tracer concentration. IC50 values (circles) from upper graph are plotted against tracer concentration. Abscissa, ratio of tracer concentration [L] to its equilibrium dissociation constant K D. Ordinate, ratio of IC50 concentration to competitor dissociation constant K X. Dependence is linear with slope equal to 1 and constant equal to 1
The application of competition binding study to determine equilibrium dissociation constant of non-labeled compound is obvious. Measurement of competition binding of tracer and non-labeled ligand with preferential affinity at individual receptor subtypes may also be applied to determine receptor subtypes and their proportion in analyzed sample [29]. A list of selective muscarinic ligands is shown in Table 3. Antagonists with varied degrees of selectivity are available for all receptor subtypes. However, no true binding selectivity was found in the case of muscarinic agonists.
8.5 Determination of Radioligand-Specific Radioactivity
The specific radioactivity is the amount of radiolabeled mass in a sample expressed as Ci/mol or Bq/mol. The specific radioactivity is required to compute mass amounts (e.g., total receptor number RT in saturation binding) from radioactivity measures of the sample. Specific radioactivity of commercial radioligands is provided by the manufacturer. For radioligands synthesized in-house the specific radioactivity can be estimated by comparing the K D value obtained by a tracer saturation binding with the value from a homologous competition experiment in which the same non-labeled ligand is used to displace the binding of the tracer. In saturation binding the concentration of radioactivity [dpm/l] at K D is assessed according to Eq. (6e). Then in a homologous competition experiment the concentration of radioligand [mol/l] at K D is assessed according to Eq. (13). Specific radioactivity [in dpm/mol] is then calculated by division of radioactive concentration [dpm/l] by radioligand concentration [mol/l]. Figure 6 shows a typical saturation experiment and homologous competition for the determination of specific radioactivity. It should be noted that the requirement of equal affinity necessitates that the non-labeled and labeled ligands are chemically identical. Thus, if the ligand is labeled with [125I], the non-labeled ligand must also be in the iodinated form.
Determination of specific radioactivity. Upper graph: Saturation binding of radiolabeled ligand L with unknown specific radioactivity. Abscissa, free radioactivity of the sample expressed in dpm. Ordinate, specific binding of the tracer expressed in dpm. Fitting Eq. (6e) to data gives maximum binding capacity RT at about 3600 dpm and equilibrium dissociation constant K D of tracer at about 38 million dpm. Lower graph: Homologous competition of the labeled ligand L with non-labeled chemically identical ligand X. Abscissa, logarithm of concentration of non-labeled ligand X. Ordinate, specific binding of labeled ligand L in dpm. Labeled ligand was used in a concentration close to its equilibrium dissociation constant K D as indicated by specific binding around 1900 dpm that is half of total receptor number RT in upper graph. Fitting Eq. (15) to data gives IC50 of 423 pM and equilibrium dissociation constant K D 212 pM. Dividing K D from upper graph by K D from lower graph gives specific radioactivity 178 dpm/fmol
9 Data Analysis
9.1 Regression Analysis
Parameters of ligand binding are determined by fitting the appropriate equation to the data by nonlinear regression. The most common assumption is that data points are randomly scattered on both sides of a curve. The goal of regression is to adjust parameters of the equation to find the curve that minimizes the sum of the squares of the differences in y-values of points and curve. Simple least square method weights each point equally. However there are methodological reasons to weight points differently. If the replicates show that standard deviation is dependent on y-value (the most common situation) then data points should be weighted according to y-value. When the standard deviation is proportional to the y-value (relative error to y-value is constant) like in Fig. 6 then it is appropriate to perform relative weighting (weighting by 1/Y 2). When the standard deviation follows Poisson distribution (e.g., error from radioactive counting) then Poisson weighting (weighting by 1/Y) should be performed. Error coming only from radioactive counting is rarely the case. In practice the source of variation is a mix of sources and general weighting (weighting by 1/Y k), where k is the slope of regression between standard deviation and y-value and ranges from 0 to 2. When k is zero or close to it then there is no correlation of standard deviation and y-value and no weighting is needed. It may be tempting at first glance to weight the data by standard deviation (weighting by 1/SD2) but a very large number of replicates (dozens of samples) are needed for weighting to be correct. However, the use of such large number of replicates is usually not the case in radioligand binding studies.
Distribution of binding parameter estimates from nonlinear regression follows data distribution along axes. Thus parameters determined from semilogarithmic plots (e.g., competition binding) are log normally distributed. This implies that the logarithms of these parameters (e.g., EC50) should be compared and statistically analyzed. Also in case of linear plots (e.g., saturation binding) uneven data distribution along the abscissa may skew distribution of binding parameter (e.g., K D) estimates. Thus it should be checked for normality.
9.2 Software
Data have to be preprocessed before fitting. Namely, replicates are averaged and standard deviations calculated. Specific binding is calculated by subtraction of nonspecific binding from total binding. Specific binding is converted to amounts of substance [mol] by division of radioactivity of the sample by specific radioactivity of the ligand. Then specific binding may be related to protein content of the sample, mass of tissue, etc. Used concentration of radioligand is determined by division of the amount of total radioactivity added to the sample by specific radioactivity of the radioligand and sample volume. The easiest way of data preprocessing is to use a spreadsheet software one is familiar with.
It is good practice to perform basic data analysis (like sample variation analysis or outlier identification) prior to nonlinear regression analysis. Nonlinear regression analysis to extract binding parameters and subsequent statistical analysis can be performed using various software ranging from software specialized to analysis of binding data, pharmacological or biochemical experiments, many plotting and curve fitting programs, as well as any general-purpose mathematical package. Table 4 lists several software packages suitable for analysis of binding experiments. A major advantage of specialized pharmacological programs is that they are easy to use and have built-in data preprocessing routines, pre-regression checks, predefined equations for all types of binding experiments, and implement various post-regression tests. The main disadvantage of these programs is their relatively high price and inability of scripting and incorporation into workflows with other software. On the other hand general-purpose mathematical and plotting programs are more knowledge demanding to the user but allow scripting and creation of various workflows. Some of them are open source and free of charge. For example for teaching purposes or when one does not have any specialized program at hand a simple least-sum-of-squares regression can be done even using common spreadsheet software (Protocol I).
Protocol I: Nonlinear regression analysis in spreadsheet
-
1.
Input variable (x values) in column A, and dependent variable (y values) in column B.
-
2.
Enter initial values for binding function parameters in column E.
-
3.
In column C enter binding function calling binding parameters from column E.
-
4.
In column D calculate square of deviations between cells in columns C and B in the current row.
-
5.
In the cell F1 calculate sum of values in column D.
-
6.
Open solver function of the spreadsheet and instruct it to minimize value in the cell F1 by changing values in column E. Choose Levenberg-Marquardt method if available.
10 Conclusions
Overall, the current status of radioligand binding experiments allows very accurate and detailed study of equilibrium binding, binding kinetics, and structure-activation relationship at muscarinic receptors. Binding experiments may be performed in various forms ranging from tissue cultures via whole cells to purified receptors when criteria discussed in this chapter are met. Their main limitation remains to be the lack of selective radiolabeled agonists and antagonists for some receptor subtypes.
References
Kubo T, Fukuda K, Mikami A, Maeda A, Takahashi H, Mishina M, Haga T, Haga K, Ichiyama A, Kangawa K, Masayasu K, Hisayuki M, Tadaaki H, Shosaku N (1986) Cloning, sequencing and expression of complementary DNA encoding the muscarinic acetylcholine receptor. Nature 323:411–416
Bonner TI, Buckley NJ, Young AC, Brann MR (1987) Identification of a family of muscarinic acetylcholine receptor genes. Science 237:527–532
Birdsall NJ, Burgen AS, Hulme EC (1979) A study of the muscarinic receptor by gel electrophoresis. Br J Pharmacol 66:337–342
Spalding TA, Birdsall NJ, Curtis CA, Hulme EC (1994) Acetylcholine mustard labels the binding site aspartate in muscarinic acetylcholine receptors. J Biol Chem 269:4092–4097
Jakubík J, El-Fakahany EE, Tuček S (2000) Evidence for a tandem two-site model of ligand binding to muscarinic acetylcholine receptors. J Biol Chem 275:18836–18844
Jakubík J, Bačáková L, El-Fakahany EE, Tuček S (1995) Subtype selectivity of the positive allosteric action of alcuronium at cloned m1–m5 muscarinic acetylcholine receptors. J Pharmacol Exp Ther 274:1077–1083
Jakubík J, Janíčková H, El-Fakahany EE, Doležal V (2011) Negative cooperativity in binding of muscarinic receptor agonists and GDP as a measure of agonist efficacy. Br J Pharmacol 162:1029–1044
Jakubík J, Randaková A, El-Fakahany EE, Doležal V (2009) Divergence of allosteric effects of rapacuronium on binding and function of muscarinic receptors. BMC Pharmacol 9:15
Massoulié J, Pezzementi L, Bon S, Krejci E, Vallette FM (1993) Molecular and cellular biology of cholinesterases. Prog Neurobiol 41:31–91
Jakubík J, El-Fakahany EE (2010) Allosteric modulation of muscarinic acetylcholine receptors. Pharmaceuticals 9:2838–2860
Eglen RM (2012) Overview of muscarinic receptor subtypes. Handb Exp Pharmacol 208:3–28
Eglen RM, Nahorski SR (2000) The muscarinic M5 receptor: a silent or emerging subtype? Br J Pharmacol 130:13–21
Felder CC, Bymaster FP, Ward J, DeLapp N (2000) Therapeutic opportunities for muscarinic receptors in the central nervous system. J Med Chem 43:4333–4353
Kawashima K, Fujii T (2008) Basic and clinical aspects of non-neuronal acetylcholine: overview of non-neuronal cholinergic systems and their biological significance. J Pharmacol Sci 106:167–173
Buckley NJ, Bonner TI, Buckley CM, Brann MR (1989) Antagonist binding properties of five cloned muscarinic receptors expressed in CHO-K1 cells. Mol Pharmacol 35:469–476
Wang SZ, Zhu SZ, El-Fakahany EE (1995) Expression of endogenous muscarinic acetylcholine receptors in Chinese hamster ovary cells. Eur J Pharmacol 291:R1–R2
Krejčí A, Tuček S (2001) Changes of cooperativity between N-methylscopolamine and allosteric modulators alcuronium and gallamine induced by mutations of external loops of muscarinic M(3) receptors. Mol Pharmacol 60:761–767
Arden JR, Nagata O, Shockley MS, Philip M, Lameh J, Sadée W (1992) Mutational analysis of third cytoplasmic loop domains in G-protein coupling of the HM1 muscarinic receptor. Biochem Biophys Res Commun 188:1111–1115
Ferguson KM, Higashijima T, Smigel MD, Gilman AG (1986) The influence of bound GDP on the kinetics of guanine nucleotide binding to G proteins. J Biol Chem 261:7393–7399
Rinken A, Kameyama K, Haga T, Engström L (1994) Solubilization of muscarinic receptor subtypes from baculovirus infected sf9 insect cells. Biochem Pharmacol 48:1245–1251
Jakubík J, Haga T, Tuček S (1998) Effects of an agonist, allosteric modulator, and antagonist on guanosine-gamma-[35s]thiotriphosphate binding to liposomes with varying muscarinic receptor/go protein stoichiometry. Mol Pharmacol 54:899–906
Berstein G, Haga T, Ichiyama A (1989) Effect of the lipid environment on the differential affinity of purified cerebral and atrial muscarinic acetylcholine receptors for pirenzepine. Mol Pharmacol 36:601–607
Shiozaki K, Haga T (1992) Effects of magnesium ion on the interaction of atrial muscarinic acetylcholine receptors and GTP-binding regulatory proteins. Biochemistry 31:10634–10642
Jakubík J, Tuček S (1994) Protection by alcuronium of muscarinic receptors against chemical inactivation and location of the allosteric binding site for alcuronium. J Neurochem 63:1932–1940
Jakubík J, Tuček S (1995) Positive allosteric interactions on cardiac muscarinic receptors: effects of chemical modifications of disulphide and carboxyl groups. Eur J Pharmacol 289:311–319
Haga K, Haga T (1985) Purification of the muscarinic acetylcholine receptor from porcine brain. J Biol Chem 260:7927–7935
Lysíková M, Fuksová K, Elbert T, Jakubík J, Tuček S (1999) Subtype-selective inhibition of [methyl-3H]-N-methylscopolamine binding to muscarinic receptors by alpha-truxillic acid esters. Br J Pharmacol 127:1240–1246
Santrůčková E, Doležal V, El-Fakahany EE, Jakubík J (2014) Long-term activation upon brief exposure to xanomleline is unique to m1 and m4 subtypes of muscarinic acetylcholine receptors. PLoS One 9:e88910
Jakubík J, Tuček S (1994) Two populations of muscarinic binding sites in the chick heart distinguished by affinities for ligands and selective inactivation. Br J Pharmacol 113:1529–1537
Jakubík J, Tucek S, El-Fakahany EE (2004) Role of receptor protein and membrane lipids in xanomeline wash-resistant binding to muscarinic m1 receptors. J Pharmacol Exp Ther 308:105–110
Aronstam RS, Narayanan TK (1988) Temperature effect on the detection of muscarinic receptor-g protein interactions in ligand binding assays. Biochem Pharmacol 37:1045–1049
Alexander SPH, Mathie A, Peters JA (2011) Guide to receptors and channels (GRAC), 5th edition. Br J Pharmacol 164(Suppl 1):S1–S324
Melchiorre C, Quaglia W, Picchio MT, Giardinà D, Brasili L, Angeli P (1989) Structure-activity relationships among methoctramine-related polymethylene tetraamines. Chain-length and substituent effects on m-2 muscarinic receptor blocking activity. J Med Chem 32:79–84
Hejnová L, Tucek S, El-Fakahany EE (1995) Positive and negative allosteric interactions on muscarinic receptors. Eur J Pharmacol 291:427–430
Visser TJ, van Waarde A, Jansen TJ, Visser GM, van der Mark TW, Kraan J, Ensing K, Vaalburg W (1997) Stereoselective synthesis and biodistribution of potent [11c]-labeled antagonists for positron emission tomography imaging of muscarinic receptors in the airways. J Med Chem 40:117–124
Dallanoce C, De Amici M, Barocelli E, Bertoni S, Roth BL, Ernsberger P, De Micheli C (2007) Novel oxotremorine-related heterocyclic derivatives: synthesis and in vitro pharmacology at the muscarinic receptor subtypes. Bioorg Med Chem 15:7626–7637
Levey AI (1993) Immunological localization of m1–m5 muscarinic acetylcholine receptors in peripheral tissues and brain. Life Sci 52:441–448
Caulfield MP (1993) Muscarinic receptors—characterization, coupling and function. Pharmacol Ther 58:319–379
Gautam D, Jeon J, Li JH, Han S, Hamdan FF, Cui Y, Lu H, Deng C, Gavrilova O, Wess J (2008) Metabolic roles of the m3 muscarinic acetylcholine receptor studied with m3 receptor mutant mice: a review. J Recept Signal Transduct Res 28:93–108
Poulin B, Butcher A, McWilliams P, Bourgognon J, Pawlak R, Kong KC, Bottrill A, Mistry S, Wess J, Rosethorne EM, Charlton SJ, Tobin AB (2010) The m3-muscarinic receptor regulates learning and memory in a receptor phosphorylation/arrestin-dependent manner. Proc Natl Acad Sci U S A 107:9440–9445
Liang JS, Carsi-Gabrenas J, Krajewski JL, McCafferty JM, Purkerson SL, Santiago MP, Strauss WL, Valentine HH, Potter LT (1996) Anti-muscarinic toxins from dendroaspis angusticeps. Toxicon 34: 1257–1267
Fruchart-Gaillard C, Mourier G, Marquer C, Ménez A, Servent D (2006) Identification of various allosteric interaction sites on m1 muscarinic receptor using 125i-met35-oxidized muscarinic toxin 7. Mol Pharmacol 69: 1641–1651
Gentry PR, Kokubo M, Bridges TM, Cho HP, Smith E, Chase P, Hodder PS, Utley TJ, Rajapakse A, Byers F, Niswender CM, Morrison RD, Daniels JS, Wood MR, Conn PJ, Lindsley CW (2014) Discovery, synthesis and characterization of a highly muscarinic acetylcholine receptor (mAChR)-selective M5-orthosteric antagonist, VU0488130 (ML381): a novel molecular probe. ChemMedChem 9:1677–1682
Acknowledgments
This research was supported by Academy of Sciences of the Czech Republic support RVO: 67985823, and Grant Agency of the Czech Republic grant P304/12/G069.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
El-Fakahany, E.E., Jakubik, J. (2016). Radioligand Binding at Muscarinic Receptors. In: Myslivecek, J., Jakubik, J. (eds) Muscarinic Receptor: From Structure to Animal Models. Neuromethods, vol 107. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-2858-3_3
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2858-3_3
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-2857-6
Online ISBN: 978-1-4939-2858-3
eBook Packages: Springer Protocols