Abstract
Objective
Operative treatment of early onset scoliosis (EOS) with Magnetically Controlled Growing Rod (MCGR) in moderate-to-severe curves poses a challenge due to the limited amount of force and length available with the implant. The purpose of this study was to assess the use of the intra-operative internal spine distraction using Harrington Outrigger, before definitive implantation of MCGR, with regard to initial correction, maintenance of correction, truncal balance, and complication rates.
Patients and methods
16 EOS patients treated with the application of MCGR using the intra-operative internal distractor technique were included in the study. More than 50% of cases were congenital scoliosis with multiple vertebral anomalies. All patients were followed up for a minimum of 2 years. Radiological measurement of change in Cobb angle, thoracic kyphosis, lumbar lordosis, T1–S1 length, T1–T12l length, and sagittal balance were done at pre-op, immediate post-op, after 1 year, and 2 years. All the complications were noted and documented.
Results
The mean age of the operated patients was 8 ± 1.7 years, range (4–10 years). Mean pre-operative Cobb angle was 70.4 degrees. The mean correction of major Cobb angle was 34.6°. The percentage correction achieved in post-operative Cobb angle was about 51%. Mean change in post-operative thoracic kyphosis was 18.5° (40%). The average gain in immediate post-operative spinal length (T1–S1) and thoracic height (T1–T12) was 46.7 mm (18.3%) and 41 mm (23%), respectively.
Conclusion
Large and rigid curves in EOS can achieve a significant correction of Cobb angle and coronal imbalance during the index operation, by the use of intra-operative internal distraction at the time of MCGR insertion.
Level and type of study
Retrospective clinical study, level 4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early Onset Scoliosis (EOS) refers to the presentation of a scoliotic deformity at 10 years of age or younger, irrespective of the underlying aetiology [1]. In some cases, EOS rapidly progresses with growth. The increase in the curve magnitude corresponds with the rate of growth of the child and the number of growth years remaining [2]. Treatment options currently available for EOS include surgical and non-surgical alternatives [3,4,5,6]. Magnetically controlled growing rod (MCGR) has shown promising results in the treatment of this difficult condition [3, 4, 7, 8].
In recent years, many studies have reported good outcomes in EOS after MCGR surgery [8,9,10]. A good mean correction has been reported with MAGEC and other growing rod constructs [8, 9]. The overall correction achieved in Cobb angle and spinal length (T1–S1) is primarily contributed by the initial/index correction obtained at the time of rod implantation [6,7,8]. Subsequent distractions primarily lead to the maintenance of this initial correction achieved [7, 8, 10]. However, MCGR has a limited length available for distractions (48 mm), and the actuator occupies a significant length of the rod that limits the desired contouring of the rod. This warrants the achievement of maximal correction and balance of the deformity during the index surgery of the rod. Various techniques have been discussed in the literature for MCGR while dealing with large and rigid curves to maximize correction achieved during the index surgery [10,11,12]. Among these, pre-operative Halo traction and intra-operative halo traction before implantation of growing rods in large and rigid curves have shown beneficial results during the index surgery [11,12,13]. Harrington’s distractor, which was the workhorse for adolescent deformity correction in the Harrington rod era, has been used in the present study for achieving better index correction of deformities during MCGR implantation in EOS.
Patients and methods
Sixteen patients diagnosed with EOS, managed with MCGR between 2014 and 2019, were included in this study retrospectively. Harrington’s distractor was used intra-operatively during the index surgery for MCGR implantation in all the patients. The study included patients of EOS, older than 5 years and less than 10 years age, managed with MCGR with minimum post-operative follow-up of 2 years. Patients with a history of previous scoliosis surgery were excluded. All the surgeries were performed by the senior author. Intra-operative spinal cord monitoring was used in all the cases.
Pre-operative, post-operative, and 2 year follow-up, whole spine anterior–posterior and lateral radiographs were accessed for measuring Cobb angle, thoracic kyphosis, and lumbar lordosis. T1–T12 and T1–S1 lengths were measured for assessing pre-operative spinal length and changes in the post-operative period. T1–T12 and T1–S1 length were measured between the upper end-plate of T1 and the lower end-plates of T12 and S1, respectively. The mean age of the operated patients was 8 ± 1.7 years (Range 4–10). Among them, 13 were female and 3 were male. The study sample included 9 congenital scoliosis, 4 juvenile idiopathic scoliosis, 2 syndrome scoliosis, and 1 neuromuscular scoliosis. The patients with congenital scoliosis were those with multiple vertebral anomalies not suitable for excision/short fusion (Fig. 1). The average pre-operative Cobb angle of the major curve was 70.4° (Range 42°–95°) with average kyphosis of 40.0° (range 18°–72°), and lumbar lordosis of 33° (range 5°–56°). In our series, we assessed the flexibility of each curve before surgery and found that a majority of the curves were congenital and inherently rigid. The pre-operative flexibility of the curve was assessed by bending films and traction films. The mean Cobb angle of the major curve on traction film was 51.1° (Range 34°–75°). The mean difference of Cobb angle between standing and traction films was 19.3° (range 30°–75°), which amounts to 27.4% correction. The mean pre-operative spinal length (T1–S1) and thoracic height (T1–T12) were 256.6 mm and 179.4 mm, respectively. The mean pre-operative coronal imbalance was 31.5 mm (range 20.3–70.2 mm).
Operative technique
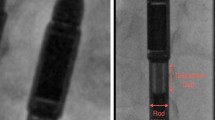
The patients were positioned prone on the operating table under general anaesthesia. Under flouroscopic control promial and distal anchor points were marked, and two separate longitudinal incisions were made at these levels. Proximal and distal anchor points were chosen according to the end vertebra of the curve proximally and distally. Sub-periosteal dissection was done at proximal anchors, and a modified Wiltse approach was used for distal anchors. Pedicle screws were placed using the free hand technique and checked under image intensifier. A minimum of two anchors were secured at cranial and caudal levels. Before implanting the magnetic growing rod, Harrington’s distractor was attached to the proximal and distal anchors on the concave side using gentle persuasion [Fig. 2]. Thereafter gradually, the spine was distracted and lengthened with Harrington's distractor using the Tommy bar under constant spinal cord monitoring. After every 1 cm of the distraction of the spine, distraction was halted for a few minutes, and soft tissues were allowed to accommodate. The neuromonitoring signals were checked at the end of each segmental distraction before starting the next quantum of distraction. The distraction was continued till the endpoint was reached. The endpoint was defined in our technique as the stage when (1) there is sufficient correction of scoliosis to balance the spine; (2) significant resistance is felt while turning the Tommy bar with two fingers or there are signs of excessive stress on bone screw interface; (3) there is a change in the neuromonitoring signals. Although none of our cases reached this 3rd endpoint, we would have reversed the distraction had there been a change in neuromonitoring. We observed and advised extra caution in attaining distraction of the vertebral column in patients with operative history for intra-spinal anomaly, rigid curves, and congenital scoliosis. In our series, nine patients had intra-spinal anomaly. Intra-operative C-arm image of the spine was taken with the distractor in situ to assess the scoliosis correction, status of proximal and distal anchors, and spinal balance.
The distance between proximal and distal anchors was measured, and MCGR was cut accordingly. The proximal and distal parts of the rod were contoured into the required kyphosis and lordosis, leaving the central part, which houses the magnet straight and un-contoured. The contoured MCGR was applied on the main curve's convex side, holding the correction achieved with the distractor in place (Fig. 2). After securing the convex rod, the distractor on the concave side was removed, followed by insertion of MCGR with final tightening of the anchors. Again, at this point, a repeat neuromonitoring signal was obtained to see any sign of cord stretching. The anaesthetist kept a close vigil on the ventilation monitor to look for any sign of increased resistance for ventilation. During distraction, the mean arterial pressure was maintained around 80–90 mm of Hg.
In most of our cases, two proximal and two distal anchors were used (Figs. 1, 4). Pedicle screws, and rarely hooks, were used as an anchor, both proximally and distally. There were no cases of screw loosening or ploughing of the anchor’s during the gradual distraction of spine. The post-operative protocol consisted of wearing a moulded PVC TLSO brace for approximately 6 months to protect the construct.
Post-operative evaluation and follow-up
The patients were followed every 8–12 weeks in the clinic for distractions. Follow-up X-rays of the whole spine were obtained every 6 monthly. The radiological parameters recorded on follow-up X-rays were Cobb angle, thoracic kyphosis, lumbar lordosis, spinal length (T1–S1), and thoracic height (T1–T12). The total number of distractions done and the length of distraction done at each visit was recorded for every patient. Any complication encountered was also recorded. All the patients included in this study were followed for a minimal duration of 2 years.
Statistical analysis
Statistical analysis was conducted using Microsoft Excel 2010 (Microsoft, Redmond, Washington) and Stat Plus (Anal soft, Microsoft). Paired Student’s t tests were used to compare means. All comparisons were two-sided. A p value < 0.05 was deemed significant. Pearson’s correlation was used for determining the statistical correlation.
Results
Cobb angle
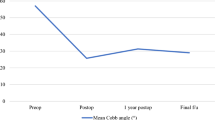
The mean pre-operative Cobb angle was 70.4° (Range 42°–95°), which was corrected in the post-operative period to 35.8° (range 17°–64°) [Table1, 3]. The mean pre-operative thoracic kyphosis 40.0° (range 18°–72°), changed in the post-operative period to 21.4° (range 12°–50°), The mean pre-operative lumbar lordosis of 33° (range 5°–56°) changed post-operatively to 26° (Range 10°–45°). The percentage correction achieved in post-operative Cobb angle was about 51%. This difference was statistically significant (p < 0.001). The mean post-operative change in thoracic kyphosis was 18.5° (40%) and the difference was statistically significant (p < 0.001). Mean post-operative change in lumbar lordosis was 7° (7.5%), and the difference was statistically significant (p = 0.036). Mean Cobb angle at 2-year follow-up was maintained and improved to 30° (Range10°–53°) (Table 4). The correction achieved in Cobb angle at the time of index surgery was maintained in the post-operative period and marginally improved by a mean of 5.9° (8.5%) at 2 year follow-up. This change in Cobb angle was not statistically significant (p > 0.05). The correlation between the post-operative correction in Cobb angle and post-traction Cobb angle was calculated by Pearson’s correlation coefficient (R = 0.526), and a moderate positive correlation was found. This association was found to be statistically significant (p = 0.036).
Spinal length (T1–S1) and thoracic length (T1–T12)
The mean pre-operative spinal length (T1–S1) of 256.6 mm (range 186–351) increased post-operatively to 303.3 mm (range 250–396 mm).The mean increase in spinal length post index surgery was 46.7 mm (18.3%), and the increase in spinal length was found to be statistically significant (p < 0.001) (Tables 1, 3 and 4). At 2 year follow-up after an average of 8 distractions, the mean T1–S1 length was 323.8 mm (range 260–414 mm). The mean increase in spinal height after index surgery at 2 year follow-up was 20.5 mm (7.8%). This increase in spinal length was found to be statistically significant (p < 0.001). There was a significant increase in thoracic length (T1–T12) after index surgery. The mean pre-operative thoracic length changed from 179.4 (range 110–267 mm) pre-operatively to 220 mm (range 175–267 mm) in the post-operative period. This change indirectly translates to an increase in thoracic volume. The mean increase in thoracic length was 40.6 mm (23%). This increase in thoracic length was found to be statistically significant (p < 0.001). The thoracic length at 2 year follow-up increased to 233.1. Mean increase in thoracic length following index surgery after 2 years was 13 mm (7.2%) (Table 4).
Coronal balance
The coronal balance improved significantly post-operatively. The mean coronal imbalance after index surgery was 10 mm (range 0–27.5 mm). The mean improvement in coronal imbalance was 21.5 mm. This improvement in coronal imbalance was found to be statistically significant (p = 0.001).
Complications
A total of eight complications occurred among 5 patients out of the 16 patients in the cohort (Table 4). In two patients, implant-related complications were noted consisting of proximal anchor loosening/pull-out. The first patient was an EOS with neurofibromatosis, required return to OR twice for the proximal anchor pull-out. In the second patient with a partial pull-out, revision was not required till the latest follow-up of 3 years. In two patients, there was a failure of the distraction mechanism of magnet, and both of them required an exchange of the magnetic rod. One patient had an unexplained intra-operative ventilation-related complication, which required letting off the acquired correction and aborting the procedure. This patient had implantation of MCGR after one and half months uneventfully. One patient had decompensation of the lumbar curve. The implant-related complication rate was 25%, requiring an unplanned return to the operating room in 4 patients. Our complication rates were comparable to the complication rates of MCGR in the available literature [14, 15].
Discussion
The importance of correction achieved during the index surgery is well documented in the recent literature [12,13,14, 16]. MCGR application, assisted by an intra-operative internal distraction during the index surgery, allowed gradual and controlled intra-operative correction of the spinal deformity. Intra-operative distractor aids to maximize the correction achieved during the index surgery in the rigid and large curves, particularly in congenital scoliosis. This could possibly help in maintaining a better spinal balance during successive distractions. It could also decrease the need for pre-operative or intra-operative halo traction, in patients with reasonable bone quality, which could be cumbersome and poorly tolerated in some paediatric patients [11,12,13]. The intra-operative Harrington distractor helps to achieve safe, controlled, and effective correction of severe and rigid spinal deformities. This technique was also found to be safe in patients with associated intra-spinal anomaly, which was present in nine patients in our series. The gradual increase in axial traction intra-operatively through the Harrington’s distractor allows gradual correction of the bigger and rigid curves. This allows for a better overall index correction over multiple spinal segments.
Correction of coronal deformity
Various pre-operative and intra-operative traction techniques have been discussed in the literature, aiming to achieve maximum correction during the index surgery before implantation of the magnetic rod [11,12,13,14]. However, there is no mention of an anchor-based internal distractor during the MCGR surgery. The extra-spinal techniques like the halo distractor require pre-operative hospitalization and close monitoring for pre-operative curve loosening, making it cumbersome, time-consuming, and unsuitable for all types of hospital settings [10,11,12]. The intra-operative technique of distraction used by us could overcome the above drawbacks and allows for easier intra-operative real-time deformity correction and implantation of magnetic growth rods. In our series, we used Harrington’s distractor directly attached to the proximal and distal two bone anchors (pedicle screws) on the concave side, intra-operatively with good results. An average correction of 51% of the primary curve was seen after the index surgery, which is comparably better than MCGR index correction data available in the literature, especially with congenital curves [15] [Fig. 3, Tables 3 and 4]. As reported by Kwan et al., in their series, correction with MCGR in congenital scoliosis was 19.9% as compared to 41.7% correction in syndrome and an overall 33% mean correction [15].
However, previously published studies of MCGR by La Rosa, Heydar, and Ridderbusch et al. [9, 17, 18] reported better index correction of 54, 57.7, and 53.2% respectively [Table2]. It is worth noting that most of the curves in these series were idiopathic, syndromic, or neuromuscular, which are inherently more flexible in nature and can be corrected by manual apex manipulation before the definitive rod implantation. This contrasts with our series, where 56% of cases were congenital scoliosis, which are inherently more rigid than the idiopathic and neuromuscular curves [15]. The outlier is the study by La Rosa et al. [9] which has documented the highest rate of index correction of 58% using intra-operative head halter traction. However, this study did not have a single case of congenital scoliosis in its cohort, explaining the high rate of index correction. On the other hand, it underscores the effectiveness of intra-operative traction. The mean correction seen in our series was 34.6°. The possible reason for attaining a better correction than what was predicted by bending films could be explained by the fact that the intra-operative distractor causes direct, gradual stretching of the spinal column and soft tissues over multiple segments in a controlled manner. In one of our most severe cases of early onset idiopathic scoliosis with Cobb angle of 95° and bending Cobb angle of 74°, we were able to bring down the curve to 35°, achieving about 60° (63%) reduction after index surgery using this technique (Fig. 3).
The importance of achieving the maximum correction during the index surgery could also be emphasized by the fact that in most of the published MCGR series, the correction gained in Cobb angle in their last follow-up was low, mean 1.5° [17,18,19]. Similar results were seen in our patients, with a mean improvement of 4.4° at their last follow-up. Cheung et al. [19] in their long-term follow-up of MCGR observed that the greatest Cobb angle correction occurred at the initial implantation surgery, and was stable after that. This technique also helped to reduce the mean coronal imbalance by 21.5 mm, maintaining an acceptable coronal balance during the distraction period.
Correction of sagittal deformity
MCGR has been shown to reduce thoracic hyper-kyphosis [16,17,18,19] [Table 2, Fig. 4]. In our series, the intra-operative distractor helped to reduce the mean thoracic kyphosis by 18.6° (40%), which is comparably better than other published series of MCGR (Fig. 3). In the comparative study by Caubet et al. [11], they demonstrated that traction before implanting MCGR in reducing thoracic kyphosis (Mean 48°) was better than the surgical release group. In the series by La Rosa [9], they were able to achieve a mean reduction of 14.1° with the use of intra-operative Head halter traction. This method is probably a more cumbersome and indirect way of intra-operative distraction with less control by the operating team as it is outside the sterile field, and possibly less effective. In one of our severe cases of kyphoscoliosis, intra-operative internal distraction was able to reduce kyphosis from 72° to 45°, achieving a reduction of 27° (35%) intra-operatively (Figs. 3, 5). Moreover, reducing severe thoracic kyphosis before implanting facilitates MCGR application, which could be difficult otherwise as there is limitation of contouring the magnetic rods [12]. Similar observations were made by Caubet et al. in their multi-centric study using halo gravity traction where they found that the traction offers a benefit to patients with severe kyphosis and facilitates the implantation of expandable devices [11].
a–c Pre-operative, post-operative, and 3 year follow-up radiographs with clinical images showing correction achieved following use of intra-operative distractor for MCGR application, in an 8 year old female patient, EOS (Juvenile idiopathic) with gluten allergy. The curve was rapidly progressive and was not getting controlled with bracing, progressed to 98 degrees
a–j Pre-operative X-rays ap & lateral view of 7 years old, female patient with congenital scoliosis (multiple thoracic hemi-vertebrae and bar) with cobb angle 55°, T1–T12 length 163 mm & T1–S1 length 253 mm. a–f Pre-operative clinical pictures. g–h AP & lateral views X-ray after index surgery, cobb angle 20, T1–T12 length 228 mm & T1–S1 length 290 mm. i–j AP & Lateral X-ray after final distraction (5 year follow-up) with cobb angle 32, T1–T12 length 272 mm & T1–S1 length 318 mm. k–l Clinical pictures at 5 year follow-up
Furthermore, it has been reported extensively in the literature that the complication rates of growing rods in hyper-kyphosis are higher [14]. Possibly, reducing hyper-kyphosis with the help of intra-operative distraction may help to avoid complications following the hyper-kyphosis of spine.
The gain in spinal length (T1–S1) and thoracic length (T1–T12)
There was a significant gain in spinal length and thoracic length of 46.7 mm (18.3%) and 40.6 mm (23%), respectively, in the immediate post-operative period in our series (Tables 1, 3, 4, Fig. 3). The length gained after the index surgery was at least 15 mm more than what was reported in most MCGR literature for both parameters after index surgery [16,17,18,19, 21] (Tables 2, Fig. 3). The length gained in our series could possibly be attributed to the intra-operative distraction, where controlled direct traction is applied to the spinal column and surrounding soft-tissue structures, leading to a more significant correction of coronal deformity and thereby achieving increased length by removing the slack over multiple vertebral segments. No literature is available at present documenting spinal length gained during intra-operative traction in EOS. However, peri-operative and post-operative traction using various methods have significantly increased spine length [11,12,13].
In MCGR surgery, it is essential to attain maximum spinal length (T1–S1) during the index surgery because of the limited amount of force generated by MCGR and interplay of the law of diminishing return during the subsequent distractions from the possible risk of autofusion and fibrosis [19,20,21,22]. This curtails the amount of spine length gained during further distractions [22]. In our series, the spinal length (T1–S1) gained at 2 year follow-up was less than 50% than the length attained after the index surgery. This fact was further attested by Wijdicks SPJ et al. [21] in their systematic review of growth among growth-friendly implants. They concluded that a considerable portion of the reported spinal growth is the result of the initial and final surgical correction and not due to the growth-friendly implant during the lengthening periods in between. This observation has also been supported by the study done by Poon S et al., which concluded that there is a statistically significant decrease in the maximal force generated by MCGR as rods are lengthened. The decrease in force generated may result in diminished spine length, gained with each subsequent MCGR lengthening [22]. Cheung et al., in their 6 year follow-up of MCGR patients, concluded that instrumented segments experience stiffness, limiting further correction and length gain during final surgery, whether fusion or rod removal is performed [18].
Conclusion
The use of intra-operative spine distractor for implantation of MCGR has shown promising results in terms of achieving a good index correction, especially in cases with rigid curves and congenital scoliosis. This technique could extend the use of MCGR in large and neglected curves where otherwise implanting MCGR is a challenge. Rediscovery of this safe and simple technique can serve as a handy tool in the routine application of MCGR. Implant-related complication rate in our series is comparable to the existing MCGR literature.
References
Dickson R (1994) Early-onset idiopathic scoliosis. In: Weinstein S (ed) The paediatric spine: principles and practice. Raven Press, New York, pp 421–429
Scott JC, Morgan TH (1955) The natural history and prognosis of infantile idiopathic scoliosis. J Bone Joint Surge Br 37:400–413
Fletcher ND, Bruce RW (2012) Early-onset scoliosis: current concepts and controversies. Curr Rev Musculoskeletal Med 5:102–110
Cunin V (2015) Early-onset scoliosis: current treatment. Northup Traumatol Surg Res 101(1 suppl):109–118
Bess S, Akbarnia BA, Thompson GH et al (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg 9-A:2533–2543
Akbarnia BA, Pawelek JB, Cheung KM et al (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2-year study. Spine Deform 2(6):493–497. https://doi.org/10.1016/j.jspd.2014.09.050
Subramanian T, Ahmad A, Mardare DM et al (2018) A six-year observational study of 31 children with early-onset scoliosis treated using magnetically controlled growing rods with a minimum follow-up of two years. Bone Joint J 100-B(9):1187–1200. https://doi.org/10.1302/0301-620X.100B9.BJJ-2018-0031.R2
Akbarnia BA, Pawelek JB, Cheung KMC et al (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2-year study. Spine Deform 2:493–497
La Rosa G, Oggiano L, Ruzzini L (2017) Magnetically controlled growing rods for the management of early-onset scoliosis: a preliminary report. J Pediatr Orthop 37:79e85
Lebon J, Batailler C, Wargny M et al (2017) Magnetically controlled growing rod in early onset scoliosis: a 30-case multicenter study. Eur Spine J 26(6):1567–1576. https://doi.org/10.1007/s00586-016-4929-y
Caubet JF, Emans JB (2011) Halo-gravity traction versus surgical release before implantation of expandable spinal devices: a comparison of results and complications in early-onset spinal deformity. JBJ Spinal Disord Tech 24(2):99–104
Welborn MC, Krajbich JI, D’Amato C (2018) Use of magnetic spinal growth rods (MCGR) with and without preoperative halo-gravity traction (HGT) for the treatment of severe early-onset scoliosis (EOS). J Pediatr Orthop. https://doi.org/10.1097/BPO.0000000000001282
Sponseller PD, Takenaga RK, Newton P et al (2008) The use of traction in the treatment of severe spinal deformity. Spine (Phila Pa 1976) 33(21):2305–2309. https://doi.org/10.1097/BRS.0b013e318184ef79
Thakar C, Kieser DC, Mardare M et al (2018) Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early onset scoliosis. Eur Spine J 27(9):2062–2071. https://doi.org/10.1007/s00586-018-5590-4
Kwan KYH, Alanay A, Yazici M et al (2017) Unplanned reoperations in magnetically controlled growing rod surgery for early onset scoliosis with a minimum of two-year follow-up. Spine (Phila Pa 1976) 42(24):E1410–E1414. https://doi.org/10.1097/BRS.0000000000002297
Dannawi Z, Altaf F, Harshavardhana NS et al (2013) Early results of a remotely-operated magnetic growth rod in early-onset scoliosis. Bone Joint J 95-B(1):75–80. https://doi.org/10.1302/0301-620X.95B1.29565
Heydar AM, Şirazi S, Okay E et al (2017) Short segment spinal instrumentation in early-onset scoliosis patients treated with magnetically controlled growing rods: surgical technique and mid-short-term outcomes. Spine (Phila Pa 1976) 42(24):1888–1894. https://doi.org/10.1097/BRS.0000000000002265
Ridderbusch K, Rupprecht M, Kunkel P et al (2017) Preliminary results of magnetically controlled growing rods for early onset scoliosis. J Pediatr Orthop 37(8):e575–e580. https://doi.org/10.1097/BPO.0000000000000752
Cheung JPY, Yiu K, Kwan K et al (2018) Mean 6-year follow-up of magnetically controlled growing rod patients with early onset scoliosis: a glimpse of what happens to graduates. Neurosurgery. https://doi.org/10.1093/neuros/nyy270
Keskinen H, Helenius I, Nandi C et al (2016) Preliminary comparison of primary and conversion surgery with magnetically controlled growing rods in children with early onset scoliosis. Eur Spine J 25(10):3294–3300. https://doi.org/10.1007/s00586-016-4597-y
Wijdicks SPJ, Tromp IN, Yazici M et al (2019) A comparison of growth among growth-friendly systems for scoliosis: a systematic review. Spine J 19(5):789–799. https://doi.org/10.1016/j.spinee.2018.08.017
Poon S, Spencer HT, Fayssoux RS et al (2018) Maximal force generated by magnetically controlled growing rods decreases with rod lengthening. Spine Deform 6(6):787–790. https://doi.org/10.1016/j.jspd.2018.03.009
Funding
The authors did not receive support from any organization for the submitted work. No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by NP, AS, AG, and AG. The first draft of the manuscript was written by NP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
Appropriate ethical approval was taken before the commencement of the study from the Ethical approval committee and Institutional review body (IRB), Reference no—PSSS/ IEC/2019/01.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Srivastava, A., Pandita, N., Gupta, A. et al. Use of intra-operative internal distraction for the application of magnetically controlled growth rods (MCGR): a technique for maximizing correction in the rigid immature spine during index surgery. Spine Deform 11, 225–235 (2023). https://doi.org/10.1007/s43390-022-00579-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00579-5