Abstract
Introduction
Magnetically controlled growing rods (MCGR) for the surgical treatment of early onset scoliosis (EOS) allow non-invasive outpatient based distractions during spinal growth. The purpose of this study is to present the results of a single center case series of 22 patients, evaluate the effect of MCGR treatment on the development of spino-pelvic parameters during growth, and report initial outcomes after end of treatment.
Materials and methods
Prospectively collected data of 22 EOS patients with MCGR treatment has been analyzed. The following radiological parameters were measured before index surgery, after index surgery, 1 year after index surgery, and at last follow-up: Cobb angle of the major curves, thoracic kyphosis (TK), lumbar lordosis (LL), sagittal vertical axis (SVA), pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS). Mean age at index surgery was 9.5 years (range: 4–14 years). Mean length of follow-up was 47.6 months (range: 25–121 months). Etiology of diagnosis was idiopathic in 14 patients, associated with neurofibromatosis in 2 patients, and neuromuscular or syndromic in 6 patients.
Results
Mean Cobb angle of the major curve was 57° preoperatively and 29° at last follow-up (p < 0.0005). Mean TK was 20.1° preoperatively and 20° at last follow-up (p > 0.05). Mean LL was 52.8° preoperatively and 53.2° at last follow-up (p > 0.05). Mean PI was 43.2° preoperatively and 46.3° at last follow-up (p > 0.05). Mean PT was 4.1° preoperatively and 5.8° at last follow-up (p > 0.05). Mean SS was 39.2° preoperatively and 41.7° at last follow-up (p > 0.05). 14 patients finished treatment: nine received final fusion and five received rod removal without fusion. Twelve complications occurred: one deep wound infection, six patients developed proximal junctional kyphosis (PJK), one rod fracture, two rods failed to distract, one deformity progressed after rod removal and required spinal fusion, and one patient developed autofusion of the spine prior to end of treatment.
Conclusion
MCGR treatment is able to control deformity progression. Complication rate was 54.5%. Sagittal balance was not altered and treatment does not seem to have a negative impact on the development of spino-pelvic parameters during growth. Optimal end of treatment for the individual patient still has to be defined.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Scoliosis that is present at less than 10 years of age is defined as early onset scoliosis (EOS). EOS has potential for poor outcomes with increased risk of curve progression, pulmonary underdevelopment and loss of the normal proportionality of trunk growth [1,2,3]. Therefore, adequate and early treatment of these patients is essential for a good long-term outcome. Optimal treatment preserves spinal growth and controls curve progression. Some patients may be treated with bracing or serial casting. However, if these treatment modalities fail to prevent curve progression, surgical intervention is mandatory.
Early fusion of the spine yields poor results with significant growth inhibition, poor respiratory development, and potential development of crankshaft phenomenon [4]. Therefore treatment strategies for EOS aim for growth-sparing techniques that allow spinal growth and pulmonary development while preventing curve progression. Growing rods follow the concept of periodic distraction to preserve spinal growth. Traditional growing rods (TGRs) have previously been the gold-standard for management of EOS because they can prevent curve deterioration while allowing for physiological spinal growth [5, 6]. Magnetically controlled growing rods (MCGR) have been developed to avoid complications associated with repeated surgeries under general anesthesia for open distraction of the TGR [7, 8]. MCGR allow non-invasive outpatient based distractions and their safety and effectiveness have been well evaluated [8,9,10,11,12,13,14,15,16].
Our aim is to provide a comprehensive evaluation of device performance in preventing EOS progression with an emphasis on its effect on spino-pelvic parameters during growth, radiological results, complications, and end of treatment using a standardized distraction technique at a single center with a mean follow-up of 47.6 months (range: 25–121 months) in a series of 22 patients.
Materials and methods
A single-center database with prospectively collected data was reviewed for patients with EOS that have been treated with dual MCGRs (MAGEC, NuVasive, San Diego, USA). Ethics approval and patient consent for collection and analysis of the data was obtained. Inclusion criteria were patients with ability to walk, who had complete radiological follow-up of at least 2 years, and had undergone primary surgery with dual rod MCGR for EOS. Patients that had traditional growing rod instrumentation before index surgery with MCGR, patients with less than 24 months of follow-up, and patients with congenital scoliosis were excluded. Twenty-two patients met the inclusion criteria and were included in the final analysis. During the study period standard radiological evaluation changed from conventional radiography to biplanar stereoradiography (EOS™, EOS Imaging, Paris, France). For standard conventional whole spine radiographs the femoral heads were not regularly captured. Therefore only 11 patients could be included into analysis of spino-pelvic parameters.
The mean age at index surgery was 9.5 years (range: 4–14 years) with a mean follow-up of 47.6 months (range: 25–121 months). All patients were premenarchal, Risser stage 0, and the triradiate cartilage was open. Diagnoses were idiopathic in 14 patients, associated with neurofibromatosis in two patients and neuromuscular or syndromic in six patients. Table 1 provides an overview of the baseline data of all patients.
All patients underwent standard implantation of the MCGR without any intraoperative rod distractions beyond squaring the instrumentation segments. Two pairs of foundation anchors were used at both proximal and distal foundations and were fused during the index surgery. All dual rods were 5.5 mm in diameter and placed in a standard and offset rod configuration. All distractions were performed by three experienced MCGR users. The first distraction was done 2 months postoperatively and followed thereafter on a monthly basis. A targeted 2 mm distraction length was applied to the external remote controller for each distraction episode. Distraction length was monitored by ultrasound at each visit and checked every 6 months by biplanar stereoradiography. When the rod reached full distraction or failed to distract the rod was changed. If the patient approached skeletal maturity treatment was ended either by final fusion or rod removal without spinal fusion.
The following radiological parameters were measured using biplanar whole spine standing radiographs (1) before index surgery, (2) after index surgery, (3) one year after index surgery, and (4) at last follow-up:
-
1.
Cobb angle of the major curve.
-
2.
Thoracic kyphosis (TK) measured from T5 to T12.
-
3.
Lumbar lordosis (LL) measured from L1 to S1.
-
4.
Sagittal vertical axis (SVA).
-
5.
Pelvic incidence (PI).
-
6.
Pelvic tilt (PT).
-
7.
Sacral slope (SS).
Radiographs were routinely acquired with patients standing relaxed and arms forward flexed at the shoulders with the middle fingers touching the middle of the clavicles using conventional radiographs or EOS™ imaging. EOS™ has been shown to be reliable for diagnosis and monitoring of children with early onset scoliosis treated with MCGR [17]. Measurements were performed by an investigator blinded to the patient details.
Due to the sample size (n = 22) non parametric Friedman test was used to perform the statistical analysis with a significance level of α = 0.05.
Results
Coronal deformity correction
The mean Cobb angle of the major curve was 57° (± 11.3) preoperatively and 29° (± 12.8) at last follow-up (p < 0.0005). Table 2 provides an overview of all radiological parameters under study. Figure 1 shows the mean major curve over time during MCGR treatment. The main correction was achieved during index surgery and was maintained without much deviation throughout follow-up.
Spino-pelvic parameters
PI, PT, and SS did not change significantly throughout follow-up as compared to preoperative measurements (Table 2). Mean PI was 43.2° (± 9.3) preoperatively and 46.3° (± 9.4) at last follow-up (p > 0.05). Mean PT was 4.1° (± 4.6) preoperatively and 5.8° (± 7.8) at last follow-up (p > 0.05). Mean SS was 39.2° (± 8.7) preoperatively and 41.7° (± 5.2) at last follow-up (p > 0.05). Comparing subgroups with an LIV above and below L3 and L4 did not show a significant difference either (p > 0.05). Figure 2 shows spino-pelvic parameters over time during MCGR treatment.
Sagittal alignment
TK, LL, and SVA did not change significantly throughout follow-up as compared to preoperative measurements (Table 2). Mean TK was 24.3° (± 20.9) preoperatively and 21.1° (± 18.1) at last follow-up. Mean LL was 50.8° (± 11.8) preoperatively and 55.3° (± 8.9) at last follow-up. SVA was − 8.1° (± 32.5) preoperatively and − 5.7° (± 29.5) at last follow-up. Figure 3 shows TK and LL over time during MCGR treatment.
Complications
Complications necessitating surgery occurred in 12 patients, resulting in a complication rate of 54.5% (Table 1). One patient developed a deep wound infection. Six patients developed proximal junctional kyphosis (PJK). Of those six patients four (66.7%) were of non-idiopathic etiology (two associated with neurofibromatosis and two neuromuscular). One rod fracture occurred and two rods failed to distract. One patient developed deformity progression after rod removal as intended end of treatment and received spinal fusion. One patient developed auto fusion of the spine prior to end of treatment.
End of treatment
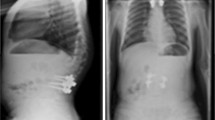
Fourteen patients of this case series finished treatment, so far. Nine received final fusion and five received rod removal without spinal fusion. Within this group the mean Cobb angle was 53.7° (± 7.9) preoperatively and 31° (± 12.9) at final follow-up. The average length of MCGR treatment was 36 months (range: 16–78 months). In those patients who finished treatment the mean T1–T12 height increased 42.5 mm (± 24.3) and the mean T1–S1 height increased 61.1 mm (± 11.6). Due to maximum distraction of the implant one patient received two planned rod exchanges, six patients received one planned rod exchange, and seven patients finished treatment with the first MCGR device. Average time of distraction with one MCGR device was 22.8 months (± 1.1). Figures 4 and 5 show two exemplary cases: one for final fusion (Fig. 4) and one for rod removal without spinal fusion (Fig. 5).
a A 9 year-old girl with a 57° thoracic idiopathic scoliosis. b The same patient after MCGR implantation. c Nine months after implantation the left rod failed to distract and thus the rods were exchanged. d After another 21 months of distraction final fusion was performed resulting in a 46° thoracic curve. The patient is stable at final follow-up
a An 11 year-old girl with a 57° thoracolumbar curve and a 38° thoracic curve. b The same patient after MCGR implantation. c The patient before rod removal, showing the second MCGR in situ. The first MCGR was exchanged after 22 months of distraction (21.45 mm distraction achieved with the right rod and 25.05 mm with the left rod). The second MCGR was in situ for 23 months (22.35 mm distraction achieved with the right rod and 25.09 mm with the left rod) until the left rod broke. d After rod removal the patient has a 22° thoracolumbar and a 23° thoracic curve, and is stable at final follow-up
Discussion
Coronal deformity correction
Coronal deformity correction in our series is similar to correction reported in the literature [6, 18]. There was a significant decrease of the mean Cobb angle of the major curve after index surgery and the curve remained stable during further treatment (Fig. 1) resulting in an improvement from 57° (± 11.3) preoperatively to 29° (± 12.8) at last follow-up (p < 0.0005).
Spino-pelvic parameters
Previous studies investigating TGRs have focused on coronal plane deformity, spinal height, and pulmonary development [5, 6, 8, 19]. However, there is a paucity of literature regarding the development of spino-pelvic parameters under treatment with growing rods, let alone MCGR. Sagittal pelvic morphology influences the standing balance in healthy adults and is relatively constant after end of growth [20, 21]. This is especially relevant to PI which greatly influences the overall sagittal balance and is strongly linked with LL [22]. PI has a direct bearing on the balance of the spine, which rests on the sacral plateau [23]. During childhood and adolescence, PI and other sagittal spino-pelvic parameters as well as thoracic kyphosis (TK) tend to increase before stabilizing at adulthood [24]. SS is stable after achieving a standing posture and is no more influenced by growth and age [25, 26]. It is known that deformity correction via distraction of the spine may decrease the thoracic kyphosis and lumbar lordosis [27]. This may as well influence the normal development of spino-pelvic parameters and therefore may have an effect on overall spinal balance. The sacral plateau forms the base of the spine and is the point of transfer of load from the trunk to the pelvis. Mac-Thiong et al. described a direct linear correlation between PI, LL, SS, and PT [24, 25]. A non-physiological load bearing or spinal balance may therefore influence the development of pelvic anatomy and vice versa. Mac-Thiong et al. described spino-pelvic parameters in healthy children during growth and tried to establish baseline values for measurement of these parameters [24]. Although these values cannot be transferred to EOS patients and corresponding baseline values for EOS patients do not exist, one may postulate that the growing spine of EOS patients is subject to similar changes during growth. Pathological changes of the sagittal balance may not only increase risk of complications of EOS patients under growing rod treatment but also affect long-term quality of life [28, 29].
The available literature on the development of spino-pelvic parameters under treatment with growing rods is heterogeneous. Atici et al. were the first to analyze spino-pelvic parameters in children under treatment with TGR instrumentation [30]. They did not find a statistically significant difference in their study. In a multicenter study with 37 patients Bekmez et al. found TGR treatment to have a negative impact on the development of spino-pelvic parameters [31]. Schlösser et al. calculated baseline data for the development of spino-pelvic parameters during growth using computed tomography scans of the abdomen of 189 children and 310 adults without spino-pelvic pathologies [32]. Using regression analysis they calculated a yearly increase in PI of 0.6° in their population. Bekmez et al. used this data to predict the PI in their study group as if the children would not have been instrumented. The use of this data is debatable since Schlösser et al. did not have repetitive scans of the same individuals. Also individuals without any spino-pelvic pathology were compared to EOS patients. Nevertheless, Bekmez et al. found a decrease of PI during treatment with traditional growing rods in their study population.
In our study cohort periodic distraction with MCGR did not affect the development of spino-pelvic parameters during growth. Figure 2 shows that PI is increasing almost linearly with time, whereas SS decreases after index surgery and increases again afterwards, correspondingly PT increases after index surgery and decreases again afterwards. However, these findings are not statistically significant (p > 0.05). Our data suggests that periodic distraction during MCGR treatment does not seem to have a negative impact on the development of spino-pelvic parameters.
Sagittal alignment
Previous studies have analyzed the effect of TGRs and MCGRs on TK and LL. Shah et al. found a significant decrease of TK and LL after index surgery and an increase until last follow-up [33]. Pepke et al. evaluated 21 children treated with MCGRs and also found a significant decrease of TK after surgery [34]. Due to the follow-up of only 1 year it is not clear if TK increases again during further follow-up. We also found a decrease of TK and LL after index surgery and an increase during further follow-up but this was not significant (p > 0.05). The reason why we did not find a significant change in TK might be due to the fact that we tried to bend the rod as much as possible according to the individual sagittal anatomy of the patient to reduce stress, especially at the cranial anchor points. SVA did not change significantly during MCGR treatment and there is a great variety within the individual patient at the different measuring points, which is reflected by the large standard deviation (Table 2). This may be due to the compliance of the children during the examination, especially with EOS™ imaging.
Complications
In a systematic review of complications in MCGR treatment Kwan et al. found a complication rate of 46.7% [35]. In our cohort the complication rate was 54.5%, whereas two complications might not be directly related to the device: one patient developed autofusion of the spine prior to end of treatment and one patient developed deformity progression after rod removal as intended end of treatment. If these complications are excluded, the complication rate of 45.6% would be consistent with the literature. Rod fracture or failure to distract the MCGR can have different reasons. An inappropriate bending of the rod near the expanded portion of the rod and incorrect rod insertion and/or configuration may lead to inability to distract along the long axis of the rod. Risk factors include increased body habitus such as older age and increased body mass index, as well as reduced distance between the two internal magnets [36]. Another reason might be the “law of diminishing returns” which is a phenomenon already known from TGRs and previous MCGR studies. Decreasing gains in spinal lengthening are observed with following lengthening of the rod [37]. Although there was a high variability for each patient, there was a clear trend towards less effective lengthening with every distraction in our cohort as well.
Six patients developed proximal junctional kyphosis (PJK) and implant loosening at the proximal foundations. The majority of them were of non-idiopathic etiology (66.7%) which is also consistent with the literature [38]. Five of the six PJK patients developed a hyperlordosis at the levels caudal to the instrumentation. Within this subgroup of patients the increase in LL was significant (p < 0.05). Figure 6 shows the lumbar lordosis (preop, postop and 1 year postop) of a patient that later developed PJK with failure. Initially the patient’s hyperlordosis in L4/5 and L5/S1 was able to compensate. But with time compensatory mechanisms failed and the patient developed proximal junctional failure that necessitated revision surgery. One might carefully observe patients with an early hyperlordosis caudal to the lower instrumented vertebra, especially in case of a non-idiopathic etiology of the deformity. These patients may develop PJK. Due to the small number of patients this conclusion should be considered with caution. Although all PJK patients showed an increase of SVA during treatment, there were also some non-PJK patients, which showed an increase in SVA. Eight patients showed an increase or decrease of more than 20 mm after index surgery. This might be related to the new spinal alignment or just due to pain, however due to the sample size and the high standard deviation it is difficult to tell.
End of treatment
The best way to end MCGR treatment remains unclear. Some surgeons may see MCGR as an internal brace which at the end of skeletal maturity and an acceptable curve may be removed without fusion. Others may regard it as relevant mostly to preserve spinal growth and see final fusion as obligatory. There are no strict criteria to end MCGR treatment in either way. In our series, six patients received rod removal without spinal fusion as intended end of treatment. One of them developed deformity progression after rod removal which necessitated instrumented fusion. Jain et al. came to a similar conclusion when they studied 30 TGR patients after rod removal without final fusion [39]. In carefully selected patients with a balanced spine and an acceptable curve reaching skeletal maturity, rod removal without fusion is an option. However, the individual patient best suitable for rod removal should be evaluated in larger, preferably, randomized trials.
Limitations
The main limitation of this study is the small sample size. However, given the standardized surgical technique, long follow-up and relative homogeneity (63.6% idiopathic etiology, only primary MCGR implantation) of the cohort, our study provides a useful insight into the outcome and complication profile after MCGR treatment in patients with EOS.
Conclusion
MCGR treatment effectively controls deformity progression while preserving spinal growth. The development of spino-pelvic parameters does not seem to be affected by MCGR treatment. The complication rate remains relatively high. Ideal strategies to prevent PJK need to be explored, while non-idiopathic deformities are at higher risk to develop PJK. Compensatory changes caudal to the instrumentation may indicate later development of PJK. In carefully selected patients reaching skeletal maturity, rod removal after MCGR treatment is an option to avoid spinal fusion.
References
Campbell RM, Smith MD, Mayes TC et al (2003) The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Jt Surg Am 85-A:399–408
Pehrsson K, Larsson S, Oden A, Nachemson A (1992) Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine 17:1091–1096
Karol LA (2019) The natural history of early-onset scoliosis. J Pediatr Orthop 39:S38–S43. https://doi.org/10.1097/BPO.0000000000001351
Vitale MG, Matsumoto H, Bye MR et al (2008) A retrospective cohort study of pulmonary function, radiographic measures, and quality of life in children with congenital scoliosis: an evaluation of patient outcomes after early spinal fusion. Spine 33:1242–1249
Akbarnia BA, Breakwell LM, Marks DS et al (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine 33:984–990
Akbarnia BA, Marks DS, Boachie-Adjei O et al (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine 30:S46–57
Sankar WN, Acevedo DC, Skaggs DL (2010) Comparison of complications among growing spinal implants. Spine 35:2091–2096
Cheung KMC, Cheung JPY, Samartzis D et al (2012) Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 379:1967–1974
Heydar AM, Şirazi S, Bezer M (2016) Magnetic controlled growing rods as a treatment of early onset scoliosis. Spine 41:E1336–E1342
Hosseini P, Pawelek J, Mundis GM et al (2016) Magnetically controlled growing rods for early-onset scoliosis. Spine 41:1456–1462
La Rosa G, Oggiano L, Ruzzini L (2017) Magnetically controlled growing rods for the management of early-onset scoliosis. J Pediatr Orthop 37:79–85
Cheung JP-Y, Samartzis D, Cheung KM-C (2014) A novel approach to gradual correction of severe spinal deformity in a pediatric patient using the magnetically-controlled growing rod. Spine J 14:e7–13
Cheung JPY, Bow C, Samartzis D et al (2016) Frequent small distractions with a magnetically controlled growing rod for early-onset scoliosis and avoidance of the law of diminishing returns. J Orthop Surg 24:332–337
Cheung JPY, Cahill P, Yaszay B et al (2015) Special article: update on the magnetically controlled growing rod: tips and pitfalls. J Orthop Surg 23:383–390
Cheung JPY, Yiu K, Kwan K, Cheung KMC (2019) Mean 6-year follow-up of magnetically controlled growing rod patients with early onset scoliosis: a glimpse of what happens to graduates. Neurosurgery 84:1112–1123. https://doi.org/10.1093/neuros/nyy270
Cheung JPY, Yiu KKL, Samartzis D et al (2018) Rod lengthening with the magnetically controlled growing rod: factors influencing rod slippage and reduced gains during distractions. Spine 43:E399–E405. https://doi.org/10.1097/BRS.0000000000002358
Obid P, Yiu KKL, Cheung KM et al (2018) Reliability of rod lengthening, thoracic, and spino-pelvic measurements on biplanar stereoradiography in patients treated with magnetically controlled growing rods. Spine 43:1579–1585. https://doi.org/10.1097/BRS.0000000000002671
Nnadi C, Thakar C, Wilson-MacDonald J et al (2018) An NIHR-approved two-year observational study on magnetically controlled growth rods in the treatment of early onset scoliosis. Bone Jt J 100:507–515. https://doi.org/10.1302/0301-620X.100B4.BJJ-2017-0813.R1
Lebon J, Batailler C, Wargny M et al (2017) Magnetically controlled growing rod in early onset scoliosis: a 30-case multicenter study. Eur Spine J 26:1567–1576. https://doi.org/10.1007/s00586-016-4929-y
Jackson RP, Hales C (2000) Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers. Spine 25:2808–2815
Marty C, Boisaubert B, Descamps H et al (2002) The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J 11:119–125. https://doi.org/10.1007/s00586-001-0349-7
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg Am 87:260–267. https://doi.org/10.2106/JBJS.D.02043
Mac-Thiong J-M, Berthonnaud E, Dimar JR et al (2004) Sagittal alignment of the spine and pelvis during growth. Spine 29:1642–1647
Mac-Thiong J-M, Labelle H, Berthonnaud E et al (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16:227–234. https://doi.org/10.1007/s00586-005-0013-8
Cil A, Yazici M, Uzumcugil A et al (2005) The evolution of sagittal segmental alignment of the spine during childhood. Spine 30:93–100
Swank SM, Mauri TM, Brown JC (1990) The lumbar lordosis below Harrington instrumentation for scoliosis. Spine 15:181–186
Thakar C, Kieser DC, Mardare M et al (2018) Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early onset scoliosis. Eur Spine J 27:2062–2071. https://doi.org/10.1007/s00586-018-5590-4
Makino T, Kaito T, Sakai Y et al (2019) Health-related quality of life and postural changes of spinal alignment in female adolescents associated with back pain in adolescent idiopathic scoliosis: a prospective cross-sectional study. Spine. https://doi.org/10.1097/BRS.0000000000002996
Atici Y, Akman YE, Erdogan S et al (2015) The effect of growing rod lengthening technique on the sagittal spinal and the spinopelvic parameters. Eur Spine J 24:1148–1157
Bekmez S, Demirkiran HG, Dede O et al (2019) Spinal instrumentation in growing children retards the natural development of pelvic incidence. J Pediatr Orthop 39:141–145. https://doi.org/10.1097/BPO.0000000000000882
Schlösser TPC, Janssen MMA, Vrtovec T et al (2014) Evolution of the ischio-iliac lordosis during natural growth and its relation with the pelvic incidence. Eur Spine J 23:1433–1441. https://doi.org/10.1007/s00586-014-3358-z
Shah SA, Karatas AF, Dhawale AA et al (2014) The effect of serial growing rod lengthening on the sagittal profile and pelvic parameters in early-onset scoliosis. Spine 39:E1311–E1317
Pepke W, Almansour H, Diebo BG, Akbar M (2019) Correction of the spine with magnetically controlled growing rods in early onset scoliosis: a pre-to-post analysis of 21 patients with 1-year follow-up. Orthopade. https://doi.org/10.1007/s00132-019-03801-x
Kwan KYH, Alanay A, Yazici M et al (2017) Unplanned reoperations in magnetically controlled growing rod surgery for early onset scoliosis with a minimum of two-year follow-up. Spine 42:E1410–E1414. https://doi.org/10.1097/BRS.0000000000002297
Cheung JPY, Yiu KKL, Samartzis D et al (2018) Rod lengthening with the magnetically controlled growing rod. Spine 43:E399–E405. https://doi.org/10.1097/BRS.0000000000002358
Sankar WN, Skaggs DL, Yazici M et al (2011) Lengthening of dual growing rods and the law of diminishing returns. Spine 36:806–809. https://doi.org/10.1097/BRS.0b013e318214d78f
Subramanian T, Ahmad A, Mardare DM et al (2018) A six-year observational study of 31 children with early-onset scoliosis treated using magnetically controlled growing rods with a minimum follow-up of two years. Bone Jt J 100B:1187–1200. https://doi.org/10.1302/0301-620X.100B9.BJJ-2018-0031.R2
Jain A, Sponseller PD, Flynn JM et al (2016) Avoidance of “final” surgical fusion after growing-rod treatment for early-onset scoliosis. J Bone Jt Surg Am 98:1073–1078. https://doi.org/10.2106/JBJS.15.01241
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethics approval for this study was obtained from the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Obid, P., Yiu, K., Cheung, K. et al. Magnetically controlled growing rods in early onset scoliosis: radiological results, outcome, and complications in a series of 22 patients. Arch Orthop Trauma Surg 141, 1163–1174 (2021). https://doi.org/10.1007/s00402-020-03518-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03518-z