Abstract
Objective
Iron deficiency in older people is common and affects physical and cognitive performance. The effects of iron deficiency on nutrition and cognitive status are well established. However, there are few studies demonstrating the impact of iron deficiency treatment on functional and cognitive outcomes in the geriatric population. The aim of this study was to determine whether iron replacement treatment was associated with an improvement in the nutritional, cognitive, and functional status of older patients with iron deficiency (ID) and iron deficiency anemia (IDA).
Methods
Geriatric patients with iron deficiency and iron deficiency anemia presenting to the geriatric clinic were included in the study. Comprehensive geriatric assessment (CGA) and blood samples to investigate iron deficiency were performed at baseline and 6 month later. 81 patients were included in the study and were evaluated at follow-up in the 6th month. The CGA included the following tests: the Katz Index of Independence in Activities of Daily Living Scale (Katz ADL), the Lawton–Brody Instrumental Activities of Daily Living Scale (IADL), the Mini-Mental State Examination (MMSE), and the Mini Nutritional Assessment Short-Form (MNA-SF), as well as the assessments of hand grip strength and walking speed.
Results
Of the 81 participating patients, 69.1% were women and 30.9% were men. The mean age was 76.8 ± 7.28 years. Follow-up after iron supplementation treatment was performed with a mean of 6.23 ± 1.58 months. Improvements occurred in the following geriatric and laboratory assessments: Lawton–Brody (IADL), MNA-SF, MMSE, hand grip strength, and walking speed evaluations and the levels of hemoglobin, iron, total iron-binding capacity, transferrin saturation, and ferritin.
Conclusions
It was shown that iron replacement treatment has a positive impact on functional and cognitive status and nutritional parameters in older patients with ID and IDA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Given the growing geriatric population in the world [1], it is of importance to assess the functionalities of older individuals by comprehensive geriatric assessment (CGA) and, in order for them to maintain their functionalities, it is of importance to detect fragile and pre-fragile patients earlier, providing possible treatment interventions [2,3,4]. For the older population, functionality is defined as the capacity of their cognitive and physical performance being sufficient to fulfill the activities of daily living independently [5]. One of the major goals of geriatrics is to detect the factors leading to negative outcomes in comprehensive geriatric tests and to provide possible treatment options. Anemia has been well recognized as one of the factors affecting CGA. The most common cause of anemia in the older population is iron deficiency (ID) [6]. ID leads to limitations in functioning even in the absence of anemia. There is an abundance of studies in the literature reporting the negative effects of iron deficiency anemia on mental and physical functions. Its negative effects have been observed in several areas, including mental well-being, muscle strength, and nutritional status, which are assessed by the CGA [7,8,9,10,11].
Iron deficiency anemia (IDA) in older persons is a common hematological problem. A society-based study in Turkey detected the prevalences of ID and IDA as 7.1 and 2.8%, respectively [12]. The prevalence of ID is higher in inpatients who are hospitalized for any reason [13]. The detection and treatment of [14] IDA, which leads to physical and cognitive limitations even in the general population, is of importance, especially in the geriatric population. The negative effects of ID on CGA, especially on cognition, are well recognized [7]. However, there are no observational studies evaluating treatment outcomes in the general population [15, 16], apart from a few studies conducted with patients having malignancies. The objective of our study was to determine whether iron supplementation has a positive impact on cognitive, functional, and nutritional status in older patients with ID or IDA.
Materials and methods
Patient selection
81 patients aged 65 and older who were admitted to the Outpatient and Inpatient Clinic of the Department of Geriatric Medicine at Ankara University Ibn-i Sina Hospital were included in the study since January 2016. Patients with severe dementia with an MMSE score < 10 were excluded. CGA and laboratory investigations were performed at baseline and 6 months later.
The characteristics of the patients including their age and gender, the presence of any comorbidities, medications, including both antiplatelet and anticoagulant medications, and patient consents for further evaluations were documented.
The underlying etiology identified in those patients consenting for further investigations was classified into five groups. No etiological findings were specified in Group 1 patients. In Group 2 patients, bleeding areas were identified in endoscopic and/or colonoscopic examinations. Group 3 patients were diagnosed with malnutrition according to the results of endoscopic and laboratory evaluations. Group 4 patients had nutritional deficiencies and they were observed to have a cachectic appearance during clinical evaluation. The Mini Nutritional Assessment Short-Form (MNA-SF) score of these patients was poor. However, no underlying causes were identified in the endoscopic examination of these patients. In this group, iron deficiency is thought to be due to insufficient intake of iron. And, finally, Group 5 consisted of patients who had already received erythropoietin (EPO) therapy.
Patients who underwent endoscopic and/or colonoscopic examinations were classified into nine groups based on the etiology. These were: (1) stomach ulcers, (2) stomach polyps, (3) gastrointestinal malignancies, (4) colon polyps, (5) diverticula of the colon, (6) esophageal varices, (7) celiac disease, (8) inflammatory bowel disease, and (9) other causes of malabsorption.
In addition, the following data of the participating patients were documented, including the history of previous iron replacement treatments, the mode of administration and the active ingredients of the treatment (oral, intravenous), the total iron amount replaced in milligrams, and whether these amounts were sufficient for replacement as regards to the targeted hemoglobin levels. The total dose required to fill the iron stores was recorded as sufficient. The patient’s nonadherence to oral treatment or the presence of any missing doses was recorded as insufficient.
Comprehensive geriatric assessment (CGA)
The CGA included the following tests: The Katz Index of the Activities of Daily Living (Katz ADL), The Lawton–Brody Instrumental Activities of Daily Living Scale (IADL), The Mini-Mental State Examination (MMSE), and The Mini Nutritional Assessment Short-Form (MNA-SF). The activities of daily living were assessed by Katz ADL. This index assesses daily functions including dressing, bathing, toileting, getting out of bed, feeding, and continence on a 6 point scale [17]. Instrumental activities of daily living were assessed by the Lawton Brody IADL. This scale assesses daily activities including the ability to use the phone, shopping, food preparation, housekeeping, laundry, mode of transportation in the same city, and responsibility for own medications on a 17 point scale [18]. Cognitive functions were examined with the MMSE. Lower scores obtained as the outcome of this 30-point questionnaire indicate cognitive dysfunction [19]. Nutritional status was evaluated with the MNA-SF. This is a 14-point questionnaire with proven validity and reliability in Turkish. Scores between 0 and 7 indicate malnutrition, scores between 8 and 11 indicate a risk for malnutrition, and scores between 12 and 14 indicate normal nutrition [20]. To assess muscle strength, hand grip strength was measured with an electronic hand dynamometer (GRIP-D, grip strength dynamometer, produced by Takei, Made in Japan). Measurements were performed when the arm was flexed at a 90° angle at the elbow. The participating patient applied a maximum gripping force to the handle of the dynamometer, gripping it with the nondominant hand. Three measurements were performed at 1-min intervals. The mean of these three measurements was calculated. Results were obtained in kilograms. Grip strengths of < 20 kg and < 30 kg for women and for men, respectively, were accepted to be in favor of decreased muscle strength. Muscle performance was evaluated measuring usual gait speed of participants over a 4-m course. Gait speed was expressed in m/s. Values less than 0.8 m/s indicated decreased gait speed. The patients were compared in two groups as patients with walking speed values < 0.8 m/s (insufficient) and patients with walking speed values ≥ 0.8 m/s (sufficient).
Laboratory assessments
Hemoglobin (Hb) (g/dL), iron (μg/dL), total iron-binding capacity (TIBC) (μg/dL), transferrin saturation (%), and ferritin (ng/mL) were evaluated.
Definitions of iron deficiency and iron deficiency anemia
The diagnosis of iron deficiency, without the presence of iron deficiency anemia, was made if serum Hb values were within normal limits (12.6–17.4 g/dL) and ferritin was below 40 ng/mL. Patients were accepted to have iron deficiency anemia if they had the following laboratory values: Hb levels < 13 g/dL in men and < 12 g/dL in women [21], iron: < 60 μg/dL, TIBC: > 450 μg/dL, transferrin saturation: < 15 (%), and ferritin: < 20 ng/mL [22, 23].
Statistical analysis
Descriptive statistics of continuous data are presented as mean, standard deviation, median, and minimum and maximum values, whereas discrete data are presented in percentages.
Study data were evaluated with the Kolmogorov–Smirnov test if they were normally distributed. Intergroup comparisons were evaluated by Wilcoxon test and by combined two-way ANOVA. Categorical variables were compared with the McNemar test between the groups.
The SPSS 15.0 (SPSS Inc., Chicago, IL, USA) program was used for the statistical evaluations and the limit for statistical significance was accepted to be p < 0.05.
Results
Of all the 81 participating patients, 69.1% (n: 56) were women and 30.9% (n: 25) were men. The mean age was 76.8 ± 7.2818. The percentages of the comorbidities present in the participating patients were as follows: diabetes mellitus 48.1% (n: 39), hypertension 90.1% (n: 73), hyperlipidemia 70.4% (n: 57), chronic obstructive pulmonary disease 29.6% (n: 24), disorders of the thyroid 17.3% (n: 14), chronic kidney disease 14.8% (n: 12), cerebrovascular events or neurological disease 21.3% (n: 17), atrial fibrillation 13.6% (n: 11), chronic liver disease 3.7% (n: 3), atherosclerotic heart disease or heart failure 49.4% (n: 40), autoimmune disease 4.9% (n: 4), malignancies 9.9% (n: 8), Parkinson’s disease 11.1% (n: 9), depression 30.9% (n: 25), falls 21% (n: 17), osteoporosis 44.4% (n: 36), and urinary incontinence 55.6% (n: 45). The median number of drugs received per patient was 6. The rate of polypharmacy (≥ 5 drugs) was 66.7% (n: 54). The percentages of patients taking either antiplatelet or anticoagulant medications and the percentages of patients taking a combination of both were as follows: antiplatelet medicine use 59.3% (n: 48), anticoagulant use 21% (n: 17), and combined treatments 19.8% (n: 16).
The percentage of patients with a history of previous iron replacement treatment was 39.5% (n: 32). 13 of 81 patients were observed to have values low enough to require erythrocyte suspension transfusions at baseline. 63% of the patients who consented for further examination underwent endoscopy and colonoscopy. The etiologies of iron deficiency anemia diagnosed in the participating patients are summarized in Table 1.
The outcomes of the endoscopic and colonoscopic examinations are summarized in Table 2. The other etiologies for malabsorption were recorded as Helicobacter pylori infection, pangastritis, atrophic gastritis, and history of bariatric surgery or gastrointestinal system (GIS) surgery.
The total iron dosages received by the patients were calculated and compared with the targeted hemoglobin levels. It was then evaluated whether the iron replacement treatment was sufficient. 85.2% (n: 69) of patients were observed to receive sufficient doses of iron replacement treatment. Follow-up evaluations were performed with a mean of 6.23 ± 1.58 months.
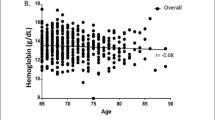
The patients before and after values of iron replacement treatment were compared with the Wilcoxon signed-rank test, resulting in significant differences in all parameters except the Katz index results. The results are summarized in Table 3. When the means of elevations of Hb values were evaluated by gender, the mean Hb values, which were detected to be 10.8527 ± 4.7447 g/dL before treatment in female patients, were observed to be increased to 11.8618 ± 1.5523 g/dL. In males, the mean of Hb values was 10.924 ± 1.5722 g/dL before treatment, and this value increased to 12.656 ± 1.9767 g/dL after treatment. The mean values for both genders are presented in Table 3.
Differences in walking speed results were evaluated with the McNemar test. When the two walking speed groups (< 0.8 m/s, insufficient, and ≥ 0.8 m/s, sufficient) were compared in terms of the values obtained before and after iron replacement treatment, a significant improvement was detected (p value: 0.000). Twenty-seven patients (35.1%) who had an insufficient walking speed before iron treatment were found to have improved measured levels of walking speed after iron replacement treatment. The results are summarized in Table 4.
In addition to iron replacement, vitamin D, vitamin B12, and folic acid replacements were also performed if the measured levels were low (low levels were determined as follows: for vitamin D < 20 μg/L, for vitamin B12: < 200 pg/mL, and for folic acid: < 5.90 ng/mL). The outcomes of geriatric assessments were evaluated before and after replacement treatment for these vitamins and the results were compared. As shown in Table 3, among these three vitamins, only the vitamin D values after 6 months were statistically different compared to baseline.
In both patient groups, those taking Vitamin D supplementation and those taking no Vitamin D supplementation, the Lawton–Brody IADL, MMSE, and the values of hand grip strength improved, with statistical significance. Taking vitamin D replacement did not cause any differences between the groups as the same levels of improvements were observed in both groups except for the MNA-SF. The impact of vitamin D on the geriatric assessments is summarized in Table 5.
When the effect of vitamin D replacement on the walking speed was examined (evaluated by the McNemar test); it was observed that 19 (32.8%) patients with insufficient values of walking speed at baseline achieved sufficient values of walking speed in the 6th month (p value 0.000). The results are summarized in Table 6.
In the group taking no vitamin D replacement, 8 (42.1%) patients with decreased walking speed at baseline improved their walking speed at follow-up (p value 0.000). The results are summarized in Table 7. Improvement in walking speed was similar in both groups.
39.5% of the patients participating in the study received oral treatment and 60.5% received intravenous treatment for iron replacement. The iron values detected after the treatment demonstrated an increase with a statistical significance in both the oral and intravenous treatment modality groups. No significant differences were detected when oral or intravenous treatment was compared (p 0.073).
Discussion
In this study, we evaluated the impact of iron replacement treatment in older patients with ID and IDA. Our results indicate that iron supplementation had a significant positive effect on instrumental daily activities of living, nutritional status, cognitive functions, muscle strength, and performance. In addition, the levels of hemoglobin, iron, TIBC, transferrin saturation, and ferritin improved in older patients taking iron replacement treatment.
There are many factors affecting the CGA. However, the detection of treatable factors, especially those affecting this assessment, is of importance. The underlying diseases causing IDA, as well as the anemia itself, may provide the grounds for the lower CGA scores and for functional dependencies in the older person, particularly in hospitalized patients [11]. Many studies conducted previously reported the negative impact of anemia, especially on cognitive status. Some of these studies included hospitalized patients [13, 17], some included nursing home patients [14], and some other studies screened the community [24]. In our study, patients treated at both outpatient and inpatient facilities were included to provide a heterogeneous group. The patients with dementia or having low scores on MMSE were excluded. However, immobilized patients were included in the group with insufficient values of walking speed < 0.8 m/s. These patients were detected to have no improvements in their walking speed values despite the iron replacement treatment; however, their data were included in the calculations.
Studies evaluating the impact of IDA on cognition, especially in children, are numerous [25]. There is a need for information in the older population as well for maintaining the stability of their cognitive functions [26]. A study by Zilinski et al. reported a 60% incidence of anemia in hospitalized patients (subtypes of anemia were not specified). CGA of these patients revealed significant associations of anemia with mobility limitations, cognitive impairment, and dysphagia [7].
There are studies reporting IDA as the cause of physical dependencies in daily functions and of dismobility [27]. Considering especially cardiac comorbidities in older people, it may be concluded that IDA leads to an increase in the extent of this kind of dependency. Our study, aiming to evaluate whether ID or IDA treatment would reverse this kind of physical dependency, showed improvements in hand grip and walking speed tests despite the presence of other factors causing dependencies in this group of patients.
Recent studies evaluating the effects of anemia on muscle function reported that anemia caused losses in muscle mass [28]. Our study revealed that iron replacement treatment led to improvements in the outcomes of hand grip strength and walking speed tests evaluating muscle strength and physical performance.
As far as we know, there are no studies in the older population comparing the outcomes of CGA tests before and after iron replacement treatment. There are several studies evaluating improvements in patients receiving treatment for malignancies. A study by Massa et al. evaluated the effects of elevation of hemoglobin levels, associated with recombinant EPO treatment in cancer patients receiving chemotherapy, on the outcomes of CGA and cognitive functions [15].
Prior studies report the negative effects of IDA on geriatric assessment tests. The achievement of improvements in geriatric test outcomes associated with normalized ferritin levels appears to confirm the negative effects of anemia in comprehensive geriatric tests. In the present study, our patients were screened for the levels of vitamin D, folic acid and B12 routinely and patients with deficiencies in these vitamins were treated. To exclude the effects of these vitamins on geriatric tests, the levels of these vitamins at baseline and after the replacement treatment were compared. Only a significant increase in the level of vitamin D was found. However, increased vitamin D levels were not associated with improving the outcomes of the CGA except for the Katz ADL and MNA-SF. This result showed that Vitamin D supplementation could be related to good basic daily activities and nutritional status. However, there were no differences in the Katz ADL scores observed with iron treatment. The present study indicates that not only iron supplementation but also Vitamin D supplementation could have a favorable effect on nutritional status. Further studies are needed to better understand the impact of these supplementations.
There are several studies showing the effect of vitamin D on cognitive function [29, 30]. In our study, vitamin D replacement was given not alone but in combination with the treatment of IDA. Significant improvements in MMSE scores were also observed in patients who were not taking a vitamin D replacement. Therefore, the achieved improvements observed in the test outcomes were associated with the treatment of ID-IDA.
There are a number of studies examining vitamin D levels and whether they are associated with muscle strength and physical performance [31,32,33,34,35]. In our study, the improvement was attributed to only the iron deficiency treatment, since the results of hand grip and walking speed tests improved in the patient group who did not take replacements for vitamin D. In a study by Formiga et al. [36], Vitamin D deficiency was associated with a low MNA-SF score, similar to our study. This study also found that low levels of vitamin D were associated with low functionality in women. Another study evaluated the effect of vitamin D replacement on short physical performance tests and walking speed in older male adults who lived sedentary lives [37]. Similar to the results of our study, Vitamin D replacement did not show a positive effect on the CGA test results. Apparently, further studies evaluating the association between CGA and vitamin D replacement should be conducted. The studies should provide homogeneity in patient groups in terms of additional diseases, current physical condition, gender, and age range.
When we evaluated the causes of IDA in the participating geriatric patients, we identified bleeding as the most common causal factor. Several studies revealed that bleeding is the most common cause of IDA [38, 39]. Patients who are diagnosed with IDA should be further investigated to screen for the possibility of occult bleeding [40, 41]. In our study, gastrointestinal system (GIS) screening was performed by endoscopy and/or colonoscopy in the study patients who accepted further examinations. GIS malignancies were detected at a rate of 8.5%. Other reasons for malabsorption were encountered as the most common reason.
In conclusion, iron replacement treatment could be related to well nutritional and cognitive status and physical performance in older adults with ID-IDA. It is required that the underlying causes should definitely be investigated and treated if possible. However, regardless of the underlying reason, iron replacement should definitely be provided with appropriate doses and for appropriate periods. The patients should be followed-up on a regular basis to evaluate their responses and adherence to treatment.
References
Centers for Disease Control and Prevention and The Merck Company Foundation. The State of Aging and Health in America 2007. http://www.cdc.gov/aging/pdf/saha_2007.pdf. Accessed 14 May 2017
Namioka N, Sakurai H, Terayama H, Iwamoto T, Fujihira T, Tsugehara H, Tsuchida A, Hanyu H (2017) Geriatric problems correlated with cognitive decline using a screening test named “Dr. SUPERMAN” for comprehensive geriatric assessment in elderly inpatients. Geriatr Gerontol Int. 17(9):1252–1256
Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ (1993) Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet 342(8878):1032–1036
Devons CA (2002) Comprehensive geriatric assessment: making the most of the aging years. Curr Opin Clin Nutr Metab Care 5(1):19–24
Lopes MJ, Escoval A, Pereira DG, Pereira CS, Carvalho C, Fonseca C (2013) Evaluation of elderly persons’ functionality and care needs. Rev Lat Am Enfermagem 21(Spec No):52–60
Andres E, Serraj K, Federici L, Vogel T, Kaltenbach G (2013) Anemia in elderly patients: new insight into an old disorder. Geriatr Gerontol Int 13(3):519–527
Zilinski J, Zillmann R, Becker I, Benzing T, Schulz RJ, Roehrig G (2014) Prevalence of anemia among elderly inpatients and its association with multidimensional loss of function. Ann Hematol 93(10):1645–1654
Lucca U, Tettamanti M, Mosconi P, Apolone G, Gandini F, Nobili A, Tallone MV, Detoma P, Giacomin A, Clerico M et al (2008) Association of mild anemia with cognitive, functional, mood and quality of life outcomes in the elderly: the “Health and Anemia” study. PLoS One 3(4):e1920
Onem Y, Terekeci H, Kucukardali Y, Sahan B, Solmazgul E, Senol MG, Nalbant S, Sayan O, Top C, Oktenli C (2010) Albumin, hemoglobin, body mass index, cognitive and functional performance in elderly persons living in nursing homes. Arch Gerontol Geriatr 50(1):56–59
Rohrig G, Becker I, Polidori MC, Schulz RJ, Noreik M (2015) Association of anemia and hypoalbuminemia in German geriatric inpatients: Relationship to nutritional status and comprehensive geriatric assessment. Z Gerontol Geriatr 48(7):619–624
Sabol VK, Resnick B, Galik E, Gruber-Baldini A, Morton PG, Hicks GE (2010) Anemia and its impact on function in nursing home residents: what do we know? J Am Acad Nurse Pract 22(1):3–16
Yildirim T, Yalcin A, Atmis V, Cengiz OK, Aras S, Varli M, Atli T (2015) The prevalence of anemia, iron, vitamin B12, and folic acid deficiencies in community dwelling elderly in Ankara, Turkey. Arch Gerontol Geriatr 60(2):344–348
Mitrache C, Passweg JR, Libura J, Petrikkos L, Seiler WO, Gratwohl A, Stahelin HB, Tichelli A (2001) Anemia: an indicator for malnutrition in the elderly. Ann Hematol 80(5):295–298
Jauregui-Lobera I (2014) Iron deficiency and cognitive functions. Neuropsychiatr Dis Treat 10:2087–2095
Massa E, Madeddu C, Lusso MR, Gramignano G, Mantovani G (2006) Evaluation of the effectiveness of treatment with erythropoietin on anemia, cognitive functioning and functions studied by comprehensive geriatric assessment in elderly cancer patients with anemia related to cancer chemotherapy. Crit Rev Oncol Hematol 57(2):175–182
Mancuso A, Migliorino M, De Santis S, Saponiero A, De Marinis F (2006) Correlation between anemia and functional/cognitive capacity in elderly lung cancer patients treated with chemotherapy. Ann Oncol 17(1):146–150
Arik G, Varan HD, Yavuz BB, Karabulut E, Kara O, Kilic MK, Kizilarslanoglu MC, Sumer F, Kuyumcu ME, Yesil Y et al (2015) Validation of Katz index of independence in activities of daily living in Turkish older adults. Arch Gerontol Geriatr 61(3):344–350
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9(3):179–186
Thal LJ, Grundman M, Golden R (1986) Alzheimer’s disease: a correlational analysis of the blessed information-memory-concentration test and the mini-mental state exam. Neurology 36(2):262–264
Guigoz Y, Vellas B (1999) The Mini Nutritional Assessment (MNA) for grading the nutritional state of elderly patients: presentation of the MNA, history and validation. Nestle Nutr Workshop Ser Clin Perform Programme 1:3–11 (discussion 11–12)
Blanc B, Clement A, Hallberg L, Herbert V et al (1968) Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser 405:5–37
Beutler E, Waalen J (2006) The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood 107(5):1747–1750
Fairbanks VF (1991) Laboratory testing for iron status. Hosp Pract (Off Ed) 26(Suppl 3):17–24
Schneider AL, Jonassaint C, Sharrett AR, Mosley TH, Astor BC, Selvin E, Coresh J, Gottesman RF (2016) Hemoglobin, anemia, and cognitive function: the atherosclerosis risk in Communities Study. J Gerontol A Biol Sci Med Sci 71(6):772–779
Subramaniam G, Girish M (2015) Iron deficiency anemia in children. Indian J Pediatr 82(6):558–564
Fairweather-Tait SJ, Wawer AA, Gillings R, Jennings A, Myint PK (2014) Iron status in the elderly. Mech Ageing Dev 136–137:22–28
Penninx BW, Pahor M, Cesari M, Corsi AM, Woodman RC, Bandinelli S, Guralnik JM, Ferrucci L (2004) Anemia is associated with disability and decreased physical performance and muscle strength in the elderly. J Am Geriatr Soc 52(5):719–724
Cesari M, Penninx BW, Lauretani F, Russo CR, Carter C, Bandinelli S, Atkinson H, Onder G, Pahor M, Ferrucci L (2004) Hemoglobin levels and skeletal muscle: results from the InCHIANTI study. J Gerontol A Biol Sci Med Sci 59(3):249–254
Kilpatrick L, Houston DK, Wilson VK, Lovato J, Ayonayon HN, Cauley JA, Harris T, Simonsick EM, Yaffe K, Kritchevsky SB et al (2018) Low 25-hydroxyvitamin D concentrations and risk of incident cognitive impairment in black and white older adults: the Health ABC Study. J Nutr Gerontol Geriatr 37:1–13. https://doi.org/10.1093/gerona/glu184
Annweiler C, Doineau L, Gerigne L, Provendier A, Karras SN, Beauchet O, Fantino B, Duval GT (2018) Vitamin D and subjective memory complaint in community-dwelling older adults. Cur Alzheimer Res. https://doi.org/10.2174/1567205015666180201153735
Haslam A, Johnson MA, Hausman DB, Cress ME, Houston DK, Davey A, Poon LW, Georgia Centenarian S (2014) Vitamin D status is associated with grip strength in centenarians. J Nutr Gerontol Geriatr 33(1):35–46
Bo Y, Liu C, Ji Z, Yang R, An Q, Zhang X, You J, Duan D, Sun Y, Zhu Y et al (2018) A high whey protein, vitamin D and E supplement preserves muscle mass, strength, and quality of life in sarcopenic older adults: a double-blind randomized controlled trial. Clin Nutr
Gimigliano F, Moretti A, de Sire A, Calafiore D, Iolascon G (2018) The combination of vitamin D deficiency and overweight affects muscle mass and function in older post-menopausal women. Aging Clin Exp Res
Dhaliwal R, Mikhail M, Usera G, Stolberg A, Islam S, Ragolia L, Aloia JF (2018) The relationship of physical performance and osteoporosis prevention with vitamin D in older African Americans (PODA). Contemp Clin Trials 65:39–45
Iolascon G, Letizia Mauro G, Fiore P, Cisari C, Benedetti MG, Panella L, A DES, Calafiore D, Moretti A, Gimigliano F (2017) Can vitamin D deficiency influence muscle performance in post-menopausal women? A multicenter retrospective study. Eur J Phys Rehabil Med
Formiga F, Ferrer A, Almeda J, San Jose A, Gil A, Pujol R (2011) Utility of geriatric assessment tools to identify 85-years old subjects with vitamin D deficiency. J Nutr Health Aging 15(2):110–114
Levis S, Gomez-Marin O (2017) Vitamin D and physical function in sedentary older men. J Am Geriatr Soc 65(2):323–331
Camaschella C (2015) Iron deficiency: new insights into diagnosis and treatment. Hematol Am Soc Hematol Educ Program 2015:8–13
Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L (2016) Iron deficiency anaemia. Lancet 387(10021):907–916
Khadem G, Scott IA, Klein K (2012) Evaluation of iron deficiency anaemia in tertiary hospital settings: room for improvement? Intern Med J. 42(6):658–664
Ho CH, Chau WK, Hsu HC, Gau JP, You JY, Chen CC (2005) Predictive risk factors and prevalence of malignancy in patients with iron deficiency anemia in Taiwan. Am J Hematol 78(2):108–112
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. This study was presented as an oral presentation at the International Academic Geriatric Congress 2017, Antalya—Turkey, 12–16 April 2017.
Ethical approval
The Ankara University Ethics Committee approved the study (No: 03-107-17). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all participants included in the study. Written informed consent was approved by the Ankara University Ethics Committee.
Additional information
Esat Çinar: No longer works at our İnstitution.
Rights and permissions
About this article
Cite this article
Selvi Öztorun, H., Çınar, E., Turgut, T. et al. The impact of treatment for iron deficiency and iron deficiency anemia on nutritional status, physical performance, and cognitive function in geriatric patients. Eur Geriatr Med 9, 493–500 (2018). https://doi.org/10.1007/s41999-018-0065-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-018-0065-z