Abstract
Iron deficiency is not just anemia; it can be responsible for a long list of other manifestations. This topic is of great importance, especially in infancy and early childhood, for a variety of reasons. Firstly, iron need is maximum in this period. Secondly, diet in infancy is usually deficient in iron. Thirdly and most importantly, iron deficiency at this age can result in neurodevelopmental and cognitive deficits, which may not be reversible. Hypochromia and microcytosis in a complete blood count (CBC) makes iron deficiency anemia (IDA) most likely diagnosis. Absence of response to iron should make us look for other differential diagnosis like β thalassemia trait and anemia of chronic disease. Celiac disease is the most important cause of true IDA not responding to oral iron therapy. While oral ferrous sulphate is the cheapest and most effective therapy for IDA, simple nonpharmacological and pharmacological measures can go a long way in prevention of iron deficiency.
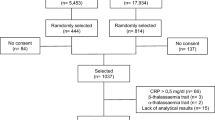
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overwhelmed by the high prevalence of nutritional anemia, especially iron deficiency anemia (IDA), in seemingly normal children, most practitioners tend to neglect this problem. Apart from the fact that most of these children are “seemingly normal”, another reason for this state of affairs could be the nomenclature.
Would this issue get the attention it deserves if instead of IDA, we use alternative terms like iron deficiency disease or iron deficiency induced cognitive deficit? This is a point worth pondering over. From the practitioners point of view, a few points need to be highlighted before the topic is discussed in detail.
-
Anemia is not a diagnosis. It is a manifestation of a large number of diseases. Do not rest till you have elucidated the cause of it.
-
Anemia is only one manifestation of IDA; one of the spectrum of manifestations of the problem of iron deficiency disease.
-
Always tell yourself that even IDA is not a complete diagnosis. Though most commonly nutritional, keep your mind open for other uncommon etiologies.
-
Microcytic, hypochromic anemia is usually, but not always due to iron deficiency.
Why are Children Especially Prone to Development of Iron Deficiency Anemia?
Iron being an essential nutrient, nature has made humans predominantly self sufficient in iron. Seventy five percent of the iron in our body is bound in heme proteins – myoglobin and hemoglobin. Approximately 20 % is bound in storage protein, ferritin and hemosiderin and 3 % is bound in critical enzyme systems – cytochromes, catalases and peroxidases [1].
Most of the iron needs of the body are met by the recycling machinery- recycled iron available from breakdown of old red blood cells by macrophages of the reticuloendothelial system, thus making us predominantly self sufficient in this critical nutrient. In adults, the diet needs to replenish only the amount lost from the gastrointestinal tract which is roughly 5 % of the daily iron needs. In infants and children diet needs to provide 30 % of the daily iron needs because of the growth spurt and increase in muscle mass. At birth, and up to 4 mo of age in a full term baby, the infant is in a state of “iron feast”. This is the result of the generous neonatal reserves of storage iron and the iron replenished from hemoglobin breakdown as the concentration of hemoglobin declines from a mean of 17 g/dl at birth to a nadir of 11 g/dl at 2 mo of age. At around 4 mo of age, as nature shifts partial responsibility of iron balance to nurture, iron “feast” transitions to iron “famine”. The rapidly expanding blood volume from 4 to 12 mo of age and thus the large amount of iron needed to maintain the mean hemoglobin concentration of 12.5 g/dl is responsible for this vulnerability. The problem is compounded by a diet which is often either poor in iron or rich in non-bioavailable iron.
Intestinal iron absorption is dependent on three factors [2]:
-
1.
Body iron stores: transferrin and ferritin
-
2.
Erythropoeitic rate
-
3.
Bioavailability of dietary iron
The bioavailability of iron is dependent on two factors. First, animal (heme) sources like fish, poultry, meat etc. have higher bioavailability than vegetable sources. Secondly, the presence of absorption enhancers and absorption inhibitors also influence boavailability. While ascorbic acid enhances absorption, tannates (tea), phosphates and phytates (plant fiber) inhibit absorption.
Main Causes of Iron Deficiency in Children (Table 1)
From the foregoing it is easy to understand the risk factors for IDA in children.
-
1.
Perinatal risk factors: Maternal iron deficiency will decrease the neonatal iron storage reserves [3], while prematurity increases the risk by virtue of the smaller blood volume at birth, increased loss through phlebotomies and poor gastrointestinal absorption of iron.
-
2.
Dietary factors: A diet poor in iron, for example, prolonged breast feeding without iron supplementation [4] and a diet rich in non-bioavailable iron, for example, a vegetarian diet, are important risk factors. Unmodified cow’s milk increases intestinal blood loss in infants [5], while bottle feeding contributes to the risk independently, probably due to the greater volume of cow’s milk consumed [6].
-
3.
Gastrointestinal diseases: Though iron is absorbed throughout the intestine, it is maximally absorbed in the duodenum. Diseases involving the duodenum – Celiac disease, Crohn’s disease and giardiasis, thereby are important etiologies. Increased gastrointestinal loss as seen in inflammatory bowel disease (IBD), cow’s milk protein induced colitis and chronic use of nonsteroidal anti-inflammatory drugs is also associated with iron deficiency.
Iron Deficiency: There is More to it Than Just Anemia!
Clinical Features
-
Anemia and its symptoms More often than not, anemia is asymptomatic. The only manifestation could be pallor which is best detected at sites where capillary beds are visible – conjunctiva, palms and nail beds. Pallor at these sites is predictive of moderate to severe anemia, but mild, or for that matter, even severe anemia, may be missed if one relies solely on this physical finding. Lethargy or fatiguability, tachycardia, irritability and poor appetite are also consequences of the anemic state. Uncommonly, one still comes across patients with severe IDA leading to congestive heart failure.
-
Neurocognitive effects Impaired psychomotor and mental development in iron deficient children with some evidence that some of the effects may not be reversible and that they can be seen even with iron deficiency without anemia, makes this issue of great public health importance [7, 8] (Table 2). The critical role of iron in the function of various enzymes in neural tissues is responsible for the neurocognitive deficits. Additionally, iron deficiency increases the risk for lead exposure through pica and increased absorption and thus may contribute further to the neurocognitive effects of iron deficiency [ID].
Table 2 IDA… beyond just anemia! -
Immunity and infection Iron has mixed effects on susceptibility to infections. Iron deficiency, by its effects on lymphocyte function including defective IL 2 and IL 6 production [9–12], increases the susceptibility to infection. On the other hand, risk of malaria is influenced by iron status and deficiency of iron protects children from malarial morbidity and mortality [13]. Several studies identify increased malarial risk in individuals treated with iron through mechanisms of rapid saturation of iron-binding proteins [14, 15], but other studies suggest that standard doses of iron supplements do not increase the risk for malaria [16–18].
-
Pica Pica, defined as a compulsive consumption of non nutritive substances, is a common symptom of IDA. Pagophagia [ice consumption], amylophagia [starch consumption] and geophagia [mud consumption] are often seen in IDA with pagophagia being rather specific for IDA [19]. It may occur even in the absence of anemia and responds well to treatment. The mechanism through which iron deficiency causes pica is not known. It is important to remember that pica also occurs in children with developmental disabilities even without the presence of iron deficiency in this group of children.
-
Thrombosis IDA has been reported to be associated with stroke, as shown in a large case control study from the stroke registry in Canada, where previously healthy children with stroke [arterial or venous] were ten times more likely to have IDA than healthy children without stroke [20].
-
Exercise capacity Iron being an essential cofactor for enzyme driven aerobic metabolism, iron deficiency leads to decreased exercise performance.
-
Epithelial changes Angular stomatitis, glossitis, formation of a post cricoid esophageal web [Plummer Vinson syndrome], platynychia [flat nails] and koilonychia [spoon shaped nails] are all well known epithelial changes seen in long standing IDA.
-
Others
-
• Breath holding spells: Iron supplementation, reduces the frequency of cyanotic breath holding spells [21].
-
• Iron deficiency has been associated with restless legs syndrome and periodic limb movement disorder. Iron supplementation, to target a serum ferritin level of 50–100 μg/L is recommended in these conditions.
-
Diagnosis
Screening for IDA
Children with any of the manifestations of IDA should obviously be investigated further. But considering that most children with IDA are asymptomatic and pallor is an unreliable sign, who should be screened for IDA? While the American Academy of Pediatrics recommends universal screening at approximately 1 y of age, there are no guidelines in India. At a bare minimum, screening should be essential for children who have any one of the following:
-
– History of prematurity
-
– Those with dietary risk factors such as:
-
• infants not exclusively breast fed till 5–6 mo of age
-
• infants exclusively breast fed beyond 6 mo of age
-
• infants fed cow’s milk below 1 y of age
-
• preschool children with excessive consumption of milk or a diet deficient in iron rich food
-
The simplest and most cost effective measurement is a complete blood count (CBC), which is performed on an automated analyser and gives data on hemoglobin, MCV (mean corpuscular volume) and RDW (red cell distribution width), a measure of variability in red cell size.
Investigations
Tests used for diagnosis differ depending on the stage in the progress of IDA [1].
Iron Deficiency (ID) without Anemia
In this stage there is a depletion of iron stores without anemia.
-
• Absent marrow reticuloendothelial iron revealed by absence of hemosiderin on iron staining of bone marrow
-
• Hemoglobin levels are normal
Iron Deficiency with Mild Anemia
-
• Decreased serum iron [<60 microgram/dl {N = 60–150 microgram/dl}]
-
• Increased total iron binding capacity [TIBC]
-
• Decreased transferrin saturation [iron/TIBC] <15 [normal 20–50]
-
• Hb 9–12 g%
-
• RBC morphology: normal or slightly hypochromic
-
• Serum ferritin <20 [Normal 40–200 microgm/L]
Severe Iron Deficiency with Moderate to Severe Anemia
-
• Significantly decreased iron, increased TIBC
-
• Transferrin saturation <10 %
-
• Hb 6–7 g%
-
• RBC morphology: hypochromia and microcytosis
-
• Serum ferritin <10 μg/L
The most commonly used parameters for diagnosis of IDA are: Hb [↓], Transferrin saturation [↓], MCH and MCV [hypochromia and microcytosis], serum ferritin [↓] (Table 3).
Differential Diagnosis
Hypochromia (↓MCH) and microcytosis (↓MCV) are the hallmarks of IDA, but there are other conditions which produce mild hypochromic, microcytic anemia and be confused with IDA. The two most important of these are β thalassemia trait (and uncommonly in the Indian context, α thalassemia trait too) and anemia of chronic disease (ACD) (Table 4).
Beta Thalassemia Trait
In this condition, there is no evidence of decreased erythropoeisis and hence the RBC count is normal. This is reflected in Mentzer index, which helps in differentiating β thalassemia trait from IDA. The Mentzer index is obtained by dividing the mean corpuscular volume (MCV, in fL) by the red blood cell count (RBC, in millions per microlitre). An index of less than 13 suggests that the patient has thalassemia trait, and an index of more than 13 suggests that the patient has iron deficiency. Secondly, anisocytosis is not seen on the peripheral smear and hence the red cell distribution width (RDW) value in the complete blood count (CBC) is normal. Conversely, anisocytosis leads to an increased RDW in IDA and the decreased erythropoeisis leads to a decrease in RBC count. Additional confirmation will be provided by iron studies (normal iron and normal transferrin saturation in β thalassemia trait) and quantitative hemoglobin A2 estimation which is increased in β thalassemia trait. However, in a patient of β thalassemia trait with concomitant IDA, HbA2 may be falsely normal.
Anemia of Chronic Disease (ACD)
Usually ACD is normocytic and normochromic with low serum iron concentration and low total iron binding capacity and thus the percent saturation of transferrin is normal. But upto 25 % of these patients have a microcytic, hypochromic anemia and approximately 20 % of patients with ACD have low transferrin saturation in the iron deficiency range [22]. In inflammatory states, serum ferritin is elevated as it is an acute phase reactant, while in iron deficiency anemia it is low. Confusion arises when the patient has ACD with coexistent IDA. There are three ways of diagnosing IDA in a child with ACD:
-
a.
Bone marrow examination for stainable iron. Absence of hemosiderin in iron staining of bone marrow is diagnostic of iron deficiency.
-
b.
Measurement of serum levels of soluble transferrin receptor [sTfr]: In IDA there is an increase in cellular membrane transferrin receptor density and truncated form of soluble transferrin receptor [sTfR] appear in the serum in increased amounts [23].
-
c.
A trial of iron supplementation and monitoring the response will help us know the contribution of iron deficiency to the anemia.
When to Suspect Conditions Other Than IDA in Any Child with Anemia
-
1.
Presence of icterus and splenomegaly. A small splenomegaly may be seen in IDA but a large splenomegaly goes against the diagnosis.
-
2.
If the anemia is not hypochromic and microcytic
-
3.
If there is reticulocytosis
-
4.
If there is pancytopenia
Justification of Empiric Therapy with Iron in a Hypochromic Microcytic Anemia
Since infants upto 24 mo of age are usually iron deficient, an empiric trial of iron is justified if the CBC reveals mild hypochromic, microcytic anemia in the absence of reticulocytosis and splenomegaly. Iron in a dose 3–6 mg/kg/d [elemental iron] given once or twice a d between meals should produce a rise of hemoglobin by 1 g/dl in 4 wk [24]. Even in older children if the history is suggestive of diet poor in iron or in bioavailable iron, one can give a trial of empiric iron therapy. When giving empiric iron therapy, it is essential to follow up regularly to confirm response to therapy and also to confirm normalisation of RBC indices. Failure of either response to therapy or normalisation of the indices, should make one consider other differentials like β thalassemia trait, ACD and refractory IDA.
IDA Treatment: Don’t Just Give Iron and Forget it
Successful treatment of IDA depends on three essential steps:
-
1.
Iron therapy
-
2.
Dietary changes
-
3.
Lab monitoring for assessment of response
Iron Therapy
Oral iron therapy is best administered as oral ferrous sulphate as it is the most cost effective. Dose is 3–6 mg/kg/d of elemental iron (maximum is 150 mg). A dose of 3 mg/kg is sufficient for treatment and this dose is also associated with fewer adverse effects. For optimum absorption, iron should be given between meals and with vitamin C containing juice rather than milk. A reticulocyte response is seen in 72 h and hemoglobin should increase by 1 g/dl in 1 mo. Other ferrous salts like ferrous fumarate and ferrous gluconate may be used; the dose of elemental iron remains the same but the amount of elemental iron varies from one salt to another.
Ascorbate combined with iron increases iron absorption but this advantage is nullified because of the higher incidence of adverse effects [25]. Heme based preparations, ferric ammonium citrate and iron polymaltose complex may be less efficacious.
Gastrointestinal symptoms like constipation and diarrhea are uncommon with iron preparations at the doses mentioned above. Grey staining of teeth is seen with liquid preparations and is temporary. This can be minimised by brushing the teeth and rinsing mouth with water after administration of the liquid preparation. All children with IDA should also be given anthelminthics.
Dietary Changes
Bottle feeding leads to consumption of large amount of milk [6]. Getting rid of the bottle is an essential first step in the treatment. Unmodified cow’s milk should be avoided under 1 y of age and if unavoidable due to failure of breast feeding and lack of affordability of formula feed, it is essential to give iron supplementation and monitor for IDA. For children more than 1 y of age, milk consumption should not be more than 500 ml/d. Consumption of iron rich food should be encouraged.
Monitoring Response
A repeat CBC after 1 mo of iron therapy should show an increase in hemoglobin by 1 g/dl. Confirm normalisation of hemoglobin (as per age adjusted normal values) by repeating a CBC every 2–3 mo and continue iron supplementation for a further 3 mo after normalisation of hemoglobin to replenish the storage pool.
Reasons for Lack of Response to Iron Therapy
Nonresponders, those who do not respond to iron could fall in one of two categories:
-
1.
Hypochromic microcytic anemia but not IDA: Thalassemia trait and ACD
-
2.
IDA but recurrent or refractory:
-
a.
Poor compliance to medications or to dietary advice.
-
b.
Overt/occult gastrointestinal blood loss, e.g. , cow milk protein induced colitis
-
c.
Parasitic infestation
-
d.
Meckel’s diverticulitis
-
e.
Celiac disease
-
f.
Pulmonary hemosiderosis (occult/overt blood loss in lungs)
-
g.
Inflammatory bowel disease
-
h.
Rare mutations of iron transport
-
a.
For the second group, further investigations like stool for occult blood, endoscopy for evidence of upper/lower gastrointestinal bleed, and tissue transglutaminase antibodies (TTG) to rule out celiac disease are recommended.
Prevention of Iron Deficiency Anemia
Iron reserves, in normal birth weight, term infants, are exhausted by 5–6 mo of age. The iron content of unfortified, conventional complementary foods is insufficient to meet the high iron requirements of growing infants. Low birth weight, premature infants and infants of mothers with anemia need added iron starting at 1 mo of age, with a dose of 2 mg/kg/d.
Simple Nonpharmacologic Interventions to Prevent IDA
-
Delayed cord clamping at birth: delaying the clamping of cord to more than 1 min after birth is, along with other benefits, associated with lesser IDA in infancy [26].
-
Use of iron pots for cooking [27]
-
Avoid use of bottle for feeding infants and children.
-
Exclusive breast feeding till 6 mo of age
-
Avoid unmodified, nonformula cow milk feeding till 1 y of age.
-
From 1 to 5 y of age, children should not consume >500 ml of milk per day
-
Prevent and treat iron deficiency in pregnant women so that the newborn is born with good iron stores
-
a.
Ensure consumption of iron rich food like chickpea [chana sag], fenugreek leaves [methi], spinach [palak], amaranth [chaulai], mustard leaves [sarson ka sag], onion stalks [pyaaz ki kali], lentil [dal], Bengal gram [kala chana], other whole pulses, ground nuts, soya bean, jaggery [gur], eggs, meat, poultry and fish.
-
a.
-
Encourage addition of absorption enhancers like vitamin C rich foods and discourage consumption of absorption inhibitors like tea, with or shortly after a meal
-
Calcium inhibits absorption of iron by almost 60 %. The two should be given separately with sufficient time interval between them.
Pharmacologic Measures for Prevention of IDA
A fixed 12.5 mg dose of elemental iron would meet almost 90 % of the total iron requirement of children between 6 and 18 mo of age [28].
Thus while actively promoting nonpharmacologic measures, it would be good to provide a 12.5 mg elemental iron supplementation to all children in the age group of 6–24 mo. Preventive antihelminthic therapy should be given to all children at 6 mo intervals.
In view of the importance of iron deficiency and the magnitude of the problem, Government of India is running several programmes namely National Nutritional Anemia Control Programme, National Nutritional Anemia Prophylaxis Programme, Adolescent Girls Anemia Control Programme, WIFS [Weekly Iron Folic Acid Supplementation], Iron Plus Initiative, to tackle this problem.
References
Brittenham GM. Disorders of iron metabolism: Iron deficiency and overload. In: Hoffman R, Benz Jr EJ, Shattil SJ, editors. Hematology Basic Principles and Practice. 4th ed. New York: Churchill Livingstone; 2005. p. 481.
Conrad ME, Umbreit JN. Iron absorption and transport-an update. Am J Hematol. 2000;64:287–98.
Kumar A, Rai AK, Basu S, Dash D, Singh JS. Cord blood and breast milk iron status in maternal anemia. Pediatrics. 2008;121:e673–7.
Calvo EB, Galindo AC, Aspres NB. Iron status in exclusively breast-fed infants. Pediatrics. 1992;90:375–9.
Ziegler EE, Fomon SJ, Nelson SE, Rebouche CJ, Edwards BB, Rogers RR, et al. Cow milk feeding in infancy: further observations on blood loss from the gastrointestinal tract. J Pediatr. 1990;116:11–8.
Sutcliffe TL, Khambalia A, Westergard S, Jacobson S, Peer M, Parkin PC. Iron depletion is associated with daytime bottle-feeding in the second and third years of life. Arch Pediatr Adolesc Med. 2006;160:1114–20.
Oski FA, Honig AS, Helu B, Howanitz P. Effect of iron therapy on behaviour performance in nonanemic, iron deficient infants. Pediatrics. 1983;71:877–80.
Akman M, Cebeci D, Okur V, Angin H, Abali O, Akman AC. The effects of iron deficiency on infant developmental test performance. Acta Pediatr. 2004;93:1391–6.
Thibault H, Galan P, Selz F, Preziosi P, Olivier C, Badoual J, et al. The immune response in iron-deficient young children: effect of iron supplementation on cell-mediated immunity. Eur J Pediatr. 1993;152:120–4.
Galan P, Thibault H, Preziosi P, Hercberg S. Interleukin 2 production in iron-deficient children. Biol Trace Elem Res. 1992;32:421–6.
Ekiz C, Agaoglu L, Karakas Z, Gurel N, Yalcin I. The effect of iron deficiency anemia on the function of the immune system. Hematol J. 2005;5:579–83.
Gera T, Sachdev HP. Effect of iron supplementation on incidence of infectious illness in children: systematic review. BMJ. 2002;325:1142.
Gwamaka M, Kurtis J, Sorensen B, Holte S, Morrison R, Mutabingwa TK, et al. Iron deficiency protects against severe plasmodium falciparum malaria and death in young children. Clin Infect Dis. 2012;54:1137–44.
Oppenheimer SJ, Gibson FD, Macfarlane SB, Moody JB, Harrison C, Spencer A, et al. Iron supplementation has been reported to increase the prevalence and effects of malaria: report on clinical studies in Papua New Guinea. Trans R Soc Trop Med Hyg. 1986;80:603–12.
Smith AW, Hendrickse RG, Harrison C, Hayes RJ, Greenwood BM. The effects on malaria of treatment of iron deficiency anemia with oral iron in Gambian children. Ann Trop Paediatr. 1989;9:17–23.
Ianotti LL, Tielsch JM, Black MM, Black RE. Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr. 2006;84:1261–76.
Mebrahtu T, Stolzfus RJ, Chwaya HM, Jape JK, Savioli L, Montresor A, et al. Low dose daily iron supplementation for 12 mo does not increase the prevalence of malarial infection or density of parasites in young Zanzibari children. J Nutr. 2004;134:3037–41.
Menendez C, Kahigwa E, Hirt R, Vounatsou P, Aponte JJ, Font F, et al. Randomised placebo controlled trial of iron supplementation and malaria chemoprophylaxis for prevention of severe anemia and malaria in Tanzanian infants. Lancet. 1997;350:844–50.
Brown WD, Dyment PG. Pagophagia and iron deficiency anemia in adolescent girls. Pediatrics. 1972;49:766–7.
Maguire JL, de Veber G, Parkin PC. Association between iron-deficiency anemia and stroke in young children. Pediatrics. 2007;120:1053–7.
Zehetner AA, Orr N, Buckmaster A, Williams K, Wheeler DM. Iron supplementation for breath-holding attacks in children. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.CD008132.pub2.
Schilling RF. Anemia of chronic disease: a misnomer. Ann Intern Med. 1991;115:572–3.
Suominen P, Motttonen T, Rajamaki A, Irjala K. Single values of serum transferring receptor and transferring receptor ferritin index can be used to detect true and functional iron deficiency in rheumatoid arthritis patients with anemia. Arthritis Rheum. 2000;43:1016–20.
American Academy of Pediatrics. Iron. In: Kleinman RE, Greer FR, editors. Pediatric nutrition. 7th ed. Elk Grove Village: American Academy of Pediatrics; 2011. p. 449.
Hallberg L, Brune M, Rossander L. Effect of ascorbic acid on iron absorption from different types of meals. Studies with ascorbic acid rich foods and synthetic ascorbic acid given in different amounts with different meals. Hum Nutr Appl Nutr. 1986;40:97.
Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Committee opinion No. 543: timing of umbilical cord clamping after birth. Obstet Gynecol. 2012;120:1522–6.
Adish AA, Esrey SA, Gyorkos TW, Jean-Baptiste J, Rojhani A. Effect of consumption of food cooked in iron pots on iron status and growth of young children: a randomised trial. Lancet. 1999;353:712–6.
Kotecha PV. Nutritional anemia in young children with focus on Asia and India. Indian J Community Med. 2011;36:8–16.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Subramaniam, G., Girish, M. Iron Deficiency Anemia in Children. Indian J Pediatr 82, 558–564 (2015). https://doi.org/10.1007/s12098-014-1643-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1643-9