Abstract
Background
Cardiac surgery-associated acute kidney injury (CSA-AKI) is associated with high risk for complications and mortality. Whether renin–angiotensin system (RAS) inhibitor should be continued or withdrawn in patients with long-term use before cardiac surgery has been lack of consensus.
Methods
We performed this prospective observational cohort study and recruited cardiac surgery patients in the surgical intensive care units between 2000 and 2011. These patients were divided into users and non-users of RAS inhibitor. Propensity score matching and multivariable models were performed to investigate the association between renal outcome, mortality, and preoperative use of RAS inhibitor.
Results
Preoperative use of RAS inhibitor was identified as the independent protective factor for AKI development (OR 0.41, 95% CI 0.23, 0.63), AKI severity (stage 3 vs. stage 1, OR 0.35, 95% CI 0.18, 0.69), and renal recovery (OR 3.41, 95% CI 1.84, 5.36). Nevertheless, there was no significant protective effect of RAS inhibitor on in-hospital dialysis, in-hospital mortality, and ensuing development of chronic kidney disease (CKD) after AKI. We created a prediction model of CSA-AKI and indicated that preoperative use of RAS inhibitor provided more protective effect in low-risk than high-risk population.
Conclusion
Preoperative use of RAS inhibitor was associated with less AKI development and severity, and higher renal recovery. Although more risk reduction of AKI development was shown in low-risk group by our prediction model, continued use of RAS inhibitor before cardiac surgery could provide protective effect in all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) has increased remarkably in intensive care unit (ICU) patients and leads to various complications and high mortality [1, 2]. No promising therapeutic agent could prevent or treat AKI up to now [3]. Nevertheless, based on previous studies, renin–angiotensin system (RAS) inhibitor might have potential protective effect to prevent AKI, especially for cardiac surgery-associated acute kidney injury (CSA-AKI). Not only because burgeoning studies have shown that long-term inhibition of RAS provides both cardiovascular and renal protection [4], but also because recent animal studies of renal ischemia–reperfusion injury (IRI), similar to the major mechanism of CSA-AKI, demonstrated the promising effect of RAS inhibitor to reduce ensuing chronic kidney disease (CKD) and mortality [5]. Furthermore, RAS inhibitors including angiotensin-converting enzyme (ACE) inhibitor and angiotensin receptor blocker (ARB) have also been reported to prevent subsequent CKD development in patients with renal recovery from CSA-AKI [6, 7]. Even so, there is still a lack of consensus for continuation or withdrawal of RAS inhibitor in patients before cardiac surgery.
CSA-AKI is the second commonest cause of AKI in ICU [8], and occurs in up to 30–42% of patients according to the population of interest and different definition [9]. The development of CSA-AKI results in dialysis in approximately 1–5% of patients, and is associated with high mortality and complicated hospital course [10, 11]. Several previous studies demonstrated that preoperative use of RAS inhibitor is associated with increased risk of CSA-AKI [12, 13]. On the contrary, some recent cohort studies, especially in Asian population and meta-analysis study reported an association between preoperative use of RAS inhibitor and lower incidence of CSA-AKI [14, 15]. These inconsistent results might be due to racial differences or elusive effect of RAS inhibitor on CSA-AKI.
To investigate the clinical application of continued use of RAS inhibitor before cardiac surgery and its impact on development of CSA-AKI as well as other outcomes such as in-hospital dialysis, in-hospital mortality and ensuing CKD, we studied these associations with propensity score matching and analysis using our prospectively collected observational cohort. Furthermore, we established a prediction model to determine the effect of preoperative continuation of RAS inhibitor on CSA-AKI. This would provide physicians with more individualized risk stratification information of the use of RAS inhibitor before cardiac surgery.
Methods
Study design and population
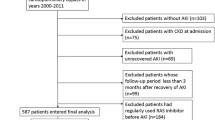
This study was performed in National Taiwan University Hospital (NTUH) which is a tertiary hospital including its three branch hospitals in different cities. We enrolled patients who were ≥ 18 years old and hospitalized in the surgical ICU (SICU) for postoperative care of cardiac surgery with or without cardiopulmonary bypass (CPB) between January 1, 2000 and December 31, 2011. Patients undergoing regular dialysis were excluded. The follow-up was continued until September 30, 2016. The study was approved by the Institutional Review Board of NTUH (No. 31MD03) and adhere to the Declaration of Helsinki. An informed consent was waived because there was no breach of privacy and no interference with patient care (Fig. 1).
Data collection
Preoperative demographic data was obtained at SICU admission. These variables included age, gender, smoking history, hypertension (HTN) (using anti-HTN agents or systolic/diastolic blood pressure > 140/90 mmHg at admission), congestive heart failure (CHF) [defined as New York Heart Association (NYHA) functional class III or IV], peripheral arterial occlusive disease (PAOD) (defined by clinical or imaging diagnosis), diabetes mellitus (DM) (using oral hypoglycemic agents or insulin), CKD (defined as abnormalities of kidney structure, hematuria, proteinuria or estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2 presented for more than 3 months), and coronary arterial disease (CAD) (defined by the diagnostic code of ischemic heart disease prior to admission and positive electrocardiographic findings). Chronic obstructive pulmonary disease (COPD), liver cirrhosis (LC), hyperlipidemia, hyperuricemia, and metastatic cancer were recorded according to diagnostic codes prior to admission.
Laboratory data such as baseline serum creatinine (SCr), albumin, hemoglobin, and urine protein were recorded at SICU admission. SCr assay was performed using reagent (OSR6178, reaction with picric acid) from Beckman Coulter Inc. (CA, USA) during the study period. Baseline SCr was determined as the last value measured at least 1 month, but no more than a year, prior to admission [16]. Baseline eGFR was calculated via the four-variable Modification of Diet in Renal Disease equation [17]. Peak SCr during AKI was also recorded. Urine protein was recorded using a dipstick within 2 days before cardiac surgery. The type of surgery was categorized as coronary artery bypass grafting (CABG), heart valve surgery, heart transplant, and others.
Medications such as anti-HTN agents (including RAS inhibitors, calcium channel blockers, β-blockers, α-blockers, clonidine) and lipid-lowering agents (statins) were recorded. Users of RAS inhibitor were defined as regular use of ACE inhibitor or ARB for at least 1 month before surgery, while the others were defined as non-users.
Outcome measures
The primary outcome was AKI development. The AKI definition and staging were based on Kidney Disease: Improving Global Outcomes (KDIGO) criteria [18]. Secondary outcomes were AKI recovery, in-hospital dialysis, in-hospital mortality, and ensuing stage 3 CKD development. AKI recovery was determined as SCr recovery to level within 0.3 mg/dl of baseline within 10 days after AKI [19]. For patients without CKD before operation, stage 3 CKD was determined by eGFR below 60 ml/min/1.73 m2 during the follow-up period. Patient who lost follow-up before September 30, 2016 were censored.
Statistical analysis
We performed statistical analyses with the SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA). Continuous variables were presented as mean ± standard deviation, and the difference between users and non-users of RAS inhibitor was compared with the Student’s t test. Categorical variables were summarized as percentages and analyzed with the Chi-square test. Two-sided P < 0.05 was considered statistically significant. Significant variables in the univariate analysis (P < 0.05) were included in the multivariate logistic regression model to investigate the association between use of RAS inhibitor and outcomes of AKI development, AKI severity, AKI recovery, in-hospital dialysis, and in-hospital mortality. For CKD development, we performed multivariate Cox regression model to identify significant associated variables. The survival curve for CKD development were plotted using Kaplan–Meier method.
Propensity score matching and analysis
To minimize the bias due to confounding by indications, the potential risk factors in the univariate analysis were adjusted in the multivariate logistic regression model, while generated similar comparison groups after using propensity scores matching based on Greedy matching algorithm [20, 21]. For outcomes of AKI development, AKI severity, in-hospital dialysis, in-hospital mortality, and CKD development, the propensity score was calculated by logistic regression which included age, sex, CKD, DM, CHF, CAD, PAOD, HTN, hyperlipidemia, COPD, LC, hyperuricemia, metastatic cancer, smoking, hemoglobin, baseline SCr, albumin, urine protein, type of surgery, anti-HTN agents, and statins. For AKI recovery, in addition to abovementioned variables, we added peak SCr in the propensity score calculation. Patients were then matched according to the difference in the logit of propensity scores that were less than a caliper of 0.2 standard deviations of this score. The matched cohorts were an attempt to group each patient who received RAS inhibitor therapy with two patients who did not receive this therapy (a 1:2 match). We used the Mantel–Haenszel test for categorical variables and generalized estimating equations (GEE) regression for continuous variables to estimate the degree of balance in these measured covariates. The multivariable analysis was conducted when the difference remained between two groups after propensity score matching. Statistical significance was set at P < 0.05.
Prediction model development
We used a combination of demographic characteristics and baseline laboratory data to determine variable selection by forward selection. In univariate logistic regression models, variables not associated with AKI (P > 0.05) were excluded from further analyses. Improvement in model performance through addition of new candidate variables in multivariate logistic regression models was tested using metrics for discrimination and goodness of fit.
Results
We enrolled 1160 patients with the median follow-up duration of 2.99 years. Of 1160 patients, mean age of the patients was 61.3 (± 15.3) years old and 69.6% were male. We found 273 patients received regular use of RAS inhibitor before cardiac surgery. Overall, 977 patients (84.2%) developed CSA-AKI and most cases of AKI were stage I (68.3%). More non-users of RAS inhibitor experienced AKI than users (87.8% vs. 72.9%, P < 0.001), especially AKI of stage II + stage III (non-users vs. users, 29.8% vs. 16.9%, P < 0.001).
Baseline characteristics
As shown in Table 1, the users of RAS inhibitor were older and had higher hemoglobin, albumin and lower baseline SCr when compared to the non-users. More users had HTN and anti-HTN medication. In contrast, more non-users had NYHA class III or IV CHF. After propensity score matching, these characteristics did not differ significantly (Supplementary Table 1).
Predictors for CSA-AKI development
Before propensity score matching, logistic regression analysis showed that predictors for CSA-AKI development included age, male sex, CHF, CAD, and hyperuricemia (Table 2). However, preoperative use of RAS inhibitor was significantly associated with lower risk for CSA-AKI [odd ratio (OR) 0.38, 95% confidence interval (CI) 0.25, 0.57, P < 0.001]. The other predictor against AKI was HTN (OR 0.56, 95% CI 0.32, 0.98, P = 0.04).
Predictors for ensuing CKD development after AKI
Before propensity score matching, Cox regression analysis showed that predictors for ensuing CKD included old age, CHF, and hyperuricemia (Table 3). In contrast, valve surgery, higher baseline eGFR and hemoglobin were associated with lower risk for ensuing CKD. However, preoperative use of RAS inhibitor was not a significant protective factor (OR 0.37, 95% CI 0.67, 1.16, P = 0.37). The Kaplan–Meier curve revealed the protective effect of preoperative use of RAS inhibitor on ensuing CKD during the early follow-up period, but this effect vanished in the late period (Fig. 2).
Propensity score matching for analysis of AKI development and other outcomes
After propensity score matching, use of RAS inhibitor remained the independent protective factor for AKI development (OR 0.41, 95% CI 0.23, 0.63, P < 0.001), AKI severity (stage 3 vs. stage 1, OR 0.35, 95% CI 0.18, 0.69, P = 0.003), and renal recovery (OR 3.41, 95% CI 1.84, 5.36, P < 0.001) (Table 4). Nevertheless, there was no significant protective effect of RAS inhibitor use on in-hospital dialysis, in-hospital mortality, and ensuing CKD development after AKI.
Prediction model of CSA-AKI
To improve patient outcomes with individualized risk prediction of CSA-AKI, we created the prediction model (Supplementary File 1), and showed the clinical and laboratory findings in three hypothetical patients (Supplementary Table 2). Male sex, CHF, hyperuricemia, CAD, heart transplant, and older patients (≥ 70 years old) were major risk factors in our prediction model. Patients with two or more of these major risk factors had probability of CSA-AKI over 75% even using RAS inhibitor and were therefore categorized as high-risk population. Under use of RAS inhibitor, patients with one or none of these major risk factors had probability of CSA-AKI 35–75% and less than 35% respectively, and were categorized as intermediate- or low-risk population. The predicted magnitude of clinical benefit from use of RAS inhibitor was much greater in low-risk patient. For example, high risk patient such as an old man with CKD, CAD, CHF underwent CABG or heart transplant without use of RAS inhibitor, the risk of CSA-AKI would be up to 96.43% and decrease to 91.03% when using RAS inhibitor (hypothetical patient A, Supplementary Table 2). On the contrary, low risk patient such as a young woman with HTN and underwent valve surgery, the risk of CSA-AKI would decrease a lot from 59.57 to 35.61% if she had preoperative use of RAS inhibitor (hypothetical patient C, Supplementary Table 2).
Discussion
This study showed that continued use of RAS inhibitor before cardiac surgery was independently associated with less CSA-AKI development, lower AKI severity, and higher renal recovery. Although the association of RAS inhibitor treatment with CSA-AKI has been controversial for a long time, our results should be highlighted. Not only because our study adopted KDIGO criteria of AKI to include milder AKI patients who were neglected in previous studies [12, 15], but also observed the associations between preoperative continued use of RAS inhibitor on severity and recovery of AKI. Moreover, we pointed out that there might be racial difference in the effect of RAS inhibitor on CSA-AKI.
Currently there is no promising pharmacologic agents to prevent AKI development. A major reason for this is that the etiology of AKI is heterogeneous and most mechanisms are not completely understood. Therefore, we chose patients undergoing cardiac surgery as the study population for two reasons, one of which is that CSA-AKI is the second commonest cause of AKI in the ICU, and the other is that IRI, an identical mechanism responsible for the animal model used in studies regarding RAS inhibition on AKI development and AKI-CKD transition, plays a critical role in the pathogenesis of CSA-AKI [9]. It is noteworthy that RAS activation occurs during AKI and sustains even after renal recovery in animal IRI model [5]. In animal model, angiotensin II level in ischemic kidneys was found to increase significantly 24 h after reperfusion, and ARB could accelerate recovery of renal function [22]. Moreover, Rodriguez-Romo et al. had indicated that the prophylactic administration of ARB before renal ischemia could prevent AKI-CKD transition. They also found that ARB pretreatment group had better renal blood flow 3 days after renal ischemia [23]. Our previous clinical and animal studies also showed that use of RAS inhibitor after complete renal recovery from CSA-AKI and IRI, respectively, was associated with less ensuing CKD development [5, 7]. Accordingly, RAS inhibitor has the potential to be extrapolated to prevent CSA-AKI development.
Physiological function of RAS inhibitor is to reduce glomerular efferent arteriolar resistance thereby attenuating glomerular hypertension, hyperfiltration and sclerosis in CKD [24]. However, RAS inhibition also leads to functional decrease of GFR and systemic hypotension, therefore making RAS inhibitor usually be discontinued before major operation including cardiac surgery and avoided during the acute phase of AKI, especially for CKD patients. In addition, several early retrospective studies had reported reduced incidence of AKI after discontinuation of RAS inhibitor before surgery [13, 25].
In an earlier meta-analysis including 29 observational studies showed that preoperative use of RAS inhibitor was associated with increased postoperative AKI and mortality in patients undergoing cardiac surgery [12]. However, odds ratios of the included studies in this analysis was not adjusted. Moreover, there were limitations such as heterogeneous definition of AKI across included studies as well as lack of randomized controlled trials (RCT). Furthermore, some CSA-AKI might be identified due to only renal functional change in users of RAS inhibitor, not real structural damage. In an observational study using novel biomarkers including neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1, interleukin-18, tissue inhibitor of metalloproteinase 2 (TIMP2), and insulin-like growth factor binding protein 7 (IGFBP7) to identify structural AKI, Coca et al. found that preoperative use of RAS inhibitor was associated with more functional than structural CSA-AKI [26].
On the contrary, Cheungpasitporn et al. conducted a meta-analysis with inclusion of more recent studies (1 RCT and 23 cohort studies) and pre-specified sensitivity analysis including only propensity score-based studies [15]. They discovered a significant association between preoperative RAS inhibitor treatment and lower incidence of AKI (OR 0.92, 95% CI 0.85, 0.99, P = 0.03). A RCT which was included in this meta-analysis also showed decreased CSA-AKI in patients with continued use of RAS inhibitor before cardiac surgery (AKI in placebo, ramipril, spironolactone groups 5.4%, 0.6%, 0.6%, respectively, P = 0.006) [27]. Nevertheless, the study enrolled only 458 patients in whom AKI was defined by SCr ≥ 2.5 mg/dl, hence mild AKI was excluded. With regards to mortality, Cheng et al. conducted a meta-analysis and indicated that preoperative use of RAS inhibitor was associated with a decreased risk of all-cause mortality in DM patients [28]. As a result, RAS inhibitor might have benefit in particular individuals undergoing cardiac surgery according to our results and recent meta-analysis. Even in non-cardiac surgery, Xu et al. retrospectively analyzed 12,545 hypertensive Chinese patients with propensity score matching and discovered a lower incidence of AKI in patients with preoperative use of RAS inhibitor. But they did not analyze the effect of RAS inhibitors on AKI severity, recovery and ensuing CKD [29].
Accordingly, the prediction model of CSA-AKI we developed in this study underlined the potential protective effect of RAS inhibitor. More risk reduction of AKI development was shown in patients with lower risk (Supplementary File 1). These results corresponded with recent meta-analysis that preoperative use of RAS inhibitor is associated with lower incidence of AKI as well as reinforced our confidence to continue use of RAS inhibitor in lower risk group because of its safety and benefit. Additionally, we also highlighted the concern of cautious use of RAS inhibitor in patients with high risk of CSA-AKI, because our prediction model showed only little benefit for high-risk groups. Our prediction model could help physicians to measure the individualized benefit of RAS inhibitor, and then make the decision of keeping its use or not.
On the other hand, our study did not show significant decrease of all-cause mortality and risk for dialysis in patients with preoperative use of RAS inhibitor. These findings could be explained partially by that the number of mortality and dialysis event in our study was not sufficient to reach appropriate statistical power. In addition, there were other more important risk factors for mortality such as emergent operation, cardiogenic shock, and surgery of aortic dissection or pulmonary embolectomy [30]. In regards to dialysis, other risk factors including CKD, severe CHF, and prolonged CPB could have more crucial effect than use of RAS inhibitor [31]. Despite the fact that the severity and recovery pattern of AKI is associated with ensuing CKD [19, 32], our results showed protective effect of RAS inhibitor only during the early follow-up period. The plausible reason is that long-term use after surgery is more important than preoperative use of RAS inhibitor on ensuing CKD development, because our previous study had revealed that use of RAS inhibitor in CSA-AKI patients after renal functional recovery is associated with lower risk of ensuing CKD development [7].
A few limitations of this study should be considered. First, although propensity score matching was performed in our prospective observational study, this might not eliminate residual unobserved confounding factors, as we could in a prospective RCT. Second, SCr was not obtained at the same time points after surgery between patients, which might fail to identify the early stage of AKI and the real peak SCr level. Third, we used a SCr and urine output–based criteria (the KDIGO criteria) for the diagnosis of AKI. SCr is an imperfect marker for AKI because volume of distribution and premorbid conditions such as age, gender, muscle mass, nutritional status, and medication affect the SCr and diagnosis of AKI [33]. However, KDIGO criteria provides a good platform to compare different studies for the diagnosis of AKI [9, 34]. Some novel biomarkers of AKI such as urinary or plasma NGAL and TIMP2-IGFBP7 may potentially refine the diagnosis and management of AKI and should be validated in the future study of CSA-AKI [35]. Because only novel biomarker could discriminate functional changes or structural renal damage.
In conclusion, our study shows that continued preoperative use of RAS inhibitor was associated with lower incidence, less severity, and higher recovery of CSA-AKI, especially in low-risk patients. The benefits of RAS inhibitor should be assessed individually including racial difference. A large RCT is needed to confirm our results and establish a well-validated prediction model or scoring system.
References
Mehta RL, Burdmann EA, Cerda J, Feehally J, Finkelstein F, Garcia-Garcia G, Godin M, Jha V, Lameire NH, Levin NW, Lewington A, Lombardi R, Macedo E, Rocco M, Aronoff-Spencer E, Tonelli M, Zhang J, Remuzzi G (2016) Recognition and management of acute kidney injury in the International Society of Nephrology 0by25 Global Snapshot: a multinational cross-sectional study. Lancet (London, England) 387(10032):2017–2025. https://doi.org/10.1016/s0140-6736(16)30240-9
Lafrance JP, Miller DR (2010) Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol JASN 21(2):345–352. https://doi.org/10.1681/asn.2009060636
Chou YH, Huang TM, Chu TS (2017) Novel insights into acute kidney injury-chronic kidney disease continuum and the role of renin–angiotensin system. J Formos Med Assoc 116(9):652–659. https://doi.org/10.1016/j.jfma.2017.04.026
Evans M, Carrero JJ, Szummer K, Akerblom A, Edfors R, Spaak J, Jacobson SH, Andell P, Lindhagen L, Jernberg T (2016) Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in myocardial infarction patients with renal dysfunction. J Am Coll Cardiol 67(14):1687–1697. https://doi.org/10.1016/j.jacc.2016.01.050
Cheng SY, Chou YH, Liao FL, Lin CC, Chang FC, Liu CH, Huang TM, Lai CF, Lin YF, Wu VC, Chu TS, Wu MS, Lin SL (2016) Losartan reduces ensuing chronic kidney disease and mortality after acute kidney injury. Sci Rep 6:34265. https://doi.org/10.1038/srep34265
Chou YH, Chu TS, Lin SL (2018) Role of renin–angiotensin system in acute kidney injury-chronic kidney disease transition. Nephrology (Carlton, Vic) 23(Suppl 4):121–125. https://doi.org/10.1111/nep.13467
Chou YH, Huang TM, Pan SY, Chang CH, Lai CF, Wu VC, Wu MS, Wu KD, Chu TS, Lin SL (2017) Renin–angiotensin system inhibitor is associated with lower risk of ensuing chronic kidney disease after functional recovery from acute kidney injury. Sci Rep 7:46518. https://doi.org/10.1038/srep46518
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294(7):813–818. https://doi.org/10.1001/jama.294.7.813
Wang Y, Bellomo R (2017) Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat Rev Nephrol 13(11):697–711. https://doi.org/10.1038/nrneph.2017.119
Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, Zarbock A (2017) Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med 43(11):1551–1561. https://doi.org/10.1007/s00134-016-4670-3
Palomba H, Castro I, Yu L, Burdmann EA (2017) The duration of acute kidney injury after cardiac surgery increases the risk of long-term chronic kidney disease. J Nephrol 30(4):567–572. https://doi.org/10.1007/s40620-016-0351-0
Yacoub R, Patel N, Lohr JW, Rajagopalan S, Nader N, Arora P (2013) Acute kidney injury and death associated with renin angiotensin system blockade in cardiothoracic surgery: a meta-analysis of observational studies. Am J Kidney Dis 62(6):1077–1086. https://doi.org/10.1053/j.ajkd.2013.04.018
Arora P, Rajagopalam S, Ranjan R, Kolli H, Singh M, Venuto R, Lohr J (2008) Preoperative use of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers is associated with increased risk for acute kidney injury after cardiovascular surgery. Clin J Am Soc Nephrol CJASN 3(5):1266–1273. https://doi.org/10.2215/cjn.05271107
Shi P, Li Z, Young N, Ji F, Wang Y, Moore P, Liu H (2013) The effects of preoperative renin–angiotensin system inhibitors on outcomes in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 27(4):703–709. https://doi.org/10.1053/j.jvca.2013.01.012
Cheungpasitporn W, Thongprayoon C, Srivali N, O’Corragain OA, Edmonds PJ, Ungprasert P, Kittanamongkolchai W, Erickson SB (2015) Preoperative renin–angiotensin system inhibitors use linked to reduced acute kidney injury: a systematic review and meta-analysis. Nephrol Dial Transplant 30(6):978–988. https://doi.org/10.1093/ndt/gfv023
Lai CF, Wu VC, Huang TM, Yeh YC, Wang KC, Han YY, Lin YF, Jhuang YJ, Chao CT, Shiao CC, Tsai PR, Hu FC, Chou NK, Ko WJ, Wu KD (2012) Kidney function decline after a non-dialysis-requiring acute kidney injury is associated with higher long-term mortality in critically ill survivors. Crit Care (London, England) 16(4):R123. https://doi.org/10.1186/cc11419
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470
Okusa MD, Davenport A (2014) Reading between the (guide)lines—the KDIGO practice guideline on acute kidney injury in the individual patient. Kidney Int 85(1):39–48. https://doi.org/10.1038/ki.2013.378
Heung M, Steffick DE, Zivin K, Gillespie BW, Banerjee T, Hsu CY, Powe NR, Pavkov ME, Williams DE, Saran R, Shahinian VB (2016) Acute kidney injury recovery pattern and subsequent risk of CKD: an analysis of veterans health administration data. Am J Kidney Dis 67(5):742–752. https://doi.org/10.1053/j.ajkd.2015.10.019
Austin PC (2014) The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 33(7):1242–1258. https://doi.org/10.1002/sim.5984
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Kontogiannis J, Burns KD (1998) Role of AT1 angiotensin II receptors in renal ischemic injury. Am J Physiol 274(1 Pt 2):F79–F90
Rodriguez-Romo R, Benitez K, Barrera-Chimal J, Perez-Villalva R, Gomez A, Aguilar-Leon D, Rangel-Santiago JF, Huerta S, Gamba G, Uribe N, Bobadilla NA (2016) AT1 receptor antagonism before ischemia prevents the transition of acute kidney injury to chronic kidney disease. Kidney Int 89(2):363–373. https://doi.org/10.1038/ki.2015.320
Kobori H, Nangaku M, Navar LG, Nishiyama A (2007) The intrarenal renin–angiotensin system: from physiology to the pathobiology of hypertension and kidney disease. Pharmacol Rev 59(3):251–287. https://doi.org/10.1124/pr.59.3.3
Radaelli G, Bodanese LC, Guaragna JC, Borges AP, Goldani MA, Petracco JB, Piccoli Jda C, Albuquerque LC (2011) The use of inhibitors of angiotensin-converting enzyme and its relation to events in the postoperative period of CABG. Revista brasileira de cirurgia cardiovascular 26(3):373–379
Coca SG, Garg AX, Swaminathan M, Garwood S, Hong K, Thiessen-Philbrook H, Passik C, Koyner JL, Parikh CR (2013) Preoperative angiotensin-converting enzyme inhibitors and angiotensin receptor blocker use and acute kidney injury in patients undergoing cardiac surgery. Nephrol Dial Transplant 28(11):2787–2799. https://doi.org/10.1093/ndt/gft405
Pretorius M, Murray KT, Yu C, Byrne JG, Billings FT, Petracek MR, Greelish JP, Hoff SJ, Ball SK, Mishra V, Body SC, Brown NJ (2012) Angiotensin-converting enzyme inhibition or mineralocorticoid receptor blockade do not affect prevalence of atrial fibrillation in patients undergoing cardiac surgery. Crit Care Med 40(10):2805–2812. https://doi.org/10.1097/ccm.0b013e31825b8be2
Cheng X, Tong J, Hu Q, Chen S, Yin Y, Liu Z (2015) Meta-analysis of the effects of preoperative renin–angiotensin system inhibitor therapy on major adverse cardiac events in patients undergoing cardiac surgery. Eur J Cardio Thorac Surg 47(6):958–966. https://doi.org/10.1093/ejcts/ezu330
Xu N, Long Q, He T, Liu X, Dai H, Lu Y, Wen J, Wu Q, Yuan H (2018) Association between preoperative renin–angiotensin system inhibitor use and postoperative acute kidney injury risk in patients with hypertension. Clin Nephrol 89(6):403–414. https://doi.org/10.5414/cn109319
Nilsson J, Ohlsson M, Thulin L, Hoglund P, Nashef SA, Brandt J (2006) Risk factor identification and mortality prediction in cardiac surgery using artificial neural networks. J Thorac Cardiovasc Surg 132(1):12–19. https://doi.org/10.1016/j.jtcvs.2005.12.055
Thiele RH, Isbell JM, Rosner MH (2015) AKI associated with cardiac surgery. Clin J Am Soc Nephrol CJASN 10(3):500–514. https://doi.org/10.2215/cjn.07830814
Kaballo MA, Elsayed ME, Stack AG (2017) Linking acute kidney injury to chronic kidney disease: the missing links. J Nephrol 30(4):461–475. https://doi.org/10.1007/s40620-016-0359-5
Edelstein CL (2008) Biomarkers of acute kidney injury. Adv Chronic Kidney Dis 15(3):222–234. https://doi.org/10.1053/j.ackd.2008.04.003
Nadim MK, Forni LG, Bihorac A, Hobson C, Koyner JL, Shaw A, Arnaoutakis GJ, Ding X, Engelman DT, Gasparovic H, Gasparovic V, Herzog CA, Kashani K, Katz N, Liu KD, Mehta RL, Ostermann M, Pannu N, Pickkers P, Price S, Ricci Z, Rich JB, Sajja LR, Weaver FA, Zarbock A, Ronco C, Kellum JA (2018) Cardiac and vascular surgery-associated acute kidney injury: the 20th international consensus conference of the ADQI (Acute Disease Quality Initiative) Group. J Am Heart Assoc. https://doi.org/10.1161/jaha.118.008834
Levante C, Ferrari F, Manenti C, Husain-Syed F, Scarpa M, Hinna Danesi T, De Cal M, Corradi V, Virzi GM, Brendolan A, Nalesso F, Bezerra P, Lopez-Giacoman S, Samoni S, Senzolo M, Giavarina D, Salvador L, Bonato R, De Rosa S, Rettore E, Ronco C (2017) Routine adoption of TIMP2 and IGFBP7 biomarkers in cardiac surgery for early identification of acute kidney injury. Int J Artif Organs 40(12):714–718. https://doi.org/10.5301/ijao.5000661
Acknowledgements
The authors acknowledge statistical assistance provided by the Center of Statistical Consultation and Research in the Department of Medical Research, NTUH.
Funding
Y.H.C. is supported by Ministry of Science and Technology, Taiwan (MOST, 107-2314-B-002 -020). S.L.L. is supported by MOST (105-2314-B-002-096-MY3, 107-2314-B-002-078), National Health Research Institutes (EX106-10633SI, EX107-10633SI, EX108-10633SI), NTUH (105-S2944, 106-S3357, 107-T02), and Taiwan Health Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chou, YH., Huang, TM., Wu, VC. et al. Associations between preoperative continuation of renin–angiotensin system inhibitor and cardiac surgery-associated acute kidney injury: a propensity score-matching analysis. J Nephrol 32, 957–966 (2019). https://doi.org/10.1007/s40620-019-00657-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-019-00657-4