Abstract
Purpose
To compare the response to denosumab (DMAb) therapy with that of oral bisphosphonate (BISPH) treatment in postmenopausal women with primary osteoporosis (PO).
Methods
In this retrospective study, we compared data of 75 PO female patients treated for 24 months with DMab (DMAb Group, age 72.6 ± 8.9 years) with those of 75 PO patients treated with oral bisphosphonates (BISPH Group), matched for age, body mass index, femoral bone mineral density (BMD), prevalent fragility fractures and familiar history of hip fracture. In all subjects at baseline and after 24 months we assessed the calcium–phosphorous metabolism parameters, BMD at lumbar spine (LS-BMD) and femoral neck (FN-BMD) by dual X-ray absorptiometry and the morphometric vertebral fractures by radiograph. The patients were considered inadequate responders in the presence of ≥ 2 incident fragility fractures and/or a decrease in BMD greater than the least significant change (LS 2.8%, FN 5.9%).
Results
After 24 months, the DMab Group showed a greater ALP decrease (− 22.8 ± 18.2%), a higher LS-BMD and FN-BMD increase (6.6 ± 6.9 and 4.4 ± 8.2%, respectively) and a lower number of patients with an incident fracture (8%) and with an inadequate response (6.7%) than BISPH Group (− 14.9 ± 15.3, 2.5 ± 4.3, 1.9 ± 4.5, 21.3 and 22.7%, respectively, p < 0.05 for all comparisons). The inadequate response was 4.5-fold more likely in BISPH Group than in DMab one (p = 0.027), regardless of possible confounders.
Conclusions
In postmenopausal PO females, denosumab was more effective than oral bisphosphonates in increasing BMD and reducing bone turnover and the number of inadequate responder patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ultimate goal of any treatment for osteoporosis is to reduce the risk of fracture. Nowadays, bisphosphonates and denosumab (DMab) have obtained the regulatory approval since randomized controlled trials (RCTs) have demonstrated their significant anti-fracture effect [1]. In postmenopausal women with osteoporosis, the oral bisphosphonates alendronate and risedronate have been demonstrated to reduce vertebral and non-vertebral fractures of about 50 and 20%, respectively [2, 3], and DMab has been shown to reduce new vertebral fractures by 68%, hip fractures by 40%, and non-vertebral fractures by 20% [4]. However, since the fracture risk reduction has been evaluated primarily in placebo-controlled trials, its entity has been largely influenced by the risk profile of the control individuals. On the other hand, head-to-head comparison studies among the various bisphosphonates or between bisphosphonates and DMab are scarce [5]. Overall, some data suggest that the DMab efficacy in reducing fractures is not significantly different from that of bisphosphonates, even though DMab is more effective in increasing bone mineral density (BMD) [6,7,8,9]. However, since most information regarding a possible different efficacy of Dmab as compared with bisphosphonates is obtained from meta-analysis studies or from short-term ones (i.e. less than 24 months), some authors suggest that in a clinical setting DMab may demonstrate greater effectiveness than bisphosphonates [6].
Another important lack of knowledge is about the efficacy of DMab in a “real-life” setting. Indeed, the enrolment criteria used in RCTs are very different from the reimbursement criteria used for treating patients in the daily clinical practice and this may influence the final efficacy of a bone-active drug that could be lower than expected on the basis of the placebo-controlled randomized clinical trials [10].
On the basis of these considerations, the present study was aimed to compare the overall response to a 24-month DMAb therapy with that to a 24-month oral bisphosphonate treatment in female patients with primary osteoporosis (PO).
Patients and methods
Patients
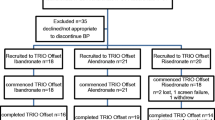
In this observational retrospective study, we evaluated data of all (n = 177) female Caucasian patients with PO referred to our out-patient Clinic for Metabolic Bone Diseases since June 2013 to June 2017, who had been treated with DMab (60 mg subcutaneously every 6 months) for at least 24 months. The PO was diagnosed after the possible causes of secondary osteoporosis had been excluded by the appropriate analyses, as per our protocols that have been described elsewhere [11]. The PO patients were included in the study if they fulfilled the following criteria: (i) a BMD T score below − 4.0 and/or prevalent vertebral and/or hip fragility fractures, or a BMD T score below − 3.0 together with a familiar history of vertebral or hip fragility fracture (as recommended by the Italian National Health Service); (ii) absence of other diseases or conditions known to affect bone metabolism (i.e. menopause before 45 years, thyrotoxicosis, gastrointestinal disorders, chronic renal failure, chronic hepatic disease, depression, alcoholism, obesity, eating disorders, rheumatological or haematological diseases, hypercortisolism, diabetes). We excluded all subjects reporting: (i) intake of drugs influencing bone metabolism (i.e. alendronate, risedronate, ibandronate, cinacalcet, glucocorticoids, teriparatide, thiazide diuretics, hormonal adjuvant therapy, selective serotonin reuptake inhibitors) in the past 2 years and/or for more than 5 years and/or present or past therapy with neridronate or zoledronate; (ii) less than 100% adherence to DMab therapy.
Eventually, 75 patients with PO treated with DMab (DMab Group, age 72.6 ± 8.9 years) fulfilled the inclusion and exclusion criteria and were enrolled in the study. In DMab Group, 42 patients have never received any anti-osteoporotic therapy. In these latter subjects the DMab therapy was given because patients refused a bisphosphonate therapy for fear of upper gastrointestinal adverse effects.
We also retrospectively evaluated data of all (n = 223) female Caucasian patients, referred to our out-patient Clinic for Metabolic Bone Diseases since June 2013 to June 2017 for PO, who had been treated for at least 24 months with oral bisphosphonates (risedronate 35 mg/weekly or alendronate 70 mg/weekly), if they fulfilled the same inclusion and exclusion criteria used for PO patients treated with DMab (for bisphosphonates a > 80% adherence to bisphosphonate therapy was requested for study inclusion). Subsequently, among the 134 patients treated with bisphosphonates, who were eligible for study inclusion, we chose 75 subjects (BISPH Group, 12 patients treated with alendronate and 63 patients treated with risedronate) matched at 1:1 ratio with patients of the DMab Group considering the following variables: age, body mass index (BMI), familiar history of hip fracture, femoral neck BMD and personal history of vertebral and/or hip fragility fractures. In BISPH Group 56 patients have never been previously treated with bone-active drugs.
As per our protocols, to normalize vitamin D (25OHVitD) levels, all patients with 25OHVitD concentration below 30 ng/mL received cholecalciferol supplementation. An oral bolus of cholecalciferol was administered in patients on the basis of baseline 25OHVitD levels: in patients with baseline 25OHVitD levels between 10 and 30 ng/mL a single oral bolus of 100,000 IU cholecalciferol was administered, while in patients with baseline 25OHVitD levels below 10 ng/mL a single oral bolus of 300,000 IU cholecalciferol was administered. Subsequently, in all patients a cholecalciferol supplementation of 50,000 IU monthly plus 400 IU daily was given [12]. In patients with a calcium intake < 1000 mg/day also an oral calcium citrate supplementation (500 mg/day or 1000 mg/day in patients with an estimated calcium intake above or below 500 mg/day, respectively) was prescribed [13, 14]. Subjects were considered current smokers if they smoked ≥ 5 cigarettes/day and/or ≥ 10 packs/year [15]. An informed consent was obtained from each patient.
Methods
We collected baseline data regarding years since menopause and familiar history of vertebral and/or hip fragility fractures at baseline and at the end of the follow-up data regarding the presence of clinical fragility fractures, weight, height, BMI and comorbidities (i.e. hypertension and dyslipidemia).
In all subjects, the following data were reported at the beginning and at the end of the follow-up: serum calcium, creatinine, alkaline phosphatase total activity (ALP), 25OHVitD. Total calcium was corrected for serum albumin according to the formula: (total calcium + (4.4 – albumin mg/dl) × 0.8) (reference interval 8.4–10.4 g/dl) [16]. Calcium, albumin, and creatinine in serum and urinary calcium and creatinine were measured by standard colorimetric techniques. Serum 25OHVitD concentration was measured by chemiluminescent immunoassay (Diasorin, reference interval: 30–100 ng/mL). Serum ALP was measured by standard colorimetric techniques (Roche Diagnostics, reference interval: 35–140 U/L, CV 12%). The difference of ALP levels between end of follow-up and baseline was expressed as percentage of baseline values. The ALP decrease was considered significant if it was greater than the least significant change (LSC), calculated by the formula 2.8 × precision error (i.e. − 22%) [17]. Serum intact PTH was measured by electrochemiluminescence immunoassay (Siemens Immulite 2000/2000 Xpi Systems Intact PTH, reference interval = 12–65 pg/mL) in 59 and 68 subjects from DMab Group and BISPH Group, respectively.
In all patients, at the beginning and at the end of the 24-month follow-up, BMD was measured by dual X-ray absorptiometry (Hologic Discovery, Software version 13.3:3, Bedford MA, USA), and expressed as Z score, at lumbar (L1–L4) spine (LS, Z-LS, in vivo precision 1.0%) and femoral neck (FN, Z-FN, in vivo precision 1.8%). The BMD change between end of follow-up (Δ) and baseline at LS and FN was expressed as percentage of baseline values (as g/cm2, ΔLS and ΔFN, respectively) and it was considered significant if above the LSC (LS 2.8%, FN 5.9%). At the same intervals, a conventional spinal radiograph in lateral and anteroposterior projection (T4–L4) was obtained in all subjects with standardized technique. Two trained physicians, who were blinded to BMD and biochemical data, independently reviewed the radiographs, and they discussed questionable cases to agree on a diagnosis. Vertebral fractures were diagnosed on visual inspection using the semiquantitative visual assessment (SQ) previously described by Genant and colleagues [18] and fractures assessed on lateral thoracolumbar spine radiographs were defined in the presence of a > 20% reduction in anterior, middle, or posterior vertebral height: 13 vertebrae (from T4 to L4) were evaluated visually and classified as intact (SQ grade 0) or as having mild (20 to 25% compression), moderate (25–40% compression), or severe (> 40% compression) deformity (SQ grades 1, 2, and 3, respectively). Subsequently, for each subject, the spinal deformity index (SDI) was calculated by summing the SQ grade for each vertebra (SDI = SQT4 + ⋯ + SQT12 + SQL1 + ⋯ +SQL4) [19]. According to the working group of the International Osteoporosis Foundation (IOF), patients were classified as inadequate responders in the presence of two or more incident fragility fractures and/or a decrease in BMD greater than the LSC [20]. A good response to the DMab or BISPH therapy was arbitrarily defined in the presence of an increase in BMD at any site greater than the LSC in the absence of both a decrease in BMD greater than LSC at any site and an incident fragility fracture.
Statistical analysis
Hypothesizing a difference in mean LS BMD variation of 2.0% between patients treated with DMab and those treated with bisphosphonates (with a 4.5% standard deviation), we needed to recruit 69 experimental subjects and 69 control subjects (90% power and I Type Error 5%) to obtain an adequate power of the study.
Statistical analysis was performed by SPSS version 21.0 statistical package (SPSS Inc, Chicago, IL). The results are expressed as mean ± SD, unless differently specified. Categorical variables were compared by χ2 test or Fisher’s exact test, as appropriate. Comparison of continuous variables among the different groups was performed using Student’s t test or Mann–Whitney U test, as appropriate.
Bivariate associations were tested by either Pearson product moment correlation or Spearman correlation, as appropriate.
In the whole group of subjects, the logistic regression analysis assessed the association between the presence of an inadequate or a good response to the therapies and the use of DMab or oral bisphosphonates, after adjusting for other possible confounding factors, such as age, BMI, familial history of hip fractures, basal Z-LS and SDI, previous use of bisphosphonates, occurrence of falls, and smoking habit.
p values of less than 0.05 were considered significant.
Results
The comparison of the biochemical and clinical characteristics between DMAb Group and BISPH Group at baseline and at the end of the follow-up is reported in Table 1.
At baseline DMab patients and BISPH patients were comparable as far as age, BMI, years since menopause, familiar history of fragility fracture, prevalence of current smokers, hypertension and dyslipidemia, SDI, serum calcium, PTH, ALP and 25OHVitD levels, the percentage of subjects with vitamin D deficiency, with 25OHVitD levels below 10 ng/mL or between 10 and 30 ng/mL and LS and FN-BMD (expressed as both T score and Z score) was concerned. At variance, the prevalence of subjects who had previously assumed an oral bisphosphonate therapy (lasted for less than 5 years and ended at least 2 years before the baseline as per exclusion criteria) was higher in DMab patients than in BISPH ones (44 and 25.3%, respectively, p = 0.04). The mean duration of previous bisphosphonate therapy and the prevalence of inadequate responders to bisphosphonate therapy was not different between DMab patients (45.2 ± 18.6 months and 35.8%) and BISPH ones (50.3 ± 11.1 months and 42.5%, p = 0.15 and p = 0.528, respectively). All subjects had at least a prevalent fragility fracture at baseline.
The number of current smokers, hypertensive and dyslipidemic patients did not vary between the baseline and the end of follow-up in both DMab and BISPH Groups. In the DMab Group but not in BISPH Group, BMD at both LS and FN increased significantly from baseline to the end of follow-up (Fig. 1). In both groups, PTH and SDI did not vary significantly, calcium levels decreased and 25OHVitD levels increased significantly during the 24-month study period. In BISPH Group the number of patients who experienced at least one fall was higher than in DMab Group.
Bone mineral density changes before and after 24 months of denosumab or oral bisphosphonates therapy in postmenopausal women with primary osteoporosis. Z-LS and Z-FN bone mineral density expressed as mean Z score at spine (L1–L4) and femoral neck, respectively; DMab denosumab (n = 75 patients); BISPH oral bisphosphonates (n = 75 patients; alendronate n = 12, risedronate n = 63). In the DMab patients but not in BISPH ones the mean Z-LS and Z-FN values increased significantly from baseline to the end of follow-up (24 months). At the end of the follow-up the Z-LS was significantly higher in DMab Group than in BISPH Group
At the end of the follow-up the LS BMD (expressed as both T score and Z score) was significantly higher in DMab Group than in BISPH Group (Fig. 1), while SDI, serum calcium, PTH, ALP and 25OHVitD levels, the percentage of subjects with vitamin D deficiency, with 25OHVitD levels below 10 ng/mL or between 10 and 30 ng/mL and Z-FN were comparable between the two groups. As shown in Table 1, in both DMAb patients and BISPH ones the percentage of patients with vitamin D deficiency and of patients with 25OHVitD levels between 10 and 30 ng/mL significantly decreased while the percentage of patients with 25OHVitD levels above 30 ng/mL significantly increased between baseline and end of follow-up. At the end of follow-up only three patients in DMab Group and no one in BISPH Group showed 25OHVitD levels below 20 ng/mL. Importantly, in the DMab Group the mean ΔLS and ΔFN were higher and the mean percentage ALP decrease was significantly greater as compared with BISPH Group. Furthermore, the mean percentage ALP change was negatively associated with the ΔLS and ΔFN (r = − 0.27, p = 0.001 and r = − 0.19, p = 0.018, respectively). The number of patients with at least an incident fracture (in more than 80% of cases at vertebrae) and the prevalence of inadequate responders to the therapy were lower in DMab Group than in BISPH one. In the DMab Group, four patients had incident vertebral fragility fractures and, specifically, two patients had two grade 2 clinical vertebral fractures, one patient had one grade 2 and one grade 3 clinical vertebral fractures and one patient had two grade 1 morphometric vertebral fractures. In the BISPH Group, four patients had 1 morphometric grade 1 vertebral fracture, three patients had two morphometric grade 1 vertebral fractures, two patients had one clinical grade 2 vertebral fracture, one patient had two grade 2 clinical vertebral fractures, two patients had one grade 1 and one grade 2 clinical vertebral fractures and three patients had one grade 1 and two grade 2 clinical vertebral fragility fractures.
The number of patients with a significant ALP decrease and the number of good responders to the therapy were higher in DMab Group than in BISPH one. In this latter group, the percentage change of ALP levels between the beginning and the end of the study was not significantly different between the 12 patients treated with alendronate (ΔALP − 13.9 ± 8.7%) and the 63 patients treated with risedronate (ΔALP − 15.1 ± 16.3%, p = 0.806).
The comparison of the biochemical and clinical characteristics between the inadequate responder patients and the adequate responder ones in the whole sample of subjects is reported in Table 2. The DMab inadequate responders (n = 5) and the BISPH inadequate responders (n = 15) were not different as far as clinical (1/5, 20% and 4/15, 26.7%, respectively) and morphometric (2/5, 40% and 6/15, 40%, respectively) vertebral fractures are considered. No patient had an incident non-vertebral and/or non-femoral fracture in both DMAb and BISPH inadequate responder groups. In patients with an inadequate response to the therapies there was a higher prevalence of smokers than in patients with an adequate response to therapies, while all the other clinical and biochemical characteristics were comparable (Table 2). In particular, among the patients with an inadequate response, PTH levels were not significantly different between Dmab patients (44.8 ± 5.3 pg/mL, data available in 4 out of 5 inadequate responders) and BISPH ones (42.5 ± 6.9 pg/mL, data available in 14 out of 17 inadequate responders, p = 0.556). In the whole group of patients the inadequate response to the therapies was 4.5-fold more probable with use of the oral bisphosphonates than with the use of DMab regardless of age, BMI, SDI and Z-LS at baseline, previous use of bisphosphonates, occurrence of falls, and smoking habit (Table 3).
Finally, in the whole group of patients, subjects with a good response to the therapies (n = 96) showed a greater ALP decrease (− 22.5 ± 15.8%) than the remaining patients with an adequate or inadequate response to therapies (n = 54, − 12.5 ± 18%, p < 0.01), while all the other clinical and biochemical characteristics were comparable (data not shown). In the whole group of patients the good response to the therapies was associated with the use of DMab (odds ratio 2.25, 95% confidence interval 1.04–4.85, p = 0.037) and with the degree of the percentage ALP decrease (odds ratio 1.04, 95% confidence interval 1.01–1.06, p = 0.004) regardless of age, BMI, SDI and Z-LS at baseline, previous use of bisphosphonates, and smoking habit.
No patient included in the DMab Group experienced any adverse effect during the study period. Among patients included in the BISPH Group, five subjects (6.7%) experienced modest flu-like symptoms during the first month of treatment and six patients (8%) complained with slight adverse upper gastrointestinal effects during the initial period (4–6 weeks) of therapy. In no cases the treatments had to be withdrawn.
Discussion
To the best of our knowledge this is the first 24-month study comparing the effect of DMab therapy with that of oral bisphosphonates in a “real-life” setting in postmenopausal women with PO. The present data suggest that in female PO patients DMab increases BMD and reduces the risk of fracture and of inadequate responses more than oral bisphosphonates, independently of the baseline fracture risk profile.
These findings may be considered somewhat expected since some data derived from meta-analysis studies suggested a possible stronger effect of DMab in respect of alendronate or risedronate in reducing the vertebral but not the hip fracture risk in postmenopausal women with PO [5,6,7,8,9, 21]. However, the few available head-to-head studies were short-term ones (i.e. 12 months) and focused only on bone turnover and BMD, while a stronger anti-fracture effect of DMab in respect of oral bisphosphonates has been suggested mainly by meta-analyses of placebo-controlled RCTs rather than by head-to-head comparison studies. In fact, in a 12-month randomized controlled head-to-head trial on 1703 postmenopausal women, transitioning to DMab was more effective in increasing BMD and reducing bone turnover than cycling to a monthly oral BISPH treatment (ibandronate or risedronate) in subjects with persistent high fracture risk despite suboptimal BISPH treatment [7]. In keeping, a subsequent 12-month randomized controlled head-to-head trial in 870 postmenopausal women, who were sub-optimally adherent to alendronate therapy, transitioning to DMab was more effective than risedronate in increasing BMD and reducing bone turnover [8]. In both studies, however, the fracture risk was not evaluated. Overall, the results of our head-to-head study are in keeping with the previous ones and suggest for the first time that the stronger effect of DMab on BMD and bone turnover, as compared with oral bisphosphonates, is associated also with a significantly greater reduction of fragility fractures.
Interestingly, in the present study, the incidence of fragility fractures and the increase of LS-BMD were similar to those of the FREEDOM study (8 vs 8.8% and 6.6 vs 6.4%, respectively) [4], even though the inclusion criteria of the FREEDOM study were different from the present ones, which are mandatory in Italy for the anti-osteoporotic drugs reimbursement. Thus, the present study also suggests that the DMab efficacy demonstrated in the FREEDOM trial is present also in a “real-life” setting. On the other hand, notwithstanding the strong efficacy of DMab in postmenopausal women with PO, about 7% of subjects treated with DMab and about 23% of patients treated with oral bisphosphonates may be inadequate responders on the basis of the IOF definition [20]. To the best of our knowledge, no data were available so far regarding the prevalence of inadequate responders in osteoporotic postmenopausal women treated with DMab, while in postmenopausal patients treated with bisphosphonates the prevalence of inadequate responders has been described to be up to 42.5%. The reduced prevalence of inadequate responders in patients treated with oral bisphosphonates in the present study (about 23%) is in keeping with previous data of our Group [10] and may be ascribed to the careful exclusion of patients with secondary osteoporosis, to the adequate vitamin D supplementation and to the optimal adherence to the therapy, this latter being probably more easily reachable with DMab than with bisphosphonates [22, 23].
On the other hand, we found that the 74.7 and 53.3% of patients treated with DMab and oral bisphosphonates were good responders. In addition, the percentage BMD increase was associated with the entity of the bone turnover reduction as mirrored by the percentage decrease of ALP levels. This is in keeping with the well-known idea that the reduction of bone turnover is among the main mechanisms responsible for the BMD increase with anti-resorptives [24,25,26,27,28]. However, as a bone turnover marker ALP reflects bone apposition more than bone resorption and more specific markers (such as the C-terminal telopeptide of type I collagen, CTX) for investigating bone resorption are available. Therefore, even though the reduction of ALP levels in DMab-treated group may indicate the important effect of this drug on bone, the possibility of predicting the DMab effect on BMD by measuring ALP levels is still to be demonstrated.
The present study has other limitations. First, its retrospective and not randomized design may have introduced unknown biases and it may be inadequate to evaluate the efficacy of both compared treatment groups. However, the precise matching between DMab patients and BISPH ones consented us to evenly reduce the risk of biases related to the individual fracture risk profile at baseline. Second, the small sample size did not consent to individuate the factors predictive of an inadequate response to DMab or to oral bisphosphonates. Third, we did not measure more sensitive bone apposition markers and/or bone resorption indexes, which could have been more informative [17]. Furthermore, the ALP levels were assessed only after 24 months therapy and concomitantly with BMD evaluation, being, thus, not usable as early predictors of the treatment efficacy [17, 29].
Notwithstanding these limitations, the present study suggests that in postmenopausal women with PO, DMab is more effective than oral bisphosphonates in increasing BMD and reducing bone turnover and incident fractures, therefore, leading to a reduced number of inadequate responses.
References
Khosla S, Hofbauer LC (2017) Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol. https://doi.org/10.1016/s2213-8587(17)30188-2 (epub ahead of print)
Bilezikian JP (2009) Efficacy of bisphosphonates in reducing fracture risk in postmenopausal osteoporosis. Am J Med 22:S14–S21. https://doi.org/10.1016/j.amjmed.2008.12.003
Maraka S, Kennel KA (2015) Bisphosphonates for the prevention and treatment of osteoporosis. BMJ 351:h3783. https://doi.org/10.1136/bmj.h3783
Papapoulos S, Lippuner K, Roux C et al (2015) The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM Extension study. Osteoporos Int 26:2773–2783. https://doi.org/10.1007/s00198-015-3234-7
Freemantle N, Cooper C, Diez-Perez A, Gitlin M, Radcliffe H, Shepherd S, Roux C (2013) Results of indirect and mixed treatment comparison of fracture efficacy for osteoporosis treatments: a meta-analysis. Osteoporos Int 24:209–217. https://doi.org/10.1007/s00198-012-2068-9
Beaudoin C, Jean S, Bessette L, Ste-Marie L-G, Moore L, Brown JP (2016) Denosumab compared to other treatments to prevent or treat osteoporosis in individuals at risk of fracture: a systematic review and meta-analysis. Osteoporos Int 27:2835–2844. https://doi.org/10.1007/s00198-016-3607-6
Brown JP, Roux C, Ho PR, Bolognese MA, Hall J, Bone HG, Bonnick S, van den Bergh JP, Ferreira I, Dakin P, Wagman RB, Recknor C (2014) Denosumab significantly increases bone mineral density and reduces bone turnover compared with monthly oral ibandronate and risedronate in postmenopausal women who remained at higher risk for fracture despite previous suboptimal treatment with an oral bisphosphonate. Osteoporos Int 25:1953–1961. https://doi.org/10.1007/s00198-014-2692-7
Roux C, Hofbauer LC, Ho PR, Wark JD, Zillikens MC, Fahrleitner-Pammer A, Hawkins F, Micaelo M, Minisola S, Papaioannou N, Stone M, Ferreira I, Siddhanti S, Wagman RB, Brown JP (2014) Denosumab compared with risedronate in postmenopausal women suboptimally adherent to alendronate therapy: efficacy and safety results from a randomized open-label study. Bone 58:48–54. https://doi.org/10.1016/j.bone.2013.10.006
Augoulea A, Tsakonas E, Triantafyllopoulos I, Rizos D, Armeni E, Tsoltos N, Tournis S, Deligeoroglou E, Antoniou A, Lambrinoudaki I (2017) Comparative effects of denosumab or bisphosphonate treatment on bone mineral density and calcium metabolism in postmenopausal women. J Musculoskelet Neuronal Interact 1(17):444–449 (PMID: 28250248)
Cairoli E, Eller-Vainicher C, Ulivieri FM, Zhukouskaya VV, Palmieri S, Morelli V, Beck-Peccoz P, Chiodini I (2014) Factors associated with bisphosphonate treatment failure in postmenopausal women with primary osteoporosis. Osteoporos Int 25:1401–1410. https://doi.org/10.1007/s00198-014-2619-3
Eller-Vainicher C, Cairoli E, Zhukouskaya VV, Morelli V, Palmieri S, Scillitani A, Beck-Peccoz P, Chiodini I (2013) Prevalence of subclinical contributors to low bone mineral density and/or fragility fractures. Eur J Endocrinol 169:225–237. https://doi.org/10.1530/EJE-13-0102
Adami S, Romagnoli E, Carnevale V, Scillitani A, Giusti A, Rossini M, Gatti D, Nuti R, Minisola S, Italian Society for Osteoporosis, Mineral Metabolism and Bone Diseases (SIOMMMS) (2011) Guidelines on prevention and treatment of vitamin D deficiency. Reumatismo 63:129–147. https://doi.org/10.4081/reumatismo.2011.129
Rossini M, Adami S, Bertoldo F, Diacinti D, Gatti D, Giannini S, Giusti A, Malavolta N, Minisola S, Osella G, Pedrazzoni M, Sinigaglia L, Viapiana O, Isaia GC (2016) Guidelines for the diagnosis, prevention and management of osteoporosis. Reumatismo 68:1–39. https://doi.org/10.4081/reumatismo.2016.870
Varenna M, Binelli L, Zucchi F, Ghiringhelli D, Sinigaglia L (2001) Unbalanced diet to lower serum cholesterol level is a risk factor for postmenopausal osteoporosis and distal forearm fracture. Osteoporos Int 12:296–301. https://doi.org/10.1007/s001980170119
Husten CG (2009) How should we define light or intermittent smoking? Does it matter? Nicotine Tob Res 11:111–121. https://doi.org/10.1093/ntr/ntp010
UpToDate calculator (2010) In Calcium Correction in Hypoalbuminemia, version 18.2. Wolters Kluwer-Health: Waltham. www.uptodate.com. Accessed 2 Sep 2009
Naylor K, Eastell R (2012) Bone turnover markers: use in osteoporosis. Nat Rev Rheumatol 8:379–389. https://doi.org/10.1038/nrrheum.2012.86
Genant HK, Wu CY, van Knijk C, Nevitt M (1993) Vertebral fracture assessment using a semi-quantitative technique. J Bone Mineral Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Crans GG, Genant HK, Krege JH (2005) Prognostic utility of a semiquantitative spinal deformity index. Bone 37:175–179. https://doi.org/10.1016/j.bone.2005.04.003
Diez-Perez A, Adachi JD, Agnusdei D, Bilezikian JP, Compston JE, Cummings SR, Eastell R, Eriksen EF, Gonzalez-Macias J, Liberman UA, Wahl DA, Seeman E, Kanis JA, Cooper C, IOF CSA Inadequate Responders Working Group (2012) Treatment failure in osteoporosis. Osteoporos Int 23:2769–2777. https://doi.org/10.1007/s00198-012-2093-8
Albert SG, Reddy S (2017) Clinical evaluation of cost efficacy of drugs for treatment of osteoporosis: a meta-analysis. Endocr Pract 23:841–856. https://doi.org/10.4158/EP161678.RA
Migliaccio S, Francomano D, Romagnoli E, Marocco C, Fornari R, Resmini G, Buffa A, Di Pietro G, Corvaglia S, Gimigliano F, Moretti A, de Sire A, Malavolta N, Lenzi A, Greco EA, Iolascon G (2017) Persistence with denosumab therapy in women affected by osteoporosis with fragility fractures: a multicenter observational real practice study in Italy. J Endocrinol Invest. https://doi.org/10.1007/s40618-017-0701-3 (epub ahead of print)
Cairoli E, Eller-Vainicher C, Chiodini I (2015) Update on denosumab in the management of postmenopausal osteoporosis: patient preference and adherence. Int J Womens Health 7:833–899. https://doi.org/10.2147/IJWH.S7568
Díez-Pérez A, Olmos JM, Nogués X, Sosa M, Díaz-Curiel M, Pérez-Castrillón JL, Pérez-Cano R, Muñoz-Torres M, Torrijos A, Jodar E, Del Rio L, Caeiro-Rey JR, Farrerons J, Vila J, Arnaud C, González-Macías J (2012) Risk factors for prediction of inadequate response to antiresorptives. J Bone Miner Res 27:817–824. https://doi.org/10.1002/jbmr.1496
Gennari L, Rotatori S, Bianciardi S, Nuti R, Merlotti D (2016) Treatment needs and current options for postmenopausal osteoporosis. Expert Opin Pharmacother 17:1141–1152. https://doi.org/10.1080/14656566.2016.1176147
Ishtiaq S, Fogelman I, Hampson G (2015) Treatment of post-menopausal osteoporosis: beyond bisphosphonates. J Endocrinol Invest 38:13–29. https://doi.org/10.1007/s40618-014-0152-z
Vescini F, Attanasio R, Balestrieri A, Bandeira F, Bonadonna S, Camozzi V, Cassibba S, Cesareo R, Chiodini I, Francucci CM, Gianotti L, Grimaldi F, Guglielmi R, Madeo B, Marcocci C, Palermo A, Scillitani A, Vignali E, Rochira V, Zini M (2016) Italian association of clinical endocrinologists (AME) position statement: drug therapy of osteoporosis. J Endocrinol Invest 39:807–834. https://doi.org/10.1007/s40618-016-0434-8
Adler RA (2016) Osteoporosis treatment: complexities and challenges. J Endocrinol Invest 39:719–720. https://doi.org/10.1007/s40618-016-0437-5
Wanby P, Nobin R, Von SP, Brudin L, Carlsson M (2016) Serum levels of the bone turnover markers dickkopf-1, sclerostin, osteoprotegerin, osteopontin, osteocalcin and 25-hydroxyvitamin D in Swedish geriatric patients aged 75 years or older with a fresh hip fracture and in healthy controls. J Endocrinol Invest 39:855–863. https://doi.org/10.1007/s40618-015-0421-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
An informed consent was obtained from each patient.
Rights and permissions
About this article
Cite this article
Cairoli, E., Palmieri, S., Goggi, G. et al. Denosumab or oral bisphosphonates in primary osteoporosis: a “real-life” study. J Endocrinol Invest 41, 1005–1013 (2018). https://doi.org/10.1007/s40618-018-0829-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0829-9