Abstract
Objectives
The aim of this study is to explore incidence and incidence-based mortality trends for endometrial cancer in the USA and project future incident cases, accounting for differences by race and histological subtype.
Methods
Data on age-adjusted and age-specific incidence and mortality rates of endometrial cancer were obtained from the Surveillance, Epidemiology, and End Results 18 registries. Trends in rates were analyzed using Joinpoint regression, and average annual percent change (AAPC) in recent years (2006–2011) was computed for histological subtypes by race. Age, histological, and race-specific rates were applied to US Census Bureau population census estimates to project new cases from 2015 to 2040, accounting for observed AAPC trends, which were progressively attenuated for the future years.
Results
The annual number of cases is projected to increase substantially from 2015 to 2040 across all racial groups. Considerable variation in incidence and mortality trends was observed both between and within racial groups when considering histology.
Conclusions
As the US population undergoes demographic changes, incidence of endometrial cancer is projected to rise. The increase will occur in all racial groups, but larger increases will be seen in aggressive histology subtypes that disproportionately affect black women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
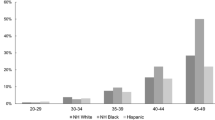
Despite declining overall cancer incidence and mortality rates, the incidence of endometrial cancer is rising. From 2008 to 2012, endometrial cancer incidence increased by 21 % [1]. In 2015, it is predicted to be the fourth most frequently diagnosed cancer in women, behind only breast, lung, and colorectal cancers [2]. Endometrial cancer is the most common gynecological cancer, and women in the USA have a 2.8 % lifetime risk of developing this disease [3, 4]. Incidence rates increase substantially with age (6.2 cases per 100,000 women less than 50 years of age and 83.3 cases per 100,000 women aged 50 or older) [4]. It is estimated that 54,870 new endometrial cancer cases and 10,170 deaths occurred in 2015 in the USA [2]. Endometrial cancer incidence is highest in white women, with black women experiencing a 30 % lower incidence [5]. Some debate surrounds this comparison, and a recent study illustrated that once the higher rate of hysterectomy among black women is taken into consideration, the incidence of endometrial cancer is relatively even between the two groups [6]. Additionally, the latest data from the Surveillance, Epidemiology, and End Results (SEER) Program reported near equal age-adjusted incidence rates for both races in 2012 (28.2 per 100,000 for white women and 25.4 per 100,000 for black women) [4]. However, the mortality rate among black women is 80 % higher than white women [7]. The five-year relative survival rate for white women is 85.3 %, while for black women it is only 65.6 % [4]. This lower survival rate has been extensively reported [8], and the literature suggests a multidimensional etiology behind this inequity. Potential causes are the incidence of more aggressive histological tumor subtypes in black women, diagnosis at later stages, less access to and unequal treatment within the health care system, and higher comorbidity rates [5, 7]. There is thus a need to project future number of cases per year by race and histological subtype in order to quantify the disparity and gauge the potential impact of prevention and control interventions.
The majority of endometrial cancers can be categorized into five frequent histological subtypes: endometrioid, serous, mixed (usually endometrioid and serous components), clear-cell, and malignant mixed Mullerian tumors (MMMT). The remaining rare subtypes are classified as “other.” Endometrioid is the most common histology, representing about 75 % of endometrial cancers, followed by serous (1–5 %) and clear cell (1–5 %) [9]. Though the endometrioid subtype can be low grade or high grade, the other histologies, especially serous and clear cell, are characteristically high in grade with a worse prognosis [1, 7]. One recent review found that black women consistently have a higher incidence of aggressive, non-endometrioid tumors when compared to their white counterparts [5].
As the US population ages and minority populations increase, the incidence of endometrial cancer is expected to rise [10]. It has been projected that the number of annual incident cases in the USA will increase from 52,000 in 2010 to 122,000 in 2030, reflecting these demographic changes [11]. Additionally, Sheikh et al. project the 2030 incidence rate of endometrial cancer at 42 cases per 100,000, representing a 55 % increase from 2010 [12]. Although reasonable, these estimates were not broken down by race or histological subtype, nor do they include the difference in average annual percent change (AAPC) that exists between race and histology-specific cancer incidence rates. Thus, there is a need for more tailored projections accounting for these factors. Here, we analyze trends of endometrial cancer by race and histology and use these to project the number of new cases from endometrial cancer annually by race and histological subtype from 2015 to 2040.
Methods
We obtained data on endometrial cancer (corpus uteri and uterus, NOS) incidence and incidence-based mortality in the US during 2000–2011 from the SEER 18 registries [13]. SEER is a population-based registry that covers 28 % of the US population. The SEER*Stat software was employed to calculate age-specific and age-adjusted incidence and mortality rates from years 2000–2011 by race and histological subtype [14]. Adjusted rates were adjusted to the 2000 US standard population. Three race and ethnicity groups were considered: non-Hispanic white women (NHWW), Hispanic white women (HWW), and non-Hispanic black women (NHBW). Other groups were excluded due to a small sample size. Histological types were defined using the International Classification of Disease for Oncology, Third Edition (ICD-O3) [15]. Endometrial cancer included site codes: C54.0-C54.3, C54.8-C54.9, and C55.9. Histological types were defined as endometrioid (8050, 8140, 8143, 8210–8211, 8260–8263, 8340, 8340, 8380–8384, 8560, 8570), serous (8441, 8460–8461), mixed (8255, 8323), clear cell (8310), MMMT or carcinosarcoma (8950–8951, 8980–8981), and other (8000,8010, 8013, 8020, 8041, 8045–8046, 8574). Endometrioid histology was additionally divided into low grade (well and moderately differentiated) and high grade (poorly differentiated or undifferentiated). Research has supported this distinction clinically and epidemiologically, as high-grade endometrioid cancers have a prognosis more similar to serous and clear-cell histologies [9, 16].
Projected population estimates for the USA from 2015 to 2040 were obtained through the US Census Bureau [17]. The census data contained the number of individuals in each year of age from 0 to over 100 for each ancestral-origin group. Since SEER age-specific incidence and mortality rates are for age groups from 0 to 85+, the last census group was correspondingly made 85+.
Trend Analyses
The Joinpoint software was used to conduct trend analyses of age-adjusted incidence and mortality rates [18]. Joinpoint fits trend lines to rates over time based on statistical significance in trends and inflection points (points where trends change). A maximum of two Joinpoints were used in our analysis. The trend analysis yielded annual percent change (APC) in age-adjusted incidence and mortality rates of endometrial cancer by race and histology for each trend segment. Thus, trends can encompass different time intervals by histology and race, explaining why different year ranges are reported in Table 2. For example, low-grade endometrioid tumors might be steadily decreasing at the same rate during all of 2000–2011 (possessing one trend), while mixed tumors see a large spike from 2000 to 2002 then level off (possessing two trends). The average annual percent change (AAPC) from years 2006 to 2011 was also calculated and used in the projections described below. The AAPC is a weighted average of the APCs contained within the specified range of dates (2006–2011). Since none of the histology-race subgroups considered contained two different APC trends within 2006–2011, the AAPC for 2006–2011 was always the single APC if only one trend existed across 2000–2011, or the second trend’s APC if two trends existed from 2000 to 2011 (but the first trend ended prior to 2006). We specified 2006–2011 because we wanted to use the five most recent annual changes in making future projections.
Projected number of new annual endometrial cancer cases by race and histological subtype were calculated for years 2015–2040 following the methodology of Rahib and Smith [11]. Briefly, age-specific incidence rates for years 2000–2011 were multiplied by the census-projected number of individuals of each corresponding age by year-to-yield unadjusted projected number of cases. These were summed up across each age group (<1 to 85+ years old) to get the total number of unadjusted projected cases for that year. The 2006–2011 AAPC was then applied to the projected total number of cases by year to adjust for observed current incidence trends using the following equation [11]:
where I d is the total number of unadjusted projected cases for a given year and “N” is the number of years since 2005.5 (interval midyear). If the AAPC was not statistically different from zero, we assumed it was zero in the projections. The equations assume that the AAPC in incidence rates will remain constant over the course of the projection period. This might lead to overestimation as the rates would increase indefinitely. To account for this, we applied an attenuation factor to the AAPCs [19]. Specifically, we assumed a progressive decay in trend so that the estimated AAPC rate was used only from 2015 to 2020, and then it was attenuated to 80 % from 2020 to 2025, 60 % from 2025 to 2030, 40 % from 2030 to 2035, and 20 % from 2035 to 2040. While a trend analysis was done on mortality rates, we did not use the results to project future deaths due to high and likely unsustainable AAPCs. Since registry incidence-based mortality cannot capture all deaths as certificates do, these AAPCs may not be reflecting the full story. Additionally, there may be floor effects where the growth is only high because it is starting from a considerably small number of deaths for a given race. Despite not calculating future death projections, we include the trend analyses because it may provide value in illustrating recent changes.
Results
Table 1 presents age-adjusted incidence rates and total number of cases each year from 2006 to 2011 for each of the endometrial cancer histologies by racial-ethnic group. While we consider the 2000–2011 time frame in our analysis, we present Table 1 to familiarize the reader with the data from the past 6 years, since the AAPC during this time frame (reported in Table 2) is used to make the projections presented in Table 3.
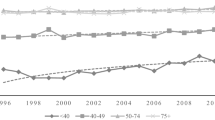
Joinpoint regression results of age-adjusted incidence trends are depicted in Table 2. A single trend (no Joinpoint) was observed for most histologies. Statistically significant AAPCs from 2006 to 2011 ranged from −1.21 for high-grade endometrioid histology among NHWW to 23.77 for mixed histology among NHBW. The age-adjusted incidence rate of low-grade endometrioid cancer is decreasing annually by −0.82 % for NHWW but is increasing for NHBW at close to 1 % annually. NHWW are the only group for which high-grade endometrial cancer incidence rates are decreasing. Incidence rates of clear-cell endometrial carcinomas and “other” endometrial carcinomas appear to be steady across all racial groups, with no statistically significant AAPCs observed, whereas the incidence of serous endometrial cancers is increasing (p < 0.05) for all racial groups. Joinpoint reported several unrealistically high APCs for mixed histologies from 2000 to 2002 among NHWW and HWW categories. In these groups, the AAPC from 2006 to 2011 reflected a much slower growth rate in incidence. While NHWW and NHBW both have statistically significant positive AAPCs for mixed histology tumors, the trend analysis yielded a considerably more substantial AAPC (23.77) for NHBW. This was the highest AAPC observed in the trend analysis and would have the largest influence on the projected number of cases. We question the long-term sustainability of such an increase in the discussion section. For MMMT/carcinosarcoma, NHWW were the only group with a statistically significant increase in incidence.
Table 3 displays the projected number of new cases of endometrial cancer in 2020, 2030, and 2040 by histology and race/ethnicity. Low-grade endometrioid tumors are consistently the largest contributor of new cases for NHWW and HWW, although the actual number of annual cases will decrease in NHWW due to the decreasing trend in age-adjusted incidence rate. For NHBW, mixed histology tumors will become dominant. This is due to an AAPC of over 23, which even when attenuated, may lead to a large overestimation. Thus, we advise caution in interpreting the high magnitude of increase in all types of histologies in NHBW, since the total increase is largely driven by the mixed histology increase. The increase in the number of new cases of serous tumors among NHBW is considerable. By 2040, we project the number of new cases of serous endometrial tumors to be comparable to that of low-grade endometrioid tumors among NHBW.
Joinpoint regression results of age-adjusted incidence-based mortality trends are presented in Table 4. The AAPCs are noticeably higher for mortality than incidence across the majority of the histologies. The largest AAPC was in NHWW for endometrioid cancer of low grade at 11.41, although HWW and NHBW also had high AAPCs. This histology was the only one among HWW that had a significant AAPC in the incidence-based mortality rates. However, for a few of the other histologies in HWW, Joinpoint could not calculate the AAPC due to some years that had values near zero; thus, this finding should be considered with caution. Mortality rates of serous cell carcinomas are also increasing steadily for NHWW and NHBW. The authors suspect that these high mortality AAPCs are to some extent a product of incidence-based mortality registry data that may not be a valid estimate of true mortality trends. Rahib et al. were able to predict deaths by amending a prior paper’s projections that used mortality that was not incidence based. This type of data was not available by race and histology. The high AAPCs were also based on increases from relatively low rates, and ceiling and floor effects may make them higher than is sustainable. For these reasons, we present the trend analysis but do not make projections for the number of deaths.
Discussion
We project a substantial increase in the annual number of endometrial cases in the USA from 2015 to 2040. In the year 2040 alone, there may be over 100,000 new cases. This represents a potential challenge to the health care system to increase preventive service care capacity for endometrial cancer patients. The projections reflect a US population that will become both older and more racially diverse. As Smith et al. have suggested, cancer incidence rates are higher in older and minority populations, and the number of cases seen at the population level is expected to mirror future demographic changes [10]. Our results for projected incidence (over 83,000 new cases in 2030) are lower compared with Rahib et al., who estimate over 120,000 cases in the year 2030 [11].
Our trend analysis of endometrial cancer age-adjusted rates found variations by histology and race. Interestingly, the incidence rate of low-grade endometrioid tumors is decreasing in NHWW but increasing in NHBW. Low-grade endometrioid is the least aggressive of the histologies considered with the best survival rates. Additionally, AAPCs were large for mixed histology tumors in both NHWW and NHBW, at 7.23 and 23.77, respectively. We strongly caution the interpretation of the mixed histology type results, as these large AAPCs and corresponding high projections are potentially a coding artifact. Since WHO coding guidelines for what constitutes a mixed tumor have changed over time, the large AAPCs for mixed histology may be reflecting these changes [20, 21]. One striking observation is that the incidence rate of serous endometrial cancers, which are an aggressive histological subtype, is increasing steadily in all racial groups. This increase has the potential to be reflected in later clinical stage presentation among patients and higher mortality. In contrast, clear-cell rates, also considered a highly aggressive subtype, were steady in all racial groups. The reason behind an increase in one aggressive subtype and not the other is unclear and warrants further investigation.
Within race comparisons also yielded interesting results. For NHWW, low-grade endometrioid tumors were projected to be the most common throughout the time period. However, they will decline somewhat and become a smaller proportion of cases as the mixed histology tumors (AAPC of 7.23) become a dominant histology. Within HWW, low-grade endometrioid tumors will continue their climb in case numbers throughout the projected time period, despite a non-significant change in the age-adjusted rate. This is largely a reflection of the census projections of the Hispanic population, which is expected to increase considerably. Serous cell carcinomas are also projected to increase and become a larger proportion of total endometrial cancers in HWW. In NHBW, it is concerning to see that aggressive serous cell tumors could be as common as low-grade and less-aggressive endometrioid cancers by the year 2040. These are expected to share an equal proportion of the total endometrial cancer burden in NHBW. This will not bode well for the racial disparity in mortality rates that exists between white and black women, as the heightened aggression of serous tumors leads to later stage presentation and lower survival.
The trend analysis of age-adjusted incidence-based mortality rates also found variations by histology and race. There were a striking number of high AAPCs, with NHWW having AAPCs near 10 for low-grade endometrioid, clear-cell, and mixed histologies. The mortality rates for HWW remained steady across all histologies, except for low-grade endometrioid, which has been increasing steadily (AAPC over 10). Aggressive histologies such as serous were found to have significant positive AAPCs for both NHWW and NHBW. The steady increase in mortality rates from MMMT tumors among NHWW and NHBW was interesting, as only NHWW had a similar increasing trend when comparing to respective incidence trends. Serous tumors also show a significant increase in mortality rates among NHWW and NHBW, but the incidence trends mirror the increase for all racial groups.
The observed increases in incidence and mortality rates may be strongly connected to the obesity epidemic in the USA. Obesity is widely accepted to be one of the strongest risk factors for endometrial cancer. Close to 90 % of women with type I endometrial cancer cases are obese, and one meta-analysis found that a 5 kg/m2 increase in body mass index is associated with 1.6 times the risk of developing endometrial cancer [22, 23]. In classifying endometrial cancer tumors, type I tumors are estrogen dependent and usually the endometrioid subtype, while type II tumors are considered estrogen independent and are usually the serous subtype [24]. The prevalence of obesity has been steadily increasing in the USA, where over one third of adults are obese [25]. Research has demonstrated that obesity confers a higher risk of endometrial cancer across subtypes (although the association is slightly stronger with type I tumors) [24], which may imply that incidence increases due to obesity trends would be expected across a range of tumor subtypes, consistent with our results [26]. Thus, it is probable that obesity is a key contributor to the trends reported in this paper.
This study has both strengths and limitations. The overriding strength is that the trends and projections are calculated from rates that come from a well-respected data source. SEER 18 is a reliable and generalizable cancer registry that provides population-representative data from its large sample. Additionally, this study adds granularity to existing projections by considering race and histology-specific rates and trends. These projections can be used as a way to measure the impact of interventions designed to reduce endometrial cancer incidence and racial disparities in mortality. There are also several limitations to the study. First, determining histologic subtype of endometrial cancer can be challenging, with inconsistencies even between subspecialty pathologists. No standardized pathology review is available for cases captured in SEER. Also, despite the large population covered by SEER, data were sparse for Asian and Native Americans, so we were unable to provide stable projections for these groups. Next, we assumed that the trends (AAPCs) in age-adjusted endometrial cancer incidence will attenuate in the future. This may hold especially true for some histologic and race categories, but may be unrealistic for others. For example, an AAPC of 23.77 for mixed histology tumors in NHBW is unlikely to persist for over 30 years. Even attenuation of the estimate led to such a high number of cases that the authors speculate the observed AAPC from 2006 to 2011 is an artifact of another cause; perhaps the changes in WHO coding guidelines mentioned previously or the fact that the APC(s) were derived from small case counts for mixed histology. More importantly, the estimates do not consider rates of hysterectomy in the population or potential changes in use of oral contraceptives (OCs) or intrauterine devices (IUDs), which reduce the risk of developing endometrial cancer [27, 28]. The prevalence of hysterectomy appears to have stabilized over the last two decades, but it appears use of OCs and IUDs are increasing, suggesting that our projections may be overestimates [29–31]. This study assumes a constant profile of risk factors in the population and consistent histology classifications.
Conclusion
In conclusion, the national incidence of endometrial cancer is expected to rise as the population undergoes demographic changes. The increase in endometrial cancers will occur in all racial groups, but the rise of aggressive endometrial cancers will disproportionately affect black women. As public health practitioners design interventions to reduce the burden of endometrial cancer and eliminate the racial disparity, these estimates will provide a way to quantify the effect of such interventions.
References
Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012;120:383–97. doi:10.1097/AOG.0b013e3182605bf1.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi:10.3322/caac.21254.
Burke WM, Orr J, Leitao M, Salom E, Gehrig P, Olawaiye AB, et al. Endometrial cancer: a review and current management strategies: part i. Gynecol Oncol. 2014;134:385–92. doi:10.1016/j.ygyno.2014.05.018.
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, (eds) et al. SEER cancer statistics review, 1975–2012, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2012/, based on November 2014 SEER data submission, posted to the SEER web site, April 2015.
Long B, Liu FW, Bristow RE. Gynecologic oncology disparities in uterine cancer epidemiology, treatment, and survival among African Americans in the United States. Gynecol Oncol. 2013;130:652–9. doi:10.1016/j.ygyno.2013.05.020.
Jamison PM, Noone A-M, Ries LAG, Lee NC, Edwards BK. Trends in endometrial cancer incidence by race and histology with a correction for the prevalence of hysterectomy, SEER 1992 to 2008. Cancer Epidemiol Biomark Prev. 2013;22:233–41. doi:10.1158/1055-9965.EPI-12-0996.
Allard JE, Maxwell GL. Race disparities between black and white women in the incidence, treatment, and prognosis of endometrial cancer 2009;16.
Maxwell GL, Tian C, Risinger J, Brown CL, Rose GS, Thigpen JT, et al. Racial disparity in survival among patients with advanced/recurrent endometrial adenocarcinoma: a gynecologic oncology group study. Cancer. 2006;107:2197–205. doi:10.1002/cncr.22232.
Murali R, Soslow RA, Weigelt B. Classification of endometrial carcinoma: more than two types. Lancet Oncol. 2014;15:e268–78. doi:10.1016/S1470-2045(13)70591-6.
Smith BD, Smith GL, Hurria A, Hortobagyi GN, TA B. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27:2758–65. doi:10.1200/JCO.2008.20.8983.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–21. doi:10.1158/0008-5472.CAN-14-0155.
Sheikh MA, Althouse AD, Freese KE, Soisson S, Edwards RP, Welburn S, et al. USA endometrial cancer projections to 2030: should we be concerned? Future Oncol. 2014;10:2561–8. doi:10.2217/fon.14.192.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2013 Sub (1973–2011 varying) - Linked To County Attributes - Total U.S., 1969–2012 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2014 (updated 5/7/2014), based on the November 2013 submission.
Surveillance Research Program, National Cancer Institute SEER*Stat software (www.seer.cancer.gov/seerstat) version 8.1.5. n.d.
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International classification of diseases for oncology. Third. World Health Organization; 2001.
Brinton LA, Felix AS, McMeekin DS, Creasman WT, Sherman ME, Mutch D, et al. Etiologic heterogeneity in endometrial cancer: evidence from a gynecologic oncology group trial. Gynecol Oncol. 2013;129:277–84. doi:10.1016/j.ygyno.2013.02.023.
United States Census Bureau. 2012 National population projections: downloadable Files. http://www.census.gov/population/projections/data/national/2012/downloadablefiles.html. Accessed April 6, 2015. n.d.
Joinpoint Regression Program, Version 4.1.1.4 - February 2015; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute. n.d.
Virani S, Sriplung H, Rozek LS, Meza R. Escalating burden of breast cancer in southern Thailand: analysis of 1990-2010 incidence and prediction of future trends. Cancer Epidemiol. 2014;38:235–43. doi:10.1016/j.canep.2014.03.003.
Kurman RJ, Carcangiu ML, Herrington CS, Young RH. WHO classification of tumours of female reproductive organs. Fourth. Lyon: IARC Press; 2014.
Tavassoli F, Devilee P, editors. World Health Organization classification of tumours: pathology and genetics: tumours of the breast and female genital organs. Lyon: IARC Press; 2003.
Fader AN, Arriba LN, Frasure HE, von Gruenigen VE. Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol Oncol. 2009;114:121–7. doi:10.1016/j.ygyno.2009.03.039.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78. doi:10.1016/S0140-6736(08)60269-X.
Setiawan VW, Yang HP, Pike MC, McCann SE, Yu H, Xiang YB, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013;31:2607–18. doi:10.1200/JCO.2012.48.2596.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–14. doi:10.1001/jama.2014.732.
Weiss JM, Saltzman BS, JA D, LF V, Chen C, Beresford SAA, et al. Risk factors for the incidence of endometrial cancer according to the aggressiveness of disease. Am J Epidemiol. 2006;164:56–62. doi:10.1093/aje/kwj152.
Cote ML, Alhajj T, Ruterbusch JJ, Bernstein L, Brinton LA, Blot WJ, et al. Risk factors for endometrial cancer in black and white women: a pooled analysis from the epidemiology of endometrial cancer consortium (E2C2). Cancer Causes Control 2014;26:287–296. doi:10.1007/s10552-014-0510-3.
Beining RM, Dennis LK, Smith EM, Dokras A. Meta-analysis of intrauterine device use and risk of endometrial cancer. Ann Epidemiol. 2008;18:492–9. doi:10.1016/j.annepidem.2007.11.011.
Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990-1997. Obstet Gynecol. 2002;99:229–34.
Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among United States women, 2009-2012. Obstetrics & Gyn. 2015;126(5):917–27.
Wright JD, Herzog TJ, Tsui J, Ananth CV, Lewin SN, Lu Y, Neugut AI, Hershman DL. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 0 1):233–41.
Acknowledgments
Dr. Meza acknowledges the support of the Department of Epidemiology at the University of Michigan. Mr. Gaber was partially supported by a Dean’s award from the School of Public Health, University of Michigan and the Karmanos Cancer Institute (2P30CA022453-34).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with animals performed by any of the authors. For this type of study, formal consent is not required.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Gaber, C., Meza, R., Ruterbusch, J.J. et al. Endometrial Cancer Trends by Race and Histology in the USA: Projecting the Number of New Cases from 2015 to 2040. J. Racial and Ethnic Health Disparities 4, 895–903 (2017). https://doi.org/10.1007/s40615-016-0292-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-016-0292-2