Abstract
Background
Exercise is highly recommended in patients with Parkinson’s disease (PD). Exercise-induced amelioration of motor, non-motor, and drug-induced symptoms are widely known. However, specific guidelines on exercise testing and prescription in PD are lacking.
Objective
This study reviews the literature on exercise-based approaches to the management of symptoms at each stage of the disease and evaluate: (1) the most suitable clinical exercise testing; (2) training programs based on testing outcomes and PD stage; (3) the effects of exercise on antiparkinsonian drugs and to suggest the most effective exercise–medication combination.
Methods
A systematic search was conducted using the databases MEDLINE, Google Scholar and, Cochrane Library using “Parkinson’s Disease AND Physical therapy”, “Training AND Parkinson”, “Exercise”, “Exercise AND Drug” as key words. In addition, references list from the included articles were searched and cross-checked to identify any further potentially eligible studies.
Results
Of a total of 115 records retrieved, 50 (43%) were included. From these, 23 were included under the rubric “exercise testing”; 20 focused on the effectiveness of different types of exercise in PD motor-functional symptoms and neuroprotective effects, throughout disease progression, were included under the rubric “training protocol prescription”; and 7 concern the rubric “interaction between exercise and medication”, although none reported consistent results.
Conclusions
Despite the lack of standardized parameters for exercise testing and prescription, all studies agree that PD patients should be encouraged to regularly train according to their severity-related limitations and their personalized treatment plan. In this manuscript, specific guidelines for tailored clinical testing and prescription are provided for each stage of PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson's disease (PD) affects 6 million people worldwide [1], making it one of the most common neurological syndromes derived from dopamine loss. Resting tremor, bradykinesia, rigidity, postural instability, and gait impairment are the main cardinal symptoms. Besides them, the psychological and emotional spheres are often involved, increasing disease severity [2]. While such diverse factors as aging, free radical toxicity, mitochondrial dysfunction, genetics, and environmental stressors can trigger PD onset [3], its etiology remains unknown.
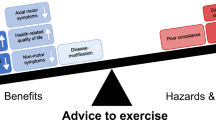
Given the wide range of symptoms and inter-individual differences, a personalized and multidisciplinary approach to appropriate treatment planning is warranted. Currently, levodopa (L-DOPA) administration in the early PD stages is the gold standard therapy. Unfortunately, its chronic use induces dyskinesias accompanied by worsening of general health [4]. However, there is evidence from both human and animal models [5, 6] that, owing to its neuroprotective role [7], exercise can improve motor impairment and physical condition in PD patients regardless of the stage of the disease. To evaluate the most effective exercise-based treatments, patients are required to undergo clinical tests to identify disease stage-specific vital and motor parameters.
Currently, clear recommendations for the most suitable clinical exercise tests are lacking. Studies describe numerous tests that evaluate the domains affected by PD [38, 71], but the necessity to prescribe the correct exercise depending on the outcome of each test is still underestimated. Likewise, little is known about exercise programs in terms of frequency, intensity, time, and type (FITT) of intervention addressed to PD patients based on disease severity. High-intensity exercise and long-term therapy have been associated with greater benefits than low-intensity and medium- or short-term therapies [6, 8]. Moreover, a combination of mobility exercise, gait, and balance training [9], occupational therapy, cued exercises, high-intensity aerobic and resistance activities are recommended [10]. The effectiveness of training different muscle groups through various activities is increasingly recognized, along with the importance of supervision and motivation during preferred training activities. However, the most effective training program for PD patients remains a matter of debate.
Additionally, it is important to couple exercise and medication to maximize the beneficial effects over time and potentially counteract long-term drug side effects. While exercise training can be added to medications to manage disease symptoms and enhance their benefits [72], more rigorous investigations have to be conducted for cognitive function, daily living activities (ADL), and psychosocial variables. Even though exercise does not change greatly medications’ effects, PD patients respond better during the “on” phase, or when they can move fluently thanks to the still circulating drug rather than during the “off” phase, when symptoms tend to reappear with compromised movements.
The present study aimed to review the PD literature on exercise testing, on personalized training programs and the impact of exercise on antiparkinsonian drug-treatment. The findings are summarized as indications for exercise-based non-pharmacological approaches to manage PD symptoms in each stage of the Hoehn and Yahr (H&Y) classification [11].
Methods
Following the PRISMA guidelines for systematic review of the literature [12], controlled clinical trials, systematic reviews, and works containing guidelines were identified and included by means of a computerized literature search in the Google Scholar, MEDLINE, Pubmed, and Cochrane Library electronic databases with the following keywords: Parkinson’s disease AND physical therapy, training AND Parkinson, exercise, exercise AND drug. Furthermore, references and cross-references, bibliographies, citations of articles or publications were reviewed. The search strategy focused on (1) articles in English published from 1986 to 2019, (2) patients with PD and the respective exercise-based non-pharmacological prescribed treatment, (3) disease stage (H&Y classification), clinical tests, exercise prescription, type, intensity, and frequency of training, and drug administration. Selection criteria for clinical tests and training protocols were feasibility, usefulness, safety of each approach, in addition to compliance of subjects, and improvements of deficits described in the included works. Retrieved articles were grouped as follows: exercise testing, training protocol prescription and interaction between exercise and medication. The first two sections were further classified into three core areas: endurance, strength, and flexibility.
After excluding non-relevant articles, a total of 50 records were included (Fig. 1).
Results
Exercise testing
To obtain maximal benefits, the prescription of a personalized program upon clinical evaluation, functional capacity, mental health, and general fitness (e.g., cardiorespiratory fitness, muscular strength and endurance, flexibility) is suggested [13]. Moreover, given the chronic and progressive nature of PD, reassessment every 6–12 months to review the diagnosis and test program is recommended [11]. Albeit just for a few PD-related deficits, the general clinical tools for PD diagnosis are the older and simpler H&Y scale [14] and the newer Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) [15]. However, in addition to scales and questionnaires, the most appropriate clinical test for examinations remain a matter of clinical judgment. Thus, the present review summarizes the most suitable exercise tests into the three main core areas of physical activity: endurance, strength, and flexibility.
Endurance assessment
Eleven articles were reviewed for endurance assessment. Generally, all studies included patients with mild-to-moderate disease (1–3 H&Y). Only one focused on advanced PD. Six researches tested patients under medication; in one study the patients were in off status, and four articles did not mention medication status. There was one randomized controlled trial, one research report, five clinical studies; the remaining two included reviews that validated the results. Additionally, a book and a research article which both contain two published guidelines were used. The endurance assessment tests are summarized in Table 1. Table 2 presents the specifics of each test.
Balance assessment
Ten articles on balance, functional mobility, and postural instability testing were included as considered indexes that are helpful for a general evaluation of PD. One report tested patients with PD (H&Y stage 1–4) and provided a guideline that generally refers to each disease stage; the other studies did not specifically mention disease stage. Patients under medication were tested in four studies, in one the patients were in “off” status; in two they were “in-between”; six articles did not mention medication status. This rubric included one research report, three clinical studies; the remaining four were reviews that validated the results. Additionally, a book and a research article which both contain guidelines were used. Balance assessment tests are summarized in Table 3. Table 4 presents the specifics of each test.
Resistance assessment
Nine studies evaluated measurement tools for assessing muscular strength; there was one research report and 6 clinical studies. The American College of Sports Medicine (ACSM) Guidelines for Exercise Testing and Prescription and the European Guidelines for Physiotherapy were examined for all disease stages. Six included PD patients with mild to moderate disease, generally in “on” status. Only one study involved older adults, without specifying the chronic conditions. All resistance assessment tests are summarized in Table 5. Table 6 presents the specifics for each test.
Flexibility assessment
One clinical study was reviewed for flexibility and range of motion (ROM) evaluation of mild to moderate disease. One book containing guidelines was used. Both works included PD patients in their “on” status. All flexibility assessment tests are summarized in Table 7. Table 8 presents the specifics of each test.
Training protocol prescription
The beneficial effects of exercise programs are marked in both healthy aging and PD [16]. There is also a strong connection between FITT of regular exercise and physical function in PD. Unfortunately, the optimal exercise type and dose are yet to be identified. There is much uncertainty about whether exercise influences the risk of developing the disease [17]. A better understanding of the mechanisms underpinning the exercise effect is important, as it will lead to more targeted interventions for optimal physical activity.
Since the current literature is scarce, the ACSM Guidelines for Exercise Testing and Prescription recommend improving of four main factors: gait, transfer, balance, and functional capacity. Major issues are the level of physical exertion which a PD patient can be subjected to and the most effective non-pharmacological modality (e.g., physiotherapy, walking, running, strength training or functional exercises) that can be safely prescribed. Recently, complementary programs like dance and Tai Chi have been positively re-evaluated [18]; such challenging exercises train multiple aspects of physical status simultaneously. For example, they improve walking speed, direction changes, and muscle strength in balance and gait. Furthermore, aerobic training and the "random practice" have beneficial effects of task-switching capability, particularly for PD patients. It is essential to prescribe a variety of activities to overcome the difficulties of PD patients to change activities and perform two actions simultaneously. Random practice and variation of movements will help to improve this.
Clinicians can adapt exercises from the training programs for healthy adults; indeed, both healthy adults and early-stage PD patients may present similar improvements in their general fitness and functional capacity [19]. The only advice is to adapt exercises to each person, taking into account cardiorespiratory functions, physical limitations, mental health, and disease stage progression assessed during a previous medical visit [11]. Differently, in stage 4 PD, patients need modified exercises because of the severe limitations in balance and gait. Contrarily, in bedridden patients in stage 5, the program is restricted to a palliative approach to prevent deformities or rapid physical decline [20]. Figure 2 illustrates the main objectives at each stage of PD.
Endurance training
In this section, 19 articles were included; the endurance training interventions are summarized in Table 4. The most recent papers were published in 2019, the oldest one dates from 2000. Seven studies were randomized controlled trials, six reviews, four works containing guidelines for PD management; among the remaining two, one was a clinical trial and the other a test–retest reliability study. All the studies reported benefits and improvements in PD patients after following a program of aerobic therapy that included a minimum of 20 min and a maximum of 60 min of activity. The outcome scores and main features of the studies are summarized in Table 9.
Resistance training
Twelve studies were included; the resistance training interventions are summarized in Table 5. The most recent articles were published in 2019, the oldest one dates from 2003. Two were randomized controlled trials, six reviews, four works include guidelines for PD management; of the remaining two, one was a clinical trial and the other a test–retest reliability study. All the studies reported benefits and improvements in PD patients after following a program of resistance physical therapy (minimum of 1–4 sets and multiple repetitions) in those with mild-to-moderate disease. Results and specifics of the studies are summarized in Table 10.
Flexibility training
None of the eight studies that analysed flexibility reported which is the best program for each H&Y stage. The studies included patients with early to moderate stage but none with more advanced stages. The most recent article was published in 2018 and the oldest in 2008. Three were randomized controlled trials, one was a review, four works contain guidelines for PD management. Only general recommendations about exercise frequency, time, and intensity were mentioned. Considering the exercise type, the patients were encouraged to follow a complete flexibility training program that mobilizes each body district, without distinction. The results and main features of the studies are summarized in Table 11.
Interaction between exercise and medication
Seven studies were reviewed that summarized current knowledge about the effects of physical exercise on drug absorption and efficacy in PD. Six specifically tested the effects of aerobic exercise on L-DOPA administration in PD patients with H&Y stage 1–3; no study tested patients with more advanced stage and no articles were found on drug response to resistance and flexibility exercises; only one exploited a MPTP-toxin parkinsonian mouse model used by two other studies about molecular mechanisms underlying the beneficial effects of physical exercise. One review article was added as support.
In three studies, patients exercised on a treadmill and on a cycle ergometer in four. As final assessment tools, blood samples were taken in three studies to monitor drug concentrations, UPDRS-III score was used in three, whereas only one trial reported physiological parameters (heart rate, blood pressure). The animal-based study also used behavioral testing, immunohistochemistry, and transcriptome analysis. Outcome scores and main features of the studies are summarized in Table 12.
Discussion
Endurance and balance assessment
There are valid strategies for performing endurance assessment; the choice will be dictated primarily by the focus of the study. During a clinical exercise test for endurance, also known as a fitness assessment, subjects are generally in their “on” status and are monitored while doing a battery of exercises at maximal or submaximal intensity depending on disease severity [21], graded workload exercises (GXT) on a treadmill or a stationary cycle ergometer until exhaustion [19, 22]. Likewise, patients can be tested with constant workload or free body exercise utilizing step tests. Aerobic fitness, an important parameter for most sports, can be severely impaired in illness, worsening the patient’s quality of life. The patient’s overall health and physical status can be evaluated to obtain the baseline measurements for programming a personalized exercise regimen.
Clinicians should exploit several different screening tools to determine baseline parameters [e.g., height, weight, resting heart rate (RHR), and resting blood pressure (RBP)] and compare them to the measurement taken during peak exercise or after the test. Another main objective of these tests is to measure cardiovascular performance, metabolic parameters (e.g., maximal oxygen uptake [VO2max], METs) via stress testing and monitor the cardiopulmonary response to oxygen supply, rate of perceived exertion (RPE) [23], and electrocardiogram (ECG) continuously monitored during activity. Moreover, test results may be helpful to determine functional problems, to predict the risk of falls [69], and to evaluate the effectiveness of an intervention [24]. Attention should be directed to testing balance, falling [25], and gait [26] using, for example, the Timed Up and Go (TUG), the Åstrand-Rhyming protocol during GXT, and the Berg Balance Scale (BBS), which are the most widely used evaluation tools [11, 27,28,29].
Common endurance tests, such as the 6-min walk test [27, 28] or the 2-min walk test [30] for patients with advanced PD [31], can be easily administered without special equipment and provide a complete framework of aerobic and gait capacities when coupled with GXT protocols. Because PD is a progressive disease, patients require repeated physical evaluations over time and adjustments to their training program according to disease stage [11], motor disabilities, and L-DOPA-induced complications, which may preclude safe adherence to an endurance exercise protocol (Tables 13–15). The following indications are recommended for all patients with PD (1–5 H&Y):
-
PD patients often suffer from cardiac dysrhythmias.
-
Exercise should start 45–60 min after medication has been taken.
-
Inquire about changes in medication.
-
Patients with significant fluctuation should be tested while in the “on” and the “off” status.
-
Individuals unable to perform a GXT (due to risk of falling, severe stooped posture, deconditioning) may require a radionuclide stress test or stress echocardiography.
-
Continuously monitor heart rate, blood pressure, ECG, RPE, and other signs.
-
Standard procedures, contraindications, recommended monitoring intervals, and standard termination criteria are used in exercise testing of individuals with PD.
-
For deconditioned patients with lower limb weakness, compromised balance or history of falling, precautions should be taken (gait belt, harness, and technician assistance), especially at the final stages of the test when fatigue occurs, and the individual’s walking may worsen.
-
Deep brain stimulation device, if present, should be deactivated to avoid interference with ECG recording. Remember that, without stimulation, the patient will be in a compromised mobile state and will not be able to achieve maximal tolerance (physical discomfort, tremor, cramping, and emotional symptoms).
Resistance assessment
Muscle weakness is a primary symptom of PD, not only due to consequences of aging and inactivity. It is directly correlated with lesion of the basal ganglia that impedes activation of motor neurons and results in muscle weakness [32]. Strength can be tested by measuring the maximal amount of force a muscle group can exert at one time. The primary goal is to train and improve muscle strength by developing a personalized program after baseline assessment. The exercise tests are definite for each muscle group with instrumental measurements using tensiometers or dynamometers [33,34,35]. Upper body exercise tests include the Static Handgrip Strength Test [36], the Manual Muscle Test [11, 36, 37], and the Arm Curl Test [11, 37, 38], while for the lower body the Chair Rise Test [37] or the Five Time Sit to Stand Test [29] are recommended. Note that the One-Repetition Maximum (1-RM) test is not limited to only one exercise type and that it can be conducted in a wide variety of assessments [39] (Tables 13, 14, 15). The following indications are recommended for all patients with PD (1–5 H&Y):
-
The standard index for strength assessment is the 1-RM, which is determined after completing a series of submaximal repetitions of a specific exercise.
-
Resistance is initially within the patient’s perceived capacity (50–70% of capacity). Only when the series is completed correctly it can be progressively increased.
-
It may be necessary to use very light weights or substitute them with household items.
-
A metronome is a useful to measure how long the patient can keep up with the rhythm.
-
A warm-up phase of 5–10 min is always recommended.
-
Patients at risk for cardiovascular, pulmonary or metabolic diseases should perform adapted tests.
Flexibility assessment
Flexibility refers to the ability to completely move a joint during sports and daily activities. Continuous training to exercise joints is important in injury prevention. At the early stages of the disease, patients often experience rigidity of limbs, neck or trunk, hip and shoulder, which leads to a reduced ROM, postural imbalance [10] and instability. Because of the increased resistance to movement, patients exhibit bradykinesia, muscle stiffness, pain, and cramps, fixed facial expression, difficulty turning over in bed or getting out of a chair and performing activities of daily living [29].
Since the entire body is often involved, diverse tests are administered to assess the level of flexibility and then tailor the best exercise battery to the patient’s needs.
Exploited devices in assessment include goniometers, electrogoniometers, tape measures, inclinometers, and Leighton flexometer [38]. While, for visual measurement of ROM, flexibility level can be estimated directly by screening the neck, trunk, hip, shoulder and postural motion observation through simple flexion, abduction, adduction, rotation, supination, pronation, and inversion recorded in degrees [11] (Tables 13, 14, 15). The following indications are recommended for all patients with PD (1–5 H&Y):
-
Have the patient warm-up before the evaluation and use adapted protocols as needed.
-
Show the patient how to perform the movement being evaluated.
-
Encourage the patient to stretch to the point of slight discomfort without pain.
-
Perform all tests during peak medication when the patient’s mobility is optimal.
Endurance training
Endurance exercise training refers to exercise that improves cardiorespiratory fitness, i.e., VO2max, and cardiorespiratory endurance that refers to how long an individual can perform an activity using large muscle groups. It has been suggested that PD patients can benefit from aerobic training and maintain high levels of physical function [40, 70] by performing high intensity exercises. Alternatively, leg cycle ergometry, arm ergometry or combined ergometry are valid strategies to record physical performance or cardiorespiratory fitness [41,42,43,44] in patients with severe limitations [11]. Exercise training may involve repetitive movements that guide and gradually activate the neuromuscular system by working on motor functions over time. Furthermore, good results can be obtained with a gradual aerobic exercise program for cardiovascular autonomic regulation by improving systolic blood pressure and response to orthostatic stress [19, 45]. Moreover, improvements in general fitness [20, 43, 46], fatigue, bradykinesia, gait [47,48,49], and ADL [50] are obtained after exercise at light-moderate intensity in patients with mild-to-moderate PD.
Animal studies have associated exercise dose (e.g., frequency, duration, intensity, and type of exercise) to neuroprotective effects [51]. Differently in humans, benefits of endurance exercise have been observed only in general motion, walking speed, balance improvement, and cortical reorganization favored by neuroplasticity events [52,53,54]. Furthermore, aerobic exercise has been proved to be effective for improving heart, lungs, metabolic, and circulatory systems by reducing the risk of chronic diseases such as diabetes, heart diseases, and stroke.
However, the evidence for optimal exercise dose treatment to improve function in PD remains unknown. While it is recognized that all approaches lead to positive effects, the choice of the protocol best tailored to each patient must, firstly, guarantee safety during execution. Clinicians need to consider the stage of the illness, drug-dependent status, and physical limitations, while encouraging engagement in light, moderate or vigorous exercise, according to maximum capability and motivation also in deconditioned PD patients (Tables 13, 14, 15).
Resistance training
In almost all PD patients, muscle strength declines most notably in the flexors and extensors of the hip, knee, wrist, hands, and core muscles [49]. This reduction compromises gait and general physical functions, increasing the risk of falls. Muscle weakness is a serious impairment that alters the individual’s ability to perform activities of daily living such as simply standing up from a chair or stepping. A valid approach is to prescribe specific training protocols that exercise major muscle groups, especially the lower limbs, without causing excessive fatigue [55,56,57]. Resistance training can comprise a variety of exercises, use of weight machines or bodyweight; generally, 2–3 days of weekly resistance exercise at moderate to high intensity with more than 1 set and multiple repetitions are recommended. Although the studies reviewed here focused on early and moderate stages (H&Y stage 1–3) of PD, the appropriate exercise type depends on the individual fitness, stage of illness and experience with physical activity (Tables 13–15).
Flexibility training
Rigidity is an obstacle to movement, especially when it affects lower limbs resulting in shorter steps and altered walking pace. All studies agree that regular stretching is essential in PD exercise programs. When performed multiple times per week or daily in adjunct with mobility and resistance exercises [15, 17], it may diminish muscle rigidity accompanying the illness [58]. Exercise also ameliorates muscles and joints flexibility and general health status [11, 53]. To facilitate routine movements, few tips are necessary to bring significant benefits, such as adapting both exercise and stretching time to comorbidities and PD limitations, not dynamic movements and avoiding pain. Information on the exact duration of stretching therapy is unknown. One study found a loss of efficacy 2 months after the end of the therapy and recommended continuation and repetition of flexibility training over time, especially near the peak effect of L-DOPA [59], to maintain benefits (Tables 13, 14, 15).
Interaction between exercise and medication
Physical activity in patients with PD shows improvements in motor symptoms, but, more importantly, also in non-motor signs, since exercise involves many different brain areas. Pharmacotherapy for motor signs is helpful but may worsen non-motor symptoms, especially in the long term, or accentuate compulsive disorders. The duration of "on" periods and drug effectiveness diminish with chronic L-DOPA usage, probably due to disease progression rather than the treatment itself [60]. However, treatment interruptions to avoid adverse effects can lead to regression of the disease. To date, no studies have evaluated the impact of physical activity without pharmacological support, given the ethical restrictions on standards of care. Nevertheless, important discoveries concern the positive effects of physical activity on drug-induced disorders, such as amantadine or L-DOPA, still considered the gold standard therapy. Although some studies did not report significant gaps in L-DOPA metabolism, a different outcome during cycling exercise and at rest indicated [61,62,63] three different responses, as exercise can either increase or decrease L-DOPA absorption or induce no significant change (H&Y stage 2–3).
In individuals with idiopathic PD (H&Y stage 1–2.5), the UPDRS motor score, together with blood sample analysis [64], during endurance exercise on a bike ergometer showed a slight improvement in motor response to L-DOPA administration when compared to resting condition under medication. Likely higher blood pressure and heart rate due to exercise contribute toward better drug transport over the blood–brain barrier and reduced drug storage in the periphery. More recently, these physiological parameters were studied together with the endocrine release of norepinephrine [65] during on and off medication status, at rest, and during a treadmill stress test. The results confirmed a lower autonomic response in the PD groups compared to the healthy controls. Indeed, while much work remains to be done, it was hypothesized that antiparkinsonian medication does not affect autonomic responses or motor outcomes; in contrast, abnormalities in heart rate or blood pressure are predominantly due to the disease. In a few conflicting cases [66] it was reported that L-DOPA and dopamine agonists may have had a negative effect on systolic blood pressure during a treadmill protocol, leading to limited cardiopulmonary responses to exercise in the PD patients under medication.
Physical and pharmacological therapies appear to act on the same molecular pathways but lead to opposite effects. Apparently both regulate dopamine and neuropeptides levels [52] but L-DOPA increases the release of neurotransmitters and interrupts the regular signaling between receptors and substrates, while physical exercise tends to rebalance dopamine levels and the body's homeostasis by mobilizing gene profiling and facilitating brain plasticity processes [67].
Other experiments conducted on MPTP-treated mice [68] identified three genes that normally regulate cell growth and neurogrowth factors, which in PD are activated by exercise and inhibited by drugs. Despite this general trend, the CREB1, RICTOR, and L-DOPA genes also respond slightly differently, depending on the cortical area in which they are expressed and on the disease stage. This difference may explain the diverse outcomes in patients during therapy and the choice to defer or limit drug dosage in those whose life quality is not seriously affected by PD. Although other data are needed to determine quantitatively and qualitatively how physical activity interacts with drugs, it is established that their combination is more beneficial than single treatment alone.
Limitations
This review has some limitations. Many of the studies were of short duration and involved a small sample of patients without a control group. Most had mild to moderate disease; few studies included patients at more advanced PD stages. Since PD is a chronic degenerative disorder, studies of longer duration and with larger populations are needed to confirm the results and to transform them into appropriate guidelines for patients with severe disease. Furthermore, future studies that clarify the sensitivity, and reliability of the assessments, as well as the compliance of patients with PD in joining different training programs are strongly needed, to improve the choice of appropriate clinical tests, protocols and the understanding of their outcomes.
Conclusions
For this review, we collected data from recently published studies that investigated physical training as a significant non-pharmacological treatment for neurodegeneration in PD. We aimed to find the most appropriate and suitable clinical tests for each disease stage and to identify the impairments to be treated with training according to each PD level. To date, there are no solutions to completely avoid drug prescription nor a standard exercise protocol to be broadly offered to patients. General modalities of exercise such as endurance training, resistance training, and flexibility training are increasingly recognized to alleviate symptoms in PD and thus improve quality of life; on the other hand, uncertainty and insufficient data remain about the interaction between exercise and drug delivery, especially for pharmacokinetics and pharmacodynamics.
A future area of focus is the correct FITT of exercise that can be personalized according to disease stage and drug dose. For now, it seems that the most effective training protocol is the one that combines multiple exercise modalities to be performed routinely during the week and in the long term, to maintain benefits on endurance, resistance, and flexibility (Tables 13, 14, 15). Hence, patients can manage symptoms and improve their general health. However, because PD is an irreversible and progressive disease, patients will require regular monitoring with specific clinical and exercise-test evaluations and adjustments to their training protocols and therapeutic plans based on symptom-related changes over time.
References
Dorsey ER, Elbaz A, Nichols E et al (2018) Global, regional, and national burden of Parkinson's disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17:939–953. https://doi.org/10.1016/s1474-4422(18)30295-3
Magrinelli F, Picelli A, Tocco P et al (2016) Pathophysiology of motor dysfunction in Parkinson's disease as the rationale for drug treatment and rehabilitation. Parkinsons Dis. https://doi.org/10.1155/2016/9832839
Abbas MM, Xu Z, Tan LCS (2018) Epidemiology of Parkinson's disease-east versus west. Mov Disord Clin Pract 5:14–28. https://doi.org/10.1002/mdc3.12568
Collamati A, Martone AM, Poscia A et al (2016) Anticholinergic drugs and negative outcomes in the older population: from biological plausibility to clinical evidence. Aging Clin Exp Res 28:25–35. https://doi.org/10.1007/s40520-015-0359-7
Hirsch MA, Farley BG (2009) Exercise and neuroplasticity in persons living with Parkinson's disease. Eur J Phys Rehabil Med 45:215–229
Kim JD, McCarter RJM, Yu BP (1996) Influence of age, exercise, and dietary restriction on oxidative stress in rats. Aging Clin Exp Res 8:123–129. https://doi.org/10.1007/BF03339566
Reuter I, Engelhardt M, Stecker K et al (1999) Therapeutic value of exercise training in Parkinson’s disease. Med Sci Sports Exerc 31:1544–1549
Suchowersky O, Gronseth G, Perlmutter J et al (2006) Practice parameter: neuroprotective strategies and alternative therapies for Parkinson disease (an evidence-based review) Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 66:976–982. https://doi.org/10.1212/01.wnl.0000206363.57955.1b
Kwakkel G, De Goede C, Van Wegen E (2007) Impact of physical therapy for Parkinson's disease: a critical review of the literature. Parkinson Relat D 13:478–487. https://doi.org/10.1016/S1353-8020(08)70053-1
Schenkman M, Moore CG, Kohrt WM et al (2018) Effect of high-intensity treadmill exercise on motor symptoms in patients with de novo parkinson disease: a phase 2 randomized clinical trial. JAMA Neurol 75:219–226. https://doi.org/10.1001/jamaneurol.2017.3517
Riebe D, Ehrman JK, Liguori JK et al (2018) ACSM’s guidelines for exercise testing and prescription, 10th ed
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Redecker C, Bilsing A, Csoti I et al (2014) Physiotherapy in Parkinson's disease patients: recommendations for clinical practice. Basal Ganglia 4:35–38. https://doi.org/10.1016/j.baga.2014.03.001
Opara JO, Małecki A, Małecka E et al (2017) Motor assessment in Parkinson's Disease. Ann Agric Environ Med 24(3):441–451. https://doi.org/10.5604/12321966.1232774
Gallo PM, Ewing Garber C (2011) A comprehensive approach to exercise prescription for the health fitness professional. ACSMs Health Fit J 15:8–17. https://doi.org/10.1249/fit.0b013e31821eca84
Rebelo-Marques A, De Sousa Lages A, Andrade R (2018) Aging hallmarks: the benefits of physical exercise. Front Endocrinol 9:258. https://doi.org/10.3389/fendo.2018.00258
Ellis T, Rochester L (2018) Mobilizing Parkinson's disease: the future of exercise. J Parkinsons Dis 8:S95–S100. https://doi.org/10.3233/JPD-181489
Dos Santos Delabary M, Komeroski IG, Monteiro EP et al (2018) Effects of dance practice on functional mobility, motor symptoms and quality of life in people with Parkinson's disease: a systematic review with meta-analysis. Aging Clin Exp Res 30:727–735. https://doi.org/10.1007/s40520-017-0836-2
Bryant MS, Jackson GR, Hou JG et al (2016) Treadmill exercise tests in persons with Parkinson's disease: responses and disease severity. Aging Clin Exp Res 28:1009–1014. https://doi.org/10.1007/s40520-015-0498-x
Oliveira de Carvalho A, Filho ASS, Murillo-Rodriguez E et al (2018) Physical exercise for Parkinson's disease: clinical and experimental evidence. Clin Pract Epidemiol Ment Health 14:89–98. https://doi.org/10.2174/1745017901814010089
Noonan V, Dean E (2000) Submaximal exercise testing: clinical application and interpretation. Phys Ther 80:782–807
Mavrommati F, Collett J, Franssen M et al (2017) Exercise response in Parkinson's disease: insights from a cross-sectional comparison with sedentary controls and a per-protocol analysis of a randomised controlled trial. BMJ Open 7:e017194. https://doi.org/10.1136/bmjopen-2017-017194
Penko AL, Barkley JE, Miller Koop M et al (2017) Borg scale is valid for ratings of perceived exertion for individuals with Parkinson’s disease. Int J Exerc Sci 10:76–86
Mancini M, Horak FB (2010) The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Med 46:239–248
Chomiak T, Pereira FV, Hu B (2015) The single-leg-stance test in Parkinson's disease. J Clin Med Res 7:182–185. https://doi.org/10.14740/jocmr1878w
Jacobs JV, Horak FB, Tran VK et al (2006) Multiple balance tests improve the assessment of postural stability in subjects with Parkinson's disease. J Neurol Neurosurg Psychiatry 77:322–326. https://doi.org/10.1136/jnnp.2005.068742
Brusse KJ, Zimdars S, Zalewski KR et al (2005) Testing functional performance in people with Parkinson disease. Phys Ther 85:134–141
Bloem BR, Marinus J, Almeida Q et al (2016) Measurement instruments to assess posture, gait, and balance in Parkinson’s disease: critique and recommendations. Mov Disord 31:1342–1355. https://doi.org/10.1002/mds.26572
Keus S, Munneke M, Graziano M et al (2014) European Physiotherapy Guideline for Parkinson's Disease Developed with twenty European professional associations Development and scientific justification, ParkinsonNet KNGF
White DK, Wagenaar RC, Ellis TD et al (2009) Changes in walking activity and endurance following rehabilitation for people with Parkinson disease. Arch Phys Med Rehabil 90:43–50. https://doi.org/10.1016/j.apmr.2008.06.034
Light KE, Behrman AL, Thigpen M et al (1997) The 2-minute walk test: a tool for evaluating walking endurance in clients with Parkinson's disease. Neurol Rep 20:136–139
Goodwin VA, Richards SH, Taylor RS et al (2008) The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis. Mov Disord 23:631–640. https://doi.org/10.1002/mds.21922
Durmus B, Baysal O, Altinayar S et al (2010) Lower extremity isokinetic muscle strength in patients with Parkinson's disease. J Clin Neurosci 17:893–896. https://doi.org/10.1016/j.jocn.2009.11.014
Clael S, Brandao E, Caland L et al (2018) Association of strength and physical functions in people with Parkinson's disease. Neurosci J 2018:8507018. https://doi.org/10.1155/2018/8507018
Frazzitta G, Ferrazzoli D, Maestri R et al (2015) Differences in muscle strength in parkinsonian patients affected on the right and left side. PLoS ONE 10:3. https://doi.org/10.1177/1545968313508474
Koller W, Kase S (1986) Muscle strength testing in Parkinson's disease. Eur Neurol 25:130–133. https://doi.org/10.1159/000115998
Lombara A (2017) Parkinson's disease: an overview. Phys Ther 20:20
Cancela JM, Ayán C, Gutiérrez-Santiago A et al (2012) The Senior fitness test as a functional measure in Parkinson’s disease: a pilot study. Parkinson Relat Disord 18:170–173. https://doi.org/10.1016/j.parkreldis.2011.09.016
Buckley TA, Hass CJ (2012) Reliability in one-repetition maximum performance in people with Parkinson's disease. Parkinsons Dis. https://doi.org/10.1155/2012/928736
Zoladz JA, Majerczak J, Zeligowska E et al (2014) Moderate-Intensity interval training increases serum brain-derived neurotrophic factor level and decreases inflammation in Parkinson's disease patients. J Physiol Pharmacol 65:441–448
Harvey M, Weston KL, Gray KG et al (2019) High-intensity interval training in people with Parkinson’s disease: a randomized, controlled feasibility trial. Clin Rehabil 33:428–438. https://doi.org/10.1177/0269215518815221
Shulman LM, Katzel LI, Ivey FM et al (2013) Randomized clinical trial of 3 types of physical exercise for patients with Parkinson disease. JAMA Neurol 70:183–190. https://doi.org/10.1001/jamaneurol.2013.646
Kim Y, Lai B, Mehta T et al (2019) Exercise training guidelines for multiple sclerosis, stroke, and Parkinson disease: rapid review and synthesis. Am J Phys Med Rehabil 98:613–621. https://doi.org/10.1097/PHM.0000000000001174
Nelson R, Petersen C (2017) The reliability and minimal detectable change of the cardiovascular response and self-selected exercise intensity during forward and backward treadmill exercise in individuals with Parkinson disease. SAGE Open Med. https://doi.org/10.1177/2050312117736229
Speelman AD, Groothuis JT, van Nimwegen M et al (2012) Cardiovascular responses during a submaximal exercise test in patients with Parkinson's disease. J Parkinsons Dis 2:241–247. https://doi.org/10.3233/JPD-2012-012111
H. Cianci (2012) A body guide to Parkinson's Disease, Fitness Count
McGraw SM, Hoover DL, Shirey MP (2013) Exercise guidelines for patients with Parkinson’s disease. Home Health Care Manag Pract 26:167–174. https://doi.org/10.1177/1084822313514977
Nadeau A, Pourcher E, Corbeil P (2014) Effects of 24 wk of treadmill training on gait performance in Parkinson's disease. Med Sci Sports Exerc 46:645–655. https://doi.org/10.1249/MSS.0000000000000144
Salgado S, Williams N, Kotian R (2013) An evidence-based exercise regimen for patients with mild to moderate Parkinson’s disease. Brain Sci 3:87–100. https://doi.org/10.3390/brainsci3010087
Miyai I, Fujimoto Y, Ueda Y (2000) Treadmill training with body weight support: its effect on Parkinson's disease. Arch Phys Med Rehabil 81:849–852. https://doi.org/10.1053/apmr.2000.4439
Hou L, Chen W, Liu X (2017) Exercise-induced neuroprotection of the nigrostriatal dopamine system in Parkinson's disease. Front Aging Neurosci 9:358. https://doi.org/10.3389/fnagi.2017.00358
Ahlskog JE (2018) Aerobic exercise: evidence for a direct brain effect to slow Parkinson Disease progression. Mayo Clin Proc 93:360–372. https://doi.org/10.1016/j.mayocp.2017.12.015
Frazzitta G, Maestri R, Ghilardi MF (2014) Intensive rehabilitation increases BDNF serum levels in parkinsonian patients: a randomized study. Neurorehabil Neural Repair 28:163–168. https://doi.org/10.1177/1545968313508474
Fisher BE, Wu AD, Salem GJ et al (2008) The effect of exercise training in improving motor performance and corticomotor excitability in people with early Parkinson's disease. Arch Phys Med Rehabil 89:1221–1229. https://doi.org/10.1016/j.apmr.2008.01.013
Steiger L, Homann CN (2019) Exercise therapy in Parkinson's disease—an overview of current interventional studies. Physiother Res Rep 1:1–10. https://doi.org/10.15761/PRR.1000117
Uhrbrand A, Stenager E, Pedersen MS et al (2015) Parkinson's disease and intensive exercise therapy—a systematic review and meta-analysis of randomized controlled trials. J Neurol Sci 353:9–19. https://doi.org/10.1016/j.jns.2015.04.004
Hirsch MA, Toole T, Maitland CG et al (2003) The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson’s disease11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors(s) or upon any organization with which the author(s) is/are associated. Arch Phys Med Rehab 84:1109–1117. https://doi.org/10.1016/s0003-9993(03)00046-7
EllisT, DeAngelis TR, Dalton D, Venne J (2016) Be active & beyond—a guide to exercise and wellness for people with Parkinson's Disease
Petersen CM, Nelson R, Steffen TM (2013) The effect of Parkinson drug timing on cardiovascular response during treadmill exercise in a person with Parkinson Disease and freezing of gait. Physiother Can 65:217–222. https://doi.org/10.3138/ptc.2011-57
Marsden CD, Parkes JD (1977) Success and problems of long-term levodopa therapy in Parkinson's disease. Lancet 20:345–349
Lopane G, Contin M, Scaglione C et al (2010) The effect of a clinically practical exercise on levodopa bioavailability and motor response in patients with Parkinson disease. Clin Neuropharmacol 33:254–256. https://doi.org/10.1097/WNF.0b013e3181f5328c
Reuter I, Harder S, Engelhardt M et al (2000) The effect of exercise on pharmacokinetics and pharmacodynamics of levodopa. Mov Disord 15:862–868. https://doi.org/10.1002/1531-8257(200009)15:5<862:AID-MDS1015>3.0.CO;2-S
Carter JH, Nutt JG, Woodward WR (1992) The effect of exercise on levodopa absorption. Neurology 42:2042–2045. https://doi.org/10.1212/wnl.42.10.2042
Muhlack S, Welnic J, Woitalla D et al (2007) Exercise improves efficacy of levodopa in patients with Parkinson’s disease. Mov Disord 22:427–430. https://doi.org/10.1002/mds.21346
DiFrancisco-Donoghue J, Elokda A, Lamberg E (2009) Norepinephrine and cardiovascular responses to maximal exercise in Parkinson's disease on and off medication. Mov Disord 24:1773–1778. https://doi.org/10.1002/mds.22612
Skidmore FM, Patterson SL, Shulman LM et al (2008) Pilot safety and feasibility study of treadmill aerobic exercise in Parkinson disease with gait impairment. J Rehabil Res Dev 45:117–124. https://doi.org/10.1682/JRRD.2006.10.0130
Cotman CW, Berchtold NC (2002) Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci 25:295–301. https://doi.org/10.1016/S0166-2236(02)02143-4
Klemann CJHM, Xicoy H, Poelmans G et al (2018) Physical exercise modulates L-DOPA-regulated molecular pathways in the MPTP mouse model of Parkinson's disease. Mol Neurobiol 55:5639–5657. https://doi.org/10.1007/s12035-017-0775-0
Dibble LE, Lange M (2006) Predicting falls in individuals with Parkinson disease: a reconsideration of clinical balance measures. J Neurol Phys Ther 30:60–67. https://doi.org/10.1097/01.npt.0000282569.70920.dc
O’Callaghan A, Harvey M, Houghton D et al (2019) Comparing the influence of exercise intensity on brain-derived neurotrophic factor serum levels in people with Parkinson’s disease: a pilot study. Aging Clin Exp Res. https://doi.org/10.1007/s40520-019-01353-w
Macleod AD, Counsell CE (2010) Timed tests of motor function in Parkinson’s disease. Parkinson Relat Disord 16:442–446. https://doi.org/10.1016/j.parkreldis.2010.04.006
Dibble LE, Foreman KB, Addison O et al (2015) Exercise and medication effects on persons with Parkinson disease across the domains of disability: a randomized clinical trial. J Neurol Phys Ther 39:85–92. https://doi.org/10.1097/NPT.0000000000000086
Funding
This work was partially supported by the Italian Ministry of Research and University (MIUR-Rome, Italy) 5-year special funding (https://www.miur.gov.it/dipartimenti-di-eccellenza).
Author information
Authors and Affiliations
Contributions
MC reviewed the literature, collected the data and drafted the manuscript; AP, MV, GG, FR and FGL revised and edited it critically; AP, MV, FS, MT, RBM and JJF supervised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any experimental study with humans or animals performed by the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martignon, C., Pedrinolla, A., Ruzzante, F. et al. Guidelines on exercise testing and prescription for patients at different stages of Parkinson’s disease. Aging Clin Exp Res 33, 221–246 (2021). https://doi.org/10.1007/s40520-020-01612-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01612-1