Opinion statement
Schizophrenia is a devastating mental illness that has profound effects on a person’s health and quality of life. Exercise represents a promising new treatment option that may supplement current psychosocial and pharmacological interventions for psychosis. A large body of work suggests that exercise can improve cardio-metabolic and health behavior and facilitate neurogenesis in areas of the brain that are notably impacted by psychosis. Recent efforts to incorporate exercise as either stand-alone or adjunctive treatment for individuals with schizophrenia range from yoga and light stretching to moderately intense walking, bike riding, or team sports. These interventions suggest that moderately intense exercise may be beneficial for improving both positive and negative symptomatology, cognition, and functioning. Indeed, exercise may be beneficial for decreasing risk factors for a wide range of health problems often observed in patients with schizophrenia, including weight gain and metabolic syndrome as well as tobacco and substance use. Given the positive results from interventions in schizophrenia patients, there is an impetus for incorporating exercise in the early stages of the disorder. Notably, individuals at ultrahigh risk (UHR) for psychosis report more sedentary behavior and perceive less benefit from exercise; interventions prior to the onset of the disorder may be helpful for increasing health behaviors, perhaps delaying or preventing the onset of psychosis. Taken together, for individuals with psychosis, exercise may provide holistic benefits for the neural to the social impairments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accumulating evidence from both animal and human studies [1,2,3] suggests that regular exercise positively affects integral functions such as neurological maintenance and cognition. Because voluntary exercise has been found to promote neuron growth factors and genetic processes that improve brain plasticity (i.e., the ability to repair or change the structure of synaptic connections) in humans [4], and neural abnormalities have been widely observed in patients with schizophrenia [5,6,7], aerobic physical activity may be an effective way to improve neural dysfunction and associated behavioral problems in psychosis. Consistent with this notion, evidence indicates that exercise ameliorates many of the cognitive deficits that are functionally disabling for individuals with schizophrenia [8, 9]. Further, several studies suggest that moderate to vigorous exercise is associated with improved quality of life in patients with schizophrenia [10]. Perhaps most critically, aerobic exercise appears to address several symptom domains in schizophrenia [8]. While most studies have focused on the effects of aerobic or cardiovascular exercise treatments, there are several other types of exercise (e.g., yoga), that may be helpful in addressing a different range of symptoms and characteristics (e.g., social support, self-esteem, self-efficacy). Further, in addition to directly addressing core impairments of psychotic illness, exercise has been found to ameliorate many common factors contributing to poor health in people with schizophrenia, including sedentary behavior and smoking [11]. In a promising related direction, investigators are exploring the potential for aerobic exercise to supplement treatment with antipsychotics in order to address the side effects of these medications [12]. Finally, there is growing interest in examining aerobic exercise as a treatment option for high-risk or prodromal individuals to ameliorate symptoms and improve cognition in this critical population, as well as potentially halt the course of illness [13, 14•]. In this review, we briefly discuss the rationale for exercise interventions as an adjunctive treatment for schizophrenia, a possible tool to improve the quality of life and overall health for individuals with a psychotic disorder, and review the recent literature supporting each of these promising developments. Next, we discuss how to address factors that can get in the way of exercise treatment for this population and finally turn toward discussing future directions for this exciting treatment option.
Physical activity and exercise
Physical activity is, broadly speaking, any body movement produced by skeletal muscles that expends energy. Exercise is any planned, structured, and repetitive physical activity that improves or maintains physical fitness [15]. There are a number of different ways to measure physical fitness. The measures in many of the studies reviewed in this paper include cardiovascular health (i.e., heart rate and lung capacity tests such as those for VO2max), weight loss, and completion of a benchmark of a specific sport (i.e., finishing a 5 km run). Exercise can be divided into two categories: aerobic and anaerobic. Aerobic activity involves the cardiorespiratory system and is usually associated with activities such as walking, running, cycling, and rowing. In contrast, anaerobic exercise involves resistance to skeletal muscles and is typically associated with weight lifting and yoga.
Exercise effects on brain abnormalities and cognitive function in psychosis
Several lines of evidence indicate that aerobic activity promotes brain health and cognitive function by promoting neurogenesis [1, 9], cell proliferation [16], and slowing apoptosis [17, 18]. It also plays a critical role in promoting neurotrophic factors, essential elements for brain function, synaptic plasticity, and learning [19]. Exercise also is central for reducing inflammation [20], which can limit the positive effects of brain-derived neurotrophic factor (BDNF) on synaptic plasticity [21]. It is noteworthy that from a mechanistic standpoint, exercise affects several brain areas disrupted in psychotic disorders, including regions associated with cognitive control, memory processing, motor behavior, and reward (e.g., prefrontal cortex (PFC), caudate, hippocampus, nucleus accumbens, parietal cortex, and anterior cingulate cortex) [2, 22, 23] as well as functional connectivity between the PFC, cingulate, and hippocampus [24, 25]. Further, exercise promotes neurotrophic factors (e.g., BDNF, IGF-1, VEGF) [26,27,28] which are lower in patients with schizophrenia [29, 30] and normalizes inflammatory cytokines [9, 31] which have been found to be abnormal in psychosis [32]. Studies also suggest that aerobic exercise can help preserve telomere length and integrity, as well as alleviate neurodegeneration, which has been implicated heavily in the pathophysiology of schizophrenia [33]. As a result, it is not surprising that interventions designed to increase aerobic or cardiovascular fitness show tremendous promise for psychosis.
Exercise effects on brain structure and function in psychosis
A majority of exercise studies in schizophrenia have focused on the hippocampus, as this is a primary site of neurogenesis, and a region with structural and functional abnormalities in psychosis. An early study found that, over a 3-month period, hippocampal volume increased as aerobic fitness increased in both patients and healthy controls [8]. Another study found decreased prefrontal and hippocampal gray matter volumes in low-physical-activity first-episode psychosis patients [34]. However, two randomized controlled trials found no change in hippocampal volume in schizophrenia patients assigned to exercise despite a significant increase in aerobic fitness [35] and another found no changes in hippocampal gray matter density [36]. While sample size, medication, and heterogeneity in study design could influence results of these individual studies, a systematic review found that increases in hippocampal volume in schizophrenia populations was correlated with improvements in both aerobic fitness and cognition [37•]. Other markers of brain function may be more sensitive to the effects of exercise than medial temporal volume changes. For example, a study on schizophrenia patients and healthy controls found increased white matter integrity after a biking exercise intervention [38]. A resting state study in healthy men found high-intensity exercise-associated changes in anterior hippocampal function [39]. Another study in older adults found aerobic exercise-induced temporal functional connectivity changes that were associated with changes in growth factors [40]. Thus, future studies could benefit from exploring multiple imaging methods in psychosis populations, focusing more broadly on other brain areas as well as further exploring connectivity.
Brain-derived neurotrophic factor
Improving neuroplasticity and neurocognitive functioning is dependent on neurotrophins that regulate neuronal survival, growth, and differentiation [41•]. Of these, the BDNF protein is particularly important, being very highly expressed in medial temporal regions and playing an important role in modulating hippocampal plasticity and memory [42]. Exercise research incorporating BDNF has been plentiful, although findings have been mixed. One study reported increased concentrations of circulating BDNF in schizophrenia patients after 3 months of exercise training [43], and another group found increased BDNF levels in patients after cognitive remediation training [30]. More recently, active-play video games were used as an aerobic exercise condition, which resulted in a positive effect on neurocognition, though BDNF levels were not significantly increased [41•]. An exercise trial incorporating 20 weeks of resistance and concurrent (mixed aerobic and resistance) training also did not show significant differences in serum BDNF concentrations [44]. Further standardizing methodology in BDNF measurements would help parse out these discrepancies, which may also be due to other factors that affect BDNF levels, such as certain medications and dietary supplements [45].
Cognition
In schizophrenia, cognitive deficits have neural underpinnings that range from neurotransmitter-level dysfunction (e.g., glutamate and dopamine [46]) and intermediate phenotypes [47] to alterations in the hypothalamo-pituitary-adrenal (HPA) axis and the neuro-immune and neurogenesis systems [37•].
Multiple studies have found exercise intervention-related cognitive benefits [8, 41•, 48, 49]. These include improvements in overall neurocognition, visual memory encoding, and short-term memory, among other cognitive measures. However, this is a nuanced area, and differences in study parameters (e.g., type of exercise, frequency, intensity, trial length, incentive) as well as patient populations contribute to some confusion. For example, despite the promise of individual investigations, a recent meta-analysis found no effect of exercise on cognition in schizophrenia with the one exception of yoga interventions [50•]. Future research crystallizing the optimal type, dose, and intensity level of exercise is needed, as studies show considerable variance in this regard.
Combined cognitive training and physical activity interventions may be particularly promising. Recent studies have looked at cognitive training in conjunction with exercise in chronic schizophrenia patients (onset at least 5 years ago). One of these studies instated a relatively short 6-week intervention in which patients showed increased cognitive performance in visual learning, working memory, and processing speed, as well as an increase in subjective quality of life [51]. Another study compiled bicycle ergometer and cognitive remediation training for 3 months [52]. Interestingly, this research found long-term memory improvements in both healthy volunteers and multi-episode schizophrenia patients. The patients who engaged in more intense exercise showed long-term improvements in cognitive flexibility as well as short- and long-term verbal memory. Another recent pilot study in first-episode patients found significantly greater cognitive improvement in the cognitive training plus exercise group than in the cognitive training group alone [53].
Links with social role functioning well-being and quality of life
Social and occupational impairments are core features of schizophrenia that contribute to the marked declines in quality of life (QoL; i.e., perceived well-being and life satisfaction) that characterize the disorder. Despite effective pharmacological treatment of positive symptoms, QoL dissatisfaction and functional deficits tend to persist for a large number of affected individuals, indicating a need for effective treatments to address these impairments [54, 55]. Lack of physical activity during leisure time is significantly related to poor health-related QoL outcomes in people with schizophrenia [56]. Furthermore, reduced aerobic capacity and obesity have been associated with worse functional and QoL outcomes [57, 58], suggesting that reduced physical capacity might be related to difficulties performing everyday tasks [59].
Several studies have demonstrated the therapeutic efficacy of many different forms of physical activity for treating functional and QoL deficits including group physical activity [60•], football [61], high-intensity interval training [62], yoga [63, 64], and dancing [65]. Corroborating these findings, a recent meta-analysis of 29 studies examining the efficacy of exercise interventions in schizophrenia showed that patients receiving exercise interventions had significant improvements in QoL compared to no exercise controls and marginal improvements compared to active controls. Concerning functional outcome, patients receiving exercise interventions had significant improvements in global, social, and occupational functioning compared to patients in passive control conditions. However, no differences were found when compared to patients in active control conditions. Furthermore, moderator analyses indicated that only yoga (and not aerobic exercise) significantly improved global functioning [50•].
Evidence also suggests that, similar to the effects on neural markers, coupling exercise with cognitive training may be an effective intervention for social functioning and QoL outcomes [51, 52]. For example, a recent study demonstrated the combined benefits of endurance training and cognitive remediation on functional outcome in schizophrenia patients. Both schizophrenia patients and healthy controls completed 3 months of aerobic endurance training (30 min, three times per week) concurrently with cognitive remediation training (CRT). A control intervention group of schizophrenia patients received the same CRT but played “foosball” rather than performing endurance training. Compared to the control group, patients receiving the combined CRT and endurance training had significantly improved functional outcomes and reduced severity of negative symptoms at 3 months. As neurocognitive dysfunction is strongly associated with persistent functional deficits [66], and negative symptoms appear to partially mediate this relationship [67], combining CRT and exercise may be a particularly effective intervention for both directly and indirectly targeting functional outcomes. Future research should investigate the mediators and mechanism(s) underlying the therapeutic benefits of exercise on QoL and global functioning.
Treatment of symptomatology
Schizophrenia is characterized by positive (e.g., hallucinations, delusions), negative (e.g., alogia, anhedonia), disorganized [68], and depressive symptoms [69•]. It is noteworthy that reports from recent meta-analyses all show improvements across each of these domains as a result of exercise interventions [68, 70•, 71]. Across these studies, aerobic exercise has been the most widely reported form of intervention, and its effects have been observed most notably for negative and depressive symptoms [62, 68]. However, it is important to point that the observed improvements in some individual studies were not statistically or clinically significant, potentially due to small sample sizes and the short-term nature of interventions [10, 68].
Although exercise prescriptions vary in the delivery of the intervention in terms of intensity, duration, and type of exercise used, the combined evidence appears to suggest that the intensity and length of the intervention are notable predictors of promising outcomes. For example, in the psychosis trials, moderate to vigorous exercise and a longer exercising duration are shown to have a higher impact on symptom improvement, while lower-intensity training such as walking and yoga are related to lesser symptom improvements [62, 69•, 70•]. However, evidence suggests that yoga, even though less vigorous, can significantly decrease symptoms, suggesting that psychological factors associated with practicing yoga may play a role in the observed effects [71]. Indeed, it is noteworthy that social support, increased self-esteem and self-efficacy, and distraction are other psychological aspects that may also mediate the improvements in symptoms [69•, 70•]. However, the exact means by which exercise reduces positive, negative, and depressive symptoms in schizophrenia are not clear [69•]. The links with depressive symptoms also suggest that traditional depression treatments such as behavioral activation may play a role. Therefore, future studies should further explore mechanisms which modulate symptom reduction to create more targeted exercise treatments.
Health, sedentary behavior, and weight gain
Schizophrenia is associated with reduced life expectancy and a risk of mortality 2.5 times greater than that of the general population [72, 73]. Although unnatural causes (e.g., suicide) account for 25–40% of the higher mortality rates in schizophrenia, preventable and modifiable medical diseases (e.g., cardiovascular disease, lung cancer, diabetes) are responsible for the majority of increased mortality [74,75,76]. High disease incidence in people with schizophrenia is the result of several contributing health-related factors (e.g., sedentary lifestyle, weight gain, and poor diet).
Obesity and sedentary behavior
A recent meta-analysis indicated higher levels of sedentary behavior and less physical activity in patients with schizophrenia compared to age- and gender-matched controls [77]. Less activity is associated with more cognitive and negative symptoms, as well as higher body mass indexes (BMIs) and fasting glucose concentrations [78]. Forty-two percent of patients with schizophrenia are obese (BMI ≥27) compared to only 27% of individuals in the general population [79, 80]. Cardiovascular and metabolic risk factors are also more prevalent in chronic schizophrenia than in first-episode patients [81], highlighting the importance of early interventions.
Recent findings for the efficacy of exercise interventions for addressing the health- and lifestyle-related risk factors associated with schizophrenia are mixed. For instance, there is evidence that 12 weeks of soccer training can reduce body weight and BMI compared to baseline in males with schizophrenia [61]. A 24-week small group aerobic exercise intervention resulted in similar weight loss and BMI reductions [82]. However, an RCT examining the effects of supervised aerobic exercise on physical health in patients with schizophrenia showed no reduction in body fat percentage or BMI, though there was a significant increase in cardiorespiratory fitness [69•]. Increased physical capacity but no weight loss has also been demonstrated in studies using combined aerobic and strength training [83], group physical activity [60•], and high aerobic intensity training [84]. Although nutritional intake was not measured, the lack of weight loss may be the result of poor diet [60•, 83].
Indeed, there is evidence that the addition of a dietary intervention in conjunction with exercise may improve weight-related outcomes in people with schizophrenia. As little as 10 weeks in a weight reduction program consisting of diet modification and moderate intensity exercise has been shown to effectively reduce weight in patients with schizophrenia [85•]. Increased intervention durations might be particularly effective. Indeed, weight loss amount was positively correlated with length of participation (1–9 months) in a diet and fitness intervention in individuals with schizophrenia [86].
Smoking
Compounding weight- and physical activity-related disease risk, a meta-analysis of worldwide studies indicates that up to 62% of people with schizophrenia are smokers [87], and are at a twofold greater risk of lung cancer compared to the general population [88,89,90]. A systematic review of the acute effects of single sessions of exercise on smoking behavior in smokers without psychiatric disorders reported reductions in cigarette cravings, withdrawal symptoms, and increases in time to next cigarette [91]. These findings suggest that even brief exercise sessions aid smoking cessation. However, few exercise interventions have examined these relationships in patients with schizophrenia. An 8-week study of the effects of exercise on smoking cessation in people with schizophrenia and schizoaffective disorder reported that three sessions of 50 min of moderately intense walking combined with smoking cessation counseling resulted in significant reductions in tobacco consumption and increased smoking cessation motivation that were maintained 6 weeks post treatment [11]. Although further research is needed to determine the effects of exercise frequency, intensity, length, and type on tobacco consumption, there is some evidence that exercise is an effective adjunctive treatment for addressing smoking behavior in people with schizophrenia.
Exercise to help with antipsychotic medication side effects
Antipsychotic medication use to reduce positive symptoms in patients with schizophrenia still remains the pillar for treatment [92]. However, health-related side effects from these medications have become an increasing concern, causing poor medication compliance. Both first (typical) and second (atypical) generation antipsychotic medications have been found to cause several motor, metabolic, and cardiovascular dysfunctions [71, 93]. Additional side effects include metabolic syndrome, obesity, diabetes, stroke, inability to concentrate, and sedation [93,94,95•]. Recent studies suggest exercise may be useful in controlling antipsychotic medication complications such as weight gain [9, 10]. Results from these studies demonstrate the advantages exercise can have in improving adverse effects and the potential for increasing medication compliance. In an animal study, after participating in an exercise regimen using a running wheel, rats suffering from medication-induced side effects exhibited significantly lower glucose intolerance [96]. In a similar animal study, exercise was found to improve akinesia from chronic treatment with haloperidol [97]. Taken together, exercise has shown success in managing antipsychotic medication-induced side effects, which can have profound impacts on medical costs and mortality rates and can improve overall QoL.
Exercise in risk populations
Several recent reports have noted decreased physical activity and healthy behavior in youth who are at ultrahigh risk (UHR) for developing psychosis. UHR individuals are characterized by attenuated psychosis symptoms and a decrease in social and role function. As many as 35% of UHR individuals will go on to develop a psychotic disorder within 3 years [98]. Research during this time is important as it may shed light on etiological factors of psychosis in the absence of 3rd-variable confounds inherent in studies with chronic schizophrenia patients (i.e., long-term medication and substance use) and serves as an important opportunity for intervention before the development of more severe mental illness. One prospective study of the Northern Finland 1986 cohort showed that people who later developed psychosis were three times as likely to be physically inactive and have markers for poorer cardiorespiratory fitness than those who did not develop the disorder [99]. A cross-sectional study of self-reported frequency, intensity, and willingness to engage in exercise suggests that UHR people may not spend as much time as their healthy peers engaging in vigorous exercise (i.e., light to moderate exercise compared to moderately intense weight lifting). In addition, UHR individuals may also perceive less benefits or more barriers to getting exercise, and may not engage in exercise that requires social interaction compared to healthy individuals [100]. Another cross-sectional study found that UHR and first-episode schizophrenia patients spend less time in structured physical activities, and that this is related to greater social withdrawal [101]. A large review and meta-analysis suggests that adolescents at risk for psychosis are less physically active and often engage in poor health behaviors compared to typically developing adolescents, including an increased rate of tobacco and alcohol use [14•]. One cross-sectional study has examined physical activity’s impact on temporal gyrus (hippocampus and parahippocampal gyrus) volume in a group of UHR individuals. Using actigraphy, an instrumental measure of body movement, the UHR group showed decreased moderate or vigorous physical activity throughout a 5-day measurement period, which was related to decreased temporal volume and poorer occupational functioning [13]. Taken together, individuals at risk for psychosis appear to be less physically healthy than typically developing young adults and this decreased physical activity may be contributing to both social and neurological impairments prior to the onset of psychosis.
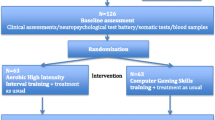
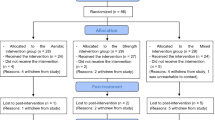
Empirically based psychosocial and pharmacological interventions in UHR samples suggest that onset of psychosis can be delayed or prevented, although subject attrition has made it difficult to reach a consensus on the effectiveness of these interventions [102]. To date, there have been no published studies that have incorporated exercise instead of or in addition to psychosocial or pharmocological approaches for individuals at risk for psychosis. Our research group is currently recruiting UHR participants for a randomized controlled trial for a supervised exercise intervention. Forthcoming work will elucidate whether exercise interventions are feasible in this population, can improve symptoms and measures of cardiometabolic fitness, and can alter putative biomarkers of risk for psychosis. The UHR period is heterogeneous with regard to presentation, need for treatment, and ultimate risk for developing psychosis [98]. It has been suggested that a staging model of treatment, whereby less invasive interventions are used prior to more extensive treatments [103, 104], may provide the best approach to treating this population. Exercise could fit in with early stages of treatment in order to promote healthier behavior and reduce stress, possibly disrupting key risk factors for psychosis and comorbid disorders [105, 106].
Addressing potential barriers to exercise treatment for schizophrenia
The nature of schizophrenia may contribute to sedentary activity as prototypic characteristic symptoms such as avolition, affect, and social deficits, and positive symptoms such as paranoia may lead to avoidance of social and peer-involved activities, causing these patients to become increasingly prone to inactivity. In a survey of physical therapists who work with patients with schizophrenia, a lack of motivation was the most frequent (45%) barrier to patients engaging in exercise and a lower emphasis was found to be given to physical activity by therapist team members [107]. Further, lack of motivation may occur because of both negative and depressive symptoms and feeling as though engaging in physical activity is unattainable [108]. A recent meta-analysis suggests that high levels of stress and low mood along with lack of social support are leading barriers to exercising [109•]. A cross-sectional study also suggests that social anxiety may contribute to sedentary behavior [110].
Currently, several studies aim to develop ways to overcome these challenges. Evidence suggests that implementing exercise routines that involve structure, incentives, motivational counseling, and support may help to facilitate engagement in physical activity [93, 111, 112]. Further, videogames utilizing movement show potential in easing transitions into more active lifestyles because social pressure may be less prevalent and overwhelming [113]. Recent trends in videogaming using augmented reality that require walking distances to complete game tasks have gained immense enthusiasm among patients with mental illness. Anecdotally, therapists have commented that these trends show promise in impacting patient routines and increasing physical activity levels. According to results from an exercise survey completed by patients that had psychological distress, 60% of participants preferred exercise that was low cost and easy to travel to as well as diverse exercise activities which are critical details to consider and may help to improve interest, initiation, and motivation [114]. Social support could improve initiation and intervention adherence, and further, one study recommended that greater attention be given to professional development [111]. Similarly, research highlights the importance in considering variability and emphasizing individually tailored exercise regimens [112, 115•]. In addition, according to a recent meta-analysis, participants report that improvements in physical and psychological health are leading motivational factors [109•]. This suggests a circular pattern where initial small gains may play an important role in removing barriers, and eventually this in turn could lead to larger gains.
Conclusions and future directions
Recent years have seen a proliferation of studies supporting exercise as a treatment modality that can address critical factors including cognitive dysfunction, quality of life, and symptomatology in schizophrenia. The intervention has a strong mechanistic rationale, supported by cognitive neuroscience and animal studies, and consequently provides a number of testable hypotheses and novel treatment targets. Exercise is also proving to be a critical treatment for addressing poor health behaviors in patients with psychosis, and for supplementing the negative side effects of primary treatment approaches involving medication. Further, new trials examining the utility of exercise for youth at high risk for psychosis are particularly promising, as there are few effective interventions for this group, and exercise provides a low-cost and low-side effect approach to treating a sensitive and important population. Although there are potential barriers to adherence (e.g., motivation, anhedonia, anxiety), thoughtful and tailored approaches can be employed to stave off or prevent these issues from getting in the way of what appears to be a revolutionary approach to treatment. There are also several important future directions that should continue to be addressed. First, the use of methods such as actigraphy and more widespread comprehensive pre- and post-treatment assessments of fitness (e.g., V02 max, which provides information about fitness via the amount of oxygen metabolized per function of time, during a high-intensity workout) are important for tracking fitness gains. Second, researchers should work to refine treatments, determining the appropriate and most efficacious exercise prescriptions (that can minimize time commitment and maximize gains, while still promoting adherence). For example, high-intensity intervals but fewer exercise sessions may hold promise in this regard. In a related point, studies should continue to work to determine the biological profiles of patients that may respond particularly well to exercise, promoting an individualized medicine approach (e.g., BDNF and inflammatory cytokines are promising markers in this regard). Investigators should also continue to pair exercise with other treatments that benefit from synaptic plasticity such as cognitive remediation. Modalities beyond aerobic or cardiovascular exercise such as yoga may also confer emotional benefits, and it will be important to test these in carefully conducted randomized controlled experiments. In a similar point, studies comparing the use of group and individualized exercise will be important to determine social benefits.
References and Recommended Reading
Paper of particular interest, published recently, have been highlighted as: • Of importance
Wolf SA, et al. Physical exercise increases adult neurogenesis and telomerase activity, and improves behavioral deficits in a mouse model of schizophrenia. Brain Behav Immun. 2011;25:971–80.
Erickson KI, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci U S A. 2011;108:3017–22.
Farrow TF, et al. Structural brain correlates of unconstrained motor activity in people with schizophrenia. Br J Psychiatry. 2005;187:481–2.
Parker BA, et al. Effect of exercise training on hippocampal volume in humans: a pilot study. Res Q Exerc Sport. 2011;82:585–91.
Walker E, et al. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psychol. 2008;4:189–216.
Allen P, et al. Abnormal relationship between medial temporal lobe and subcortical dopamine function in people with an ultra high risk for psychosis. Schizophr Bull. 2012;38:1040–9.
Pantelis C, et al. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet. 2003;361:281–8.
Pajonk FG, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67:133–43.
Cotman CW, Berchtold NC. Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci. 2002;25:295–301.
Gorczynski P and Faulkner G. Exercise therapy for schizophrenia. Cochrane Database Syst Rev. 2010; CD004412
Bernard PP, et al. Counseling and exercise intervention for smoking reduction in patients with schizophrenia: a feasibility study. Arch Psychiatr Nurs. 2013;27:23–31.
Krogh J, et al. Can exercise increase fitness and reduce weight in patients with schizophrenia and depression? Front Psychiatry. 2014;5:89.
Mittal VA, et al. Physical activity level and medial temporal health in youth at ultra high-risk for psychosis. J Abnorm Psychol. 2013;122:1101–10.
• Carney R, et al. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and meta-analysis. Schizophr Res. 2016;170:290–300. Of importance because the paper reviews the evidence of poor physical health prior to the onset of psychosis. Overall, UHR individuals engage in less physical activity and more unhealthy behaviors (i.e., tobacco and alcohol use) that put them at risk for further health problems
Caspersen CJ, et al. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–31.
Koehl M, et al. Exercise-induced promotion of hippocampal cell proliferation requires beta-endorphin. FASEB J. 2008;22:2253–62.
Avula CP, et al. Inhibitory effects of voluntary wheel exercise on apoptosis in splenic lymphocyte subsets of C57BL/6 mice. J Appl Physiol (1985). 2001;91:2546–52.
Phaneuf S, Leeuwenburgh C. Apoptosis and exercise. Med Sci Sports Exerc. 2001;33:393–6.
Hariri AR, et al. Brain-derived neurotrophic factor val66met polymorphism affects human memory-related hippocampal activity and predicts memory performance. J Neurosci. 2003;23:6690–4.
Nichol KE. Exercise alters the immune profile in aged Tg2576 (APP) toward an adaptive response coincident with improved cognitive performance. Society for Neuroscience Abstract 2006, GA
Cotman CW, et al. Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci. 2007;30:464–72.
Colcombe SJ, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol A Biol Sci Med Sci. 2006;61:1166–70.
Erickson KI, et al. Physical activity, fitness, and gray matter volume. Neurobiol Aging. 2014;35(Suppl 2):S20–8.
Burdette JH, et al. Using network science to evaluate exercise-associated brain changes in older adults. Front Aging Neurosci. 2010;2:23.
Voss MW et al. Plasticity of brain networks in a randomized intervention trial of exercise training in older adults. Front Aging Neurosci. 2010;2
Knaepen K, et al. Neuroplasticity—exercise-induced response of peripheral brain-derived neurotrophic factor: a systematic review of experimental studies in human subjects. Sports Med. 2010;40:765–801.
Griffin EW, et al. Aerobic exercise improves hippocampal function and increases BDNF in the serum of young adult males. Physiol Behav. 2011;104:934–41.
Kraus RM, et al. Circulating plasma VEGF response to exercise in sedentary and endurance-trained men. J Appl Physiol (1985). 2004;96:1445–50.
Durany N, et al. Brain-derived neurotrophic factor and neurotrophin 3 in schizophrenic psychoses. Schizophr Res. 2001;52:79–86.
Vinogradov S, et al. Is serum brain-derived neurotrophic factor a biomarker for cognitive enhancement in schizophrenia? Biol Psychiatry. 2009;66:549–53.
Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454:463–9.
Potvin S, et al. Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry. 2008;63:801–8.
Archer T, Kostrzewa RM. Physical exercise alleviates health defects, symptoms, and biomarkers in schizophrenia spectrum disorder. Neurotox Res. 2015;28:268–80.
McEwen SC, et al. Prefrontal and hippocampal brain volume deficits: role of low physical activity on brain plasticity in first-episode schizophrenia patients. J Int Neuropsychol Soc. 2015;21:868–79.
Rosenbaum S, et al. Aerobic exercise intervention in young people with schizophrenia spectrum disorders; improved fitness with no change in hippocampal volume. Psychiatry Res. 2015;232:200–1.
Falkai P, et al. The effect of aerobic exercise on cortical architecture in patients with chronic schizophrenia: a randomized controlled MRI study. Eur Arch Psychiatry Clin Neurosci. 2013;263:469–73.
• Vancampfort D, et al. Neurobiological effects of physical exercise in schizophrenia: a systematic review. Disabil Rehabil. 2014;36:1749–54. Important because it offers a review of the neurobiological effects of exercise in schizophrenia populations specifically
Svatkova A, et al. Physical exercise keeps the brain connected: biking increases white matter integrity in patients with schizophrenia and healthy controls. Schizophr Bull. 2015;41:869–78.
Bar KJ, et al. Hippocampal-brainstem connectivity associated with vagal modulation after an intense exercise intervention in healthy men. Front Neurosci. 2016;10:145.
Voss MW, et al. Neurobiological markers of exercise-related brain plasticity in older adults. Brain Behav Immun. 2013;28:90–9.
• Kimhy D, et al. The impact of aerobic exercise on brain-derived neurotrophic factor and neurocognition in individuals with schizophrenia: a single-blind, randomized clinical trial. Schizophr Bull. 2015;41:859–68. Of importance because it discusses a novel active-play videogame method of aerobic exercise that increases adherence to aerobic exercise intervention and decreases study dropout rates
Ninan I. Synaptic regulation of affective behaviors; role of BDNF. Neuropharmacology. 2014;76:684–95.
Kim HJ, et al. Increase of circulating BDNF levels and its relation to improvement of physical fitness following 12 weeks of combined exercise in chronic patients with schizophrenia: a pilot study. Psychiatry Res. 2014;220:792–6.
Silva BA, et al. A 20-week program of resistance or concurrent exercise improves symptoms of schizophrenia: results of a blind, randomized controlled trial. Rev Bras Psiquiatr. 2015;37:271–9.
Dogan T, Agilli M. Circulating brain derived neurotrophic factor levels and its relation with exercise in chronic patients with schizophrenia. Psychiatry Res. 2015;228:233.
Howes O, et al. Glutamate and dopamine in schizophrenia: an update for the 21st century. J Psychopharmacol. 2015;29:97–115.
Skelley SL, et al. Verbal and visual memory: characterizing the clinical and intermediate phenotype in schizophrenia. Schizophr Res. 2008;105:78–85.
Floel A, et al. Physical activity and memory functions: are neurotrophins and cerebral gray matter volume the missing link? NeuroImage. 2010;49:2756–63.
Gomez-Pinilla F, Hillman C. The influence of exercise on cognitive abilities. Compr Physiol. 2013;3:403–28.
• Dauwan M, et al. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2016;42:588–99. A recent meta-analysis of 29 studies indicating that, compared to control conditions, exercise treatments improve clinical symptoms and several domains of well-being, global functioning, and quality of life in individuals with schizophrenia. Also covers current gaps in knowledge and future directions
Oertel-Knochel V, et al. Effects of aerobic exercise on cognitive performance and individual psychopathology in depressive and schizophrenia patients. Eur Arch Psychiatry Clin Neurosci. 2014;264:589–604.
Malchow B, et al. Effects of endurance training combined with cognitive remediation on everyday functioning, symptoms, and cognition in multiepisode schizophrenia patients. Schizophr Bull. 2015;41:847–58.
Nuechterlein KH, et al. Enhancing cognitive training through aerobic exercise after a first schizophrenia episode: theoretical conception and pilot study. Schizophr Bull. 2016;42(Suppl 1):S44–52.
Harrison G. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001;178:506–17.
Tandon R, et al. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res. 2009;110:1–23.
Vancampfort D, et al. Lack of physical activity during leisure time contributes to an impaired health related quality of life in patients with schizophrenia. Schizophr Res. 2011;129:122–7.
Allison DB, et al. The impact of weight gain on quality of life among persons with schizophrenia. Psychiatr Serv. 2003;54:565–7.
Vancampfort D, et al. Aerobic capacity is associated with global functioning in people with schizophrenia. J Ment Health. 2015;24:214–8.
Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. 2012;11:73–9.
• Gomes E, et al. Effects of a group physical activity program on physical fitness and quality of life in individuals with schizophrenia. Ment Health and Phys Act. 2014;7:155–62. Of importance because this study demonstrates the combined benefits of cognitive remediation training and exercise for addressing functional outcomes and negative symptoms in individuals with schizophrenia
Battaglia G, et al. Soccer practice as an add-on treatment in the management of individuals with a diagnosis of schizophrenia. Neuropsychiatr Dis Treat. 2013;9:595–603.
Wu MH, et al. Effectiveness of high-intensity interval training on the mental and physical health of people with chronic schizophrenia. Neuropsychiatr Dis Treat. 2015;11:1255–63.
Varambally S, et al. Therapeutic efficacy of add-on yogasana intervention in stabilized outpatient schizophrenia: randomized controlled comparison with exercise and waitlist. Indian J Psychiatry. 2012;54:227–32.
Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: a randomized, controlled pilot study. J Altern Complement Med. 2011;17:601–7.
Kaltsatou A, et al. Effects of exercise training with traditional dancing on functional capacity and quality of life in patients with schizophrenia: a randomized controlled study. Clin Rehabil. 2015;29:882–91.
Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30.
Ventura J, et al. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113:189–99.
Malchow B, et al. The effects of physical exercise in schizophrenia and affective disorders. Eur Arch Psychiatry Clin Neurosci. 2013;263:451–67.
• Scheewe TW, et al. Exercise therapy improves mental and physical health in schizophrenia: a randomised controlled trial. Acta Psychiatr Scand. 2013;127:464–73. Of importance because the article demonstrates significant improvements in positive and negative schizophrenia symptoms and comorbid depressive symptoms in individuals engaging in an exercise intervention when compared to individuals engaging in occupational therapy
• Firth J, et al. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45:1343–61. A large meta-analysis examining both motivational factors for and barriers to exercising in individuals with severe mental illnesses
Stanton R, Happell B. A systematic review of the aerobic exercise program variables for people with schizophrenia. Curr Sports Med Rep. 2014;13:260–6.
Joukamaa M, et al. Schizophrenia, neuroleptic medication and mortality. Br J Psychiatry. 2006;188:122–7.
Saha S, et al. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–31.
Brown S. Causes of the excess mortality of schizophrenia. Br J Psychiatry. 2000;177:212–7.
von Hausswolff-Juhlin Y et al. Schizophrenia and physical health problems. Acta Psychiatr Scand Suppl. 2009;15–21
Ösby U, et al. Mortality and causes of death in schizophrenia in Stockholm County. Sweden Schizophrenia Research. 2000;45:21–8.
Soundy A, et al. Physical activity and sedentary behaviour in outpatients with schizophrenia: a systematic review and meta-analysis. International Journal of Therapy and Rehabilitation. 2013;20:588–95.
Vancampfort D, et al. Associations between sedentary behaviour and metabolic parameters in patients with schizophrenia. Psychiatry Res. 2012;200:73–8.
Allison DB, et al. The distribution of body mass index among individuals with and without schizophrenia. The Journal of Clinical Psychiatry. 1999;60:215–20.
Homel P, et al. Changes in body mass index for individuals with and without schizophrenia, 1987–1996. Schizophr Res. 2002;55:277–84.
Mitchell AJ, et al. Is the prevalence of metabolic syndrome and metabolic abnormalities increased in early schizophrenia? A comparative meta-analysis of first episode, untreated and treated patients. Schizophr Bull. 2013;39:295–305.
Dodd KJ, et al. A small group aerobic exercise programme that reduces body weight is feasible in adults with severe chronic schizophrenia: a pilot study. Disabil Rehabil. 2011;33:1222–9.
Marzolini S, et al. Feasibility and effects of a group-based resistance and aerobic exercise program for individuals with severe schizophrenia: a multidisciplinary approach. Ment Health and Phys Act. 2009;2:29–36.
Heggelund J, et al. Effects of high aerobic intensity training in patients with schizophrenia: a controlled trial. Nord J Psychiatry. 2011;65:269–75.
• Kuo FC, et al. Lifestyle modification and behavior therapy effectively reduce body weight and increase serum level of brain-derived neurotrophic factor in obese non-diabetic patients with schizophrenia. Psychiatry Res. 2013;209:150–4. Of importance because this study shows that the addition of dietary modification to a moderate intensity exercise intervention significantly increases serum BDNF levels and reduces weight in patients with schizophrenia. Increases in serum BDNF levels were positively correlated with body weight and BMI reductions
Amiaz R, et al. A diet and fitness program similarly affects weight reduction in schizophrenia patients treated with typical or atypical medications. Pharmacopsychiatry. 2016;49:112–6.
de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. 2005;76:135–57.
Kelly C. Cigarette smoking and schizophrenia. Adv Psychiatr Treat. 2000;6:327–31.
Crump C, et al. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry. 2013;170:324–33.
Levander S et al. Nicotine use and its correlates in patients with psychosis. Acta Psychiatr Scand Suppl. 2007;27–32
Taylor AH, et al. The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect and smoking behaviour: a systematic review. Addiction. 2007;102:534–43.
Leucht S, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379:2063–71.
De Hert M, et al. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2012;8:114–26.
Fusar-Poli P, et al. Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies. Neurosci Biobehav Rev. 2013;37:1680–91.
• Young SL, et al. “First do no harm.” A systematic review of the prevalence and management of antipsychotic adverse effects. J Psychopharmacol. 2015;29:353–62. A review discussing the high prevalence of side-effects accompanying antipsychotic medication use, forms of intervention, and future recommendations
Boyda HN, et al. Routine exercise ameliorates the metabolic side-effects of treatment with the atypical antipsychotic drug olanzapine in rats. Int J Neuropsychopharmacol. 2014;17:77–90.
Baptista PP, et al. Physical exercise down-regulated locomotor side effects induced by haloperidol treatment in Wistar rats. Pharmacol Biochem Behav. 2013;104:113–8.
Fusar-Poli P, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220–9.
Koivukangas J, et al. Physical activity and fitness in adolescents at risk for psychosis within the Northern Finland 1986 Birth Cohort. Schizophr Res. 2010;116:152–8.
Deighton S, Addington J. Exercise practices in individuals at clinical high risk of developing psychosis. Early Interv Psychiatry. 2015;9:284–91.
Hodgekins J, et al. Comparing time use in individuals at different stages of psychosis and a non-clinical comparison group. Schizophr Res. 2015;161:188–93.
McGorry PD, et al. Intervention in individuals at ultra-high risk for psychosis: a review and future directions. J Clin Psychiatry. 2009;70:1206–12.
McGorry PD, et al. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatr. 2010;55:486–97.
McGorry PD, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006;40:616–22.
Parker AG, et al. The effectiveness of simple psychological and physical activity interventions for high prevalence mental health problems in young people: a factorial randomised controlled trial. J Affect Disord. 2016;196:200–9.
Parker AG, et al. The effectiveness of simple psychological and exercise interventions for high prevalence mental health problems in young people: a factorial randomised controlled trial. Trials. 2011;12:76.
Soundy A, et al. Barriers to and facilitators of physical activity among persons with schizophrenia: a survey of physical therapists. Psychiatr Serv. 2014;65:693–6.
Vancampfort D, et al. Negative symptoms are associated with lower autonomous motivation towards physical activity in people with schizophrenia. Compr Psychiatry. 2015;56:128–32.
• Firth J, et al. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. 2016;46:1–13. This article demonstrates the benefits of exercise, but also reviews the barriers contributing to exercise intervention participation and adherence
De Herdt A, et al. Social anxiety in physical activity participation in patients with mental illness: a cross-sectional multicenter study. Depress Anxiety. 2013;30:757–62.
Stanton R. Accredited exercise physiologists and the treatment of people with mental illnesses. Clinical Practice. 2013;5–9
Glover CM, et al. Barriers to exercise among people with severe mental illnesses. Psychiatr Rehabil J. 2013;36:45–7.
Leutwyler H, et al. Adherence to a videogame-based physical activity program for older adults with schizophrenia. Games Health J. 2014;3:227–33.
Khan A, et al. What physical activity contexts do adults with psychological distress prefer? J Sci Med Sport. 2013;16:417–21.
• Firth J, et al. The effects and determinants of exercise participation in first-episode psychosis: a qualitative study. BMC Psychiatry. 2016;16:36. This article demonstrates the benefits of exercise, but also reviews the barriers contributing to exercise intervention participation and adherence
Acknowledgements
Dr. Mittal is a consultant with Takeda Pharmaceuticals. No other authors have conflict to disclose. Dr. Mittal was supported by R01MH094650 and R21/R33MH103231.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Mittal is a consultant with Takeda Pharmaceuticals.
Dr. Mittal was supported by R01MH094650 and R21/R33MH103231.
Vijay A. Mittal declares that he has no conflict of interest.
Teresa Vargasa declares that she has no conflict of interest.
Juston Osbornea declares that he has no conflict of interest.
Derek Deane declares that he has no conflict of interest.
Tina Guptae declares that she has no conflict of interest.
Ivanka Ristanovica declares that she has no conflict of interest.
Christine Hooker declares that she has no conflict of interest.
Stewart A. Shankman declares that he has no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Schizophrenia and Other Psychotic Disorders
Rights and permissions
About this article
Cite this article
Mittal, V.A., Vargas, T., Juston Osborne, K. et al. Exercise Treatments for Psychosis: a Review. Curr Treat Options Psych 4, 152–166 (2017). https://doi.org/10.1007/s40501-017-0112-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-017-0112-2